Abstract
How people respond to health threats can influence their own health and, when people are facing communal risks, even their community’s health. We propose that people commonly respond to health threats by managing their emotions with cognitive strategies such as reappraisal, which can reduce fear and protect mental health. However, because fear can also motivate health behaviors, reducing fear may also jeopardize health behaviors. In two diverse U.S. samples (N = 1,241) tracked across 3 months, sequential and cross-lagged panel mediation models indicated that reappraisal predicted lower fear about an ongoing health threat (COVID-19) and, in turn, better mental health but fewer recommended physical health behaviors. This trade-off was not inevitable, however: The use of reappraisal to increase socially oriented positive emotions predicted better mental health without jeopardizing physical health behaviors. Examining the costs and benefits of how people cope with health threats is essential for promoting better health outcomes for individuals and communities.
Keywords: emotion regulation, reappraisal, fear, positive emotions, health behaviors, mental health, COVID-19, open data, open materials
The way people respond to health threats affects not only their own health but also the health of others. This is particularly true for infectious diseases, where one person’s actions can have downstream impacts for the broader community. Thus, understanding what underlies people’s reactions to health threats and harnessing this knowledge to promote adaptive responses to threats can be fundamental to improving individual and community well-being.
At the heart of how people respond to health threats is the emotion of fear (Folkman & Greer, 2000). Although fear feels unpleasant, it motivates people to protect their physical health by engaging in recommended health behaviors (Harper et al., 2020). However, precisely because fear is unpleasant, people are often—understandably—motivated to reduce fear (Gross, 2015). Reducing one’s day-to-day experience of fear should provide important benefits for longer-term mental health, especially in the face of ongoing health threats (Dieng et al., 2016). But because reducing fear also reduces the motivation it provides, people who successfully reduce fear about a health threat may also be less likely to engage in physical health behaviors that protect not only themselves but also their communities. We examined this dilemma in the present research, focusing on a commonly used form of emotion regulation that can effectively reduce fear: cognitive reappraisal, or reframing situations to change their emotional impact (Gross, 2015).
The present research bridges affective science with health psychology to generate novel predictions about how emotion regulation can influence health and illness. In doing so, this research makes three theoretical contributions. First, the scientific community does not know whether the very forms of emotion regulation designed to help people cope with the stress of health threats can further jeopardize people’s physical health outcomes. We addressed this core gap by examining the effects of reappraisal on people’s real-world health behaviors in the context of a health threat and by providing evidence for the underlying mechanisms of this effect. Second, the present research examined a crucial trade-off of emotion regulation: Although using reappraisal to reduce fear may predict fewer health behaviors, it should also predict better mental health—an unfortunate dilemma that puts people in a difficult situation as they attempt to cope with the stress of a health crisis. By bringing this trade-off to light, this work can help researchers in both the affective sciences and health fields update how they conceptualize the benefits and costs of reappraisal. Third, we investigated an alternative pathway through which the trade-offs of reappraisal can be avoided. Although much research examining emotion regulation in the context of stress focuses on the role of negative emotion, we highlighted the crucial role of positive emotion: Theorizing that positive emotion’s unique features may help people avoid the trade-offs of using reappraisal to decrease fear, we predicted that certain positive emotions would provide emotional relief that can protect mental health without carrying the same costs to health behaviors that can jeopardize physical health. By considering this understudied target of reappraisal, we were able to suggest a potential solution for the drawbacks of reappraisal when people manage threats to their physical health. To test these predictions, we examined two large, diverse U.S. samples across 10 waves of longitudinal data during the COVID-19 pandemic—a powerful threat to both physical and mental health.
The Role of Fear in Responding to Health Threats
When people face significant threats to their health, they often experience fear (Folkman & Greer, 2000). Consistent with functional accounts of emotions (Frijda, 1986), results have shown that this fear serves an important purpose by motivating people to engage in behaviors that can protect health (Mayne, 1999). For example, people who felt afraid of breast cancer were more likely to consider procedures to reduce their risk of developing breast cancer (Tesson et al., 2017), those who felt afraid of sexually transmitted infections were more willing to take a screening test (Shepherd & Smith, 2017), and parents who felt afraid that their child would contract measles were more likely to have their child vaccinated (Feigelman et al., 1993). This evidence suggests that although fear is unpleasant, it can effectively motivate people to engage in behaviors that protect their physical health—and even their community’s health, in the case of communal health risks.
Statement of Relevance.
Health outcomes—both individual and communal—are influenced by how people respond to health threats. Commonly, people respond to these threats by regulating their emotions, a process that can reduce fear and thereby protect mental health. However, because fear can motivate effective health behaviors, reducing fear may also jeopardize the physical health of individuals and their communities. In the context of the salient health threat posed by the COVID-19 pandemic, the present research indicates that although successfully using the emotion-regulation strategy of reappraisal predicted lower fear and, in turn, better mental health, it also predicted lower physical-health-protective behaviors, putting individuals and their communities at risk. However, reappraisal was also used to cultivate positive emotions (e.g., gratitude, inspiration), thereby predicting better mental health without jeopardizing physical health behaviors. These findings are among the first to point to the perils (in addition to the promise) of using emotion regulation in the face of health threats.
As useful as fear can be for motivating physical health behaviors, fear is highly unpleasant (Russell & Barrett, 1999) and can, over time, negatively impact people’s mental health (Kotov et al., 2010). To protect themselves from undesirable or painful emotions, people often use emotion-regulation strategies to reduce these emotions. One particularly common regulation strategy—even when facing health threats (Moskowitz et al., 1996)—is cognitive reappraisal (Ford et al., 2017). Because reappraisal involves changing one’s perspective on the nature of the threat one is facing (Uusberg et al., 2019), it can powerfully shape people’s emotional experiences. For example, reappraisal can be used to minimize or downplay the severity of a threatening situation. Such potent shifts to one’s perspective can, in turn, effectively reduce fear.
The Benefits and Costs of Reappraisal
Reappraisal is typically considered so helpful for managing emotions that it is viewed as a gold-standard regulation strategy and has even become popular in various fields outside of psychology (see Ford & Troy, 2019). In many ways, this popularity is warranted: Reappraisal has been consistently linked to better mental health outcomes when used in general (Aldao et al., 2010) and when used in the context of health threats. For example, using reappraisal to cope with health-related fear predicted lower depression and anxiety in HIV-positive men (Kraaij et al., 2008), in people undergoing infertility treatment (Kraaij et al., 2010), and in newly diagnosed cancer patients (Peh et al., 2016; Wang et al., 2013). On the basis of these findings, one might conclude that reappraisal should be widely used by individuals facing health threats.
