Abstract
The present study explored college women’s perceptions of how dietary self-monitoring alters eating and body image-related cognitions and behaviors. The sample consisted of undergraduate women (N = 20), aged ≥ 18 (mean = 21.9 ± 6.6 years) from a cross-sectional qualitative study using semi-structured interviews conducted upon participants’ completion of a randomized controlled trial testing the effects of dietary self-monitoring via the smartphone app, MyFitnessPal. Inductive content analysis was utilized to identify participants’ perceptions of how engaging in dietary self-monitoring for one month impacted them. Participants’ experiences dietary self-monitoring was highly variable, with some participants reporting increased negative feelings (n = 9), positive feelings (n = 7), or both (n = 2). Other notable findings included increases in weight and/or shape concerns (n = 10) and a number of changes in dietary intake and other behaviors. Participants indicated that dietary self-monitoring may be helpful when trying to lose weight but harmful if the behavior becomes obsessive or if the user has poor body image. Individual experiences with dietary self-monitoring varies widely, and while dietary self-monitoring may be a useful tool for some college women, use should be monitored to avoid possible harmful side effects.
Keywords: college, women, dietary self-monitoring, Qualitative, weight-related
INTRODUCTION
The college years are a time when individuals, particularly women, are increasingly concerned with their physical appearance and weight (Croll et al., 2002). College students may seek out lifestyle support and weight management tools, such as dietary self-monitoring, due to growing body image-concerns and to help navigate challenges to healthy eating posed by stress and academic pressure, unstable schedules, and access to less healthful foods in college dining facilities (Deshpande et al., 2009). Dietary self-monitoring apps such as MyFitnessPal, have become particularly popular among emerging adults, with college women being among the most likely demographic to use such apps (Fox & Duggan, 2012; Hahn, Bauer, et al., 2021).
Dietary self-monitoring is thought to improve dietary intake by increasing an individual’s awareness of their current intake, allowing them to set goals, and monitor progress towards these goals, thereby building self-regulatory skills and improving self-efficacy (E.S. Anderson et al., 2007; Bandura, 1998; Bracken & Waite, 2020). However, self-awareness brought about by self-monitoring may also result in increased self-criticism of dietary behavior, belief that weight and shape is malleable, and pressure to meet body ideals (Berry et al., 2020), leading to poorer mental health, particularly increased eating disorder risk (Neumark-Sztainer et al., 2006; Ogden & Whyman, 1997). Failure to meet unrealistic goals may lead to rumination, negative affect, and ultimately disordered eating (Eikey et al., 2021; McCaig et al., 2020). Previous studies have consistently found that individuals who engage in dietary self-monitoring report higher eating disorder risk, particularly college women (Hahn, Bauer, et al., 2021; Hahn, Sonneville, et al., 2021; Romano et al., 2018; Simpson & Mazzeo, 2017). Further, many individuals with eating disorders report that dietary self-monitoring contributed to the development of their eating disorder (Levinson et al., 2017). However, it may be that individuals who are already concerned about their eating and weight choose to engage in dietary self-monitoring, rather than self-monitoring leading to increases in body image concerns. Additionally, the impact of dietary self-monitoring may differ based on the individual. For example, personality traits or thought patterns, such as perfectionism or obsessive thinking, may make dietary self-monitoring harmful for some but not others (McCaig et al., 2020). Because qualitative research has relied on individuals with existing body image concerns, it may be that previous samples are not reflective of the variability in experiences using dietary self-monitoring. Therefore, research on the range of behavioral and cognitive effects of dietary self-monitoring is needed, particularly among the general population of undergraduate women.
Among college women participating in a trial that involved dietary self-monitoring for approximately thirty days, we therefore sought to gain insight into the students’ perceptions of how being introduced to dietary self-monitoring affected their eating and body image-related cognitions and behaviors. Findings from this qualitative study could provide insight into whether dietary self-monitoring is helpful and/or harmful for different individuals.
