Abstract
Background:
Breast cancer is responsible for up to 25% of all cancers in Iran. The age at diagnosis of Iranian breast cancer patients starts a decade earlier than most of developed countries. This study aimed to evaluate the mean age at diagnosis of Iranian breast cancer patients.
Methods:
In this systematic review and meta-analysis, the mean age at diagnosis of Iranian breast cancer patients and its pattern between 2008 and 2017, were evaluated. All papers with age at diagnosis of histopathological verified breast cancer patients were considered eligible to enter to the analysis. We used databases including Medline/PubMed, Scopus, Embase, Cochrane Library, Iranmedex and SID for the search process. The meta-analysis was performed only on studies with separate data for female patients, using random-effects model, Mantel and Haenszel method and the Comprehensive Meta-analysis software.
Results:
Finally, 92 studies with 19,784 patients (both-genders) were included. The mean age at diagnosis had increased from 47.93 (2008) to 49.91 (2016) years. The meta-analysis was done on 78 studies containing of 15,071 female patients and the mean age at diagnosis was 46.76±1.19. There was a wide range of age at diagnosis within different provinces. The mean age at Hamadan and Khuzestan provinces were the lowest and highest, respectively (42.48±7.96 vs. 51.00±11.47). The heterogeneity of studies was statistically significant (I2=99.744).
Conclusion:
Mean age at diagnosis of Iranian women with breast cancer was 46.76±1.19. There was an increasing pattern in mean age of diagnosis at breast cancer patients within the past 10 years.
Keywords: Age at diagnosis, Breast cancer, Iran, Meta-analysis
Introduction
Breast cancer, with nearly 1.7 million new cases annually, is the most common malignancy among female population worldwide; corresponding to about 25% of all cancers among women and 12% of all new cancer cases. Over the past fifty years, changes in human lifestyle have led to the occurrence and spread of breast cancer throughout the world (1, 2). Tumor characteristics such as size, tumor grade, receptor status, and lymph node involvement are known to be the most important prognostic factors in breast cancer (3, 4).
In Iran, breast cancer is responsible for up to 25% of all cancers (5). In a recent meta-analysis, the one-, five-, and ten-year survival rates of breast cancer in Iran were estimated 95.8%, 69.5%, and 58.1%, respectively (6).
One of the reasons patients tend to treat the cancer at the advanced stages and accompanying high mortality rate of diagnosed patients is lack of screening tests to facilitate early diagnosis (7, 8). Screening mammography has played a key role in reducing breast cancer mortality. By identifying subset of cancers diagnosed before they reach clinical presentation, intervention is more likely to result in a long-term survival (9, 10).
The role of age at diagnosis as a prognostic factor is still controversial because there is no consensus on age thresholds to define “young” age breast cancer (4, 11–14). Low life expectancy, especially in developing countries, is relatively associated with high population of young age breast cancer which accounts for up to 30% of the total number of breast cancer patients, based on various age definitions (15).
The mean age of breast cancer diagnosis among female population in Iran is about 10–15 yr lower than that reported in developing countries (4, 16). According to the Iranian national reports, the mean age at diagnosis has decreased. It started a decade earlier than developed countries (5, 6, 17). Furthermore, more than 30% of the patients are under 30 yr old at the time of diagnosis (5).
Considering the young population and increasing tendency of breast cancer incidence in Iran (18, 19), current systematic review and meta-analysis was conducted to assess the age at diagnosis of breast cancer patients in Iran during past ten years (2008–2017), and achieve a better understanding of diagnosis age distribution in order to guide healthcare authorities.
Methods
Study Design and Search Protocol
Present systematic review and meta-analysis study was conducted at Community and Family Medicine Department of Tabriz University of Medical Sciences (Tabriz, Iran) between 2018 (Jan) and 2019 (Sep) following guidelines of PRISMA-P statement (20, 21). The mean age at diagnosis of breast cancer patients and its trend in Iran within a ten-year’ period from 2008–2017 was evaluated. All of published papers with information about age of Iranian breast cancer patients at the time of diagnosis were considered eligible in our study. Inclusion criteria were consisted of histopathological confirmation of breast cancer and mentioning the phrase “age at diagnosis” or “newly diagnosed” or their synonyms. Exclusion criteria were consisted of studies with patients of specific age group, patients with specific characteristics or features which could affect the diagnosis of breast cancer, studies with only male gender patients and the studies in which the age was reported more than 3 months after the time of diagnosis (The ages mentioned in the studies were considered as age at diagnosis if the current age was less than 3 months away from the age of diagnosis).
The search protocol defined by using the main keywords “Breast Cancer”, “Breast Neoplasm”, “Ductal Carcinoma”, “Breast Carcinoma”, “Lobular Carcinoma”, “Paget’s Disease of Nipple” and their synonyms. Also, all the subtypes of breast carcinoma with specific definition were added to the search protocol. In order to limit the search results to Iran, the keyword “Iran” and the name of each cities of this region was considered in search protocol.
Databases used were consisted of Medline/PubMed, Scopus, Embase, and Cochrane Library as selected databases. Moreover, Iranmedex and SID were used to look for published manuscript in Persian language. The publication date was limited between 2008 and 2017 and for the papers with overlap of mentioned period, they were considered eligible if the majority of time-period of the study was within that period. Moreover, only the original studies have been considered eligible for inclusion, so letters to editorials, commentaries, perspectives, reviews, case studies and conference abstracts were excluded.