In addition to its benefits, however, reappraisal also has drawbacks (Ford & Troy, 2019). By reducing emotions that drive functional behavior, reappraisal can impair motivation to take appropriate action when action is needed most (Feinberg et al., 2020; Troy et al., 2013; van’t Wout et al., 2010), even when that action can protect one’s community (Ford et al., 2019). In the context of health threats, using reappraisal to reduce fear (e.g., by minimizing the severity of the threat) should reduce the motivation that fear provides to avoid these health threats. Although these drawbacks have not yet been examined in the high-impact domain of health threats, one recent study provides suggestive evidence: In line with our reasoning, people who used reappraisal to reduce negative emotions in the face of threat-inducing health messages were less convinced by those messages (i.e., anti-binge-drinking messages; Doré et al., 2019)—a result strongly suggesting that such people would be less likely to follow the health behaviors recommended by the message.
Given the influence that health behaviors can have on social networks (Christakis & Fowler, 2008), using reappraisal to reduce fear of a health threat may affect not only individuals’ physical health outcomes but also community outcomes. For example, when people or communities face an infectious disease, less engagement in health behaviors (e.g., handwashing) can exacerbate the spread of disease. Taken together, prior theory and indirect evidence suggests that using reappraisal to reduce fear in the face of physical health threats may require a crucial trade-off: greater mental health but fewer behaviors that protect physical health of individuals and communities.
An Alternative to Reducing Fear in the Face of Health Threats
Using reappraisal can help reduce fear in the face of health threats and, in turn, protect mental health while also jeopardizing physical health behaviors. But is this trade-off inevitable? Reducing fear is not the only way to feel better, and striving to avoid fear can be problematic in itself (Mennin, 2005). Fortunately, reappraisal can also be used to increase the experience of positive emotions (Shiota & Levenson, 2012), which can promote mental health (Jans-Beken et al., 2019) and help one avoid the trade-offs associated with reducing fear (Cook & Chater, 2010). Even in the face of health threats, reappraisal can be used to reconsider such situations as opportunities for growth, meaning, and connection (Folkman, 1997) and can thereby enhance positive emotional experiences without necessarily minimizing the threat as less severe or consequential. Given this, using reappraisal to cultivate positive emotions is unlikely to interfere with health behaviors. In the high-impact context of communal health threats—when health behaviors are not only self-protective but also community protective—positive emotions that are oriented toward other people (e.g., gratitude, love, and admiration) may even promote preventative physical health behaviors that can keep oneself and others safe.
The Current Investigation
In the current investigation, we bridged affective science with health psychology to test whether using reappraisal to reduce fear evokes a trade-off between mental health and physical-health-protective behaviors. The COVID-19 outbreak provided a unique opportunity to examine this trade-off in the context of a salient and fear-provoking communal health threat. We expected that many people would feel fearful in response to the outbreak, and many would use reappraisal to manage their emotions about the outbreak. We expected that successful reappraisal would predict lower fear and, in turn, better mental health (i.e., reduced depression and anxiety symptoms) but would also predict less engagement in preventative health behaviors recommended by the U.S. Centers for Disease Control and Prevention (CDC; e.g., mask wearing, social distancing). We also tested an alternative pathway that may avoid these trade-offs: whether successful reappraisal can also help people cultivate positive emotions toward other people (e.g., gratitude, inspiration) in the context of the outbreak and, in turn, predict greater mental health without jeopardizing engagement in recommended health behaviors.
To test these questions, we leveraged two multiwave longitudinal samples across a real unfolding health crisis. We recruited two large U.S. samples (total N = 1,241) that were diverse in racial and ethnic identity, political orientation, and socioeconomic status and analyzed 10 waves of data collection across 3 months, beginning in late February 2020 before COVID-19 was declared a pandemic. This design enabled us to capture the time period when the pandemic first emerged and when it became a global crisis, covering this event more comprehensively than research that typically begins after a crisis has occurred. Given the structure of these data, the present research was uniquely able to address how reappraisal predicts change in negative emotion (and positive emotion) and, in turn, change in health behaviors and mental health over time. Specifically, we compared results across two types of mediation models: first capitalizing on our longitudinal design with sequential mediation models (samples A and B) and then providing a stronger test of causality with cross-lagged panel mediation models that control for previous levels of each variable (sample A). Although true causality cannot be tested using observational data, cross-lagged panel models test Granger causality, a statistical concept that in this case means that reappraisal (the hypothesized cause) precedes and predicts emotions (the hypothesized mediator), which in turn precede and predict health behaviors and mental health (the hypothesized outcomes; Cain et al., 2017). This is a key strength of the present longitudinal design, given that we could not ethically manipulate factors expected to reduce health-protective behaviors that are vital for slowing the spread of COVID-19.
Method
Participants
Participants were recruited from Amazon’s Mechanical Turk—an online platform that allowed us to rapidly collect time-sensitive data from diverse participants. Participants were required to be residents of the United States, have a 95% approval rating, and have completed at least 100 tasks on the Mechanical Turk platform. On an a priori basis, data were excluded from measurement occasions in which a participant did not pass all of the provided attention checks, provided incomplete data, or took the survey more than once (for more details about data-quality checks and exclusions, see the Supplemental Material available online). In all models, the size of both samples exceeded best-practice recommendations of 20 participants per parameter estimate and a minimum total sample size of 200 (Kline, 2015).
Sample A
Sample A contained 742 participants originally recruited in February 2020, and the number of participants included in each analysis ranged from 518 to 696 depending on different missing-data patterns for the sequential and cross-lagged panel mediation models. The participants included in at least one analysis ranged from 18 to 75 years old (M = 36.96, SD = 11.18) and were 53% women, 44% men, 3% other gender or did not report gender; 30% African or African American, 22% East Asian or East Asian American, 34% European American/White/Caucasian, 9% South Asian or South Asian American, 4% other racial or ethnic identities; and 50% Democrats, 16% Republicans, and 30% independents. Participants in sample A were recruited to be relatively diverse with respect to ethnic and racial identity.
Sample B
Sample B was completely separate from sample A and consisted of 842 participants originally recruited in February 2020; 545 participants provided data for all of the time points and measures used in the sequential mediation models (cross-lagged panel models comparable with those used in sample A were not possible in sample B). The participants included in the present analyses ranged from 20 to 81 years old (M = 43.22, SD = 13.16) and were 50% women, 49% men, 1% other gender or did not report gender; 6% African or African American, 5% East Asian or East Asian American, 83% European American/White/Caucasian, 3% South Asian or South Asian American, 3% other race or ethnic identities; and 51% Democrats and 49% Republicans. Participants in sample B were recruited to be relatively diverse with respect to political ideology.
