Abstract
Background:
End-Stage Renal Disease (ESRD) is an irreversible impairment of kidney function that leads to permanently dependent on alternative therapies such as hemodialysis, peritoneal dialysis, and renal transplantation. This study aimed to systematically investigate the survival rate of patients with renal transplantation, graft, and its related factors in Iran.
Methods:
This systematic review and meta-analysis drew on articles indexed in six international and one internal databases (Medline/PubMed, ProQuest, Scopus, Embase, SID, and Web of knowledge) until Nov 2020. The reporting of the present study was performed in terms of PRISMA statement. All analyzes were performed using the STATA software.
Results:
Overall, 367 titles from 6 databases were evaluated of which 86 articles met the inclusion criteria. According to the random model, the graft survival rate at one, three, five, and 10 years were 92.48%, 85.08%, 79.96% and 68.15% respectively. Additionally, the patient survival rates at one, three, five, and 10 years were 91.27%, 86.46%, 81.17% and 78.15% respectively. There was a significant relationship between the age recipient and three-year graft survival rate (P=0.021). Additionally, there was an inverse and significant relationship between the donor age and 10-year patient survival rate (P=0.011).
Conclusion:
The patient and graft survival in transplanted kidney patients is comparable with most developed countries.
Keywords: Kidney transplantation, End stage renal disease, Graft survival, Patient survival, Meta-analysis
Introduction
Chronic kidney disease (CKD) is a public health concern which includes a range of different pathophysiological processes with abnormal renal function and progressive decrease in Glomerular Filtration Rate (GFR) (1, 2). Additionally, as one of the debilitating diseases with a high mortality rate, the incidence of CKD is increasing worldwide (1, 3). The term End-Stage Renal Disease (ESRD) is an irreversible impairment of kidney function that leads to permanently dependent on alternative therapies such as hemodialysis, peritoneal dialysis, and renal transplantation (4–6). The prevalence of ESRD in Iran is estimated at about 357 per million with an annual incidence of about 57 per million (7). Kidney transplantation is currently considered as the best and the most effective treatment of ESRD. In addition, kidney transplantation increases the quality of life as well as the chances of survival rate of the patients (3, 8–11).
Similar to the other parts of the world, kidney transplantation in Iran is also increasing alarmingly. A large number of ESRD patients, including the older ones previously considered unsuitable for the treatment, were undergone renal transplantation in recent years (12). To evaluate the effectiveness of kidney transplantation, the survival rate and quality of life of the patients are the two most important indicators. Hassanzadeh et al. reported the one, 3, 5, 7, and 10-year graft survival rates in shiraz is 98.3%, 96.4%, 92.5%, 90.8%, and 89.2%, respectively (13). In a study on 19 cases of kidney transplant patients in Germany, one-year graft survival rate was 94.7% (14). One-year graft survival rate was 85% in another study (15). In Taiwan and in the USA graft one-year survival rate was 92.2% (16).
Based on the discrepancy in the reported survival rates of kidney transplant patients around the world, the survival rate is affected by several influencing factors. Understanding the survival rate of kidney transplant patients in Iran along with identifying the most important influencing factors, could provide valuable information on therapeutic measures and outcomes of the transplant. One-year uncensored graft survival of patients who were ABO-incompatible was 96% versus 98% in ABO-compatible. Three-year uncensored graft survival of patients who were ABO-incompatible was 92% versus 94% in ABO-compatible. Moreover, One-year uncensored graft patient of patients who were ABO-incompatible was 98% versus 99% in ABO-compatible (17).
Up to now, no comprehensive study has been conducted on the survival rate of kidney transplant patients and the allograft in Iran. This study aimed to perform a systematic review on the published studies to estimate the survival rate of kidney transplant patients and its major related factors in Iran.
Methods
Eligibility Criteria and Information Sources
The present study is a systematic review and meta-analysis of allograft and recipient’s (kidney transplantation) survival rate in Iran up to Nov 2020. The reporting of the present study was performed in terms of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement (18). All observational studies (cross-sectional, case-control, and cohort) referring to the survival rate of the kidney recipients, in English and Persian languages published before Nov 2018 were included in the present study. Other review and meta-analysis studies reporting the survival rate of patients and kidney allograft with no reported sample size or confidence interval for the estimated survival rate were excluded.
This study was approved by the research Ethics Committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1398.1155).
