This cohort study uses registry data from Denmark to evaluate the association between discontinuation of long-term statin treatment and major adverse cardiovascular events among individuals aged 75 years or older.
Key Points
Question
Is statin discontinuation associated with a higher rate of major adverse cardiovascular events than statin continuation among older people receiving long-term treatment with statins?
Findings
In this cohort study of 27 463 people treated with statins for primary prevention and 39 955 treated for secondary prevention, statin discontinuation was associated with a significantly higher rate of major adverse cardiovascular events for primary prevention and secondary prevention compared with treatment continuation.
Meaning
In this study, statin discontinuation was associated with a higher rate of cardiovascular events than statin continuation among older people receiving long-term statin treatment, but more definitive evidence is needed.
Abstract
Importance
Statin use is common in older persons. Given uncertainties in ongoing benefit, changes in health status, and shifting goals of care and preferences, statin discontinuation may be considered in some older persons, although there is currently little evidence to guide this decision.
Objective
To evaluate the association between statin discontinuation and the rate of major adverse cardiovascular events (MACE) among people aged 75 years or older who receive long-term statin treatment.
Design, Setting, and Participants
This cohort study included all persons in Denmark aged 75 years or older who were treated with statins for at least 5 consecutive years as of January 1, 2011. Participants were followed up until December 31, 2016. Data were analyzed from July to November, 2020.
Exposure
Statin discontinuation.
Main Outcomes and Measures
Rate of occurrence of MACE and its components (myocardial infarction, ischemic stroke or transient ischemic attack, coronary revascularization, and death due to myocardial infarction or ischemic stroke) in persons continuing statins compared with those discontinuing statins. Confounding adjustment was done using inverse probability of treatment weighting. Analyses were conducted separately for primary prevention (no history of cardiovascular disease) and secondary prevention (history of cardiovascular disease).
Results
The study included 67 418 long-term statin users, including 27 463 in the primary prevention analysis (median age, 79 years [IQR, 77-83 years]; 18 134 [66%] female) and 39 955 in the secondary prevention analysis (median age, 80 years [IQR, 77-84 years]; 18 717 [47%] female). In both primary and secondary prevention analyses, the rate of MACE was higher among persons who discontinued statins compared with those who continued statins. In the primary prevention cohort, the weighted rate difference was 9 per 1000 person-years (95% CI, 5-12 per 1000 person-years) and the adjusted sub–hazard ratio was 1.32 (95% CI, 1.18-1.48), corresponding to 1 excess MACE per 112 persons who discontinued statins per year. In the secondary prevention cohort, the weighted rate difference was 13 per 1000 person-years (95% CI, 8-17 per 1000 person-years) and the adjusted sub–hazard ratio was 1.28 (95% CI, 1.18-1.39), corresponding to 1 excess MACE per 77 persons who discontinued statins per year.
Conclusions and Relevance
In this cohort study, among older adults receiving long-term statin treatment, discontinuation of statins was associated with a higher rate of MACE compared with statin continuation in both the primary and the secondary prevention cohorts. These findings suggest a need for robust evidence from randomized clinical trials.
Introduction
Statins are recommended both in persons with no history of cardiovascular disease who are at moderate or high risk of a future cardiovascular event (primary prevention) and in those with a history of cardiovascular disease, such as prior myocardial infarction (MI) or ischemic stroke (secondary prevention). The prevalence of statin use ranges from approximately 10% to 60% among persons aged 80 years or older depending on the setting.1 People may start taking statins in midlife and continue treatment for many years.2 Over this time, they may develop additional chronic diseases and their goals of care and treatment preferences may change.3,4 As such, guidelines suggest individualized decision-making about statin use in older persons.5,6,7,8,9,10 This can involve consideration of discontinuation, especially in the context of serious illness and frailty.5,7,11,12 Discontinuation of statins appears to be common clinical practice.13 Among older persons, there has been uncertainty about the benefit of statins for primary prevention and for the treatment of frail older persons and those with chronic multimorbidity,5,7,14 although some recent studies15,16,17,18 suggest possible benefit among older persons. There remains limited evidence on the potential effects of discontinuing long-term statin use. Existing studies have been conducted among persons with mean ages in the 60s or 70s19,20,21 and in specific contexts, particularly in palliative care20 and for exclusively or predominantly primary prevention.19,21,22 Given the lack of randomized clinical trials (RCTs) on statin discontinuation, real-world observational data can provide important evidence to support clinical decision-making.23 The aim of our study was to examine the association of statin discontinuation with the rate of major adverse cardiovascular events (MACE) among individuals aged 75 years or older who were prescribed long-term statins for primary and secondary prevention.
Methods
This was a nationwide cohort study in Denmark that compared the incidence of MACE among people aged 75 years or older who discontinued statin therapy with those who continued treatment, with up to 6 years of follow-up. The study was approved by Statistics Denmark, the Danish Data Protection Agency, and the University of Southern Denmark Research and Innovation Organization. Approval from the ethics committee and informed consent was not required according to section 14 of the Act on Research Ethics Review of Health Research Projects24 because the study was based solely on register data. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Data Sources
The data for this study were obtained from the Danish Health Data Authority. We obtained data on redeemed medications from the Danish National Prescription Registry25 and diagnoses from the Danish National Patient Registry, which includes primary and secondary diagnoses for a hospitalization or hospital visit (specialist, hospital-based outpatient care) and procedures.26 Data on cohabitation status, age, and sex were from the Danish Population Registry.27 Information on deaths was obtained from the Danish Register of Causes of Death.28
Population
The population of interest was all Danish residents aged 75 years or older who received long-term statin treatment as of January 1, 2011, defined as persons who had filled at least 1 statin prescription annually between January 1, 2006, and December 31, 2010, and had a medication possession ratio (MPR) of 70% or greater over this period (the MPR is the ratio of the days’ supply of a medication over a particular period to the number of days in that period).29 Analyses were conducted separately for people treated with statins for secondary prevention (history of cardiovascular disease [January 1, 1995, to December 31, 2010 (baseline)], including MI, ischemic heart disease, angina, peripheral artery disease, ischemic stroke, and transient ischemic attack) and those taking statins for primary prevention (no history of cardiovascular disease).
Exposures
At cohort entry (January 1, 2011), all individuals were assigned to the continuation group (continuers) and contributed time for statin continuation until either discontinuation, death, or the end of the observation period (December 31, 2016). Those who, during follow-up, did not fill another statin prescription during the number of days covered by their previous prescription plus a 180-day grace period were classified as discontinuers. The length of the grace period (180 days) was selected to minimize the risk of exposure misclassification that could arise from irregular drug filling patterns and was based on previous exploratory work.30 Individuals were assigned to the discontinuation group on the day after the end of the grace period and contributed time to the discontinuation group until either statin therapy reinitiation (on the day of refill), death, or December 31, 2016.
