Abstract
Background
The COVID-19 pandemic has hugely impacted upon people’s psychological and physical wellbeing; however, the effects of the COVID-19 lockdown on mothers of young children, with particular regard to breastfeeding, are unknown.
Research Aims
To explore: (1) Sources of advice and support available to breastfeeding mothers during and prior to the COVID-19 lockdown; (2) Mothers’ opinions on statements and recommendations made by the World Health Organization on the importance of breastfeeding and breastfeeding during the COVID-19 pandemic; (3) Maternal emotional states (i.e., anxiety and depression symptoms) experienced by breastfeeding mothers during the COVID-19 lockdown; and (4) influence of breastfeeding duration and number of children on breastfeeding opinions and emotional states.
Methods
Mothers of children aged 0–36 months (N = 4018) took part in an online survey. The survey included demographic questions, as well as the Generalised Anxiety Disorder Questionnaire and the Patient Health Questionnaire. Mothers were further probed on opinions regarding breastfeeding practices during the COVID-19 pandemic.
Results
Participants strongly agreed with the importance of breastfeeding, even if a mother showed symptoms of COVID-19. Differences in opinions on breastfeeding practices (e.g., the use of donor human milk and relactation), were found between participants in relation to breastfeeding duration and number of children. Participants with more than one child showed higher negative emotional states, namely anxiety symptoms. Except for Internet usage, participants indicated a decline in all sources of advice and support for breastfeeding during the COVID-19 lockdown.
Conclusions
Health bodies and professionals should consider maternal viewpoints and opinions regarding breastfeeding during the COVID-19 pandemic. Interventions are urgently needed in order to support breastfeeding mothers and prevent the development of mental health issues.
Keywords: breastfeeding, breastfeeding experience, breastfeeding support, maternal psychology, mental health, COVID-19, COVID-19 lockdown, COVID-19 pandemic
Background
The World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommend mothers to initiate breastfeeding within the first hour after childbirth and exclusively breastfeed an infant for the first 6 months of life, with supplemental breastfeeding continuing for 2 years and beyond (WHO, 2020a; WHO & UNICEF, 2003). In 2003, the Department of Health in the United Kingdom (UK) adopted the WHO recommendations (Scientific Advisory Committee on Nutrition [SACN], 2003), advising mothers to breastfeed their infant for at least 6 months postpartum (National Health Service [NHS], 2020a). A large body of scientific evidence supports the relevance of breastfeeding for the health, development, and growth of an infant (WHO, 2021a). Human milk is the best source of nutrition that an infant may receive (Oddy, 2017) as it contains antibodies (Andreas et al., 2015), enzymes (Di Lauro et al., 2016), and hormones (Hull, 2018).
The results of breastfeeding, however, go beyond infancy; indeed, human milk continues to be rich in proteins, vitamins, and minerals even after 12 months postpartum (Czosnykowska-Łukacka et al., 2018; Perrin et al., 2017). The importance of breastfeeding for both mother and infant are widely known. It has been found that breastfeeding positively influences the child’s health (Pattison et al., 2019); for instance, breastfed infants have had lower incidence of respiratory and urinary infections (Frank et al., 2019), asthma (Klopp et al., 2018), and leukemia (Gao et al., 2019) relative to infants who were not breastfed. Breastfeeding also is beneficial to the mother (National Health Service [NHS], 2020b); for instance, it is associated with lower risk of breast cancer (Unar-Munguía et al., 2017), osteoporosis (Duan et al., 2017), endometrial cancer (Jordan et al., 2017), and cardiovascular disease (Peters et al., 2017).
In addition, breastfeeding assists the development of a positive dyadic relationship, supporting mother–infant bonding (Liu et al., 2014) and may help attachment development via the provision of regular intimate mother–infant interactions (Gibbs et al., 2018). Breastfeeding enhances the psychological wellbeing of both mother and child (Abul-Fadl et al., 2005; Krol & Grossmann, 2018), contributing to the quality of mother–child relationship (Papp, 2014), maternal sensitivity (Weaver et al., 2018), and child secure attachment (Linde et al., 2020). Recently, researchers have further shown that breastfeeding is protective of the quality of maternal caregiving in mothers with depressive symptoms as it influences mother-infant affectionate touch patterns (Hardin et al., 2021). However, researchers have also shown that mothers with depressive symptoms are less likely to initiate and continue breastfeeding than women with no psychopathological symptoms (Mathews et al., 2014). Maternal anxiety has been associated with reduced exclusivity and continuation of breastfeeding (Adedinsewo et al., 2014).
Different factors may influence mothers’ decisions regarding breastfeeding initiation; for instance, care and help provided by health professionals, specifically breastfeeding counsellors in hospital (Meedya et al., 2010), personal and professional support, namely midwives, health visitors, and trained volunteer mothers (peer supporters; Brown et al., 2011; Radzyminski & Callister, 2016), and maternal breastfeeding knowledge (i.e., best nutrition for an infant; Radzyminski & Callister, 2016). Fathers also play an important role; their practical and emotional support has been found to influence mothers’ decisions to initiate and continue breastfeeding (Datta et al., 2012; Rempel et al., 2017). First-time mothers are most likely to initiate breastfeeding if they receive support from their partner (Hinic, 2016) and are able to take part in breastfeeding groups and intervention programs (Liu et al., 2017; Maleki-Saghooni et al., 2020).
Key Messages.
Little is known regarding the impact that the COVID-19 lockdown has had on mothers in the United Kingdom, with regard to breastfeeding support and maternal opinions.
In the scenario of coronavirus symptoms, differences of opinions in relation to breastfeeding duration and number of children were found.
The Internet was the main source of support and advice on breastfeeding that participants used prior to and during the COVID-19 lockdown in the United Kingdom.
Maternal viewpoints and preferences need to be considered by health professionals in order to support breastfeeding mothers during the COVID-19 pandemic.
In the 1990s, the WHO in collaboration with UNICEF established the Baby-Friendly Hospital Initiative (BFHI) to promote breastfeeding and support mothers initiating early and exclusive continued breastfeeding via prompt interventions (i.e., individual counseling or group education; Philipp & Merewood, 2004; WHO, 2021b). In the UK, BFHI has been extensively adopted (Radford, 2001; UNICEF, 2019a); however, despite the importance of breastfeeding for both infant and mother as well as BFHI in UK hospitals, the breastfeeding rate in the UK is rather low in comparison to other European countries (Bagci Bosi et al., 2016).
In recent times, due to the COVID-19 pandemic, the health service in the UK has changed from one-to-one appointments with health professionals to digital health services (Hutchings, 2020); consequently, breastfeeding groups have not been able to support mothers with face-to-face interaction. However, electronic leaflets have been made accessible via the Internet and support via telephone helplines has been available (see UNICEF, 2020). Although Baby Friendly resources on infant feeding have been made available online, several queries regarding breastfeeding practices during the COVID-19 pandemic have been raised (UNICEF, 2020). At present, UNICEF (2020) recommends that:
to facilitate breastfeeding, mothers and babies should be enabled to stay together as much as possible, to have skin-to-skin contact, to feed their baby responsively and to have access to ongoing support when this is needed. When mothers are partially breastfeeding, they can be encouraged to maximise the amount of breastmilk they are able to give or, if they choose, to be supported to return to full breastfeeding. If mothers are considering stopping breastfeeding, it is worth having a sensitive conversation about the value of continuing during the COVID-19 outbreak (p.1)
The impact that the lockdown, and its undeniable challenges, has had on mothers and infants in the UK, with particular regard to breastfeeding practices, is unknown.