The researchers investigated six international databases including Medline/PubMed, Scopus, Embase, Web of knowledge, SID, and ProQuest until Nov 2020. Google Scholar was also explored to detect any grey literature. Selected keywords for searching international databases were as follows: “renal transplantation”, “kidney grafting”, “kidney transplantations”, “survival”, “survival rate”, “survival analysis”, and “Iran”. The collected data was entered into EndNote, X7 software, and duplicate articles were automatically deleted. Two researchers examined the articles independently.
Study Selection and Data Extraction
After removing duplicate results, the abstracts of all articles were screened for eligibility by two independent reviewers (FM and MV). Two researchers independently performed screening of the studies, extraction of the results, and evaluation of the articles. Additionally, a supervisor was appointed to make the final decision in disputed cases or lack of agreement between the two assessors. A datasheet was used to extract data from the selected articles. The data included the author’s name, year of publication, study period, sample size, donor and recipient age and sex, donor type (live related, live non-related and cadaver donor) and for one, three, five, and 10-year survival rates of allograft and patients.
Risk of Bias (Quality) Assessment
The Newcastle-Ottawa Quality Assessment Form was employed to evaluate the quality of the selected papers. This tool comprises of three sections as following: 1) sampling (4 questions), 2) comparability (1 question) and 3) outcome (3 questions). Accordingly, based on the final scores, the studies were divided into three categories namely: good (3 or 4 scores in sampling domain and 1 or 2 scores in comparability domain and 2 or 3 scores in outcome/exposure domain), Fair (2 scores in selection domain and 1 or 2 scores in comparability domain and 2 or 3 scores in outcome/exposure domain), and Poor (0 or 1 score in selection domain or 0 score in comparability domain or 0 or 1 score in outcome/exposure domain) (19).
Statistical Analysis
The heterogeneity of the studies and its composition were assessed by Cochran test (with significance level less than 0.1) and I2 statistic respectively. In the case of heterogeneity, a random effect model along with the inverse-variance method were used. A fixed effect model was applied in the absence of heterogeneity. In the case of heterogeneity of the results of studies, subgroup analysis was used. All analyzes were performed using the STATA software (ver. 13). Due to the heterogeneity of the results of the included studies, meta-regression with factors such as the year of study, sample size, and donor and recipient age analysis was employed. A random effects model was used to reduce bias risk in studies (20, 21). Additionally, Egger test was used to evaluate the risk of publication bias (22). In this study index is Survival as percentage.
Results
Search Results
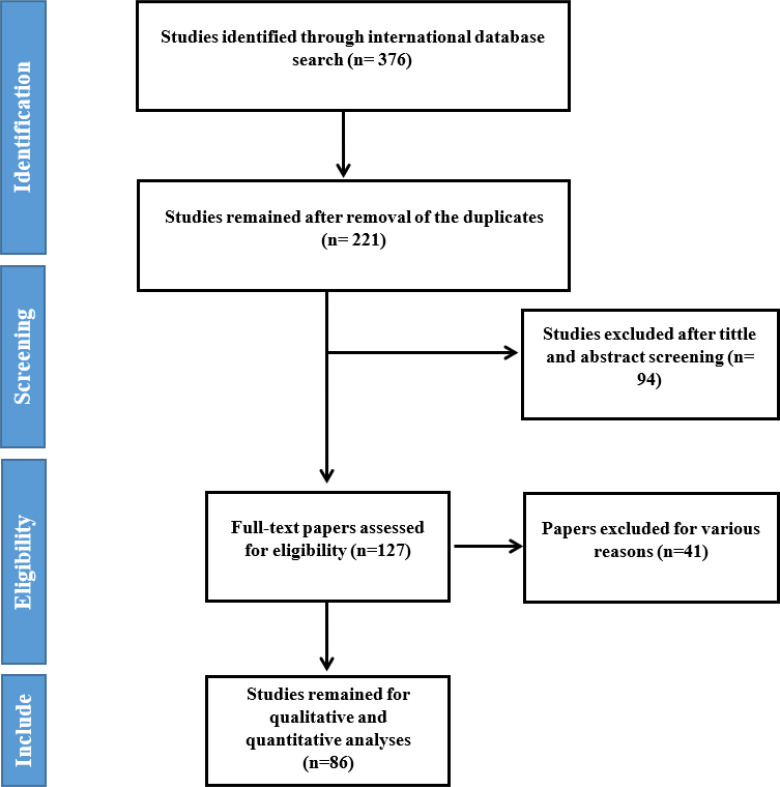
As the initial phase of this study, 376 articles were selected from the international databases. Subsequently, duplicate studies were excluded and 221 studies were moved into the review phase in terms of title and abstract. Following the review of the titles and abstracts, 127 articles selected for the next phase, at which the full text was examined and 86 articles were finally selected for analysis. The references of the articles were also reviewed to add relevant studies (Fig. 1).
