Abstract
Objective:
Test differential prospective prediction of growth in externalizing behavior, including oppositional defiant disorder (ODD), conduct disorder (CD) and substance use disorders (SUDs), by earlier hyperactive-impulsive (HI) versus inattentive (IN) symptoms of attention-deficit/hyperactivity disorder (ADHD).
Method:
Participants in the Longitudinal Assessment of Manic Symptoms (LAMS) Study (N=685 at study entry), including 458 boys and 227 girls ages 6–12, completed full parent- and self-report assessments every year for eight years on the Kiddie Schedule for Affective Disorders and Schizophrenia. Three sets of analyses were conducted. First, hierarchal regression (block entry) was used to test independent associations between (a) HI symptoms and later externalizing outcomes, controlling for IN symptoms, and (b) IN symptoms and later externalizing outcomes, controlling for HI symptoms. Second, logistic regression was used to test progression of DSM externalizing disorders. Third, tests of mediation were used to assess potentiation of externalizing progression through environmental risk mediators (eg, family environment, neighborhood violence).
Results:
Consistent with hypotheses derived from trait impulsivity theories of externalizing behavior, HI symptoms were associated independently with long-term externalizing outcomes, whereas IN symptoms were not. Between months 48 and 96, ADHD-HI/C diagnoses predicted later ODD diagnoses, ODD diagnoses predicted later CD diagnoses, and CD diagnoses predicted later SUD diagnoses. Evidence for environmental risk mediation (eg, parental monitoring, neighborhood violence) was also found.
Conclusion:
Findings support trait impulsivity models of externalizing progression, whereby ADHD-HI/C predisposes to increasingly severe externalizing behaviors, which are magnified in contexts of environmental risk.
Keywords: ADHD, conduct disorder, externalizing, impulsivity, inattention
Introduction
Traditionally, externalizing behavior disorders including attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), conduct disorder (CD), substance use disorders (SUDs), and antisocial personality disorder (ASPD) have been treated as distinct, as instantiated in the DSM-5.1 However, high rates of both concurrent and sequential comorbidity of externalizing disorders are well characterized. In fact, progression of increasingly severe externalizing disorders across the lifespan has been described for over 50 years2,3,4,5,6, and verified longitudinally.7
Prominent theoretical models attribute concurrent comorbidity and externalizing progression to shared genetic liability to impulsivity and its interactions with environmental risk.8,9,10 Behavioral genetics studies of child, adolescent, and adult samples invariably yield a single, highly heritable trait on which all externalizing syndromes load.9,11 Certain environmental risk factors, such as abuse, maltreatment, and neighborhood violence, can potentiate this genetic liability to “pull” some individuals along the externalizing spectrum.12 Such theories are supported by twin studies showing that comorbidity among ADHD, ODD, and CD is explained by both genetic vulnerability and shared environmental risk.13 Thus, in many cases, externalizing progression might best be understood as a series of pathoplastic expressions of disease etiology whereby a single, multifactorial genetic trait—expressed as impulsivity—is shaped by potentiating environments into different presentations across development (ADHD, ODD, CD, SUDs, ASPD).8,14
According to trait impulsivity theory, genetic liability to externalizing disorders and externalizing progression is expressed as early as preschool by temperamental irritability, negative affectivity, and poor inhibitory control.15,16 This trait predisposes affected individuals specifically to hyperactive-impulsive (HI) symptoms of ADHD. Etiologically, this pathway is linked to low tonic and low phasic midbrain dopamine (DA) responding8,17, well-replicated neural correlates of ADHD18. Although this neurodevelopmental vulnerability gives rise to both the ADHD-HI and ADHD combined (C) presentations19, inattentive (IN) symptoms are presumed to arise secondarily to hyperactivity-impulsivity. In contrast, the primarily ADHD-IN pathway involves fronto-parietal dysfunction20, which yields direct (versus secondary) development of inattention. The etiological distinction between ADHD-HI/C and ADHD-IN is supported by bifactor structural models that show strong associations between ODD and HI symptoms but not between ODD and IN symptoms.21 Moreover, network analyses identify impulsivity—not inattention—as a core mechanism underlying increasingly severe externalizing symptoms in cross-sectional studies spanning early childhood to adolescence.22
Despite empirical support for trait impulsivity theory, more longitudinal research is needed. Existing research comprises mostly short-term studies of limited size. These studies show that (1) ADHD-HI/C confers vulnerability to externalizing progression, over-and-above effects of ADHD-IN7, (2) ADHD-HI/C usually precedes emergence of ODD5,23, and (3) ODD confers prospective vulnerability to CD6,24 (see Supplement 1, available online, for expanded discussion). These findings are consistent with the progression of externalizing disorders specified above.8,6,7 Nevertheless, validation is needed in large, prospective samples. Tests of the theory may have important implications for targeted prevention among vulnerable children with ADHD-HI/C.
In this study, we test trait impulsivity theory in the Longitudinal Assessment of Manic Symptoms (LAMS) Study25, described below. We note that other externalizing etiologies exist26,27. Here, however, we test the trait impulsivity pathway by evaluating whether (1) HI symptoms predict later development of ODD, CD, and SUDs, over-and-above IN symptoms; (2) IN symptoms predict later development of ODD, CD, and SUDs, over-and-above HI symptoms; (3) progression of externalizing disorders follows a pattern from ADHD-HI/C→ODD→CD→SUDs; and (4) externalizing progression is mediated by environmental risk factors, including parenting, stressful life events, and neighborhood violence. Based on literature cited above, we expected HI but not IN symptoms to predict independent variance in future externalizing behaviors, and environmental risk factors to potentiate (mediate) such effects.