METHODS
Study Design and Population
Participants (N = 20) were recruited from those in the intervention condition of the Tracking our Lives study, a randomized control trial aimed at assessing the cognitive and behavioral impacts of dietary self-monitoring use by undergraduate women (Hahn, Kaciroti, et al., 2021). To recruit participants for Tracking our Lives, the Office of the Registrar at the University of Michigan randomly selected 2,101 female identifying undergraduate students and sent them an email informing them of a study aimed at examining how the use of a smartphone app that track aspects of daily life impact well-being and inviting them to complete an online screening survey to determine if they were eligible to participate. Eligibility criteria for the study included: 1) undergraduate women; 2) aged 18 or older; 3) no prior or current diagnosis of an eating disorder; 4) low risk for an eating disorder (Eating Disorder Examination – Questionnaire Short [EDE-QS] Mean Score < 2) (Gideon et al., 2016); 5) no medical conditions affecting food consumption; 6) daily access to a smartphone; and 7) no use of any form of dietary self-monitoring in the year prior to screening.
Participants were randomized prior to the baseline study visit to either intervention or control condition. For participants randomized to the intervention condition, after data collection, MyFitnessPal was downloaded to their smart phone and research assistants set up an account using standardized settings including the individuals’ daily caloric needs for weight maintenance as calculated by the Mifflin St. Jeor equation and MyFitnessPal generated standardized macronutrient goals (Mifflin et al., 1990). Participants were then informed that they were to track everything that they ate for the study, starting the following morning and continuing until the post-intervention study visit. Daily reminders to track were sent to participants and participants were instructed not to change any of the app settings and to only use the app to track their dietary intake.
Data Collection and Study Procedure
Data for the current study were collected during the second, post-intervention study visit conducted approximately 30 days after the first data collection visit (Mean: 31.7 days, Range: 21.0-60.0 days). During this follow-up visit, the first 20 participants assigned to the intervention condition participated in a single semi-structured interview. A sample size of 20 was selected a priori to approximate sample sizes used in other exploratory qualitative studies of self-monitoring (K. Anderson et al., 2016; Eborall et al., 2015) Sociodemographic characteristics for study participants can be found in Table 1, including baseline body image and eating disorder risk, which did not significantly change post-intervention.
Table 1:
Baseline Characteristics of Study Population Overall and by Intervention Condition
| Overall Study Sample (N =200) |
Randomized to Intervention (N =100) |
Participated in Qualitative Interviews (N =20) |
|
|---|---|---|---|
| N (%) | |||
| Race/Ethnicity | |||
| White | 118 (59.0) | 59 (59.0) | 9 (45.0) |
| Black or African American | 16 (8.0) | 6 (6.0) | 1 (5.0) |
| Hispanic/Latina | 12 (6.0) | 6 (6.0) | 0 (0) |
| Asian | 66 (33) | 36 (36.0) | 9 (45.0) |
| Other | 6 (3) | 2 (2.0) | 1 (5.0) |
| Parent Education | |||
| Less than high school | 5 (2.5) | 1 (1.0) | 0 (0) |
| High school or less | 14 (7.0) | 7 (7.0) | 2 (10.0) |
| Some college or Associate’s degree | 31 (15.5) | 15 (15.0) | 0 (0) |
| Bachelor’s degree | 50 (25.0) | 23 (23.0) | 7 (35.0) |
| Advanced degree | 100 (50.0) | 54 (54.0) | 11 (55.0) |
| Academic Status | |||
| Freshmen | 36 (18.0) | 18 (18.0) | 3 (15.0) |
| Sophomore | 40 (20.0) | 17 (17.0) | 2 (10.0) |
| Junior | 76 (38.0) | 17 (17.0) | 4 (20.0) |
| Senior | 48 (24.0) | 28 (28.0) | 11 (55.0) |
| Mean (Standard Deviation) | |||
| Body Mass Index | 23.1 (4.8) | 22.6 (4.0) | 22.7 (3.1) |
| Age (years) | 20.0 (2.4) | 20.4 (3.1) | 21.9 (6.6) |
| EDE-QS a | 0.4 (0.4) | 0.4 (0.3) | 0.6 (0.5) |
| BISS b | 5.3 (1.2) | 5.4 (1.1) | 4.9 (1.1) |
Eating Disorder Examination Questionnaire Short (Gideon et al., 2016)
Body Image States Scale (Cash et al., 2002)
The goal of the semi-structured interviews was to elucidate the behavioral and cognitive consequences of dietary self-monitoring among study participants who were assigned to dietary self-monitor. Interview questions were designed to encourage participants to share their experience with dietary self-monitoring via MyFitnessPal. Specifically, participants were asked: 1) their personal experiences of how self-monitoring dietary intake via MyFitnessPal altered their eating and body image-related cognitions and behaviors, and 2) in general, among whom they thought dietary self-monitoring via MyFitnessPal could be helpful or harmful (see Table 2 for interview guide). The interview guide was developed by the research team and was informed by previous research findings and aimed at elucidating specific cognitions and behavioral impacts of dietary self-monitoring (Burke et al., 2011; Romano et al., 2018; Simpson & Mazzeo, 2017). All interviews were conducted by the trained primary investigator who first asked broad questions and then used specific prompts to follow up on participants’ responses as needed. Interviews took approximately 20 minutes on average to complete and at the end of interviews, participants were provided with a list of local and online mental health resources. Interviews were recorded with permission and transcribed verbatim and reviewed by a second transcriptionist for accuracy. Study procedures were approved by the Institutional Review Board at the University of Michigan.