Fig. 1:
Flowchart of the included eligible studies in Systematic Review
Characteristics of Eligible Study
The included studies were published from 1999 to 2020 (86 were selected). Based on their geographical locations, 40 studies were conducted in Tehran, eight in Shiraz, five in Urmia, nine in Mashhad, three in Ahvaz, two in Hamadan, two in Tabriz, two in Arak, two in Kerman, three in Isfahan, three in Babol, two in Rasht, one in Central province, one in Zahedan, one in Qom and two in Kermanshah.
Quality appraisal
Overall, 52 studies had well and 34 of them had a fair quality.
Heterogeneity
Chi-square test and I2 index showed a significant heterogeneity in the reported patient’s and graft’s survival rates among studies. For allograft, the heterogeneity test for one-year (I2=96.2%, P<0.001), three-year (I2=98.1%, P<0.001), five-year (I2=98.4%, P<0.001), and ten-year (I2=99.2%, P<0.001) survival rates were significant. Similarly, the heterogeneity test for the patients’, one-year (I2=98.9%, P<0.001), three-year (I2=97.9%, P<0.001), five-year (I2=97.5%, P<0.001) and ten-year (I2=97.2%, P<0.001) survival rates were significant. As a result, a random effect model was used for all analyzes.
One-year patient and graft survival rates
Among the most recently published papers, 48 of them reported the one-year patient survival rate. Based on the results of the random-effect model, one-year patient survival rate was 91.27% (95%CI= 89.44% to 93.10%). Additionally, based on the results of 73 studies the one-year graft survival rate was estimated at 92.48% (95%CI=91.35% to 93.61%).
Three-year patient and graft survival rates
Of 24 selected studies, the three-year patient survival rate was 86.46% (95%CI= 84.64% to 88.27%). Additionally, of 42 selected studies, the three-year graft survival rate was 85.08% (95%CI=82.18% to 87.99%).
Five-year patient and graft survival rate
Out of the selected papers, 37 reported the five-year patient survival rate. The five-year patient survival rate was 81.17% (95%CI= 95 %CI=78.71% to 83.63%). Additionally, of 53 studies, the five-year graft survival rate was 79.96% (95%CI= 77.55% to 82.38%).
10-year patient and graft survival rates
Fourteen studies reported 10-year patient survival rate. Accordingly, the gender-age adjusted 10-year patient survival rate was 78.15% (95%CI=73.58%–82.73%). Additionally, of 20 studies, the gender-age adjusted 10-year graft survival rate was 68.15% (95%CI=58.79% to 77.52%).
Meta-regression of graft survival rates
The results of meta-regression suggested no significant relationship between sample size and graft survival rate (coef = −0.001, P=0.213). However, a significant relationship were observed between the year of study publication and three-year graft survival rate (coef=0.010, P=0.003).Additionally, There was also a strong relationship between donor age and 10-year graft survival rate (coef=0.042, P=0.015).
Meta-regression of patients’ survival rate
The results of meta-regression suggested no significant relationship between sample size and patient survival rate (Coef=−0.000, P=0.342). However, a significant relationship was observed between the years of study publication and one-year patients survival rate (Coef=0.004, P=0.034).
Subgroup analysis: graft survival rate
The one and five-year graft survival rate for recipients of kidney from related living donor were 92.14% (95%CI=88.26% to 96.03%) and 77.99% (95%CI=59.36% to 96.63%) respectively. Whereas, the one and five-year graft survival rates in recipients with non-related living donors were 84.62% (95%CI=77.49% to 91.75%) and 79.87% (95%CI=74.39% to 89.65%). Moreover, the one and five-year graft survival rates in cadaver recipients were 90.41% (95%CI=86.63% to 94.19%) and 78.77% (95%CI=70.23% to 87.32%), respectively.