Outcomes
The primary outcome was MACE, a composite of MI, ischemic stroke or transient ischemic attack, coronary revascularization procedure (percutaneous coronary intervention and/or coronary artery bypass graft),31 or death from myocardial infarction or ischemic stroke as underlying cause of death). Each of these 4 individual events were defined as secondary outcomes. Follow-up began on June 30, 2011, corresponding to January 1, 2011, plus 180 days, because people could only be classified as discontinuers after a 180-day grace period. People could only experience the first event for each type of secondary outcome, but individuals who experienced 1 type of event (other than death) were still followed up for other types of secondary outcomes. Death from any cause other than MI or ischemic stroke was treated as a competing event.32,33
Statistical Analysis
Data were analyzed from July to November, 2020. We reported crude incidence rates and rate differences per 1000 person-years for all outcomes. To adjust for measured differences between statin continuers and discontinuers, we first calculated propensity scores at cohort entry (January 1, 2011) based on age, sex, cohabitation status, statin intensity, number of medications, chronic comorbidities, and concomitant medications (eTables 1-4 and eFigure 1 in the Supplement). Propensity score distribution curves were used to evaluate the degree of conditional exchangeability (eFigures 2 and 3 in the Supplement).34 We then used inverse probability treatment weighting with stabilized weights to create a pseudo-population in which statin discontinuation was independent of measured covariates.35 Covariate balance in the weighted cohorts was evaluated using standardized mean differences (eTables 5 and 6 in the Supplement).36 We used competing-risk regression models (Fine-Gray subdistribution hazard models) to evaluate outcomes, which incorporated the competing risk of death from causes other than MI or stroke. The relative difference in occurrence of outcomes between groups was thereafter estimated as propensity score–weighted sub–hazard ratios (HRs) with 95% CIs.37 Analyses were performed using Stata, version 16 (StataCorp LLC).
We conducted prespecified sensitivity analyses (eTables 7-12 in the Supplement) by varying the definition of prevalent use (increasing the MPR requirement to ≥80% and ≥90% and removing the MPR requirement). We also shortened the grace period used to define discontinuation (from 180 to 30 and 90 days). Furthermore, we adjusted for confounding using high-dimensional propensity scores based on age, sex, statin intensity, cohabitation status, and the 500 most common diagnoses and drugs.38,39 Finally, we calculated the E-value40 for MACE in the main analysis, to identify the influence of unmeasured confounders in our analysis. The E-value is the minimum strength of association that an unmeasured confounder would need to have with both the treatment (statin discontinuation) and the outcome to fully explain away the observed association between the treatment and outcome after adjustment for the measured covariates.40 In nonprespecified post hoc analyses (eTables 13-20 in the Supplement), we analyzed percutaneous coronary intervention and coronary artery bypass graft separately. We also compared the incidence of general practitioner visits and incidence of mortality from causes other than MI or stroke in the discontinuation and continuation groups, described use of other cardiovascular medications leading to statin discontinuation, and calculated the annual incidence of MACE. We conducted nonprespecified post hoc analyses for all-cause mortality (using a Cox proportional hazards regression model), noncardiovascular mortality, and a negative control outcome (hip fracture) using the same parameters as in the main analysis. Finally, we stratified analyses by sex.
Results
Characteristics of the Cohorts
We identified a total of 67 418 long-term statin users as of January 1, 2011. This included 27 463 (41%) persons without a history of cardiovascular disease (primary prevention) and 39 955 (59%) with a history of cardiovascular disease (secondary prevention). In the primary prevention cohort, the median age was 79 years (IQR, 77-83 years), and 18 134 persons (66%) were female. In the secondary prevention cohort, the median age was 80 years (IQR, 77-84 years), and 18 717 persons (47%) were female. The median duration of follow-up in the main analysis was 5.5 years (IQR, 2.8-5.5 years) in the primary prevention cohort and 4.2 years (IQR, 1.8-5.5 years) in the secondary prevention cohort. The discontinuation rate over the follow-up period the primary prevention cohort was 30% (89 311 of 279 463 persons) and in the secondary prevention cohort was 25% (9 853 of 39 955 persons). In the primary prevention group, 3085 discontinuers (37%) were censored for restarting statins, and in the secondary prevention group, 3541 (36%) were censored for restarting. Table 1 and Table 2 show full details of the study population, including comorbidities and coprescriptions.
Table 1. Baseline Characteristics of the Primary Prevention Cohort.
