Abstract
Background
Strict isolation precautions limit formal echocardiography use in the setting of COVID-19 infection. Information on the importance of handheld focused ultrasound for cardiac evaluation in these patients is scarce. This study investigated the utility of a handheld echocardiography device in hospitalised patients with COVID-19 in diagnosing cardiac pathologies and predicting the composite end point of in-hospital death, mechanical ventilation, shock, and acute decompensated heart failure.
Methods
From April 28 through July 27, 2020, consecutive patients diagnosed with COVID-19 underwent evaluation with the use of handheld ultrasound (Vscan Extend with Dual Probe; GE Healthcare) within 48 hours of admission. The patients were divided into 2 groups: “normal” and “abnormal” echocardiogram, as defined by biventricular systolic dysfunction/enlargement or moderate/severe valvular regurgitation/stenosis.
Results
Among 102 patients, 26 (25.5%) had abnormal echocardiograms. They were older with more comorbidities and more severe presenting symptoms compared with the group with normal echocardiograms. The prevalences of the composite outcome among low- and high-risk patients (oxygen saturation < 94%) were 3.1% and 27.1%, respectively. Multivariate logistic regression analysis revealed that an abnormal echocardiogram at presentation was independently associated with the composite end point (odds ratio 6.19, 95% confidence interval 1.50-25.57; P = 0.012).
Conclusions
An abnormal echocardiogram in COVID-19 infection settings is associated with a higher burden of medical comorbidities and independently predicts major adverse end points. Handheld focused echocardiography can be used as an important “rule-out” tool among high-risk patients with COVID-19 and should be integrated into their routine admission evaluation. However, its routine use among low-risk patients is not recommended.
Résumé
Contexte
Les précautions d’isolement strictes limitent l’utilisation de l’échocardiographie formelle en présence de COVID-19. Les renseignements sur l’importance des appareils portatifs d’échographie focalisée pour l’évaluation cardiaque en pareil cas sont rares. La présente étude vise à examiner l’utilité d’un appareil d’échocardiographie portatif chez les patients hospitalisés atteints de COVID-19 pour le diagnostic de maladies cardiaques et pour la mesure du critère d’évaluation composé regroupant le décès en milieu hospitalier, la ventilation mécanique, le choc et l’insuffisance cardiaque en décompensation aiguë.
Méthodologie
Du 28 avril au 27 juillet 2020, des patients consécutifs ayant reçu un diagnostic de COVID-19 ont été évalués au moyen d’un échographe portatif (échographe Vscan Extend à double sonde de GE Healthcare) dans les 48 heures suivant leur admission. Les patients ont été répartis en deux groupes selon que l’échocardiogramme était « normal » ou « anormal », l’évaluation étant fondée sur la présence d’une dysfonction systolique ou d’une hypertrophie biventriculaire, ou d’une régurgitation ou d’une sténose valvulaires modérées ou graves.
Résultats
Parmi les 102 patients, 26 (25,5 %) présentaient un échocardiogramme anormal. Ils étaient plus âgés, avaient plus des comorbidités et présentaient des symptômes plus graves comparativement aux patients dont l’échocardiogramme était normal. La prévalence des manifestations formant le critère d’évaluation composé, chez les patients à risque faible et les patients à risque élevé (saturation en oxygène < 94 %), a été de 3,1 % et de 27,1 %, respectivement. Une analyse de régression logistique multivariée a révélé qu’un échocardiogramme anormal lors de l’admission était associé de façon indépendante au critère d’évaluation composé (rapport de cotes : 6,19, intervalle de confiance à 95 % : 1,50-25,57; p = 0,012).
Conclusions
Un échocardiogramme anormal dans un cas de COVID-19 est associé à un fardeau plus lourd sur le plan des maladies concomitantes, et permet de prédire de façon indépendante la survenue de manifestations graves. L’échocardiographie focalisée réalisée à l’aide d’un appareil portatif peut être un outil important pour exclure certains troubles chez les patients à risque élevé atteints de COVID-19 et devrait être intégrée dans l’évaluation systématique de ces patients au moment de l’admission. Toutefois, son utilisation systématique chez les patients à risque faible n’est pas recommandée.
COVID-19 interacts with the cardiovascular system on multiple levels. It is well established that known cardiovascular disease or risk factors are associated with a significant increase in morbidity and mortality among patients with COVID-19. In addition, it has been demonstrated that elevation in cardiac biomarkers such as high-sensitivity cardiac troponin I (hs-cTnI) is correlated with a poor prognosis in COVID-19 patients.1
The association between COVID-19 and the cardiovascular system has led researchers to try to better identify predictors for severe disease and adverse outcomes. Possible predictors for disease severity might be cardiac systolic function, including left (LV) and right (RV) ventricular systolic function or valvular functional abnormalities as determined with the use of echocardiography. Routine echocardiographic evaluation of all patients admitted with COVID-19, however, is currently discouraged according to various guidelines and consensus papers owing to concerns of excessive workload in the setting of a pandemic,2 , 3 risk of infection of echocardiography professionals, and increased equipment contamination with long imaging times.4
Handheld ultrasound has been shown to be accurate when used by cardiologists for many aspects of cardiac evaluation. This includes evaluation of LV ejection fraction (LVEF), regional wall motion abnormalities, LV hypertrophy, inferior vena cava size, valvular pathology, and pericardial effusion.5 , 6 As point-of-care ultrasound (POCUS) is increasingly being used, its application in cardiac systolic function assessment is likely to markedly increase.7 , 8 LVEF, RV systolic function, and basic valvular function can be determined on admission by means of bedside echocardiography using the POCUS approach.9 , 10 In addition, echocardiography with the use of handheld devices can be performed by noncardiologists, does not need a sonography technician, can be easily cleaned, and can be stored in COVID-19 units for ease of use without disruption to the clinical setting. Furthermore, some devices can be used for lung assessment as well, with a quick and > 90% accurate interpretation for common causes of acute respiratory failure.11
The objective of the present study was to characterise the utility of handheld echocardiography in hospitalised patients with COVID-19 to predict end points based on identified cardiac abnormalities, including ventricular size and systolic function, and valvular pathologies.
