Abstract
Purpose
The COVID-19 pandemic disrupted normal operations of health care services, broad sectors of the economy, and the ability to socialize freely. For those with tinnitus, such changes can be factors in exacerbating tinnitus. The purpose of this study was to determine tinnitus help-seeking behavior, which resources individuals utilized to cope during the pandemic, and what additional support is desired.
Method
An exploratory cross-sectional study design including 1,522 adults with tinnitus living in North America (Canada and the United States) was used. Data were collected through an online survey distributed by the American Tinnitus Association via e-mail. Free text from open-ended questions was analyzed using the automated content analysis. The responses to the structured questionnaire were analyzed using descriptive and nonparametric statistics.
Results
Significantly less tinnitus support was sought during the pandemic, and very few respondents utilized tinnitus support networks during the pandemic at the time the survey was conducted. Nonetheless, seeking support during the pandemic was significantly associated with significantly less tinnitus distress. The most frequently utilized resources for coping during the pandemic were contacting family and friends, spending time outdoors or in nature, relaxation, and exercise. Such tools for coping were associated with significantly less tinnitus distress. The support requested and advice provided by participants to health care services had overlap. The main support needs related to managing tinnitus included addressing hearing loss, providing peer support, finding cures, and accessing trained and understanding health care providers to help. The advice for professionals related to tinnitus management included the need for cures, personalized support, addressing hearing loss, targeting the tinnitus percept, and providing more information about the condition.
Conclusions
These findings provide suggestions on how to better support those with tinnitus at a time when health care is undergoing rapid changes. Findings can be used by stakeholders, clinical practitioners, and tinnitus support services to devise ways to work more effectively together to improve access to patient-driven, suitable, accessible, and evidence-based support.
Supplemental Material
The rapid spread of the COVID-19 infection resulted in the outbreak of a global pandemic (World Health Organization, 2020). To break the chain of transmission in this human-to-human virus, numerous regional lockdowns were enforced. People were asked to stay at home, maintain social distance guidelines, and many venues—such as schools, offices, and recreational venues—were closed, particularly in hotspot regions with higher points of contact between people (Roy & Ghosh, 2020). These measures also disrupted the normal operation of health care services, and support was not always available, particularly for medical concerns that were not critical. Such service included care for hearing health care, such as addressing hearing loss with the fitting or maintenance of hearing aids and managing tinnitus, which is the perception of sound/s when no external sound is present.
Since there is a bidirectional relationship between tinnitus and stress (Mazurek et al., 2019), the additional stress associated with the pandemic may be a contributing factor to the reports of increased tinnitus severity during the pandemic (Anzivino et al., 2020). Lifestyle changes during the pandemic may have further impacted on tinnitus experiences, as found in a global tinnitus study, including 3,103 adults (Beukes, Baguley, et al., 2020). Almost a third (32%) reported their pre-existing tinnitus was exacerbated. Tinnitus was worse for those who were self-isolating, experiencing loneliness, sleeping poorly, and exercising less than before the pandemic. Increased levels of depression, anxiety, irritability, and financial worries further contributed to tinnitus being more bothersome. As tinnitus is often associated with anxiety and depression (Salazar et al., 2019; Trevis et al., 2018), identifying ways to support such individuals should be prioritized, especially considering it affects around 10% of the U.S. population (Bhatt et al., 2016; Shargorodsky et al., 2010). Moreover, help should be readily available for those who developed tinnitus and/or hearing loss following COVID-19 infection, since this might be an unknown and a possible consequence of the infection (Munro et al., 2020; Viola et al., 2020).
Although tinnitus was exacerbated during the pandemic for some, Beukes, Baguley, et al. (2020) found 67% of the respondents reported their tinnitus was not affected, and 1% indicated their tinnitus improved. It may be assumed that such individuals had effective coping skills to manage stress, which thereby minimized the impact on their tinnitus, Understanding their coping techniques is important to aid future intervention and support planning and should be investigated. The aim of this study was to (a) investigate tinnitus help-seeking behavior during the pandemic, (b) identify what resources were utilized to cope with tinnitus, and (c) what additional support is needed by those with tinnitus.
Method
Study Design
An exploratory cross-sectional survey study design was used to investigate tinnitus experiences (see Beukes, Baguley, et al., 2020) and examine how those with tinnitus coped during the COVID-19 pandemic. Ethical approval was granted by Lamar University (IRB-FY20-215). The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) reporting guidelines (von Elm et al., 2007) were used to report the methods and results of the study.
Data Collection
Eligibility to complete the survey included being 18 years old or older, reporting the presence of tinnitus, and living in North America (Canada and the United States). The American Tinnitus Association (ATA) distributed the survey via e-mail in May 2020. The survey was available for 6 weeks. Online informed consent was required before taking the survey, and only one submission from each IP address was permitted by the survey software. The survey was distributed online via Qualtrics. No randomization of items was used, and respondents were unable to change their responses once submitted. No identifiable data were collected.
To investigate the research questions, the following information was gathered using closed-ended questions where relevant answers could be selected and free text could be added if required: (a) demographic information including age, gender, nationality, ethnicity, tinnitus duration, and use of hearing aids; (b) help-seeking prior to and during the pandemic; (c) resources utilized to cope during the pandemic; and (d) support required to better manage tinnitus by asking the following open-ended questions:
Support question: What type of support would help you better manage your tinnitus or hearing-related issues during these uncertain times?
Advice question: What advice/suggestions for health care professionals and/or researchers can you offer so that we might provide/develop more effective care for the future?
