ABSTRACT.
Chromoblastomycosis is a chronic cutaneous fungal infection caused by dematiaceous fungi. It is a therapeutic challenge because of the lack of specific treatments. We describe a refractory case of chromoblastomycosis in which the lesion did not respond to initial treatment, but then use of topical imiquimod cured the lesion successfully.
INTRODUCTION
Chromoblastomycosis (CBM) is a common implantation mycosis that has seen an increased incidence in tropical regions.1 Patients are usually infected through the inoculation of hyphae or conidia after transcutaneous trauma. CBM is chronic and progressive. Treatment has always been challenging; there is a low cure rate and a high rate pf recurrence. Traditional antifungal drugs such as itraconazole and terbinafine are usually requested for constant use and. in some cases, without noticeable improvement.2,3 Recently, antifungal immune therapies have been used to treat CBM. Imiquimod, an immune stimulant, shows specific efficiency at enhancing host immune responses against CBM.4–6 We report a case of recalcitrant CBM resulting from Fonsecaea monophora fungal infection that was treated successfully with short-term use of topical 5% imiquimod. Our experience provides evidence that short-term use of imiquimod as a monotherapy is beneficial for refractory CBM.
CASE REPORT
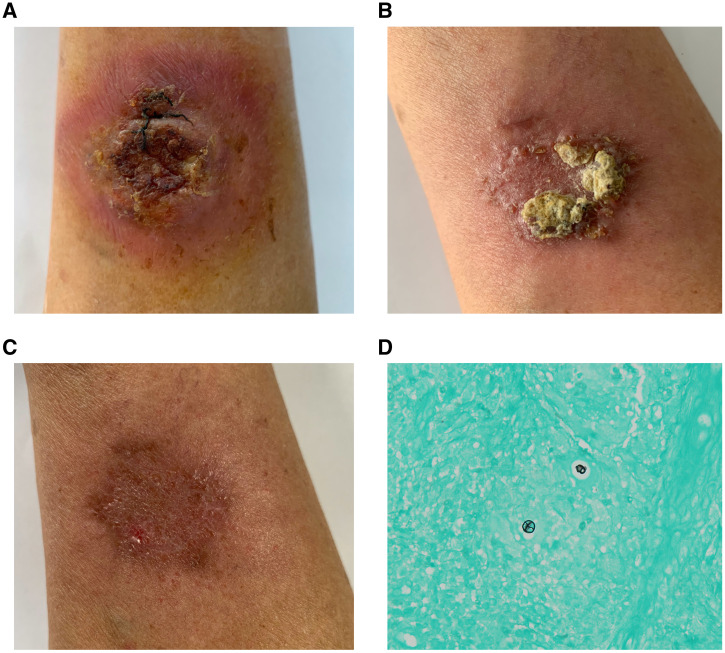
A 72-year-old man presented with an 11-month history of a progressive lesion on the dorsum of the right arm after local trauma. On physical examination, inflammatory erythema and verrucous plaque was noted on his right forearm (Figure 1A). Sclerotic bodies were observed in the biopsy specimen (Figure 1D), and F. monophora was identified as the pathogen. The patient was diagnosed with CBM and was treated with itraconazole (400 mg/d) for 6 months, which was then combined with terbinafine (250 mg/d) for another month. No noticeable improvement was noted. We then treated the lesion with 5% topical imiquimod five times per week as a monotherapy. The patient did not complain of any side effects of imiquimod, such as itching or burning. One month later, the lesion exhibited verrucous and infiltrative aspects (Figure 1B). After 3 months of treatment with imiquimod, the patient exhibit erythematous cicatricial macula only (Figure 1C).
Figure 1.
(A) Inflammatory erythema and verrucous plaque on the forearm before treatment. (B) Exacerbation of lesion under treatment with topical imiquimod 5% for 1 month. (C) The cicatricial macula after 3 months of topical imiquimod. (D) Sclerotic bodies noted using Gomori methenamine silver staining of the lesion. This figure appears in color at www.ajtmh.org.
