Abstract
Background:
COVID-19 was first declared as an international public health emergency and then a pandemic by the WHO. In this systematic review, the importance of isolation and contact tracing has been explained, and what kinds of practices exist in different countries are mentioned.
Methods:
A systematic review was conducted in accordance with the PRISMA and Cochrane guidelines by searching articles from major medical databases such as Google Scholar, PubMed/MEDLINE, Cochrane Library, EMBASE, CINAHL between Jan 1, 2020 and Apr 1, 2021. Observational and modeling studies written on contact tracing, screening, quarantine and isolation were included.
Results:
27 observational and modeling studies were included. It was seen that rapid contact tracing to reduce the basic reproduction number (R0) from 3.11 to 0.21. Additionally, each new case requires an average of 36 people to be monitored. Since screening programs missed 75% of cases, high-level contact tracing should also be done simultaneously. Wide quarantine would prevent 79.27% deaths and 87.08% infections.
Conclusion:
Effective, rapid contact tracing is the cornerstone of an effective public health response in outbreaks. Its success depends on quickly identifying cases, gathering information from them about their last contacts, and tracing and isolating those contacts.
Keywords: COVID-19, Isolation, Quarantine, Contact tracing
Introduction
Coronavirus Disease-2019 (COVID-19) was first declared as an international public health emergency and then a pandemic by the World Health Organization (WHO) (1). The disease is mainly transmitted from the infected person through the inhalation of respiratory droplets. If a person touches their eyes, nose or mouth after touching a surface contaminated with virus-containing droplets, they can become infected through viruses that can live for up to several days. Some people become infected without developing symptoms and can transmit the infection, although the risk is lower. The infected person spreads the virus from 48 h before to 2 wk after the onset of symptoms (2).
Vaccines that can prevent COVID-19 have just been introduced and their protection will be seen over time. The best prevention is to avoid exposure to the virus. Control measures that can reduce the risk; use of masks, using a napkin while coughing/sneezing, washing hands with soap or disinfecting hands with a disinfectant containing at least 60% alcohol, avoiding contact with infected people and maintaining the proper distance as much as possible and not touching eyes, nose and mouth with unwashed hands (3). In addition, finding the contacts of the cases early and isolating them, just like the cases, is the most important way to protect the society from this disease.
In this review, the importance of isolation and contact tracing has been explained, and what kinds of practices exist in different countries are mentioned.
Methods
Firstly, a study protocol was developed and followed in the process. In accordance with the rules of Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) Guidelines (4) and Cochrane Handbook for Systematic Reviews of Interventions (5); articles published between Jan 1, 2020 and Apr 1, 2021, containing information about different prevention strategies such as contact tracing, screening, quarantine and isolation, and studies evaluating their effectiveness were scanned.
Literature search strategy
Electronic bibliographic databases and libraries such as Google Scholar, PubMed/MEDLINE, Cochrane Library, Experta Medica Database (EMBASE), Cumulative Index to Nursing and Allied Health Literature (CINAHL) and MedRxiv were used. Additionally, the gray literatures, preprints, and resource centers of The Lancet, The Journal of the American Medical Association (JAMA) and The New England Journal of Medicine were investigated. Finally, reference lists of systematic reviews were scanned for additional resources. The MESH terms used for this search were: “Coronavirus”, “Coronavirus disease”, “SARS CoV-2”, “COVID-19”, “Novel corona”, “Prevention”, “Control”, “Contact tracing”, “Screening”, “Quarantine”, “Isolation”. Combinations of these terms with “AND”, “OR” were searched together. Studies were scanned by titles and abstracts, and then full texts and bibliographies were reviewed.
Eligibility (inclusion and exclusion) criteria
If the titles and abstracts of the articles found with the literature review meet one or more of the eligibility criteria, the full text of the articles was examined. References published in peer-reviewed journals, gray literature, and websites are eligible for inclusion, especially if they have researched one or more of the contact tracing topics. Standard forms have been prepared and used to summarize the articles by narrative. Randomized controlled trials were not included due to COVID-19 being a new epidemic, lack of research, and ethical concerns. Therefore, nonrandomized observational studies and modeling (mathematical/epidemiological) studies were considered to support the available evidence.