In addition, tinnitus severity was measured using the Tinnitus Handicap Inventory–Screening Version (C. W. Newman et al., 2008) consisting of 10 questions, with scoring between 0 and 40, with higher scores indicating more severe tinnitus. Scores less than 6 indicate no difficulty, while scores above 6 indicate some degree of difficulty and that benefit may be obtained from audiological and/or psychological support. The survey questions used in this study can be found in Supplemental Material S1.
Data Analysis
Statistical Analysis
The Statistical Package for Social Sciences Version 26.0 was used to perform the descriptive and nonparametric tests on the responses to structured questions. Descriptive statistics, including frequencies, means, and standard deviations, were computed. Linear regression was used to look at the association between variables. Statements from the free-text responses were used as examples to support the descriptive analysis of the results.
Automated Content Analysis
The automated content analysis (ACA) was used to analyze the free-text responses to two open-ended questions using the Leximancer software (Edition 4.0). ACA is a type of “topic modeling” approach for analyzing qualitative data using quantitative technique to identify patterns within the data (Nunez-Mir et al., 2016). ACA is underpinned by Bayesian theory and uses advanced statistical methods to examine the semantic and linguistic complexity of the text to produce concepts and themes related to the text. ACA is found to have equivalent and/or higher sematic coherence than human interrater correlations in qualitative analysis (D. Newman et al., 2010). ACA provides a bird's-eye view of the data, showing primary themes, concepts, frequencies, and examples of meaning units by mapping the text to theme/concept. The terms “theme” and “concept” in ACA refer to “category” and “subcategory,” respectively, in qualitative content analysis. After the initial review of the themes, redundant words, which included “COVID,” “none,” “sure,” and “told,” were removed, and the analysis was done again. The themes are presented in a concept map showing the main concepts, their frequency, and interconnectedness (or co-occurrence). The bubbles represent the themes, while the dots within the bubbles represent the concepts included within the theme. A detailed description of concept mapping by Leximancer software was provided by Smith and Humphreys (2006).
Results
Characteristics of the Individuals With Tinnitus
There were 1,522 eligible respondents who completed the survey. Of these, 896 provided free-text responses for open-ended questions. The mean tinnitus severity was 23.85 (SD = 10.10) out of 40, indicating tinnitus levels in which such persons might benefit from information counseling and management strategies from health care professionals in audiology and/or psychology. The mean tinnitus duration was 15 years (SD = 15). The average age was 64.05 years (SD = 11.58), among an age range of 18–97 years. There were more men (n = 856, 56%) than women (n = 651, 43%), with 15 (1%) being gender diverse and/or preferring not to state their gender.
Tinnitus Support Sought Prior to and During the Pandemic
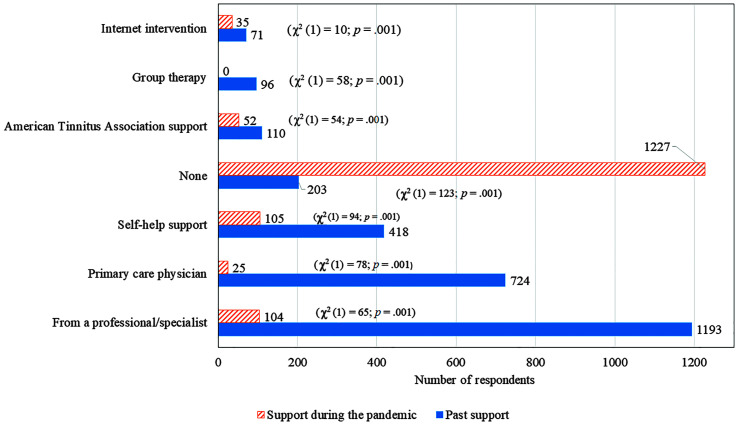
To ascertain support sought during the pandemic, comparisons were made between the support sought prior to and during the pandemic. The analysis of the responses to structured questions indicated that significantly less support was sought during the pandemic, as shown in Figure 1.
Figure 1.
Comparison of support prior to and during the pandemic (chi-square analysis provided in brackets indicating significant differences).
Linear regression indicated that help seeking was related to tinnitus severity, F(4) = 5.31, p < .001, and how bothersome tinnitus was (scale of 1–5), F(4) = 3.41, p = .009, in a model excluding help seeking via the Internet or helplines. Tinnitus distress was significantly less for those who sought help via their usual clinics (B = −2.77, SE = 1.19, t = −2.33, p = .02), had ongoing support (B = −1.89, SE = 0.73, t = 2.60, p = .01), or had remote support (B = −1.51, SE = 0.59, t = −2.54, p = .01).
Those providing additional free-text responses indicated that less support was sought due to concerns regarding the risks of going out as supported by such statements as, “My general practitioner has referred me to an Ear Nose Throat doctor but I am hesitant to make an appointment due to the risks[of infection] involved” (male, 60 years old, California). Some participants also indicated in free-text responses that they sought help but were unsure where to access it, as noted by such statements as, “I don't know what I can do about my tinnitus and wish there was information on where to access online help at a time like this” (man, 67 years old, Oklahoma).
The majority of those who sought additional help rated the support as generally helpful (n = 49/74, 66%) or very helpful (n = 18/74, 24%), with 9% (n = 7/74) indicating that the support was not helpful. Concerns were raised by 9% (n = 141) that they would not be able to access professional help for their tinnitus during the pandemic, as noted by the following statement: “I hope to see a doctor later as the offices are closed now due to the virus” (woman, 80 years old, Florida).
