Abstract
Background and purpose
Hashimoto thyroiditis (HT) is the most common inflammatory autoimmune thyroid disease and also the most common cause of hypothyroidism in developed countries. There is evidence of the role of HT in developing thyroid cancers (TCs). This study investigated the association between HT and different types of TCs.
Methods
Results of a comprehensive search in three major databases, as well as hand searching, were screened in title/abstract and full-text stages and the relevant data were extracted from the studies that met the inclusion criteria. Risk of bias (RoB) was assessed using the Joanna Briggs Institute (JBI) critical appraisal tools and the meta-analysis was conducted with Comprehensive Meta-Analysis software.
Results
Out of 4785 records, 50 studies were included in the systematic review, and 27 of them met the criteria for quantitative synthesis. The results indicated a significant role for HT in developing papillary TC (OR: 1.65; 95% CI: 1.04 to 2.61), medullary TC (OR: 2.70; 95% CI: 1.20 to 6.07) and lymphoma (OR:12.92; 95% CI: 2.15 to 77.63); but not anaplastic TC (OR: 1.92; 95% CI: 0.29 to 1.90) and follicular TC (OR: 0.73; 95% CI: 0.41 to 1.27). Also, this study found a significant association between HT and thyroid malignancies (OR: 1.36; 95% CI: 1.05 to 1.77).
Conclusion
Although we found a significant association between HT and some types of TCs, High RoB studies, high level of heterogeneity, and the limited number of well-designed prospective studies, suggested the need for more studies to reach more reliable evidence.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13044-021-00117-x.
Keywords: Hashimoto Thyroiditis, Chronic autoimmune thyroiditis, Thyroid neoplasms, Systematic review, Meta-analysis
Introduction
Chronic lymphocytic thyroiditis also called “Hashimoto thyroiditis” (HT) is the most common inflammatory autoimmune thyroid disease and the most common cause of hypothyroidism in regions with adequate amounts of iodine [1]. HT was first delineated by Japanese surgeon Hakaru Hashimoto as an autoimmune disease [2]. HT is characterized by immune cells infiltration of the thyroid gland as a result of failure in immune tolerance. This condition frequently affects females (more than 10:1 ratio of females to males) [3]. The occurrence of HT has increased during the last decades. Thyroid cancer (TC) is the most common endocrine tumor and the occurrence of TC has increased rapidly worldwide. Papillary thyroid carcinoma (PTC) is the most common type of thyroid neoplasms and accounts for 80-90% of all thyroid cancers. It occurs more frequently in females.
Rudolf Virchow first described the link between chronic inflammation and cancer in 1893, which is now well determined [4]. The association between HT and PTC was first described by Dailey et al. in 1955 [5]. Despite several retrospective and prospective studies performed, the relationship between them remains controversial. A recent meta-analysis of 64,628 patients in 36 studies reported a relation between HT and PTC and an association between HT and thyroid lymphoma [6]. Consistently with this finding, several studies have been performed and they reported that HT is associated with a greater probability of developing PTC [7]. Another meta-analysis revealed the correlation between HT and PTC and this systematic review only investigated the incidence of HT in TC patients and not the incidence of TC in HT patients [8]. In contrast with this finding, Jankovic et al. reported no significant association between HT and TC based on 8 fine-needle aspiration studies [9].
Given the selection bias and limitations of previous studies as well as new publications in this area, an updated systematic review is needed to better clarify the association between HT and TC. Therefore, we elaborated a new meta-analysis via a complete investigation of the literature aiming to evaluate the association between HT and TCs, and also the investigation of the role of HT in different subgroups of TC, based on current knowledge.
Methods
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [10].
Search
After getting the approval of the study protocol, an electronic search was conducted in 3 major databases including Medline via PubMed, EMBASE, and Scopus, with ((Chronic autoimmune thyroiditis) OR Hashimoto) AND (thyroid neoplasm* OR thyroid carcinoma* OR thyroid cancer* OR thyroid adenoma* OR thyroid malignanc*) and related MeSH keywords on 23 February 2021.
Study selection
Results of the electronic search were imported into EndNote 20 and after removing the duplicated studies, the remaining records were screened in two title/abstract and full-text stages. Two independent authors screened the studies and in case of any disagreements, a third author deemed the issue. For full coverage of any published studies, after selecting the final articles to be included in this systematic review, the reference lists of these articles and recently published reviews have been checked for possible inclusion in our study.
Eligibility criteria
We included the journal articles which assess the possible relation between HT and TC with both retrospective and prospective study designs. In case of lack of a control group, the study was included in our systematic review but excluded from the meta-analysis. We only selected the articles which have been written in English and animal studies, case reports, review articles, editorials, letters, conference abstracts, and withdrawn articles were excluded from our study.
Data extraction
Data extraction was conducted by two authors with an electronic table in Microsoft Word. The following data were extracted from each study: the name of the first author of the study, the year of study publication, the study design which could be retrospective or prospective, the setting of the study, the method for diagnosis of thyroid cancer, the sample size, the mean and standard deviation of ages, the number of female and male cases, the type of thyroid cancer and finally the rate of TC between HT cases and control group, or rate of HT between TC and control group.
Risk of Bias assessment
The risk of bias (RoB) in included studies was assessed using the Joanna Briggs Institute (JBI) critical appraisal tools for cohort or case-control studies based on the study design [11]. The checklist for case-control studies includes 10 questions and the cohort studies’ checklist includes 11 questions. These tools assess the similarity of case and control groups, using a standard and similar method for assessing the condition, appropriate dealing with cofounding factors, enough period of interest, and appropriate statistical analysis.
Statistics
All the statistical analyses were conducted using the second version of Comprehensive Meta-Analysis (CMA.2) software with 95% confidence intervals and a 0.05 level of significance. I2 model was used for assessing the heterogeneity between the studies, and for outcomes with more than 50% level of heterogeneity, a random effect model was used. The number of events in case and control groups in both study designs and also the size of the group was imported into the CMA and the odds ratio (OR) was collected for each study. Then the results were then combined in both random and fixed effect models and the ORs for each subgroup (based on the type of thyroid cancer) as well as the overall result were calculated and presented by forest plot.