Data synthesis and analysis
Qualitative data were systematically reviewed and presented in accordance with Cochrane Guidelines. The results obtained from quantitative measures were synthesized narratively. Quantitative analysis (meta-analysis) could not be done due to the heterogeneity of the studies.
Results
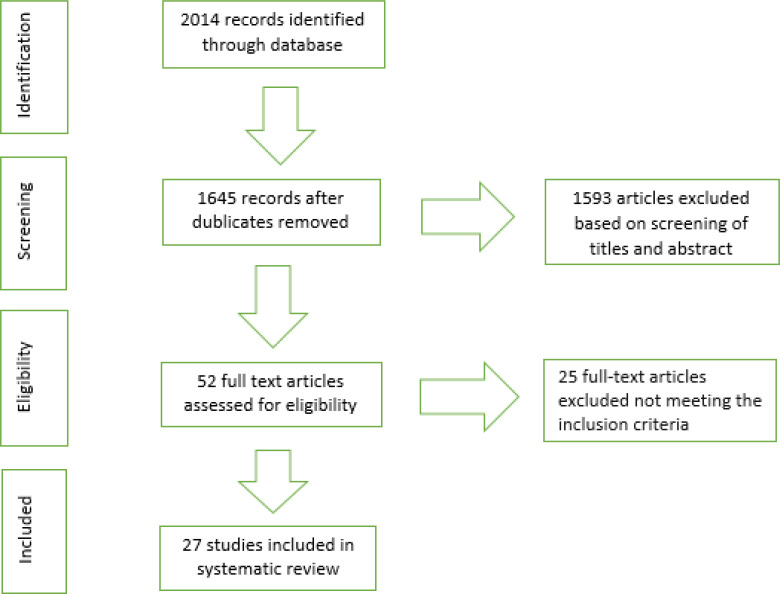
The PRISMA flowchart and conformity assessment for selected studies in the search process are summarized in Fig. 1. Overall, 2014 article was reached as a result of the first electronic database search. 1645 records identified after dublicates removed. Overall, 1593 articles excluded based on screening of titles and abstract. 52 full text articles were assessed for eligibility. Twenty-five full-text articles were excluded not meeting the inclusion criteria. Thus, 27 studies met the inclusion criteria and were included in the systematic review.
Fig. 1:
Flow chart for study search, selection, and screening for the systematic review
What is Isolation and Contact Tracing?
Contact tracing is the process that involves identifying someone who has been in contact with someone positive for an infectious disease. These identified people should be recorded, monitored closely, and taken into isolation even if they do not show symptoms. WHO recommends regular follow-up to “monitor symptoms and test for signs of infection” (6).
People who have close contact with the infected person are identified during the case investigation. Teams talk to patients or relatives to determine when symptoms started and who they had been in contact with, from 2 d before to 14 d after symptoms began. If the patient has used public transport, has been in busy public places, it may be difficult to individually identify people who have been in close contact with the case. It is important to remember that proximity is important in the definition of contact (1.5–2 m) and not all people can be in close contact (7). People are asked not to leave home for 14 days after contact with a COVID-19 patient. If the person in contact with the case did not come into contact with the people in the household, he/she should separate himself/herself and minimize the risk of contamination (eg avoiding bed-food sharing) (7).
Some countries have identified places (facility/dormitory) where people with contact are placed to wait for 14-day quarantine periods. This can be used to save resources when there are a limited number of cases. However, these facilities may be sites of disease amplification causing the outbreak to grow. In addition, if the facilities are viewed as patient concentration camps, people can avoid telling their risky contacts to avoid going to the quarantine facility (7).
People who have been in contact with the case but do not have symptoms of COVID-19 do not need to be tested. This is because a negative test seen that day does not mean the person is not infected. Current laboratory tests are positive only when the viral load reaches a certain level (7).