Thus, the main aim of this study was to explore maternal emotional states and personal opinions as well as support received during the lockdown in the UK. Due to the impact of breastfeeding experiences on mothers’ infant feeding decisions (DiGirolamo et al., 2005; Huang et al., 2019), the effects of breastfeeding duration and number of children were investigated. More specifically, the current study aimed to explore:
Sources of advice and support available to breastfeeding mothers during and prior to the COVID-19 lockdown.
Mothers’ opinions on statements and recommendations made by the WHO on the importance of breastfeeding and breastfeeding during the COVID-19 pandemic.
Maternal emotional states (i.e., anxiety and depression symptoms) experienced by breastfeeding mothers during the COVID-19 lockdown.
The influence of breastfeeding duration and number of children on breastfeeding opinions and emotional states.
It was predicted that sources of support used by mothers would change as a result of the pandemic, and that breastfeeding opinions and emotional states would vary depending on the current duration of breastfeeding and number of children in the family.
Methods
Research Design
This study was a cross-sectional, prospective online (self-report) survey. Due to the COVID-19 pandemic and social distancing rules, an online self-report survey was used.
This study followed the International Ethics Declaration of Helsinki (World Medical Association [WMA], 2001) and obtained ethical approval from the Psychology Research Ethics Committee, Regent’s University London, UK.
Setting and Relevant Context
Although a high percentage of UK mothers initially breastfeed their infant (NHS, 2015), the UK has one of the lowest breastfeeding rates in Europe (Bagci Bosi et al., 2016). It appears that breastfeeding continuation remains critical (Public Health England, 2016). Increasing breastfeeding practices in the UK would save up to £50 million in NHS expenditure (UNICEF, 2019b).
In March 2020, 3,912 deaths involving the coronavirus occurred in England and Wales (UK Office for National Statistics, 2020). The COVID-19 pandemic has negatively influenced the physical and psychological wellbeing of the British population, with lockdown leading to lifestyle changes and an increase in negative emotions. Lifestyle restrictions, stressful situations, and unhealthy behaviors have been related to negative moods in the British population (Ingram et al., 2020).
Sample
Women who were at least 18 years old, UK residents, breastfeeding at the time of the study, with a child aged 0–36 months, were invited to participate in the survey. Participants were recruited through social media (e.g., breastfeeding Facebook pages). Overall, 4,627 women initiated the survey, however 609 participants did not complete it and their responses were not included in the analysis. Thus, the final sample consisted of 4,018 participants.
Measurement
Aims 1-4: The Survey
Participants were asked questions about their age, ethnicity, education level, and household income. Participants were further asked about their child’s age, birth order, and sex as well as breastfeeding duration, exclusivity, and the sources of support utilized before and during the lockdown. In addition, participants were asked their personal opinions about breastfeeding a child during the COVID-19 pandemic, as well as their emotional states, using the Generalised Anxiety Disorder Questionnaire (GAD-7; Spitzer et al., 2006), which assesses generalized anxiety, and the Patient Health Questionnaire (PHQ-9; Kroenke & Spitzer, 2002), which assesses depression symptoms. The National Institute for Health and Care Excellence (NICE) in the UK recommends the use of the GAD-7 and PHQ-9 to identify and assess mental health issues and disorders; thus, both questionnaires have been considered reliable and valid for detecting negative emotional states (NICE, 2020).
Aim 2: Maternal Opinions on the Importance of Breastfeeding and Breastfeeding Practices During the COVID-19 Pandemic
Participants were asked to rate the degree to which they agreed or disagreed with statements and recommendations made by the WHO on the importance of breastfeeding and breastfeeding during the COVID-19 pandemic. Responses ranged from 1 (strongly disagree) to 5 (strongly agree). The statements were chosen based on—and adapted from—the WHO’s (2020c) recommendations on breastfeeding practices during the COVID-19 pandemic. Example statements include “Due to the benefits of breastfeeding a mother should continue breastfeeding even if she shows symptoms of COVID-19” and “Breastfeeding protects new-borns from getting sick and helps them throughout their infancy and childhood.” Table 1 shows the nine statements rated by the participants.
Table 1.
Statements about the Importance of Breastfeeding and Breastfeeding Practices During the COVID-19 Pandemic.
| S1. Breastfeeding protects new-borns from getting sick and helps them throughout their infancy and childhood. |
| S2. Breastfeeding is particularly effective against infectious diseases as it strengthens the immune system by transferring antibodies from the mother to the child via breast milk. |
| S3. Due to the benefits of breastfeeding a mother should continue breastfeeding even if she shows symptoms of COVID-19. |
| S4. If a mother is ill with coronavirus, practising respiratory hygiene during breastfeeding should be recommended. |
| S5. Due to COVID-19, weaning a breastfed child should be advised. |
| S6. If a mother is ill with coronavirus expressing milk should be encouraged. |
| S7. If a mother is ill with coronavirus relactation should be advised. |
| S8. If a mother is ill with coronavirus wet nursing should be recommended. |
| S9. If a mother is ill with coronavirus donor human milk should be considered. |
Note. The questions were created by the authors based on the WHO (2020c) recommendations.
Aim 3: Maternal Emotional States
The Generalised Anxiety Disorder Questionnaire (GAD-7) is a 7-item self-report instrument used to assess adult generalized anxiety during the past 2 weeks (Spitzer et al., 2006). Questions concern, for instance, feeling nervous and worrying too much. Items are scored on a 4-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day). If participants had one or two missing items, their average item score was used for the missing items; participants with three or more missing items were excluded. A total score ranging between 0 and 5 indicates mild anxiety, between 6 and 10 indicates moderate anxiety, between 11 and 15 indicates moderately severe anxiety, and between 16 and 21 indicates severe anxiety. The GAD-7 has shown high internal consistency in previously reported research (Cronbach’s α > .80; see Maroufizadeh et al., 2019; Spitzer et al., 2006) and in the current study (Cronbach’s α = .91). The GAD-7 has further shown high construct and factorial validity (see Spitzer et al., 2006).
The Patient Health Questionnaire (PHQ-9) is a 9-item self-report instrument used to measure depression symptoms in adults over the last 2-week period (Kroenke & Spitzer, 2002). Questions concern, for instance, feeling tired, feeling depressed, and sleeping too much. Previously, researchers have reported high internal consistency (Cronbach’s α > .80; see Kroenke & Spitzer, 2002); similarly, in the current study, Cronbach’s α was .87. Equally to the GAD-7, items are scored on a 4-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day). Scores were summed to give a total score. If participants had one or two missing items, their average item score was used for the missing items; participants with three or more missing items were excluded. A total score between 0 and 5 represents mild depression, between 6 and 10 indicates moderate depression, between 11 and 15 indicates moderately severe depression, and 16 and above represents severe depression. The PHQ-9 has further been reported to have high construct and factorial validity (see Maroufizadeh et al., 2019).
Data Collection
This study was conducted through an online survey, which was developed using Qualtrics (USA, 2002), between April 23–25, 2020. This time frame was chosen to assess participants’ responses after the WHO’s declaration of a global pandemic on March 11, 2020 (WHO, 2020b) and the UK Government’s declaration of lockdown on March 23, 2020 (UK Government, 2020).
Informed consent was obtained by asking participants to click on a consent radial button, to confirm that they agreed to participate in the study. In the information sheet, participants were informed that they could withdraw at any time and that the data would not be used for research purposes. The survey was anonymous and data confidentiality was assured in accordance with the Data Protection Act (UK Government, 2018a) and the General Data Protection Regulation (UK Government, 2018b). At the end of the survey, participants were provided with further information on the purpose of the study, NHS guidelines regarding breastfeeding, as well as information on coronavirus.