Table 2:
Semi-Structured Interview Guide
Personal Experiences
|
General Experiences
|
Data Analysis
Semi-structured interview transcripts were reviewed by three researchers, including the interviewer/primary investigator, to identify overarching themes that emerged from the data using inductive content analysis (Schamber, 2000). Inductive content analysis was used given the exploratory nature of the analysis, and followed the steps outlined by Elo & Knygäs (2008). After reviewing all the transcripts, the researchers met to discuss identified themes. Once the researchers reached a consensus on identified themes, a codebook was created that identified themes and sub-themes. Two trained coders then independently coded the same two transcripts to identify discrepancies in interpretation of participant meaning in transcripts, and whether information warranted positive endorsement of themes and sub-themes. Researchers then met again to further refine the codebook, this process was repeated twice to reach 85% agreement for all themes. The remaining transcripts were coded by both coders and any discrepancies were reviewed and resolved by the primary investigator. Themes were often associated with specific questions in the interview guide, however because semi-structured interviews are participant driven and we utilized inductive content analyses, if participants reported information that qualified for the theme outside of the direct question, the theme was still coded as present. Data saturation was determined by the primary investigator using inductive thematic saturation (Saunders et al., 2018).
RESULTS
Impacts of Dietary Self-Monitoring on Participants
When asked how dietary self-monitoring via MyFitnessPal affected participants, three overarching themes emerged: Feelings, Cognitions, and Behaviors (Figure 1). The primary investigator determined that data saturation had been reached.
Figure 1.
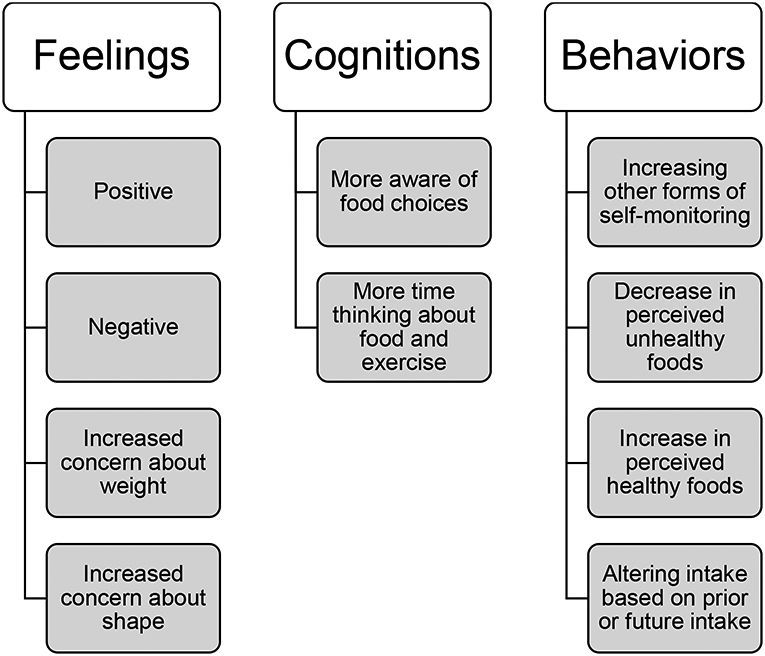
Themes and sub-themes of participant identified impacts of dietary self-monitoring via MyFitnessPal
Feelings
Participants reported experiencing both negative (n = 9) and positive emotional changes (n = 7) resulting from dietary self-monitoring, with two participants reporting both negative and positive experiences. Most commonly, increased negative affect was expressed as increased self-consciousness around their food choices, and body shape and weight (n = 7), guilt (n = 4), and worry or anxiety (n = 4), with several (n = 4) participants expressing more than one type of negative affect. As one participant stated, “…at times I knew why I look like this was because I was eating bad or not being healthy enough or like fit um, so I felt like because I found the reason I felt much more guilty or like I blamed myself more for it.”
