Abstract
BACKGROUND:
A large proportion of noncommunicable diseases (NCDs) can be prevented by reducing unhealthy nutrition, inadequate physical activity, smoking, and alcohol consumption. The high burden of NCDs underlines the need for a greater understanding of the causes of these risk factors. This paper aims to identify factors affecting smoking, alcohol consumption, unhealthy nutrition, and inadequate physical activity in current and future times.
MATERIALS AND METHODS:
A scoping review was conducted in Iran University of Medical Sciences, Tehran, Iran, in 2020 to identify factors affecting smoking, alcohol consumption, unhealthy nutrition, and inadequate physical activity. The review was guided by the five-step Arksey and O'Malley model. A deductive qualitative content analysis was employed to identify the factors synthesized through descriptive and narrative synthesis. The search was conducted in English without date restrictions up to January 2020.
RESULTS:
We identified 1437 studies through database search and other sources and finally included 72 studies in the review. The content analysis of the data led to the identification of 27 factors affecting smoking, alcohol consumption, nutrition, and physical activity. The factors categorized into social, technological, environmental, economic, political, and values factors.
CONCLUSION:
Political and economic factors have a significant effect on all risk factors, and it is necessary to take comprehensive measures to improve these factors. Technological factors have a greater impact on healthy nutrition. Physical activity is more affected by environmental factors than other risk factors. However, smoking and alcohol consumption are more influenced by social factors and individual attitudes.
Keywords: Alcohol, noncommunicable diseases, nutrition, physical activity, risk factors, smoking
Introduction
Noncommunicable diseases (NCDs) occur as a result of the interaction of a set of risk factors including behavioral risk factors, metabolic risk factors, and environmental risk factors. A large proportion of NCDs can be prevented by reducing the main risk factors, namely, unhealthy nutrition, inadequate physical activity, smoking, and alcohol consumption.[1] Evidence shows that low consumption of fruits and vegetables causes 16 million (1%) disability-adjusted life-years and 1.7 million (2.8%) deaths worldwide, while adequate consumption can reduce the risk of cardiovascular disease, diabetes, and some cancers. Excessive standard salt intake is an important determinant of stroke, ischemic heart disease, and gastric cancer. High consumption of saturated fats and transfatty acids also have a great impact on NCDs and their mortality. Disease burden and mortality attributable to insufficient physical activity in ischemic heart disease are above 9%, and regular physical activity can reduce the risk of disease. Direct smoking or exposure to smoke kills approximately 6 million people a year. The burden of disease attributed to smoking in diabetes, lung cancer, bladder cancer, ischemic heart disease, and chronic obstructive pulmonary disease in the world is 15%, 63%, 36%, 28%, and 40%, respectively.[2] Alcohol consumption is the cause of death of 2.3 million people in the world, half of which are due to NCDs including cancer, cardiovascular disease, and liver cirrhosis.[2,3]
The high burden of NCDs underlines the need for a greater understanding of the causes of risk factors. Health-promoting behaviors and a healthy lifestyle are affected by various factors including social, economic, environmental, and policy factors. Socioeconomic status can affect the health by multiple mechanisms such as promoting a lifestyle, increasing access to health care, and enhancing the living environment.[4] People with low socioeconomic status have worse access to health care and are less likely to have healthy lifestyle habits such as healthy nutrition and sufficient physical activity.[5] Hence, the various social and economic policies are needed to improve the lifestyle and the living conditions. Successful adoption of these policies requires economic development and political commitment.[4] Political commitment and political leadership at the highest level are necessary to facilitate the implementation of priority interventions.[6] In addition to the above factors, environmental factors such as urban planning, transportation systems, residential density, and access to recreation facilities are also influencing behavior risk factors, particularly physical inactivity.[7]
Studies were conducted to determine factors affecting smoking, alcohol consumption, healthy nutrition, or physical activity. However, most studies focus on one group of factors (social, economic, environment, or policy), one age or sex group, or one of the risk factors. It is important to identify the causes of all behavioral risk factors, because of the interrelationship between risk factors and the necessity of integrated interventions. In some studies such as those by Reisi et al.,[8] Rae et al.,[9] and Momenabadi et al.,[10] factors affecting hookah smoking trend, smoking cessation, and smoking consumption in groups such as students and patients have been considered. Factors affecting nutrition and physical activity have also been studied in some studies such as those conducted by Ball et al.,[11] Booth et al.,[12] and Haase et al.[13] In these studies, one of the social, economic, and environmental factors have been emphasized. However, there is no comprehensive study identifying all factors impacting on behavioral risk factors. For this, we conducted a scoping review to identify all types of factors (including social, technological, economic, environmental, political, and value factors) affecting smoking, alcohol consumption, healthy nutrition, and physical activity, both in current and future times.
Materials and Methods
Study design and setting
A scoping review was conducted in Iran University of Medical Sciences, Tehran, Iran in 2020 to identify factors affecting smoking, alcohol consumption, healthy nutrition, and physical activity. The review was guided by the five-step Arksey and O'Malley model.[14] The review process is reported according to PRISMA Extension for Scoping Reviews (PRISMA-Scar).[15]
Study participants and sampling
Studies were included that examined social, economic, environmental, technological, political, and value factors affecting one or more risk factors. We excluded studies that investigated clinical characteristics of NCDs patients, service provision for the patients, and the prevalence of risk factors or diseases. We searched for English-language studies without date restrictions up to January 2020.