Procedure
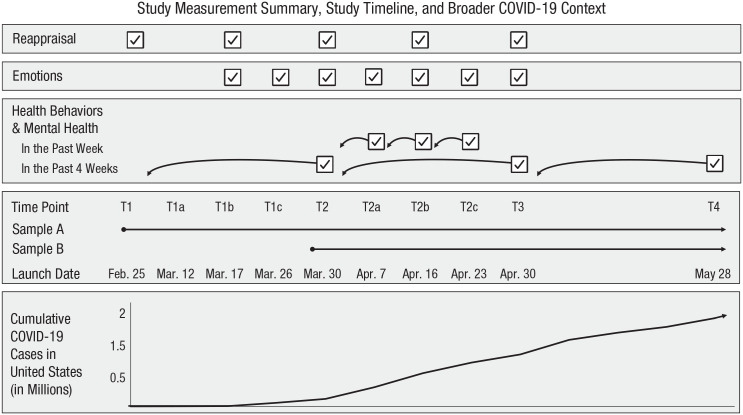
The present research was part of a large longitudinal study aimed at understanding how psychosocial factors influence individuals’ responses to the COVID-19 pandemic. Data from the first 10 waves of data collection were included in the present study. Figure 1 displays the temporal sequencing of each wave of data collection, including when constructs were assessed for samples A and B. Sample A participants were originally recruited for a longitudinal study centered on coping with the stress of the COVID outbreak; these participants were invited to complete a baseline survey in late February (Time 1). Participants who passed attention checks at Time 1 were invited to participate in future waves of the study. Sample B participants were originally recruited for a different longitudinal study centered on coping with the stress of politics; these participants were invited to complete a different baseline survey in mid-February that did not include any COVID-related questions. These participants were invited into the COVID-focused study at Time 2, and participants who passed attention checks at Time 2 were invited to all future waves of the COVID-focused study.
Fig. 1.
Summary of measurements included in the present analyses, the timeline along which these measures were collected for samples A and B, and the broader COVID-19 context, as represented by concurrent cumulative case numbers. Participants in sample B completed a Time 1 survey in mid-February, but it did not include any measures related to COVID (and thus is not included in any analyses reported in the present article). Data for the COVID-19 graph were obtained from Ritchie et al. (2021). T = time.
After the baseline survey (Time 1), all participants were invited to complete longer monthly surveys in late March, late April, and late May (Time 2, Time 3, Time 4, respectively) and shorter weekly surveys in March (Time 1a, Time 1b, and Time 1c; sample A only) and April (Time 2a, Time 2b, and Time 2c). The longer monthly surveys ranged from approximately 30 to 35 min, and participants were compensated between $4.50 and $5.00 for their time depending on the length of the survey. The shorter weekly surveys ranged from 1 min to 20 min, and participants were compensated between $0.25 and $3.50 for their time depending on the length of the survey (effective median hourly rate = ~$9). All procedures were approved by the ethics board at the University of Toronto (Protocol No. 33962).
Measures
Reappraisal
Participants completed separate ratings of how frequently they used reappraisal and how successfully they used reappraisal when feeling stressed about the COVID-19 outbreak at Time 1, Time 1b, Time 2, Time 2b, and Time 3 in sample A and at Time 2, Time 2b, and Time 3 in sample B. First, participants rated four reappraisal-frequency items on a scale from 0 (I never try this) to 6 (I always try this). Example items were, “When you want to feel less negative emotion about the recent coronavirus outbreak (such as anxiety, disgust, or frustration), do you try to change the way you’re thinking about the outbreak?” and “When you want to feel more positive emotion about the outbreak (such as hope or relief), do you try to change the way you’re thinking about the outbreak?” Then participants rated their reappraisal success on a scale from 0 (I am definitely unable to do this) to 6 (I am definitely able to do this). Example items were, “When you want to feel less negative emotion about the recent outbreak (such as anxiety, disgust, or frustration), are you able to change the way you’re thinking about the outbreak, if you try?” and “When you want to feel more positive emotion about the outbreak (such as hope or relief), are you successful at changing the way you’re thinking about the outbreak, if you try?” (all items for both reappraisal frequency and success are reported in the Supplemental Material). We computed a mean reappraisal-frequency composite and a mean reappraisal-success composite at each time point (αs = .88–.93). For illustrative purposes, we report descriptive statistics for reappraisal frequency below. However, for our inferential analyses, we focus on reappraisal success, given that emotion-regulation successes and attempts are conceptually and empirically distinct (Ford et al., 2017), and it is the successful use of a given strategy that should impact emotional outcomes, not merely the number of times people attempt the strategy.
Emotions
We assessed emotions about the COVID-19 pandemic at each time point. Participants responded to the prompt “In the past day or two, to what extent have you felt these emotions when thinking about the outbreak?” Response options ranged from 0 (not at all) to 6 (extremely). Socially oriented positive emotions were introduced beginning at Time 1b, and thus earlier measurements of emotions were not used in the present analyses. We assessed up to 24 emotion items at each time point, but on an a priori basis, focused on the two item triplets related to fear and three item triplets related to socially oriented positive emotions for the present study. To assess fear, we used the following item triplets: “worried, nervous, fearful” and “panicked, alarmed, freaked out” (αs = .81–.88). To assess socially oriented positive emotions, we used the following item triplets: “love, closeness, trust”; “inspired, uplifted, elevated”; and “grateful, appreciative, thankful” (αs = .80–.86).
Preliminary analyses revealed that although fear and socially oriented positive emotions are related, they are also empirically distinct: In a multilevel model that predicted socially oriented positive emotions from fear, there was a modest negative association between fear and socially oriented positive emotions at the between-persons level: Sample A: b = −0.23, p < .001; Sample B: b = −0.23, p < .001 (these variables are z-standardized here so that these coefficients can be roughly interpreted as βs). To examine the specificity of the link between fear and health behaviors, we also considered other negative emotions (i.e., the relatively social negative emotions of guilt and shame), and to examine the specificity of the link between socially oriented positive emotions and health behaviors, we also considered other positive emotions (i.e., the relatively less social emotions of happiness and amusement). These findings (reported in the Supplemental Material) indicate that the pattern of results reported here in the main text are specific to fear and socially oriented positive emotions: Although reappraisal predicted lower negative and greater positive emotions broadly construed (consistent with the broad hedonic benefits of reappraisal), only fear and socially oriented positive emotions were consistent predictors of health behaviors (consistent with a functional account of particular emotions).
