ABSTRACT
Background: Vaccine hesitancy is a leading threat to public health. It has been studied extensively in North America and Europe but much less in Arab countries. The Parent Attitudes about Childhood Vaccines (PACV) survey is a validated tool for identifying vaccine-hesitant parents; however, Arabic version is not available. This study aimed to assess the reliability of the PACV survey in the Arabic language and to determine the prevalence of vaccine hesitancy among parents in the United Arab Emirates (UAE).
Methods Forward and backward translation of the PACV in the Arabic language was carried out. The reliability of the Arabic-PACV survey was tested among parents with children. The same survey was used to study vaccine hesitancy among parents attending seven ambulatory health-care services in Al-Ain city, UAE. The associations between vaccine hesitancy and socio-demographic characteristics were explored.
Results: The Cronbach alpha for Arabic-PACV scores was 0.79. Three hundred participants answered the survey (response rate, 85.7%). The majority were Emirati mothers (77%) in the age group (30–49 years). Only 36 parents (12%, 95% CI 8.5,16.2) were found to be vaccine-hesitant. Parent’s greatest concerns were mainly the side effects (35%), safety of vaccines (17% unsure and 28% concerned) and getting too many injections (28%). Divorced marital status was significantly associated with vaccine hesitancy (p < .001).
Conclusion: The Arabic-PACV survey could serve as a tool in the evaluation of vaccine hesitancy among parents in UAE and other Arabic-speaking countries. Many parents in our community were concerned about the vaccine safety. Targeted preventive measures are needed.
KEYWORDS: Vaccine hesitancy, UAE, PACV, vaccine safety
Introduction
Vaccine hesitancy presents a real threat to global health as declared by the World Health Organization (WHO).1 It is one of the major challenges facing childhood vaccination nowadays.2 While vaccinations are preventing around 2–3 million deaths every year, more than 19 million infants worldwide did not benefit from routine immunization services in 2018.3 The success of any vaccination program relies heavily on maintaining high vaccine coverage that ensures direct protection to the vaccinated people as well as indirect protection for the overall community.4
The WHO defines vaccine hesitancy as a “delay in acceptance or refusal of vaccines despite the availability of vaccination services.” It is complex, context-specific, and varies across time, place, and vaccines.5 Vaccine-hesitant individuals are a heterogeneous group. They may refuse some vaccines but agree to others; they may also delay vaccines or accept vaccines according to the recommended schedule while still remaining unsure.6,7
As observed in other countries, social media in the United Arab Emirates (UAE) greatly influence people’s beliefs and behaviors and might have an impact on vaccination uptake.8 Health-carevaccination opinions in the UAE are on the rise especially during the recent national measles vaccine campaign and following the introduction of Human Papillomavirus vaccine. In Italy, there was around an 18% decline in influenza vaccine coverage between the years 2013 and 2014 because of media reporting on the adverse effects of vaccines.9 In the UAE, vaccine coverage estimates for the last 10 years have been consistently above 95% for most childhood vaccines including DTP and MMR.10 Despite the high coverage, in the year 2018, 4290 cases of chickenpox, 57 cases of measles, 227 cases of mumps, and 65 cases of pertussis were reported to the Health Authority of Abu Dhabi, UAE. Unfortunately, the vaccination status of these individuals was not documented.11
To the best of our knowledge, parents’ vaccine hesitancy has never been explored in the UAE.12 In the wake of these new movements against vaccination, exploring and understanding vaccine hesitancy among parents in the UAE is essential to inform decision-makers so that appropriate strategies can be adopted to mitigate these barriers and improve public health.
The Parent Attitudes About Childhood Vaccines (PACV) survey is a validated tool that has been successfully used in several countries to identify vaccine-hesitant parents.13-17 It can predict child under-immunization especially in those of parents with high PACV scores.6 However, as the PACV was originally developed in the English language and used mainly among parents in North America and Europe, its performance among Arab populations is unknown.
The aims of this study are to evaluate the reliability of the PACV survey in the Arabic language, assess the prevalence of vaccine hesitancy, analyze the parental attitudes and concerns pertaining to vaccines, and identify sociodemographic factors associated with vaccine hesitancy among parents in the UAE.