Electronic searches were conducted to identify related studies in PubMed, Scopus, Embase, and web of science. The search was performed through titles, abstracts, and keywords using a combination of keywords such as “smok*,” “tobacco,” “alcohol,” “nutrition,” “diet,” “food,” “Exercises,” “Physical Activity,” “effect,” “driver,” “cause,” and “driving forces.” In addition, Google Scholar and Google searches, Hand searching relevant journals, and scanning of references of retrieved articles were also conducted. The search strategies used to search the PubMed, Scopus, Embase, and web of science databases are presented in Table 1.
Table 1.
Search strategy of databases
| Database | Search strategy | Search results |
|---|---|---|
| Web of sciences | Title: (alcohol or smoking or tobacco or “physical activit” or exercise* or “physical exercise” or diet or nutrition) and title: (trend or driver or factor or “driving force”) and topic: (“noncommunicable disease” or “chronic disease” or “noninfectious disease”) | 124 |
| Scopus | Title (alcohol or smoking or tobacco or “physical activit” or exercise* or “physical exercise” or diet or nutrition) and title (trend or driver or factor or “driving force”) and title-abs-key (“noncommunicable disease” or “chronic disease” or “noninfectious disease”) | 434 |
| Embase | (Alcohol: Ti or smoking: Ti or tobacco: Ti or “physical activit”: ti or exercise*:ti or “physical exercise”: ti or diet: ti or nutrition: ti) and (trend: ab, ti or driver: ab, ti or factor: ab, ti or “driving force”: ab, ti) and (“noncommunicable disease”: ab, ti or “chronic disease”: ab, ti or “noninfectious disease”: ab, ti) | 385 |
| PubMed | ((((((alcohol[title] or smok*[title] or tobacco[title] or physical activity[title] or exercise*[title] or physical exercise*[title] or diet*[title] or nutrition[title]))) and (((trend*[title] or driver*[title] or factor*[title] or driving forc*[title]))) and ((((“non*communicable disease*”[title/abstract] or “chronic disease*” [title/abstract] or “non*infectious disease*”[title/abstract]))) | 482 |
Following the search, titles and abstracts of identified studies were independently examined by two of the authors, and then full-text articles were reviewed to determine eligibility. Any disagreement between reviewers on whether to include or exclude a study were resolved through discussion.
Data collection tool and technique
The content of studies including introduction, results, and discussion sections was coded using manifest content analysis,[16] and key information was extracted. The data extraction form contained the following items: author, year, study design, name of risk factor (smoking, alcohol consumption, unhealthy nutrition, and physical inactivity), and type of factors affecting risk factors.
A deductive qualitative content analysis was employed to explore factors affecting behavior risk factors of NCDs. For this, a categorization matrix was developed based on STEEPV approach which is an acronym for social, technological, environmental, economic, political, and values. Social factors are related to attitudes and beliefs of people in society, behavioral patterns, demographic characteristics, social relationships, level of the education, and so on. Technology refers to innovations such as those in the field of biotechnology, internet and communication, transportation, and intellectual property issue. Economic factors refer to domestic and foreign economics, tax changes, employment and unemployment, economic growth, etc., Environmental factors are related to the environment, urban spaces, the characteristics of the living environment, etc., Political and legal factors are related to leadership and governance, trade policies, institutions and legislative processes, regulations, and so on. Value factors also refer to values of people in society.[17]
Ethical consideration
The ethical code of the study was IR.IUMS.REC.1397.1105.
Results
In total, 1424 studies were identified through the database search, and 13 through other sources. After removing duplicates, the titles, and abstracts of 1216 studies were examined in detail. One thousand and eighty-nine of these studies were excluded due to the inclusion criteria. The remaining 127 studies were considered, and their reference lists were also examined. Seventy-two studies were finally included in the review. The study selection process is detailed schematically in Figure 1.
Figure 1.
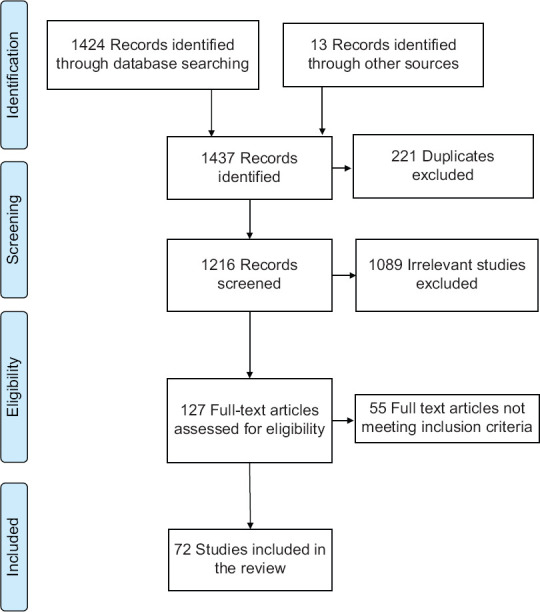
PRISMA flow diagram representing the study selection process
We identified 27 factors affecting smoking, alcohol consumption, nutrition and physical activity, and categorized them based on STEEPV approach. These factors include eight social factors, five technological factors, four economic factors, six environmental factors, three political factors, and one value factor. The factors are presented in Table 2.
Table 2.