Data Analysis
The data were analyzed using SPSS Version 26. Prior to analysis, the data were inspected for normality and outliers using the Shapiro Wilk test of normality and Cook’s distance > 1 respectively. No outliers were removed (maximum Cook’s distance = .06). Since the data tended to be skewed and deviated significantly from normality on all variables, nonparametric tests were used for all analyses.
In order to address the first aim of this study, percentages were calculated to explore sources of advice and support used by breastfeeding participants prior to and during the COVID-19 lockdown in the UK. The chi-square test on proportions was used to assess whether use of different sources of advice changed before and during the lockdown.
To address the second aim, frequencies of opinions on breastfeeding statements were examined. To address the third aim, mean scores on the GAD-7 and PHQ-9 were examined; frequencies of participants scoring with mild, moderate, and severe anxiety (GAD-7) and depression symptoms (PHQ-9) were further examined.
To address the fourth aim, Mann-Whitney U tests were conducted to examine differences between breastfeeding duration (participants who breastfed for more than 6 months vs. participants who breastfed for less than 6 months) and total number of children in the family (1 child vs. 2 or more children) in relation to opinions on breastfeeding practices during the COVID-19 pandemic as well total scores for anxiety and depression symptoms. The cut-off point for breastfeeding duration was chosen in accordance with WHO (2020a) current recommendations on exclusive breastfeeding for 6 months.
Results
Tables 2 and 3 display the participants’ characteristics.
Table 2.
Participants’ Characteristics (N = 4,018).
| Characteristics | Total n (%) |
BF < 6 Months (n = 1234, 31%) n (%) |
BF > 6 Months (n = 2784, 69%) n (%) |
One Child (n = 1723, 43%) n (%) |
> One Child (n = 2291, 57%) n (%) |
|---|---|---|---|---|---|
| Mother’s education | |||||
| No formal qualifications | 40 (1) | 12 (1) | 28 (1) | 0 (0) | 23 (1) |
| GCSEs/A-levels | 1366 (34) | 420 (34) | 919 (33) | 482 (28) | 871 (38) |
| Bachelor’s Degree | 1728 (43) | 543 (44) | 1197 (43) | 810 (47) | 939 (41) |
| Master’s Degree | 723 (18) | 210 (17) | 529 (19) | 345 (20) | 389 (17) |
| Doctoral Degree | 161 (4) | 49 (4) | 111 (4) | 86 (5) | 69 (3) |
| Mother’s ethnicity | |||||
| White | 3857 (96) | 1185 (96) | 2673 (96) | 1654 (96) | 2222 (97) |
| Other | 161 (4) | 49 (4) | 111 (4) | 69 (4) | 69 (3) |
| Household income | |||||
| < £20,000 | 482 (12) | 136 (11) | 362 (13) | 172 (10) | 298 (13) |
| £20,001-£40,000 | 1286 (32) | 370 (30) | 891 (32) | 517 (30) | 756 (33) |
| > £40,001 | 2250 (56) | 728 (59) | 1531 (55) | 1034 (60) | 1237 (54) |
| Child sex | |||||
| Female | 2089 (52) | 642 (52) | 1448 (52) | 896 (52) | 1191 (52) |
| Male | 1929 (48) | 592 (48) | 1336 (48) | 827 (48) | 1100 (48) |
| Childbirth order | |||||
| First | 1728 (43) | 506 (41) | 1225 (44) | 1723 (100) | 0 (0) |
| Subsequent | 2290 (57) | 728 (59) | 1559 (56) | 0 (0) | 2291 (100) |
Note. BF = breastfeeding; GCSE = General Certificate of Secondary Education. Data missing for four participants with incomplete data for number of children in the family.
Table 3.
Participants’ mean (SD) ages (N = 4018).
| Ages | Total sample M (SD) |
BF < 6 months (n = 1234; 31%) M (SD) |
BF > 6 months (n = 2784; 69%) M (SD) |
One child family (n = 1723; 43%) M (SD) |
> One Child (n = 2291; 57%) M (SD) |
|---|---|---|---|---|---|
| Mother’s age (years) | 32 (4.87) | 31 (4.62) | 33 (4.93) | 31 (4.74) | 33 (4.78) |
| Child age (months) | 12 (8.75) | 3 (1.77) | 15 (7.80) | 12 (8.63) | 12 (8.84) |
Note. BF = breastfeeding. Data missing for four mothers with incomplete data for number of children in the family.
Aim 1: Breastfeeding Support Before and During the COVID-19 Lockdown
Eighty-eight per cent of the participants reported exclusively breastfeeding their child, whereas 12% used a mixed feeding approach (i.e., human and formula milk). Overall, 98% of the participants stated they received support from their partner during their breastfeeding journey.
Sources of advice used by participants changed considerably from before lockdown to during lockdown. Use of NHS and National Childbirth Trust (NCT) classes, friends and family, leaflets, books, and other sources (e.g., midwives and telephone helplines), were all significantly reduced. The only source of advice with no significant change was the use of online sources, in particular websites, forums, and online support groups (see Table 4).
Table 4.
Comparisons of Participants’ Sources for Advice Before and During the UK COVID-19 Lockdown (N = 4,018).
| Source of advice | Before n (%) |
During n (%) |
X² | p |
|---|---|---|---|---|
| National Health Service classes | 506 (13) | 26 (1) | 463.79 | <.001 |
| National Childbirth Trust classes | 360 (9) | 43 (1) | 262.52 | <.001 |
| Friends and family | 2064 (51) | 1269 (32) | 324.01 | <.001 |
| Leaflets | 725 (18) | 121 (3) | 481.96 | <.001 |
| Books | 359 (9) | 144 (4) | 98.04 | <.001 |
| Internet | 2481 (62) | 2421 (60) | 1.88 | .170 |
| Other | 1526 (38) | 907 (23) | 225.87 | <.001 |
Note. Other = midwives, health visitors, telephone helplines, peer support groups.
Aims 2 and 4: Opinions on the Importance of Breastfeeding During the COVID-19 Pandemic
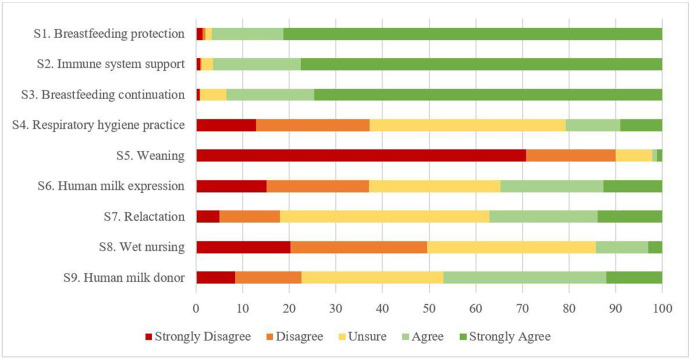
The range of responses to the nine statements on breastfeeding are illustrated in Figure 1. The highest levels of agreement were for Statements 1, 2, and 3 on the efficacy of breastfeeding for protection of the infant against getting sick, infectious diseases, and the recommendation for a mother to continue breastfeeding if she became ill with COVID-19. Participants most strongly disagreed with Statement 5, regarding weaning a breastfed child due to COVID-19. When asked about whether “breastfeeding protects newborns from getting sick and helps them throughout their infancy and childhood”, participants who had one child were more positive about this statement than participants who had two or more children. In addition, participants with one child were more in favor of practicing respiratory hygiene than participants who had subsequent children. Participants who breastfed their child for less than 6 months and participants who had one child agreed with advice to wean a breastfed child during the COVID-19 pandemic. Similarly, participants who breastfed for a shorter period (< 6 months) and participants with one child highly agreed with expressing human milk if a mother presented with symptoms of the coronavirus. Additionally, participants who breastfed for less than 6 months were more in favor of considering relactation in case of COVID-19 symptoms. In contrast, participants who breastfed for more than 6 months and participants who had more than one child were more positive about considering human milk donation as well as wet nursing if a mother became ill due to the coronavirus. Table 5 shows statistical comparisons and mean ranks for the statements.