Prior to the pandemic, 83% (n = 1,247/1,490) reported not attending a tinnitus support group, 7% reported attending an in-person tinnitus support group (n = 105/1,490), 6% (n = 83/1,490) received online support or information from a support group, and 4% (n = 55/1,490) from an online discussion forum. Some indicated a desire to be part of a group and have more information about tinnitus, as noted by the following statement: “I would not mind being part of a tinnitus help group, even if it is online. [I'm] already part of an online hearing support group that I enjoy very much” (woman, 79 years old, Arizona).
During the pandemic and at the time of the survey, only three individuals (0.2% of the sample) reported attending an online tinnitus support group, as these may not have been readily available as noted by such statements as “I think it would be great if Zoom meetings were available for support groups” (woman, 77 years old, Minnesota). Twenty individuals (2% of the sample) reported being negatively affected by not being able to attend support group meetings during the pandemic, explained as “I miss my in-person group support. Since the pandemic, everything closed down. I am missing support, which leaves me feeling less confident in dealing with the ups and downs of everyday tinnitus, and each day I struggle with who is stronger, me or tinnitus, as it is on constant [and is a] relentless tyrant at times” (woman, 66 years old, Massachusetts).
Support for Tinnitus-Related Comorbidities
Support may also have been needed for other tinnitus-related comorbidities. In addition to tinnitus, 702 (46%) reported hearing loss, 346 (23%) reported hyperacusis, and 96 (6%) also experienced misophonia (severe annoyance caused by such sounds as chewing and throat clearing). There were 899 (57%) respondents not wearing any devices and 488 (31%) using unilateral or bilateral hearing aids. Other devices used were wearable sound generator/s (n = 137, 9%), hearable/s (n = 35, 2%), cochlear implant/s (n = 15, 0.7%), and bone-anchored hearing aids (0.3%). Some reported needing devices but being unable to afford them, as noted by the following comment: “It costs $4,000 for me to get wearable sound generators to assist with my tinnitus. Our family budget cannot afford that. I would like to get financial assistance to pay for sound generator treatments” (woman, 42 years old, North Carolina). Concerns were raised by 7% (n = 114) of respondents that they were unable to get support for their hearing-related needs, including hearing aids, during the pandemic. This was supported by such statements as “My hearing aids were such an expensive investment and I can't go for my check. If something should happen to one or both of them, I am concerned I would not be able to get them repaired” (woman, 67 years old, New York) and “My left hearing aid squeals. I am in a retirement home and we are in lockdown, so I am unable to have the aid repaired” (woman, 85 years old, Texas).
In additional to tinnitus, 70% of respondents reported experiencing additional health problems, including hypertension (n = 455, 30%), back/neck pain (n = 326, 21%), osteoarthritis (n = 273, 18%), chronic allergies (n = 220, 14%), thyroid disease (n = 174, 11%), and cancer (n = 134, 9%). For this sample, linear regression indicated that the presence of additional health problems were not associated with tinnitus severity, F(13) = 1.62, p = .07, or how bothersome tinnitus was (scale of 1–5), F(13) = 1.16, p = .30. Obtaining support for additional health problems during the pandemic was a concern raised by 26% (n = 394). This was supported by such statements as “They need to understand that other health problems didn't stop because the coronavirus arrived. People still need health care” (man, 68 years old, Oregon).
In addition to tinnitus, anxiety (n = 503/1,840, 27%), depression (n = 424/1,840, 23%) and other psychiatric disorders (n = 51/1,840, 3%) were reported to have been diagnosed in the past. These conditions were managed through use of medication (n = 373/724, 51%), professional support (n = 178/724, 25%), and online tools (42/724, 6%). For this sample, linear regression indicated that the reporting past diagnosis of a mental health issue was not associated with tinnitus severity, F(3) = 1.68, p = .17, or how bothersome tinnitus was (scale of 1–5), F(3) = .71, p = .55. No help for mental health concerns was noted by 18% (n = 132/724). Seeking support for mental health issues during the pandemic was a concern raised by 4% (n = 56), supported by statements such as “My anxiety has worsened during the pandemic because of my tinnitus, which causes more stress and anxiety—[it's] a vicious circle” (woman, 50 years old, Georgia).
Resources to Cope With the Present Situation
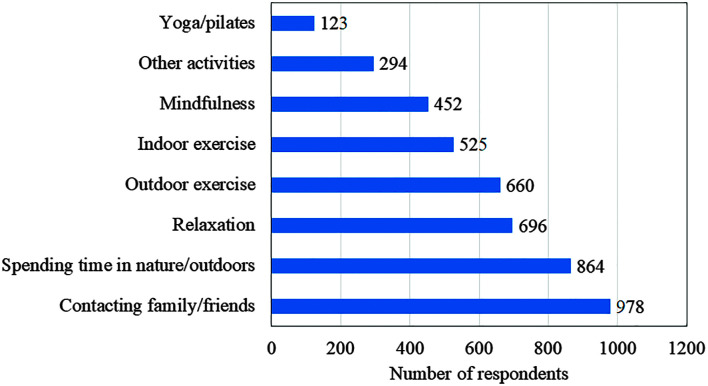
Participants indicated the most frequently utilized resource for coping during the pandemic was family and friends (reported by 65%), followed by spending time outdoors or in nature (reported by 57%), as shown in Figure 2. Free-text responses indicated that other support activities for coping included arts and crafts, woodwork, cooking, reading, online courses, pet therapy, music, prayer, movies, gardening, house/yard maintenance, or other projects. Linear regression indicated that using additional resources to cope was related to tinnitus severity, F(7) = 3.83, p < .001, and how bothersome tinnitus was (scale of 1–5), F(7) = 2.37, p = .02. Tinnitus distress was less for those who used relaxation (B = −2.65, SE = 1.13, t = −2.34, p = .02), outdoor exercise (B = −1.51, SE = 0.60, t = 2.53, p = .01), and/or spent time outdoors to cope (B = −0.63, SE = 0.19, t = −3.31, p < .001).