Publication bias
Finally, according to the results presented by a funnel plot and egger test (bias: −6.70, a 95%CI=−8.83 to −4.58, P<0.001) a significant release bias for graft survival rate was observed.
Discussion
ESRD is a widespread global problem, and the renal transplantation is the preferred treatment for patients with the condition as it improves their survival rate and quality of life when compared with hemodialysis (8, 23–26). We aimed to evaluate the patient and graft survival rate with regard to major related factors in Iran.
With moving to the more recent years, the survival of patients and grafts (especially for one and three-year patient and graft survival rates) increased, suggesting a relative improvement in the success of the surgical procedures. In our study, the one-year patient and graft survival rate were 91.27% and 92.48% respectively. The results are in accordance to the report from Iranian Organ procurement Network that reported the one-year survival rate of renal transplantation was 94.7% (27). However, a study on Greek and Albanian patients suggested higher one-year survival rates for the patient’s (100%) and grafts (93.1%) (28). Another study (29) reported considerably higher one-year survival rate of patients in live and cadaver recipients in the USA, Australia and New Zealand, Europe and Canada (98.7% and 97.0% for US, 99% and 95% for AN, 98.6% and 90.7% for Europe, 97.7% and 94.9% for Canada respectively). Similarly, the one-year survival rate of graft in live and cadaver recipients in the USA, Australia and New Zealand, Europe and Canada (97.2% and 93.40% for US, 98% and 95% for AN, 95.8% and 90.7% for Europe, 97.7% and 94.9% for Canada respectively) were higher than the estimated rates in Iran. In addition, the one-year graft survival rate reported in the US by a study conducted on 109 live donor kidney transplants was 93.2% (30). On the other hand, another study on 2300 kidney transplants in China reported that the one-year graft survival rate as about 87.3% (31). In Germany, the one-year graft survival rate in children was about 88% and the one-year survival rate of patients was 93.63% (32).
The survival rate of the graft and patient is marginally lower than several western countries and higher than China. According to our results, the three-year survival rate of patients was 86.46%, and the three-year survival rate of grafts was 85.08%. Higher rates was reported for the three-year graft survival rates for non-Asians (89%) and South Asians (85%) (33). On the other hand, few studies reported lower survival rates. For example, three-year graft survival rate was 80% among Chinese patients (34). Moreover, three-year survival rate was reported for South Asian and European patients as 73% and 72%, respectively (35).
The five-year patient and graft survival rate was 81.17% and 79.96% respectively. In that regard, in South Asians, five-year survival rate of graft was 64% and 65% for South Asian and whites races, respectively (36). Kidney transplant patients in South Asian races had more mortality rate after five years (about 58% versus 71% for other races) (37).
On the other hand, another study reported considerably higher five-year survival rate of patients in live and cadaver recipients in the USA, Australia, New Zealand, Europe, and Canada (93.1% and 86.1% for US, 95% and 90% for AN, 94.3% and 87.1% for Europe, respectively) (29). Similarly, the five-year survival rate of graft in live and cadaver recipients in the USA, Australia and New Zealand, Europe and Canada (84.6% and 72.4% for US, 90% and 81% for AN, 86.9% and 77.8% for Europe, 90.8% and 81.4% for Canada respectively). However, the five-year survival rate of patients in the US was 77.4% (38), significantly lower survival rate compared to the present study. The discrepancy in the reports may reflect the difference in the year of conduction of the studies and characteristics of the patients or donors (39).
The present study reported that 10-year survival rate of the patients and grafts were 78.15% and 68.15%, respectively. According to the latest results of the American Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients in 2004, the survival rate of patients was 75.5% after 10 years (40). Based on our results, the 10-year survival rate of Iranian kidney transplant patients was higher than some other reports in the United States, influenced by factors such as Studies of donor type (cadaver or living donor), donor and recipient age, recipient underlying diseases especially hypertension, diabetes, coronary artery disease, medication regimen, infections and the functioning of transplanted kidney that may affect the patients’ survival rate (40–43).