The search protocol confined to English and Persian language. It has been done at 20th of Jan 2018 and only human studies were entered.
Study Selection and Data Extraction Process
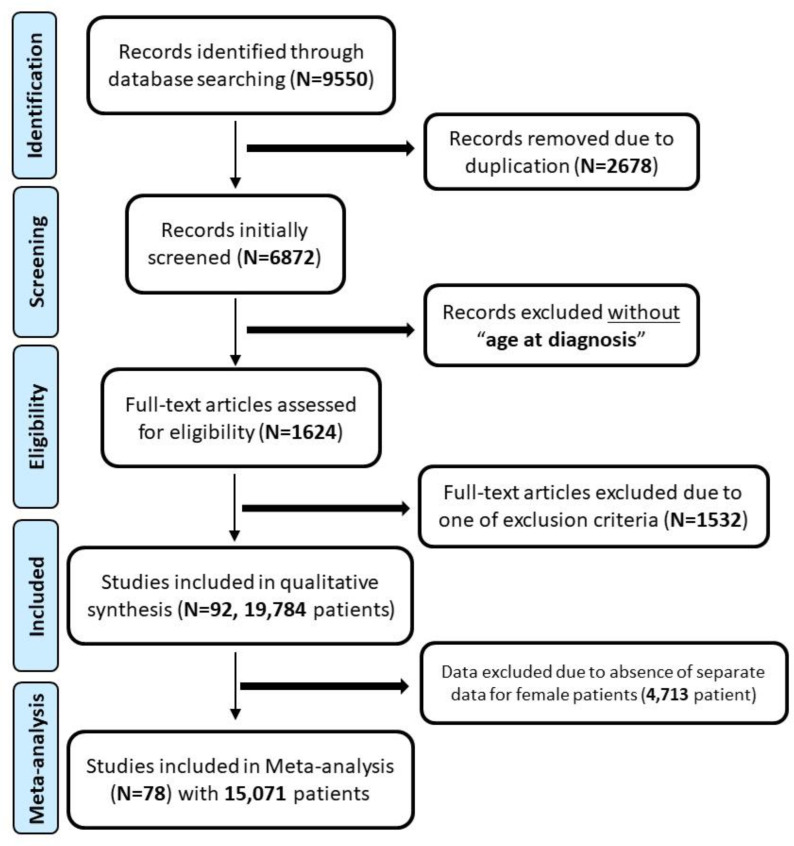
The search process will be executed in all mentioned databases separately and the articles will be compiled using EndNote software (Package for Windows ver. 7.2). After deleting the duplicated articles, in order to further narrow down the search, titles and abstracts of entered studies will be inspected by two researchers independently and disagreements will be resolved by consensus with a senior researcher. After initial assessment of titles and abstracts, full-text articles were collected and evaluated for eligibility by two authors (MNB and RP) independently, resolving the disagreement by supervision of the senior researchers (MA and MG). The complete flowchart of included studies is shown in Fig. 1.
Fig. 1:
Flow diagram of study about age at diagnosis in breast cancer patients
Reporting Quality Assessment
The QUADAS-2 tool was used to assess the methodological quality of selected studies (22), and the meta-analysis was performed on eligible studies which contained separate data on female patients. Bias analysis was only performed based on the characteristic of the included study, which was “age at time of diagnosis”.
Study Analysis and Synthesis of Results
After examining the eligibility of manuscripts, the included articles were analyzed by the research team. Period of the study, study subjects, region of study population and age of the patients at time of diagnosis at both genders and separate data for female patients were investigated. In addition, some studies’ authors were contacted to obtain additional information consisted of separate data for female patients, separate data for the period after 2008 and also for the confirmation of “time of diagnosis” for the mentioned age at the manuscripts.
Statistical analysis
The required information for the systematic review was extracted and summarized using extraction table in Microsoft Office Excel software. Meta-analysis was performed using random-effects model and Mantel and Haenszel method and the Comprehensive Meta-analysis software (CMA ver. 2.0, Englewood, NJ, USA) was used to conduct the meta-analysis. The study-to-study variance (tau-squared) was assumed to be the same for all subgroups - this value is computed within subgroups and then pooled across subgroups. In case median and interquartile range of the variables were expressed, to aggregate data in a meta-analysis, Hozo et al. method was used to convert the median and interquartile range to mean and standard deviation (23). Forest plot diagrams was use to illustrate the study findings in which the area of each square will proportionally size to signify the sample size and the lines drawn in each square represent 95% confidence interval for the age of breast cancer patients in each of the studies (24, 25). A funnel plot was derived to evaluate the publication bias visually for each analysis, and the I2 value was used to measure the heterogeneity of the included studies (26).