Results
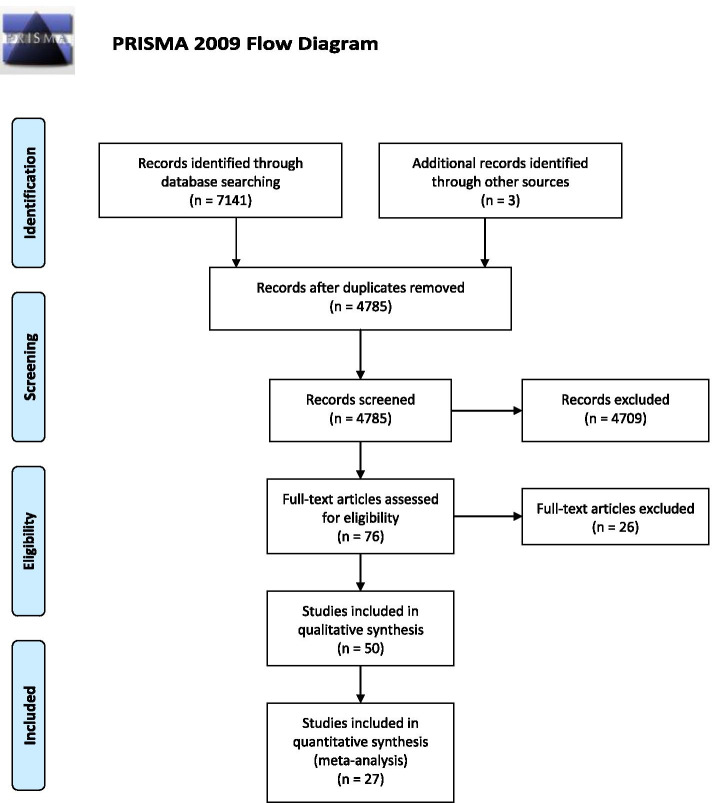
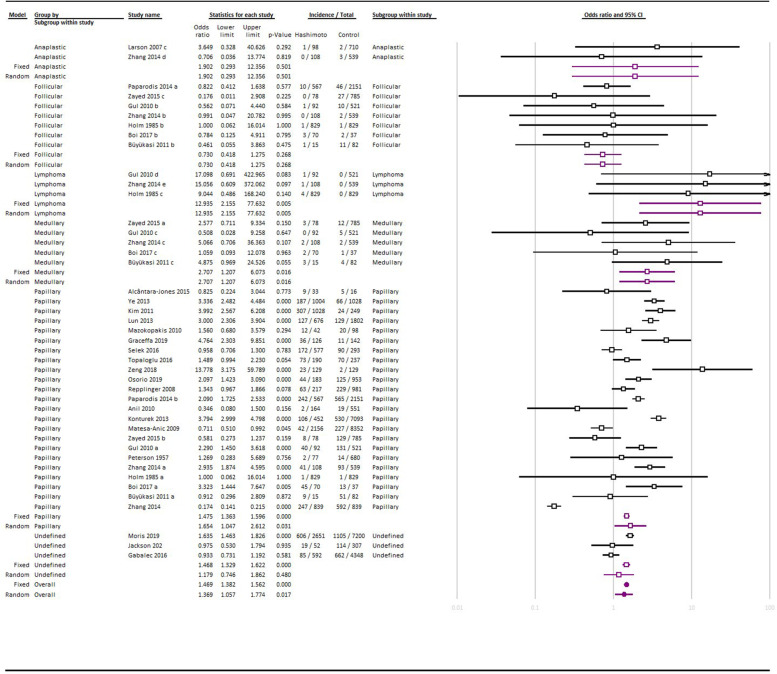
Globally, 7141 records were identified through database searching, and after removing the duplicated studies, 4785 studies were screened. Finally, 50 studies were selected for qualitative synthesis and 27 of them, were included in the quantitative synthesis (Fig. 1). Among them, 23 studies found the rate of HT in TC cases; on the other hand, 29 of them assessed the rate of TC in HT cases, whereas 3 of them reported both of these findings. The characteristics of the included studies are summarized in Table 1. Figure 2 summarized the results of the meta-analysis.
Fig. 1.
PRISMA flow diagram
Table 1.
characteristics and summary of findings in the included studies
| Study | Study design | Setting | Study method | Sample size | Mean age ± SD | Female: Male | Thyroid cancer type | Rate of Hashimoto’s thyroiditis (in percent) | |
|---|---|---|---|---|---|---|---|---|---|
| Thyroid cancer | Control group | ||||||||
| Alcântara-Jones 2015 [12] | Retrospective | Brazil | Thyroidectomy | 49 | 48.5 | 30:3 | Papillary |
27.27 (9/33) |
31.25 (5/16) |
| Zeng 2016 [13] | Retrospective | China | Thyroidectomy | 619 | 45.9 | 484:135 | Papillary | 35.86 (222/619) | |
| Campos 2012 [1] | Retrospective | Brazil | Thyroidectomy | 315 | 44.9 | 34:7 | Papillary | 26.83 (11/41) |
1.12 (3/268) |
| Ye 2013 [14] | Retrospective | China | Thyroidectomy | 2052 | – | 828:176 | Papillary | 18.63 (187/1004) | 6.42 (66/1028) |
| Cipolla 2005 [15] | Retrospective | Italy | Thyroidectomy | 178 | – | 68:21 | Papillary |
26.76 (19/71) |
|
| Kim 2011 [16] | Retrospective | Korea | Thyroidectomy | 1329 | 47.5 | 821:207 | Papillary |
29.86 (307/1028) |
9.64 (24/249) |
| 32:20 | Follicular |
9.62 (5/52) |
|||||||
| Ahn 2011 [17] | Retrospective | Korea | Thyroidectomy | 303 | 42.8 | 225:44 | Papillary |
21.56 (58/269) |
|
| Huang 2011 [18] | Retrospective | China | Thyroidectomy | 1997 | 39.9 | 1450:338 | Papillary |
4.75 (85/1788) |
|
| 153:56 | Follicular |
3.83 (8/209) |
|||||||
| Lun 2013 [19] | Retrospective | China | Thyroidectomy | 2478 | 41.3 | 538:138 | Papillary |
18.79 (127/676) |
7.16 (129/1802) |
| Moshynska 2008 [20] | Retrospective | Canada | Thyroidectomy | 20 | – | – | Lymphoma |
60 (12/20) |
|
| Singh 1999 [21] | Retrospective | United States | Thyroidectomy | 453 | 41 | 267:121 | Papillary |
14.69 (57/388) |
|
| – | Follicular |
2.08 (1/48) |
|||||||
| – | Lymphoma |
5.88 (1/17) |
|||||||
| Zhang 2014 [22] | Retrospective | China | Thyroidectomy | 8524 | 43.1 | – | Papillary |
28.46 (592/2080) |
|
| Nemetz 2011 [23] | Retrospective | Brazil | Thyroidectomy | 52 | 51.3 | 48:4 | Papillary |
32.69 (17/52) |
|
| Jeong 2012 [24] | Retrospective | Korea | Thyroidectomy | 1357 | 44.5 | 1176:181 | Papillary |
26.46 (359/1357) |
|
| Kashima 1998 [25] | Retrospective | Japan | Thyroidectomy | 1533 | 42.6 | 1402:131 | Papillary |
18.33 (281/1533) |
|
| Kebebew 2001 [26] | Retrospective | United States | Thyroidectomy | 136 | 45.5 | 95:41 | Papillary |
30.15 (41/136) |
|
| Yoon 2012 [27] | Retrospective | Korea | Thyroidectomy | 195 | 45.9 | 166:29 | Papillary |
28.72 (56/195) |
|
| Graceffa 2019 [28] | Retrospective | Italy | Thyroidectomy | 305 | 50.6 | 258:47 | Papillary |
28.6 (36/126) |
7.7 (11/142) |
| Selek 2016 [29] | Retrospective | Turkey | Thyroidectomy | 870 | 47 ± 12 | Papillary |
30 (172/ 577) |
31 (90/ 293) |
|
| Topaloglu 2016 [30] | Retrospective | Turkey | Thyroidectomy | 427 |
Malignant: 49.10 ± 12.23 Benign: 47.78 ± 12.39 |
341:86 | Papillary |
38.4 (73/190) |
29.5 (70/237) |
| Zeng 2018 [31] | Retrospective | China | Thyroidectomy | 258 | 17.31 ± 3.21 | 212:46 | Papillary |
17.8 (23/129) |
1.6 (2/129) |
| Osorio 2019 [7] | Retrospective | Colombia | Thyroidectomy | 1136 | 47.5 ± 14.3 | 1047: 89 | Papillary |
24 (44/183) |
13.11 (125/953) |
| Youssef Mohamed 2020 [32] | Retrospective | Egypt | Thyroidectomy | 80 | – | 22: 58 | Papillary |
20 16/80 |
|