Health behaviors
We assessed the frequency with which participants engaged in COVID-19 preventative health behaviors recommended by the CDC. In the weekly assessments, beginning with Time 2a, participants rated how often they engaged in each of four health behaviors over the past week (i.e., practicing hygiene, wearing a face mask, social distancing, and social isolation; see the Supplemental Material for exact item wording). In the monthly assessments, beginning with Time 2, participants rated how often they engaged in each of five health behaviors over the past month (i.e., practicing hygiene, wearing a face mask, sanitizing surfaces, social distancing, and social isolation). Response options ranged from 0 (I did not do this) to 4 (I very often or always did this). We computed a mean composite across the four (or five) health behaviors at each time point (αs = .60–.80).
Mental health symptoms
We assessed two aspects of mental health: depressive symptoms and anxiety symptoms. In the weekly assessments, beginning at Time 2a, we used single-item measures to assess depression and anxiety in the past week: “This week, I felt depressed” and “This week, I felt anxious.” Response options ranged from 0 (I do not agree with this at all) to 6 (I completely agree with this). We computed the mean of the two items at each time point (αs = .79–.82). In the monthly assessments, we used the Center for Epidemiological Studies Depression Scale (Radloff, 1977) to assess depression symptoms over the past 4 weeks and the Hospital Anxiety and Depression Scale (Snaith, 2003) to assess anxiety symptoms over the past 4 weeks. To create an aggregate score, we first z-standardized each scale score at each time point and then computed a mean mental health composite of the two z-scored variables at each time point (α = .91).
Analytic strategy
To examine the effects of reappraisal on emotions and, in turn, on health behaviors and mental health, we used two types of mediation models: 2-1-2 sequential mediation models and cross-lagged panel mediation models. Note that all reported coefficients for these analyses are unstandardized.
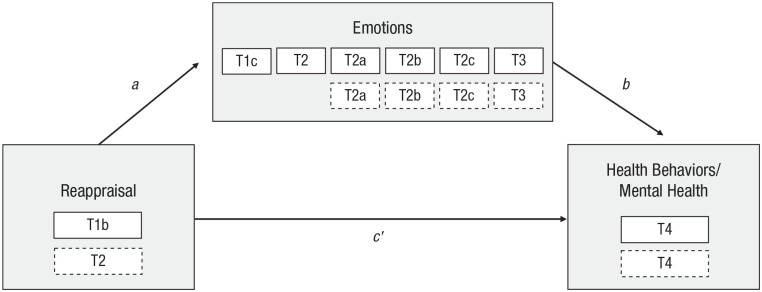
Sequential mediation
In the first set of mediation models, we used sequential mediation, a form of longitudinal mediation (Cain et al., 2017). Longitudinal mediation is preferable to cross-sectional mediation because it allows time for the predictor to influence the mediator and for the mediator to influence the outcome (Maxwell & Cole, 2007). On an a priori basis, we chose Time 1b for our measure of reappraisal success in sample A because this measurement occasion took place approximately 1 week after the World Health Organization declared COVID-19 a pandemic, allowing time for emotional responses to the pandemic and, thus, emotion regulation to take place. For sample B, we used the first measurement occasion at which reappraisal was assessed, Time 2. To provide parallel tests across similar time spans in the 2-1-2 sequential and cross-lagged panel mediation models, we chose Time 4 for the outcome measures in both samples. We used all available measurement occasions of emotions between our reappraisal measure and our outcome measures. We used a 2-1-2 random-effects sequential mediation model in which the predictor (reappraisal) and the outcome (health behaviors or mental health symptoms) were included at Level 2 (i.e., one observation per participant) and repeated measures of the mediator (emotions) were included at Level 1 (i.e., multiple observations per participant consisting of one observation per measurement occasion), as described in Preacher et al. (2011; see Fig. 2).
Fig. 2.
Path diagram of 2-1-2 sequential mediation model, in which the predictor (reappraisal) and the outcome (health behaviors or mental health symptoms) were included at Level 2 and repeated measures of the mediator (emotions) were included at Level 1. White boxes with solid outlines indicate the time points from which data from sample A were drawn. White boxes with dashed outlines indicate time points from which data from sample B were drawn. T = time.
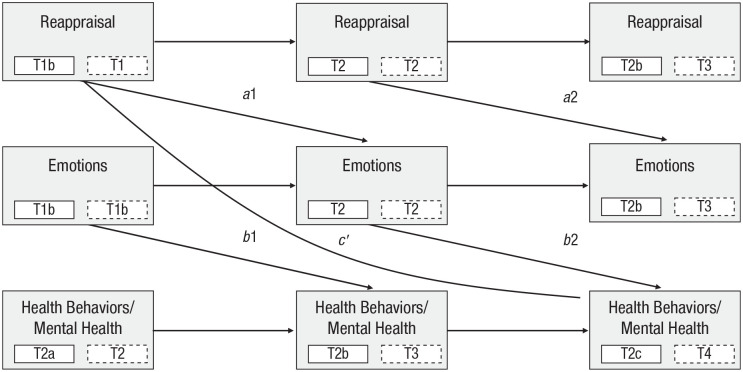
Cross-lagged panel mediation
Although sequential mediation allows effects to take place over time, it does not account for previous values of the variables in the model. To address this limitation, we also tested cross-lagged panel mediation models (Selig & Preacher, 2009) in sample A (requisite data were not available in sample B because the use of reappraisal in response to COVID was not assessed until Time 2). Cross-lagged panel models test the prospective effect of individual differences in a construct (in this case, reappraisal) on change in individual differences in another construct (in this case, emotions, health behaviors, and mental health). By accounting for previous values of the variables with autoregressive paths, cross-lagged panel mediation provides a stronger test of causality relative to sequential mediation (Cain et al., 2017).
One challenge of lagged analyses is specifying a time lag that approximates the true causal lag (Selig & Preacher, 2009). To address this, we tested two versions of a cross-lagged panel mediation model that differed according to the specified time lag (see Fig. 3). In the first model, we used a time lag of approximately 1 week between measurement occasions. In the second model, we used a time lag of approximately 1 month between measurement occasions. In the weekly model, the predictor (reappraisal) and the mediator (emotions) were always assessed at the same time as one another (at Time 1b, Time 2, and Time 2b), and the outcomes (health behaviors and mental health symptoms) were assessed approximately 1 week later (at Time 2, Time 2b, and Time 2c). This was done because the measures used to assess the outcomes referred to health behaviors and mental health symptoms “in the past week.” We used a similar approach for the monthly models: Reappraisal and emotions were assessed at the same time as one another (Time 1, Time 2, Time 3), and health behaviors and mental health symptoms were assessed 1 month later (Time 2, Time 3, Time 4), because the measures used to assess the outcomes referred to health behaviors and mental health symptoms “in the past month.” This monthly model had one exception: Because socially oriented positive emotions were not assessed at Time 1, the first wave of emotion measurements occurred at Time 1b.
Fig. 3.