Figure 1.
Showing range of responses from mothers to each statement.
Table 5.
Comparison of Frequency Distributions of Participants who Responded Agree or Strongly Agree on Pandemic Survey (N = 4,018).
| Statement | Total n (%) |
Breastfeeding Duration | Number of Children | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| < 6 months (n = 1234; 31%) |
> 6 months (n = 2784; 69%) |
Statistical comparisons | One child (n = 1723; 43%) |
> One child (n = 2291; 57%) |
Statistical comparisons | ||||||
| M rank | n (%) | M rank | n (%) | M rank | n (%) | M rank | n (%) | ||||
| S1. BF protection | 3878 (97) | 1975 | 1193 (97) | 2024 | 2685 (96) |
U = 1,675,113.50 z = −1.83, p = .068 |
2045 | 1679 (97) | 1978 | 2195 (96) |
U = 1,907,162.00 z = −2.67, p = .008 |
| S2. Immune system support | 3842 (96) | 1981 | 1183 (97) | 2002 | 2659 (96) |
U = 1,674,006.50 z = −0.74, p = .460 |
2015 | 1653 (97) | 1977 | 2186 (96) |
U = 1,909,834.00 z = −1.42, p = .157 |
| S3. BF continuation | 3747 (93) | 1965 | 1132 (92) | 2023 | 2615 (94) |
U = 1,662,363.00 z = −1.91, p = .056 |
1997 | 1607 (93) | 2007 | 2137 (94) |
U = 1,955,068.00 z = −0.37, p = .715 |
| S4. Respiratory hygiene practice | 832 (21) | 2040 | 272 (22) | 1984 | 560 (20) |
U = 1,655,588.00 z = −1.48, p = .138 |
2064 | 394 (23) | 1951 | 438 (19) |
U = 1,847,512.50 z = −3.23, p =.001 |
| S5. Weaning | 88 (2) | 2213 | 35 (3) | 1909 | 53 (2) |
U = 1,446,641.00 z = −9.62, p <.001 |
2089 | 39 (2) | 1933 | 49 (2) |
U = 1,807,946.50 z = −5.29, p <.001 |
| S6. Human milk expression | 1389 (35) | 2211 | 507 (41) | 1909 | 882 (32) |
U = 1,446,512.50 z = −7.81, p <.001 |
2067 | 622 (36) | 1949 | 766 (34) |
U = 1,843,605.50 z = −3.27, p = .001 |
| S7. Relactation | 1485 (37) | 2089 | 488 (40) | 1966 | 997 (36) |
U = 1,602,146.00 z = −3.30, p = .001 |
2004 | 638 (37) | 2000 | 846 (37) |
U = 1,958,110.00 z = −0.13, p = .897 |
| S8. Wet nursing | 569 (14) | 1889 | 125 (10) | 2052 | 444 (16) |
U = 1,564,487.00 z = −4.30, p <.001 |
1955 | 214 (12) | 2033 | 355 (16) |
U = 1,882,052.00 z = −2.23, p = .026 |
| S9. Human milk donor | 1885 (47) | 1923 | 530 (43) | 2043 | 1355 (49) |
U = 1,609,179.50 z = −3.13, p = .002 |
1962 | 775 (45) | 2036 | 1109 (49) |
U = 1,894,570.00 z = −2.08, p = .04 |
Note. BF = breastfeeding. See Table 1 for the list of complete statements. Data missing for four mothers with incomplete data for number of children in the family.
Aims 3 and 4: Maternal Emotional States During the COVID-19 Lockdown
Participants with two or more children showed a significantly higher level of anxiety than mothers with one child; however, no differences were found with regard to breastfeeding duration on the GAD-7 total scores. There was no significant influence of breastfeeding duration or number of children on the PHQ-9 total scores. Descriptive statistics for emotional states along with the percentage of participants falling into categories for mild to severe anxiety and depression levels are reported in Tables 6 and 7.
Table 6.
Comparisons of Participants’ Mean (SD) Scores on the GAD-7 and PHQ-9.
| Instrument | Total N; M (SD) | Breastfeeding Duration | Number of children | ||||
|---|---|---|---|---|---|---|---|
| < 6 mos. (n = 1232); M (SD) | > 6 mos. (n = 2781); M (SD) | Comparisons | One Child (n = 1723) M (SD) | > One Child (n = 2287) M (SD) | Comparisons | ||
| GAD-7 | 6.76 (5.17) | 6.86 (5.19) | 6.72 (5.16) | U = 1,692,808.50; z = −.64, p = .521 | 6.01 (5.16) | 6.23 (5.35) | U = 1,862,345.50; z = −2.98, p = .003 |
| PHQ-9 | 6.14 (5.27) | 6.07 (5.21) | 6.17 (5.30) | U = 1,699,678.00; z = −.42, p = .678 | 6.02 (5.15) | 6.19 (5.32) | U = 1,936,182.50; z = −.94, p = .346 |
Note. Data missing for four mothers with incomplete questionnaire data, and four mothers with incomplete data for number of children in the family. GAD-7 = Generalised Anxiety Disorder Questionnaire; PHQ-9 = Patient Health Questionnaire.
Table 7.
Frequency Distribution of Participants’ Scores for Anxiety (GAD-7) and Depression (PHQ-9).
| Scores | Anxiety; n = 4014; n (%) | Depression; n = 4014; n (%) |
|---|---|---|
| Mild | 1962 (49) | 2260 (56) |
| Moderate | 1230 (31) | 1035 (26) |
| Moderately severe | 479 (12) | 439 (11) |
| Severe | 343 (8) | 280 (7) |
Note. GAD-7 = Generalized Anxiety Disorder Questionnaire (Spitzer et al., 2006); PHQ-9 = Patient Health Questionnaire (Kroenke & Spitzer, 2002). Data missing for four mothers with incomplete questionnaire data.
Discussion
To the authors’ knowledge, the present study was the first to explore maternal experiences, opinions, and emotional states in relation to breastfeeding during the COVID-19 lockdown in the UK. Our results suggested that participants who breastfed for longer than 6 months and participants who had two or more children had different opinions about breastfeeding practices than participants who breastfed for less than 6 months and those who had one child. More specifically, participants who breastfed for a longer period and those with more than one child were more in favor of the use of human milk donation and wet nursing in case of COVID-19 symptoms.
Donor human milk is considered the best option in case a mother’s own milk is not available and infants are vulnerable (Renfrew et al., 2020). According to NICE (2010a) there are 17 human milk banks available in the UK; the donor human milk is mainly provided to preterm infants and those with growth limitations. However, the COVID-19 pandemic has also had an impact on human milk banks; for instance, human milk donors may have difficulty accessing phlebotomy services (Shenker et al., 2021) for serological screening tests, which are essential for human milk donations (NICE, 2010b).