Method
Sample
Participants were recruited from nine child outpatient mental health clinics in the Midwestern U.S.25 Children ages 6–12 years were screened for symptoms of mania using the Parent General Behavior Inventory 10-item Mania Scale (PGBI-10M).28 Children who scored ≥ 12 were invited to participate. A smaller sample of children matched on age, sex, and race who scored ≤ 11 served as controls. Following explanation of procedures, 707 children (621 with elevated PGBI-10M scores, 86 controls) enrolled. These groups did not differ on rates of any psychiatric diagnosis29. Parental consent and child assent for data collection and publication were obtained using local IRB-approved procedures. Following baseline assessments, 685 children were eligible for the longitudinal phase (22 were excluded for autism, IQ<70, or family relocation). Demographics of the full sample appear in Table 1. Although children were not recruited for ADHD, most (n=527, 76.9%) met criteria at study entry. Among them, 66% met criteria for ADHD-HI/C, 20% met criteria for ADHD-IN and 13% met criteria for ADHD-NOS. Children were assessed annually using the full Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS)30 for up to 10 years (six-month assessments did not include all K-SADS modules and are not used here).31 For this study, eight years of data were available. Thus, long-term follow-up refers to 96-month assessments. Most variables at baseline had < 5% missing. By month 96, data from almost half of participants (n=329, 48%) were missing. We discuss imputation procedures and analytic approaches to handling missing data below.
Table 1:
Demographics at Baseline
| Variable | M | SD | N | % |
|---|---|---|---|---|
| Age in years | 9.40 | 1.93 | ||
| Sex | ||||
| Male | 458 | 66.86 | ||
| Female | 227 | 33.14 | ||
| Race | ||||
| White | 442 | 64.53 | ||
| Black/African American | 210 | 30.66 | ||
| Asian | 6 | 8.76 | ||
| Native Hawaiian/Other Pacific Islander | 2 | 0.29 | ||
| American Indian/Alaska Native | 24 | 3.50 | ||
| Missing | 1 | 0.15 | ||
| Ethnicity | ||||
| Not Hispanic or Latino | 654 | 95.47 | ||
| Hispanic or Latino | 31 | 4.53 | ||
| Household educationa | 7.25 | 4.29 | ||
| Household incomeb | 1.96 | 2.17 | ||
| Wechsler IQ score | 98.40 | 15.78 |
Note:
Education indexed as sum of high school education (1=some high school, 2=general education diploma (GED), 3=high school diploma) plus years of college and graduate programs for primary and secondary caregivers.
Family income based on an 8-point scale ranging from 1=$0–$19,000 through 8>$200,000.
Baseline descriptive statistics for participants diagnosed with ADHD-HI/C, and comparisons between these participants and all others in the sample on measures of psychopathology and environmental risk appear in Supplement 1 and Tables S1–S3, available online. Among 52 contrasts, 2 were significant. These included 1 of 8 DSM-IV mood disorders (those diagnosed with ADHD-HI/C scored lower) and neighborhood violence (those diagnosed with ADHD-HI/C experienced less).
Measures
Child Functioning and Psychopathology
The K-SADS assessed DSM externalizing syndromes. Additional items assessing mood disorders and pervasive developmental disorders were added from the Washington University (WASH-U)-K-SADS.32 Interviews were administered separately to children and caregivers by trained interviewers. Test-retest reliabilities were good to excellent for clinical diagnoses.30 Symptoms were rated on 0–3 point ordinal scales anchored from not present to above clinical threshold. All participants were administered the main K-SADS section, which includes screening symptoms for all diagnoses. Participants who received clinically elevated scores on screening variables were administered supplemental sections with remaining diagnostic criteria for behavior disorders, anxiety, SUDs, etc. Participants who completed the main K-SADS but were not administered supplemental sections were assigned “not present” values for those symptoms. KSADS summary items used for analyses were derived from combinations of parent- and child-reports based on expert judgements (clinical decisions) of licensed psychiatrists and/or psychologists, who also rendered consensus diagnoses. Externalizing diagnoses include ADHD-HI/C, ODD, CD, and SUDs. We analyze both dimensional scores (summary of symptom ratings) and diagnoses for all externalizing disorders and ADHD-IN.
Children’s IQs were assessed using the Children’s Wechsler Abbreviated Scale of Intelligence (WASI).33 The WASI is validated for ages 6–89 years. We used full-scale IQs (FSIQ).
Parent Behavior
The Parent Stress Survey (PSS)34 assesses severity of parental stress across 25 self-report, Likert-type items ranging from 0 (not at all stressful) to 4 (very stressful). Previous analyses in this sample found high internal consistency, α=.91.31
The Parent Monitoring Form (PMF)35 assesses whether parents/caregivers know where their children are, and with whom and how they spend free time. PMF scores correlate with police contacts and delinquent behaviors.35 PMF collection began at month 60.
Environment
Participants reported demographic information at baseline including age, sex, race, ethnicity, etc. Socioeconomic status was indexed by (1) annual household income (8-point scale from $0–19,000 to >$200,000) and (2) household educational attainment (0=no high school to 12=post-secondary education).36
The Stressful Life Events Schedule for Children and Adolescents (SLES)37 is a parent- and child-report measure of 80 stressful life events and their effects on children during the past 12 months. Parent and child agreement on occurrence of severe events is acceptable (κ=.73). The SLES demonstrates convergent validity with related measures.37 We used life events including parent-reported neighborhood violence, child-reports of being caught committing crimes, and a composite of stressful events endorsed by parents.
Results
Descriptive Statistics
Children’s mean age at baseline was 9.4 years (range=6–12; see Table 1). The sample was 66.9% male and 64.5% white. Mean annual family income was between $40,000–$80,000. For 48.3% of families, the primary and/or secondary caretaker completed at least some college. For 10.0% of families, neither the primary nor secondary guardian/caretaker finished high school. Boys (M=9.26, SD=1.89) were slightly younger than girls (M=9.68, SD=1.98, d=0.21). Ethnicity was not associated with age, sex, SES, or IQ. Family income and education were correlated with IQ, r=.23, p<.001 and r=.36, p<.001, respectively.
