The number of patients undergoing transcatheter aortic valve replacement (TAVR) has grown over the past decade.1 The incidence of coronary artery disease (CAD) in patients with severe aortic stenosis (AS) undergoing TAVR ranges between 40 and 75%, thereby necessitating concurrent or staged percutaneous coronary intervention (PCI) with TAVR.2 However, there is a constant debate with varying options with regard to the timing of the PCI, on whether to perform PCI before, after or at the time of TAVR. This study aimed at reporting the trend, demographics, and outcomes of PCI with TAVR hospitalization in the United States.
We used the national inpatient sample (NIS) 2012–2018 for the present analysis. After filtering of hospitalizations appropriately using ICD-9 CM/ICD-10 CM procedural codes, hospitalizations over 18 years of age undergoing concurrent PCI with TAVR were identified and included in the analysis. The NIS clustering, survey nature, stratification, and weights were all considered while analyzing the data for this study. Categorical data were expressed in frequency and percentages. Continuous variables were expressed as mean and standard deviations or as median and interquartile range (IQR). The Jonckheere-Terpstra trend test was used to analyze trends of PCI in TAVR hospitalization and further, trend of mortality in PCI with TAVR hospitalization. Statistical significance was set at a p-value of <0.05 for all statistical tests used in the study. All analyses were performed using SAS, version 9.4 (SAS Institute Inc.).
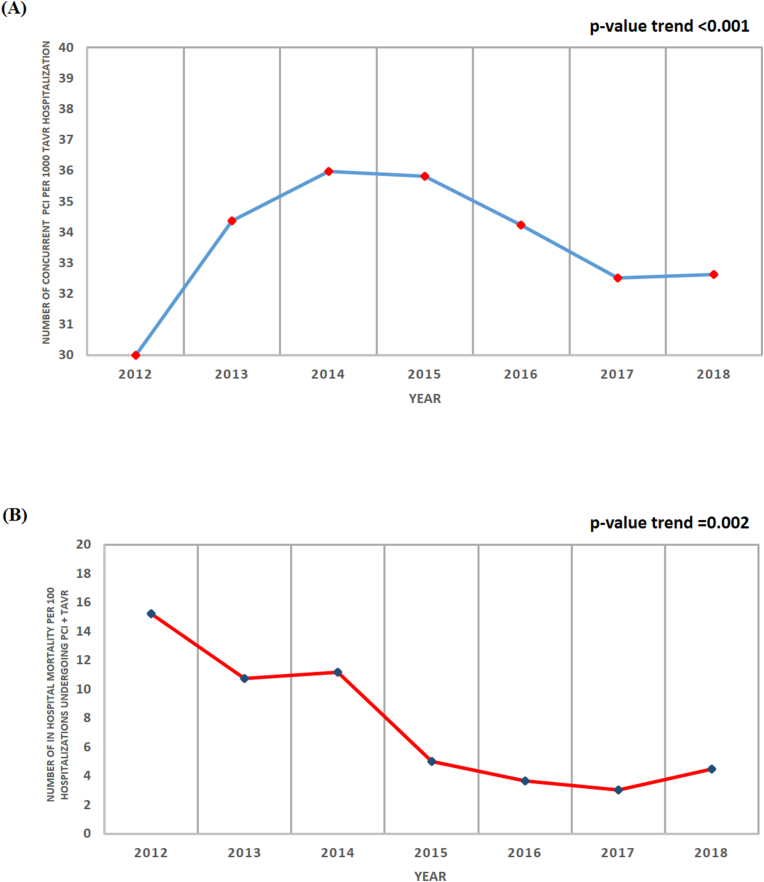
A total of 7295 hospitalizations undergoing PCI with TAVR were included in the final analysis. PCI with TAVR hospitalizations had a mean age of 79.73 ± 8.86 years, of which, 52.36% were males. 53.72% admissions were elective, while the rest were emergent (46.28%). The majority were of the Caucasian race (85.03%). Medicare was the primary insurance payer (88.55%). The prevalence of comorbidities among these hospitalizations were hypertension (47.70%), diabetes mellitus (19.26%), hypothyroidism (17.27%), congestive heart failure (2.74%), history of prior MI (10.90%), history of prior PCI (14.19%), history of prior CABG (13.37%), peripheral vascular disease (23.58%), valvular heart disease (1.17%), COPD (24.06%), chronic kidney disease (32.76%), coagulopathy (15.08%), deficiency anemia (22.69%), and tobacco use disorder (10.09%). Majority of procedures were performed in urban teaching hospitals (90.13%). There was a significant increase in the trend of concurrent PCI per 1000 TAVR hospitalization from 2012 to 2018 [p-value <0.001] [Fig. 1A].