Methods
Study setting
This was a prospective study of real-time focused echocardiography and lung ultrasound performed using a handheld device. The study was conducted on consecutive patients with polymerase chain reaction–confirmed COVID-19 hospitalised in designated medical wards at a tertiary care medical center from April 28 through July 27, 2020. The study was approved by the hospital’s institutional review board.
All echocardiographic clips were acquired by cardiologists or intensivists and were later interpreted by a fellowship-trained echocardiographer. Variables including demographics, past medical history, electrocardiography (ECG), imaging modalities, and laboratory results obtained from the medical record.
Study end points
The primary end point was defined as a composite end point of in-hospital death, mechanical ventilation, shock, and acute decompensated heart failure (ADHF). Secondary end points included the composite end point, individual parameters of the composite end point, advanced ventilatory support (high-flow nasal cannula, noninvasive positive airway pressure support, and invasive ventilation), chronic ventilation, myocardial injury (defined as hs-cTnI > 3 times upper normal limit), venous thromboembolism, anti–COVID-19 drug use, sepsis, and length of hospital stay.
Study protocol
Patients with confirmed COVID-19 who were hospitalised in designated internal medicine departments were recruited into the study. Conscious patients consented verbally. Patients who were not able to give informed consent underwent echocardiography if it was clinically indicated. Patients that refused to participate in the study were excluded. Basic characteristics included age, sex, and known previous medical illness. Routine chest X-ray, ECG, and blood workup were performed for every patient on admission to the designated COVID-19 wards. The routine laboratory tests included complete blood count, renal function, electrolytes, hs-cTnI, d-dimer, coagulation function tests, and C-reactive protein (CRP). B-Type natriuretic peptide was measured according to the clinical judgment of the treating physician. The study physicians performing the ultrasound examination wore personal protective equipment including a full gown, N95 face mask, face shield, and at least 2 sets of gloves. Participants were evaluated by focused echocardiographic examination and lung ultrasound within 48 hours of their hospitalisation with the use of a handheld ultrasound machine (Vscan Extend with Dual Probe; General Electric, Northville, MI). The cardiac POCUS was conducted using the sector transducer from the apical, parasternal, and substernal views. Valves were evaluated visually using both 2-dimensional (2D) and color Doppler echocardiography. The acquired video clips were stored in the Digital Imaging and Communications in Medicine format and sent wirelessly to a picture archiving and use platform (McKesson Cardiology, version 14.0, Alpharetta, GA, USA) routinely used by the cardiology department. The echocardiogram clips were then interpreted by visual evaluation by an experienced echocardiographer (A.B.), blinded to the patient’s clinical course and presentation, for evaluation of LVEF and LV diameter, RV visual systolic function and RV diameter, severity of valvular dysfunction (the valves were visually assessed for functional abnormalities, ie, regurgitation or stenosis, with the use of both 2D and Doppler echocardiograms), pericardial effusion, and any additional significant echocardiographic findings. Offline measurements of LV end-diastolic diameter (LVEDD), tricuspid annular plane systolic excursion (TAPSE), and fractional area change were made. POCUS lung ultrasound was performed using the linear transducer and included a 10-location assessment (standard approach: 4 quadrants on each anterior hemithorax and 2 on each posterior hemithorax) for B-lines, subpleural consolidations/lung hepatisation, and pleural effusions. Each assessed variable was graded separately for each location according to the severity as 0 (normal), 1 (several lines or small consolidation/effusion), or 2 (coalescent B-lines or diffuse/widespread consolidation/effusion). The lung ultrasound assessment scoring was calculated as the sum of the entire graded variables (range of 0-20).
Data management
All data obtained in this study were entered into 2 Microsoft Excel spreadsheets. One file contained the case-identifying number, patient identifiers, and other pertinent variables. POCUS results were inserted into a second file by the patient’s identifying number. The 2 files were then matched.
Study participants were divided into normal or abnormal echocardiograms according to POCUS results. Abnormal echocardiograms included those with LVEF < 50%, LV dilation, RV systolic dysfunction/dilation, and moderate/severe valvular dysfunction (functional regurgitation or stenosis).