| JNawarathna 2018 [33] | Retrospective | Sri Lanka | Thyroidectomy | 684 | 48 ± 12.5 | 611: 73 | Papillary | OR: 0.867 (0.25-2.99) | |
| Follicular | OR: 1.02 (0.22-4.58) | ||||||||
| Rate of thyroid cancer (in percent) | |||||||||
| Hashimoto’s thyroiditis | Control group | ||||||||
| Repplinger 2008 [34] | Retrospective | United States | Thyroidectomy | 1198 | 215:77 | Papillary |
29.03 (63/217) |
23.34 (229/981) |
|
| Paparodis 2014 [35] | Retrospective | United States | Thyroidectomy | 2718 | Papillary |
42.68 (242/567) |
26.27 (565/2151) |
||
| Follicular |
1.76 (10/567) |
2.14 (46/2151) |
|||||||
| Anil 2010 [36] | Prospective | Turkey | FNA | 715 | Papillary |
1.22 (2/164) |
3.45 (19/551) |
||
| Konturek 2013 [37] | Retrospective | Poland | Thyroidectomy | 7545 | 53.5 | Papillary |
23.45 (106/452) |
7.47 (530/7093) |
|
| Mukasa 2011 [38] | Retrospective | Japan | FNA | 2036 | Papillary |
1.77 (36/2036) |
|||
| Lymphoma |
0.10 (2/2036) |
||||||||
| Matesa-Anic 2009 [39] | Retrospective | Croatia | FNA | 10,508 | 50 | 236:33 | Papillary |
1.95 (42/2156) |
2.72 (227/8352) |
| Dailey 1955 [5] | Prospective | United States | Thyroidectomy | 2336 | 37.5 | Papillary |
10.43 (29/278) |
||
| Larson 2007 [40] | Retrospective | United States | Thyroidectomy | 812 | 41 | 142:37 | Papillary |
34.7 (34/98) |
20.4 (145/710) |
| 16:5 | Follicular |
9.2 (9/98) |
1.69 (12/710) |
||||||
| 3:0 | Anaplastic |
1.02 (1/98) |
0.28 (2/710) |
||||||
| Zayed 2015 [41] | Retrospective | Jordan | Thyroidectomy | 180 | 51.3 | 9:6 | Medullary |
3.85 (3/78) |
1.53 (12/785) |
| 102:35 | Papillary |
10.26 (8/78) |
16.43 (129/785) |
||||||
| 18:9 | Follicular |
0 (0/78) |
3.44 (27/785) |
||||||
| Gul 2010 [42] | Retrospective | Turkey | Thyroidectomy | 613 | 43 | Papillary | 43.48 (40/92) | 25.14 (131/521) | |
| Follicular |
1.09 (1/92) |
1.92 (10/521) |
|||||||
| Medullary |
0 (0/92) |
0.96 (5/521) |
|||||||
| Lymphoma |
1.09 (1/92) |
0 (0/521) |
|||||||
| Mazokopakis 2010 [43] | Retrospective | Greece | Thyroidectomy | 140 | 49.3 | 25:7 | Papillary |
28.57 (12/42) |
20.41 (20/98) |
| Sclafani 1993 [44] | Retrospective | United States | Thyroidectomy | 48 | 51.7 | Papillary |
12.5 (6/48) |
||
| Peterson 1957 [45] | Retrospective | United States | Thyroidectomy | 757 | Papillary |
2.60 (2/77) |
2.06 (14/680) |
||
| Zhang 2014 [46] | Retrospective | China | Thyroidectomy | 647 | 43.3 | Papillary |
37.96 (41/108) |
17.25 (93/539) |
|
| Follicular |
0 (0/108) |
0.37 (2/539) |
|||||||
| Medullary |
1.85 (2/108) |
0.37 (2/539) |
|||||||
| Anaplastic |
0 (0/108) |
0.56 (3/539) |
|||||||
| Lymphoma |
0.93 (1/108) |
0 (0/539) |
|||||||
| Holm 1985 [47] | Prospective | Sweden | FNA | 1656 | Papillary |
0.12 (1/829) |
0.12 (1/829) |
||
| Follicular |
0.12 (1/829) |
0.12 (1/829) |
|||||||
| Lymphoma |
0.48 (4/829) |
0 (0/829) |
|||||||
| Moris 2019 [48] | prospective | United States | Thyroidectomy | 9851 | 52.2 ± 15 |
8263: 1588 |
Undefined |
22.8 (606/2651) |
15.4 (1105/7200) |
| FNA | Undefined |
7.3 (284/3895) |
4.7 (473/10168) |
||||||
| Jackson 2020 [49] | retrospective | United States | Thyroidectomy | 359 | Incidental thyroid cancer |
15 (8/52) |
10 (31/307) |
||
| Thyroid cancer | 37 (19/52) | 37 (114/307) | |||||||
| Keskin 2016 [50] | prospective | Turkey | FNA and Thyroidectomy | 300 | 12.1 ± 3.1 | 238: 62 | Papillary |
0.66 (2/300) |
|
| Liu2017 [51] | retrospective | China | Thyroidectomy | 927 | 46 ± 0 |
706: 221 |
Papillary | ||
| Radetti 2019 [52] | prospective | Italy | FNA | 904 | 10.6 ± 3.2 |
709: 195 |
Papillary |
1.1 (10/904) |
|
| Won2018 [53] | retrospective | Korea | FNA | 89 |
11.1 ± 3.7 |
76: 13 | Papillary |
7.9 (7/89) |
|
| Boi 2017 [54] | retrospective | Italy | FNA | 645 |
28.9 (44/152) |
7.4 (12/161) |
|||
| Thyroidectomy | Papillary |
64.3 (45/70) |
35.1 (13/37) |
||||||
| Thyroidectomy | Follicular |
4.3 (3/70) |
5.4 (2/37) |
||||||
| Thyroidectomy | Medullary | 2.8 (2/70) |
2.7 (1/37) |
||||||
| Gabalec 2016 [55] | retrospective | Czech republic | Thyroidectomy | 4947 | Undefined |
29.5 (26/88) |
15.2 (231/1515) |