Path diagram of cross-lagged panel mediation model (sample A only) testing the prospective effect of the predictor (reappraisal) on change in the outcome (health behaviors or mental health) via change in the mediator (emotions). White boxes with solid outlines indicate the time points that were included in the weekly models. White boxes with dashed outlines indicate time points that were included in the monthly models. Note that to estimate a single indirect effect, we constrained a1 and a2 to be equal and b1 and b2 to be equal. T = time.
Results
Data and statistical code to reproduce all results is available at https://osf.io/y8kp3/. Descriptive statistics for study variables are shown in Table S1 in the Supplemental Material.
Fear and socially oriented positive emotions were common responses to the COVID-19 outbreak: 80% to 94% of participants experienced at least some fear, and 89% to 97% of participants experienced at least some socially oriented positive emotions across measurement occasions and samples. Most people—97% in both samples—used reappraisal to at least some degree in response to emotions about the COVID-19 outbreak at the first assessment point. The average reappraisal-frequency values (Sample A: M = 3.13, SD = 1.33; Sample B: M = 3.10, SD = 1.39) corresponded to people using reappraisal “sometimes” in daily life, on average, and there was wide individual variability. The average reappraisal-success values (Sample A: M = 3.47, SD = 1.39; Sample B: M = 3.37, SD = 1.48) corresponded to people being “somewhat” to “moderately” successful, and there was substantial individual variation. These descriptive findings set the stage for examining how people’s successful use of reappraisal predicts downstream emotional experiences and, in turn, health behaviors and mental health.
Fear and health behaviors
In the sequential mediation models (see Table 1), reappraisal predicted lower fear, which in turn predicted fewer health behaviors. The indirect effect of reappraisal on fewer health behaviors, mediated by fear, was statistically significant in both samples.
Table 1.
Results of Sequential and Cross-Lagged Panel Mediation Models With Reappraisal Predicting Fear and, in Turn, Health Behaviors and Mental Health
| Sample and path | Outcome: health behaviors | Outcome: mental health symptoms | ||||||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | SE | p | b | 95% CI | SE | p | |
| Sequential mediation model | ||||||||
| Sample A (n = 696) | ||||||||
| a path | −0.309 | [−0.394, −0.223] | 0.044 | < .001 | −0.311 | [−0.396, −0.225] | 0.044 | < .001 |
| b path | 0.129 | [0.077, 0.182] | 0.027 | < .001 | 0.441 | [0.393, 0.489] | 0.024 | < .001 |
| c′ path | 0.022 | [−0.033, 0.077] | 0.028 | .430 | −0.014 | [−0.065, 0.037] | 0.026 | .585 |
| a path × b path (indirect effect) | −0.040 | [−0.060, −0.020] | 0.010 | < .001 | −0.137 | [−0.178, −0.097] | 0.021 | < .001 |
| Sample B (n = 545) | ||||||||
| a path | −0.479 | [−0.554, −0.404] | 0.038 | < .001 | −0.479 | [−0.554, −0.403] | 0.039 | < .001 |
| b path | 0.165 | [0.101, 0.229] | 0.033 | < .001 | 0.513 | [0.464, 0.563] | 0.025 | < .001 |
| c′ path | 0.064 | [0.004, 0.124] | 0.031 | .036 | −0.019 | [−0.065, 0.027] | 0.024 | .415 |
| a path × b path (indirect effect) | −0.079 | [−0.112, −0.046] | 0.017 | < .001 | −0.246 | [−0.291, −0.200] | 0.023 | < .001 |
| Cross-lagged panel mediation model | ||||||||
| Sample A weekly (n = 530) | ||||||||
| a path | −0.067 | [−0.123, −0.011] | 0.029 | .019 | −0.067 | [−0.123, −0.010] | 0.029 | .020 |
| b path | 0.026 | [0.009, 0.042] | 0.008 | .002 | 0.091 | [0.046, 0.135] | 0.023 | < .001 |
| c′ path | 0.009 | [−0.019, 0.037] | 0.014 | .517 | −0.011 | [−0.077, 0.054] | 0.033 | .733 |
| a path × b path (indirect effect) | −0.002 | [−0.004, 0.000] | 0.001 | .062 | −0.006 | [−0.012, 0.000] | 0.003 | .044 |
| Sample A monthly (n = 530) | ||||||||
| a path | −0.089 | [−0.146, −0.031] | 0.029 | .002 | −0.087 | [−0.144, −0.029] | 0.029 | .003 |
| b path | 0.030 | [0.008, 0.051] | 0.011 | .008 | 0.027 | [0.004, 0.049] | 0.011 | .020 |
| c′ path | 0.020 | [−0.016, 0.057] | 0.019 | .275 | 0.008 | [−0.027, 0.042] | 0.018 | .656 |
| a path × b path (indirect effect) | −0.003 | [−0.005, 0.000] | 0.001 | .045 | −0.002 | [−0.005, 0.000] | 0.001 | .066 |
Note: CI = confidence interval.
The cross-lagged panel mediation models (Table 1) replicated the sequential mediation models: Reappraisal predicted lower fear, which in turn predicted fewer health behaviors. The indirect effect of reappraisal on fewer health behaviors, mediated by fear, was marginally significant in the weekly model and was statistically significant in the monthly model.
Fear and mental health symptoms
In the sequential mediation models (see Table 1), reappraisal was associated with lower fear, which in turn predicted fewer mental health symptoms (i.e., better mental health). The indirect effect of reappraisal on fewer mental health symptoms, mediated by fear, was statistically significant in both samples.
The cross-lagged panel mediation models (Table 1) replicated the sequential mediation models: Reappraisal predicted lower fear, which in turn predicted fewer mental health symptoms. The indirect effect of reappraisal on fewer mental health symptoms, mediated by fear, was statistically significant in the weekly model and marginally significant in the monthly model.
Socially oriented positive emotions and health behaviors
In the sequential mediation models (see Table 2), reappraisal predicted greater socially oriented positive emotions, which in turn predicted greater health behaviors. The indirect effect of reappraisal on greater health behaviors, mediated by socially oriented positive emotions, was statistically significant in both samples.
Table 2.