Among those who reported dietary self-monitoring evoked positive feelings (n = 7), participants described that they felt better or prideful when eating within MyFitnessPal’s recommendations. Participants expressed feeling physically and emotionally better on days when they stayed within the daily calorie and macronutrient recommendations provided from MyFitnessPal relative to days when they exceeded the preset goals. One participant shared, “I think I liked it a lot the first couple of weeks because it did make me feel better about what I was eating like I felt like I was eating the right things.”
When asked if using MyFitnessPal changed the way they felt about their weight and shape, seven participants reported increased concern about their weight, seven reported increased concern about their shape, and over half of these participants (n = 4) reported increases in both weight and shape concerns. One participant noted, “I wasn’t really worried about my weight as much as I was about body shape. Like I was less about like losing weight or gaining weight, more about trying to make sure I’m eating the right foods and getting the right amount of exercise to get the body shape that I want.”
Cognitions
When exploring changes in cognition, nearly all participants (n =18) reported that dietary self-monitoring made them more aware of their food choices. Participants felt more cognizant of not only the type of foods they were eating, but also what they were not eating. “[I] was much more aware of what I was eating and what I was not eating for sure. I definitely felt like when I was putting down how many if I was eating certain vegetables, I was also aware that I wasn’t eating certain things.” Participants also noted becoming more aware of their eating patterns, “I think, well most of the time I found out that I really don’t eat that much but the days I would eat more or stop, like my sister’s graduation party for example, it’s really easy to overeat at something like that so tracking my food helped me not go over my calorie goal which I think I would have done if I wasn’t using the app.” Additionally, 15 participants said that they spent more time thinking about food and exercise overall due to dietary self-monitoring.
Behaviors
Participants reported several changes to their behavior while dietary self-monitoring with MyFitnessPal. Eleven participants reported increasing other types of self-monitoring including tracking exercise and water intake. Six participants reported that tracking led to them consuming less food they perceived as unhealthy and six participants also reported eating more foods they perceived as healthy. One participant noted, “I didn’t realize how much sugar I was eating so it really impacted what I did. I think the first couple days I ate a lot of sugar and then I was like ‘Wait, this is really bad, I’m like at negative calories like every day‘”.
Twelve participants noted altering how much they planned to eat and when based on what they had already eaten during the day or what they planned to eat later in order to compensate for their intake. “Before using the app I’d be like ‘okay breakfast, lunch, dinner‘ like set for the day like I knew what I was going to eat. But when I put in each meal and I saw how many calories I had left, that definitely changed the amount that I was going to eat for dinner and for lunch and stuff like that.”
Perception of Helpfulness and Potential Harm of Dietary Self-Monitoring
Helpful
The most commonly reported reason participants believed that dietary self-monitoring could be helpful to themselves and/or others when trying to lose weight (n = 12) and when trying to be “healthy” or “healthier” (n = 12). Participants’ examples of trying to be healthy included being pregnant, training for an athletic event, or trying to be more conscious about what types of foods they consume.
Harmful
Participants felt that using MyFitnessPal for dietary self-monitoring could be harmful when it becomes obsessive (n = 9), for those with poor body image (n = 8), or if it negatively impacts your life (n = 6). “I think there are certain people who it could become an obsession like ‘omg I’ve eaten this this and this and I’m getting too close to my calorie goal or something ’.” Another participant noted, “I think it can definitely be bad for people who have poor body image to be keeping track and scrutinizing what they eat ‘cause they probably go back and reflect and scrutinize like ‘oh, I shouldn’t have eaten this’ and then a reflection of that not eat as much the next day and something like that.”