Methods
Study setting, population, and sampling
This cross-sectional study was conducted from April to July 2019 among parents attending antenatal and postnatal clinics in the Ambulatory Healthcare Services (AHS) in Al-Ain city, UAE. We used a convenience sample of parents attending seven AHS centers in different geographic parts of Al Ain city capturing both urban and rural areas. We approached Arabic-speaking parents who were present in the waiting areas and invited them to participate. Parents who are expecting a child or have had at least one child before were approached to fill in the questionnaire. The questionnaire was completed autonomously by the respondent unless the respondent herself or himself approached the researchers for help and assistance. Participation was voluntary. We obtained a written informed consent from all participants. Assuming that 10.5% are hesitant, in accordance with regional literature, 15,18 to obtain a representative sample of the population with a 95% confidence and an error of 5%, a sample size of 120 subjects was required. However, considering a potential low response rate of 30% in our population, the final sample size was increased to 350 subjects.
PACV translation into Arabic
For the purpose of this study, we translated the original PACV survey into the Arabic language using forward and backward method. First, a bilingual investigator (SA) individually translated the PACV survey into the Arabic version. Next, another bilingual investigator (IE), unaware of the original English version, performed a back translation into the English language. All investigators discussed the discrepancies resulting from the forward-backward translations and refined the Arabic version accordingly to maintain the meanings of the original survey. Moreover, the Arabic version was pretested on a random sample of 25 parents (not included in the final sample) to assess the clarity of questions before finalizing the Arabic-PACV version.
PACV description
The Arabic-PACV used in the current study (Supplementary Material) contains 15 items under 3 domains: behavior (items 1–2), safety and efficacy (items 7–10), and general attitude and trust (items 3–6 and 11–15). We also added demographic questions including parental age, parental educational level, marital status, nationality, relationship to child, number of children in the household and household income. As previously described, the PACV was scored by assigning a numeric score of 2 for non-demographic items answered with a hesitant response, a score of 1 for items answered with a response of “don’t know or not sure,” and a score of 0 for items answered with a non-hesitant response. PACV scores range from 0 to 100 and a non-hesitant parent was defined with a score <50 and a hesitant with a value ≥50. For converting the PACV raw score to the scale of 0 to100, we used a simple linear transformation that accounts for missing data similar to that used by the original PACV author.13
Data analysis
Data was analyzed using STATA 15 package (College Station, Texas, USA.). Internal consistency for the Arabic-PACV was evaluated using Cronbach’s alpha test. The univariate association between the hesitancy status with each of the explanatory variables was analyzed with Chi-square test for proportions and expressed as unadjusted odds ratio (OR) with 95% confidence intervals (ci). The variables significant in the univariate model with a P value < .1 were then fitted into a stepwise backward logistic regression model to test their association with hesitancy while adjusting for all the other variables. Only the variables with a P value <.05 were considered to be significantly associated with hesitancy and the results were expressed as adjusted OR with 95% ci.
Ethics consideration
Ethics approval was obtained from the Ambulatory Healthcare Services (AHS) – Human Research Ethics Committee at Abu Dhabi Health Services Company – SEHA.
Results
Participation and inclusion in the study
A total of 350 surveys were distributed (50 surveys to each of the 7 health-care centers), 300 were filled and returned (response rate, 85.7%), Figure 1. As this number exceeded the calculated sample size of 120, we then stopped further enrollment.
Figure 1.

Flowchart of parents attending Ambulatory Healthcare Services who were offered participation in the study
PACV: Parent Attitudes About Childhood Vaccines.
Participants sociodemographic characteristics
Table 1 demonstrates the sociodemographic characteristics of 300 recruited parents. The majority of participants were Emirati mothers (77%) in the age group (30–49 years). About half had attended university or higher education. Around one-quarter of parents (27%) had a monthly household income less than 10,000 Emirati dirhams (≈US$ 2,700).
Table 1.