Figure 2.
Resources used to cope during the pandemic.
For respondents who consume alcohol, 34% (n = 486) reported similar consumption levels during the pandemic, with 16% (n = 218) reporting lower levels due to such things as decreased restaurant visits and social gatherings. However, a smaller percentage (n = 160, 11%) reported higher consumption due to more home dining. More substance and drug usage (e.g., marijuana) was reported by 0.5% (n = 8/1,393), as noted by the following comment: “[I am] smoking more marijuana to help me cope with the present stress and to sleep” (man, 42 years old, Canada). Some reported using medication to cope, particularly for sleep, including the use of valium, doxepin, antidepressants, as well as alternative homeopathic remedies.
Respondents living with others indicated that such individuals were moderately (n = 479, 31%) or very (n = 646, 43%) understanding and/or supportive of issues related to their tinnitus, with only 7% (n = 84) feeling that they were not supportive. An example statement was “I want to discuss my problems with someone who has experienced the debilitating events that occur with tinnitus and understand without them rolling their eyes” (woman, 71 years old, Colorado). During the pandemic, respondents indicated that the people living with them generally provided similar support (n = 1,074, 92%) compared with prior to the pandemic and, in some cases, provided more support (n = 64, 6%), with a few respondents reporting less support (n = 27, 2%).
Type of Support Required During the Pandemic
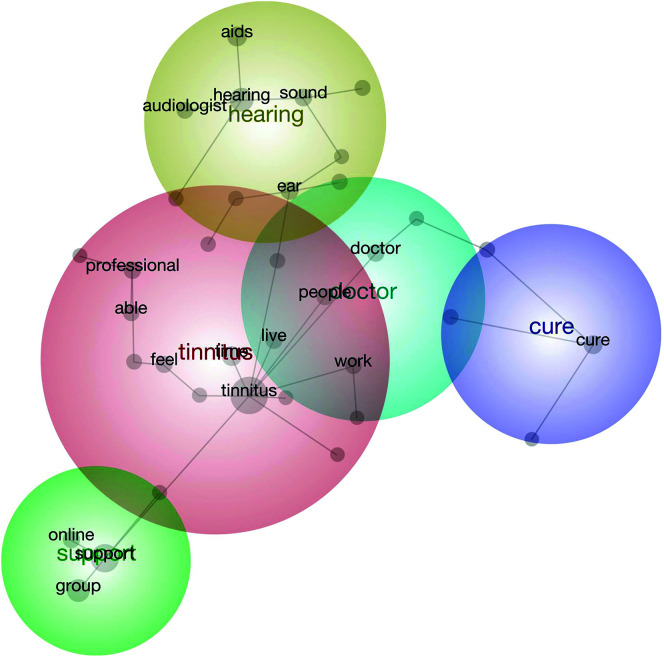
Table 1 and Figure 3 present the ACA results for the open-text data to examine the support question that identified five support themes related to tinnitus, including hearing loss, providing peer support, finding a cure for tinnitus, and ensuring access to trained and understanding doctors to help.
Table 1.
Themes and concepts regarding the type of support desired.
| Themes | Concepts | Hits | Descriptions of the theme | Examples |
|---|---|---|---|---|
| Tinnitus | Tinnitus, time, professional, feel, live, able | 304 | This theme mainly covered statements that expressed respondent's sentiment that there is no additional support needed and that learning to live with tinnitus is what is needed. | “I do not feel I could do anything better to manage my tinnitus. It was very difficult in the beginning, but over the course of time, it has gotten easier to live with.” “I have learned to live with it, and most times, even though it is like having a jet engine in my head, I am able for the most part to tune it out. The worst thing for me to do is dwell on it, discuss it, join groups to discuss it.” |
| Hearing | Hearing, aids, ear, sound, audiologist, need | 148 | This theme covered statements related to respondents' hearing needs (e.g., get hearing checked, hearing aid adjusted) either met or not met during the pandemic lockdown. |
“Prior to the coronavirus crisis, I had an appointment to see an audiologist and ENT. I think I probably need hearing aids.” “I am unable to see my out-of-state audiologist and my sound generators need adjustment.” |
| Support | Support, group, online | 146 | This theme identified the need for group online support for tinnitus. | “[I'd like a] therapy group online to assist with dealing with the buzzing noise.” “[I'd like a] support group…online, Zoom, etc.” |
| Cure | Cure | 92 | This theme identifies that some respondents are still looking for a cure and/or have understood that since there is no current cure, they rely on symptom management using alternative therapies. |
“Someone discovering a cure!” “Since there is no cure, I cannot expect any management. I take CBD to help me fall asleep.” |
| Doctor | Doctor, people, work | 81 | This theme included statements concerning need to consult with health care professionals for tinnitus and/or other general health issues. |
“Talking with a doctor that is trained in working with tinnitus issues.” “Busy working and going to doctors. May have walking pneumonia, or permanent scarring on lungs from COVID, takes all [my] time.” |
Figure 3.
Concept map regarding the type of support desired. The bubbles represent the themes while the dots within the bubble represent the concepts included within the theme, and the lines indicate their interconnectedness.