||
| FNA |
14.2 (85/592) |
15.2 (662/4348) |
|||||||
| Büyükaşi 2011 [56] | retrospective | Turkey | Thyroidectomy | 917 | adult | 743:174 | All Cancer Types |
19.4 (15/77) |
9.8 (82/840) |
| Papillary |
60.0 (9/15) |
63.41 (52/82) |
|||||||
| Follicular |
6.6 (1/15) |
13.41 (11/82) |
|||||||
| Medullary |
20.0 (3/15) |
4.87 (4/82) |
|||||||
| Chen 2013 [57] | prospective | Taiwan | 7605 | adult | 6845:755 | 1.58 | 0.14 | ||
| Cipolla 2005 [15] | Retrospective | Italy | Thyroidectomy | 178 | – | 68:21 | Papillary |
27.6 (13/47) |
|
| Zhang 2014 [22] | Retrospective | China | Thyroidectomy | 8524 | 43.1 | – | Papillary |
14.24 (247/839) |
70 (592/839) |
| Graceffa 2019 [28] | Retrospective | Italy | Thyroidectomy | 305 | 50.6 | 258:47 | Papillary |
28.83 (47/163) |
|
| Follicular |
1.84 (3/163) |
||||||||
| Medullary |
0.61 (1/163) |
||||||||
| Uhliarova 2017 [58] | prospective | Slovakia | Thyroidectomy | 2117 | 11.1 ± 3.7 | 1738: 379 | All cancer types |
83.64%) (266/318) |
|
Fig. 2.
forest plot of the studies included in the meta-analysis
Papillary thyroid cancer
45 of the included studies investigated the possible relation between HT and PTC. In these studies, the rate of HT in PTC cases was ranged between 4.75 to 38.4%, whereas the rate of PTC in HT ranged between 0.12 to 64.3%. The meta-analysis of 23 studies with an appropriate control group, found 1.65 OR (95% CI: 1.04 to 2.61; I2 test for heterogeneity: 96.48%) and the difference between the groups was significant (p = 0.03).
Follicular thyroid cancer
13 studies assessed the possible association between HT and follicular thyroid cancer (FTC). In these studies, the rate of HT in the FTC group ranged between 2.08 to 9.62% and the rate of FTC in HT ranged between 0 to 9.2%. The meta-analysis of the 7 studies that met the proper inclusion criteria, reached 0.73 OR (95% CI: 0.41 to 1.27; I2 test for heterogeneity: 0%) and the difference between the groups was not statistically significant (p = 0.26).
Medullary thyroid cancer
The possible role of HT in developing medullary thyroid cancer (MTC) was investigated in 6 studies. All of these studies assessed the rate of MTC in the HT group and it ranged between 0 to 20%. The meta-analysis of 5 studies with an appropriate control group, reached 2.70 OR for this outcome (95% CI: 1.20 to 6.07; I2 test for heterogeneity: 0%) and the difference between the groups was significant (p = 0.01).
Lymphoma
6 studies investigated the relation between HT and lymphoma and the rate of HT in the lymphoma group was 5.88 and 60% in two studies. The range of lymphoma in HT was between 0.1 to 1.09%. The meta-analysis of 3 studies concerning this outcome reached 12.93 OR (95% CI: 2.15 to 77.63; I2 test for heterogeneity: 0%) and the difference between these groups was significant (p = 0.01).
Anaplastic thyroid cancer
Only two studies assessed the relation between anaplastic thyroid cancer (ATC) and HT and the rate of TC in the HT group was 0 and 1.02% in these studies. The meta-analysis reached 1.92 OR (95% CI: 1.90 to 0.29; I2 test for heterogeneity: 0%) and the difference between groups was not statistically significant (p = 0.05).
All cancer types
Twenty seven studies had an appropriate control group which allowed us to calculate the OR and include them in the meta-analysis. The results showed 1.36 OR (95% CI: 1.05 to 1.77; I2 test for heterogeneity: 93.66%) and there was a significant difference between case and control groups in terms of incidence of TCs (p = 0.01).
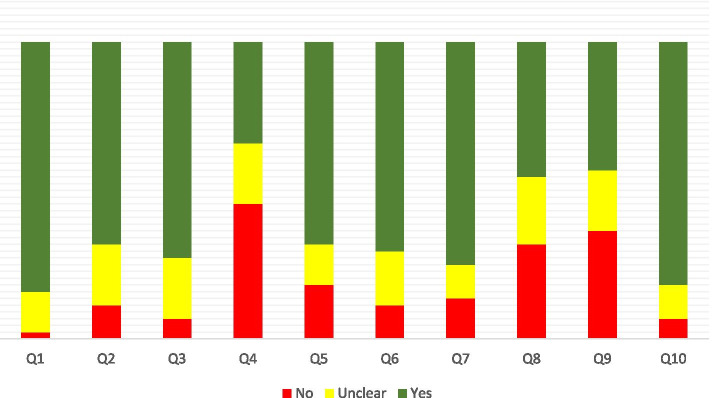
Risk of Bias
The RoB assessment based on the JBI checklist is presented in Fig. 3. Based on our assessment, appropriately dealing with confounding factors was the most prevalent source of bias in included studies. The appropriate and complete follow-up period was the other source of bias in these studies. Generally, there is a concerning risk of bias in these studies which can affect these outcomes. The details of the RoB assessment are presented in Supplementary material 1.