Factors affecting behavioral risk factors of noncommunicable diseases
| Affecting factors | Risk factor | |||
|---|---|---|---|---|
|
| ||||
| Tobacco | Alcohol | Unhealthy nutrition | Physical inactivity | |
| Social | ||||
| Acculturation | * | * | * | * |
| Urbanization | * | * | * | * |
| Social capital | * | * | * | * |
| Family | * | * | * | * |
| Citizen empowerment | * | * | * | * |
| Demographic changes | * | |||
| Neighborhood safety | * | |||
| Media | * | * | * | * |
| Technological | ||||
| Food chain technology | * | |||
| Behaviour monitoring technologies | * | * | * | * |
| Behaviour change technologies | * | * | * | * |
| Electronic health record | * | * | * | * |
| Medical technology | * | * | * | |
| Economic | ||||
| Globalization | * | * | * | |
| Industries development | * | * | ||
| Economic development | * | * | * | * |
| Healthy food market | * | |||
| Environmental | ||||
| Interior design of work spaces, schools and houses | * | * | * | * |
| Transport systems | * | |||
| Climate changes | * | * | ||
| Traffic and air pollution | * | |||
| Natural disasters | * | * | ||
| Built environment | * | * | * | * |
| Policy and political | ||||
| Political commitment | * | * | * | * |
| The war | * | * | * | * |
| Political ideology | * | * | ||
| Values | ||||
| Individual attitudes | * | * | * | * |
| *affected risk factor | ||||
Social factors
Identified social factors include acculturation, urbanization, social capital, family, citizen empowerment, demographic change, neighborhood safety, and media. Urbanization and rising slum population are global health issues and affect people's health behaviors. Urban development reduces available agricultural land and energy consumption, resulting in a reduction in the supply of local food products.[18] Urbanization, on the other hand, increases access to health care and education, which have positive effects on obesity control. The development of urbanization has led to an increase in leisure time sedentary behavior such as watching TV, playing computer games, and using the internet instead of physical activity.[19,20,21,22] Social capital has two structural and cognitive dimensions and through various mechanisms such as providing information, influencing, social credibility, and strengthening the sense of identity influences on health behaviors.[22,23,24,25] The family factor refers to the structure, interactions, and values of the family, parents’ behaviors, maternal employment, and gender role change and parents education.[22,26,27] Citizens’ empowerment includes cognitive and behavioral dimensions (knowledge, attitude, and practice) and refers to the opportunities and capabilities of individuals to change individual behaviors.[22,28] Neighborhood safety is another social factor that specifically affect physical activity.[29,30,31,32] The influence of the media on behavioral risk factors is through its role in informing and advertising.[22,33,34,35]
Technological factors
Food chain technology, behavior monitoring technologies, behavior change technologies, electronic health records, and medical technologies are technological factors affecting behavioral risk factors. Behavior monitoring technologies and behavior change technologies refer to information and communication technologies such as smartphones laptops, iPods, and Internet, entertainment technologies, and software programs for monitoring risk factors.[36,37,38]
Economic factors
Globalization and international trade in food, expansion of tobacco and alcohol trade, and free flow of information can be effective in behavioral risk factors. Implementing free trade and market-oriented agricultural policies will change the food supply and have a direct impact on the obesity epidemic.[19,20,22,39] Factors related to economic development such as unemployment rate, the active presence of women in social spheres, household income, fair distribution of income and access to education, directly and indirectly, affect smoking, alcohol consumption, nutrition, and physical activity.[22,40,41,42,43,44] Healthy food market as a valuable setting ensures food safety, nutritional status, and environmental health.[45]
Environmental factors
Environmental factors include interior design, transportation system, climate change, natural disasters such as floods, traffic and air pollution, and built environment. The interior design of workspaces, schools, houses, and public places such as prisons and sanatoriums play a major role in physical activity, healthy eating, and even less exposure to secondhand smoke.[22,35] The transportation system refers to the physical infrastructure and services such as availability of sidewalks and biking infrastructure and affects physical activity. Built environment refers to human-made infrastructure such as hiking and cycling routes designed to support human activities.[29,32,46]
Political factors
Political factors include political commitment to health promotion, political ideology, and war. The government's political commitment refers to the purposeful and sustained actions of the actors to achieve the goals of reducing or eliminating the causes of an issue and includes mobilizing stakeholders and political institutions, adopting policies, allocating resources, and coordinating responses until the results are guaranteed and the goals achieved.[47,48,49]
Values
Individuals’ attitudes affect healthy behaviors and include social acceptance of the diet, physical activity, smoking and alcohol, belief in the effect of behavioral risk factors on NCDs, and people's sense of personal responsibility for their health.[50,51,52,53]
Discussion
Based on our results, eight social factors, five technological factors, four economic factors, six environmental factors, three political factors, and one value factor have been identified that impact on one or more risk factors and expected to affect them in future. Environmental factors such as demographic changes, neighborhood safety, transport systems, traffic and air pollution, climate changes, and natural disasters often focus on nutrition and physical activity. Study by Ball et al. shows similar results. On the basis of this study, environmental factors such as access to fast food restaurants, family environment, and neighborhood environments are important determinants of nutrition and physical activity behaviors among adults and children.[11] The results of the study by Seefeldt conducted in ethnic minorities revealed that crime rate, safety concerns, and culturally inappropriate activities influence significantly on levels of physical activity in adults,[54] while in our study, cultural factors and crime rate received less attention than other factors. This difference may be due to the population differences, because their study was conducted in ethnic minorities with low socioeconomic status.
Among social factors, family and social capital received more attention which this finding is consistent with the studies by Moxley et al.,[55] Åslund and Nilsson,[56] and Karimian et al.[57] These studies focused on the importance of family solidarity and social capital in promoting nutrition and physical activity and preventing smoking and alcohol consumption.