Characteristics of the participants (N = 300)
| N | % | |
|---|---|---|
| Parent | ||
| Mother | 230 | 77 |
| Father | 69 | 23 |
| Health center | ||
| Rural | 83 | 28 |
| Urban | 217 | 72 |
| Age group (years) | ||
| < 18 | 9 | 3 |
| 18–29 | 60 | 20 |
| 30–39 | 133 | 45 |
| 40–49 | 86 | 29 |
| ≥ 50 | 9 | 3 |
| Marital status | ||
| Married | 266 | 94 |
| Widowed | 5 | 2 |
| Divorced | 12 | 4 |
| Nationality | ||
| Emirati | 225 | 77 |
| Others | 68 | 23 |
| Educational level | ||
| Illiterate | 2 | 1 |
| Less than high school | 34 | 11 |
| High school | 97 | 33 |
| University | 131 | 44 |
| Masters or PhD | 32 | 11 |
| Household income (Emirati dirhams*) | ||
| < 10,000 | 75 | 27 |
| 10,000–30,000 | 134 | 48 |
| 30,000–50,000 | 48 | 17 |
| >50,000 | 24 | 8 |
| Is this child your firstborn? Yes | 70 | 23 |
| Number of children in the household | ||
| 1 | 35 | 12 |
| 2 | 59 | 20 |
| 3 | 55 | 18 |
| ≥4 | 149 | 50 |
Total number for each characteristic may not add up to 300 because of missing values.
* 10,000 Emirati dirhams ≈ US$ 2,700.
Performance of Arabic-PACV and vaccine hesitancy in the studied population
The Cronbach alpha for the total Arabic-PACV scores was 0.79. Using the Arabic-PACV survey, only 36 parents (12%, 95% CI 8.5,16.2) were identified to be vaccine-hesitant (PACV score ≥50). This is consistent with the 10% self-reported prevalence of vaccine hesitancy in the survey (item 12).
Parental attitudes and concerns pertaining to vaccines
Forty-four (16%) of all 300 surveyed parents self-reported that they ever delayed their children’s vaccination and 6% of them had decided not to vaccinate their children, Table 2. Of the 36 vaccine-hesitant parents, 14 (40%) self-reported delaying their child receiving a shot versus 30 (11.5%) of those with no hesitancy (P < .001). Moreover, 10 (27.8%) of the parents with vaccine hesitancy had already decided at some point not to have their child get a shot versus 8 (3%) of those with no hesitancy (P < .001). Parent’s greatest concerns were mainly the vaccines side effects (35%), safety of vaccines (17% unsure and 28% concerned) and getting too many injections (28%), Figure 2 and Table 2.
Table 2.
Responses to individual PACV statements by 300 participants
| No. | Item | Response | N (%) |
|---|---|---|---|
| 1 | Have you ever delayed having your child get a shot (not including seasonal flu) for reasons other than illness or allergy? | Yes | 44 (16) |
| No | 235 (84) | ||
| Don’t know | |||
| 2 | Have you ever delayed having your child get a shot (not including seasonal flu) for reasons other than illness or allergy? | Yes | 18 (6) |
| No | 271 (94) | ||
| Don’t know | |||
| 3 | How sure are you that following the recommended shot schedule is a good idea for your child? From 0 (not at all sure) to 10 (completely sure) | 0–5 | 44 (15) |
| 8–10 | 234 (79) | ||