In the UK, human milk donor banks have employed policies to ensure the safety of donated human milk during the COVID-19 pandemic (Shenker, 2020); however, little is known regarding the availability of human milk, about mothers affected by coronavirus. As our findings may indicate, mothers with longer breastfeeding experience may be more aware of breastfeeding resources (i.e., human milk donor banks), information about availability of human milk should be made accessible to mothers who have shorter or no breastfeeding experience. According to the WHO (2020c) if a mother has COVID-19 and is not able to breastfeed her child, expressed human milk, as well as donor human milk and wet nursing, should be advised by health professionals.
We further showed that participants who breastfed for less than 6 months and who had one child were more prone to agreeing with expressing human milk and weaning the child in case of coronavirus symptoms; moreover, those who breastfed for a shorter period were pro-relactation. Additionally, participants with one child were favorable to the practice of respiratory hygiene and they had stronger opinions about the benefits that breastfeeding has on children’s health. According to the WHO (2020c), if a mother is suspected or confirmed to have COVID-19, she should wear a mask while breastfeeding (WHO, 2020c), as well as strictly following the instructions on infection control, for instance hand hygiene (Davanzo et al., 2020).
Our findings suggest that mothers of a single child may be more motivated to establish exclusive breastfeeding and develop breastfeeding self-efficacy (Henshaw et al., 2015); they may also be more informed about the value of breastfeeding (e.g., lifelong health and development advantages to new-borns and infants (WHO, 2020c). Additional factors (e.g., family support and education) may play an important role in the initiation and duration of exclusive breastfeeding, especially in first-time mothers (Semenic et al., 2008).
In a study by Salvatori et al. (2020), expressed human milk from mothers who were affected by the coronavirus was analysed; the results indicated no detection of SARS-CoV-2 in the milk. Similarly, Marín Gabriel et al. (2020) found no evidence of SARS-CoV-2 in colostrum samples from women who tested positive for COVID-19. Previously researchers have further supported these findings (Chen et al., 2020); in fact, the WHO (2020c) has recently declared that the transmission of COVID-19 through human milk and breastfeeding has not been detected. On the contrary, the transmission from mother to child may occur through respiratory droplets (Salvatori et al., 2020).
We suggest that in case of coronavirus symptoms, health professionals should take into account mothers’ viewpoints about breastfeeding practices; indeed, mothers’ involvement in decision-making may influence breastfeeding continuation and initiation. The WHO (2020c) has advised health professionals to assist mothers who have recovered from COVID-19 with relactation, as well as supporting mothers of infants aged more than 6 months to continue breastfeeding along with complementary foods. According to Salvatori et al. (2020) “medical staff and nurses should not only focus on care of COVID-19 mothers and infants, but also protect, promote, and support breastfeeding” (p. 347).
Given the interrelations between breastfeeding opinions, perceptions, and decisions, and their influence on psychological wellbeing and breastfeeding outcomes (see Henshaw et al., 2015), health bodies and professional organizations must consider mothers’ experiences and viewpoints in order to create a supportive environment (Brown, 2017). At present, implementing aid and strategies for breastfeeding initiation and continuation during the COVID-19 pandemic is urgent. More specifically, first-time mothers and mothers with little or no previous breastfeeding experience may benefit from receiving information about breastfeeding a child during the COVID-19 pandemic; they may further benefit from enhanced support by health professionals, as they may be vulnerable to ceasing breastfeeding.
Additionally, we found that the number of children influenced maternal anxiety; mothers who had more than one child scored higher on the GAD-7 than mothers of a single child. Recently, researchers reporting about maternal mental health during the COVID-19 lockdown in the UK have demonstrated that low mood and solitude were typical of mothers during this time; apprehension about COVID‐19 infection was associated with maternal emotional issues (Dib et al., 2020).
The number of children in the family may increase their level of anxiety. This could be due to worries regarding the coronavirus contagion; moreover, looking after two or more children at home and with little support may be exhausting. Although anxiety symptoms presented in the participants in this study may not be entirely related to breastfeeding (e.g., fatigue), previously researchers have found a positive association between breastfeeding groups and healthier maternal mental health (Dib et al., 2020). This demonstrates that sharing experience and getting support may facilitate mothers to feel less lonely and stressed. Additionally, according to Black et al. (2020), mothers who were members of social media groups had greater breastfeeding success and longer breastfeeding duration. In contrast, we found no influence of number of children on depression symptoms, nor was there an influence of breastfeeding duration on the GAD-7 or PHQ-9 total scores.
One important aspect to consider is that the questionnaires used in this study assess psychological symptoms during the last 2-week period; the data collection of the current study took place 1 month after the beginning of the lockdown. It is possible that more severe psychological symptoms (i.e., depression) developed in due course. Alternatively, a study by Ozamiz-Etxebarria et al. (2020) showed that psychological symptoms arose after 3 weeks of quarantine in comparison to the beginning of the lockdown; thus, it also is possible that levels of anxiety and depression in our study were already inflated from pre-lockdown levels.
It is important to highlight that almost all participants in this study stated they had received breastfeeding support from their partner; this indicates that when participants were assisted, they could rely on emotional and practical support about breastfeeding their child. Researchers have reported that mothers who breastfed for at least 6 months benefited from partner support (Guyer et al., 2012); clearly, encouragement is an essential aspect of breastfeeding continuation.
Half of our study participants relied on friends and family for advice and support about breastfeeding prior to the lockdown; it is not surprising that due to the impossibility of seeing family members and friends the percentage decreased. In a previous study, Costantini et al. (2019) reported that British mothers (pre-pandemic) used to receive and seek advice from family and friends, as well as books and leaflets. We showed that sources of advice significantly changed from before the lockdown to during the lockdown as participants were restricted to using advice, which was available to them (e.g., the Internet, midwives, telephone helplines, friends and family). However, participants indicated no variation in the use of the Internet as the main source for seeking advice. This suggested that the Internet (e.g., websites, forums) may be the preferred source that breastfeeding mothers use to gather information and advice. However, Watson et al. (2020) has highlighted the use of the Internet mainly for white and scholarly participants.
Although we demonstrated the importance of mothers’ opinions on breastfeeding practices in the scenario of coronavirus symptoms, further investigation is needed in order to understand breastfeeding practices during the COVID-19 pandemic in lower socio-economic groups, as well as social and environmental supports for ethnic minority groups and those who suffer from mental health issues. In the future, researchers should investigate factors that may influence maternal decisions about breastfeeding initiation and continuation, namely lactation stage and maternal physical and psychological wellbeing.
Limitations
Although online surveys are considered a robust and flexible method for data collection (Couper, 2017), as well as an effective approach to collect nationwide data during the COVID-19 pandemic (Ali et al., 2020), there are some limitations that need to be discussed. For instance, online surveys are subject to coverage error, which concerns the access to the Internet for the whole population (Dillman & Bowker, 2001); the Internet may not be available to everyone. Mothers who did not have access to the network at the time of data collection could not take part in this study.
Researchers have indicated that mainly white, wealthy, and scholarly individuals participate in research studies (Schulz et al., 2018), particularly online surveys (e.g., Watson et al., 2020). Although this study aimed to recruit mothers from all backgrounds and ethnicities, the sample was skewed, consisting of predominantly highly educated and white participants. Nevertheless, it is important to highlight that, due to the overwhelming response, the survey was closed after 48 hr; this may have contributed to the exclusion of participants with different backgrounds and minorities.
The high number of responses from mothers may indicate that women who were breastfeeding their child during the first lockdown in the UK, felt the need to share their experiences and viewpoints, and to have a voice in this matter; future research should explore maternal breastfeeding experiences in order to identify mothers’ needs and wants.