There was a significant relationship between the kidney recipient’s age and three-year, five-year and 10-year survival rates of the patients. The results was in agreement with another study in the USA in which the recipient’s and donor’s age are suggested to have a detrimental effect on long-term allograft survival rate (44). On the other hand, several studies in Brazil, Australia and Italy found no significant relationship between age of the recipient and 200 survival rate of transplantation (45–47). In contrast, another study showed a strong relationship between the Age of donor, recipient of kidney and survival rate of graft. Additionally, the recipient age group of 40 to 60 yr old had higher survival rate compared to the age group of less than 20 yr old, a result reported by several studies in Italy, United Kingdom and USA which were similar to the results of present study (47–50).
No association was reported between age and allograft survival in children and older patients due to the small size of anatomical parts of kidney (51). It was also a lower survival rate of the patients and grafts that received from non-familial donor. Accordingly, the possible reason for the discrepancy in the results from different countries could be the greater rate of acute rejection events occurred when the kidney is from a non-family donor.
As with any systematic review, the present study has limitations in certain ways. The first drawback of the present study was lack of information provided by the studies with regard to gender of the recipients and donors, living status of the donors and history of kidney transplant among the patients. The missing data could affect the significant heterogeneity between studies and (to some extend) the observed difference in the reported survival rates in Iran and other countries.
Conclusion
With few important exceptions, the survival rates of allografts and kidney transplant patients are comparable to reports from several large centers in the world. The results of this review can provide basic evidence for the reconsideration of treatment strategies in various medical sectors. The results emphasize the need for more extensive programs for the evaluation of treatment strategies in CKD.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This study was supported financially by Shiraz University of Medical Sciences, Shiraz, Iran (Grant Number: 97-01-04-19006).
Footnotes
Data availability
Additional information is available. All readers may contact the corresponding author to provide all supplementary and additional data.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Ghelichi Ghojogh M, Taghizadeh Afshari A, et al. (2017). The Effect of Body Mass Index on Patient and Graft Survival Rate in Kidney Transplanted Patients in Iran. Nephro-Urol Mon, 9(4): e14386. [Google Scholar]
- 2.El Nahas AM, Bello AK. (2005). Chronic kidney disease: the global challenge. lancet, 365:331–40. [DOI] [PubMed] [Google Scholar]
- 3.Florit E, Diekmann F, Budde K, et al. (2015). Living Donor Transplantation: Long-Term Evolution Related to Age Matching. Transplantation proceedings, Elsevier, pp. 2346–2350. [DOI] [PubMed] [Google Scholar]
- 4.Einollahi B. (2004). Iranian experience with the non-related renal transplantation. Saudi J Kidney Dis Transpl, 15:421–428. [PubMed] [Google Scholar]
- 5.Jahromi SE, Ahmed F, Pourahmad S, et al. (2019). Predictors of peritoneal dialysis associated peritonitis; application of the zero-inflated negative binomial model. J Nephropathol, 8:e36. [Google Scholar]
- 6.Zeraati AA, Nazemian F, Takalloo L, et al. (2016). The relationship between serology of hepatitis E virus with liver and kidney function in kidney transplant patients. EXCLI J, 15:343–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahdavi-Mazdeh M, Rouchi AH, Norouzi S, et al. (2007). Renal replacement therapy in Iran. Urol J, 4:66–70. [PubMed] [Google Scholar]
- 8.Ghojogh MG, Salarilak S, Afshari AT, et al. (2018). Impact of type of donor on graft and patient survival rate in kidney transplanted patients in Iran. J Renal Inj Prev, 7:264–268. [Google Scholar]