Suggestions for Health Care Professionals and Researchers
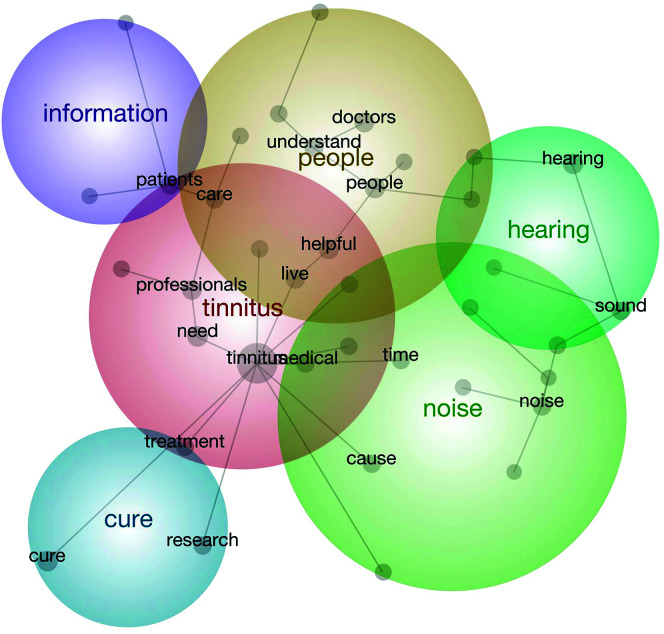
Table 2 and Figure 4 present the ACA results for the open-text data to examine the advice question that identified six suggestion themes related to tinnitus, finding a cure, personalized support, addressing hearing loss, addressing the tinnitus percept, and need for more information.
Table 2.
Themes and concepts regarding advice/suggestions for health care professionals.
| Themes | Concepts | Hits | Descriptions of the theme | Example |
|---|---|---|---|---|
| Tinnitus | Tinnitus, need, live, professionals, patients, medical, care | 468 | This theme covered respondents' suggestions in terms of tinnitus management by improving training for health care professionals and also developing evidence-based treatments for tinnitus. Some statements also included suggestions for health care professionals to be hopeful when talking to individuals with tinnitus because it is likely to help the patient cope. |
“Health care professionals have to STOP telling tinnitus patients that nothing can be done…go home and live it, there is no cure.” “Health care professionals need to be trained to answer questions related to tinnitus and be able to steer us in the right direction as far as what CAN be done to make it less bothersome and [easier] to live with.” “I would like to see a better connection between traditional medical health care (‘learn to live with it’) and alternative healing methods (several modalities have proven successful).” |
| Cure | Cure, research, treatment | 218 | This theme recognizes that many individuals with tinnitus are hoping for cures, although they are aware there are no cures currently available. |
“Health care professionals and researchers must be more vocal in their advocacy for treatment and ultimately cures for tinnitus. Many millions of people have this condition and suffer in silence.” “Find a cure or a truly effective treatment. Be honest but not cruel.” |
| People | People, helpful, doctors, understand | 198 | This theme identifies that it is necessary to understand individual needs and experiences related to tinnitus, which may aid in providing personalized support. | “Not a ‘common’ malady. Do not lump people together or make assumptions about [tinnitus] based on limited understanding of what in fact [tinnitus] sufferers individually experience.” “Be more understanding of tinnitus. Some doctors think I'm faking it.” |
| Hearing | Hearing, sound, ear | 138 | This theme covered statements related to respondents' hearing needs. | “The cross hearing aids are amazing; they can only get better with technology. Adding that extra sound in my good ear seemed to help my tinnitus.” “I was told I had hearing loss, but I could not hear all sounds because of the noise in my ear.” |
| Noise | Noise, cause, time | 124 | This theme specifically covered statements that focused on the need for addressing the tinnitus sound perception rather than its effects. | “I had been using CBD oil 2 to 3 times a day (have not been consistent [recently] since I'm almost out). It seems to help distract/manage/dissipate the noise.” “Find the mechanism in the brain that's causing all this noise. I know this is being studied and I feel someday it will be found.” |
| Information | Information | 26 | This theme identified user statements requesting more information and advice, especially through electronic media. | “More communication (i.e., e-mails, articles, etc.) providing information on coping options.” “Provide ongoing information on promising studies and studies that are available to participate in. It is very hard to find clinical trials for this disease.” “Develop an information program and an actual treatment program.” |
Figure 4.
Concept map regarding advice/suggestions for health care professionals and researchers. The bubbles represent the themes while the dots within the bubble represent the concepts included within the theme, and the lines indicate their interconnectedness.
Discussion
This study investigated which coping resources people with tinnitus utilized, as well as the support needed (medical and nonmedical) for tinnitus, during the COVID-19 pandemic. When comparing help seeking, the level of support sought for tinnitus during the pandemic was significantly less than prior to the pandemic. Help sought during the pandemic included both medical and nonmedical help from professional health care providers (8%), self-help resources (7%), the ATA (3%), and Internet interventions (2%). This decrease in help-seeking behavior during the pandemic appeared to be partly attributable to people being unable to access support or not realizing support was available. It could also be that people were afraid to seek care during the pandemic. It was found that tinnitus distress was significantly lower for those who had sought support during the pandemic, either from their usual health care or support networks, including online support. The COVID-19 pandemic undoubtedly disrupted and transformed usual health care services; however, these findings demonstrate the need to make services more readily and safely available to people who might benefit from them (Rosenbaum, 2020).