Conclusion
In conclusion, our study has highlighted the importance of examining the influence of COVID-19 on breastfeeding dyads concerning breastfeeding continuation, as well as maternal viewpoints and psychological wellbeing. Interventions are urgently needed in order to aid breastfeeding mothers and prevent the development of mental health issues. Professionals, organizations, and health bodies need to consider mothers’ knowledge, experience, and care responsibilities with the purpose of providing support during the COVID-19 pandemic.
Acknowledgements
The authors would like to thank all the mothers who voluntarily took part in this study.
Footnotes
*Editor’s Note: JHL has a policy of not publishing references from predatory publishers. The references in the Reference List with * were published in journals whose publishers have been criticized by some academics for low standards of peer review as well as some allegations of academic misconduct. Others have felt these publishers have done their due diligence. Due to the importance of the topic covered in this review, we left the inclusion of these articles to the authors’ discretion. The authors have reviewed all references and take responsibility for their quality.
**Editor’s Note: Reprints are preliminary reports that have not undergone peer review. They should not be considered conclusive, used to inform clinical practice, or referenced by the media as validated information. The reference in the reference list below indicated by ** is a preprint.
Disclosures and conflicts of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Cristina Costantini, Dr.BSc, MSc, ClinPsyD, PhD https://orcid.org/0000-0002-6897-5870
References
- Abul-Fadl A., Fahmy E. M., Narouz K. N. (2005). The psychological benefits of continued breastfeeding into the second year for mother and child. International Journal of Child Neuropsychiatry, 2(2), 143–153.doi:10.1007/s00103-018-2769-0 [Google Scholar]
- Adedinsewo D. A, Fleming A. S, Steiner M, Meaney M. J, Girard A. W, MAVAN team . (2014). Maternal anxiety and breastfeeding: Findings from the MAVAN (maternal adversity, vulnerability and neurodevelopment) study. Journal of Human Lactation: Official Journal of International Lactation Consultant Association, 30(1), 102–109.doi:10.1177/089033441350424424065719 [DOI] [PubMed] [Google Scholar]
- Ali S. H., Foreman J., Capasso A., Jones A. M., Tozan Y., DiClemente R. J. (2020). Social media as a recruitment platform for a nationwide online survey of COVID-19 knowledge, beliefs, and practices in the United States: Methodology and feasibility analysis. BMC Medical Research Methodology, 20(1), 1–11.doi:10.1186/s12874-020-01011-032404050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreas N. J., Kampmann B., Mehring Le-Doare K., Le-Doare K. M. (2015). Human breast milk: A review on its composition and bioactivity. Early Human Development, 91(11), 629–635.doi:10.1016/j.earlhumdev.2015.08.01326375355 [DOI] [PubMed] [Google Scholar]
- Bagci Bosi A. T., Eriksen K. G., Sobko T., Wijnhoven T. M. A., Breda J. (2016). Breastfeeding practices and policies in who European region member states. Public Health Nutrition, 19(4), 753–764.doi:10.1017/S136898001500176726096540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black R., McLaughlin M., Giles M. (2020). Women’s experience of social media breastfeeding support and its impact on extended breastfeeding success: A social cognitive perspective. British Journal of Health Psychology, e12451.doi:10.1111/bjhp.12451 [DOI] [PubMed] [Google Scholar]
- Brown A. (2017). Breastfeeding as a public health responsibility: A review of the evidence. Journal of Human Nutrition and Dietetics, 30(6), 759–770. doi:https://doi.org/10.1111/jhn.12496. [DOI] [PubMed] [Google Scholar]
- Brown A., Raynor P., Lee M. (2011). Healthcare professionals’ and mothers’ perceptions of factors that influence decisions to breastfeed or formula feed infants: A comparative study. Journal of Advanced Nursing, 67(9), 1993–2003.doi:10.1111/j.1365-2648.2011.05647.x21507050 [DOI] [PubMed] [Google Scholar]
- Chen L., Li Q., Zheng D., Jiang H., Wei Y., Zou L., Feng L., Xiong G., Sun G., Wang H., Zhao Y., Qiao J. (2020). Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. New England Journal of Medicine, 382(25), e100.doi:10.1056/NEJMc2009226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini C., Harris G., Reddy V., Akehurst L., Fasulo A. (2019). Introducing complementary foods to infants: Does age really matter? A look at feeding practices in two European communities: British and Italian. Child Care in Practice, 25(3), 326–341.doi:10.1080/13575279.2017.1414033 [Google Scholar]
- Couper M. P. (2017). New developments in survey data collection. Annual Review of Sociology, 43(1), 121–145.doi:10.1146/annurev-soc-060116-053613 [Google Scholar]
- *Czosnykowska-Łukacka M., Królak-Olejnik B., Orczyk-Pawiłowicz M. (2018). Breast milk macronutrient components in prolonged lactation. Nutrients, 10(12), 1893.doi:10.3390/nu1012189330513944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta J., Graham B., Wellings K. (2012). The role of fathers in breastfeeding: Decision-making and support. British Journal of Midwifery, 20(3), 159–167.doi:10.12968/bjom.2012.20.3.159 [Google Scholar]
- Davanzo R., Moro G., Sandri F., Agosti M., Moretti C., Mosca F. (2020). Breastfeeding and coronavirus disease-2019: Ad interim indications of the Italian Society of Neonatology endorsed by the Union of European Neonatal & Perinatal Societies. Maternal & Child Nutrition, 16(3), e13010.doi:10.1111/mcn.1301032243068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Lauro S., Unger S., Stone D., O’Connor D. L. (2016). Human milk for ill and medically compromised infants: Strategies and ongoing innovation. Journal of Parenteral and Enteral Nutrition, 40(6), 768–782. doi:https://doi.org/10.1177/0148607116629676. [DOI] [PubMed] [Google Scholar]
- Dib S., Rougeaux E., Vázquez‐Vázquez A., Wells J. C., Fewtrell M. (2020). Maternal mental health and coping during the COVID‐19 lockdown in the UK: Data from the COVID‐19 New Mum Study. International Journal of Gynecology and Obstetrics, 151(3), 407–414. doi:https://doi.org/10.1002/ijgo.13397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGirolamo A., Thompson N., Martorell R., Fein S., Grummer-Strawn L. (2005). Intention or experience? Predictors of continued breastfeeding. Health Education & Behavior, 32(2), 208–226.doi:10.1177/109019810427197115749967 [DOI] [PubMed] [Google Scholar]
- Dillman D. A., Bowker D. K. (2001). The web questionnaire challenge to survey methodologists. Online Social Sciences, 53–71.doi:10.1146/annurev.so.17.080191.001301 [Google Scholar]
- Duan X., Wang J., Jiang X. (2017). A meta-analysis of breastfeeding and osteoporotic fracture risk in the females. Osteoporosis International, 28(2), 495–503.doi:10.1007/s00198-016-3753-x27577724 [DOI] [PubMed] [Google Scholar]