- 9.Heldal K, Hartmann A, Grootendorst DC, et al. (2010). Benefit of kidney transplantation beyond 70 years of age. Nephrol Dial Transplant, 25:1680–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jawoniyi O, Gormley K, McGleenan E, Noble HR. (2018). Organ donation and transplantation: awareness and roles of healthcare professionals—a systematic literature review. J Clin Nurs, 27:e726–e738. [DOI] [PubMed] [Google Scholar]
- 11.Tekin S, Yavuz H, Yuksel Y, et al. (2015). Kidney transplantation from elderly donor. Transplant Proc, 47(5):1309–11. [DOI] [PubMed] [Google Scholar]
- 12.Abbaszadeh S, Nourbala MH, Taheri S, et al. (2008). Renal transplantation from deceased donors in Iran. Saudi J Kidney Dis Transpl, 19:664–8. [PubMed] [Google Scholar]
- 13.Hassanzadeh J, Hashiani A, Rajaeefard A, et al. (2010). Long-term survival of living donor renal transplants: A single center study. Indian J Nephrol, 20:179–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vester U, Kranz B, Testa G, et al. (2004). Medical and surgical aspects of pediatric renal transplantation using living donors. Transplant Proc, 36(5):1308–10. [DOI] [PubMed] [Google Scholar]
- 15.Lee C-Y, Yang C-Y, Lin W-C, et al. (2020). Prognostic factors for renal transplant graft survival in a retrospective cohort of 1000 cases: The role of desensitization therapy. J Formos Med Assoc, 119(4):829–837. [DOI] [PubMed] [Google Scholar]
- 16.Chhabra D, Grafals M, Skaro AI, Parker M, Gallon L, et al. (2008). Impact of anemia after renal transplantation on patient and graft survival and on rate of acute rejection. Clin J Am Soc Nephrol, 3:1168–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Weerd AE, Betjes MG. (2018). ABO-incompatible kidney transplant outcomes: a meta-analysis. Clin J Am Soc Nephrol, 13:1234–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Shamseer L, Clarke M, et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev, 4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Penson D, Krishnaswami S, Jules A. Evaluation and treatment of cryptorchidism. Rockville (MD): Agency for Healthcare Research and Quality (US); 2012. Dec. Report No.: 13-EHC001-EF. [PubMed] [Google Scholar]
- 20.Bagos PG, Nikolopoulos GK. (2009). Mixed-effects Poisson regression models for meta-analysis of follow-up studies with constant or varying durations. The International Journal of Biostatistics, 5(1):21. [Google Scholar]
- 21.Harris RJ, Deeks JJ, Altman DG, et al. (2008). Metan: fixed-and random-effects meta-analysis. The Stata Journal, 8:3–28. [Google Scholar]
- 22.Lin L, Chu H. (2018). Quantifying publication bias in meta-analysis. Biometrics, 74:785–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hassani Z, Emami N. (2018). Prediction of the Survival of Kidney Transplantation with imbalanced Data Using Intelligent Algorithms. Computer Science Journal of Moldova, 26(2):77. [Google Scholar]
- 24.Wang D, Xu Tz, Chen Jh, et al. (2009). Factors influencing second renal allograft survival: a single center experience in China. Transpl Immunol, 20:150–154. [DOI] [PubMed] [Google Scholar]
- 25.Dinis P, Nunes P, Marconi L, et al. (2014). Kidney retransplantation: removal or persistence of the previous failed allograft? Transplant Proc, 46(6):1730–4. [DOI] [PubMed] [Google Scholar]
- 26.Segoloni G, Messina M, Basso E, et al. (2009). Kidney retransplantation: indications and limits. G Ital Nefrol, 26(2):191–200. [PubMed] [Google Scholar]
- 27.Kazemeyni S, Aghighi M. (2012). Organ procurement from deceased donors and its impact on organ transplantation in Iran during the first ten years of cadaveric transplantation. Int J Organ Transplant Med, 3(3):125–9. [PMC free article] [PubMed] [Google Scholar]
- 28.Vergoulas G, Ioannidis I, Nikodimopoulou M, et al. (2008). Outcomes of kidney transplantation in Greek and Albanian patients: a single centre experience. Hippokratia, 12(3):176–80. [PMC free article] [PubMed] [Google Scholar]
- 29.Wang JH, Skeans MA, Israni AK. (2016). Current status of kidney transplant outcomes: dying to survive. Adv Chronic Kidney Dis, 23:281–286. [DOI] [PubMed] [Google Scholar]
- 30.Pallet N, Thervet E, Alberti C, et al. (2005). Kidney transplant in black recipients: are African Europeans different from African Americans? Am J Transplant, 5:2682–2687. [DOI] [PubMed] [Google Scholar]