| Characteristic | Individuals, No. (%) | ||||
|---|---|---|---|---|---|
| Overall (N = 27 463) | Before weighting | After weighting | |||
| Discontinuation group (n = 8311) | Continuation group (n = 19 152) | Discontinuation group (n = 8310) | Continuation group (n = 19 153) | ||
| Sex | |||||
| Female | 18 134 (66.0) | 5854 (70.4) | 12 280 (64.1) | 5487 (66.0) | 12 648 (66.0) |
| Male | 9329 (34.0) | 2457 (29.6) | 6872 (35.9) | 2823 (34.0) | 6506 (34.0) |
| Age, y | |||||
| Median (IQR) | 79 (77-83) | 80 (77-83) | 79 (76-82) | 79 (77-83) | 79 (77-83) |
| 75-84 | 23 233 (84.6) | 6704 (80.7) | 16 529 (86.3) | 7049 (84.8) | 16 169 (84.4) |
| ≥85 | 4230 (15.4) | 1607 (19.3) | 2623 (13.7) | 1261 (15.2) | 2984 (15.6) |
| Statin intensity | |||||
| Low or moderate | 26 408 (96.2) | 8027 (96.6) | 18 381 (96.0) | 7995 (96.2) | 18 420 (96.2) |
| High | 1055 (3.8) | 284 (3.4) | 771 (4.0) | 315 (3.8) | 734 (3.8) |
| Unique medications | |||||
| Median (IQR) | 6 (4-9) | 6 (4-8) | 6 (4-9) | 6 (4-9) | 6 (4-9) |
| 0-4 | 8885 (32.4) | 2866 (34.5) | 6019 (31.4) | 2691 (32.4) | 6172 (32.2) |
| 5-9 | 13 366 (48.7) | 3935 (47.3) | 9431 (49.2) | 4006 (48.2) | 9352 (48.8) |
| ≥10 | 5212 (19.0) | 1510 (18.2) | 3702 (19.3) | 1613 (19.4) | 3629 (18.9) |
| Comorbidities | |||||
| Dementia | 2858 (10.4) | 1098 (13.2) | 1760 (9.2) | 870 (10.5) | 1999 (10.4) |
| Diabetes | 9524 (34.7) | 2539 (30.5) | 6985 (36.5) | 2885 (34.7) | 6643 (34.7) |
| Atrial fibrillation or flutter | 2819 (10.3) | 777 (9.3) | 2042 (10.7) | 853 (10.3) | 1967 (10.3) |
| Heart failure | 1186 (4.3) | 337 (4.1) | 849 (4.4) | 361 (4.3) | 829 (4.3) |
| Hypertension | 9347 (34.0) | 2752 (33.1) | 6595 (34.4) | 2845 (34.2) | 6528 (34.1) |
| Parkinson disease | 196 (0.7) | 75 (0.9) | 121 (0.6) | 60 (0.7) | 137 (0.7) |
| COPD | 5691 (20.7) | 1730 (20.8) | 3961 (20.7) | 1722 (20.7) | 3970 (20.7) |
| Depression | 565 (2.1) | 189 (2.3) | 376 (2.0) | 174 (2.1) | 396 (2.1) |
| Schizophrenia | NR | NR | NR | NR | NR |
| Cancer | 4687 (17.1) | 1399 (16.8) | 3288 (17.2) | 1420 (17.1) | 3269 (17.1) |
| Medications | |||||
| Low-dose aspirin | 12 480 (45.4) | 3549 (42.7) | 8931 (46.6) | 3785 (45.5) | 8708 (45.5) |
| ADP receptor inhibitors | 297 (1.1) | 93 (1.1) | 204 (1.1) | 90 (1.1) | 208 (1.1) |
| Anticoagulants | 2304 (8.4) | 583 (7.0) | 1721 (9.0) | 695 (8.4) | 1608 (8.4) |
| Thiazides | 7796 (28.4) | 2314 (27.8) | 5482 (28.6) | 2360 (28.4) | 5437 (28.4) |
| Spironolactone | 901 (3.3) | 256 (3.1) | 645 (3.4) | 270 (3.2) | 627 (3.3) |
| β blockers | 7432 (27.1) | 2063 (24.8) | 5369 (28.0) | 2244 (27.0) | 5180 (27.0) |
| ACEIs or ARBs | 16 297 (59.3) | 4651 (56.0) | 11 646 (60.8) | 4936 (59.4) | 11 368 (59.4) |
| CCBs | 10 122 (36.9) | 2849 (34.3) | 7273 (38.0) | 3070 (36.9) | 7064 (36.9) |
| Antidepressants | 4374 (15.9) | 1369 (16.5) | 3005 (15.7) | 1331 (16.0) | 3058 (16.0) |
| Antipsychotics | 678 (2.5) | 194 (2.3) | 484 (2.5) | 207 (2.5) | 474 (2.5) |
| NSAIDs (nonselective) | 3789 (13.8) | 1163 (14.0) | 2626 (13.7) | 1148 (13.8) | 2642 (13.8) |
| COX-2 inhibitors | 38 (0.1) | 10 (0.1) | 28 (0.1) | 11 (0.1) | 26 (0.1) |
| Cohabitation status | |||||
| Alone | 12 559 (45.7) | 3603 (43.4) | 8956 (46.8) | 3794 (45.7) | 8753 (45.7) |
| Cohabiting | 14 904 (54.3) | 4708 (56.6) | 10 196 (53.2) | 4516 (54.3) | 10 400 (54.3) |
Abbreviations: ACEIs, angiotensin converting enzyme inhibitors; ADP, adenosine diphosphate receptor; ARBs, angiotensin receptor blockers; CCB, calcium channel blocker; COPD, chronic obstructive pulmonary disease; COX-2, cyclooxygenase-2; NR, not reported (numbers were <10); NSAIDs, non-steroidal anti-inflammatory drugs.
Table 2. Baseline Characteristics of the Secondary Prevention Cohort.
| Characteristic | Individuals, No. (%) | ||||
|---|---|---|---|---|---|
| Overall (N = 39 955) | Before weighting | After weighting | |||
| Discontinuation group (n = 9853) | Continuation group (n = 30 102) | Discontinuation group (n = 9855) | Continuation group (n = 30 102) | ||
| Sex | |||||
| Female | 18 717 (46.8) | 5261 (53.4) | 13 456 (44.7) | 4606 (46.7) | 14 098 (46.8) |
| Male | 21 238 (53.2) | 4592 (46.6) | 16 646 (55.3) | 5249 (53.3) | 16 005 (53.2) |
| Age, y | |||||
| Median (IQR) | 80 (77-84) | 81 (78-85) | 80 (77-83) | 80 (77-84) | 80 (77-84) |