Fig. 3.
Risk of Bias in the studies based on Joanna Briggs Institute (JBI) checklist
Discussion
This study investigated the possible relationship between HT and different types of TCs. The results indicated a significant correlation between HT and thyroid malignancies in particular with PTC, MTC, lymphoma but not with ATC and FTC. Also, this study found a significant association between HT and thyroid malignancies.
As the most common cause of hypothyroidism in developed countries [59], the role of HT in developing thyroid malignancies, should be considered by the clinicians. As fine needle aspiration (FNA) has poor accuracy in the diagnosis of TCs in patients with thyroiditis, diagnosis of TC in the presence of HT is challenging. Previous studies have found a better prognosis for TC in case of coexistence of HT, because of earlier diagnosis based on routine medical follow-up [18]. Moreover, a less aggressive form of malignancy in PTC patients in the top of HT has been reported, though but this conclusion was associated with controversies in an endemic area of iodine deficiency goiter [60].
Despite multiple hypotheses in this regard, the underlying mechanism of developing malignancies in HT patients is not fully understood [61, 62]. One of these mechanisms may rely on the inflammatory process in HT. Inflammatory reactions create free radical oxygen, resulting in DNA damage and mutations that finally cause the development of PTC [9]. Another hypothesis states that malignant transformation is caused by increased levels of TSH that stimulate thyroid tissue epithelial proliferation [61]. A recently published study assessed the prognostic value of FOXP3 in PTC and the difference in its expression in concomitant HT. FOXP3 is a PTC-related marker and its expression by HT infiltrating lymphocytes suggested a relationship between HT and PTC [32].
Despite the historical discussion about the possible role of HT in developing TCs, current guidelines didn’t accept HT as a risk factor for developing thyroid malignancies [63]. Some experts believe that a good prognosis of TCs and particularly PTC, as the most incident thyroid malignancy, leads to a decrease in allocation of resources toward designing and conducting well-designed studies to identify predictive factors and improving the management of outcomes [64]. The controversial outcomes of the studies highlighted a need for more prospective studies with appropriate control groups and considering the possible cofounding factors to reach more reliable evidence.
Our meta-analysis as the most reliable evidence in this regard found a significant association between HT and MTC based on 5 published studies. This finding is obtained based on a retrospective point of view and only 11 cases of MTC were reported in 526 investigated cases of HT in our included studies. MTC is the third most common TC that originates from the parafollicular cells with an unfavorable prognosis [65, 66]. Previously the reports of this relation were limited to case reports [67–72]. One of the suggested pathophysiological bases for this relation is the occurrence of HT in response to MTC, so future prospective studies can give better insight in this regard. Also, the results of Zayed et al. only found such an association only in female patients [41], which should be more investigated in future studies.
One of the limitations of this study was the high level of heterogeneity between different studies. These differences can arise from multiple sources. Differences in pathological interpretation of HT, genetic factors, diagnostic methods for thyroid malignancies including the FNA and total thyroidectomy can cause variations in the reported rate of coexistence of HT and TC in our included studies. Besides, the variation in OR can arise from differences in defining the control groups.
A comprehensive search in three major databases and the adding of hand searching results was one of the strengths of this study that led to full coverage of published studies that met our inclusion. Besides, carefully selecting and extracting the data, was the other strength of this systematic review. Unlike previous studies, we conducted our meta-analysis based on OR, therefore, the studies without an appropriate control group were excluded from our meta-analysis. This made the findings of our study more practical and obvious.
Conclusion
Based on the current knowledge, HT is associated with developing thyroid malignancies, particularly PTC, MTC, lymphoma but not with ATC and FTC. Studies with high RoB, the high level of heterogeneity between different studies, and the limited number of well-designed prospective studies make the available evidence uncertain, so there is a need for more studies to reach more reliable conclusions.
Supplementary Information
Acknowledgments
The research protocol was approved and supported by Student Research Committee, Tabriz University of Medical Sciences (grant number: 64115).
Conflict of interest
None.
Abbreviations
- HT
Hashimoto thyroiditis
- TC
Thyroid cancer
- PTC
Papillary thyroid carcinoma
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RoB
Risk of bias
- JBI
Joanna Briggs Institute
- CMA
Comprehensive Meta-Analysis
- OR
Odds ratio
- FTC
Follicular thyroid cancer
- MTC
Medullary thyroid cancer
- ATC
Anaplastic thyroid cancer
Authors’ contributions
PA and EN: Funding acquisition; Investigation; Resources; Project administration; Conceptualization AN: Formal analysis; Investigation; Methodology; Resources; Validation; Roles/Writing - original draft; VS*: Conceptualization; Data curation; Funding acquisition; Methodology; Writing - review & editing. All authors read and approved the final manuscript.
Funding
This work was supported by Deputy for Research of Tabriz University of Medical Sciences.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of Tabriz University of Medical Sciences (approval code: IR.TBZMED.VCR.REC.1399.434).
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Pouya Abbasgholizadeh, Email: pouya.abbasgholizadeh@yahoo.com.
Amirreza Naseri, Email: amirx2eza@gmail.com, Email: naseria@tbzmed.ac.ir.
Ehsan Nasiri, Email: nasiriehsan1377@gmail.com.
Vahideh Sadra, Email: sadra.vahideh@gmail.com.