Results
Literature search and study selection
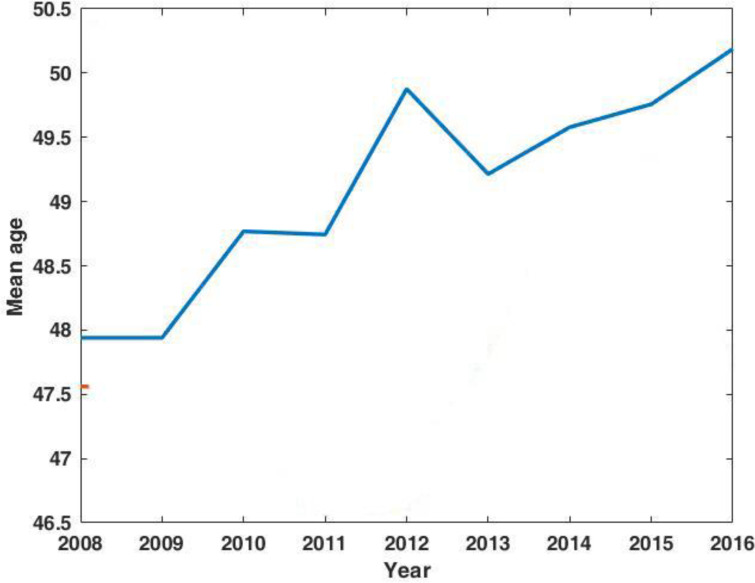
The initial search resulted in 9,950 records, which after removing duplications, full-text assessment, evaluation of eligibility for inclusion and quality assessment, 92 studies with 19,784 patients were included in the systematic review. Details of 92 included studies are presented in Supplementary Material 1. The flowchart of the study is shown in Fig. 1. The trend of mean age at diagnosis of breast cancer of both genders in 2008–2016 period is shown in Fig. 2. Data about last year of study (2017) was excluded from this part, due to low number of included patients. The mean age of diagnosis had increased from 47.93 to 49.91 yr through this period.
Fig. 2:
Time trend of age at diagnosis among patients with breast cancer in both genders
Meta-Analysis
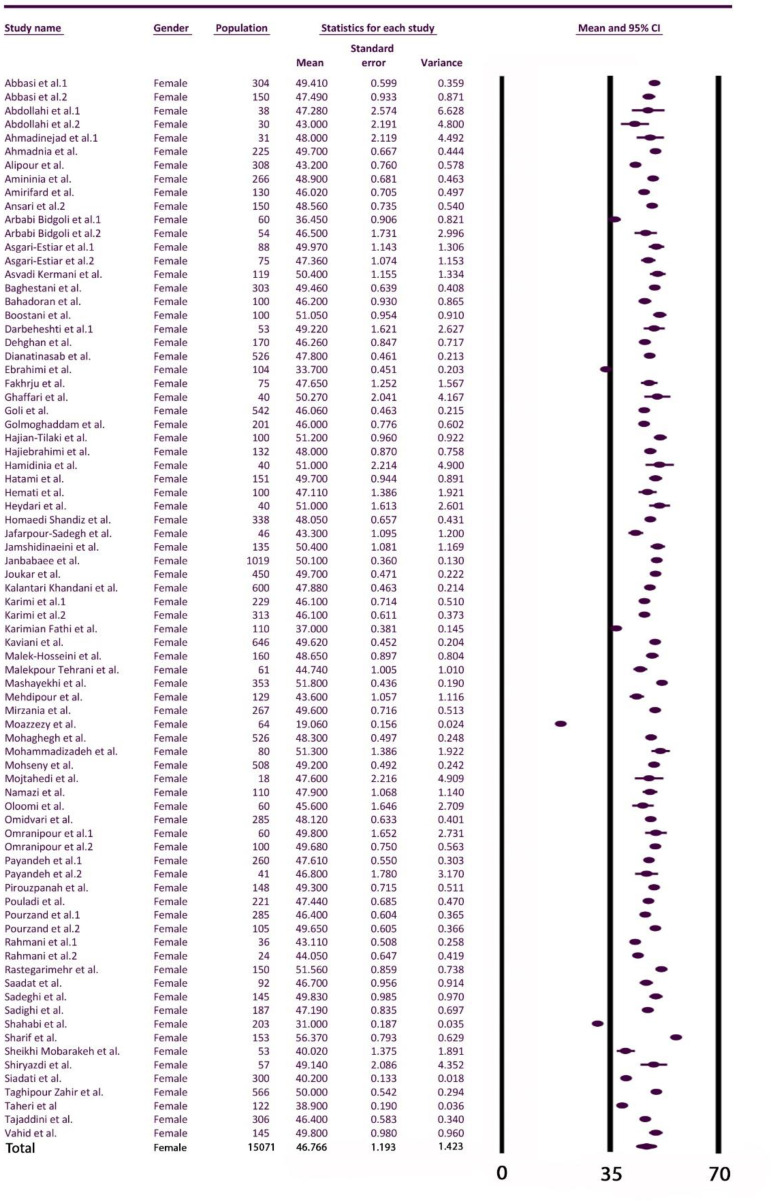
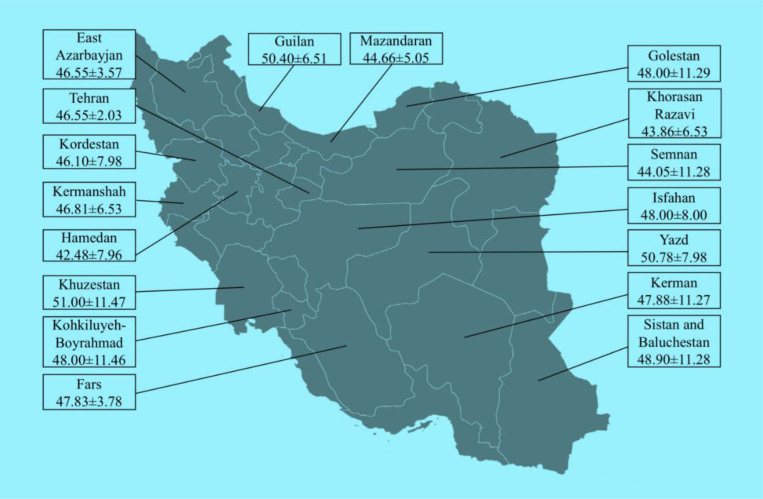
Critical appraisal was accomplished for 92 included studies, and 14 studies were excluded to enter to the meta-analysis due to absence of separated data for women. Therefore, 4,713 patients excluded due to male gender or absence of separate data for female patients, and the meta-analysis was conducted on data from 78 studies containing of 15,071 patients. The mean age at diagnosis of breast cancer among included female patients was 46.76±1.19; the forest plot regarding the included studies is shown in Fig. 3. The mean age at diagnosis for 17 provinces of Iran reported in the included articles are shown in Fig. 4 and studies categorized based on the provinces are shown in Supplementary Material 2. There was a wide range of age at time of diagnosis within different provinces in which Hamadan province with mean of 42.48±7.96 and Khuzestan Province with mean of 51.00±11.47 had the lowest and highest age, respectively, although there was no statistically significant difference in mean age at diagnosis among the provinces (P=0.99).