| 75-84 | 31 931 (79.9) | 7372 (74.8) | 24 559 (81.6) | 7837 (79.5) | 24 109 (80.1) |
| ≥85 | 8024 (20.1) | 2481 (25.2) | 5543 (18.4) | 2018 (20.5) | 5993 (19.9) |
| Statin intensity | |||||
| Low or moderate | 37 469 (93.8) | 9376 (95.2) | 28 093 (93.3) | 9239 (93.7) | 28 229 (93.8) |
| High | 2486 (6.2) | 477 (4.8) | 2009 (6.7) | 616 (6.3) | 1873 (6.2) |
| Unique medications | |||||
| Median (IQR) | 8 (5-11) | 8 (5-11) | 8 (5-11) | 8 (5-11) | 8 (5-11) |
| 0-4 | 6905 (17.3) | 1855 (18.8) | 5050 (16.8) | 1732 (17.6) | 5162 (17.1) |
| 5-9 | 19 605 (49.1) | 4795 (48.7) | 14 810 (49.2) | 4770 (48.4) | 14 845 (49.3) |
| ≥10 | 13 445 (33.7) | 3203 (32.5) | 10 242 (34.0) | 3354 (34.0) | 10 095 (33.5) |
| Comorbidities | |||||
| Dementia | 4108 (10.3) | 1313 (13.3) | 2795 (9.3) | 1022 (10.4) | 3102 (10.3) |
| Diabetes | 11 702 (29.3) | 2575 (26.1) | 9127 (30.3) | 2900 (29.4) | 8822 (29.3) |
| Atrial fibrillation or flutter | 9079 (22.7) | 2077 (21.1) | 7002 (23.3) | 2267 (23.0) | 6849 (22.8) |
| Heart failure | 8373 (21.0) | 1873 (19.0) | 6500 (21.6) | 2076 (21.1) | 6312 (21.0) |
| Hypertension | 21 903 (54.8) | 5344 (54.2) | 16 559 (55.0) | 5401 (54.8) | 16 500 (54.8) |
| Parkinson | 412 (1.0) | 105 (1.1) | 307 (1.0) | 104 (1.1) | 311 (1.0) |
| COPD | 11 286 (28.2) | 2708 (27.5) | 8578 (28.5) | 2800 (28.4) | 8509 (28.3) |
| Depression | 1551 (3.9) | 405 (4.1) | 1146 (3.8) | 384 (3.9) | 1170 (3.9) |
| Schizophrenia | 16 (0.0) | NR | NR | NR | 12 (0.0) |
| Cancer | 7254 (18.2) | 1738 (17.6) | 5516 (18.3) | 1783 (18.1) | 5465 (18.2) |
| Medications | |||||
| Low dose aspirin | 30 562 (76.5) | 7294 (74.0) | 23 268 (77.3) | 7532 (76.4) | 23 021 (76.5) |
| ADP receptor inhibitors | 3263 (8.2) | 700 (7.1) | 2563 (8.5) | 812 (8.2) | 2460 (8.2) |
| Anticoagulants | 5745 (14.4) | 1241 (12.6) | 4504 (15.0) | 1436 (14.6) | 4332 (14.4) |
| Thiazides | 9160 (22.9) | 2279 (23.1) | 6881 (22.9) | 2247 (22.8) | 6897 (22.9) |
| Spironolactone | 2687 (6.7) | 553 (5.6) | 2134 (7.1) | 658 (6.7) | 2024 (6.7) |
| β blockers | 20 849 (52.2) | 4684 (47.5) | 16 165 (53.7) | 5128 (52.0) | 15 701 (52.2) |
| ACEIs or ARBs | 23 018 (57.6) | 5471 (55.5) | 17 547 (58.3) | 5687 (57.7) | 17 341 (57.6) |
| CCBs | 14 505 (36.3) | 3454 (35.1) | 11 051 (36.7) | 3572 (36.2) | 10 930 (36.3) |
| Antidepressants | 7958 (19.9) | 2001 (20.3) | 5957 (19.8) | 1954 (19.8) | 5992 (19.9) |
| Antipsychotics | 1007 (2.5) | 251 (2.5) | 756 (2.5) | 254 (2.6) | 761 (2.5) |
| NSAIDs (nonselective) | 4697 (11.8) | 1220 (12.4) | 3477 (11.6) | 1154 (11.7) | 3538 (11.8) |
| COX-2 inhibitors | 50 (0.1) | 12 (0.1) | 38 (0.1) | 12 (0.1) | 38 (0.1) |
| Cohabitation status | |||||
| Alone | 19 571 (49.0) | 4483 (45.5) | 15 088 (50.1) | 4836 (49.1) | 14 748 (49.0) |
| Cohabitating | 20 384 (51.0) | 5370 (54.5) | 15 014 (49.9) | 5019 (50.9) | 15 355 (51.0) |
Abbreviations: ACEIs, angiotensin converting enzyme inhibitors; ADP, adenosine diphosphate receptor; ARBs, angiotensin receptor blockers; COPD, chronic obstructive pulmonary disease; CCB, calcium channel blocker; COX-2, cyclooxygenase-2; NR, not reported (numbers were <10); NSAIDs, non-steroidal anti-inflammatory drugs.
Primary Prevention Cohort
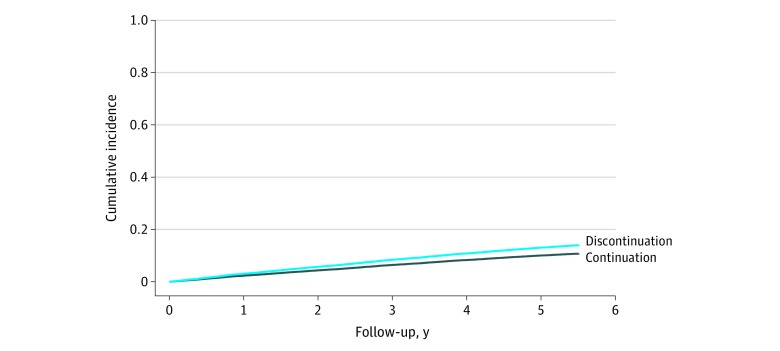
In the primary prevention cohort, the crude incidence rate of MACE was 33 per 1000 person-years (95% CI, 30-36 per 1000 person-years) in the discontinuation group and 24 per 1000 person-years (95% CI, 23-25 per 1000 person-years) in the continuation group (Table 3 and Figure 1). The crude difference in the rate of MACE was 9 per 1000 person-years (95% CI, 5-12 per 1000 person-years), and the weighted rate difference was 9 per 1000 person-years (95% CI, 5-12 per 1000 person-years), corresponding to 1 excess MACE per 112 discontinuers per year. The rate of occurrence of MACE was higher in the discontinuation group than in the continuation group (HR, 1.32; 95% CI 1.18-1.48). The rates of occurrence of MI (HR, 1.37; 95% CI, 1.11-1.70), ischemic stroke or transient ischemic attack (HR, 1.33; 95% CI, 1.14-1.54), and death due to MI or stroke (HR, 1.43; 95% CI, 1.11-1.85) were higher in the discontinuation group than in the continuation group, and there was no significant difference in the rate of occurrence of revascularization (HR, 1.12; 95% CI, 0.82-1.52) (Table 3).