| 6–7 | 20 (6) | ||
| 4 | Children get more shots than are good for them. | Disagree | 131 (44) |
| Unsure | 84 (28) | ||
| Agree | 84 (28) | ||
| 5 | I believe that many of the illnesses that shots prevent are severe. | Disagree | 242 (81) |
| Unsure | 40 (13) | ||
| Agree | 18 (6) | ||
| 6 | It is better for my child to develop immunity by getting sick than to get a shot | Disagree | 146 (49) |
| Unsure | 59 (20) | ||
| Agree | 92 (31) | ||
| 7 | It is better for children to get fewer vaccines at the same time. | Disagree | 140 (47) |
| Unsure | 78 (26) | ||
| Agree | 81 (27) | ||
| 8 | How concerned are you that your child might have a serious side effect from a shot? | Not concerned | 160 (53) |
| Unsure | 33 (11) | ||
| Concerned | 106 (35) | ||
| 9 | How concerned are you that anyone of the childhood shots might not be safe? | Not concerned | 161 (53) |
| Unsure | 53 (17) | ||
| Concerned | 85 (28) | ||
| 10 | How concerned are you that a shot might not prevent the disease? | Not concerned | 162 (54) |
| Unsure | 81 (27) | ||
| Concerned | 56 (19) | ||
| 11 | If you had another infant today, would you want him/her to get all the recommended shots | Yes | 258 (87) |
| Don’t know | 23 (8) | ||
| No | 15 (5) | ||
| 12 | Overall, how hesitant about childhood shots would you consider yourself to be? | Not hesitant | 245 (82) |
| Unsure | 23 (8) | ||
| Hesitant | 29 (10) | ||
| 13 | I trust the information I receive about shots. | Agree | 251 (84) |
| Unsure | 37 (12) | ||
| Disagree | 9 (3) | ||
| 14 | I am able to openly discuss my concerns about shots with my child’s doctor. | Agree | 247)83) |
| Unsure | 38 (13) | ||
| Disagree | 12 (4) | ||
| 15 | All things considered; how much do you trust your child’s doctor? From 0 (no trust at all) to 10 (completely trust) | 8–10 | 216 (73) |
| 6–7 | 45 (15) | ||
| 0–5 | 34 (11) |
PACV: Parent Attitude about Childhood Vaccines. The answer “Do not know” in questions 1 and 2 is counted as missing data. The shaded answers reflect vaccine hesitancy. The total number for each characteristic may not add up to 300 because of missing values.
Figure 2.
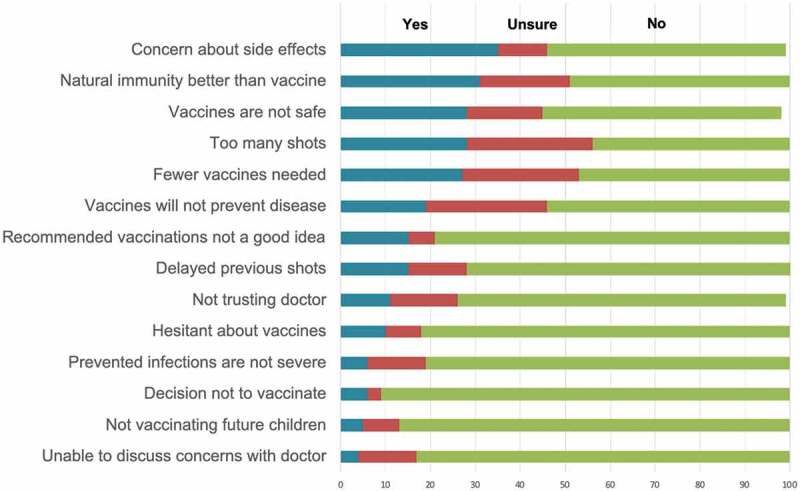
PACV factors associated with vaccine hesitancy (coded as Yes), by descending order of frequency (percentage)
Univariate and multivariate analysis of factors predicting vaccine hesitancy among parents
In the univariate analysis, fathers and divorced status were significantly more vaccine-hesitant (p < .05) than mothers or other listed marital statuses, while other sociodemographic factors such as age, educational level, household income, nationality, and first-born child status did not have any significant association with vaccine hesitancy. In the multivariate logistic regression model, only the divorced status remained significantly associated with hesitancy (P < .001), Table 3.
Table 3.