Fig. 1.
(A) Trend graph for concurrent PCI per 1000 TAVR hospitalizations from 2012 to 2018; (B) Trend graph of all-cause in-hospital mortality per 100 PCI with TAVR hospitalizations.
PCI with TAVR hospitalizations had an all-cause in-hospital mortality of 5.83% and the median length of hospital stay was 7 days (IQR 3–13 days). There was a significant decrease in the trend of all-cause mortality per 100 PCI with TAVR hospitalizations from 2012 to 2018 [p–value = 0.002] [Fig. 1B]. The average cost of hospitalization was $66,944 ($50,636- $88,465). Cardiac arrest was reported in 4.25% of hospitalizations, acute myocardial infarction in 14.60%, cardiogenic shock in 8.84%, cardiac tamponade in 1.23%, complete heart block in 16.59%, permanent pacemaker implantation in 10.28%, and ventricular arrhythmia occurrence in 8.77%. Stroke occurred in 4.52% and acute kidney injury occurred in 24.67% of hospitalizations. Access site hemorrhage was reported in 1.78% of the hospitalizations, while access site hematoma was reported in 2.26% of the hospitalizations. 9.80% of the hospitalizations required blood transfusion in the perioperative period, and 2.26% of the hospitalizations developed respiratory complications during hospitalization.
The present study, using the NIS reported the trend, demographics and outcomes of PCI with TAVR hospitalizations. Although, there was a statistically significant increase in the trend of PCI per 1000 TAVR hospitalization from 2012 to 2018, the increase was of little significance. Using the NIS, the in-hospital mortality rates of hospitalizations undergoing isolated TAVR have been reported to be 3.6%, while in-hospital mortality rates post PCI were around 5% in STEMI patients and around 1% in unstable angina/stable ischemic heart disease patients.3,4 The in-hospital mortality rate of 5.83% reported in our study for PCI with TAVR hospitalizations is in accordance with these numbers. Also, an important finding is a decreasing trend of all-cause in-hospital mortality in PCI with TAVR hospitalizations from 2012 to 2018. This could be attributed to both better outcomes post PCI and post TAVR implantation in the recent years.
The current study has several limitations. NIS being an administrative data is subject to coding errors. However, since the main cohort was defined by procedure codes, the chances of coding error are minimal. Further, we did not account for the timing of the procedure during the hospitalizations.
Concurrent PCI with TAVR hospitalizations, whenever indicated, are associated with favorable outcomes. Future studies should aim at optimizing the treatment strategy in this specific cohort.
Funding
None.
Declaration of competing interest
None.
References
- 1.Landes U., Barsheshet A., Finkelstein A., et al. Temporal trends in transcatheter aortic valve implantation, 2008–2014: patient characteristics, procedural issues, and clinical outcome. Clin Cardiol. 2017;40:82–88. doi: 10.1002/clc.22632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goel S.S., Ige M., Tuzcu E.M., et al. Severe aortic stenosis and coronary artery disease--implications for management in the transcatheter aortic valve replacement era: a comprehensive review. J Am Coll Cardiol. 2013;62:1–10. doi: 10.1016/j.jacc.2013.01.096. [DOI] [PubMed] [Google Scholar]
- 3.Hernandez-Suarez D.F., Kim Y., Villablanca P., et al. Machine learning prediction models for in-hospital mortality after transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2019;12:1328–1338. doi: 10.1016/j.jcin.2019.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alkhouli M., Alqahtani F., Kalra A., et al. Trends in characteristics and outcomes of hospital inpatients undergoing coronary revascularization in the United States, 2003–2016. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2019.21326. e1921326–e1921326. [DOI] [PubMed] [Google Scholar]