Dear Editor-in-Chief
Chronic kidney disease (CKD) is an established predictor for atheroegenesis, because of a high aggregation in the affected population of traditional risk factors (dyslipidaemia, hypertension, diabetes) and non-traditional risk (microalbuminuria, oxidative stress, anaemia, and hyperparathyroidism), these risk factors having an additive effect on the cardiovascular morbidity (1). Once acute coronary syndrome (ACS) develops, CKD is associated with a an increased mortality, studies made on large cohorts reporting a mortality of 44% in patients with ACS and CKD at 1 month compared to a mortality of 13% in patients with ACS without CKD (2). Several reasons have been identified as potential causes of higher mortality in patients with CKD and ACS. CKD patients have statistically higher frequency of other comorbidities and data from literature confirms that is this category of patients there is an underutilisation of beneficial therapeutic interventions such as antithrombotic agents or percutaneous coronary interventions and generally a less aggressive treatment because of clinician’s fear of potential complications (3). There is another intriguing aspect that limits the knowledge of the beneficial interventions in patents with CKD and ACS, the fact that these patients are frequently excluded from randomized control trails (4).
In our study, we aimed to compare the mortality and morbidity of patients with CKD and ACS compared to patients with ACS without CKD from northwestern Romania. The study included 435 patients with ACS, 209 patients with CKD and 226 without CKD, admitted in the Cardiology Department of the Clinical County Emergency Hospital of Oradea, Romania from 1 January 2015 to 31 December 2017.
CKD group included patients with a GFR<60ml/min/1.73 m2 that could be documented in the previous year before current presentation for ACS. Acute kidney injury (AKI) was defined as an increase in serum creatinine during the current presentation ≥0.3 mg/dl and acute heart failure as Killip class II, III or IV. Patients were fallowed for 30 days from discharge. Patients with ACS and CKD had statistically significant higher prevalence of chronic comorbidities: hypertension, diabetes mellitus type 2, dyslipidaemia, peripheral artery disease than patients with ACS without CKD (Table 1). Anaemia was statistically significant more present in patients with CKD than in patients without CKD. An important fact was the presence of a conservative in patients with CKD. Percutaneous revascularisation was statistically significant less used in patients with CKD compared to patients without CKD (53.39% vs. 63.72%, P=0.03), surgical revascularisation was used in similar percentages (15.79% vs. 16.81%, P=0.77), while conservative management was statistically significant more used in patients with CKD than in patients without CKD (30.62% vs. 19.47%, P<0.01).
Table 1:
Chronic comorbidities in patients with ACS with or without CKD
| Parameter | CKD (n=209) | Without CKD (n=226) | p |
|---|---|---|---|
| Hypertension (%) | 84.21 | 63.27 | <0.01 |
| Diabetes type II (%) | 58.85 | 33.62 | <0.01 |
| COPD (%) | 10.04 | 5.35 | 0.06 |
| Stroke (%) | 11 | 7.58 | 0.21 |
| Dyslipidemia (%) | 60.09 | 49.55 | 0.02 |
| Peripheral artery disease (%) | 20 | 4.9 | <0.01 |
Killip classes II, III and IV were statistically significant more prevalent in patients with ACS and CKD. Killip class I was identified in 63.15% of individuals with CKD and 86.28% of individuals without CKD (P<0.01). Killip class II in 13.87% of individuals with CKD and 4.86% of individuals without CKD (P <0.01). KIlip III in 15.31% of patients with CKD and 6.63% of patients without CKD (P <0.01) while Kilip IV class was identified in 7.65% of patients with CKD and 2.1% of patients without CKD (P <0.01).
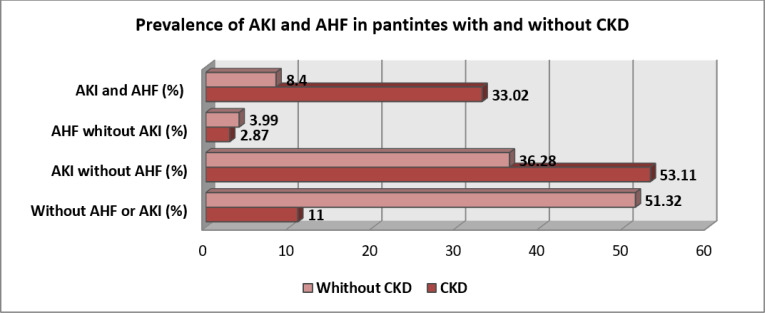
Fig. 1 demonstrates statistically significant higher rates of AKI without AHF and AKI with AHF in patients with CKD compared to patients without CKD. The association of AKI and AHF represents a particular entity, the cardio-renal syndrome. The mortality in patients with CKD was statistically significant higher than in patients without CKD. At 30th days, 13.39% of patients with CKD (28 deaths) died and 6.11% (14 deaths) of patients without CKD died (P <0.05).
Fig. 1:
Prevalence of AHF, AKI alone or in combination in patients with ACS with or without CKD
In conclusion, the presence of CKD is associated with numerous chronic comorbidities, with a high incidence of cardio-renal syndrome, defined as the combination of AKI and AHF, and with a higher mortality in patients with ACS. Physicians have a conservative attitude towards patients with ACS and CKD compared with patients with normal renal function, a fact that, as shown in literature, is one of the factors that decreases the survival of these patients.
Footnotes
Conflict of interest
The authors declare that they do not have any conflict of interest.
References
- 1.Subbiah AK, Chhabra YK, Mahajan S. (2016). Cardiovascular disease in patients with chronic kidney disease: a neglected subgroup. Heart Asia, 8(2):56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marenzi G, Cabiati A, Assanelli E. (2012). Chronic kidney disease in acute coronary syndromes. World J Nephrol,1(5):134–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rihal CS, Textor SC, Grill DE, et al. (2002). Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation, 105:2259–2264. [DOI] [PubMed] [Google Scholar]
- 4.Rodrigues FB, Bruetto RG, Torres US, et al. (2010). Effect of kidney disease on acute coronary syndrome. Clin J Am Soc Nephrol, 5(8):1530–6. [DOI] [PubMed] [Google Scholar]