Statistical analyses
The patients were divided into normal and abnormal echocardiograms, and analyses were performed accordingly. Descriptive statistics were used to analyse differences in baseline and clinical characteristics, echocardiography and lung ultrasound results, and end points, with the use of chi-square or Fisher exact test for categoric variables and t test or Mann-Whitney U test for continuous variables, as appropriate. Test selection was based on data distribution and normalcy.
High-risk patients were defined as those with room-air oxygen saturation < 94%. The ability of the echocardiography results to identify patients with and without the composite outcome was then tested for sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) among low- and high-risk patients.
Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to test the univariate associations between abnormal echocardiogram and the composite end point and individual end points.
Multivariate logistic regression analysis (OR and 95% CI) was calculated for the association between abnormal echocardiogram and the composite end point among the entire cohort and individually among high-risk patients, including pertinent baseline characteristics covariates (those with P values < 0.05). Statistical analyses were performed with the use of SPSS Statistics for Windows version 21 (SPSS, Chicago, IL, USA).
Results
A total of 102 hospitalised patients with COVID-19 were recruited into the study, including 76 (74.5%) with normal and 26 (25.5%) with abnormal echocardiograms (Table 1 ). Four patients refused to participate in the trial and were therefore excluded.
Table 1.
Baseline and clinical characteristics
| Variable | All (n = 102) | Normal echocardiogram (n = 76) | Abnormal echocardiogram (n = 26) | P value |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age, years | 59.7 ± 18.4 | 57.0 ± 18.6 | 67.6 ± 15.5 | 0.010 |
| Male | 65 (63.7) | 48 (63.2) | 17 (65.4) | 0.838 |
| Body mass index, kg/m2 | 27.9 ± 6.2 | 27.6 ± 6.2 | 28.9 ± 6.2 | 0.378 |
| Smoking | 16 (15.7) | 8 (10.5) | 8 (30.8) | 0.014 |
| Diabetes mellitus | 33 (32.4) | 21 (27.6) | 12 (46.2) | 0.081 |
| Hypertension | 39 (38.2) | 23 (30.3) | 16 (61.5) | 0.005 |
| Hyperlipidemia | 32 (31.4) | 18 (23.7) | 14 (53.8) | 0.004 |
| IHD | 20 (19.6) | 9 (11.8) | 11 (42.3) | 0.001 |
| CVA | 5 (4.9) | 2 (2.6) | 3 (11.5) | 0.103 |
| Revascularisation | 17 (16.7) | 7 (9.2) | 10 (38.5) | 0.001 |
| Heart failure | 12 (11.8) | 3 (3.9) | 9 (34.6) | < 0.001 |
| Valve replacement | 3 (2.9) | 0 (0.0) | 3 (11.5) | 0.015 |
| CIED | 3 (2.9) | 0 (0.0) | 3 (11.5) | 0.015 |
| Cognitive decline | 23 (22.5) | 14 (18.4) | 9 (34.6) | 0.088 |
| Debilitation | 26 (25.5) | 16 (21.1) | 10 (38.5) | 0.079 |
| Chronic lung disease | 9 (8.8) | 6 (7.9) | 3 (11.5) | 0.690 |
| Liver disease | 2 (2.0) | 2 (2.6) | 0 (0.0) | 1.000 |
| Previous VTE | 4 (3.9) | 2 (2.6) | 2 (7.7) | 0.268 |
| Malignancy | 2 (2.0) | 1 (1.3) | 1 (3.8) | 0.447 |
| Immunosuppression | 4 (3.9) | 3 (3.9) | 1 (3.8) | 1.000 |
| Hypothyroidism | 13 (12.7) | 8 (10.5) | 5 (19.2) | 0.251 |
| Chronic medications | ||||
| ACE-I/ARB | 24 (23.5) | 14 (18.4) | 10 (38.5) | 0.038 |
| β-Blockers | 29 (28.4) | 15 (19.7) | 14 (53.8) | 0.001 |
| CCB | 12 (11.8) | 9 (11.8) | 3 (11.5) | 1.000 |
| Antiplatelets | 26 (25.5) | 12 (15.8) | 14 (53.8) | < 0.001 |
| Oral anticoagulation | 13 (12.7) | 8 (10.5) | 5 (19.2) | 0.251 |
| Diuretics | 11 (10.8) | 4 (5.3) | 7 (26.9) | 0.005 |
| Inhalations | 7 (6.9) | 5 (6.6) | 2 (7.7) | 1.000 |
| SGLT2 inhibitors | 7 (6.9) | 5 (6.6) | 2 (7.7) | 1.000 |
| Statins | 33 (32.4) | 17 (22.4) | 16 (61.5) | < 0.001 |
| COVID-19 presentation | ||||
| Chest pain | 28 (27.5) | 22 (28.9) | 6 (23.1) | 0.563 |
| Shortness of breath | 54 (52.9) | 37 (48.7) | 17 (65.4) | 0.141 |