As tinnitus seldom occurs as an isolated hearing disorder, 46% of the participants reported hearing and/or hyperacusis (23%) and misophonia (6%). Accessing support for these hearing-related difficulties and associated treatment devices, such as hearing aids, was also reported to be problematic. This may be partly attributed to the fact that many audiology clinics had reduced access during the pandemic. A United Kingdom–based survey indicated that, although the use of tele-audiology is increasing, this was not the case at the start of the pandemic (Saunders & Roughley, 2020). Further development of tele-audiology should be prioritized to ensure continued hearing health care support (Beukes et al., 2019; Manchaiah & Beukes, 2020; Manchaiah et al., 2020; Swanepoel & Hall, 2020). It was also noted that hearing aids were recommended to help with tinnitus and hearing loss, but respondents were not always able to purchase them because of cost. Due to the detrimental effects of untreated hearing loss, such as increased risk of dementia (Loughrey et al., 2018), ensuring access to affordable hearing aids/assistive listening devices should be prioritized (Sinha et al., 2020).
Seeking help for mental health issues during the pandemic was raised as a concern by 26%, in contrast to only 4% raising concerns about support for other health problems. This may reflect that, although most in-person health care was disrupted, telehealth was available in some instances and provided a continuation of general health care services (Hollander & Carr, 2020; Zhou et al., 2020).
The use of self-guided coping techniques, such as relaxation, exercising outdoors, and spending time outdoors, were reported strategies to reduce tinnitus distress during the pandemic. The most frequently used resource for coping with tinnitus during the pandemic was contact with family and friends. The importance of living with supportive people was also highlighted, which underscores the importance of educating significant others on the impact of tinnitus. Other resources that enhanced coping included spending time outdoors and in nature. Relaxation, exercise, and mindfulness were also cited as useful for coping during the pandemic. Tinnitus interventions that incorporate relaxation and mindfulness have been shown repeatedly to reduce tinnitus severity (Beukes, Bauley, et al., 2018; McKenna et al., 2017). Overall, this survey population appeared to draw on active methods of coping behaviors and to rely less on unhelpful behaviors. Using such coping techniques for managing tinnitus has been found to lower tinnitus severity (Beukes, Manchaiah, et al., 2018; Fludra et al., 2020), which might have contributed to the overall degree of tinnitus being less severe in this population.
Tinnitus support groups are often a valuable resource for those with tinnitus because they provide social connectedness and shared social identity (Pryce et al., 2019). Considering this, it was interesting that the majority of respondents (82%) reported not attending a support group prior to the pandemic and very few attended the limited online tinnitus support groups that formed because of the pandemic. Many respondents, even those wanting to join a support group, did not appear to be aware of the existence of support groups, such as those associated with the ATA. The need for peer support and more information about tinnitus were prominent themes in the analysis of responses related to desired support. As such, more should be done by health care professionals and tinnitus patient advocacy associations to actively promote support groups, particularly the cultivation of online groups, which can be accessed by anyone via the Internet. This is key since access in-person support groups are generally limited to larger metropolitan areas. Support groups could also share information about current tinnitus research and management strategies, which were other areas of desired support that respondents identified.
When planning tinnitus support and management services, it is important to include input from those actually experiencing tinnitus (Pryce et al., 2018). Thus, respondents were given the opportunity to make suggestions regarding the help they desired and advice they would give to health care professionals. The identified themes for the suggestions and advice were very similar, indicating these are prominent needs within the population. The identified themes included hope for cures, need to understand why they had tinnitus, and what caused the tinnitus. Similar themes have been reported when identifying patient preferences in tinnitus treatments in a U.K. population (Pryce et al., 2018).
An additional identified theme was the availability of qualified professionals who understood the impact of tinnitus and could provide management guidance. This indicated a clear need for improvement in tinnitus training for all professionals who might see tinnitus patients (El-Shunnar et al., 2011). A need for accessible Internet-based tinnitus interventions, such as those currently being developed for the United States (Beukes, Fagelson, et al., 2020; Manchaiah et al., 2020), was also mentioned.
Another prominent theme was addressing hearing loss. Those with tinnitus often experience hearing difficulties and/or report that tinnitus makes it hard to hear. Addressing hearing loss when present is an important aspect of tinnitus management. During the pandemic, this was not always possible. Providers need to ensure that hearing difficulties are appropriately managed using suitable tele-audiology solutions. Respondents also indicated a need for people to be more aware of tinnitus and understand its negative impact. Tinnitus is often reported to be exacerbated in noisy situations, which results in some people limiting social outings. Access to quieter recreational spaces (e.g., restaurants) was also suggested. Overall, these results point to a range of support needed by individuals with tinnitus to effectively manage their tinnitus and its negative effects.
Limitations and Future Directions
There are numerous limitations in the interpretation of this study that should be considered. Although this study attempted to capture a wide range of responses from those living with tinnitus in the United States, it is more biased toward those within the ATA tinnitus community. It could be the case that this population is better informed about managing tinnitus and available support services. Comparisons of these desired support findings to that in other countries should be made.
Clinical Implications
Although it has been many months since the COVID-19 pandemic was declared, many of the social distancing restrictions remain. Health care services, especially nonurgent care, have not fully resumed, and social interactions remain limited for many people. The impact of this is far reaching for those with tinnitus (Beukes, Baguley, et al., 2020), and additional support should be provided. It is noteworthy that these findings are patient driven and are not those of stakeholders or professionals. The findings can therefore guide stakeholders, clinical services, tinnitus organizations, clinical training facilities, and tinnitus support groups. Common themes were the desire for peer support and more information about research into tinnitus cures and treatments. Participants suggested that more online information, such as talks by professionals and online support groups, would be valued. There was a clear need for effective treatments. Individual- and group-based guided cognitive behavioral therapy and/or Internet-based interventions may be a means of providing such support (Beukes et al., 2019); at present, few such interventions exist. The pandemic may have a positive impact if the outcome is greater coordination and cooperation among professionals in providing accessible, evidence-based care for individuals with tinnitus.