Table 2 shows frequencies of diagnoses at each assessment. Participants scored very high on externalizing disorders at baseline. Over three-quarters (76.9%) received an ADHD diagnosis (51.1% ADHD-HI/C, 15.6% ADHD-IN, 10.2% ADHD-NOS (DSM-IV criteria). In addition, 35.2% of participants received an ODD diagnosis at baseline and 7.6% received a CD diagnosis. None received SUDs diagnoses. Sample-wide, rates of ADHD, ODD, and CD decreased over time, whereas SUDs increased. Increases and decreases in diagnoses over time were not due to selective attrition (see below).
Table 2:
Frequencies of Kiddie Schedule for Affective Disorders and Schizophrenia Diagnoses at Each Assessment
| Disorder | Baseline | Month | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 12 | 24 | 36 | 48 | 60 | 72 | 84 | 96 | ||
| N(%) | N(%) | N(%) | N(%) | N(%) | N(%) | N(%) | N(%) | N(%) | |
| ADHD-HI/C | 350(51.1) | 193(36.8) | 151(32.3) | 137(31.1) | 104(24.5) | 93(23.3) | 90(23.7) | 67(13.7) | 58(16.3) |
| ADHD-IN | 107(15.6) | 129(24.6) | 113(24.2) | 90(20.5) | 98(23.1) | 74(18.5) | 84(22.2) | 76(15.5) | 79(22.2) |
| ADHD-NOS | 70(10.2) | 64(12.2) | 71(15.2) | 59(13.4) | 62(14.6) | 55(13.8) | 41(10.8) | 44(9.0) | 33(9.3) |
| ODD | 241(35.2) | 151(28.8) | 125(26.8) | 99(22.5) | 89(21.0) | 67(16.8) | 69(18.2) | 56(11.5) | 47(13.2) |
| CD | 52(7.6) | 23(4.4) | 22(4.7) | 24(5.5) | 26(6.1) | 25(6.3) | 15(4.0) | 20(4.1) | 17(4.8) |
| SUD | 0(0.0) | 0(0.0) | 0(0.0) | 5(1.1) | 5(1.2) | 6(1.5) | 7(1.8) | 14(2.9) | 24(6.7) |
| Missing (%) | 0(0.0) | 160(23.4) | 218(31.8) | 245(35.8) | 261(38.1) | 286(41.8) | 306(44.7) | 196(28.6) | 329(48.0) |
Note: ADHD-HI/C=attention-deficit/hyperactivity disorder hyperactive-impulsive/combined subtypes; ADHD-IN=ADHD inattentive subtype; ADHD-NOS=ADHD not otherwise specified; CD=conduct disorder; ODD=oppositional defiant disorder; SUD=substance use disorder.
Analytic Plan and Missing Data
Analyses proceeded in three phases. First, hierarchal regressions (block entry) tested independent associations between (a) HI symptoms and later externalizing outcomes, controlling for IN symptoms, and (b) IN symptoms and later externalizing outcomes, controlling for HI symptoms. Second, logistic regressions tested progression of DSM-IV disorders, including ADHD-HI/C, ODD, CD, and SUDs. Third, mediational analyses tested potentiating effects on externalizing progression by environmental risk factors (parenting, stressful life events).
Before conducting analyses, we evaluated attrition. By long-term follow-up, up to 329 (48%) participants had missing data on certain variables (Table 2). Attritted participants reported higher baseline parent-child relationship dysfunction, t(682)=2.31, p=.021, d=0.18. However, neither K-SADS symptoms nor diagnoses differed at baseline between children who remained versus those lost to attrition. Nevertheless, we replaced missing data via 30 imputations in SPSS 25, consistent with current standards.38
Hyperactive-Impulsive Versus Inattentive Symptoms and Externalizing Progression
To evaluate independent effects of baseline HI and IN symptoms on 96-month externalizing behaviors, we used a block entry approach in which K-SADS ODD, CD, and SUD symptoms were outcomes. For Block 1, symptoms were predicted by/adjusted for covariates including (1) age at study entry given that participants varied in age (6 to 12 years) at enrollment and given that ADHD-HI/C participants were slightly younger than others (see Table S1, available online); (2) sex, given generally higher rates of externalizing among boys vs. girls and given that there was a higher proportion of boys in the ADHD-HI/C subsample (see Table S1, available online); (3) SES, given slightly lower family income and parental education for the ADHD-HI/C subsample (see Table S1, available online); (4) race/ethnicity, which often correlates with SES; and (5) IQ, which often correlates inversely with externalizing scores.
For Block 2, baseline K-SADS ADHD-IN symptoms were added to the model. For Block 3, baseline ADHD-HI symptoms were added to test their unique contribution to later ODD, CD, and SUDs. We then repeated this approach, exchanging order of entry for ADHD-HI and ADHD-IN symptoms, to test the unique contribution of ADHD-IN to later ODD, CD, and SUDs. A similar approach has been used previously.7
Results appear in Table 3. Although effect sizes were modest, baseline HI symptoms accounted for significant variance in 96-month ODD and CD symptoms, whereas IN symptoms did not, consistent with hypotheses. Neither HI nor IN symptoms accounted for SUD symptoms at 96-month follow-up. Of note, however, predictive power was limited because only 6.7% of participants reported a SUD at follow-up.