Results of Sequential and Cross-Lagged Panel Mediation Models With Reappraisal Predicting Socially Oriented Positive Emotions and, in Turn, Health Behaviors and Mental Health
| Sample and path | Outcome: health behaviors | Outcome: mental health symptoms | ||||||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | SE | p | b | 95% CI | SE | p | |
| Sequential mediation model | ||||||||
| Sample A (n = 696) | ||||||||
| a path | 0.314 | [0.239, 0.389] | 0.038 | < .001 | 0.316 | [0.241, 0.391] | 0.038 | < .001 |
| b path | 0.096 | [0.037, 0.155] | 0.030 | .001 | −0.155 | [−0.223, −0.087] | 0.034 | < .001 |
| c′ path | −0.060 | [−0.115, −0.004] | 0.028 | .035 | −0.141 | [−0.205, −0.076] | 0.033 | < .001 |
| a path × b path (indirect effect) | 0.030 | [0.010, 0.050] | 0.010 | .003 | −0.049 | [−0.073, −0.025] | 0.012 | < .001 |
| Sample B (n = 545) | ||||||||
| a path | 0.392 | [0.313, 0.471] | 0.040 | < .001 | 0.391 | [0.312, 0.470] | 0.040 | < .001 |
| b path | 0.103 | [0.041, 0.164] | 0.031 | .001 | −0.194 | [−0.257, −0.131] | 0.032 | < .001 |
| c′ path | −0.058 | [−0.115, −0.001] | 0.029 | .048 | −0.192 | [−0.250, −0.134] | 0.030 | < .001 |
| a path × b path (indirect effect) | 0.040 | [0.015, 0.066] | 0.013 | .002 | −0.076 | [−0.105, −0.047] | 0.015 | < .001 |
| Cross-lagged panel mediation model | ||||||||
| Sample A weekly (n = 530) | ||||||||
| a path | 0.159 | [0.104, 0.214] | 0.028 | < .001 | 0.160 | [0.105, 0.215] | 0.028 | < .001 |
| b path | 0.007 | [−0.010, 0.024] | 0.009 | .415 | −0.028 | [−0.068, 0.013] | 0.021 | .183 |
| c′ path | −0.002 | [−0.029, 0.026] | 0.014 | .902 | −0.028 | [−0.094, 0.037] | 0.033 | .400 |
| a path × b path (indirect effect) | 0.001 | [−0.002, 0.004] | 0.001 | .420 | −0.004 | [−0.011, 0.002] | 0.003 | .195 |
| Sample A monthly (n = 530) | ||||||||
| a path | 0.117 | [0.062, 0.171] | 0.028 | < .001 | 0.115 | [0.061, 0.169] | 0.028 | < .001 |
| b path | 0.007 | [−0.016, 0.031] | 0.012 | .529 | 0.002 | [−0.018, 0.022] | 0.010 | .820 |
| c′ path | 0.008 | [−0.028, 0.044] | 0.019 | .665 | 0.000 | [−0.034, 0.035] | 0.018 | .983 |
| a path × b path (indirect effect) | 0.001 | [−0.002, 0.004] | 0.001 | .533 | 0.000 | [−0.002, 0.003] | 0.001 | .820 |
Note: CI = confidence interval.
The cross-lagged panel mediation models (Table 2) indicated that reappraisal predicted greater socially oriented positive emotions, replicating the results of the sequential mediation models. However, unlike in the sequential mediation models, socially oriented positive emotions did not predict greater health behaviors in the cross-lagged panel models. Because of this, the indirect effect of reappraisal on health behaviors, mediated by socially oriented positive emotions, was nonsignificant in the weekly and monthly models. 1
Socially oriented positive emotions and mental health symptoms
In the sequential mediation models (see Table 2), reappraisal predicted greater socially oriented positive emotions, which in turn predicted fewer mental health symptoms (i.e., better mental health). The indirect effect of reappraisal on fewer mental health symptoms, mediated by socially oriented positive emotions, was statistically significant in both samples.
The cross-lagged panel mediation models (Table 2) again indicated that reappraisal predicted greater socially oriented positive emotions, replicating the sequential mediation models. However, unlike in the sequential mediation models, socially oriented positive emotions did not predict mental health symptoms in the cross-lagged panel models. Because of this, the indirect effect of reappraisal on mental health symptoms, mediated by socially oriented positive emotions, was nonsignificant in the weekly and monthly models.
Discussion
Bridging affective science with health psychology, the present research provides several theoretical contributions. When one faces a frightening health crisis, it is understandable to want to seek comfort. However, feeling better can have important costs that can jeopardize not only one’s personal health but also the health of the community. In two diverse samples across 3 months of an unfolding pandemic and using multiple types of longitudinal mediation analyses, we found that successfully reappraising the situation surrounding a pandemic predicted less fear, which in turn predicted better long-term mental health. However, by reducing fear, successful reappraisals also predicted less engagement in health behaviors that were recommended by the CDC to slow the spread of infection, thereby generating potentially fatal risk to individuals and their communities. This research is among the first to indicate that the very strategies meant to help people cope with the stress of health threats may further jeopardize people’s physical health outcomes, and these findings provide evidence for the underlying mechanisms of these outcomes. From a public health perspective, our findings suggest that health messages that emphasize reduced fear (e.g., “keep calm and carry on”) may actually backfire and promote fewer health behaviors. These results underscore an unfortunate dilemma of seeking comfort during times of stress, when comfort is most needed.
There is more than one way to seek comfort, however. The present findings extend beyond prior work on the costs of reappraisal (Ford & Troy, 2019), suggesting a potential solution: Reappraisal predicted increased socially oriented positive emotions (e.g., gratitude, inspiration), even in the face of a global health crisis. Indeed, 89% to 97% of our sample reported feeling at least some socially oriented positive emotions within the first 3 months of the COVID-19 pandemic (comparable with the prevalence of fear: 80%–94%). Importantly, across all of our well-powered longitudinal analyses, we found no evidence that socially oriented positive emotions interfered with people’s motivation to engage in CDC-recommended health behaviors. People were able to experience the comfort of these positive emotional experiences without jeopardizing their own or others’ health. In fact, in the sequential mediation models, socially oriented positive emotions predicted greater engagement in health behaviors. In the cross-lagged panel models, the effect of socially oriented positive emotions of health behaviors was null. Although we caution against interpreting null results as evidence against an effect, the 95% confidence intervals around these null effects are consistent with a negligible negative effect to a small positive effect.
In addition to these contributions, the present research has several limitations that suggest key directions for future work. First, although the present results were replicated across multiple diverse U.S. samples, time frames, and analysis types, future research is needed to confirm whether reappraisal influences people’s responses in the context of other cultures (e.g., which differ in outbreak severity, health behavior guidelines, and culturally informed responses to emotions) or other types of health threats. Second, we assessed individual’s use of reappraisal at a broad level (i.e., changing how one is thinking) and focused on hedonic regulation (i.e., striving to feel better), but reappraisal can be used in many different ways. For example, specific reappraisal tactics may have unique outcomes (e.g., minimizing vs. benefit finding; Shiota & Levenson, 2012), reappraisal could be used to increase negative emotions (e.g., to achieve instrumental benefits; Tamir, 2015), or reappraisal could be used to change other people’s emotions in the context of a collective crisis (Netzer et al., 2020). Future research would benefit from a more comprehensive examination of reappraisal. Finally, because the present research used observational data, we cannot draw strong causal conclusions. The cross-lagged panel models provide evidence for directionality but not necessarily causality. Specifically, because they included autoregressive paths, these models account for preexisting individual differences in the predictor variables as well as shared variance with correlated third variables. Despite the strengths of these models, it is possible that third variables change with change in the predictor variables or that third variables predispose individuals to change in the predictor variables. These possibilities are an inherent limitation to nonexperimental work, and future work is needed to investigate and untangle potential third variables.