Table 3. Summary of Results for the Primary and Secondary Prevention Cohorts.
| Outcome | Discontinuation group | Continuation group | Crude rate difference, per 1000 person-years (95% CI) | Weighted rate difference, per 1000 person-years (95% CI)a | Sub–hazard ratio (95% CI)a | ||
|---|---|---|---|---|---|---|---|
| Crude events | Crude incidence rate, per 1000 person-years (95% CI) | Crude events | Crude incidence rate, per 1000 person-years (95% CI) | ||||
| Primary prevention | |||||||
| Person-years of follow-upb | 11 709 | NA | 103 664 | NA | NA | NA | NA |
| MACE | 382 | 33 (30 to 36) | 2481 | 24 (23 to 25) | 9 (5 to 12) | 9 (5 to 12) | 1.32 (1.18 to 1.48) |
| MI | 105 | 9 (7 to 11) | 692 | 6 (6 to 7) | 2 (0 to 4) | 2 (1 to 4) | 1.37 (1.11 to 1.70) |
| Stroke | 230 | 19 (17 to 22) | 1390 | 13 (13 to 14) | 6 (4 to 9) | 6 (3 to 8) | 1.33 (1.14 to 1.54) |
| Revascularization procedure | 47 | 4 (3 to 5) | 477 | 4 (4 to 5) | −1 (−2 to 1) | 0 (−1 to 2) | 1.12 (0.82 to 1.52) |
| Death from MI or stroke | 76 | 6 (5 to 8) | 433 | 4 (4 to 4) | 2 (1 to 4) | 2 (1 to 4) | 1.43 (1.11 to 1.85) |
| Secondary prevention | |||||||
| Person-years of follow-upb | 12 350 | NA | 133 374 | NA | NA | NA | NA |
| MACE | 739 | 60 (56 to 64) | 6472 | 49 (47 to 50) | 11 (7 to 16) | 13 (8 to 17) | 1.28 (1.18 to 1.39) |
| MI | 248 | 19 (17 to 21) | 2326 | 17 (16 to 17) | 2 (−0 to 5) | 4 (1 to 6) | 1.25 (1.09 to 1.43) |
| Stroke | 382 | 30 (27 to 33) | 2953 | 21 (21 to 22) | 8 (5 to 12) | 8 (5 to 11) | 1.34 (1.20 to 1.50) |
| Revascularization procedure | 74 | 6 (4 to 7) | 1416 | 10 (10 to 11) | −5 (−6 to −3) | −3 (−5 to −2) | 0.73 (0.57 to 0.93) |
| Death from MI or stroke | 211 | 16 (14 to 18) | 1387 | 10 (9 to 10) | 6 (4 to 8) | 6 (4 to 8) | 1.57 (1.35 to 1.83) |
Abbreviations: MACE, major adverse cardiovascular events; MI, myocardial infarction; NA, not applicable.
Adjusted estimates were obtained using an inverse probability of treatment weighted pseudo-population with stabilized weights. Weights incorporated propensity scores calculated from baseline age, sex, number of concomitant medications, individual medications, comorbidities, statin intensity, and cohabitation status.
Person-years of follow-up for MACE outcome.
Figure 1. Cumulative Incidence Curve for the Outcome of Major Adverse Cardiovascular Events in the Primary Prevention Cohort.
Secondary Prevention Cohort
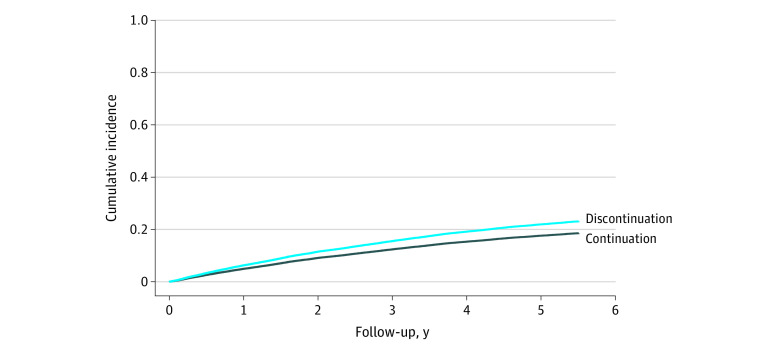
In the secondary prevention cohort, the crude incidence rate of MACE was 60 per 1000 person-years (95% CI, 56-64 per 1000 person-years) in the discontinuation group and 49 per 1000 person-years (95% CI, 47-50 per 1000 person-years) in the continuation group (Table 3 and Figure 2). The crude difference in the rate of MACE was 11 per 1000 person-years (95% CI, 7-16 per 1000 person-years), and the weighted rate difference was 13 per 1000 person-years (95% CI, 8-17 per 1000 person-years), corresponding to 1 excess MACE per 77 discontinuers per year. The rate of occurrence of MACE was higher in the discontinuation group than in the continuation group (HR, 1.28; 95% CI, 1.18-1.39). The rates of occurrence of MI (HR, 1.25; 95% CI, 1.09-1.43), ischemic stroke or transient ischemic attack (HR, 1.34; 95% CI, 1.20-1.50), and death due to MI or stroke (HR, 1.57; 95% CI, 1.35-1.83) were higher in the discontinuation group than in the continuation group (Table 3). The rate of occurrence of revascularization was lower in the discontinuation group (HR, 0.73; 95% CI, 0.57-0.93), which was attributable to a lower rate of coronary artery bypass graft (eTable 13 in the Supplement).
Figure 2. Cumulative Incidence Curve for the Outcome of Major Adverse Cardiovascular Events in the Secondary Prevention Cohort.
Supplementary Analyses
The results of all supplementary and post hoc analyses are given in eTables 7 to 20 in the Supplement. In the primary prevention cohort, modifying the grace period for discontinuation, changing the MPR requirement to 80% or removing it completely, or using high-dimensional propensity score had little effect on the results (eTables 7-12 in the Supplement). However, increasing the MPR requirement to 90% before cohort entry lowered the adjusted HR for MACE to 1.21 (95% CI, 1.04-1.39). Decreasing the grace period to 30 days led to a nonsignificant decrease in HR for revascularizations (0.77; 95% CI, 0.53-1.11) but a higher HR for death due to MI or stroke (HR, 1.98; 95% CI, 1.44-2.72). The E-value for MACE in the main analysis was 1.97, indicating that an unmeasured confounder would need to be associated with discontinuation and MACE by approximately 2-fold beyond the measured confounders to fully explain away our results.
In the secondary prevention cohort, post hoc analyses showed a lower rate of coronary artery bypass graft but a higher rate of percutaneous coronary intervention in the discontinuation group compared with the continuation group; however, neither difference was statistically significant (eTable 13 in the Supplement). Modifying the MPR requirement or using a high-dimensional propensity score did not substantially alter our results (eTables 7-12 in the Supplement). The E-value for MACE in the main analysis was 1.88.
In our post hoc analyses, statin discontinuation was associated with a higher rate of all-cause mortality and noncardiovascular mortality (eTable 18 in the Supplement). In our negative control outcome analysis (eTable 19 in the Supplement), statin discontinuation was associated with a higher rate of hip fracture in both the primary and the secondary prevention cohorts. In the sex-stratified analyses (eTable 20 in the Supplement), discontinuation of statin therapy prescribed for primary prevention was associated with a slightly higher absolute rate of MACE in men compared with women, whereas the rates in the secondary prevention cohort were similar between men and women.