References
- 1.Campos LA, Picado SM, Guimarães AV, Ribeiro DA, Dedivitis RA. Thyroid papillary carcinoma associated to Hashimoto's thyroiditis. Braz J Otorhinolaryngol. 2012;78(6):77–80. [DOI] [PMC free article] [PubMed]
- 2.Hashimoto H. Zur kenntniss der lymphomatosen veranderung der Schilddruse (Struma lymphomatosa) Arch Klin Chir. 1912;97:219–248. [Google Scholar]
- 3.Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. 2018;14(5):301. doi: 10.1038/nrendo.2018.18. [DOI] [PubMed] [Google Scholar]
- 4.Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–545. doi: 10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- 5.Me D, Lindsay S, Skahen R. Relation of thyroid neoplasms to hashimoto disease of the thyroid gland. AMA Arch Surg. 1955;70(2):291–297. doi: 10.1001/archsurg.1955.01270080137023. [DOI] [PubMed] [Google Scholar]
- 6.Resende de Paiva C, Grønhøj C, Feldt-Rasmussen U, CJFio v B. Association between Hashimoto’s thyroiditis and thyroid cancer in 64,628 patients. Front Oncol. 2017;7:53. doi: 10.3389/fonc.2017.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osorio C, Ibarra S, Arrieta J, Sarmiento M, Barrios D, Sierra L, et al. Association between chronic lymphocytic thyroiditis and papillary thyroid carcinoma: A retrospective study in surgical specimens. Rev Esp Patol. 2020;53(3):149–157. doi: 10.1016/j.patol.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Lai X, Xia Y, Zhang B, Li J, Jiang YJO. A meta-analysis of Hashimoto’s thyroiditis and papillary thyroid carcinoma risk. Oncotarget. 2017;8(37):62414. doi: 10.18632/oncotarget.18620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jankovic B, Le KT, Hershman JM, Metabolism Hashimoto’s thyroiditis and papillary thyroid carcinoma: is there a correlation? J Clin Endocrinol Metab. 2013;98(2):474–482. doi: 10.1210/jc.2012-2978. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: systematic reviews of etiology and risk. Joanna Briggs Institute Reviewer's Manual The Joanna Briggs Institute; 2017. [Google Scholar]
- 12.Alcântara-Jones DM, Alcântara-Nunes TF, Rocha BO, Oliveira RD, Santana ACP, Alcântara FT, et al. Is there any association between Hashimoto’s thyroiditis and thyroid cancer? A retrospective data analysis. Radiol Bras. 2015;48(3):148–153. doi: 10.1590/0100-3984.2014.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rc Z, Lp J, Ed C, Dong S, Yf C, Gl H, et al. Potential relationship between Hashimoto's thyroiditis and BRAFV600E mutation status in papillary thyroid cancer. Head Neck. 2016;38(S1):E1019–E1E25. doi: 10.1002/hed.24149. [DOI] [PubMed] [Google Scholar]
- 14.Ye Z-q, Gu D-n, Hu H-y, Zhou Y-l, Hu X-q, Zhang X-h. Hashimoto’s thyroiditis, microcalcification and raised thyrotropin levels within normal range are associated with thyroid cancer. World J Surg Oncol. 2013;11(1):56. doi: 10.1186/1477-7819-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cipolla C, Sandonato L, Graceffa G, Fricano S, Torcivia A, Vieni S, et al. Hashimoto thyroiditis coexistent with papillary thyroid carcinoma. Am Surg. 2005;71(10):874–878. [PubMed] [Google Scholar]
- 16.Kim KW, Park YJ, Kim EH, Park SY, Park DJ, Ahn SH, et al. Elevated risk of papillary thyroid cancer in Korean patients with Hashimoto's thyroiditis. Head Neck. 2011;33(5):691–695. doi: 10.1002/hed.21518. [DOI] [PubMed] [Google Scholar]
- 17.Ahn D, Heo SJ, Park JH, Kim JH, Sohn JH, Park JY, et al. Clinical relationship between Hashimoto's thyroiditis and papillary thyroid cancer. Acta Oncol. 2011;50(8):1228–1234. doi: 10.3109/0284186X.2011.602109. [DOI] [PubMed] [Google Scholar]
- 18.Huang B-Y, Hseuh C, Chao T-C, Lin K-J, Lin J-D. Well-differentiated thyroid carcinoma with concomitant Hashimoto’s thyroiditis present with less aggressive clinical stage and low recurrence. Endocr Pathol. 2011;22(3):144. doi: 10.1007/s12022-011-9164-9. [DOI] [PubMed] [Google Scholar]
- 19.Lun Y, Wu X, Xia Q, Han Y, Zhang X, Liu Z, et al. Hashimoto’s thyroiditis as a risk factor of papillary thyroid cancer may improve cancer prognosis. Otolaryngol Head Neck Surg. 2013;148(3):396–402. doi: 10.1177/0194599812472426. [DOI] [PubMed] [Google Scholar]
- 20.Moshynska OV, Saxena A. Clonal relationship between Hashimoto thyroiditis and thyroid lymphoma. J Clin Pathol. 2008;61(4):438–444. doi: 10.1136/jcp.2007.051243. [DOI] [PubMed] [Google Scholar]
- 21.Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery. 1999;126(6):1070–1077. doi: 10.1067/msy.2099.101431. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Dai J, Wu T, Yang N, Yin Z. The study of the coexistence of Hashimoto’s thyroiditis with papillary thyroid carcinoma. J Cancer Res Clin Oncol. 2014;140(6):1021–1026. doi: 10.1007/s00432-014-1629-z. [DOI] [PubMed] [Google Scholar]
- 23.Nemetz MA, Thomazelli FCS, Granero LCS, Nemetz AB, dos Santos MB. Does chronic lymphocytic thyroiditis influence the staging of differentiated thyroid carcinoma? Braz J Otorhinolaryngol. 2011;77(1):77–83. doi: 10.1590/S1808-86942011000100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jeong JS, Kim HK, Lee CR, Park S, Park JH, Kang SW, et al. Coexistence of chronic lymphocytic thyroiditis with papillary thyroid carcinoma: clinical manifestation and prognostic outcome. J Korean Med Sci. 2012;27(8):883–889. doi: 10.3346/jkms.2012.27.8.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kashima K, Yokoyama S, Noguchi S, Murakami N, Yamashita H, Watanabe S, et al. Chronic thyroiditis as a favorable prognostic factor in papillary thyroid carcinoma. Thyroid. 1998;8(3):197–202. doi: 10.1089/thy.1998.8.197. [DOI] [PubMed] [Google Scholar]
- 26.Kebebew E, Treseler PA, Ituarte PH, Clark OH. Coexisting chronic lymphocytic thyroiditis and papillary thyroid cancer revisited. World J Surg. 2001;25(5):632–637. doi: 10.1007/s002680020165. [DOI] [PubMed] [Google Scholar]