This research provides a novel test of the complex trade-offs associated with seeking comfort during a large-scale health threat. Emotion regulation is clearly a powerful tool and as such must be wielded with caution and knowledge of both its benefits and its costs.
Supplemental Material
Supplemental material, sj-docx-1-pss-10.1177_09567976211024260 for Coping With Health Threats: The Costs and Benefits of Managing Emotions by Angela M. Smith, Emily C. Willroth, Arasteh Gatchpazian, Amanda J. Shallcross, Matthew Feinberg and Brett Q. Ford in Psychological Science
Although these null results should not be interpreted as evidence for the absence of an effect, the 95% confidence intervals around these null effects are consistent with a negligible negative effect to a small positive effect of socially oriented positive emotions on health behaviors. Thus, the full range of these 95% confidence intervals is consistent with the hypothesis that socially oriented positive emotions are not associated with meaningfully reduced health behaviors.
Footnotes
ORCID iDs: Angela M. Smith  https://orcid.org/0000-0003-2933-2482
https://orcid.org/0000-0003-2933-2482
Emily C. Willroth  https://orcid.org/0000-0002-4780-6883
https://orcid.org/0000-0002-4780-6883
Matthew Feinberg  https://orcid.org/0000-0001-8626-1620
https://orcid.org/0000-0001-8626-1620
Brett Q. Ford  https://orcid.org/0000-0002-7943-4447
https://orcid.org/0000-0002-7943-4447
Supplemental Material: Additional supporting information can be found at http://journals.sagepub.com/doi/suppl/10.1177/09567976211024260
Transparency
Action Editor: Daniela Schiller
Editor: Patricia J. Bauer
Author Contributions
B. Q. Ford, A. M. Smith, A. Gatchpazian, A. J. Shallcross, and M. Feinberg designed the study. All the authors contributed to the analysis plan, and E. C. Willroth analyzed the data. A. M. Smith, E. C. Willroth, A. Gatchpazian, and B. Q. Ford wrote the first draft of the manuscript. All the authors provided substantive revisions and approved the final manuscript for submission.
Declaration of Conflicting Interests: The author(s) declared that there were no conflicts of interest with respect to the authorship or the publication of this article.
Funding: This work was supported by the Social Science and Humanities Research Council of Canada, the University of Toronto, and the Mind and Life Institute.
Open Practices: All data, analysis code, and materials have been made publicly available via OSF and can be accessed at https://osf.io/y8kp3/. The design and analysis plans for the study were not preregistered. This article has received the badges for Open Data and Open Materials. More information about the Open Practices badges can be found at http://www.psychologicalscience.org/publications/badges.


References
- Aldao A., Nolen-Hoeksema S., Schweizer S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychological Review, 30, 217–237. [DOI] [PubMed] [Google Scholar]
- Cain M. K., Zhang Z., Bergeman C. S. (2017). Time and other considerations in mediation design. Educational and Psychological Measurement, 78(6), 952–972. 10.1177/0013164417743003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis N. A., Fowler J. H. (2008). The collective dynamics of smoking in a large social network. New England Journal of Medicine, 358(21), 2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook E., Chater A. (2010). Are happier people, healthier people? The relationship between perceived happiness, personal control, BMI and health preventive behaviours. International Journal of Health Promotion and Education, 48(2), 58–64. 10.1080/14635240.2010.10708183 [DOI] [Google Scholar]
- Dieng M., Butow P. N., Costa D. S. J., Morton R. L., Menzies S. W., Mireskandari S., Tesson S., Mann G. J., Cust A. E., Kasparian N. A. (2016). Psychoeducational intervention to reduce fear of cancer recurrence in people at high risk of developing another primary melanoma: Results of a randomized controlled trial. Journal of Clinical Oncology, 34(36), 4405–4414. 10.1200/jco.2016.68.2278 [DOI] [PubMed] [Google Scholar]
- Doré B. P., Tompson S. H., O’Donnell M. B., An L. C., Strecher V., Falk E. B. (2019). Neural mechanisms of emotion regulation moderate the predictive value of affective and value-related brain responses to persuasive messages. The Journal of Neuroscience, 39(7), 1293–1300. 10.1523/JNEUROSCI.1651-18.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feigelman S., Stanton B., Rubin J. D., Cartelli N. A. (1993). Effectiveness of family notification efforts and compliance with measles post-exposure prophylaxis. Journal of Community Health, 18(2), 83–93. 10.1007/bf01324417 [DOI] [PubMed] [Google Scholar]
- Feinberg M., Ford B. Q., Flynn F. J. (2020). Rethinking reappraisal: The double-edged sword of regulating negative emotions in the workplace. Organizational Behavior and Human Decision Processes, 161, 1–19. 10.1016/j.obhdp.2020.03.005 [DOI] [Google Scholar]
- Folkman S. (1997). Positive psychological states and coping with severe stress. Social Science & Medicine, 45(8), 1207–1221. 10.1016/s0277-9536(97)00040-3 [DOI] [PubMed] [Google Scholar]
- Folkman S., Greer S. (2000). Promoting psychological well-being in the face of serious illness: When theory, research and practice inform each other. Psycho-Oncology, 9(1), 11–19. [DOI] [PubMed] [Google Scholar]
- Ford B. Q., Feinberg M., Lam P., Mauss I. B., John O. P. (2019). Using reappraisal to regulate negative emotion after the 2016 U.S. Presidential election: Does emotion regulation trump political action? Journal of Personality and Social Psychology, 117(5), 998–1015. 10.1037/pspp0000200 [DOI] [PubMed] [Google Scholar]
- Ford B. Q., Karnilowicz H. R., Mauss I. B. (2017). Understanding reappraisal as a multicomponent process: The psychological health benefits of attempting to use reappraisal depend on reappraisal success. Emotion, 17(6), 905–911. 10.1037/emo0000310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford B. Q., Troy A. S. (2019). Reappraisal reconsidered: A closer look at the costs of an acclaimed emotion-regulation strategy. Current Directions in Psychological Science, 28(2), 195–203. 10.1177/0963721419827526 [DOI] [Google Scholar]
- Frijda N. (1986). The emotions. Cambridge University Press. [Google Scholar]