DISCUSSION
The purpose of this study was to qualitatively explore Tracking Our Lives study participants’ perceptions of how dietary self-monitoring impacted them, principally their eating and body image-related cognitions and behaviors and to gain insight to potential risk and benefits of dietary self-monitoring. We found that the experience of dietary self-monitoring is highly variable among college women introduced to dietary self-monitoring as part of a randomized controlled trial; most participants believed that dietary self-monitoring increased awareness of their eating and led to higher consumption of foods perceived to be healthy. However, a considerable proportion of participants also reported negative effects of dietary self-monitoring including increased body image-concerns and using compensatory restriction. Moreover, some participants experienced negative and positive impacts simultaneously, while others reported no impact at all.
For many participants, dietary self-monitoring increased their awareness of their food choices, which research suggests is necessary to improve self-regulation and self-efficacy to support changes in dietary intake (Samdal et al., 2017). For example, participants reported making food choices to stay within their calorie or nutrition goals, such as increasing their vegetable intake. Additionally, many participants reported positive mood changes related to dietary self-monitoring, specifically when they perceived to have eaten healthfully. For some, following the guidelines may have elicited a sense of pride or accomplishment, which could further reinforce positive health behavior changes (Gokke-LaRose et al., 2009).
Though many found dietary self-monitoring to be helpful, a portion of participants also reported harmful responses including increased fixation on food and exercise, increased eating and body image-related self-consciousness, anxiety, and guilt. Even participants who did not have negative outcomes themselves forecasted that dietary self-monitoring could be problematic for those with pre-existing body image-concerns. While this belief could reflect a cognitive bias (e.g. overconfidence) on the part of participants, future research should examine whether body dissatisfaction moderates the impacts of dietary self-monitoring. These findings extend qualitative work conducted among eating disorder populations showing that dietary self-monitoring can lead to negative emotions and obsessive thinking even among the general population of college students (Eikey & Reddy, 2017; McCaig et al., 2020). For some vulnerable populations, unrealistic or unmet goals may lead to rumination, resulting in negative emotion, ultimately serving as a mediator between dietary self-monitoring and eating disorder risk (Eikey et al., 2021; Hahn, Pacanowski, et al., 2021). Overall, our findings indicate that there is heterogeneity in students’ experiences with and perceptions of dietary self-monitoring. To help better tailor recommendations and reduce possible unintended consequences, future research is needed to understand how individual characteristics and experiences may account for the variability of impact or potentially design elements of the app that seem helpful or harmful.
The use of semi-structured interviews was a strength of the study as it allowed us to capture the breadth of impacts experienced by participants and ideas of when dietary self-monitoring may be helpful and harmful, rather than imposing researcher-generated ideas. Another significant strength is that qualitative data were collected from participants in a randomized control trial allowing us to examine the experimental effects of introducing dietary self-monitoring, rather than examining individuals who self-selected to dietary self-monitor. Conversely, individuals who initiate self-monitoring outside of the context of a research study may be differentially affected by dietary self-monitoring. Participation was also limited to 20 individuals from a study of undergraduate women from a single institution and thus may not be representative of all college students, or more broadly, all young adults. Recall bias is another potential limitation of the current study; it is possible that being asked about how dietary self-monitoring impacted their body image led to overestimation the impacts. Future research would benefit from examining the dietary tracking experiences of those who do not identify as female, emerging adults not attending college, and other vulnerable ages.
CONCLUSIONS
Dietary self-monitoring is common among college women and the widespread promotion of dietary self-monitoring has the potential to have profound public health implications. Dietary self-monitoring may be a helpful tool for improving dietary intake. However, given that self-monitoring may be harmful for some, practitioners should also take into account the possibility that some individuals may experience negative outcomes, such as those who have poor body image. Findings from the current study regarding individual differences in experiences with dietary self-monitoring, along with insight regarding when dietary self-monitoring may be helpful or harmful among college women can lay the groundwork for future studies aimed at understanding variability in response to dietary self-monitoring.
Highlights.