- 27.Yoon Y-H, Kim HJ, Lee JW, Kim JM, Koo BS. The clinicopathologic differences in papillary thyroid carcinoma with or without co-existing chronic lymphocytic thyroiditis. Eur Arch Otorhinolaryngol. 2012;269(3):1013–1017. doi: 10.1007/s00405-011-1732-6. [DOI] [PubMed] [Google Scholar]
- 28.Graceffa G, Patrone R, Vieni S, Campanella S, Calamia S, Laise I, et al. Association between Hashimoto’s thyroiditis and papillary thyroid carcinoma: a retrospective analysis of 305 patients. BMC Endocr Disord. 2019;19(1):1–6. doi: 10.1186/s12902-019-0351-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Selek A, Cetinarslan B, Tarkun I, Canturk Z, Ustuner B, Akyay Z. Thyroid autoimmunity: is really associated with papillary thyroid carcinoma? Eur Arch Otorhinolaryngol. 2017;274(3):1677–1681. doi: 10.1007/s00405-016-4414-6. [DOI] [PubMed] [Google Scholar]
- 30.Topaloglu O, Baser H, Cuhaci FN, Sungu N, Yalcin A, Ersoy R, et al. Malignancy is associated with microcalcification and higher AP/T ratio in ultrasonography, but not with Hashimoto’s thyroiditis in histopathology in patients with thyroid nodules evaluated as Bethesda category III (AUS/FLUS) in cytology. Endocrine. 2016;54(1):156–168. doi: 10.1007/s12020-016-0982-x. [DOI] [PubMed] [Google Scholar]
- 31.Zeng R, Zhao M, Niu H, Yang K, Shou T, Zhang G, et al. Relationship between Hashimoto’s thyroiditis and papillary thyroid carcinoma in children and adolescents. Eur Rev Med Pharmacol Sci. 2018;22:7778–7787. doi: 10.26355/eurrev_201811_16401. [DOI] [PubMed] [Google Scholar]
- 32.Mohamed SY, Ibrahim TR, Elbasateeny SS, Abdelaziz LA, Farouk S, Yassin MA, et al. Clinicopathological characterization and prognostic implication of FOXP3 and CK19 expression in papillary thyroid carcinoma and concomitant Hashimoto's thyroiditis. Sci Rep. 2020;10(1):10651. doi: 10.1038/s41598-020-67615-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thyroiditis CL. Association between nonspecific chronic lymphocytic Thyroiditis and differentiated epithelial thyroid carcinoma: Clinicopathological analysis of patients who underwent thyroidectomy in a tertiary Care Center in Sri Lanka. World. 2018;10(2):119–126. [Google Scholar]
- 34.Repplinger D, Bargren A, Zhang Y-W, Adler JT, Haymart M, Chen H. Is Hashimoto's thyroiditis a risk factor for papillary thyroid cancer? J Surg Res. 2008;150(1):49–52. doi: 10.1016/j.jss.2007.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paparodis R, Imam S, Todorova-Koteva K, Staii A, Jaume JC. Hashimoto's thyroiditis pathology and risk for thyroid cancer. Thyroid. 2014;24(7):1107–1114. doi: 10.1089/thy.2013.0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anil C, Goksel S, Gursoy A. Hashimoto's thyroiditis is not associated with increased risk of thyroid cancer in patients with thyroid nodules: a single-center prospective study. Thyroid. 2010;20(6):601–606. doi: 10.1089/thy.2009.0450. [DOI] [PubMed] [Google Scholar]
- 37.Konturek A, Barczyński M, Wierzchowski W, Stopa M, Nowak W. Coexistence of papillary thyroid cancer with Hashimoto thyroiditis. Langenbeck's Arch Surg. 2013;398(3):389–394. doi: 10.1007/s00423-012-1021-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mukasa K, Noh JY, Kunii Y, Matsumoto M, Sato S, Yasuda S, et al. Prevalence of malignant tumors and adenomatous lesions detected by ultrasonographic screening in patients with autoimmune thyroid diseases. Thyroid. 2011;21(1):37–41. doi: 10.1089/thy.2010.0050. [DOI] [PubMed] [Google Scholar]
- 39.Mateša-Anić D, Mateša N, Dabelić N, Kusić Z. Coexistence of papillary carcinoma and Hashimoto's thyroiditis. Acta Clin Croatica. 2009;48(1):9–12. [PubMed] [Google Scholar]
- 40.Larson SD, Jackson LN, Riall TS, Uchida T, Thomas RP, Qiu S, et al. Increased incidence of well-differentiated thyroid cancer associated with Hashimoto thyroiditis and the role of the PI3k/Akt pathway. J Am Coll Surg. 2007;204(5):764–773. doi: 10.1016/j.jamcollsurg.2006.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zayed AA, Ali MKM, Jaber OI, Moh’d JS, Ashhab AA, Al_Shweiat WM et al. Is Hashimoto’s thyroiditis a risk factor for medullary thyroid carcinoma? Our experience and a literature review. Endocrine. 2015;48(2):629–636. doi: 10.1007/s12020-014-0363-2. [DOI] [PubMed] [Google Scholar]
- 42.Gul K, Dirikoc A, Kiyak G, Ersoy PE, Ugras NS, Ersoy R, et al. The association between thyroid carcinoma and Hashimoto's thyroiditis: the ultrasonographic and histopathologic characteristics of malignant nodules. Thyroid. 2010;20(8):873–878. doi: 10.1089/thy.2009.0118. [DOI] [PubMed] [Google Scholar]
- 43.Mazokopakis EE, Tzortzinis AA, Dalieraki-Ott EI, Tsartsalis AN, Syros PK, Karefilakis CM, et al. Coexistence of Hashimoto’s thyroiditis with papillary thyroid carcinoma. A retrospective study. Hormones. 2010;9(4):312–317. doi: 10.14310/horm.2002.1282. [DOI] [PubMed] [Google Scholar]
- 44.Sclafani AP, Valdes M, Cho H. Hashimoto’s thyroiditis and carcinoma of the thyroid: optimal management. Laryngoscope. 1993;103(8):845–849. doi: 10.1288/00005537-199308000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Peterson CA, Shidler FP. Lymphocytic thyroiditis in 757 thyroid operations. Am J Surg. 1957;94(2):223–231. doi: 10.1016/0002-9610(57)90649-9. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Y, Ma X-P, Deng F-S, Liu Z-R, Wei H-Q, Wang X-H, et al. The effect of chronic lymphocytic thyroiditis on patients with thyroid cancer. World J Surg Oncol. 2014;12(1):277. doi: 10.1186/1477-7819-12-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holm L-E, Blomgren H, Löwhagen T. Cancer risks in patients with chronic lymphocytic thyroiditis. N Engl J Med. 1985;312(10):601–604. doi: 10.1056/NEJM198503073121001. [DOI] [PubMed] [Google Scholar]