Fig. 3:
Forest plot of included studies to Meta-analysis regarding age at diagnosis
Fig. 4:
Mean age at diagnosis of breast cancer patients in different provinces of Iran
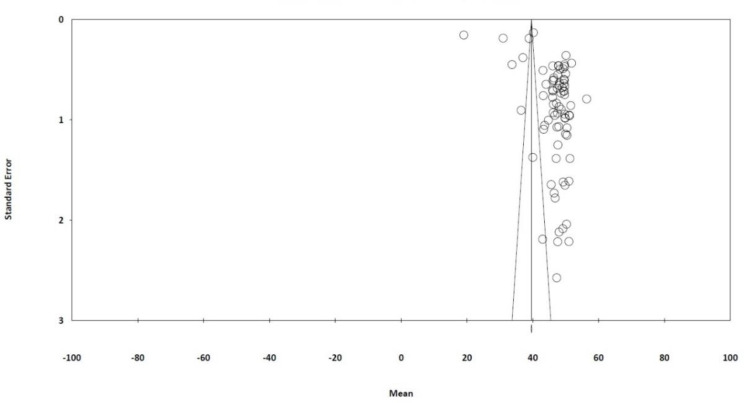
The heterogeneity of the included studies is shown in Fig. 5 using funnel plots; there was a statistically significant publication bias (Egger’s regression intercept=17.99, I2=99.744).
Fig. 5:
Funnel plot of the current meta-analysis of breast cancer patients’ age at diagnosis
Discussion
The mean age of patients with breast cancer at the time of diagnosis is 46.76±1.19 within the study period. Moreover, the mean age at the time of diagnosis has been increased between 2008 and 2016. There was high heterogeneity (I2=99.744) through included studies expected due to different types of study design and wide spectrum of the purposes for performing the studies.
This was the first systematic review with large included sample size (over 15,000 female patients) through past years in Iran, which could present an overview of estimate age of diagnosis time in breast cancer patients. However, our results could have some biases since we only considered studies without any limitation in patients’ selection part in order to generalize the study population. Therefore, the studies evaluating the specific age groups (both young and elderly groups of women) (27, 28), postmenopausal women (29), high risk patients (30) or studies containing patients with specific immunohistochemistry profile (31) have been excluded. Moreover, another limitation was geographic distribution of included studies, in which the included patients to the meta-analysis were from 17 out of 31 provinces of Iran. This could cause bias to generalize the finding to the whole country.
Based on WHO recommendation and guidelines, role of cancer registries in providing information on prevalence, monitoring and trends in mortality and morbidity of cancer patients is remarkable (32). Therefore, extraction of data regarding age at diagnosis time from registries’ datasets would be more accurate comparing with our study as the meta-analysis of performed studies. However, based on limitations of current cancer registries in Iran to cover the whole country’s population (33), the results of current study could stand as primary analysis of breast cancer patients in Iran. Besides, our meta-analysis focuses only on female gender, since male breast cancer represents approximately 1% of all breast cancer worldwide (34) and previous studies from Iran showed higher age at diagnosis in men (ranging from 57.9 to 60.3) (35–37).
A similar systematic review, evaluating the age at diagnosis of breast cancer through Arab nations, have been conducted on 18 studies from 11 Arabic countries in which they found the average of 48±2.8 (range 43–52) for 7,455 patients (12). They included both genders out of papers published until 2008 in the final analysis, while our study included only female patients and studies published after 2008. Considering the higher age of male breast cancer comparing with female patients (38), and different time periods, the results of two studies are almost comparable due to same design and high heterogeneity of included population.