Table 3:
Block Regressions Predicting Externalizing Symptoms at 96 Months by Baseline Hyperactive-Impulsive and Inattentive Symptoms of Attention-Deficit/Hyperactivity Disorder
| 96-month | Baseline model (covariates only)a | IN symptoms added first HI symptoms added last | HI symptoms added first IN symptoms added last | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | F | df | P | R 2 | ΔF | p | β | ΔR2 | ΔF | p | β | ΔR2 |
| K-SADS ODD symptoms | 5.79 | 8,665 | < .001 | .05 | 5.63 | .018 | 0.15 | .01 | 1.20 | .273 | −0.07 | < .01 |
| age* | ||||||||||||
| sex | ||||||||||||
| SES (income, parent education) race/ethnicity | ||||||||||||
| KBIT IQ* | ||||||||||||
| K-SADS CD symptoms | 3.09 | 8,665 | .002 | .04 | 7.58 | .006 | 0.18 | .01 | 1.95 | .164 | −0.09 | < .01 |
| age | ||||||||||||
| sex | ||||||||||||
| SES (income, parent education) race/ethnicity | ||||||||||||
| KBIT IQ | ||||||||||||
| K-SADS SUD symptoms | 5.01 | 8,665 | < .001 | .06 | 0.72 | .398 | −0.06 | <.01 | 1.74 | .187 | 0.08 | < .01 |
| age* | ||||||||||||
| sex* | ||||||||||||
| SES (income, parent education) race/ethnicity | ||||||||||||
| KBIT IQ | ||||||||||||
Notes. CD=conduct disorder; IN=inattention; HI-hyperactivity-impulsivity; KBIT=Kaufman Brief Intelligence Test; K-SADS = Kiddie Schedule for Affective Disorders and Schizophrenia. ODD=oppositional defiant disorder; SES=socioeconomic status; SUD=substance use disorder;.
All models included age at study entry, sex, SES, race/ethnicity, and IQ as covariates (see text for details).
p < .05 in baseline model.
Progression of Categorical Disorders
To evaluate progression of externalizing diagnoses (versus symptoms), we first ran a logistic regression in which we entered baseline externalizing diagnoses to predict externalizing diagnoses at month 96—a strategy used in previous studies.39 The only significant finding was baseline ADHD-HI/C predicting 96-month ODD, OR=1.97, CI=1.02–3.78, p=.043. These null results were unexpected given well-established prospective associations among externalizing disorders, as reviewed above. As shown in Table 2, however, rates of ADHD-HI/C diagnoses decreased after baseline, which is not unusual in studies of highly symptomatic youth40, who often fluctuate above and below diagnostic thresholds over time. In this study, decreases in ADHD-HI/C diagnoses worked against tests of externalizing progression, and may account for limited effect sizes observed. We therefore ran two additional logistic regressions. In the first, we entered baseline externalizing diagnoses in predicting future externalizing diagnoses at month 48. In the second, we entered month 48 externalizing diagnoses in predicting future externalizing diagnoses at month 96. Odds ratios, adjusted for previous comorbidity, appear in Table 4. For 0- to-48 month regressions, no evidence of externalizing progression was found. In contrast, 48-to-96 month regressions showed significant prediction of ODD by earlier ADHD-HI/C, CD by earlier ODD, and SUDs by earlier CD (all ORs≥2.69, all ps≤.038). Thus, from 48–96 months, each externalizing disorder predicted a later, more severe externalizing disorder (ADHD-HI→ODD→CD→SUDs). Of note, CD diagnoses at month 48 also predicted ADHD-HI/C diagnoses at month 96.
Table 4:
Continuity and Progression of Externalizing Diagnoses from Baseline to Month 48 and From Month 48 to Month 96
| Baseline diagnosis | Month 48 diagnosis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADHD-HI/C (n=104) | ODD (n=89) | CD (n=26) | SUD (n=5) | |||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| ADHD-HI/C (n=350) | - | - | - | 1.12 | 0.68–1.82 | .659 | 1.39 | 0.56–3.47 | .481 | N/A | N/A | N/A |
| ODD (n=241) | 1.32 | 0.82–2.13 | .260 | - | - | - | 1.46 | 0.48–4.43 | .505 | N/A | N/A | N/A |
| CD (n=52) | 2.40 | 1.08–5.34 | .032 | 3.22 | 1.35–7.70 | .009 | - | - | - | N/A | N/A | N/A |
| SUD (n=0) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | - | - | - |
| Month 48 diagnosis | Month 96 diagnosis | |||||||||||
| ADHD-HI/C (n=58) | ODD (n=47) | CD (n=17) | SUD (n=24) | |||||||||
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| ADHD-HI/C (n=104) | - | - | - | 2.69 | 1.33–5.44 | .006 | 1.15 | 0.37–3.61 | .805 | 0.52 | 0.15–1.82 | .304 |
| ODD (n=89) | 0.97 | 0.44–2.12 | .935 | - | - | - | 5.24 | 1.61–17.12 | .006 | 1.70 | 0.61–4.74 | .314 |
| CD (n=26) | 2.89 | 0.95–8.78 | .061 | 10.08 | 3.55–28.63 | <.001 | - | - | - | 3.78 | 1.08–13.28 | .038 |
| SUD (n=5) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | - | - | - |
Note. All diagnoses derived from the Kiddie Schedule for Affective Disorders and Schizophrenia (see text for details). N/A indicates no diagnoses or no comorbid associations to predict later diagnoses. ADHD-HI/C=attention-deficit/hyperactivity disorder hyperactive-impulsive/combined subtypes; ADHD-IN=ADHD inattentive subtype; CD=conduct disorder; ODD=oppositional defiant disorder; OR=odds ratio. SUD=substance use disorder;