Economic development is a main driver for behavioral risk factors, which has been emphasized in various studies. The results of consistent studies show that economic development at micro and macro levels may impact on smoking, alcohol consumption, unhealthy nutrition, and physical inactivity.[13,58,59]
Economic development and higher incomes can improve health status at the individual and country levels in a variety of ways including strengthening health systems and improving nutrition.[60] Evidence shows that well-being and favorable socioeconomic status at the individual level such as high income, education, and proper employment, play a key role in promoting health.[61] However, there is conflicting evidence about the impact of economic growth on population health at the macro level. A case study of China shows that health promotion has been more affected by public health media campaigns and public access to primary care than by market reforms and economic growth. China has faced new challenges in reducing health inequalities and promoting population health, despite significant economic development over the past 40 years.[62] Increasing income at the individual level and economic growth at the macro level can lead to nutritional transitions and changes in food consumption patterns. Evidence shows that property ownership, high income, access to health care, agricultural development, and women's education are important determinants of nutritional status.[61] In 2015, Burggraf et al. showed that rising incomes in Russia and China over the past few years have reduced demand for carbohydrates and increased demand for meat, fruits, and vegetables. Although these changes have led to a reduction in malnutrition in these countries, chronic nutrition-related diseases are a major health problem in Russia and China. Price elasticity for oils and fats is low, especially in China, and raising taxes has not had a positive effect on reducing consumption.[63] Similar studies show that economic development can have a positive impact on eliminating malnutrition, preventing disease, and improving people's health.[64,65] The results of a study by Allen et al. show that countries that have sufficient investment in health care and education are also investing in NCD prevention policies. Although financial and human resources help implement NCD policies, implementing these policies is not necessarily costly.[66] Although economic development has a great impact on promoting healthy behaviors and controlling behavioral risk factors, some countries, including China and African countries whose economies are highly dependent on the tobacco industry, are at a crossroads between economic growth and health promotion. The governments of these countries are encouraged to develop the tobacco industry by arguing that the tobacco industry has a positive impact on increasing tax revenues and expanding employment and income. Tobacco industry stakeholders in the areas of tobacco agriculture, tobacco production, and the tobacco trade, by influencing the policymaking process, prevent the successful implementation of tobacco control policies.[67,68] Conflict of interest is one of the most effective factors in behavior risk factors. The alcohol industry and transnational corporations influence policymakers’ decisions to control alcohol consumption with economic arguments including increased tax revenues and job creation for individuals.[69] The results of a study by Collins et al. in the United Kingdom show that people's social status, education level, and housing status have a great impact on alcohol consumption, but people's income and employment are not significant determinants of alcohol consumption.[70] Although economic development and urbanization are important for improving living standards, they may increase the risk of NCDs by changing lifestyles and reducing mobility. The results of numerous studies in different countries, including Argentina and South Africa, indicate that income and level of education as important indicators of economic development have a significant relationship with the level of physical activity.[71,72] Physical activity refers to moderate to vigorous activity during working hours, leisure, and commuting. Evidence suggests that physical activity is significantly associated with income, education, and urbanization. Findings from the study by Bauman et al. showed that, in Asian countries such as China and the Philippines, the physical activity of high-income and educated people in leisure time is higher than low-income and low-educated people, but their physical activity is low during working hours and travel times.[73] Various evidence indicates the positive effect of social capital on the general health status and control of behavioral risk factors. The results of the studies of Berry and Welsh and Johnson et al. show the positive effect of structural and cognitive dimensions of social capital including social cohesion and community participation on the health status of individuals.[74,75] The results of the studies by Davison et al. and Prins et al. also show that social capital and the support of parents and neighbors play an important role in promoting physical activity.[76,77] The results of the study by Chen et al. also show that social capital and the support of friends and family members promote health literacy and thus increase physical activity and improve the nutritional status of individuals.[78,79] Evidence shows that membership in friendship groups and relationships with neighbors increases alcohol consumption, but the cognitive dimension of social capital and the widespread support of friends and family members prevent adolescents and young people from consuming alcohol.[56,80]
Addressing NCDs risk factors requires the political commitment of the government and the provision of sufficient resources.[62,81] Cuba's experience shows that political commitment to health promotion and policy actions play a significant role in promoting public health.[48] Experiences of various countries including Malawi, Nigeria, and Uganda, also show that the political commitment of the government and the political participation of managers in improving nutrition are the most important factors for the successful implementation of nutrition policies. In this case, nutrition is crucial to national development.[82] The results of Murphy et al.'s study show that some countries are facing challenges despite cross-sectoral coordination in legislation and the creation of appropriate social and physical environments for proper nutrition and adequate physical activity.[83] According to a study by Goins et al., low political commitment is the most important factor for inadequate physical activity. The results of this study show that promoting political commitment can play an important role in promoting physical activity by removing the limitations of human resources in the field of public health and coordinating the sectors involved in promoting physical activity, including the transportation sector.[84] Creating and strengthening political commitment to improve nutrition is not an easy task and will be achieved over a long period through strategic measures. Implementation of these measures requires a coherent network of stakeholders with sufficient resources and strong leadership.[46,85] The results of the study by Hawkins and McCambridge show that the political commitment of the highest levels of the country is required to implement controversial policies to control alcohol consumption, even if there is strong scientific evidence and support.[86]
Individual attitudes refer to social acceptance of behavioral risk factors, belief in the impact of behavioral risk factors on NCDs, and a sense of personal responsibility for one's own health and that of others. Theoretical models and research findings show that the attitudes, values, and self-confidence of individuals play an important role in promoting people's health behaviors.[87] Eating habits and food choices are one of the health behaviors that are strongly influenced by individual attitudes. The results of the study by Acheampong and Haldeman show that people's beliefs and attitudes toward eating healthy foods and their role in promoting healthy nutrition have a positive effect on diet quality and body mass index.[88] Evidence shows that students in developed countries such as northwestern Europe, the United States, and Japan have positive beliefs about the impact of physical activity on health, and are more physically active in their leisure time than other students.[13]
People's attitudes affect people's behaviors not only at the individual level but also at the social level. The results of the study of Martin-Moreno et al. show that community attitudes and social acceptance are determinants of chronic diseases.[89] Various evidence shows that social acceptance has a great impact on alcohol consumption and smoking. In African countries, due to the importance of social acceptance of alcohol consumption, a lot of money is spent on its specific marketing to increase the social acceptance of alcohol consumption and add new consumers, especially women, in the alcohol market. In general, it can be said that people's attitudes and beliefs at the individual and social level play an important role in people's health behaviors, and people's choices are strongly influenced by social environments and cultural changes due to globalization.[69]
Limitation and recommendation
The main limitation of this study is that it did not analyze the factors from the perspective of the policy and decision-makers and experts and only focused on English studies. This calls for studies to investigate experts’ perspectives on the factors.