Discussion
In this cohort study, statin discontinuation was associated with a higher rate of occurrence of MACE compared with statin continuation among older people receiving long-term statin treatment for both primary and secondary prevention. Although the relative effect estimates for statin discontinuation were similar in both cohorts, the overall rate of cardiovascular events and the magnitude of the rate difference between discontinuation and continuation were higher in the secondary prevention cohort than among statin users without a history of cardiovascular disease.
Comparison to Existing Literature
Few studies have explored the effects of statin discontinuation in older persons. One RCT demonstrated that, among patients with advanced illness and a physician-estimated life expectancy of less than a year, statin discontinuation did not increase risk of mortality over 60 days.20 Although useful, that study did not inform clinical decision-making for older adults who are, in general, not nearing the end of life.
In a recent observational study conducted in France19 that included older persons aged 75 years with no history of cardiovascular disease, statin discontinuation was associated with an increased risk of hospitalizations for cardiovascular events during the 2.5-year follow-up (HR, 1.33; 95% CI, 1.18-1.50). Rea et al22 also reported that statin discontinuation was associated with an increased risk of cardiovascular events (HR, 1.14; 95% CI, 1.03-1.26) in a predominantly primary prevention population. Our findings about the association between statin discontinuation and the rate of MACE cannot be directly compared with evidence on statin initiation during older age; our study included long-term statin users (who are not fully comparable to treatment-naive patients), and the time to benefit associated with initiating therapy may be substantially longer than the time to harm associated with withdrawing that same medication. Furthermore, long-term statin use may have a substantial treatment benefit that persists after a trial has ended (ie, legacy benefit), as suggested by a recent meta-analysis of RCTs.41
Survey studies and qualitative literature suggest that patient preferences, physical frailty, and remaining life expectancy can influence prescribers’ decisions about statin discontinuation.42,43 Therefore, confounding by indication and prognosis bias are 2 important concerns in drug discontinuation studies relying on observational data. For instance, statin discontinuation may reflect an overall preference for less medical care and a willingness to shift from preventive or curative goals of care to a more palliative approach. Poor health and severe frailty may also be associated with an increased likelihood of statin discontinuation43,44 and with a reduced likelihood of receiving revascularization procedures, particularly coronary artery bypass graft.45,46,47 Our post hoc analyses support this hypothesis because we found a lower rate of coronary artery bypass graft in the discontinuation group than in the continuation group, especially in the secondary prevention cohort. The finding that statin discontinuation was associated with a higher risk of hip fracture (negative control analysis) and with higher rates of all-cause and noncardiovascular mortality also support the hypothesis that statin discontinuation is a marker of frailty and poorer health in general.
Implications and Future Research
Our results provide important evidence on statin discontinuation in people receiving long-term statin treatment for both primary and secondary prevention. Clinicians and policy makers should be aware of a possible increased risk of MACE associated with discontinuation of long-term statin treatment. This finding may be of clinical and public health importance because of the magnitude of excess risk (1 excess MACE per 112 discontinuers per year in the primary prevention cohort and 1 MACE per 77 discontinuers per year in the secondary prevention cohort). Consideration of absolute risk is particularly important for shared decision-making in the context of statin use for individual patients.
Statin discontinuation occurs frequently in practice,1 and thus evidence to inform shared decision-making on this topic may be useful to clinicians. Our findings of a higher rate of cardiovascular events among those discontinuing statins, along with the findings of previous studies,19,22 highlight the importance of RCTs on this topic. To our knowledge, there is currently only 1 RCT23 that has investigated the effects of statin discontinuation for primary prevention among persons aged 75 years or older. Additional RCTs investigating statin initiation in primary prevention for older persons are also ongoing and should provide additional context about statins in this population.48,49
Limitations
This study has limitations. First, no data were available about the specific reasons that prompted statin discontinuation. The discontinuation patterns that we captured in the data may represent either a purposeful and planned deprescribing process or patients stopping therapy on their own without consulting a health care professional. Second, we did not incorporate time-varying confounding into our analysis. Cardiovascular medications may have changed during the study period, or people may have developed additional comorbidities that may have influenced statin discontinuation and the risk of acute cardiovascular outcomes. Third, statin exposure was defined based on redeemed prescriptions only. Unmeasured confounding is a concern in any non-RCT. However, the sensitivity analysis using the high-dimensional propensity score (adjusting for the 500 most common medications and comorbidities) did not change the results. We could only incorporate potential confounders available to us in Danish registers and thus could not include lifestyle factors, patient preferences, and other potential confounders. Frailty may be a particularly relevant confounder. A negative control outcome analysis revealed an association of statin discontinuation with hip fracture, highlighting that discontinuation may be a marker of frailty in general. However, an E-value for 2 of the main analyses suggested that an unmeasured confounder would need to be associated with discontinuation and with MACE by 2-fold each beyond the measured confounders to explain away our results.40 The validity of cardiovascular diagnosis and procedure codes is another potential consideration; however, the validity of cardiovascular diagnosis50 and procedure codes31 has been demonstrated to be excellent in Danish health registers. Thus, we do not believe that this affected our results. In addition, our post hoc analyses of all-cause mortality and noncardiovascular mortality should be interpreted with caution because these outcomes are particularly prone to confounding by indication and thus were not selected as prespecified outcomes.
Conclusions
In this cohort study, among older Danes receiving long-term statin treatment, discontinuation was associated with a higher rate of MACE compared with statin continuation. Although the relative effect of statin discontinuation was similar in the primary and secondary prevention cohorts, the rate difference was larger in the secondary prevention cohort. These findings suggest a need for further evidence from RCTs on this topic to inform shared decision-making in clinical practice.