| HR, beats/min | 88.8 ± 22.3 | 88.1 ± 19.3 | 90.7 ± 30.0 | 0.626 |
| SBP, mm Hg | 124.3 ± 20.9 | 123.4 ± 19.9 | 126.8 ± 23.7 | 0.461 |
| DBP, mm Hg | 74.1 ± 12.0 | 73.6 ± 11.2 | 75.6 ± 14.3 | 0.375 |
| SpO2, % | 87.4 ± 11.4 | 87.3 ± 11.9 | 87.8 ± 10.3 | 0.752 |
| In-hospital course | ||||
| Sinus bradycardia | 2 (2.0) | 2 (2.7) | 0 (0.0) | 1.000 |
| ECG changes | 0.040 | |||
| Normal | 74 (72.5) | 59 (77.6) | 15 (57.7) | |
| Nonspecific changes | 19 (18.6) | 12 (15.8) | 7 (26.9) | |
| TWI/ST-segment depression | 6 (5.9) | 4 (5.3) | 2 (7.7) | |
| ST-segment elevation | 2 (2.0) | 0 (0.0) | 2 (7.7) | |
| Chest X-ray infiltrates | 75 (73.5) | 51 (67.1) | 24 (92.3) | 0.012 |
| AF/AFL | 11 (10.8) | 7 (9.2) | 4 (15.4) | 0.130 |
| Laboratory results | ||||
| WBC (p), 103/μL | 10.4 ± 5.7 | 9.6 ± 5.0 | 12.8 ± 6.7 | 0.013 |
| ANC/ALC (a) | 5.9 (3.0-10.6) | 5.4 (2.6-8.9) | 9.0 (4.4-13.4) | 0.032 |
| Hemoglobin (a), g/dL | 13.0 ± 2.3 | 13.1 ± 2.1 | 12.6 ± 2.7 | 0.240 |
| Platelets (a), 103/μL | 200.6 ± 73.6 | 203.0 ± 73.3 | 193.2 ± 75.3 | 0.802 |
| Creatinine (a), mg/dL | 1.0 ± 0.7 | 0.9 ± 0.4 | 1.4 ± 1.1 | 0.002 |
| K (a), mmol/L | 4.0 ± 0.6 | 3.9 ± 0.5 | 4.1 ± 0.7 | 0.168 |
| Albumin (t), g/dL | 3.0 ± 0.8 | 3.1 ± 0.8 | 2.6 ± 0.7 | 0.044 |
| hs-cTnI (p), ng/L | 7.0 (5.0-40.8) | 5.5 (5.0-22.0) | 37 (6.5-541.5) | 0.001 |
| BNP (a), pg/mL | 76.5 (22.5-229.5) | 59.8 (15.0-200.8) | 224.5 (94.5-753.5) | 0.065 |
| CRP (p), mg/L | 13.0 ± 11.8 | 11.2 ± 11.6 | 18.2 ± 10.9 | 0.003 |
| d-dimer (p), ng/mL | 925 (522-1188) | 803 (392-1362) | 1178 (878-2707) | 0.014 |
| Fibrinogen (a), mg/dL | 594.9 ± 186.5 | 572.9 ± 187.8 | 660.1 ± 169.3 | 0.015 |
| aPTT (p), seconds | 35.0 ± 9.7 | 33.9 ± 9.7 | 38.1 ± 9.2 | 0.009 |
Values are presented as mean ± SD, n (%), or median (interquartile range).
a, admission; ACE-I, angiotensin-converting enzyme inhibitor; AF, atrial fibrillation; AFL, atrial flutter; ALC, absolute lymphocytes count; ANC, absolute neutrophils count; aPTT, activated partial thromboplastin time; ARB, angiotensin receptor blocker; BNP, B-type natriuretic peptide; CCB, calcium channel blocker; CIED, cardiovascular implantable electronic device; CRP, C-reactive protein; CVA, cerebrovascular accident; DBP, diastolic blood pressure; ECG, electrocardiography; HR, heart rate; hs-cTnI, high sensitive cardiac troponin I; IHD, ischemic heart disease; IQR, interquartile range; K, potassium; p, peak; SBP, systolic blood pressure; SGLT2, sodium-glucose transport protein 2; SpO2, oxygen saturation; t, trough; TWI, T-wave inversion; VTE, venous thromboembolism; WBC, white blood cells.
Baseline and medical characteristics
As presented in Table 1, the mean age of the total cohort was 59.7 ± 18.4 years, and 63.7% were male. Patients with an abnormal echocardiogram were older and more likely to suffer from comorbidities including smoking, hypertension, hyperlipidemia, ischemic heart disease, past revascularisation, and heart failure compared with patients with a normal echocardiogram. They had a higher proportion of past valve replacement and cardiac implantable electronic devices. Moreover, they were treated more often with chronic heart failure evidence-based medications, antiplatelets, diuretics, and statins.
Presentation characteristics and laboratory results
As presented in Table 1, the 2 groups did not differ in their presenting complaints or vital signs. Patients with abnormal echocardiograms had a higher rate of pathologic ECG (including nonspecific and ST-segment changes or T-wave inversion) and chest X-ray infiltrates, compared with those with normal echocardiograms. Laboratory results of creatinine, hs-cTnI, fibrinogen, activated partial thromboplastin time, white blood cell count, neutrophil/lymphocyte count ratio, CRP, and d-dimer were higher in the abnormal than in the normal echocardiogram group, whereas albumin was lower.