Comparing results of current study with other Asian and African countries consisted of Turkey (19,503 patients with mean age of 51.8±12.6) (39), Egypt (3,819 patients with mean age of 51.0±11.5) (40), Iraq (536 Iraqi Kurdish patients with mean age of 49.42±11.66) (41), South Korea (28,989 patients with mean age of 48.3±10.5) (42), Oman (1,248 female patients with mean age of 49.05 (range: 17–99)) (43) and Tunisia (7,736 patients with mean age of 50.2 (range 22–91)) (44), showed that the age at diagnosis of breast cancer in Iran is lower compared to these countries.
However, the age at diagnosis in Iran (46.76±1.19) appeared to be lower near to one decade than American continent, for example United States (110,153 patients with mean age of 58.4), Canada (36,455 patients with mean of 60.1), Latin American countries (25,876 patients from Brazil, Colombia, Costa Rica and Ecuador with mean age of 53.7) (45) and Mexico (3,488 patients with mean age of 55.7±13.7) (46).
Previous studies from Iran related to time before our study, reported wide range of age at time of diagnosis (4, 37, 47–50). Comparing the current results with other studies including Afsharfard et al. (49.4±13.1) (47), Haghighat et al. (45.9±10.5) (48), Baghestani et al. (48.13±10.77) (49), Vostakolaei et al. (46.0±12.0) (4), Jazayeri et al. (49.6) (37), Kadivar et al. (50±12) (50), showed that the diagnosis age of breast cancer patients in Iran is not decreased through recent years.
Comparing the results between different provinces shows a great difference regarding the mean age at diagnosis time (Hamadan Province with mean of 42.48±7.96 vs. Khuzestan Province with mean of 51.00±11.47) which indicate that each province should evaluate and compare independently. Previous studies from Tehran province (51–53) showed wide range of diagnosis age (46.3–51.34), and the result of current study for this province (46.55±2.33) is within the same range.
In other individual comparisons of provinces with previous studies, the age at diagnosis in our study was higher in Guilan (54), Golestan (55), Yazd (56), and Fars (57) provinces. However, the only province with higher age at diagnosis in previous study (58) compared to our study, was Khorasan Razavi Province (43.86±6.53 vs. 47.88±10.86).
One of the regions, which had close results to the mean age of diagnosis at the whole country (46.76±1.19), was East Azerbaijan with mean age of 46.55±3.57. The previous study from this region reported the mean age at diagnosis of 47.2 (CI: 46.6 to 47.7) for the patients registered from 1988–2008 (16). Moreover, other studies from northwest of Iran (West Azerbaijan Province with mean age of 47.83±10.76 (59), and Ardabil province with mean age of 45.5±12.3 (17)), showed that this area could acted as candidate in future pilot studies. Detailed comparison between the results of the current study with previous studies is summarized at Table 1.
Table 1:
Comparison of results of current study with previous published papers
| Authors | Country/Province | Time Period | Population | Age at diagnosis* | Gender |
|---|---|---|---|---|---|
| Present study | Iran (17 provinces) | 2008–2017 | 15,071 | 46.76±1.19 | Female |
| Najjar et al. (12) | Arab nations | 1985–2008 | 7,455 | 48±2.8 | Both |
| Özmen et al. (39) | Turkey | 2005–2017 | 19,503 | 51.8±12.6 | Female |
| Schlichting et al. (40) | Egypt | 2004–2008 | 3,819 | 51.0±11.5 | Female |
| Molah Karim et al. (41) | Iraq (Kurdish) | 2011–2013 | 536 | 49.42±11.66 | Female |
| Lee et al. (42) | South Korea | 1993–2009 | 28,989 | 48.3±10.5 | Female |
| Mehdi et al. (43) | Oman | 1996–2010 | 1,248 | 49.05 | Female |
| Missaouib et al. (44) | Tunisia | 1993–2007 | 7,736 | 50.2 | Female |
| Franco-Marina et al. (45) | United States | 2003–2007 | 1,110,153 | 58.4 | Female |
| Canada | 36,455 | 60.1 | |||
| Brazil | 4,651 | 51.6 | |||
| Colombia | 7,469 | 54.3 | |||
| Costa Rica | 10,225 | 54.4 | |||
| Ecuador | 3,526 | 53.9 | |||
| Salinas-Martínez et al. (46) | México | 2003–2012 | 3,488 | 55.7±13.7 | Both |
| Afsharfard et al. (47) | Iran | 1994–2009 | 714 | 49.4±13.1 | Female |
| Haghighat et al. (48) | Iran | 1997–2007 | 615 | 45.9±10.5 | Female |
| Baghestani et al. (49) | Iran | 1998–2013 | 366 | 48.13±10.77 | Female |
| Vostakolaei et al. (4) | Iran | 1999–2001 | 1,500 | 46.0±12.0 | Female |
| Jazayeri et al. (37) | Iran | 2000–2010 | 50,590 | 49.6 | Female |
| Kadivar et al. (50) | Iran | 2002–2011 | 428 | 50±12 | Female |
| Bab et al. (61) | Iran | 2000–2005 | 20,791 | 49.4±12.6 | Both |
| Mousavi et al. (53) | Iran / Tehran | 1998–2001 | 986 | 51.34±12.46 | Female |
| Harirchi et al. (51) | Iran / Tehran | 1985–2005 | 2946 | 48.39 | Female |
| Abdollahi (52) | Iran / Tehran | 1986–2006 | 568 | 46.3±11.1 | Both |
| Eivazi et al. (16) | Iran / Tabriz | 1988–2008 | 1746 | 47.2 | Female |
| Lakzaei et al. (59) | Iran / Urmia | 2001–2013 | 1402 | 47.83±10.76 | Female |
| Fallahzadeh et al. (56) | Iran / Yazd | 2002 | 200 | 48.3±11.7 | Female |
| Taheri et al. (55)** | Iran / Golestan | 2004–2009 | 1,101 | 46 (16)** | Female |
| Fouladi et al. (17) | Iran / Ardabil | 2003 | 161 | 45.5±12.3 | Both |
| Ghavami et al. (58) | Iran / Mashhad | 2001–2007 | 550 | 47.88±10.86 | Female |
| Heydari et al. (57) | Iran / Fars | 2001–2006 | 863 | 46.3±11.5 | Female |
| Najafi et al. (54) | Iran / Guilan | 2001–2010 | 592 | 47.9±9.6 | Both |
Data were shown as Mean ± standard deviation.