Conclusion
Political and economic factors have a significant effect on all risk factors, and it is necessary to take comprehensive measures to improve these factors. Technological factors have a greater impact on healthy nutrition. Physical activity is more affected by environmental factors than other risk factors. However, smoking and alcohol consumption are more influenced by social factors and individual attitudes. Therefore, new policies, strong leadership, and active participation of the public are needed to control the risk factors for NCDs.
Financial support and sponsorship
This study was financially supported by Iran University of Medical Sciences, Tehran, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was a part of a PhD thesis supported by Iran University of Medical Sciences, (Grant no: IUMS/SHMIS_97-4-37-14385).
References
- 1.Dobe M. Health promotion for prevention and control of non-communicable diseases: Unfinished agenda. Indian J Public Health. 2012;56:180–6. doi: 10.4103/0019-557X.104199. [DOI] [PubMed] [Google Scholar]
- 2.Institute for Health Metrics and Evaluation. Global Burden of Disease (GBD) 2017. [Last accessed on 2020-09-30]. Available from: https://vizhub.healthdata.org/gbd-compare/
- 3.Capizzi S, De Waure C, Boccia S. Global burden and health trends of non-communicable diseases. A systematic review of key issues in public health. Springer International Publishing Switzerland. 2015:19–32. doi: 10.1007/978-3-319-13620-2_3. [Google Scholar]
- 4.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: How interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14(Suppl):S8–17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Di Cesare M, Khang YH, Asaria P, Blakely T, Cowan MJ, Farzadfar F, et al. Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381:585–97. doi: 10.1016/S0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- 6.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377:1438–47. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 7.Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW, et al. Correlates of physical activity: Why are some people physically active and others not? Lancet. 2012;380:258–71. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 8.Reisi M, Javadzade SH, Shahnazi H, Sharifirad G, Charkazi A, Moodi M. Factors affecting cigarette smoking based on health-belief model structures in pre-university students in Isfahan, Iran. J Educ Health Promot. 2014;3:23. doi: 10.4103/2277-9531.127614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rae J, Pettey D, Aubry T, Stol J. Factors affecting smoking cessation efforts of people with severe mental illness: A qualitative study. J Dual Diagn. 2015;11:42–9. doi: 10.1080/15504263.2014.992096. [DOI] [PubMed] [Google Scholar]
- 10.Momenabadi V, Hossein Kaveh M, PhD, Hashemi SY, Borhaninejad VR. Factors affecting hookah smoking trend in the society: A review article. Addict Health. 2016;8:123–35. [PMC free article] [PubMed] [Google Scholar]
- 11.Ball K, Timperio AF, Crawford DA. Understanding environmental influences on nutrition and physical activity behaviors: Where should we look and what should we count? Int J Behav Nutr Phys Act. 2006;3:33. doi: 10.1186/1479-5868-3-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Booth SL, Sallis JF, Ritenbaugh C, Hill JO, Birch LL, Frank LD, et al. Environmental and societal factors affect food choice and physical activity: Rationale, influences, and leverage points. Nutr Rev. 2001;59:S21–36. doi: 10.1111/j.1753-4887.2001.tb06983.x. [DOI] [PubMed] [Google Scholar]
- 13.Haase A, Steptoe A, Sallis JF, Wardle J. Leisure-time physical activity in university students from 23 countries: Associations with health beliefs, risk awareness, and national economic development. Prev Med. 2004;39:182–90. doi: 10.1016/j.ypmed.2004.01.028. [DOI] [PubMed] [Google Scholar]
- 14.Arksey H, O'Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 15.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 16.Bengtsson M. How to plan and perform a qualitative study using content analysis. Nurs Plus Open. 2016;2:8–14. [Google Scholar]
- 17.Kyler J. Assessing your external environment: STEEP analysis. Competia. 2003;33:1. [Google Scholar]
- 18.Satterthwaite D, McGranahan G, Tacoli C. Urbanization and its implications for food and farming. Philos Trans R Soc B Biol Sci. 2010;365:2809–20. doi: 10.1098/rstb.2010.0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malik VS, Willett WC, Hu FB. Global obesity: Trends, risk factors and policy implications. Nat Rev Endocrinol. 2013;9:13–27. doi: 10.1038/nrendo.2012.199. [DOI] [PubMed] [Google Scholar]
- 20.Sahal Estimé M, Lutz B, Strobel F. Trade as a structural driver of dietary risk factors for noncommunicable diseases in the Pacific: An analysis of household income and expenditure survey data. Global Health. 2014;10:48. doi: 10.1186/1744-8603-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blouin C, Chopra M, van der Hoeven R. Trade and social determinants of health. Lancet. 2009;373:502–7. doi: 10.1016/S0140-6736(08)61777-8. [DOI] [PubMed] [Google Scholar]
- 22.Wepner B, Giesecke S. Drivers, trends and scenarios for the future of health in Europe. Impressions from the FRESHER project. Eur J Futures Res. 2018;6:2. [Google Scholar]