- Frank N. M, Lynch K. F, Uusitalo U, Yang J, Lönnrot M, Virtanen S. M, Hyöty H, Norris J. M, TEDDY Study Group . (2019). The relationship between breastfeeding and reported respiratory and gastrointestinal infection rates in young children. BMC Pediatrics, 19(1), 339.doi:10.1186/s12887-019-1693-231533753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Z., Wang R., Qin Z., Dong A., Liu C. -B. (2019). Protective effect of breastfeeding against childhood leukemia in Zhejiang Province, P. R. China: A retrospective case-control study. Libyan Journal of Medicine, 14(1), 1508273.doi:10.1080/19932820.2018.1508273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbs B. G., Forste R., Lybbert E. (2018). Breastfeeding, parenting, and infant attachment behaviors. Maternal and Child Health Journal, 22(4), 579–588.doi:10.1007/s10995-018-2427-z29388115 [DOI] [PubMed] [Google Scholar]
- Guyer J., Millward L. J., Berger I. (2012). Mothers’ breastfeeding experiences and implications for professionals. British Journal of Midwifery, 20(10), 724–733.doi:10.12968/bjom.2012.20.10.724 [Google Scholar]
- Hardin J. S., Jones N. A., Mize K. D., Platt M. (2021). Affectionate touch in the context of breastfeeding and maternal depression influences infant neurodevelopmental and temperamental substrates. Neuropsychobiology, 80(2), 158–175.doi:10.1159/00051160433461198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henshaw E. J., Fried R., Siskind E., Newhouse L., Cooper M. (2015). Breastfeeding self-efficacy, mood, and breastfeeding outcomes among primiparous women. Journal of Human Lactation, 31(3), 511–518.doi:10.1177/089033441557965425829478 [DOI] [PubMed] [Google Scholar]
- Hinic K. (2016). Predictors of breastfeeding confidence in the early postpartum period. Journal of Obstetric, Gynecologic & Neonatal Nursing, 45(5), 649–660.doi:10.1016/j.jogn.2016.04.01027472996 [DOI] [PubMed] [Google Scholar]
- Huang Y., Ouyang Y. -Q., Redding S. R. (2019). Previous breastfeeding experience and its influence on breastfeeding outcomes in subsequent births: A systematic review. Women and Birth, 32(4), 303–309.doi:10.1016/j.wombi.2018.09.00330274877 [DOI] [PubMed] [Google Scholar]
- Hull H. R. (2018). Are protein levels in infant formula a driving factor for childhood obesity development? Obesity, 26(7), 1114–1114.doi:10.1002/oby.2224229932514 [DOI] [PubMed] [Google Scholar]
- Hutchings R. (2020). The impact of Covid-19 on the use of digital technology in the NHS. Nuffield Trust . https://www.nuffieldtrust.org.uk/research/the-impact-of-covid-19-on-the-use-of-digital-technology-in-the-nhs
- *Ingram J., Maciejewski G., Hand C. J. (2020). Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Frontiers in Psychology, 11, 2328.doi:10.3389/fpsyg.2020.588604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan S. J., Na R., Johnatty S. E., Wise L. A., Adami H. O., Brinton L. A., Chen C., Cook L. S., Dal Maso L., De Vivo I., Freudenheim J. L., Friedenreich C. M., La Vecchia C., McCann S. E., Moysich K. B., Lu L., Olson S. H., Palmer J. R., Petruzella S., Webb P. M. et al. (2017). Breastfeeding and endometrial cancer risk: An analysis from the epidemiology of endometrial cancer consortium. Obstetrics and Gynecology, 129(6), 1059doi:10.1097/AOG.000000000000205728486362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klopp A., Vehling L., Becker A., Subbarao P., Mandhane P., Turvey S., Azad M. (2018). Modes of infant feeding and childhood asthma development: Is there a difference between direct breastfeeding and expressed breast milk? Pediatrics, 141.doi:10.1016/j.jpeds.2017.07.012 [Google Scholar]
- Kroenke K., Spitzer R. L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 509–515.doi:10.3928/0048-5713-20020901-06 [Google Scholar]
- Krol K. M., Grossmann T. (2018). Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz, 61(8), 977–985.doi:10.1007/s00103-018-2769-029934681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde K., Lehnig F., Nagl M., Kersting A. (2020). The association between breastfeeding and attachment: A systematic review. Midwifery, 81, 102592.doi:10.1016/j.midw.2019.10259231830673 [DOI] [PubMed] [Google Scholar]
- *Liu J., Leung P., Yang A. (2014). Breastfeeding and active bonding protects against children’s internalizing behavior problems. Nutrients, 6(1), 76–89.doi:10.3390/nu6010076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maleki-Saghooni N., Amel Barez M., Karimi F. Z. (2020). Investigation of the relationship between social support and breastfeeding self-efficacy in primiparous breastfeeding mothers. The Journal of Maternal-Fetal & Neonatal Medicine, 33(18), 3097–3102.doi:10.1080/14767058.2019.156898630632820 [DOI] [PubMed] [Google Scholar]
- Liu L., Zhu J., Yang J., Wu M., Ye B. (2017). The effect of a perinatal breastfeeding support program on breastfeeding outcomes in primiparous mothers. Western Journal of Nursing Research, 39(7), 906–923.doi:10.1177/019394591667064527681668 [DOI] [PubMed] [Google Scholar]
- Marín Gabriel M. Á., Malalana Martínez A. M., Marín Martínez M. E., Anel Pedroche J. (2020). Negative Transmission of SARS-CoV-2 to Hand-Expressed Colostrum from SARS-CoV-2 Positive Mothers. Breastfeeding Medicine, 15(8).doi:10.1089/bfm.2020.0183 http://www.ncbi.nlm.nih.gov/pubmed/32644841 [DOI] [PubMed] [Google Scholar]
- Maroufizadeh S., Omani-Samani R., Almasi-Hashiani A., Amini P., Sepidarkish M. (2019). The reliability and validity of the patient health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with infertility. Reproductive Health, 16(1), 137.doi:10.1186/s12978-019-0802-x31500644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews M. E., Leerkes E. M., Lovelady C. A., Labban J. D. (2014). Psychosocial predictors of primiparous breastfeeding initiation and duration. Journal of Human Lactation, 30(4), 480–487.doi:10.1177/089033441453770724938527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meedya S., Fahy K., Kable A. (2010). Factors that positively influence breastfeeding duration to 6 months: A literature review. Women and Birth, 23(4), 135–145.doi:10.1016/j.wombi.2010.02.00220299299 [DOI] [PubMed] [Google Scholar]
- National Health Service . (2015). Maternity and breastfeeding. https://www.england.nhs.uk/statistics/statistical-work-areas/maternity-and-breastfeeding/
- National Health Service . (2020. a). Your breastfeeding questions answered. https://www.nhs.uk/conditions/pregnancy-and-baby/your-breastfeeding-questions/
- National Health Service . (2020. b). Benefits of breastfeeding. https://www.nhs.uk/conditions/pregnancy-and-baby/benefits-breastfeeding/
- National Institute for Health and Care Excellence . (2010. a). Donor breast milk banks: the operation of donor milk bank services. https://pubmed.ncbi.nlm.nih.gov/22319806/ [PubMed]
- National Institute for Health and Care Excellence . (2010. b). Donor milk banks: service operation. https://www.nice.org.uk/guidance/cg93 [PubMed]
- National Institute for Health and Care Excellence . (2020). Common mental health disorders in primary care overview. https://pathways.nice.org.uk/pathways/common-mental-health-disorders-in-primary-care
- Oddy W. H. (2017). Breastfeeding, childhood asthma, and allergic disease. Annals of Nutrition and Metabolism, 70(Suppl. 2), 26–36.doi:10.1159/00045792028521318 [DOI] [PubMed] [Google Scholar]