- 31.Tang Y, Zhang Y, Jia B. (2001). Analysis of 2200 kidney transplantations. Zhonghua Yi Xue Za Zhi, 81:82–85. [PubMed] [Google Scholar]
- 32.Adams J, Mehls O, Wiesel M. (2004). Pediatric renal transplantation and the dysfunctional bladder. Transpl Int, 17:596–602. [DOI] [PubMed] [Google Scholar]
- 33.Loucaidou M, Prasad S, Van Tromp J, et al. (2004). Outcome of renal transplantation in South Asian recipients is similar to that in non-Asians. Transplantation, 78:1021–1024. [DOI] [PubMed] [Google Scholar]
- 34.Chen JH, Shen W, He Q, et al. (2004). [Pediatric renal transplantation: clinical analysis of 23 cases]. Zhonghua Wai Ke Za Zhi, 42:1100–3. [PubMed] [Google Scholar]
- 35.Higgins R, West N, Edmunds M, et al. (1997). Effect of a strict HLA matching policy on distribution of cadaveric kidney transplants to Indo-Asian and white European recipients: regional study. BMJ, 315:1354–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Richardson C, Butterworth P, Feehally J, Nicholson M. (1998). Results of renal transplantation in Indo-Asian recipients. Br J Surg, 85(5):653–4.9635814 [Google Scholar]
- 37.Jeffrey RF, Woodrow G, Mahler J, et al. (2002). Indo-Asian experience of renal transplantation in Yorkshire: results of a 10-year survey. Transplantation, 73:1652–1657. [DOI] [PubMed] [Google Scholar]
- 38.Collins AJ, Foley R, Herzog C, et al. (2008). Excerpts from the United States Renal Data System 2007 annual data report. Am J Kidney Dis, 51(1 Suppl 1):S1–320. [DOI] [PubMed] [Google Scholar]
- 39.Abdi E, Savaj S, Nejadgashti H, et al. (2006). Renal Transplantation Results in Hashemi Nejad Hospital during 1996–2005 and its Comparison with that of 1986–1996. Razi J Med Sci, 13:113–120. [Google Scholar]
- 40.Becker BN, Becker YT, Pintar TJ, et al. (2000). Using renal transplantation to evaluate a simple approach for predicting the impact of end-stage renal disease therapies on patient survival: observed/expected life span. Am J Kidney Dis, 35:653–659. [DOI] [PubMed] [Google Scholar]
- 41.Herzog CA, Ma JZ, Collins AJ. (2000). Long-term survival of renal transplant recipients in the United States after acute myocardial infarction. Am J Kidney Dis, 36:145–152. [DOI] [PubMed] [Google Scholar]
- 42.Ojo AO, Hanson JA, Wolfe RA, et al. (2000). Long-term survival in renal transplant recipients with graft function. Kidney Int, 57:307–313. [DOI] [PubMed] [Google Scholar]
- 43.Rubin RH. (1993). Infectious disease complications of renal transplantation. Kidney Int, 44:221–36. [DOI] [PubMed] [Google Scholar]
- 44.Hariharan S, Johnson CP, Bresnahan B A, et al. (2000). Prediction of renal allograft function with early doppler ultrasonography. N Engl J Med, 342(9):605–12. [DOI] [PubMed] [Google Scholar]
- 45.Abbud-Filho M, Ramalho H, Barberato J, et al. (1998). Factors influencing the outcome of pediatric renal transplantation at a single center. Transplant Proc, 30(6):2871. [DOI] [PubMed] [Google Scholar]
- 46.Briganti EM, Wolfe R, Russ GR, et al. (2002). Graft loss following renal transplantation in Australia: is there a centre effect? Nephrol Dial Transplant, 17(6):1099–104. [DOI] [PubMed] [Google Scholar]
- 47.Orsenigo E, Socci C, Carlucci M, et al. (2005). Multivariate analysis of factors affecting patient and graft survival after renal transplant. Transplant Proc, 37(6):2461–3. [DOI] [PubMed] [Google Scholar]
- 48.Courtney A, McNamee P, Maxwell A. (2008). The evolution of renal transplantation in clinical practice: for better, for worse? QJM, 101:967–978. [DOI] [PubMed] [Google Scholar]
- 49.Feyssa E, Charlotte J-B, Ellison G, et al. (2009). Racial/Ethnic Disparity in Kidney Transplantation Outcomes: Influence of Donor and Recipient Characteristics. J Natl Med Assoc, 101:111–115. [DOI] [PubMed] [Google Scholar]
- 50.Pugliese O, Quintieri F, Mattucci DA, et al. (2005). Kidney graft survival in Italy and factors influencing it. Prog Transplant, 15:385–391. [DOI] [PubMed] [Google Scholar]
- 51.Almasi Hashiani A, Rajaeefard A, Hassanzade J, Salahi H. (2010). Survival analysis of renal transplantation and its relationship with age and sex. Koomesh, 11:302–306. [Google Scholar]