Date from other registries (Khorasan Razavi, Mazandaran and Tehran) were added and were shown as median (interquartile range)
Overall comparison of current study from Iran with other studies, indicate that the age at diagnosis of breast cancer patients has been increased in Iran recently. However, it is still considerably lower than other comparable countries and even much lower than western countries. Most of Iranian breast cancer patients were diagnosed beyond initial stages (1), and proven role of age at diagnosis in patients overall survival (60), the necessity of structured screening program to detect early stage patients in lower ages is much more highlighted
Further researches on characteristics of breast cancer patients through national cancer registries would provide information that is more precise for healthcare policy makers. Survival analysis of diagnosed patients as well as detection of prognostic factors could offer a great overview of current situation of these patients in Iran.
Conclusion
The mean age at diagnosis of breast cancer patients was 46.76±1.19 yr, which is much lower in comparison with other similar countries. There was an increasing pattern in age at diagnosis of patients during past 10 years. Moreover, there was a considerable difference among provinces of Iran. The age at diagnosis in Hamedan Province as the lowest case (42.48±7.96 yr) was around one decade lower than Khuzestan Province with the highest (51.00±11.47 yr).
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This research was supported by Tabriz University of Medical Sciences (Tabriz, Iran). This is a report of thesis (MPH degree) registered at Medical Faculty of Tabriz University of Medical Sciences.
Footnotes
Conflicts of interest
The authors declare that there is no conflict of interest.
References
- 1.Akbari ME, Sayad S, Sayad S, et al. (2017). Breast Cancer Status in Iran: Statistical Analysis of 3010 Cases between 1998 and 2014. Int J Breast Cancer, 2017:2481021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wahba HA, El-Hadaad HA. (2015). Current approaches in treatment of triple-negative breast cancer. Cancer Biol Med, 12(2):106–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Qadire M, Alkhalaileh M, Hedaya H. (2018). Risk Factors for Breast Cancer among Jordanian Women: A Case-control Study. Iran J Public Health, 47(1):49–56. [PMC free article] [PubMed] [Google Scholar]
- 4.Vostakolaei FA, Broeders MJ, Rostami N, et al. (2012). Age at diagnosis and breast cancer survival in Iran. Int J Breast Cancer, 2012:517976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mousavi SM, Montazeri A, Mohagheghi MA, et al. (2007). Breast cancer in Iran: an epidemiological review. Breast J, 13(4):383–91. [DOI] [PubMed] [Google Scholar]
- 6.Abedi G, Janbabai G, Moosazadeh M, et al. (2016). Survival rate of breast cancer in Iran: a meta-analysis. Asian Pac J Cancer Prev, 17(10):4615–4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeSantis C, Ma J, Bryan L, Jemal A. (2014). Breast cancer statistics, 2013. CA Cancer J Clin, 64(1):52–62. [DOI] [PubMed] [Google Scholar]
- 8.Smink DS. (2015). Schwartz’s Principles of Surgery. Ann Surg, 261(5):1026. [Google Scholar]
- 9.Friedewald SM, Rafferty EA, Rose SL, et al. (2014). Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA, 311(24):2499–507. [DOI] [PubMed] [Google Scholar]
- 10.Oeffinger KC, Fontham ET, Etzioni R, et al. (2015). Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA, 314(15):1599–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harirchi I, Ebrahimi M, Zamani N, et al. (2000). Breast cancer in Iran: a review of 903 case records. Public health, 114(2):143–5. [DOI] [PubMed] [Google Scholar]
- 12.Najjar H, Easson A. (2010). Age at diagnosis of breast cancer in Arab nations. Int J Surg, 8(6):448–52. [DOI] [PubMed] [Google Scholar]
- 13.Sant M, Gatta G, Micheli A, et al. (1991). Survival and age at diagnosis of breast cancer in a population-based cancer registry. Eur J Cancer, 27(8):981–4. [DOI] [PubMed] [Google Scholar]
- 14.Parvizpour S, Razmara J, Omidi Y. (2018). Breast cancer vaccination comes to age: impacts of bioinformatics. BioImpacts, 8(3):223–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harford JB. (2011). Breast-cancer early detection in low-income and middle-income countries: do what you can versus one size fits all. Lancet Oncol, 12(3):306–12. [DOI] [PubMed] [Google Scholar]
- 16.Ziaei JE, Dastgiri S, Vaez J, et al. (2011). Age Pattern of the Occurrence of Breast Cancer in the Northwest of Iran. Indian J Cancer, 48(4):406–9. [DOI] [PubMed] [Google Scholar]