Mediation of Externalizing Progression
Finally, we assessed progression of externalizing disorders through environmental risk mediators. Given differentially relevant mediators based on age (see above)8, we conducted three sets of analyses. The first assessed mediating effects of parent-child relationship dysfunction and parental stress on progression of externalizing from baseline to month 48.41 The second assessed mediating effects of neighborhood violence and reported crimes on progression of externalizing from months 48 to 96.12 The third assessed mediating effects of parental monitoring on progression of SUDs from months 72 to 96 (parental monitoring was not assessed at earlier timepoints).42 We report all outcomes for K-SADS symptoms and diagnoses in Table 5. No additional mediational models were run that are not reported. We used the SPSS MEMORE macro, which assesses longitudinal relations between earlier predictors and later outcomes through change in putative mediators over time.43
Table 5:
Mediational Effects of Relations Between Hyperactive-Impulsive Symptoms of Attention-Deficit/Hyperactivity Disorder and Later Symptoms and Diagnoses
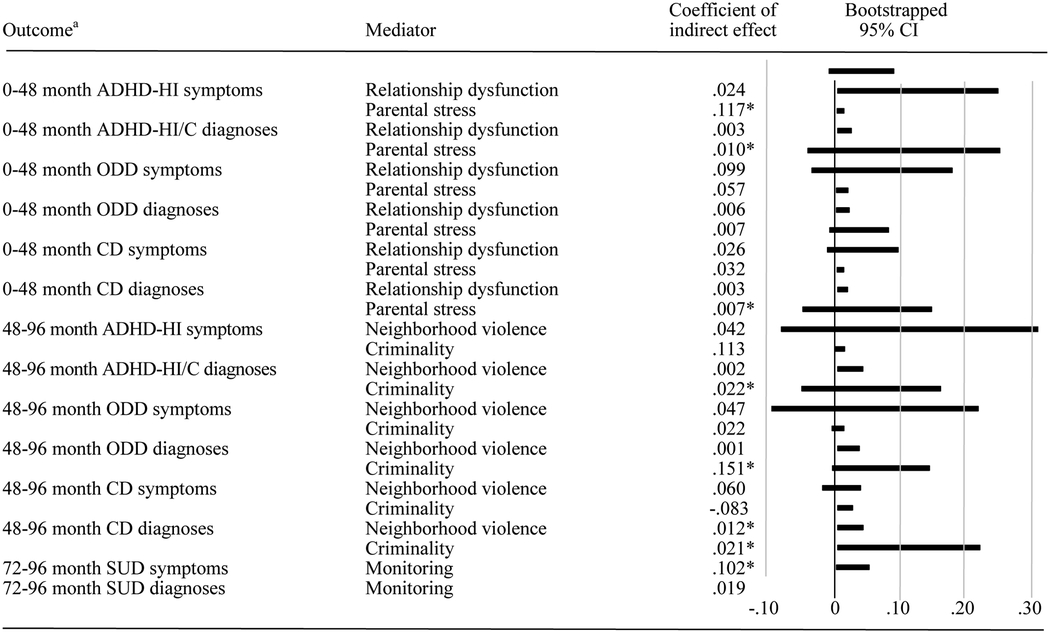
|
Note: All symptoms and diagnoses from the Kiddie Schedule for Affective Disorders and Schizophrenia (see text for details). MEMORE43 assesses whether change in a mediator (e.g., parental stress) over time (e.g., months 0–48) accounts for the association between an independent variable (e.g., ADHD-HI/C at month 0) and a dependent variable (eg, CD at month 48). Data for all mediators across all 685 participants appear in Table S4, available online. ADHD-HI/C=attention-deficit/hyperactivity disorder hyperactive-impulsive/combined subtypes; CD=conduct disorder; ODD=oppositional defiant disorder; SUD=substance use disorder.
p <.05.
Several significant mediators were identified. From 0–48 months, parental stress mediated growth in ADHD-HI/C symptom severity and diagnoses, as well as progression of ADHD-HI/C to later CD. From 48–96 months, crime mediated increases in ADHD-HI/C diagnoses and progression of ADHD-HI/C to later ODD and CD. In addition, neighborhood violence mediated progression of earlier ADHD-HI/C to later CD. From 72–96 months, parental monitoring mediated the relation between earlier ADHD-HI/C and increasing SUD symptoms. Although remaining effects were not significant, CIs fell overwhelmingly to the right of zero (Table 5), consistent with previous research.8,12,41,44
Discussion
We evaluated three hypotheses, following from trait impulsivity theory. This perspective suggests that for some individuals, a single, multifactorial genetic liability, expressed early in life as temperamental impulsivity and ADHD-HI/C, predisposes to increasingly severe externalizing disorders across development, especially in contexts of risk8. Our first hypothesis was that baseline ADHD-HI/C would predict 96-month externalizing outcomes, including ODD, CD, and SUDs, over-and-above effects of baseline ADHD-IN, but baseline ADHD-IN would not predict 96-month externalizing outcomes, over-and-above effects of baseline ADHD-HI/C. For both ODD and CD, this hypothesis was supported. Although effect sizes were modest, the timespan of prediction was eight years. Baseline ADHD-HI/C did not predict 96-month SUDs. However, frequency of SUDs was low (6.7%).
Second, we hypothesized progression of externalizing disorders from ADHD-HI/C→ODD→CD→SUDs. This hypothesis was partly supported. Across 48- to 96-month but not 0- to 48-month assessments, ADHD-HI/C predicted later ODD, ODD predicted later CD, and CD predicted later SUDs. Even though ADHD-HI/C predicted later ODD, it did not predict later CD or SUDs when all were in the same model (Table 4). Such is not unexpected for disorders that derive from a common trait given that variance shared by all disorders is statistically removed once the ADHD-HI/C→ODD pathway is accounted for.45 Put another way, if the etiologic pathway is serial, removing the first “leg” of the pathway leaves later legs “cut off”.
We were careful to address directions of externalizing progression. The regressions reported in Tables 3 and 4 demonstrate that (1) ADHD-HI and not ADHD-IN predicted later ODD, CD, and SUDs; and (2) ODD, CD, and SUDs did not predict later ADHD. Thus, ADHD predicts later ODD, not vice versa, similar to previous reports6,23. However, ODD did predict later CD, and CD predicted later SUDs. We tested these pathways explicitly, controlling for other disorders in the model. Because the models in Table 4 control for previous diagnoses, they evaluate diagnostic progression, over-and-above diagnostic stability.