- 23.Derose KP, Varda DM. Social capital and health care access: A systematic review. Med Care Res Rev. 2009;66:272–306. doi: 10.1177/1077558708330428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coll-Planas L, Nyqvist F, Puig T, Urrútia G, Solà I, Monteserín R. Social capital interventions targeting older people and their impact on health: A systematic review. J Epidemiol Community Health. 2017;71:663–72. doi: 10.1136/jech-2016-208131. [DOI] [PubMed] [Google Scholar]
- 25.Treiber FA, Baranowski T, Braden DS, Strong WB, Levy M, Knox W. Social support for exercise: Relationship to physical activity in young adults. Prev Med. 1991;20:737–50. doi: 10.1016/0091-7435(91)90068-f. [DOI] [PubMed] [Google Scholar]
- 26.Yelick A. The effects of family structure on consumption and exercise patterns for adolescent youth. Child Adolesc Soc Work J. 2017;34:381–95. [Google Scholar]
- 27.Bowden JA, Delfabbro P, Room R, Miller CL, Wilson C. Prevalence, perceptions and predictors of alcohol consumption and abstinence among South Australian school students: A cross-sectional analysis. BMC Public Health. 2017;17:549. doi: 10.1186/s12889-017-4475-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rogacheva A, Laatikainen T, Patja K, Paavola M, Tossavainen K, Vartiainen E. Smoking and related factors of the social environment among adolescents in the Republic of Karelia, Russia in 1995 and 2004. Eur J Public Health. 2008;18:630–6. doi: 10.1093/eurpub/ckn083. [DOI] [PubMed] [Google Scholar]
- 29.Umstattd Meyer MR, Sharkey JR, Patterson MS, Dean WR. Understanding contextual barriers, supports, and opportunities for physical activity among Mexican-origin children in Texas border colonias: A descriptive study. BMC Public Health. 2013;13:14. doi: 10.1186/1471-2458-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Story M, Giles-Corti B, Yaroch AL, Cummins S, Frank LD, Huang TT, et al. Work group IV: Future directions for measures of the food and physical activity environments. Am J Prev Med. 2009;36:S182–8. doi: 10.1016/j.amepre.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Ishii K, Shibata A, Oka K. Environmental, psychological, and social influences on physical activity among Japanese adults: Structural equation modeling analysis. Int J Behav Nutr Phys Act. 2010;7:61. doi: 10.1186/1479-5868-7-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adlakha D, Hipp AJ, Marx C, Yang L, Tabak R, Dodson EA, et al. Home and workplace built environment supports for physical activity. Am J Prev Med. 2015;48:104–7. doi: 10.1016/j.amepre.2014.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wulff H, Wagner P. Media use and physical activity behaviour of adolescent participants in obesity therapy: Impact analysis of selected socio-demographic factors. Obes Facts. 2018;11:307–17. doi: 10.1159/000490178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neiner JA, Howze EH, Greaney ML. Using scenario planning in public health: Anticipating alternative futures. Health Promot Pract. 2004;5:69–79. doi: 10.1177/1524839903257692. [DOI] [PubMed] [Google Scholar]
- 35.Foresight Programme of the Office of Science and Technology. United Kingdom: Trends and drivers of obesity: A literature review for the Foresight project on obesity. 2007, Foresight Programme of the Office of Science and Technology. Foresight Programme of the Office of Science and Technology. [Google Scholar]
- 36.Consortium FCE. Brussels: European Commission; 2013. Scoping Study: Delivering on EU Food Safety and Nutrition in 2050 – Scenarios of Future Change and Policy Responses. [Google Scholar]
- 37.Von Ah D, Ebert S, Ngamvitroj A, Park N, Kang DH. Factors related to cigarette smoking initiation and use among college students. Tob Induc Dis. 2005;3:27–40. doi: 10.1186/1617-9625-3-1-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tagliente I, Solvoll T, Trieste L, De Cecco CN, Murgia F, Bella S. Which indicators for measuring the daily physical activity? An overview on the challenges and technology limits for Telehealth applications. Technol Health Care. 2016;24:665–72. doi: 10.3233/THC-161216. [DOI] [PubMed] [Google Scholar]
- 39.Evans M, Sinclair RC, Fusimalohi C, Liava'a V. Globalization, diet, and health: An example from Tonga. Bull World Health Organ. 2001;79:856–62. [PMC free article] [PubMed] [Google Scholar]
- 40.Kant AK, Graubard BI. Family income and education were related with 30-year time trends in dietary and meal behaviors of American children and adolescents. J Nutr. 2013;143:690–700. doi: 10.3945/jn.112.165258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McInnes MM, Shinogle JA. Economic Aspects of Obesity. National Bureau of Economic Research: University of Chicago Press; 2011. Physical activity: Economic and policy factors; pp. 249–82. [Google Scholar]
- 42.Humphreys BR, Ruseski JE. Unpublished Working Paper Series. International Association of Sports Economists; North American Association of Sports Economists; 2006. Economic determinants of participation in physical activity and sport; pp. 1–25. [Google Scholar]
- 43.Georgiadou C, Lavdaniti M, Psychogiou M, Tzenalis A, Sgantzos M, Sapountzi-Krepia D. Factors affecting the decision to quit smoking of the participants of a hospital-based smoking cessation program in Greece. J Caring Sci. 2015;4:1. doi: 10.5681/jcs.2015.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCrady BS, Zucker RA, Molina BS, Ammon L, Ames GM, Longabaugh R. Social environmental influences on the development and resolution of alcohol problems. Alcohol Clin Exp Res. 2006;30:688–99. doi: 10.1111/j.1530-0277.2006.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Souza NP, Lira PI, Fontbonne A, Pinto FC, Cesse EÂ. (Mal) nutrition and the new epidemiological trend in a context of development and inequalities. Cien Saude Colet. 2017;22:2257–66. doi: 10.1590/1413-81232017227.03042017. [DOI] [PubMed] [Google Scholar]