- 17.Fouladi N, Amani F, Harghi AS, et al. (2011). Five year survival of women with breast cancer in Ardabil, north-west of Iran. Asian Pac J Cancer Prev, 12(7):1799–801. [PubMed] [Google Scholar]
- 18.Vostakolaei FA, Broeders MJ, Mousavi SM, et al. (2013). The effect of demographic and lifestyle changes on the burden of breast cancer in Iranian women: A projection to 2030. Breast, 22(3):277–81. [DOI] [PubMed] [Google Scholar]
- 19.Zahmatkesh B, Keramat A, Alavi N, et al. (2016). Breast Cancer Trend in Iran from 2000 to 2009 and Prediction till 2020 using a Trend Analysis Method. Asian Pac J Cancer Prev, 17(3):1493–8. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med, 6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shamseer L, Moher D, Clarke M, et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ, 350:g7647. [DOI] [PubMed] [Google Scholar]
- 22.Whiting PF, Sterne JA. (2012). The Revised QUADAS-2 Tool. Ann Intern Med, 156(4):323–4. [DOI] [PubMed] [Google Scholar]
- 23.Hozo SP, Djulbegovic B, Hozo I. (2005). Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol, 5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sterne J, Egger M, Smith G. (2001). Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ, 323 (7304): 101–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sterne JA, Egger M. (2001). Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol, 54(10):1046–55. [DOI] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414):557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moradzadeh R, Mansournia MA, Baghfalaki T, et al. (2015). Misclassification adjustment of family history of breast cancer in a case-control study: a Bayesian approach. Asian Pac J Cancer Prev, 16(18):8221–6. [DOI] [PubMed] [Google Scholar]
- 28.Ghiasvand R, Maram ES, Tahmasebi S, et al. (2011). Risk factors for breast cancer among young women in southern Iran. Int J Cancer, 129(6):1443–9. [DOI] [PubMed] [Google Scholar]
- 29.Mohammadianpanah M, Ashouri Y, Hoseini S, et al. (2012). The efficacy and safety of neoadjuvant chemotherapy+/− letrozole in postmenopausal women with locally advanced breast cancer: a randomized phase III clinical trial. Breast Cancer Res Treat, 132(3):853–61. [DOI] [PubMed] [Google Scholar]
- 30.Sedghi M, Esfandiari E, Fazel-Najafabadi E, et al. (2016). Genomic rearrangement screening of the BRCA1 from seventy Iranian high-risk breast cancer families. J Res Med Sci, 21:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Payandeh M, Sadeghi M, Sadeghi E, et al. (2017). Is there any concordance between of IHC with FISH in HER2-positive breast cancer patients? Int J Hematol Oncol Stem Cell Res, 11(1):43–48. [PMC free article] [PubMed] [Google Scholar]
- 32.Parkin DM. (2008). The role of cancer registries in cancer control. Int J Clin Oncol, 13(2):102–11. [DOI] [PubMed] [Google Scholar]
- 33.Etemadi A, Sadjadi A, Semnani S, et al. (2008). Cancer registry in Iran: a brief overview. Arch Iran Med, 11(5):577–80. [PubMed] [Google Scholar]
- 34.Gucalp A, Traina TA, Eisner JR, et al. (2019). Male breast cancer: a disease distinct from female breast cancer. Breast Cancer Res Treat, 173(1):37–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shahraki HR, Salehi A, Zare N. (2015). Survival prognostic factors of male breast cancer in Southern Iran: a LASSO-Cox regression approach. Asian Pac J Cancer Prev, 16(15):6773–7. [DOI] [PubMed] [Google Scholar]
- 36.Salehi A, Zeraati H, Mohammad K, et al. (2011). Survival of male breast cancer in Fars, South of Iran. Iran Red Crescent Med J, 13(2):99–105. [PMC free article] [PubMed] [Google Scholar]
- 37.Jazayeri SB, Saadat S, Ramezani R, et al. (2015). Incidence of primary breast cancer in Iran: Ten-year national cancer registry data report. Cancer Epidemiol, 39(4):519–27. [DOI] [PubMed] [Google Scholar]
- 38.Yetkin G, Celayir MF, Tanik C, et al. (2019). Male breast cancer: A 10 year retrospective case series in a tertiary care hospital. J Pak Med Assoc, 69(8):1209–1212. [PubMed] [Google Scholar]
- 39.Özmen V, Özmen T, Doğru V. (2019). Breast Cancer in Turkey; An Analysis of 20.000 Patients with Breast Cancer. Eur J Breast Health, 15(3):141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schlichting JA, Soliman AS, Schairer C, et al. (2015). Breast cancer by age at diagnosis in the Gharbiah, Egypt, population-based registry compared to the United States surveillance, epidemiology, and end results program, 2004–2008. BioMed Res Int, 2015:381574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Karim SAM, Ghalib HHA, Mohammed SA, et al. (2015). The incidence, age at diagnosis of breast cancer in the Iraqi Kurdish population and comparison to some other countries of Middle-East and West. Int J Surg, 13:71–75. [DOI] [PubMed] [Google Scholar]