The impacts of dietary self-monitoring on college women were highly varied
Dietary self-monitoring led to changes in thoughts, feelings, and behaviors
Use of dietary self-monitoring may help improve dietary patterns of college women
Body concerns may be exacerbated among those who are body dissatisfied
Acknowledgements:
We would like to thank the students who participated in the research study as well as the research assistants who made this study possible.
Funding/Financial disclosures:
The University of Michigan Rackham Predoctoral Fellowship assisted in the funding for the dissertation of Samantha L. Hahn, of which this research stemmed from. Additionally, the Rackham Graduate Student Research Grant assisted in paying for Tracking our Lives Study. The time to write this manuscript by Samantha L. Hahn was partially funded by Grant Number T32MH082761 from the National Institute of Mental Health (PI: Scott Crow). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institute of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest disclosures: The authors declare that they have no conflicts of interests to declare.
REFERENCES
- Anderson ES, Winett RA, & Wojcik JR (2007). Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Annals of Behavioral Medicine, 37(3), 304–312. 10.1007/BF02874555 [DOI] [PubMed] [Google Scholar]
- Anderson K, Burford O, & Emmerton L (2016). Mobile health apps to facilitate self-care: A qualitative study of user experiences. PLoS ONE, 11(5), e0156164. 10.1371/journal.pone.0156164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A (1998). Health promotion from the perspective of social cognitive theory. Psychology and Health, 13(4), 623–649. 10.1080/08870449808407422 [DOI] [Google Scholar]
- Berry RA, Rodgers RF, & Campagna J (2020). Outperforming iBodies: A Conceptual Framework Integrating Body Performance Self-Tracking Technologies with Body Image and Eating Concerns. Sex Roles, 1–12. 10.1007/s11199-020-01201-6 [DOI] [Google Scholar]
- Bracken ML, & Waite BM (2020). Self-Efficacy and Nutrition-Related Goal Achievement of MyFitnessPal Users. Health Education and Behavior, 47(5), 677–681. 10.1177/1090198120936261 [DOI] [PubMed] [Google Scholar]
- Burke LE, Wang J, & Sevick MA (2011). Self-Monitoring in Weight Loss: A Systematic Review of the Literature. Journal of the American Dietetic Association, 777(1), 92–102. 10.1016/j.jada.2010.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash TF, Fleming EC, Alindogan J, Steadman L, & Whitehead A (2002). Beyond body image as a trait: The development and validation of the body image states scale. Eating Disorders, 10(2), 103–113. 10.1080/10640260290081678 [DOI] [PubMed] [Google Scholar]
- Croll J, Neumark-Sztainer D, Story M, & Ireland M (2002). Prevalence and risk and protective factors related to disordered eating behaviors among adolescents: Relationship to gender and ethnicity. Journal of Adolescent Health, 31(2), 166–175. 10.1016/S1054-139X(02)00368-3 [DOI] [PubMed] [Google Scholar]
- Deshpande S, Basil MD, & Basil DZ (2009). Factors influencing healthy eating habits among college students: An application of the health belief model. Health Marketing Quarterly, 26(2), 145–164. 10.1080/07359680802619834 [DOI] [PubMed] [Google Scholar]
- Eborall HC, Dallosso HM, McNicol S, Speight J, Khunti K, Davies MJ, & Heller SR (2015). Explaining engagement in self-monitoring among participants of the DESMOND self-monitoring trial: A qualitative interview study. Family Practice, 32(5), 596–602. 10.1093/fampra/cmv060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eikey EV, Caldeira CM, Figueiredo MC, Chen Y, Borelli JL, Mazmanian M, & Zheng K (2021). Beyond self-reflection: introducing the concept of rumination in personal informatics. Personal and Ubiquitous Computing, 25(3), 601–616. 10.1007/s00779-021-01573-w [DOI] [Google Scholar]
- Eikey E. v., & Reddy MC (2017). “It’s definitely been a journey”: A qualitative study on how women with eating disorders use weight loss apps. In Conference on Human Factors in Computing Systems - Proceedings (Vols. 2017-May, pp. 642–654). Association for Computing Machinery, 10.1145/3025453.3025591 [DOI] [Google Scholar]
- Elo S, & Kyngäs H (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Fox S, & Duggan M (2012). Mobile Health 2012 ∣ Pew Research Center. In Mobile Health. Pew Research Center. http://www.pewinternet.org/2012/11/08/mobile-health-2012/ [Google Scholar]