eTable 1. Anatomical Therapeutic Chemical codes used in the study
eTable 2. International Classification of Diseases codes used in the study
eTable 3. Surgical procedure codes used in the study
eTable 4. Statin intensity (based on American College of Cardiologists 2018 guidelines)
eFigure 1. Cohort design
eFigure 2. Propensity score distribution in the primary prevention cohort
eFigure 3. Propensity score distribution in the secondary prevention cohort
eTable 5. Balance of covariates in primary prevention cohort
eTable 6. Balance of covariates in secondary prevention cohort
eTable 7. Summary of results with grace period of 90 days
eTable 8. Summary of results with grace period of 30 days
eTable 9. Summary of results with medication possession ratio threshold of ≥80%
eTable 10. Summary of results with medication possession ratio threshold of ≥90%
eTable 11. Summary of results with no medication possession ratio threshold
eTable 12. Summary of results using high dimensional propensity score in inverse probability of treatment weighting procedure
eTable 13. Revascularization outcome broken down by PCI and CABG
eTable 14. General Practitioner (GP) contacts each year of follow-up
eTable 15. Crude incidence of mortality for causes other than MI and ischemic stroke
eTable 16. Other cardiovascular medication use approaching statin discontinuation date in statin discontinuation group
eTable 17. Crude incidence of MACE each year of follow-up
eTable 18. Summary of results for all-cause and non-cardiovascular mortality
eTable 19. Summary of results for negative control outcome (hip fracture)
eTable 20. Summary of results sex-stratified MACE analysis
References
- 1.Thompson W, Pottegård A, Nielsen JB, Haastrup P, Jarbøl DE. How common is statin use in the oldest old? Drugs Aging. 2018;35(8):679-686. doi: 10.1007/s40266-018-0567-x [DOI] [PubMed] [Google Scholar]
- 2.Gulliford M, Ravindrarajah R, Hamada S, Jackson S, Charlton J. Inception and deprescribing of statins in people aged over 80 years: cohort study. Age Ageing. 2017;46(6):1001-1005. doi: 10.1093/ageing/afx100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hilmer SN, McLachlan AJ, Le Couteur DG. Clinical pharmacology in the geriatric patient. Fundam Clin Pharmacol. 2007;21(3):217-230. doi: 10.1111/j.1472-8206.2007.00473.x [DOI] [PubMed] [Google Scholar]
- 4.Holmes HM, Hayley DC, Alexander GC, Sachs GA. Reconsidering medication appropriateness for patients late in life. Arch Intern Med. 2006;166(6):605-609. doi: 10.1001/archinte.166.6.605 [DOI] [PubMed] [Google Scholar]
- 5.Hawley CE, Roefaro J, Forman DE, Orkaby AR. Statins for primary prevention in those aged 70 years and older: a critical review of recent cholesterol guidelines. Drugs Aging. 2019;36(8):687-699. doi: 10.1007/s40266-019-00673-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Strandberg TE, Kolehmainen L, Vuorio A. Evaluation and treatment of older patients with hypercholesterolemia: a clinical review. JAMA. 2014;312(11):1136-1144. doi: 10.1001/jama.2014.10924 [DOI] [PubMed] [Google Scholar]
- 7.Krishnaswami A, Steinman MA, Goyal P, et al. ; Geriatric Cardiology Section Leadership Council, American College of Cardiology . Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol. 2019;73(20):2584-2595. doi: 10.1016/j.jacc.2019.03.467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Ploeg MA, Floriani C, Achterberg WP, et al. Recommendations for (discontinuation of) statin treatment in older adults: review of guidelines. J Am Geriatr Soc. 2020;68(2):417-425. Published online October 30, 2019. doi: 10.1111/jgs.16219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boyd C, Smith CD, Masoudi FA, et al. Decision making for older adults with multiple chronic conditions: executive summary for the American Geriatrics Society Guiding Principles on the Care of Older Adults With Multimorbidity. J Am Geriatr Soc. 2019;67(4):665-673. doi: 10.1111/jgs.15809 [DOI] [PubMed] [Google Scholar]
- 10.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25). [DOI] [PMC free article] [PubMed]
- 11.van Middelaar T, Moll van Charante EP. Deprescribing preventive medication in older patients. Br J Gen Pract. 2018;68(675):456-457. doi: 10.3399/bjgp18X698933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yourman LC, Cenzer IS, Boscardin WJ, et al. Evaluation of time to benefit of statins for the primary prevention of cardiovascular events in adults aged 50 to 75 years: a meta-analysis. JAMA Intern Med. 2021;181(2):179-185. doi: 10.1001/jamainternmed.2020.6084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ofori-Asenso R, Jakhu A, Zomer E, et al. Adherence and persistence among statin users aged 65 years and over: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci. 2018;73(6):813-819. doi: 10.1093/gerona/glx169 [DOI] [PubMed] [Google Scholar]
- 14.Strandberg TE. Role of statin therapy in primary prevention of cardiovascular disease in elderly patients. Curr Atheroscler Rep. 2019;21(8):28. doi: 10.1007/s11883-019-0793-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armitage J, Baigent C, Barnes E, et al. ; Cholesterol Treatment Trialists’ Collaboration . Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407-415. doi: 10.1016/S0140-6736(18)31942-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gencer B, Marston NA, Im K, et al. Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2020;396(10263):1637-1643. doi: 10.1016/S0140-6736(20)32332-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orkaby AR, Driver JA, Ho Y-L, et al. Association of statin use with all-cause and cardiovascular mortality in us veterans 75 years and older. JAMA. 2020;324(1):68-78. doi: 10.1001/jama.2020.7848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mortensen MB, Nordestgaard BG. Elevated LDL cholesterol and increased risk of myocardial infarction and atherosclerotic cardiovascular disease in individuals aged 70-100 years: a contemporary primary prevention cohort. Lancet. 2020;396(10263):1644-1652. doi: 10.1016/S0140-6736(20)32233-9 [DOI] [PubMed] [Google Scholar]
- 19.Giral P, Neumann A, Weill A, Coste J. Cardiovascular effect of discontinuing statins for primary prevention at the age of 75 years: a nationwide population-based cohort study in France. Eur Heart J. 2019;40(43):3516-3525. doi: 10.1093/eurheartj/ehz458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kutner JS, Blatchford PJ, Taylor DH Jr, et al. Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med. 2015;175(5):691-700. doi: 10.1001/jamainternmed.2015.0289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luymes CH, Poortvliet RKE, van Geloven N, et al. Deprescribing preventive cardiovascular medication in patients with predicted low cardiovascular disease risk in general practice—the ECSTATIC study: a cluster randomised non-inferiority trial. BMC Med. 2018;16(1):5. doi: 10.1186/s12916-017-0988-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rea F, Biffi A, Ronco R, et al. Cardiovascular outcomes and mortality associated with discontinuing statins in older patients receiving polypharmacy. JAMA Netw Open. 2021;4(6):e2113186. doi: 10.1001/jamanetworkopen.2021.13186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benard A. Statins in the elderly (SITE). Published 2020. Accessed November 24, 2020. https://clinicaltrials.gov/ct2/show/NCT02547883