Associations between vaccine hesitancy and sociodemographic characteristics. Results expressed as number of respondents (percentage)
| Univariate analysis* |
Multivariate analysis¶ |
|||||
|---|---|---|---|---|---|---|
| Hesitant n = 36 (12%) |
Non hesitant n = 264 (88%) |
OR (95% ci) | P value | aOR (95% ci) | P value | |
| Parent | 0.3 (0.1, 0.6) | 0.001 | 0.2 (0.09, 0.76) | 0.01 | ||
| Mother | 20 (9) | 210 (91) | 0.3 | |||
| Father | 16 (23) | 53 (77) | Reference | |||
| Health Center | 0.7 (0.4, 1.8) | 0.2 | NA | NA | ||
| Rural | 11 (13) | 72 (87) | 0.8 | |||
| Urban | 25 (12) | 192 (88) | Reference | |||
| Age group (years) | 0.9 (0.6, 1.4) | 0.6 | NA | NA | ||
| < 18 | 1 (11) | 8 (89) | Reference | |||
| 18–29 | 9 (15) | 51 (85) | 1.4 | |||
| 30–39 | 13 (10) | 120 (90) | 0.8 | |||
| 40-49 | 12 (14) | 74 (86) | 1.3 | |||
| ≥ 50 | 0 (0) | 9 (199) | NA | |||
| Marital status | 3.0 (1.6, 5.4) | <0.001 | 15.6 (2.9, 82.6) | <0.001 | ||
| Married | 23 (8) | 243 (92) | Reference | |||
| Widowed | 0 (0) | 5 (100) | 1.0 | |||
| Divorced | 6 (50) | 6 (50) | 10.5 | |||
| Nationality | 0.5 (0.2, 1.4) | 0.2 | NA | NA | ||
| Emirati | 29 (13) | 196 (87) | 1.8 | |||
| Others | 5 (7) | 63 (93) | Reference | |||
| Educational level | 0.7 (0.5, 1.2) | 0.2 | NA | NA | ||
| Illiterate | 0 (0) | 2 (100) | NA | |||
| Less than high school | 5 (15) | 29 (85) | Reference | |||
| High school | 15 (15) | 82 (84) | 1.06 | |||
| University | 11 (8) | 120 (92) | 0.53 | |||
| Masters or PhD | 4 (12) | 28 (88) | 0.8 | |||
| Household income (Emirati dirhams*) | 1.3 (0.9, 1.9) | 0.1 | 1.5 (0.3, 8.5) | 0.7 | ||
| < 10,000 | 9 (12) | 66 (88) | Reference | |||
| 10,000–30,000 | 11 (8) | 123 (92) | 0.6 | |||
| 30,000–50,000 | 10 (21) | 38 (79) | 1.9 | |||
| >50,000 | 4 (12) | 20 (88) | 1.4 | |||
| This child your firstborn | 13 (19) | 57 (81) | 0.5 (0.2, 1.0) | 0.06 | 0.9 (0.2, 3.9) | 0.3 |
| Number of children in the household | 0.9 (0.8, 1.3) | 0.8 | NA | NA | ||
| 1 | 4 (11) | 31 (89) | Reference | |||
| 2 | 7 (12) | 52 (88) | 1.04 | |||
| 3 | 8 (15) | 47 (85) | 1.3 | |||
| >4 | 16 (11) | 133 (89) | 0.9 | |||
PACV: Parent Attitude about Childhood Vaccines; OR: odds ratio; aOR: adjusted odds ratio; *: Chi-squared test; Multivariate logistic regression; NA: not applicable.
Total number for each characteristic may not add up to 300 because of missing values.
Discussion
The Arabic-PACV has an overall Cronbach alpha score of 0.79 indicating a reliable internal consistency that is comparable with the original PACV and other translated versions.14,16,19
Using the Arabic-PACV, we identified that 12% of the studied UAE population are vaccine-hesitant. These findings are similar to other studies using the same tool form Kuala Lumpur, Malaysia (11.6%) and Erbil, Iraq (9.9%) and lower than those reported in USA (30.4%) and Italy (34.7%).6,16,18,19 Using an 11-item vaccine hesitancy scale, designed by the WHO Strategic Advisory Group of Experts (SAGE) on immunization, a recent study from Saudi Arabia reported that 20% of parents were hesitant to get their child vaccinated.20 The reported differences in the prevalence of vaccine hesitancy are likely related to the unique characteristics of the different studied populations, study settings (hospital vs. community) and the survey tool used.
Although 16% of parents in our studied population self-reported delaying their children’s vaccination and 6% decided not to vaccinate their children, neither the reasons for the delay or decision not to vaccinate, nor if those decisions were vaccine-specific are known. To overcome this limitation, Abd Halim et al. suggested to convert items 1 and 2 on the PACV survey into a numerical scale indicating the number of times vaccines have been delayed or refused and to provide space for parents to provide their reasons.19
A national survey involving more than 11,000 parents in the USA identified that parents who delayed and refused vaccines were more likely to have vaccine safety concerns and perceive fewer benefits associated with vaccines.21 Similarly, in this study, vaccine safety issues and getting too many shots were cited as parents’ top concerns. Vaccine providers must understand parents’ specific beliefs and concerns about vaccines and tailor counseling to the family from a sociocultural perspective.