Finally, we tested whether externalizing progression was mediated by environmental risk. From 0–48 months, parental stress mediated growth in ADHD-HI/C and CD. From 48–96 months, criminality mediated growth in ADHD-HI/C and progression of ADHD-HI/C to later ODD and CD. In addition, neighborhood violence mediated progression of earlier ADHD-HI/C to later CD. From 72–96 months, low parental monitoring mediated growth in ADHD-HI/C and SUDs. These mediators were chosen for specific age ranges following existing research.8,12,41,42 Confidence intervals for remaining mediational effects, though not significant, skewed heavily to the right of zero. Of note, our tests of mediation followed from theory, and we did not test other possible mediation models (e.g., whether child symptom progression mediated relations between family function and later child diagnoses).
In sum, marked but not full support was found for the notion that common liability—expressed as trait impulsivity—portends externalizing progression, which is amplified by environmental risk. To our knowledge, this is the second study to test the entire ADHD→ODD→CD→SUDs pathway. The first supported the pathway in a girls-only sample.7 Our findings extend previous research by capitalizing on a rich sample of children, most of whom were affected by ADHD, across eight years.
We cannot eliminate the possibility of passive gene-environment correlation. In such situations, genes shared by parents and children influence home environments, including parenting. Genetically vulnerable parents may also be more likely to live in disadvantaged/violent neighborhoods, thereby conferring both genetic and environmental risk to their children. This could in part account for links between ADHD-HI/C and later CD.
One important limitation is the decline in ADHD-HI/C diagnoses following baseline assessments. LAMS participants were highly symptomatic at baseline (76.9% were diagnosed with a DSM-IV subtype of ADHD). Regression to mean is expected over time as symptoms fluctuate—often above and below diagnostic thresholds.40 High scores at intake also produce ceiling effects and restrict range, which may have worked against some hypotheses. In addition, LAMS participants were not recruited with these hypotheses in mind. Instead, they were recruited based on manic symptoms. Nevertheless, very few developed a bipolar spectrum disorder.46
Those who reported higher parent-child relationship dysfunction were more likely to drop out, and almost half of the original sample was lost to attrition by month 96. However, baseline K-SADS symptoms and diagnoses were unrelated to attrition. Nevertheless, we used state-of-the art imputation procedures that minimize bias. That said, better retention would have been ideal, however difficult across eight years.
It is also possible that ongoing treatment affected results. Participants from multiple LAMS sites were recruited from clinics where they initiated treatment. This may have dampened diagnostic progression, working against hypotheses. Given a clinical sample, generalization to community youth with externalizing psychopathology should be made with caution.
Finally, recent research identifies irritability as a transdiagnostic feature of externalizing (and other) disorders47. Some neuroscientific accounts identify common neural mechanisms of irritability (an emotion) and impulsivity (a behavior). According to these models, impulsive behavior is sometimes motivated by irritable mood and emotion48. Because LAMS was planned prior to the current upsurge in irritability research, no validated measure of irritability was included. We chose not to derive a patchwork measure and instead evaluated traits for which well-validated measures were available.
Data from LAMS provided an opportunity to evaluate hypotheses related to trait impulsivity theory of externalizing progression across eight years. Externalizing diagnoses exhibited substantial continuity, and evidence of symptom progression was found. Several mediators of externalizing progression identified in previous, short-term longitudinal studies were also confirmed despite less precise measures (parent-reports not direct observations). Findings extend existing literature, and point toward the need to intervene early in life among young children with ADHD-HI/C. Reversing established conduct problems more difficult than preventing them among vulnerable children using family interventions.49 We hope findings presented herein contribute to earlier diagnosis and treatment.
Supplementary Material
Acknowledgments
The manuscript is a publication of secondary analyses from a multi-site study supported by the National Institute of Mental Health (NIMH); Case Western Reserve University: R01 MH073967-06A1, Cincinnati Children’s Hospital Medical Center: R01 MH073816-06A1, The Ohio State University: R01 MH073801-06A1, and University of Pittsburgh: R01 MH073953-06A1. Preparation of this article was also supported by Grants UH2DE025980 and UL1TR002733 from the National Institutes of Health (NIH).
The research was performed with permission from Ohio State’s Biomedical Sciences Institutional Review Board #00000294.
Drs. Beauchaine and Youngstrom served as the statistical experts for this research.