- 46.Humpel N, Owen N, Leslie E. Environmental factors associated with adults’ participation in physical activity: A review. Am J Prev Med. 2002;22:188–99. doi: 10.1016/s0749-3797(01)00426-3. [DOI] [PubMed] [Google Scholar]
- 47.Baker P, Hawkes C, Wingrove K, Demaio AR, Parkhurst J, Thow AM, et al. What drives political commitment for nutrition? A review and framework synthesis to inform the United Nations Decade of Action on Nutrition. BMJ Glob Health. 2018;3:e000485. doi: 10.1136/bmjgh-2017-000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lezine DA, Reed GA. Political will: A bridge between public health knowledge and action. Am J Public Health. 2007;97:2010–3. doi: 10.2105/AJPH.2007.113282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pagliccia N, Alvarez Pérez A. The Cuban experience in public health: Does political will have a role? Int J Health Serv. 2012;42:77–94. doi: 10.2190/HS.42.1.h. [DOI] [PubMed] [Google Scholar]
- 50.Benjamins MR. Religious beliefs, diet, and physical activity among Jewish adolescents. J Sci Study Relig. 2012;51:588–97. [Google Scholar]
- 51.Luoma J, Guinther P, Potter J, Cheslock M. Experienced-based versus scenario-based assessments of shame and guilt and their relationship to alcohol consumption and problems. Subst Use Misuse. 2017;52:1692–700. doi: 10.1080/10826084.2017.1305416. [DOI] [PubMed] [Google Scholar]
- 52.Sherwood NE, Neumark-Sztainer D. Internalization of the sociocultural ideal: Weight-related attitudes and dieting behaviors among young adolescent girls. Am J Health Promot. 2001;15:228–31. doi: 10.4278/0890-1171-15.4.228. [DOI] [PubMed] [Google Scholar]
- 53.Li J, Wu B, Selbæk G, Krokstad S, Helvik AS. Factors associated with consumption of alcohol in older adults – A comparison between two cultures, China and Norway: The CLHLS and the HUNT-study. BMC Geriatr. 2017;17:172. doi: 10.1186/s12877-017-0562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Seefeldt V, Malina RM, Clark MA. Factors affecting levels of physical activity in adults. Sports Med. 2002;32:143–68. doi: 10.2165/00007256-200232030-00001. [DOI] [PubMed] [Google Scholar]
- 55.Moxley RL, Jicha KA, Thompson GH. Testing the importance of family solidarity, community structure, information access, and social capital in predicting nutrition health knowledge and food choices in the Philippines. Ecol Food Nutr. 2011;50:215–39. doi: 10.1080/03670244.2011.568907. [DOI] [PubMed] [Google Scholar]
- 56.Åslund C, Nilsson KW. Social capital in relation to alcohol consumption, smoking, and illicit drug use among adolescents: A cross-sectional study in Sweden. Int J Equity Health. 2013;12:33. doi: 10.1186/1475-9276-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Karimian J, Hosseini TA, Shekarchizadeh P, Nafchi SM. The relationship between social capital and the way of spending leisure time, based on physical activities. J Educ Health Promot. 2015;4:79. doi: 10.4103/2277-9531.171793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lallukka T, Laaksonen M, Rahkonen O, Roos E, Lahelma E. Multiple socio-economic circumstances and healthy food habits. Eur J Clin Nutr. 2007;61:701–10. doi: 10.1038/sj.ejcn.1602583. [DOI] [PubMed] [Google Scholar]
- 59.Dumbili E. Changing patterns of alcohol consumption in Nigeria: An exploration of responsible factors and consequences. A Journal of the BSA MedSoc Group. 2013;7(1):20–33. [Google Scholar]
- 60.Weil DN. Handbook of Economic Growth. Vol. 2. Elsevier; 2014. Health and economic growth; pp. 623–82. [Google Scholar]
- 61.Headey DD. Developmental drivers of nutritional change: A cross-country analysis. World Dev. 2013;42:76–88. [Google Scholar]
- 62.Liu S, Griffiths SM. From economic development to public health improvement: China faces equity challenges. Public Health. 2011;125:669–74. doi: 10.1016/j.puhe.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 63.Burggraf C, Kuhn L, Zhao QR, Teuber R, Glauben T. Economic growth and nutrition transition: An empirical analysis comparing demand elasticities for foods in China and Russia. J Integr Agric. 2015;14:1008–22. [Google Scholar]
- 64.Pourreza A, Geravandi S, Pakdaman M. Food security and economic growth. J Nutr Food Secur. 2018;3:113–5. [Google Scholar]
- 65.Ghosh S. India: Nutrition intake and economic growth, a causality analysis. Dev Stud Res. 2018;5:69–82. [Google Scholar]
- 66.Allen LN, Nicholson BD, Yeung BYT, Goiana-da-Silva F. Implementation of non-communicable disease policies: A geopolitical analysis of 151 countries. Lancet Glob Health. 2020;8:e50–8. doi: 10.1016/S2214-109X(19)30446-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang H. Tobacco control in China: The dilemma between economic development and health improvement. Salud Publica Mex. 2006;48(Suppl 1):S140–7. doi: 10.1590/s0036-36342006000700017. [DOI] [PubMed] [Google Scholar]
- 68.Hu TW, Lee AH. Commentary: Tobacco control and tobacco farming in African countries. J Public Health Policy. 2015;36:41–51. doi: 10.1057/jphp.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ferreira-Borges C, Dias S, Babor T, Esser MB, Parry CD. Alcohol and public health in Africa: Can we prevent alcohol-related harm from increasing? Addiction. 2015;110:1373–9. doi: 10.1111/add.12916. [DOI] [PubMed] [Google Scholar]