In a study involving more than 7000 parents, around 80% of parents stated that their decision to vaccinate was positively influenced by their primary care provider.22 Another recent multi-center study involving 1820 pregnant women from 15 Italian cities revealed that women who had confidence in health-care professional information agreed more on mandatory vaccination than did the other women.23 Consistently, in the present study, 216 (73%) parents indicated almost complete trust in their child’s doctor. Therefore, training of health-care providers to effectively communicate immunization issues should be included in their teaching curriculum and throughout their continuous medical education.
In the univariate analysis, fathers and divorced status were found significantly associated with vaccine hesitancy. However, there were no associations with parent’s age, educational level, household income, nationality, and first-born child status. The NAVIDAD study in Italy showed that vaccine hesitancy is mainly present in higher-income and highly educated mothers older than 35 years.23 In contrast, a Malaysian study found that pregnant mothers expecting their first child and unemployed parents were more vaccine-hesitant.15 It is likely that the significant differences in demographic, social, cultural, religious, educational, economic, and environmental factors amongst countries account for any observed differences in underlying determinants of vaccine hesitancy.
In the multivariate analysis and following adjustment for all other variables, vaccine hesitancy was found to be associated with divorced status only. Similarly, Anokye et al. reported that being divorced (p = .048) had a significant and positive association with immunization incompletion among 280 caregivers/mothers in Koforidua, Ghana.24 In the UAE, divorce cases are rising up.25 In 2010, the divorce rate in Abu Dhabi was 0.9 per 1000 population.26 In 2017, Dubai Statistics Center reported an average divorce rate of 2.4 per 1,000 citizens at the age of marriage for UAE nationals residing in Dubai. This rate goes up to 3.9 cases per 1000 citizens when considering both UAE and non-UAE nationals.27 In a study involving 1742 divorced women in the UAE, health effects on children after divorce were apparent and involved sleep disorders, weight changes, depression, headaches, thumb sucking, stuttering, bed-wetting, bad language, and alcohol abuse.28 Our study is the first in UAE to report the association between divorced status and vaccine hesitancy. Taken together, society including health-care authorities and workers should support the family structure that has the best chance of generating healthy children.
In some European countries, mandatory vaccination policies were found associated with higher vaccination coverage.29 However, mandatory vaccination should not be the sole approach in addressing vaccine hesitancy. In the context of UAE and the adoption of mandatory vaccination policies, it would be valuable to consider a multiple approach method, which includes educational intervention and raising awareness as well as ensuring strong immunization programs. Parents should be advised to understand why the immunization of their children is so important. Additionally, the possibility of enforcing a law for mandatory vaccination could be considered.
This study has a few limitations. First, as with any self-administered survey, there is a risk of potential recall bias because participants may not accurately remember or truthfully report the information. Additionally, immunization records were not verified to corroborate the parental response. Furthermore, we approached a convenience sample of Arabic-speaking parents attending public primary health-care centers in Al Ain city and this may bias the results as most parents attending these centers are UAE national benefiting from a specific type of health insurance unavailable to others. As the study was undertaken in Al-Ain city, with different socioeconomic and educational backgrounds of its population when compared to other parts of the country, selection bias is possible and generalization beyond the study population cannot, therefore, be made. Future studies should involve community settings in different parts of the UAE such as Dubai and Abu Dhabi where the majority of the population are non-UAE nationals and with different health insurance schemes.
In conclusion, many parents in our community were concerned of the safety and side effects of vaccines. Targeted preventive and educational measures should be carried out to prevent the emerging and increasing trend of vaccine hesitancy in the country. More support is needed for vulnerable groups like divorced parents to improve compliance with vaccination schedule. Moreover, our findings support the use of the validated Arabic-PACV among parents in any Arabic-speaking country.