Supplementary Material
Acknowledgments
This work was partly funded by the National Institute on Deafness and Other Communication Disorders under Award R21DC017214 to V. M. We would like to thank the many people who completed the online survey distributed by the American Tinnitus Association.
Funding Statement
This work was partly funded by the National Institute on Deafness and Other Communication Disorders under Award R21DC017214 to V. M.
References
- Anzivino, R. , Sciancalepore, P. , Petrone, P. , D'Ella, A. , Petrone, D. , & Quaranta, N. (2020). Tinnitus revival during COVID-19 lockdown: How to deal with it? European Archives of Oto-Rhino-Laryngology, 28, 295–296. https://doi.org/10.1007/s00405-020-06147-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beukes, E. W. , Baguley, D. M. , Allen, P. M. , Manchaiah, V. , & Andersson, G. (2018). Audiologist-guided internet-based cognitive behavior therapy for adults with tinnitus in the United Kingdom: A randomized controlled trial. Ear and Hearing, 39(3), 423–433. https://doi.org/10.1097/AUD.0000000000000505 [DOI] [PubMed] [Google Scholar]
- Beukes, E. W. , Baguley, D. M. , Jacquemin, L. , Lourenco, M. P. C. G. , Allen, P. A. , Onozuka, J. , Stockdale, D. , Kaldo, V. , Andersson, G. , & Manchaiah, V. (2020). Changes in tinnitus experiences during the COVID-19 pandemic. Frontiers in Public Health, 8, 592878. https://doi.org/10.3389/fpubh.2020.592878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beukes, E. W. , Fagelson, M. , Aronson, E. P. , Munoz, M. F. , Andersson, G. , & Manchaiah, V. (2020). Readability following cultural and linguistic adaptations of an internet-based intervention for tinnitus for use in the United States. American Journal of Audiology, 29(2), 97–109. https://doi.org/10.1044/2019_AJA-19-00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beukes, E. W. , Manchaiah, V. , Allen, P. M. , Baguley, D. M. , & Andersson, G. (2019). Internet-based interventions for adults with hearing loss, tinnitus, and vestibular disorders: A systematic review and meta-analysis. Trends in Hearing, 23, 2331216519851749. https://doi.org/10.1177/2331216519851749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beukes, E. W. , Manchaiah, V. , Andersson, G. , Allen, P. M. , Terlizzi, P. M. , & Baguley, D. M. (2018). Situationally influenced tinnitus coping strategies: A mixed methods approach. Disability and Rehabilitation, 40(24), 2884–2894. https://doi.org/10.1080/09638288.2017.1362708 [DOI] [PubMed] [Google Scholar]
- Bhatt, J. , Harrison, W. , Lin, M. , & Bhattacharyya, M. (2016). Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngology—Head & Neck Surgery, 142(10), 959–965. https://doi.org/10.1001/jamaoto.2016.1700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Shunnar, S. K. , Hoare, D. J. , Smith, S. , Gander, P. E. , Kang, S. , Fackrell, K. , & Hall, D. A. (2011). Primary care for tinnitus: practice and opinion among GPs in England. Journal of Evaluation in Clinical Practice, 17(4), 684–692. https://doi.org/10.1111/j.1365-2753.2011.01696.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fludra, M. , Kobosko, J. , Gos, E. , Karendys-Łuszcz, K. , & Skarżyński, H. (2020). Role of personal resources from the perspective of experiencing tinnitus annoyance in adults. European Archives of Oto-Rhino-Laryngology, 277, 1617–1623. https://doi.org/10.1007/s00405-020-05843-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollander, J. E. , & Carr, B. G. (2020). Virtually perfect? Telemedicine for COVID-19. New England Journal of Medicine, 382(18), 1679–1681. https://doi.org/10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- Loughrey, D. G. , Kelly, M. E. , Kelley, G. A. , Brennan, S. , & Lawlor, B. A. (2018). Association of age-related hearing loss with cognitive function, cognitive impairment, and dementia: A systematic review and meta-analysis. JAMA Otolaryngology—Head & Neck Surgery, 144(2), 115–126. https://doi.org/10.1001/jamaoto.2017.2513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchaiah, V. , & Beukes, E. W. (2020). How to develop and deliver an audiological internet-based intervention. The Hearing Journal, 23, 2020. https://journals.lww.com/thehearingjournal/blog/onlinefirst/pages/post.aspx?PostID=61 [Google Scholar]
- Manchaiah, V. , Valescu, G. , Varadaraj, S. , Aronson, E. P. , Fagelson, M. A. , Munoz, M. F. , Andersson, G. , & Beukes, E. W. (2020). Features, functionality, and acceptability of internet-based cognitive behavioral therapy for tinnitus in the United States. American Journal of Audiology, 29(3), 476–490. https://doi.org/10.1044/2020_AJA-20-00002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurek, B. , Boecking, B. , & Brueggemann, P. (2019). Association between stress and tinnitus—New aspects. Otology & Neurotology, 40(4), e467–e473. https://doi.org/10.1097/MAO.0000000000002180 [DOI] [PubMed] [Google Scholar]
- McKenna, L. , Marks, E. M. , Hallsworth, C. A. , & Schaette, R. (2017). Mindfulness-based cognitive therapy as a treatment for chronic tinnitus: A randomized controlled trial. Psychotherapy and Psychosomatics, 86(6), 351–361. https://doi.org/10.1159/000478267 [DOI] [PubMed] [Google Scholar]
