During the COVID-19 pandemic, vaccines have had an important role as a public health intervention. As of Nov 21, 2021, more than 7·4 billion doses of COVID-19 vaccine have been administered worldwide.1 However, data on COVID-19 vaccines are still scarce in individuals who are immunocompromised, including those with autoimmune rheumatic diseases, who are less likely to have an adequate immune response after primary vaccination than are healthy populations. Considering the increased risk of SARS-CoV-2 infection and severe outcomes of COVID-19, the immune response of immunocompromised people to COVID-19 vaccines needs to be further assessed. The phase 4 CoronavRheum study,2 which examined the immunogenicity and safety of the inactivated SARS-CoV-2 vaccine CoronaVac in patients with autoimmune rheumatic diseases in Brazil, showed lower seroconversion rates in patients than in healthy controls. However, in this initial report, patients exposed to SARS-CoV-2 were excluded from the analysis, and so the effect of CoronaVac in patients who have recovered from SARS-CoV-2 infection was unknown.
In The Lancet Rheumatology, Nadia E Aikawa and colleagues report a subgroup analysis of the CoronavRheum study,3 comparing CoronaVac immunogenicity in patients with autoimmune rheumatic disease who were SARS-CoV-2 seropositive or seronegative with controls who were seropositive or seronegative. 942 participants were included in the subgroup analysis, of whom 157 were seropositive patients, 157 were seropositive controls, 471 were seronegative patients with autoimmune rheumatic diseases and 157 were seronegative controls (median age was 48 years [IQR 38–56] and 594 [63%] were female and 348 [37%] were male). All participants received two doses of CoronaVac at day 0 and day 28. Similar proportions of seropositive patients and controls had anti-SARS-CoV-2 S1 or S2 IgG seropositivity at day 28 (149 [95%] of 157 vs 155 [99%] of 157; p=0·10) and day 69 (154 [98%] vs 157 [100%]; p=0·25). High proportions of participants with neutralising antibody positivity were seen at day 28 (138 [88%] vs 151 [96%]; p=0·0067) and day 69 (141 [90%] vs 155 [99%]; p=0·0005); although a lower proportion of patients were neutralising antibody positive than controls. By contrast, vaccine-elicited immune responses in seronegative patients and controls were significantly lower than in seropositive patients and controls at both day 28 and day 69. In terms of immunogenicity dynamics, both seropositive groups showed a robust immune response after the first dose of CoronaVac without a further increase after the second dose, whereas the seronegative groups required the second dose to obtain a similar immune response.
This study provides evidence that, in patients with autoimmune rheumatic diseases who have been exposed to natural SARS-CoV-2 infection, a single dose of CoronaVac might be sufficient to produce robust antibody responses, by contrast with unexposed individuals who need at least two doses.3 Several previous studies of other COVID-19 vaccines showed similar results in the general population or in patients with autoimmune diseases. A single dose of mRNA vaccine or adenovirus-vectored vaccine in patients who had recovered from COVID-19 has been found to elicit similar humoral immunity as elicited by two doses of vaccine in unexposed patients, which is possibly related to the enhanced recall response of pre-existing memory B cells compared with the primary response.4, 5, 6, 7 To date, more than 294 million doses of CoronaVac have been deployed for use in dozens of countries and regions worldwide, and uninfected individuals who have received two doses of CoronaVac are recommended to get an additional dose after 6 months.1 However, Aikawa and colleagues3 found that the antibody responses of SARS-CoV-2-exposed populations did not increase within 6 weeks after the second dose of vaccine, and so whether this population would need an additional dose remains to be determined in longer-term studies, and the effects of previous SARS-CoV-2 exposure also need to be verified in further clinical trials.
Another highlight of the study is that Aikawa and colleagues could provide evidence of a robust response to vaccination for populations with immunodeficiencies, who are more likely to develop severe forms of COVID-19 and die as a result of COVID-19. Multiple studies have shown that immunocompromised individuals usually have weaker antiviral immune responses and vaccine responsiveness than healthy controls.8 To mitigate risks in this population and to maximise the potential effectiveness of vaccination, WHO and the US Food and Drug Administration recently recommended that immunocompromised individuals should have an additional dose of vaccine.8, 9
Nevertheless, Aikawa and colleagues' study suggests that an additional dose of vaccine for immunocompromised individuals who have already been exposed to SARS-CoV-2 might not be needed. With the limited supply and uneven distribution of COVID-19 vaccines among regions worldwide, tailoring vaccine doses for different populations will be more conducive to rational allocation of vaccine resources.
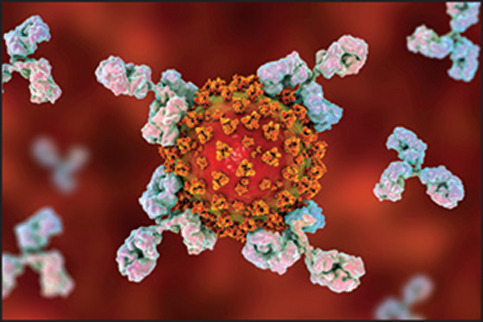
© 2022 Shutterstock
We declare no competing interests.
References
- 1.WHO COVID-19 vaccines. World Health Organization, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines
- 2.Medeiros-Ribeiro AC, Aikawa NE, Saad CGS, et al. Immunogenicity and safety of the CoronaVac inactivated vaccine in patients with autoimmune rheumatic diseases: a phase 4 trial. Nat Med. 2021;27:1744–1751. doi: 10.1038/s41591-021-01469-5. [DOI] [PubMed] [Google Scholar]
- 3.Aikawa NE, Kupa LVK, Pasoto SG, et al. Immunogenicity and safety of two doses of the CoronaVac SARS-CoV-2 vaccine in SARS-CoV-2 seropositive and seronegative patients with autoimmune rheumatic diseases in Brazil: a subgroup analysis of a phase 4 prospective study. Lancet Rheumatol. 2021 doi: 10.1016/S2665-9913(21)00327-1. published online Dec 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ebinger JE, Fert-Bober J, Printsev I, et al. Antibody responses to the BNT162b2 mRNA vaccine in individuals previously infected with SARS-CoV-2. Nat Med. 2021;27:981–984. doi: 10.1038/s41591-021-01325-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krammer F, Srivastava K, Alshammary H, et al. Antibody responses in seropositive persons after a single dose of SARS-CoV-2 mRNA vaccine. N Engl J Med. 2021;384:1372–1374. doi: 10.1056/NEJMc2101667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boekel L, Steenhuis M, Hooijberg F, et al. Antibody development after COVID-19 vaccination in patients with autoimmune diseases in the Netherlands: a substudy of data from two prospective cohort studies. Lancet Rheumatol. 2021;3:e778–e788. doi: 10.1016/S2665-9913(21)00222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goel RR, Apostolidis SA, Painter MM, et al. Distinct antibody and memory B cell responses in SARS-CoV-2 naïve and recovered individuals following mRNA vaccination. Sci Immunol. 2021;6:eabi6950. doi: 10.1126/sciimmunol.abi6950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Interim recommendations for an extended primary series with an additional vaccine dose for COVID-19 vaccination in immunocompromised persons. World Health Organization, Oct 26, 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-vaccines-SAGE_recommendation-immunocompromised-persons
- 9.US Food and Drug Administration Coronavirus (COVID-19) update: FDA authorizes additional vaccine dose for certain immunocompromised individuals. Aug 12, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-additional-vaccine-dose-certain-immunocompromised