Echocardiography and lung ultrasound results
Echocardiography and lung ultrasound results are presented in Table 2 . Compared with patients with a normal echocardiogram, those with an abnormal echocardiogram had a lower LVEF (49.2 ± 8.2% vs 57.2 ± 4.1%; P < 0.001), higher LVEDD (4.8 ± 0.6 cm vs 4.5 ± 0.5 cm; P = 0.016), and higher proportions of LVEF < 50%, RV systolic dysfunction and dilation, pericardial effusion, and significant valvulopathy (including significant mitral and tricuspid regurgitation and aortic stenosis). Comparing lung scores between patients with a normal echocardiogram and those with an abnormal echocardiogram yielded no association (2.9 ± 2.4 vs 3.7 ± 2.5; P = 0.119).
Table 2.
Echocardiography results, measurements, and lung ultrasound score for patients with and without in-hospital advanced ventilatory support
| Parameter | All (n = 102) | Normal echocardiogram (n = 76) | Abnormal echocardiogram∗ (n = 26) | P value† | No advanced ventilatory support (n = 76) | Advanced ventilatory support (n = 26) | P value‡ |
|---|---|---|---|---|---|---|---|
| LVEF, % | 53.4 ± 6.8 | 57.2 ± 4.1 | 49.2 ± 8.2 | < 0.001 | 55.8 ± 6.3 | 53.4 ± 6.6 | 0.096 |
| LVEF < 50% | 16 (15.7) | 0 (0.0) | 16 (61.5) | < 0.001 | 9 (11.8) | 7 (26.9) | 0.068 |
| LVEDD, cm | 4.6 ± 0.5 | 4.5 ± 0.5 | 4.8 ± 0.6 | 0.016 | 4.6 ± 0.6 | 4.6 ± 0.5 | 0.692 |
| RV dysfunction | 8 (7.8) | 0 (0.0) | 8 (30.8) | < 0.001 | 5 (6.6) | 3 (11.5) | 0.425 |
| RV dilation | 7 (6.7) | 0 (0.0) | 7 (26.9) | < 0.001 | 5 (6.6) | 2 (7.7) | 1.000 |
| Ventricular abnormality | 24 (23.5) | 0 (0.0) | 24 (92.3) | < 0.001 | 14 (18.4) | 10 (38.5) | 0.034 |
| TAPSE, cm | 1.9 ± 0.3 | 2.0 ± 0.3 | 1.8 ± 0.2 | 0.159 | 2.0 ± 0.3 | 1.8 ± 0.2 | 0.045 |
| FAC, % | 35.2 ± 6.5 | 35.6 ± 6.0 | 34.1 ± 7.7 | 0.518 | 34.9 ± 6.5 | 36.4 ± 6.7 | 0.563 |
| Significant MR | 7 (6.9) | 0 (0.0) | 7 (26.9) | < 0.001 | 4 (5.3) | 3 (11.5) | 0.365 |
| Significant TR | 6 (5.9) | 0 (0.0) | 6 (23.1) | < 0.001 | 3 (3.9) | 3 (11.5) | 0.167 |
| Significant AS | 6 (5.9) | 0 (0.0) | 6 (23.1) | < 0.001 | 4 (5.3) | 2 (7.7) | 0.636 |
| Significant valvulopathy | 9 (8.8) | 0 (0.0) | 9 (34.6) | < 0.001 | 5 (6.6) | 4 (15.4) | 0.225 |
| Pericardial effusion | 6 (5.9) | 0 (0.0) | 6 (23.1) | < 0.001 | 3 (3.9) | 3 (11.5) | 0.171 |
| Lung score | 3.1 ± 2.4 | 2.9 ± 2.4 | 3.7 ± 2.5 | 0.119 | 2.7 ± 2.3 | 4.5 ± 2.4 | 0.001 |
Values are presented as mean ± SD or n (%).
AS, aortic stenosis; FAC, fractional area change; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; MR, mitral regurgitation; RV, right ventricular; TAPSE, tricuspid annular plane systolic excursion; TR, tricuspid regurgitation.
Abnormal echocardiogram was defined as left or right ventricular dysfunction or enlargement, or moderate/severe valvular regurgitation/stenosis echocardiographic study.
P value for the difference between normal and abnormal echocardiograms.
P value for the difference between advanced ventilatory support and no support.
Four patients underwent an official echocardiography after the study examination during the index hospitalisation, which confirmed the findings of the focused echocardiogram.
Results among patients with and without advanced ventilatory support
Echocardiogram results and measurements among patients with and without advanced ventilatory support are presented in Table 2. Compared with patients with no advanced ventilatory support, patients with such support had a higher proportion of ventricular abnormalities (38.5% vs 18.4%; P = 0.034), a lower TAPSE (1.8 ± 0.2 cm vs 2.0 ± 0.3 cm; P = 0.045) and a higher lung score (4.5 ± 2.4 vs 2.7 ± 2.3; P = 0.001). The groups did not differ in other assessed or measured POCUS parameters.
Sensitivity and specificity among low- and high-risk patients
Among the 102 patients included in the study, only 32 were defined as low risk (with room-air oxygen saturation ≥ 94%), including 6 patients with abnormal echocardiograms, of which only 1 patient had the composite outcome. The sensitivity of focused echocardiography for the composite outcome among low-risk patients was 100% and the specificity 83.9% with PPV 16.7% and NPV 100%.