- Gross J. J. (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. [Google Scholar]
- Harper C. A., Satchell L. P., Fido D., Latzman R. D. (2020). Functional fear predicts public health compliance in the COVID-19 pandemic. International Journal of Mental Health and Addiction. Advance online publication. 10.1007/s11469-020-00281-5 [DOI] [PMC free article] [PubMed]
- Jans-Beken L., Jacobs N., Janssens M., Peeters S., Reijnders J., Lechner L., Lataster J. (2019). Gratitude and health: An updated review. The Journal of Positive Psychology, 15(6), 743–782. 10.1080/17439760.2019.1651888 [DOI] [Google Scholar]
- Kline R. B. (2015). Principles and practice of structural equation modeling. Guilford Publications. [Google Scholar]
- Kotov R., Gamez W., Schmidt F., Watson D. (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136(5), 768–821. 10.1037/a0020327 [DOI] [PubMed] [Google Scholar]
- Kraaij V., Garnefski N., Schroevers M. J., Weijmer J., Helmerhorst F. (2010). Cognitive coping, goal adjustment, and depressive and anxiety symptoms in people undergoing infertility treatment. Journal of Health Psychology, 15(6), 876–886. 10.1177/1359105309357251 [DOI] [PubMed] [Google Scholar]
- Kraaij V., Van Der Veek S. M. C., Garnefski N., Schroevers M., Witlox R., Maes S. (2008). Coping, goal adjustment, and psychological well-being in HIV-infected men who have sex with men. AIDS Patient Care and STDs, 22(5), 395–402. 10.1089/apc.2007.0145 [DOI] [PubMed] [Google Scholar]
- Maxwell S. E., Cole D. A. (2007). Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods, 12(1), 23–44. [DOI] [PubMed] [Google Scholar]
- Mayne T. J. (1999). Negative affect and health: The importance of being earnest. Cognition & Emotion, 13(5), 601–635. 10.1080/026999399379203 [DOI] [Google Scholar]
- Mennin D. S. (2005). Emotion and the acceptance-based approaches to the anxiety disorders. In Orsillo S. M., Roemer L. (Eds.), Acceptance and mindfulness-based approaches to anxiety: Conceptualization and treatment (pp. 37–68). Springer. 10.1007/0-387-25989-9_2 [DOI] [Google Scholar]
- Moskowitz J. T., Folkman S., Collette L., Vittinghoff E. (1996). Coping and mood during aids-related caregiving and bereavement. Annals of Behavioral Medicine, 18(1), 49–57. 10.1007/bf02903939 [DOI] [PubMed] [Google Scholar]
- Netzer L., Halperin E., Tamir M. (2020). Be afraid, be very afraid! Motivated intergroup emotion regulation. Personality and Social Psychology Bulletin, 46(11), 1596–1613. 10.1177/0146167220910833 [DOI] [PubMed] [Google Scholar]
- Peh C. X., Liu J., Bishop G. D., Chan H. Y., Chua S. M., Kua E. H., Mahendran R. (2016). Emotion regulation and emotional distress: The mediating role of hope on reappraisal and anxiety/depression in newly diagnosed cancer patients. Psycho-Oncology, 26(8), 1191–1197. 10.1002/pon.4297 [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Zhang Z., Zyphur M. J. (2011). Alternative methods for assessing mediation in multilevel data: The advantages of multilevel SEM. Structural Equation Modeling, 18(2), 161–182. [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. [Google Scholar]
- Ritchie H., Ortiz-Ospina E., Beltekian D., Mathieu E., Hasell J., Macdonald B., Giattino C., Appel C., Rodés-Guirao L., Roser M. (2021). United States: Coronavirus pandemic country profile. Our World in Data. https://ourworldindata.org/coronavirus/country/united-states?country=~USA [Google Scholar]
- Russell J. A., Barrett L. F. (1999). Core affect, prototypical emotional episodes, and other things called emotion: Dissecting the elephant. Journal of Personality and Social Psychology, 76(5), 805–819. 10.1037/0022-3514.76.5.805 [DOI] [PubMed] [Google Scholar]
- Selig J. P., Preacher K. J. (2009). Mediation models for longitudinal data in developmental research. Research in Human Development, 6(2–3), 144–164. [Google Scholar]
- Shepherd L., Smith M. A. (2017). The role of fear in predicting sexually transmitted infection screening. Psychology & Health, 32(7), 876–894. 10.1080/08870446.2017.1307375 [DOI] [PubMed] [Google Scholar]
- Shiota M. N., Levenson R. W. (2012). Turn down the volume or change the channel? Emotional effects of detached versus positive reappraisal. Journal of Personality and Social Psychology, 103(3), 416–429. 10.1037/a0029208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snaith R. P. (2003). The Hospital Anxiety and Depression Scale. Health and Quality of Life Outcomes, 1(1), Article 29. 10.1186/1477-7525-1-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamir M. (2015). Why do people regulate their emotions? A taxonomy of motives in emotion regulation. Personality and Social Psychology Review, 20(3), 199–222. 10.1177/1088868315586325 [DOI] [PubMed] [Google Scholar]
- Tesson S., Richards I., Porter D., Phillips K.-A., Rankin N., Costa D., Musiello T., Marvin M., Butow P. (2017). Women’s preferences for contralateral prophylactic mastectomy following unilateral breast cancer: What risk-reduction makes it worthwhile? The Breast, 31, 233–240. 10.1016/j.breast.2016.11.025 [DOI] [PubMed] [Google Scholar]
- Troy A. S., Shallcross A. J., Mauss I. B. (2013). A person-by-situation approach to emotion regulation: Cognitive reappraisal can either help or hurt, depending on the context. Psychological Science, 24(12), 2505–2514. 10.1177/0956797613496434 [DOI] [PubMed] [Google Scholar]
- Uusberg A., Taxer J. L., Yih J., Uusberg H., Gross J. J. (2019). Reappraising reappraisal. Emotion Review, 11, 267–282. 10.1177/1754073919862617 [DOI] [Google Scholar]
- van’t Wout M., Chang L. J., Sanfey A. G. (2010). The influence of emotion regulation on social interactive decision-making. Emotion, 10(6), 815–821. 10.1037/a0020069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Yi J., He J., Chen G., Li L., Yang Y., Zhu X. (2013). Cognitive emotion regulation strategies as predictors of depressive symptoms in women newly diagnosed with breast cancer. Psycho-Oncology, 23(1), 93–99. 10.1002/pon.3376 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-pss-10.1177_09567976211024260 for Coping With Health Threats: The Costs and Benefits of Managing Emotions by Angela M. Smith, Emily C. Willroth, Arasteh Gatchpazian, Amanda J. Shallcross, Matthew Feinberg and Brett Q. Ford in Psychological Science