Supplementary Material
Acknowledgments
We thank clinic managers, physicians, and nurses at the participating Ambulatory Healthcare Services (AHS) centers for their support of the study. We are also grateful to Ms. Asma Al Ali for helping with data collection.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Authors’ contributions
ARA conceptualized and designed the study, coordinated data collection and drafted the manuscript. IE participated in the study design and manuscript preparation. SA carried out data collection, reviewed and revised the manuscript. RA participated in data collection, reviewed and revised the manuscript. MSH participated in the study design, reviewed and revised the manuscript. HN carried out data analysis and interpretation and participated in manuscript preparation. All authors approved the final manuscript.
Data availability
All data generated or analyzed in this study are included in the manuscript.
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/21645515.2020.1753439.
References
- 1.Ten threats to global health in 2019; n.d.. [accessed 2019 Dec 21]. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019.
- 2.Dubé E, Vivion M, MacDonald NE.. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev Vaccines. 2015;14:99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 3.Immunization coverage ; n.d.. [Accessed 2019 Dec 21]. https://www.who.int/news-room/fact-sheets/detail/immunization-coverage.
- 4.Fine P, Eames K, Heymann DL. “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52:911–16. doi: 10.1093/cid/cir007. [DOI] [PubMed] [Google Scholar]
- 5.MacDonald NE, SAGE Working Group on Vaccine Hesitancy . Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Opel DJ, Taylor JA, Zhou C, Catz S, Myaing M, Mangione-Smith R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatr. 2013;167:1065–71. doi: 10.1001/jamapediatrics.2013.2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Centre for Disease Prevention and Control . Catalogue of interventions addressing vaccine hesitancy. Stockholm: ECDC; 2017.
- 8.Marti M, de Cola M, MacDonald NE, Dumolard L, Duclos P. Assessments of global drivers of vaccine hesitancy in 2014-looking beyond safety concerns. PLoS One. 2017;12:e0172310. doi: 10.1371/journal.pone.0172310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Capanna A, Gervasi G, Ciabattini M, Volpe E, Spadea A, Sgricia S, Zaratti L, Franco E. Effect of mass media on influenza vaccine coverage in the season 2014/2015: a regional survey in Lazio, Italy. J Prev Med Hyg. 2015;56:E72–76. [PMC free article] [PubMed] [Google Scholar]
- 10.WHO World Health Organization: Immunization, Vaccines And Biologicals . Vaccine preventable diseases vaccines monitoring system 2019 global summary reference time series: BCG; n.d.. [Accessed 2019 Dec 21]. http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tscoveragebcg.html.
- 11.Communicable Diseases Bulletin ; n.d.. [Accessed 2019 Dec 21]. https://www.haad.ae/haad/tabid/1177/Default.aspx.
- 12.Elbarazi I, Raheel H, Cummings K, Loney T. A content analysis of Arabic and English Newspapers before, during, and after the human papillomavirus vaccination campaign in the United Arab emirates. Front Public Health. 2016;4:176. doi: 10.3389/fpubh.2016.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Opel DJ, Mangione-Smith R, Taylor JA, Korfiatis C, Wiese C, Catz S, Martin DP. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin. 2011;7(4):419–25. doi: 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29:6598–605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 15.Mohd Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35:2955–61. doi: 10.1016/j.vaccine.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Napolitano F, D’Alessandro A, Angelillo IF. Investigating Italian parents’ vaccine hesitancy: a cross-sectional survey. Hum Vaccin Immunother. 2018;14:1558–65. doi: 10.1080/21645515.2018.1463943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cunningham RM, Kerr GB, Orobio J, Munoz FM, Correa A, Villafranco N, Monterrey AC, Opel DJ, Boom JA. Development of a Spanish version of the parent attitudes about childhood vaccines survey. Hum Vaccin Immunother. 2019;15:1106–10. doi: 10.1080/21645515.2019.1578599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raof AM, Attitude P. Beliefs towards child vaccination : identifying vaccine hesitant groups in a family health center, Erbil City, Iraq. ME-JFM. 2018;16:17–26. doi: 10.5742/MEWFM.2018.93386. [DOI] [Google Scholar]