Among the 70 patients defined as high risk (with room-air oxygen saturation < 94%), the sensitivity of focused echocardiography for the composite outcome was 57.9% and the specificity 82.4% with PPV 55.0% and NPV 84.0%.
Association between abnormal echocardiogram and study end points
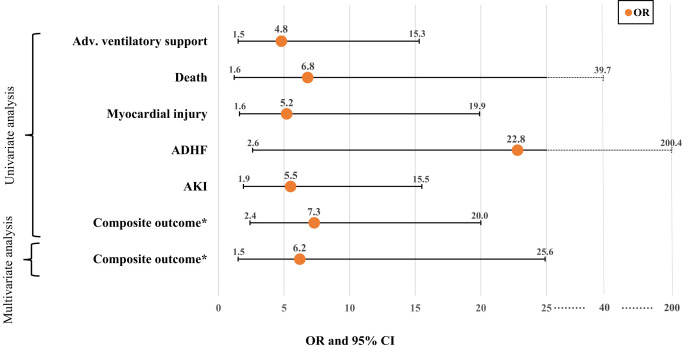
The associations between an abnormal echocardiogram and the end points are presented in Table 3 and Figure 1 . An abnormal echocardiogram was associated with the end points of the need for advanced ventilatory support, ADHF, myocardial injury, acute kidney injury, death, and the composite end point (in-hospital death, mechanical ventilation, shock, and ADHF; unadjusted OR 7.29, 95% CI 2.44-20.00).
Table 3.
The association between abnormal echocardiogram and serious adverse events (end points)
| Variable | All (n = 102) | Normal echocardiography (n = 76) | Abnormal echocardiography (n = 26) | P value | Unadjusted OR (95% CI) |
|---|---|---|---|---|---|
| Composite outcome∗ | 20 (19.6) | 8 (10.5) | 12 (46.2) | < 0.001 | 7.29 (2.44-20.00) |
| In-hospital death | 6 (5.9) | 2 (2.6) | 4 (15.4) | 0.033 | 6.82 (1.2-39.7) |
| Mechanical ventilation | 12 (11.8) | 7 (9.2) | 5 (19.2) | 0.164 | 2.38 (0.68-8.29) |
| Shock | 7 (6.9) | 4 (5.3) | 3 (11.5) | 0.249 | 2.35 (0.5-11.3) |
| ADHF | 6 (5.9) | 0 (0.0) | 6 (23.1) | 0.005 | 22.8 (2.6-200.4) |
| Advanced ventilatory support | 26 (25.5) | 15 (19.7) | 11 (42.3) | 0.021 | 4.83 (1.5-15.3) |
| Myocardial injury | 14 (13.7) | 6 (7.9) | 8 (30.8) | 0.003 | 5.19 (1.6-19.9) |
| Chronic ventilation | 9 (8.8) | 6 (7.9) | 3 (11.5) | 0.414 | 1.52 (0.4-6.6) |
| Venous thromboembolism | 3 (2.9) | 2 (2.6) | 1 (3.8) | 1.000 | 1.48 (0.1-17.0) |
| Anti–COVID-19 drugs | 40 (39.2) | 27 (35.5) | 13 (50.0) | 0.192 | 1.82 (0.7-4.7) |
| Sepsis | 11 (10.8) | 6 (7.9) | 5 (19.2) | 0.108 | 2.78 (0.8-10.0) |
| Acute kidney injury | 20 (19.6) | 9 (11.8) | 11 (42.3) | 0.001 | 5.46 (1.9-15.5) |
| New renal replacement therapy | 3 (2.9) | 0 (0.0) | 3 (11.5) | 0.052 | 9.9 (0.98-99.9) |
| LOS, days | 8.1 (3.0-16.3) | 7 (2.8-14.1) | 10.4 (6.8-29.3) | 0.202 | 5.07 (−2.75-12.89) |
Values are presented as n (%) or median (interquartile range).
ADHF, acute decompensated heart failure; CI, confidence interval; LOS, length of stay; OR, odds ratio.
Composite outcome included in-hospital death, mechanical ventilation, shock, and acute decompensated heart failure.
Figure 1.
Significant associations (odds ratio [OR] and 95% confidence interval [CI]) between abnormal echocardiogram and serious adverse events (end points). ∗The primary end point was defined as a composite end point of in-hospital death, mechanical ventilation, shock, and acute decompensated heart failure. Numeric results of OR and 95% CI and are detailed in Table 3. ADHF, acute decompensated heart failure; Adv., advanced; AKI, acute kidney injury.
Multivariate analysis adjusting for age, heart failure, ischemic heart disease, smoking, hypertension, hyperlipidemia, previous revascularisation, cardiovascular implantable electronic device (CIED) implantation, or valve replacement revealed that among the entire cohort, an abnormal echocardiogram was independently associated with a higher probability for the composite end point (OR 6.19, 95% CI 1.50-25.57; P = 0.012).
Multivariate analysis adjusting for age, heart failure, hypertension, hyperlipidemia, smoking, and CIED implantation revealed that among high-risk patients, an abnormal echocardiogram was independently associated with a higher probability for the composite end point (OR 5.47, 95% CI 1.29-23.30; P = 0.022).