Disclosure:
Dr. Fristad has reported research support from Janssen, royalties from American Psychiatric Publishing, Child and Family Psychological Services, Guilford Press, and JandK Seminars, and travel support from the Society of Clinical Child and Adolescent Psychology. Dr. Youngstrom has consulted about psychological assessment with Pearson, Janssen, Lundbeck, and Western Psychological Services. He has received royalties from the American Psychological Association and Guilford Press and has received funding from NIH. He is the co-founder and CEO of Helping Give Away Psychological Science (HGAPS.org), a 501c3. Dr. Arnold has received research funding from Curemark, Forest, Eli Lilly and Co., Neuropharm, Novartis, Noven, Otsuka, Roche/Genentech, Shire (a Takeda company), Supernus, YoungLiving, NIH, and Autism Speaks, has consulted with Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD), Neuropharm, Organon, Pfizer, Sigma Tau, Shire, Tris Pharma, and Waypoint, and has been on advisory boards for Arbor, Ironshore, Novartis, Noven, Otsuka, Pfizer, Roche, Seaside Therapeutics, Sigma Tau, and Shire. Dr. Beauchaine has received speaking honoraria and book royalties from Wiley and Oxford University Press for related work. Dr. Bell has reported no biomedical financial interests or potential conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Press; 2013. doi: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 2.Robins LN, Deviant children grown up. Williams & Wilkins; 1966. doi: 10.1007/BF00538543 [DOI] [PubMed] [Google Scholar]
- 3.Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychol Rev. 1993;100:674–701. doi: 10.4324/9781315096278-3 [DOI] [PubMed] [Google Scholar]
- 4.Storebø OJ, Simonsen E. The association between ADHD and antisocial personality disorder (ASPD): A review. J Atten Disord. 2016;20:815–824. doi: 10.1177/1087054713512150 [DOI] [PubMed] [Google Scholar]
- 5.Loeber R, Burke JD. Developmental pathways in juvenile externalizing and internalizing problems. J Res Adolesc. 2011;21:34–46. doi: 10.1111/j.1532-7795.2010.00713.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nock MK, Kazdin AE, Hiripi E, Kessler RC. Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: Results from the National Comorbidity Survey Replication. J Child Psychol Psychiatry. 2007;48:703–713. doi: 10.1111/j.1469-7610.2007.01733.x [DOI] [PubMed] [Google Scholar]
- 7.Ahmad SI, Hinshaw SP. Attention-deficit/hyperactivity disorder, trait impulsivity, and externalizing behavior in a longitudinal sample. J Abn Child Psychol. 2017;45:1077–1089. doi: 10.1007/s10802-016-0226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beauchaine TP, Zisner AR, Sauder CL. Trait impulsivity and the externalizing spectrum. Ann Rev Clin Psychol. 2017;13:343–368. doi: 10.1146/annurev-clinpsy-021815-093253 [DOI] [PubMed] [Google Scholar]
- 9.Krueger RF, Hicks BM, Patrick CJ, et al. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. J Abn Psychol, 2002;111:411–424. doi: 10.1037/0021-843X.111.3.411 [DOI] [PubMed] [Google Scholar]
- 10.Lahey BB, Waldman ID. A developmental propensity model of the origins of conduct problems during childhood and adolescence. In: Lahey BB, Moffitt TE, Caspi A, eds. Causes of conduct disorder and juvenile delinquency. New York, NY: Guilford;2003:76–117. no doi. [Google Scholar]
- 11.Tuvblad C, Zheng M, Raine A, Baker LA. A common genetic factor explains the covariation among ADHD, ODD, and CD symptoms in 9–10-year-old boys and girls. J Abn Child Psychol. 2009;37:153–167. doi: 10.1007/s10802-008-9278-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meier MH, Slutske WS, Arndt S, Cadoret RJ. Impulsive and callous traits are more strongly associated with delinquent behavior in higher risk neighborhoods among boys and girls. J Abn Psychol. 2008;117:377–385. doi: 10.1037/0021-843X.117.2.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burt SA, Krueger RF, McGue M, Iacono WG. Sources of covariation among attention-deficit/hyperactivity disorder, oppositional defiant disorder, and conduct disorder: The importance of shared environment. J Abn Psychol. 2001;110:516–525. doi: 10.1037/0021-843X.110.4.516 [DOI] [PubMed] [Google Scholar]
- 14.Beauchaine TP, Constantino JN, Hayden EP. Psychiatry and developmental psychopathology: Unifying themes and future directions. Compr Psychiat. 2018;87:143–152. doi: 10.1016/j.comppsych.2018.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stringaris A, Maughan B, Goodman R. What’s in a disruptive disorder? Temperamental antecedents of oppositional defiant disorder: Findings from the Avon Longitudinal Study. J Am Acad Child Adolesc Psychiat. 2010;49:474–483. doi: 10.1016/j.jaac.2010.01.021 [DOI] [PubMed] [Google Scholar]
- 16.Beauchaine TP, Tackett JL Irritability as a transdiagnostic vulnerability trait: Current issues and future directions. Behav Ther. 2020;51:350–364. doi: 10.1016/j.beth.2019.10.009 [DOI] [PubMed] [Google Scholar]
- 17.Beauchaine TP, Constantino JN. Redefining the endophenotype concept to accommodate transdiagnostic vulnerabilities and etiological complexity. Biomark Med. 2017;11:769–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plichta MM, Scheres A. Ventral-striatal responsiveness during reward anticipation in ADHD and its relation to trait impulsivity in the healthy population: A meta-analytic review of the fMRI literature. Neurosci Biobehav Rev. 2014;38:125–134. doi: 10.1016/j.neubiorev.2013.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sagvolden T, Johansen EB, Aase H, Russell VA. A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive/impulsive and combined subtypes. Behav Brain Sci. 2005;28:397–419. doi: 10.1017/S0140525X05000075 [DOI] [PubMed] [Google Scholar]
- 20.Fair DA, Nigg JT, Iyer S, et al. Distinct neural signatures detected for ADHD subtypes after controlling for micro-movements in resting state functional connectivity MRI data. Front Systems Neurosci. 2013;6:80. doi: 10.3389/fnsys.2012.00080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burns GL, Geiser C, Servera M, Becker SP, Beauchaine TP. Application of the bifactor S – 1 model to multisource ratings of ADHD/ODD symptoms: An appropriate bifactor model for symptom ratings. J Abn Child Psychol. 2020;48:881–894. doi: 10.1007/s10802-019-00608-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martel MM, Levinson CA, Lee CA, Smith TE. Impulsivity symptoms as core to the developmental externalizing spectrum. J Abn Child Psychol. 2017;45:83–90. doi: 10.1007/s10802-016-0148-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harvey EA, Breaux RP, Lugo-Candelas CI. Early development of comorbidity between symptoms of attention deficit hyperactivity disorder and oppositional defiant disorder. J Abn Psychol. 2016;125:154–167. doi: 10.1037/abn0000090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Servera M, Seijas R, Garcia-Banda G, Barry CT, Beauchaine TP, Burns GL. Longitudinal associations of callous/unemotional and oppositional defiant behaviors over a three-year interval for Spanish children. Dev Psychopathol. 2020;32:481–490. doi: 10.1017/S0954579419000221 [DOI] [PubMed] [Google Scholar]