- 19.Abd Halim H, Abdul-Razak S, Md Yasin M, Isa MR. Validation study of the Parent Attitudes About Childhood Vaccines (PACV) questionnaire: the Malay version. Hum Vaccin Immunother. 2019:1–10. doi: 10.1080/21645515.2019.1674112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alsubaie SS, Gosadi IM, Alsaadi BM, Albacker NB, Bawazir MA, Bin-Daud N, Almanie W, Alsaadi M, Alzamil F. Vaccine hesitancy among Saudi parents and its determinants. Result from the WHO SAGE working group on vaccine hesitancy survey tool. Saudi Med J. 2019;40:1242–50. doi: 10.15537/smj.2019.12.24653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, Hibbs B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the health belief model. Public Health Rep. 2011;126(Suppl 2):135–46. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics. 2011;127(Suppl 1):S92–99. doi: 10.1542/peds.2010-1722N. [DOI] [PubMed] [Google Scholar]
- 23.Gualano MR, Bert F, Voglino G, Buttinelli E, D’Errico MM, De Waure C, Di Giovanni P, Fantini MP, Giuliani AR, Marranzano M, et al. Attitudes towards compulsory vaccination in Italy: results from the NAVIDAD multicentre study. Vaccine. 2018;36(23):3368–74. doi: 10.1016/j.vaccine.2018.04.029. [DOI] [PubMed] [Google Scholar]
- 24.Anokye R, Acheampong E, Budu-Ainooson A, Edusei AK, Okyere P, Dogbe J, Nadutey A. Socio-demographic determinants of childhood immunization incompletion in Koforidua, Ghana. BMC Res Notes. 2018;11(1):656. doi: 10.1186/s13104-018-3767-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al Gharaibeh F, Bromfield NF. An analysis of divorce cases in the United Arab Emirates: a rising trend. J Divorce Remarriage. 2012;53:436–52. doi: 10.1080/10502556.2012.682896. [DOI] [Google Scholar]
- 26.Marriage and divorce rates in the emirates of Abu Dhabi_116.pdf. Abu Dhabi: Statistics Centre; n.d.
- 27.Divorce cases stands at 2.4 per 1000 emiratis at the age of marriage in Dubai; n.d.. [Accessed 2019 Dec 21]. https://www.dsc.gov.ae/en-us/DSC-News/Pages/Divorce-Cases-Stands-at-2.4-Per-1000-Emiratis-at-the-Age-of-Marriage-in-Dubai.aspx.
- 28.Al Gharaibeh FM. The effects of divorce on children: mothers’ perspectives in UAE. J Divorce Remarriage. 2015;56:347–68. doi: 10.1080/10502556.2015.1046800. [DOI] [Google Scholar]
- 29.Vaz OM, Ellingson MK, Weiss P, Jenness SM, Bardají A, Bednarczyk RA, Omer SB. Mandatory vaccination in Europe. Pediatrics. 2020;145:e20190620. doi: 10.1542/peds.2019-0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Ten threats to global health in 2019; n.d.. [accessed 2019 Dec 21]. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019.
- Immunization coverage ; n.d.. [Accessed 2019 Dec 21]. https://www.who.int/news-room/fact-sheets/detail/immunization-coverage.
- WHO World Health Organization: Immunization, Vaccines And Biologicals . Vaccine preventable diseases vaccines monitoring system 2019 global summary reference time series: BCG; n.d.. [Accessed 2019 Dec 21]. http://apps.who.int/immunization_monitoring/globalsummary/timeseries/tscoveragebcg.html.
- Communicable Diseases Bulletin ; n.d.. [Accessed 2019 Dec 21]. https://www.haad.ae/haad/tabid/1177/Default.aspx.
- Divorce cases stands at 2.4 per 1000 emiratis at the age of marriage in Dubai; n.d.. [Accessed 2019 Dec 21]. https://www.dsc.gov.ae/en-us/DSC-News/Pages/Divorce-Cases-Stands-at-2.4-Per-1000-Emiratis-at-the-Age-of-Marriage-in-Dubai.aspx.
Supplementary Materials
Data Availability Statement
All data generated or analyzed in this study are included in the manuscript.