Association between lung score and study end points
The lung score was associated with the end points of the need for advanced ventilatory support, anti–COVID-19 medication use, myocardial injury, hospital length of stay, mechanical ventilation, ADHF, in-hospital death, and the composite end point (unadjusted OR 1.44, 95% CI 1.18-1.77).
Multivariate analysis adjusting for the above pertinent variables revealed that the continuous lung score was independently associated with a higher probability for the composite end point (OR 1.56, 95% CI 1.12-2.03; P = 0.001).
Discussion
This study is, to the best of our knowledge, the first to investigate the utility of handheld echocardiography in hospitalised patients with COVID-19 to predict end points based on identified cardiac abnormalities. Hospitalised patients with COVID-19 and an abnormal echocardiogram presented with a higher proportion of comorbidities and worse baseline functioning. Abnormal ventricular function/size or significant valvular pathology identified with the use of handheld ultrasound were associated with worse end points and were independently predictive of the composite end point of death, mechanical ventilation, shock, and ADHF. Also, the lung score with the use of a handheld ultrasound was associated with worse end points and was independently predictive of the composite end point. Among low-risk patients (with room-air oxygen saturation ≥ 94%) the prevalence of the composite end point was very low (3.1%) and focused echocardiography had a positive predictive value of only 14.3% in this group of patients.
COVID-19 is known to manifest a wide spectrum of cardiac pathologies and the use of echocardiography in these patients has an important role in the settings of myocarditis, acute coronary syndrome, cardiomyopathy, pericardial effusion, arrhythmia, and shock. Therefore, a timely echocardiogram is integral to the clinical evaluation and management of patients with COVID-19. The burden of the pandemic on health care systems necessitates achieving an appropriate balance between the relative necessity of the examination and the duty of sonographers, nurses, advanced practice providers, and physicians to provide high-quality imaging while limiting viral spread, reducing staff exposure, and protecting patients. In these settings, traditional criteria for echocardiography use seem too extensive and clinicians are required to prioritise the need for this valuable resource. The handheld devices have smaller nonsterile exposed areas compared with standard machines and can be easily decontaminated with disinfectant wipes, and their size allows for them to be entirely enclosed by a sterile covering to limit iatrogenic virus transmission.12 , 13 The findings of the present study support the acquisition of a cardiac assessment sonographic tool that can be dedicated to the COVID-19 departments and can be operated more conveniently in accordance with recommended precautions.
An abnormal echocardiogram was observed in 25.5% of the study population. Other studies using standard cart-based machines or laptops and conducted on hospitalised patients with COVID-19 have found a relatively high rate of sonography-based cardiac abnormalities, ranging up to 68%, with RV systolic dysfunction being the most predominant finding (10%-52.8%).14, 15, 16, 17, 18, 19, 20 This discrepancy may be explained by selection bias (patients with advanced illness), differing timelines between echocardiography and disease onset, lack of Doppler usage, partial RV visualisation, and discrepancies in the definition of an abnormal echocardiogram. Another important difference is the use of high-end devices or detailed full echocardiographic examinations in most of the studies. Because none of the studies used handheld ultrasound, their examination may be more meticulous but less practical in the COVID-19 clinical setting.
An example of studies focusing on patients with advanced illness is one in which an echocardiogram was performed only after approval by 3 physicians and on patients with elevated high-sensitivity troponin or a clinical need for the examination.19 In that study, 82% of the patients required mechanical ventilation and 58% required vasopressor support. A correlation between disease severity and the prevalence of an abnormal echocardiogram can be found in a cross-sectional study comparing patients with nonsevere COVID-19 and those with severe disease, demonstrating larger biventricular diameters alongside lower LVEF and RV fractional area change in those with severe disease.21
An association between mortality and cardiac abnormality on the echocardiogram was also found by Karagodin et al., who demonstrated an association between both LV and RV strain and mortality.22 However, the routine use of strain for ventricular assessment is limited for patients hospitalised in COVID-19–designated departments. Also, unlike in our study, their cohort included a very high in-hospital mortality rate of 21.6%, which may reflect selection bias of patients with more severe COVID-19.
Study limitations
This was a prospective, single-centre, observational study and not a randomised trial, and as such is subjected to associated confounding factors. However, after constructing a multivariate analysis, the independent predictive value remained substantial. Also, data regarding previous echocardiographic examinations are lacking and not included in the analysis. Lack of pulsed- and continuous-wave Doppler usage and simultaneous electrocardiography limited the evaluation of valvular pathologies, hemodynamics, and echocardiographic images, which may have led to an underestimation of cardiac pathologies. Nonetheless, the study provides data in real-world settings that are relevant to the day-to-day limited clinical use of POCUS echocardiography in COVID-19 wards. A prospective POCUS study with noncardiologists vs cardiologists and low-risk vs high-risk patients would assist in clarifying the limitations of this study.