- 48.Silva de Morais N, Stuart J, Guan H, Wang Z, Cibas ES, Frates MC, et al. The impact of Hashimoto Thyroiditis on thyroid nodule cytology and risk of thyroid Cancer. Journal of the endocrine. Society. 2019;3(4):791–800. doi: 10.1210/js.2018-00427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jackson D, Handelsman RS, Farrá JC, Lew JI. Increased incidental thyroid Cancer in patients with subclinical chronic lymphocytic Thyroiditis. J Surg Res. 2020;245:115–118. doi: 10.1016/j.jss.2019.07.025. [DOI] [PubMed] [Google Scholar]
- 50.Keskin M, Savas-Erdeve S, Aycan Z. Co-existence of thyroid nodule and thyroid Cancer in children and adolescents with Hashimoto Thyroiditis: a single-center study. Horm Res Paediatr. 2016;85(3):181–187. doi: 10.1159/000443143. [DOI] [PubMed] [Google Scholar]
- 51.Liu Y, Li C, Zhao W, Wang Y. Hashimoto's Thyroiditis is an important risk factor of papillary thyroid microcarcinoma in younger adults. Horm Metab Res. 2017;49(10):732–738. doi: 10.1055/s-0043-117892. [DOI] [PubMed] [Google Scholar]
- 52.Radetti G, Loche S, D’Antonio V, Salerno M, Guzzetti C, Aversa T, et al. Influence of Hashimoto Thyroiditis on the development of thyroid nodules and Cancer in children and adolescents. J Endocrine Soc. 2019;3(3):607–616. doi: 10.1210/js.2018-00287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Won JH, Lee JY, Hong HS, Jeong SH. Thyroid nodules and cancer in children and adolescents affected by Hashimoto’s thyroiditis. Br J Radiol. 2018;91(1087):20180014. doi: 10.1259/bjr.20180014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Boi F, Pani F, Calò PG, Lai ML, Mariotti S. High prevalence of papillary thyroid carcinoma in nodular Hashimoto's thyroiditis at the first diagnosis and during the follow-up. J Endocrinol Investig. 2018;41(4):395–402. doi: 10.1007/s40618-017-0757-0. [DOI] [PubMed] [Google Scholar]
- 55.Gabalec F, Srbova L, Nova M, Hovorkova E, Hornychova H, Jakubikova I, et al. Impact of Hashimoto's thyroiditis, TSH levels, and anti-thyroid antibody positivity on differentiated thyroid carcinoma incidence. Endokrynol Pol. 2016;67(1):48–53. doi: 10.5603/EP.a2016.0022. [DOI] [PubMed] [Google Scholar]
- 56.Büyükaşık O, Hasdemir AO, Yalçın E, Celep B, Sengül S, Yandakçı K, et al. The association between thyroid malignancy and chronic lymphocytic thyroiditis: should it alter the surgical approach? Endokrynol Pol. 2011;62(4):303–308. [PubMed] [Google Scholar]
- 57.Chen YK, Lin CL, Cheng FT, Sung FC, Kao CH. Cancer risk in patients with Hashimoto's thyroiditis: a nationwide cohort study. Br J Cancer. 2013;109(9):2496–2501. doi: 10.1038/bjc.2013.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Uhliarova B, Hajtman A. Hashimoto’s thyroiditis-an independent risk factor for papillary carcinoma. Bra J Otorhinolaryngol. 2018;84(6):729–735. doi: 10.1016/j.bjorl.2017.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mincer DL, Jialal I. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2021. Hashimoto Thyroiditis. [Updated 2020 Aug 10] [PubMed] [Google Scholar]
- 60.Hussein O, Abdelwahab K, Hamdy O, Awny S, Megahed NA, Hafez MT, et al. Thyroid cancer associated with Hashimoto thyroiditis: similarities and differences in an endemic area. J Egypt Natl Cancer Inst. 2020;32(1):1–4. doi: 10.1186/s43046-020-0017-9. [DOI] [PubMed] [Google Scholar]
- 61.Anand A, Singh KR, Kushwaha JK, Hussain N, Sonkar AA. Papillary thyroid cancer and Hashimoto’s thyroiditis: an association less understood. Indian J Surg Oncol. 2014;5(3):199–204. doi: 10.1007/s13193-014-0325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kadam SM, Ghadhban BR, AbduljabbarSaleh M. Hashimoto’s Thyroiditis increases risk for differentiated thyroid carcinoma. Ann Romanian Soc Cell Biol. 2021;25(6):5952–5961. [Google Scholar]
- 63.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Feldt-Rasmussen U. Hashimoto’s thyroiditis as a risk factor for thyroid cancer. Curr Opin Endocrinol Diabetes Obesity. 2020;27(5):364–371. doi: 10.1097/MED.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 65.Viola D, Elisei R. Management of Medullary Thyroid Cancer. Endocrinol Metab Clin. 2019;48(1):285–301. doi: 10.1016/j.ecl.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 66.Stamatakos M, Paraskeva P, Stefanaki C, Katsaronis P, Lazaris A, Safioleas K, et al. Medullary thyroid carcinoma: the third most common thyroid cancer reviewed. Oncol Lett. 2011;2(1):49–53. doi: 10.3892/ol.2010.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zeman V, Hanika J. Bilateral pheochromocytoma of the adrenal glands and a solitary neurofibroma of the dorsal mucosa of the tongue associated with a solid medullary carcinoma of the thyroid gland in Hashimoto's lymphocytic thyroiditis. Cesk Patol. 1977;13(4):185–191. [PubMed] [Google Scholar]
- 68.Weiss LM, Weinberg DS, Warhol MJ. Medullary carcinoma arising in a thyroid with Hashimoto's disease. Am J Clin Pathol. 1983;80(4):534–538. doi: 10.1093/ajcp/80.4.534. [DOI] [PubMed] [Google Scholar]
- 69.De Pasquale L, Sommaruga L, Andreani S, Bastagli A. Hashimoto's thyroiditis and medullary carcinoma in the same gland: a purely random occurrence? Chir Ital. 2004;56(4):557–562. [PubMed] [Google Scholar]
- 70.Segal K, Ben-Bassat M, Avraham A, Har-El G, Sidi J. Hashimoto's thyroiditis and carcinoma of the thyroid gland. Int Surg. 1985;70(3):205–209. [PubMed] [Google Scholar]
- 71.Gaskin D, Parai SK, Parai MR. Hashimoto's thyroiditis with medullary carcinoma. Can J Surg. 1992;35(5):528–530. [PubMed] [Google Scholar]
- 72.Mousa U, Gursoy A, Ozdemir H, Moray G. Medullary thyroid carcinoma in a patient with Hashimoto's thyroiditis diagnosed by calcitonin washout from a thyroid nodule. Diagn Cytopathol. 2013;41(7):644–646. doi: 10.1002/dc.21850. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.