- 70.Collins SE. Associations between socioeconomic factors and alcohol outcomes. Alcohol Res. 2016;38:83–94. [PMC free article] [PubMed] [Google Scholar]
- 71.Linetzky B, De Maio F, Ferrante D, Konfino J, Boissonnet C. Sex-stratified socio-economic gradients in physical inactivity, obesity, and diabetes: Evidence of short-term changes in Argentina. Int J Public Health. 2013;58:277–84. doi: 10.1007/s00038-012-0371-z. [DOI] [PubMed] [Google Scholar]
- 72.Mlangeni L, Makola L, Naidoo I, Chibi B, Sokhela Z, Silimfe Z, et al. Factors associated with physical activity in South Africa: Evidence from a National Population Based Survey. Open Public Health J. 2018;11:516–525. doi: 10.2174/1874944501811010516. [Google Scholar]
- 73.Bauman A, Ma G, Cuevas F, Omar Z, Waqanivalu T, Phongsavan P, et al. Cross-national comparisons of socioeconomic differences in the prevalence of leisure-time and occupational physical activity, and active commuting in six Asia-Pacific countries. J Epidemiol Community Health. 2011;65:35–43. doi: 10.1136/jech.2008.086710. [DOI] [PubMed] [Google Scholar]
- 74.Johnson CM, Sharkey JR, Dean WR. Eating behaviors and social capital are associated with fruit and vegetable intake among rural adults. J Hunger Environ Nutr. 2010;5:302–15. doi: 10.1080/19320248.2010.504094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Berry HL, Welsh JA. Social capital and health in Australia: An overview from the household, income and labour dynamics in Australia survey. Soc Sci Med. 2010;70:588–96. doi: 10.1016/j.socscimed.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 76.Davison KK, Nishi A, Kranz S, Wyckoff L, May JJ, Earle-Richardson GB, et al. Associations among social capital, parenting for active lifestyles, and youth physical activity in rural families living in upstate New York. Soc Sci Med. 2012;75:1488–96. doi: 10.1016/j.socscimed.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 77.Prins RG, Mohnen SM, van Lenthe FJ, Brug J, Oenema A. Are neighbourhood social capital and availability of sports facilities related to sports participation among Dutch adolescents? Int J Behav Nutr Phys Act. 2012;9:90. doi: 10.1186/1479-5868-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen WL, Zhang CG, Cui ZY, Wang JY, Zhao J, Wang JW, et al. The impact of social capital on physical activity and nutrition in China: The mediating effect of health literacy. BMC Public Health. 2019;19:1–10. doi: 10.1186/s12889-019-8037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hasan MZ, Cohen JE, Bishai D, Kennedy CE, Rao KD, Ahuja A, et al. Social capital and peer influence of tobacco consumption: A cross-sectional study among household heads in rural Uttar Pradesh, India. BMJ Open. 2020;10:e037202. doi: 10.1136/bmjopen-2020-037202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Koutra K, Kritsotakis G, Orfanos P, Ratsika N, Kokkevi A, Philalithis A. Social capital and regular alcohol use and binge drinking in adolescence: A cross-sectional study in Greece. Drugs Educ Prev Policy. 2014;21:299–309. [Google Scholar]
- 81.Strittmatter A, Sunde U. Health and economic development – Evidence from the introduction of public health care. J Popul Econ. 2013;26:1549–84. [Google Scholar]
- 82.Oyewole Oyediran E. Approaches to enhanced political will for achieving nutrition-related millennium development goals in Nigeria. J Nutr Food Sci. 2015;5:2. [Google Scholar]
- 83.Murphy MM, Unwin N, Samuels T, Hassell TA, Bishop L, Guell C. Evaluating policy responses to noncommunicable diseases in seven Caribbean countries: Challenges to addressing unhealthy diets and physical inactivity. Rev Panam Salud Púlica. 2019;42:e174. doi: 10.26633/RPSP.2018.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Goins KV, Schneider KL, Brownson R, Carnoske C, Evenson K, Eyler A, et al. Municipal officials’ perceived barriers to consideration of physical activity in community design decision making. J Public Health Manag Pract. 2013;19(3 Suppl 1):S65. doi: 10.1097/PHH.0b013e318284970e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fox AM, Balarajan Y, Cheng C, Reich MR. Measuring political commitment and opportunities to advance food and nutrition security: Piloting a rapid assessment tool. Health Policy Plan. 2015;30:566–78. doi: 10.1093/heapol/czu035. [DOI] [PubMed] [Google Scholar]
- 86.Hawkins B, McCambridge J. Policy windows and multiple streams: An analysis of alcohol pricing policy in England. Policy Polit. 2020;48:315–33. [Google Scholar]
- 87.Sheeran P, Maki A, Montanaro E, Avishai-Yitshak A, Bryan A, Klein WM, et al. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychol. 2016;35:1178. doi: 10.1037/hea0000387. [DOI] [PubMed] [Google Scholar]
- 88.Acheampong I, Haldeman L. Are nutrition knowledge, attitudes, and beliefs associated with obesity among low-income Hispanic and African American women caretakers? J Obes. 2013;2013:123901. doi: 10.1155/2013/123901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Martin-Moreno JM, Apfel F, Sanchez JL, Galea G, Jakab Z. The social nature of chronic noncommunicable diseases and how to tackle them through communication technology, training, and outreach. J Health Commun. 2011;16(Suppl 2):94–106. doi: 10.1080/10810730.2011.596915. [DOI] [PubMed] [Google Scholar]