- Gideon N, Hawkes N, Mond J, Saunders R, Tchanturia K, & Serpell L (2016). Development and psychometric validation of the EDE-QS, a 12 item short form of the eating disorder examination questionnaire (EDE-Q). PLoS ONE, 11(5). 10.1371/journal.pone.0152744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gokke-LaRose J, Gorin AA, & Wing RR (2009). Behavioral self-regulation for weight loss in young adults: A randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity, 6, 10. 10.1186/1479-5868-6-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn SL, Bauer KW, Kaciroti N, Eisenberg D, Lipson SK, & Sonneville KR (2021). Relationships between patterns of weight-related self-monitoring and eating disorder symptomology among undergraduate and graduate students. International Journal of Eating Disorders, 54(4), 595–605. 10.1002/eat.23466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn SL, Kaciroti N, Eisenberg D, Weeks HM, Bauer KW, & Sonneville KR (2021). Introducing Dietary Self-monitoring to Undergraduate Females via a Calorie Counting App has no Effect on Mental Health or Health Behaviors: Results from a Randomized Controlled Trial. Journal of the Academy of Nutrition and Dietetics, In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn SL, Pacanowski CR, Loth KA, Miller J, Eisenberg ME, & Neumark-Sztainer D (2021). Self-weighing among young adults: who weighs themselves and for whom does weighing affect mood? A cross-sectional study of a population-based sample. Journal of Eating Disorders, 9(1), 37. 10.1186/s40337-021-00391-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn SL, Sonneville KR, Kaciroti N, Eisenberg D, & Bauer KW (2021). Relationships between patterns of technology-based weight-related self-monitoring and eating disorder behaviors among first year university students. Eating Behaviors, 42, 101520. 10.1016/j.eatbeh.2021.101520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Fewell L, & Brosof LC (2017). My Fitness Pal calorie tracker usage in the eating disorders. Eating Behaviors, 27, 14–16. 10.1016/j.eatbeh.2017.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaig D, Elliott MT, Prnjak K, Walasek L, & Meyer C (2020). Engagement with MyFitnessPal in eating disorders: Qualitative insights from online forums. International Journal of Eating Disorders, 53(3), 404–411. 10.1002/eat.23205 [DOI] [PubMed] [Google Scholar]
- Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, & Koh YO (1990). A new predictive equation for resting energy expenditure in healthy individuals. American Journal of Clinical Nutrition, 51(2), 241–247. 10.1093/ajcn/51.2.241 [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, van den Berg P, Hannan PJ, & Story M (2006). Self-Weighing in Adolescents: Helpful or Harmful? Longitudinal Associations with Body Weight Changes and Disordered Eating. Journal of Adolescent Health, 39(6), 811–818. 10.1016/j.jadohealth.2006.07.002 [DOI] [PubMed] [Google Scholar]
- Ogden J, & Whyman C (1997). The effect of repeated weighing on psychological state. European Eating Disorders Review, 5(2), 121–130. [DOI] [Google Scholar]
- Romano KA, Swanbrow Becker MA, Colgary CD, & Magnuson A (2018). Helpful or harmful? The comparative value of self-weighing and calorie counting versus intuitive eating on the eating disorder symptomology of college students. Eating and Weight Disorders, 23(6), 841–848. 10.1007/s40519-018-0562-6 [DOI] [PubMed] [Google Scholar]
- Samdal GB, Eide GE, Barth T, Williams G, & Meland E (2017). Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 42. 10.1186/s12966-017-0494-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, & Jinks C (2018). Saturation in qualitative research: exploring its conceptualization and operationalization. Quality and Quantity, 52(4), 1893–1907. 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schamber L (2000). Time-line interviews and inductive content analysis: Their effectiveness for exploring cognitive behaviors. Journal of the American Society for Information Science and Technology, 57(8), 734–744. [DOI] [Google Scholar]
- Simpson CC, & Mazzeo SE (2017). Calorie counting and fitness tracking technology: Associations with eating disorder symptomatology. Eating Behaviors, 26, 89–92. 10.1016/j.eatbeh.2017.02.002 [DOI] [PubMed] [Google Scholar]