Conclusion
Abnormal echocardiographic results in hospitalised patients with COVID-19, when performed by a cardiologist or intensivist and interpreted by a fellowship-trained echocardiographer in a tertiary care setting, are associated with a higher burden of comorbidities and independently predict major adverse end points. Hand-held POCUS of hospitalised patients with COVID-19 can be utilized as an important “rule-out” tool among high-risk patients (with room-air oxygen saturation < 94%) and should be integrated as part of their routine admission evaluation. The routine use of focused echocardiography among low-risk patients is not recommended for prognostication or as a screening tool.
Acknowledgements
The authors thank GE Healthcare for the temporary supply of a Vscan Extend ultrasound device for research purposes.
Funding Sources
This study was funded by Shaare Zedek Scientific (fund no. 18004712), Shaare Zedek Medical Center’s technology transfer company.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 345 for disclosure information.
References
- 1.Zhou F., Ting Yu, Ronghui Du, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.European Society of Cardiology ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic. Eur Heart J. 2021 doi: 10.1093/eurheartj/ehab696. ehab696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirkpatrick J.N., Mitchell C., Taub C., et al. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak: endorsed by the American College of Cardiology. J Am Soc Echocardiogr. 2020;33:648–653. doi: 10.1016/j.echo.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skulstad H., Cosyns B., Popescu B.A., et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging. 2020;21:592–598. doi: 10.1093/ehjci/jeaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoica R., Heller E.N., Bella J.N. Point-of-care screening for left ventricular hypertrophy and concentric geometry using hand-held cardiac ultrasound in hypertensive patients. Am J Cardiovasc Dis. 2011;1:119–125. [PMC free article] [PubMed] [Google Scholar]
- 6.Khan H.A., Wineinger N.E., Uddin P.Q., et al. Can hospital rounds with pocket ultrasound by cardiologists reduce standard echocardiography? Am J Med. 2014;127:669.e1–669.e7. doi: 10.1016/j.amjmed.2014.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore C.L., Copel J.A. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 8.Dietrich C.F., Goudie A., Chiorean L., et al. Point of care ultrasound: a WFUMB position paper. Ultrasound Med Biol. 2017;43:49–58. doi: 10.1016/j.ultrasmedbio.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 9.McKaigney C.J., Krantz M.J., La-Rocque C.L., Hurst N.D., Buchanan M.S., Kendall J.L. E-point septal separation: a bedside tool for emergency physician assessment of left ventricular ejection fraction. Am J Emerg Med. 2014;32:493–497. doi: 10.1016/j.ajem.2014.01.045. [DOI] [PubMed] [Google Scholar]
- 10.Wright J., Jarman R., Connolly J., Dissmann P. Echocardiography in the emergency department. Emerg Med J. 2009;26:82–86. doi: 10.1136/emj.2008.058560. [DOI] [PubMed] [Google Scholar]
- 11.Kiamanesh O., Harper L., Wiskar K., et al. Lung ultrasound for cardiologists in the time of COVID-19. Can J Cardiol. 2020;36:1144–1147. doi: 10.1016/j.cjca.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jenkins S., Garg P. Prime time for handheld echocardiography in COVID-19 pandemic. Clin Med (Lond) 2020;20:e132. doi: 10.7861/clinmed.Let.20.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gibson L.E., Bittner E.A., Chang M.G. Handheld ultrasound devices: an emerging technology to reduce viral spread during the Covid-19 pandemic. Am J Infect Control. 2020;48:968–969. doi: 10.1016/j.ajic.2020.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Szekely Y., Lichter Y., Taieb P., et al. Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation. 2020;142:342–353. doi: 10.1161/CIRCULATIONAHA.120.047971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y., Li H., Li M., Zhang L., Xie M. The prevalence, risk factors and outcome of cardiac dysfunction in hospitalized patients with COVID-19. Intensive Care Med. 2020;46:2096–2098. doi: 10.1007/s00134-020-06205-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jain S.S., Liu Q., Raikhelkar J., et al. Indications for and findings on transthoracic echocardiography in COVID-19. J Am Soc Echocardiogr. 2020;33:1278–1284. doi: 10.1016/j.echo.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moody W.E., Mahmoud-Elsayed H.M., Senior J., et al. Impact of right ventricular dysfunction on mortality in patients hospitalized with COVID-19, according to race. CJC Open. 2021;3:91–100. doi: 10.1016/j.cjco.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van den Heuvel F.M., Vos J.L., Koop Y., et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth Heart J. 2020;28:410–417. doi: 10.1007/s12471-020-01458-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahmoud-Elsayed H.M., Moody W.E., Bradlow W.M., et al. Echocardiographic findings in patients with COVID-19 pneumonia. Can J Cardiol. 2020;36:1203–1207. doi: 10.1016/j.cjca.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dweck M.R., Bularga A., Hahn R.T., et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21:949–958. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barman H.A., Atici A., Tekin E.A., et al. Echocardiographic features of patients with COVID-19 infection: a cross-sectional study. Int J Cardiovasc Imaging. 2021;37:825–834. doi: 10.1007/s10554-020-02051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karagodin I., Singulane C.C., Woodward G.M., et al. WASE-COVID Investigators Echocardiographic correlates of in-hospital death in patients with acute COVID-19 infection: the World Alliance Societies of Echocardiography (WASE-COVID) study. J Am Soc Echocardiogr. 2021;34:819–830. doi: 10.1016/j.echo.2021.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]