- 42.Lee J, Oh M. (2014). Effects of interval between age at first pregnancy and age at diagnosis on breast cancer survival according to menopausal status: a register-based study in Korea. BMC Women’s Health, 14(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mehdi I, Monem EA, Al Bahrani BJ, et al. (2014). Age at diagnosis of female breast cancer in Oman: Issues and implications. South Asian J Cancer, 3(2):101–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Missaoui N, Landolsi H, Jaidaine L, et al. (2012). Breast cancer in Central Tunisia: An Earlier Age at Diagnosis and Incidence Increase over a 15 Year Period. Breast J, 18(3):289–91. [DOI] [PubMed] [Google Scholar]
- 45.Franco-Marina F, López-Carrillo L, Keating NL, et al. (2015). Breast cancer age at diagnosis patterns in four Latin American Populations: A comparison with North American countries. Cancer Epidemiol, 39(6):831–7. [DOI] [PubMed] [Google Scholar]
- 46.Salinas-Martinez AM, Juarez-Ruiz A, Mathiew-Quiros A, et al. (2014). [Breast cancer in Mexico: a 10-year trend analysis on incidence and age at diagnosis]. Rev Invest Clin, 66(3):210–7. [PubMed] [Google Scholar]
- 47.Afsharfard A, Mozaffar M, Orang E, Tahmasbpour E. (2013). Trends in epidemiology, clinical and histopathological characteristics of breast cancer in Iran: results of a 17 year study. Asian Pac J Cancer Prev, 14(11):6905–11. [DOI] [PubMed] [Google Scholar]
- 48.Haghighat S, Akbari M, Ghaffari S, et al. (2012). Standardized breast cancer mortality rate compared to the general female population of Iran. Asian Pac J Cancer Prev, 13(11):5525–8. [DOI] [PubMed] [Google Scholar]
- 49.Baghestani AR, Shahmirzalou P, Zayeri F, et al. (2015). Prognostic factors for survival in patients with breast cancer referred to omitted cancer research center in Iran. Asian Pac J Cancer Prev, 16(12):5081–4. [DOI] [PubMed] [Google Scholar]
- 50.Kadivar M, Mafi N, Joulaee A, et al. (2012). Breast cancer molecular subtypes and associations with clinicopathological characteristics in Iranian women, 2002–2011. Asian Pac J Cancer Prev, 13(5):1881–6. [DOI] [PubMed] [Google Scholar]
- 51.Harirchi I, Kolahdoozan S, Karbakhsh M, et al. (2010). Twenty years of breast cancer in Iran: downstaging without a formal screening program. Ann Oncol, 22(1):93–97. [DOI] [PubMed] [Google Scholar]
- 52.Abdollahi M, Hajizadeh E, Baghestani AR, et al. (2016). Determination of a change point in the age at diagnosis of breast cancer using a survival model. Asian Pac J Cancer Prev, 17(S3):5–10. [DOI] [PubMed] [Google Scholar]
- 53.Mousavi SM, Mohagheghi MA, Mousavi-Jerrahi A, et al. (2008). Outcome of breast cancer in Iran: a study of Tehran Cancer Registry data. Asian Pac J Cancer Prev, 9(2):275–8. [PubMed] [Google Scholar]
- 54.Najafi B, Anvari S, Roshan ZA. (2013). Disease free survival among molecular subtypes of early stage breast cancer between 2001 and 2010 in Iran. Asian Pac J Cancer Prev, 14(10):5811–6. [DOI] [PubMed] [Google Scholar]
- 55.Taheri NS, Nosrat SB, Aarabi M, et al. (2012). Epidemiological pattern of breast cancer in Iranian women: is there an ethnic disparity? Asian Pac J Cancer Prev, 13(9):4517–20. [DOI] [PubMed] [Google Scholar]
- 56.Fallahzadeh H, Momayyezi M, Akhundzardeini R, et al. (2014). Five year survival of women with breast cancer in Yazd. Asian Pac J Cancer Prev, 15(16):6597–601. [DOI] [PubMed] [Google Scholar]
- 57.Heydari ST, Mehrabani D, Tabei S, et al. (2009). Survival of breast cancer in southern Iran. Iranian Journal of Cancer Prevention, 2(1):51–54. [Google Scholar]
- 58.Ghavami V, Mahmoudi M, Foroushani AR, et al. (2017). Long-Term Disease-Free Survival of Non-Metastatic Breast Cancer Patients in Iran: A Survival Model with Competing Risks Taking Cure Fraction and Frailty into Account. Asian Pac J Cancer Prev, 18(10):2825–2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lakzaei M, Salarilak S, Khalkhali HR, et al. (2015). Association between age of morbidity and prognosis of breast breast cancer. Stud Med Sci, 26(7):625–33. [Google Scholar]
- 60.Sinaga ES, Ahmad RA, Shivalli S, et al. (2018). Age at diagnosis predicted survival outcome of female patients with breast cancer at a tertiary hospital in Yogyakarta, Indonesia. Pan Afr Med J, 31:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bab S, Abdifard E, Elyasianfar S, et al. (2019). Time trend analysis of breast cancer in Iran and its six topographical regions: a population-based study. J Med Life, 12(2):140–149. [DOI] [PMC free article] [PubMed] [Google Scholar]