- Munro, K. , Uus, K. , Almufarrij, I. , Chaudhuri, N. , & Yioe, V. (2020). Persistent self-reported changes in hearing and tinnitus in post-hospitalisation COVID-19 cases. International Journal of Audiology, 59(12), 889–890. https://doi.org/10.1080/14992027.2020.1798519 [DOI] [PubMed] [Google Scholar]
- Newman, C. W. , Sandridge, S. A. , & Bolek, L. (2008). Development and psychometric adequacy of the screening version of the Tinnitus Handicap Inventory. Otology & Neurotology, 29(3), 276–281. https://doi.org/10.1097/MAO.0b013e31816569c4 [DOI] [PubMed] [Google Scholar]
- Newman, D. , Noh, Y. , Talley, E. , Karimi, S. , & Baldwin, T . (2010). Evaluating topic models for digital libraries. Paper presented at the Proceedings of the 10th Annual Joint Conference on Digital Libraries, Gold Coast, Australia. [Google Scholar]
- Nunez-Mir, G. C. , Iannone, B. V. , Pijanowski, B. C. , Kong, N. , & Fei, S. (2016). Automated content analysis: Addressing the big literature challenge in ecology and evolution. Methods in Ecology and Evolution, 7(11), 1262–1272. https://doi.org/10.1111/2041-210X.12602 [Google Scholar]
- Pryce, H. , Hall, A. , Shaw, R. , Culhane, B. A. , Swift, S. , Straus, J. , & Claesen, B. (2018). Patient preferences in tinnitus outcomes and treatments: A qualitative study. International Journal of Audiology, 57(10), 784–790. https://doi.org/10.1080/14992027.2018.1484184 [DOI] [PubMed] [Google Scholar]
- Pryce, H. , Moutela, T. , Bunker, C. , & Shaw, R. (2019). Tinnitus groups: A model of social support and social connectedness from peer interaction. British Journal of Health Psychology, 24(4), 913–930. https://doi.org/10.1111/bjhp.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum, L. (2020). The untold toll—The pandemic's effects on patients without COVID-19. The New England Journal of Medicine, 382, 2368–2371. https://doi.org/10.1056/NEJMms2009984 [DOI] [PubMed] [Google Scholar]
- Roy, S. , & Ghosh, P. (2020). Factors affecting COVID-19 infected and death rates inform lockdown-related policymaking. PLOS ONE, 15(10), e0241165. https://doi.org/10.1371/journal.pone.0241165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar, J. , Meisel, K. , Smith, E. , Quiggle, A. , McCoy, D. , & Amans, M. (2019). Depression in patients with tinnitus: A systematic review. Otolaryngology—Head & Neck Surgery, 161(1), 28–35. https://doi.org/10.1177/0194599819835178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders, G. H. , & Roughley, A. (2020). Audiology in the time of COVID-19: Practices and opinions of audiologists in the UK. International Journal of Audiology, 1–8. https://doi.org/10.1080/14992027.2020.1814432 [DOI] [PubMed] [Google Scholar]
- Shargorodsky, J. , Curhan, G. , & Farwell, W. (2010). Prevalence and characteristics of tinnitus among US adults. The American Journal of Medicine, 123, 711–718. https://doi.org/10.1016/j.amjmed.2010.02.015 [DOI] [PubMed] [Google Scholar]
- Sinha, S. , Irani, U. D. , Manchaiah, V. , & Bhamla, M. S. (2020). LoCHAid: An ultra-low-cost hearing aid for age-related hearing loss. PLOS ONE, 15(9), e0238922. https://doi.org/10.1371/journal.pone.0238922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, A. E. , & Humphreys, M. S. (2006). Evaluation of unsupervised semantic mapping of natural language with Leximancer concept mapping. Behavior Research Methods, 38(2), 262–279. https://doi.org/10.3758/BF03192778 [DOI] [PubMed] [Google Scholar]
- Swanepoel, D. W. , & Hall, J. W. (2020). Making audiology work during COVID-19 and beyond. The Hearing Journal, 73(6), 20–24. https://doi.org/10.1097/01.HJ.0000669852.90548.75 [Google Scholar]
- Trevis, K. , McLachlan, N. , & Wilson, S. (2018). A systematic review and meta-analysis of psychological functioning in chronic tinnitus. Clinical Psychology Review, 60, 62–86. https://doi.org/10.1016/j.cpr.2017.12.006 [DOI] [PubMed] [Google Scholar]
- Viola, P. , Ralli, M. , Pisani, D. , Malanga, D. , Sculco, D. , Messina, L. , Laria, C. , Aragona, T. , Leopardi, G. , Ursini, F. , Scarpa, A. , Topazio, D. , Cama, A. , Vespertini, V. , Quintieri, F. , Cosco, L. , Cunsolo, E. M. , & Chiarella, G. (2020). Tinnitus and equilibrium disorders in COVID-19 patients: Preliminary results. European Archives of Oto-Rhino-Laryngology, 1–6. https://doi.org/10.1007/s00405-020-06440-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Elm, E. , Altman, D. , Egger, M. , Pocock, S. , Gotzsche, P. , & Vandenbroucke, J. (2007). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. The Lancet, 370(9596), 1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2020). Coronavirus disease 2019 (COVID-19): Situation report. https://www.worldometers.info/coronavirus/
- Zhou, X. , Snoswell, C. L. , Harding, L. E. , Bambling, M. , Edirippulige, S. , Bai, X. , & Smith, A. C. (2020). The role of telehealth in reducing the mental health burden from COVID-19. Telemedicine and e-Health, 26(4), 377–379. https://doi.org/10.1089/tmj.2020.0068 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.