- 24.National Committee on Health Research Ethics. Act on Research Ethics Review of Health Research Projects. Accessed October 27, 2021. https://en.nvk.dk/rules-and-guidelines/act-on-research-ethics-review-of-health-research-projects
- 25.Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M. Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol. 2016;dyw213. doi: 10.1093/ije/dyw213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. Published online November 2015:449. doi: 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed]
- 27.Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541-549. doi: 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 28.Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39(7)(suppl):26-29. doi: 10.1177/1403494811399958 [DOI] [PubMed] [Google Scholar]
- 29.Elseviers M, Wettermark B, Almarsdóttir AB, et al. , eds. Drug Utilization Research. John Wiley & Sons, Ltd; 2016. doi: 10.1002/9781118949740 [DOI] [Google Scholar]
- 30.Thompson W, Jarbøl DE, Nielsen JB, Haastrup P, Pottegård A. Statin use and discontinuation in Danes age 70 and older: a nationwide drug utilisation study. Age Ageing. 2021;50(2):554-558. doi: 10.1093/ageing/afaa160 [DOI] [PubMed] [Google Scholar]
- 31.Adelborg K, Sundbøll J, Munch T, et al. Positive predictive value of cardiac examination, procedure and surgery codes in the Danish National Patient Registry: a population-based validation study. BMJ Open. 2016;6(12):e012817. doi: 10.1136/bmjopen-2016-012817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdel-Qadir H, Fang J, Lee DS, et al. Importance of Considering Competing Risks in Time-to-Event Analyses: Application to Stroke Risk in a Retrospective Cohort Study of Elderly Patients With Atrial Fibrillation. Circ Cardiovasc Qual Outcomes. 2018;11(7):e004580. doi: 10.1161/CIRCOUTCOMES.118.004580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berry SD, Ngo L, Samelson EJ, Kiel DP. Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc. 2010;58(4):783-787. doi: 10.1111/j.1532-5415.2010.02767.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014;49(5):1701-1720. doi: 10.1111/1475-6773.12182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661-3679. doi: 10.1002/sim.6607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083-3107. doi: 10.1002/sim.3697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Austin PC, Fine JP. Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med. 2017;36(27):4391-4400. doi: 10.1002/sim.7501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hallas J, Pottegård A. Performance of the High-dimensional Propensity Score in a Nordic Healthcare Model. Basic Clin Pharmacol Toxicol. 2017;120(3):312-317. doi: 10.1111/bcpt.12716 [DOI] [PubMed] [Google Scholar]
- 39.Austin PC, Wu CF, Lee DS, Tu JV. Comparing the high-dimensional propensity score for use with administrative data with propensity scores derived from high-quality clinical data. Stat Methods Med Res. 2020;29(2):568-588. doi: 10.1177/0962280219842362 [DOI] [PubMed] [Google Scholar]
- 40.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the e-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 41.Nayak A, Hayen A, Zhu L, et al. Legacy effects of statins on cardiovascular and all-cause mortality: a meta-analysis. BMJ Open. 2018;8(9):e020584. doi: 10.1136/bmjopen-2017-020584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goyal P, Anderson TS, Bernacki GM, et al. Physician perspectives on deprescribing cardiovascular medications for older adults. J Am Geriatr Soc. 2020;68(1):78-86. doi: 10.1111/jgs.16157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van der Ploeg MA, Streit S, Achterberg WP, et al. Patient characteristics and general practitioners’ advice to stop statins in oldest-old patients: a survey study across 30 countries. J Gen Intern Med. 2019;34(9):1751-1757. doi: 10.1007/s11606-018-4795-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thompson W, Le JV, Haastrup P, Nielsen JB, Pedersen LB, Jarbøl DE. Exploring how GPs discuss statin deprescribing with older people: a qualitative study. BJGP Open. 2020;4(1):bjgpopen20X101022. doi: 10.3399/bjgpopen20X101022 [DOI] [PMC free article] [PubMed]
- 45.Damluji AA, Huang J, Bandeen-Roche K, et al. Frailty among older adults with acute myocardial infarction and outcomes from percutaneous coronary interventions. J Am Heart Assoc. 2019;8(17):e013686. doi: 10.1161/JAHA.119.013686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O’Brien SM, Feng L, He X, et al. The Society of Thoracic Surgeons 2018 adult cardiac surgery risk models: part 2—statistical methods and results. Ann Thorac Surg. 2018;105(5):1419-1428. doi: 10.1016/j.athoracsur.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 47.De Marzo V, D’amario D, Galli M, Vergallo R, Porto I. High-risk percutaneous coronary intervention: how to define it today? Minerva Cardioangiol. 2018;66(5):576-593. doi: 10.23736/S0026-4725.18.04679-0 [DOI] [PubMed] [Google Scholar]
- 48.A Clinical Trial of Statin Therapy for Reducing Events in the Elderly (STAREE). ClinicalTrials.gov idenitifer: NCT02099123. Accessed November 24, 2020. https://clinicaltrials.gov/ct2/show/NCT02099123
- 49.Pragmatic Evaluation of Events And Benefits of Lipid-lowering in Older Adults (PREVENTABLE). ClinicalTrials.gov identifier: NCT04262206. Accessed November 24, 2020. https://clinicaltrials.gov/ct2/show/NCT04262206
- 50.Sundbøll J, Adelborg K, Munch T, et al. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open. 2016;6(11):e012832. doi: 10.1136/bmjopen-2016-012832 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Anatomical Therapeutic Chemical codes used in the study
eTable 2. International Classification of Diseases codes used in the study
eTable 3. Surgical procedure codes used in the study
eTable 4. Statin intensity (based on American College of Cardiologists 2018 guidelines)
eFigure 1. Cohort design
eFigure 2. Propensity score distribution in the primary prevention cohort
eFigure 3. Propensity score distribution in the secondary prevention cohort
eTable 5. Balance of covariates in primary prevention cohort
eTable 6. Balance of covariates in secondary prevention cohort
eTable 7. Summary of results with grace period of 90 days
eTable 8. Summary of results with grace period of 30 days
eTable 9. Summary of results with medication possession ratio threshold of ≥80%
eTable 10. Summary of results with medication possession ratio threshold of ≥90%
eTable 11. Summary of results with no medication possession ratio threshold
eTable 12. Summary of results using high dimensional propensity score in inverse probability of treatment weighting procedure
eTable 13. Revascularization outcome broken down by PCI and CABG
eTable 14. General Practitioner (GP) contacts each year of follow-up
eTable 15. Crude incidence of mortality for causes other than MI and ischemic stroke
eTable 16. Other cardiovascular medication use approaching statin discontinuation date in statin discontinuation group
eTable 17. Crude incidence of MACE each year of follow-up
eTable 18. Summary of results for all-cause and non-cardiovascular mortality
eTable 19. Summary of results for negative control outcome (hip fracture)
eTable 20. Summary of results sex-stratified MACE analysis