DISCUSSION
CBM is challenging to treat, and there are limited therapeutic options. In addition to traditional antifungal agents and physiotherapies, alternative treatment methods may be necessary. Our patient demonstrated a positive response to short-term treatment with topical imiquimod, which is consistent with previous reports4–6 and provides more evidence supporting the efficiency of imiquimod in CBM treatment. Based on publications and our own clinical experiences, the limited lesions of CBM, even the refractory ones, had good responses to imiquimod. However, for lesions that have multiple, eruptive verrucous plaques and nodules, topical imiquimod might not a first-choice treatment.
Some immune-stimulating agents such as imiquimod and glucan have been used to treat fungal infections, including CBM,4–6 candidiasis,7 hyalohyphomycosis,8 and tinea pedis.9 Imiquimod is a potent agonist for toll-like receptor (TLR)-7 and TLR-8. As a potent immune modulator, imiquimod is used initially for topical treatment of genital and perianal warts caused by human papilloma virus. Its use later expanded to the treatment of other skin infections. We realize that intracellular pattern recognition receptors (TLR-3, TLR-7, TLR-8, and TLR-9) are critical in the pathophysiology of mycoses,10 and studies focus on stimulating the host reaction to improve defenses against fungal pathogens. It has been proved that exogenously applied TLR agonists are necessary to promote the induction of proinflammatory cytokines and clearance of fungal infection in vivo.11
To our knowledge, there are nine cases of CBM treated with topical imiquimod, as monotherapy or combined with antifungal agents, with visible improvement.4–6 The treatment duration of topical imiquimod in these cases ranged from 6 to 19 months (mean, 10.6 months). Compared with other reports, the treatment duration in our case is much shorter, at only 3 months. Nevertheless, the lesion improved significantly, and the final pathogen examination results were negative. Progression of the verrucous and infiltrative aspects of lesions under imiquimod treatment have been reported and were demonstrated in our patient as well. We observed an exacerbation after the first month of using imiquimod, as shown in Figure 1B, which resolved subsequently. This exacerbation might relate to the stimulation of local immune cells and possibly could lead to the resolution of CBM lesions.
Our case confirms the efficacy of imiquimod in treating CBM, even in the short term. Topical imiquimod is an optimal choice for CMB treatment—particularly for patients who fail to respond to various antifungals—because it is cost-effective and shows positive results in the short term, improving patients’ quality of life.
REFERENCES
- 1. Queiroz-Telles F et al. 2017. Chromoblastomycosis. Clin Microbiol Rev 30: 233–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brito AC Bittencourt M , 2018. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol 93: 495–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Purim K Peretti MC Fillus JN Olandoski M , 2017. Chromoblastomycosis: tissue modifications during itraconazole treatment. An Bras Dermatol 92: 478–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. de Sousa MG et al. 2014. Topical application of imiquimod as a treatment for chromoblastomycosis. Clin Infect Dis 58: 1734–1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Belda W Criado PR Domingues PL , 2020. Case report: treatment of chromoblastomycosis with combinations including acitretin: a report of two cases. Am J Trop Med Hyg 103: 1852–1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Belda WJ Criado PR Passero L , 2020. Successful treatment of chromoblastomycosis caused by Fonsecaea pedrosoi using imiquimod. J Dermatol 47: 409–412. [DOI] [PubMed] [Google Scholar]
- 7. Kofler L Nagele U Kofler H , 2013. Recurrent vulvovaginal candidiasis: successful suppression with imiquimod. J Dermatol 40: 851. [DOI] [PubMed] [Google Scholar]
- 8. Erbagci Z Tuncel AA Erkilic S Zer Y , 2005. Successful treatment of antifungal- and cryotherapy-resistant subcutaneous hyalohyphomycosis in an immunocompetent case with topical 5% imiquimod cream. Mycopathologia 159: 521–526. [DOI] [PubMed] [Google Scholar]
- 9. Gupta AK , 2004. The treatment of chronic interdigital tinea pedis infection using imiquimod cream 5%. J Am Acad Dermatol 50: 104.14699376 [Google Scholar]
- 10. Jannuzzi GP de Almeida J Paulo L de Almeida SR Ferreira KS , 2020. Intracellular PRRs activation in targeting the immune response against fungal infections. Front Cell Infect Microbiol 10: 591970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wuthrich M et al. 2015. Fonsecaea pedrosoi-induced Th17-cell differentiation in mice is fostered by dectin-2 and suppressed by Mincle recognition. Eur J Immunol 45: 2542–2552. [DOI] [PMC free article] [PubMed] [Google Scholar]