- 25.Horwitz SM, Demeter C, Pagano ME. et al. Longitudinal Assessment of Manic Symptoms (LAMS) Study: Background, design and initial screening results. J Clin Psychiat. 2010;71:1511–1517. doi: 10.4088/JCP.09m05835yel [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frick PJ. Developmental pathways to conduct disorder. Child Adolesc Psychiatr Clin N Am. 2006;15:311–331. doi: 10.1080/15374416.2012.664815 [DOI] [PubMed] [Google Scholar]
- 27.Gerring JP, Vasa RA. Head injury and externalizing behavior. In: Beauchaine TP, Hinshaw SP, eds. The Oxford handbook of externalizing spectrum disorders. New York, NY: Oxford University Press; 2017:403–415. doi: 10.1093/oxfordhb/9780199324675.013.27 [DOI] [Google Scholar]
- 28.Youngstrom EA, Frazier TW, Demeter C. et al. Developing a 10-Item mania scale from the Parent General Behavior Inventory for children and adolescents. J Clin Psychiat. 2008;69:831–839. doi: 10.4088/JCP.v69n0517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Findling RL, Youngstrom EA, Fristad FA et al. Characteristics of children with elevated symptoms of mania: The Longitudinal Assessment of Manic Symptoms (LAMS) study. J Clin Psychiatr. 2010;71:1664–1672. doi: 10.4088/JCP.09m05859yel [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaufman J, Birmaher B, Brent D, Rao U. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS): Initial reliability and validity data. J Am Acad Child Adolesc Psychiat. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- 31.Van Meter AR, Youngstrom EA, Birmaher B. et al. Longitudinal course and characteristics of cyclothymic disorder in youth. J Affect Disord. 2017;215:314–322. doi: 10.1016/j.jad.2017.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Geller B, Zimerman B, Williams M et al. (2001). Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-K-SADS) mania and rapid cycling sections. J Am Acad Child Adolesc Psychiat. 2001;40:450–455. doi: 10.1097/00004583-200104000-00014 [DOI] [PubMed] [Google Scholar]
- 33.Wechsler D Wechsler abbreviated scale of intelligence. Psychological Corporation; 1999. no doi. [Google Scholar]
- 34.Sisson DP, Fristad MA. Stress and support for parents of children with early-onset bipolar disorder. Isr J Psychiat Relat Sci. 2012;49:104–110. no doi. [PMC free article] [PubMed] [Google Scholar]
- 35.Patterson GR, Stouthamer-Loeber M. The correlation of family management practices and delinquency. Child Dev. 1984;55:1299–1307. no doi. [PubMed] [Google Scholar]
- 36.Diemer MA, Mistry R, Wadsworth ME, López I, Reimers F. Best practices in conceptualizing and measuring social class in psychological research. Analys Soc Issues Pub Policy. 2013;13:77–113. doi: 10.1111/asap.12001 [DOI] [Google Scholar]
- 37.Williamson DE, Birmaher B, Ryan ND. et al. The Stressful Life Events Schedule for children and adolescents: Development and validation. Psychiat Res. 2003;119:225–241. doi: 10.1016/S0165-1781(03)00134-3 [DOI] [PubMed] [Google Scholar]
- 38.Graham JW. Missing data analysis: Making it work in the real world. Ann Rev Psychol. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- 39.Bufferd SJ, Dougherty LR, Carlson GA, Rose S, Klein DN. Psychiatric disorders in preschoolers: Continuity from ages 3 to 6. Am J Psychiatr. 2012;169:1157–1164. doi: 10.1176/appi.ajp.2012.12020268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Atherton OE, Ferrer E, Robins RW. The development of externalizing symptoms from late childhood through adolescence: A longitudinal study of Mexican-origin youth. Dev Psychol. 2018;54:1135–1147. doi: 10.1037/dev0000489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patterson GR, DeGarmo DS, Knutson NM. Hyperactive and antisocial behaviors: Comorbid or two points in the same process? Dev Psychopathol. 2000;12:91–107. doi: 10.1017/s0954579400001061 [DOI] [PubMed] [Google Scholar]
- 42.DiClemente RJ, Wingood GM, Crosby R et al. Parental monitoring: Association with adolescents’ risk behaviors. Pediatrics, 2001;107:1363–1368. doi: 10.1542/peds.107.6.1363 [DOI] [PubMed] [Google Scholar]
- 43.Montoya AK, Hayes AF. Two-condition within-participant statistical mediation analysis: A path-analytic framework. Psych Methods. 2017;22:6–27. doi: 10.1037/met0000086 [DOI] [PubMed] [Google Scholar]
- 44.Mackler JS, Kelleher RT, Shanahan L et al. Parenting stress, parental reactions, and externalizing behavior from ages 4 to 10. J Marriage Fam. 2015;77:388–406. doi: 10.1111/jomf.12163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Beauchaine TP, Hinshaw SP. RDoC and psychopathology among youth: Misplaced assumptions and an agenda for future research. J Clin Child Adolesc Psychol. 2020;49:322–340. doi: 10.1080/15374416.2020.1750022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arnold LE, Demeter C, Mount K. et al. Pediatric bipolar spectrum disorder and ADHD: Comparison and comorbidity in the LAMS clinical sample. Bipolar Disord. 2011;13:509–521. doi: 10.1111/j.1399-5618.2011.00948.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brotman MA, Kircanski K, Leibenluft E. Irritability in children and adolescents. Ann Rev Clin Psychol. 2017;13:317–341. doi: 10.1146/annurev-clinpsy-032816-044941 [DOI] [PubMed] [Google Scholar]
- 48.Zisner A, Beauchaine TP. Neural substrates of trait impulsivity, anhedonia, and irritability: Mechanisms of heterotypic comorbidity between externalizing disorders and unipolar depression. Dev Psychopathol. 2016;28:1179–1210. doi: 10.1017/S0954579416000754 [DOI] [PubMed] [Google Scholar]
- 49.Webster-Stratton C, Reid MJ, Beauchaine TP. One-year follow-up of combined parent and child intervention for young children with ADHD. J Clin Child Adolesc Psychol. 2013;42:251–261. doi: 10.1080/15374416.2012.723263 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