- *Ozamiz-Etxebarria N., Idoiaga Mondragon N., Dosil Santamaría M., Picaza Gorrotxategi M. (2020). Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: An investigation in a sample of citizens in northern Spain. Frontiers in Psychology, 11, 1491.doi:10.3389/fpsyg.2020.0149132625157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papp L. M. (2014). Longitudinal associations between breastfeeding and observed mother-child interaction qualities in early childhood. Child: Care, Health and Development, 40(5), 740–746.doi:10.1111/cch.1210624117653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattison K. L., Kraschnewski J. L., Lehman E., Savage J. S., Downs D. S., Leonard K. S., Adams E. L., Paul I. M., Kjerulff K. H. (2019). Breastfeeding initiation and duration and child health outcomes in the first baby study. Preventive Medicine, 118, 1–6.doi:10.1016/j.ypmed.2018.09.02030287329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrin M. T., Fogleman A. D., Newburg D. S., Allen J. C. (2017). A longitudinal study of human milk composition in the second year postpartum: Implications for human milk banking. Maternal & Child Nutrition, 13(1).doi:10.1111/mcn.1223926776058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters S. A. E., Yang L., Guo Y., Chen Y., Bian Z., Du J., Yang J., Li S., Li L., Woodward M., Chen Z. (2017). Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300 000 Chinese Women. Journal of the American Heart Association, 6(6), e006081.doi:10.1161/JAHA.117.00608128637778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philipp B. L., Merewood A. (2004). The Baby-Friendly way: The best breastfeeding start. Pediatric Clinics of North America, 51(3), 761–783.doi:10.1016/j.pcl.2004.01.00715157597 [DOI] [PubMed] [Google Scholar]
- Public Health England . (2016). Official Statistics Breastfeeding prevalence at 6-8 weeks after birth(Experimental Statistics). https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/779458/2015_16_Annual_Breastfeeding_Statistical_Commentary.pdf
- Radford A. (2001). Unicef is crucial in promoting and supporting breast feeding. BMJ, 322(7285), 555.doi:10.1136/bmj.322.7285.55511263456 [PMC free article] [PubMed] [Google Scholar]
- Radzyminski S., Callister L. C. (2016). Mother’s beliefs, attitudes, and decision making related to infant feeding choices. The Journal of Perinatal Education, 25(1), 18–28.doi:10.1891/1058-1243.25.1.1826848247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rempel L. A., Rempel J. K., Moore K. C. J. (2017). Relationships between types of father breastfeeding support and breastfeeding outcomes. Maternal & Child Nutrition, 13(3), e12337.doi:10.1111/mcn.1233727460557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renfrew M. J., Cheyne H., Dykes F., Entwistle F., McGuire W., Shenker N., Page L. (2020). Optimising mother-baby contact and infant feeding in a pandemic. Royal College of Midwives. [Google Scholar]
- Salvatori G., De Rose D. U., Concato C., Alario D., Olivini N., Dotta A., Campana A. (2020). Managing COVID-19-Positive maternal-infant dyads: An Italian experience. Breastfeeding Medicine, 15(5), 347–348.doi:10.1089/bfm.2020.009532311273 [DOI] [PubMed] [Google Scholar]
- **Schulz J., Bahrami-Rad D., Beauchamp J., Henrich J. (2018). The origins of WEIRD psychology. [pre-print] Available at SSRN 3201031.doi:10.31234/osf.io/d6qhu [Google Scholar]
- Scientific Advisory Committee on Nutrition . (2003). http://www.sacn.gov.uk/pdfs/smcn_03_08.pdf
- Semenic S., Loiselle C., Gottlieb L. (2008). Predictors of the duration of exclusive breastfeeding among first-time mothers. Research in Nursing & Health, 31(5), 428–441.doi:10.1002/nur.2027518324667 [DOI] [PubMed] [Google Scholar]
- Shenker N. (2020). Human milk and SARS-CoV-2—A summary of knowledge to date. Compiled for the British Association of Perinatal Medicine. https://hubble-live-assets.s3.amazonaws.com/bapm/redactor2_assets/files/562/Human_milk_and_SARS-CoV-2_-_A_summary_of_knowledge_to_date.pdf [Google Scholar]
- Shenker N, Staff M, Vickers A, Aprigio J, Tiwari S, Nangia S, Sachdeva R. C, Clifford V, Coutsoudis A, Reimers P, Israel-Ballard K, Mansen K, Mileusnic-Milenovic R, Wesolowska A, Goudoever J. Bvan, Hosseini M, Klotz D, Grøvslien A. H, Weaver G, Virtual Collaborative Network of Milk Banks and Associations . (2021). Maintaining human milk bank services throughout the COVID-19 pandemic: A global response. Maternal & Child Nutrition, 17(3), e13131.doi:10.1111/mcn.1313133403779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R. L., Kroenke K., Williams J. B. W., Löwe B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.doi:10.1001/archinte.166.10.109216717171 [DOI] [PubMed] [Google Scholar]
- UK Government . (2018. a). Data protection. https://www.gov.uk/data-protection
- UK Government . (2018. b). Guide to the general data protection regulation. https://www.gov.uk/government/publications/guide-to-the-general-data-protection-regulation
- UK Government . (2020). Coronavirus (COVID‑19). https://www.gov.uk/coronavirus
- UK Office for National Statistics . (2020). Deaths involving COVID-19, England and Wales: deaths occurring in March 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19englandandwales/deathsoccurringinmarch2020
- Unar-Munguía M., Torres-Mejía G., Colchero M. A., González de Cosío T. (2017). Breastfeeding mode and risk of breast cancer: A dose-response meta-analysis. Journal of Human Lactation, 33(2), 422–434.doi:10.1177/089033441668367628196329 [DOI] [PubMed] [Google Scholar]
- United Nations Children’s Fund . (2019. a). The baby friendly initiative. https://www.unicef.org.uk/babyfriendly/
- United Nations Children’s Fund . (2019. b). Preventing disease and saving resources. https://www.unicef.org.uk/babyfriendly/about/preventing-disease-and-saving-resources/
- United Nations Children’s Fund . (2020). Unicef UK baby friendly initiative. https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2020/04/Unicef-UK-Baby-Friendly-Initiative-statement-on-infant-feeding-during-the-Covid-19-outbreak.pdf
- Watson S., Costantini C., Clegg M. E. (2020). The role of complementary feeding methods on early eating behaviors and food neophobia in toddlers. Child Care in Practice, 26(1), 94–106.doi:10.1080/13575279.2018.1516625 [Google Scholar]
- Weaver J. M., Schofield T. J., Papp L. M. (2018). Breastfeeding duration predicts greater maternal sensitivity over the next decade. Developmental Psychology, 54(2), 220–227.doi:10.1037/dev000042529083214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2021. a). COVID-19 and breastfeeding - Position paper, 8 April 2020 (produced by WHO/Europe). https://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newborn-health/publications/2020/covid-19-and-breastfeeding-position-paper,-8-april-2020-produced-by-whoeurope
- World Health Organization . (2021. b). Breastfeedingin the 21st century. https://www.who.int/pmnch/media/news/2016/breastfeeding_brief.pdf
- World Health Organization . (2020. a). Infant and young child feeding. https://www.who.int/en/news-room/fact-sheets/detail/infant-and-young-child-feeding
- World Health Organization . (2020. b). https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020
- World Health Organization . (2020. c). Frequently asked questions: breastfeeding and COVID-19: For health care workers, 12 May 2020. World Health Organization. [Google Scholar]
- World Health Organization & United Nations Children’s Fund . (2003). Global strategy for infant and young child feeding. WHO. [Google Scholar]
- World Medical Association . (2001). World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. Journal of the American Medical Association, 310(20), 2191–2194.doi:10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]