Technological applications can help in contact tracing, but the need for large workforce is inevitable. For example, 1000 contact tracing workers were recruited at the beginning of the epidemic in Massachusetts, the USA (8). Health Canada has called for a volunteer workforce for contact tracing (9). South Korea employed a massive public health worker at the height of the epidemic (10). In Turkey, according to the Health Minister’s statement dated October 9, 2020; 11800 filiation teams, each consisting of 3 people, were on duty to monitor contact (11).
Since contact tracing is resource intensive, alternative methods can be used:
Using non-health personnel and volunteers; this approach is based on the idea of trained non-public health personnel (staff working in other areas of the public, students, retired health personnel, non-governmental organization employees) to carry out contact monitoring activities. Some countries have used military students. These staff should be trained in areas such as basic epidemiology, public health requirements, health communication, ethics, and data protection (12).
Repositioning existing resources; an example of this is the use of call centers/national helplines set up for other purposes (12).
Reducing the follow-up intensity of people who have been in contact; with a large number of cases, it may not be possible to maintain active follow-up of all contacts. Instead of calling people, initial information can be given by text message. While some countries stopped active daily contact tracing as the numbers increased, others focused on alternatives such as sending a text message asking people if they developed symptoms (12).
Using technology; mobile apps offer many possibilities to support people tracing, but manual contact tracing remains the main method of people tracing. The use of mobile applications can never be the only method because the entire population will not download the mobile communication tracing application and usage will be low in some important populations (eg the elderly). Some countries use Go.Data, proprietary communication management software developed by WHO. This software allows the recording of cases and contacts, thus making it easy to keep trace of contacts. Go.Data facilitates the analysis of person tracing data, visualizes the transmission chains by category, and can export person tracing data for sharing in different software or for detailed analysis (12).
Country Samples
Contact tracing practices
Current evidence on the COVID-19 pandemic shows the importance of contact tracing as an effective tool in terms of both limiting the virus and spreading the transmission.
Singapore and China; was able to limit the size of initial outbreaks through widespread testing, contact tracing, and quarantine. Contact tracing led to the identification of many new cases before symptom onset and shortened the time from symptom onset to isolation. Thus, it reduced the possibility of continuous transmission (13–15). Contact tracing reduced the spread of the disease in China and South Korea (13,16). From a healthcare perspective, experience in China has shown that contact tracing can provide effective hospital control when accompanied by testing and quarantine (17). Evidence from Singapore highlighted the role of symptomatic pre-transmission in epidemic dynamics, showing that people with close contact should be immediately put in isolation to prevent transmission in pandemic control (18). In Vietnam, where intense efforts have been made to isolate cases, monitor and isolate their contacts, the use of artificial intelligence was considered to further improve contact tracing and patient management (19). New Zealand was able to control the outbreak using aggressive traditional contact monitoring supplemented by other methods (20).
One of the studies evaluating the effect of isolation in different populations and isolation strategies found that isolation should be integrated with travel restriction (21). Another study evaluating the effects of metropolitan-wide quarantine in China found that quarantine would prevent 79.27% (75.10%–83.45%) deaths and 87.08% (84.68%–89.49%) infections (22). Unless the level of contact tracing and screening is high, prevention through isolation only is very limited, as the screening programs misses 75% of cases (23). Keeling et al. evaluated the effectiveness of contact tracing to control COVID-19 in the UK. Rapid contact tracing to reduce the basic reproduction number (R0) from 3.11 to 0.21 allowed the outbreak to be contained. Additionally, each new case requires an average of 36 people to be monitored (24).
As part of the monitoring process, case investigation and contact tracing metrics for Jun 25–July 24, 2020, were submitted to CDC by 62 health departments of the USA. Descriptive analyses of case investigation and contact tracing load, timeliness, and yield (i.e., the number of contacts elicited divided by the number of patients prioritized for interview) were performed. A median case load per investigator during the evaluation period was 31 (1–196). 57% of patients were interviewed within 24 h of report of the case to a health department (interquartile range [IQR] = 27%–82%); a median of 1.15 contacts were identified per patient prioritized for interview (IQR = 0.62–1.76), and a median of 55% of contacts were notified within 24 h of identification by a patient (IQR=32%–79%). With higher caseloads, the percentage of patients interviewed within 24 h of case report was lower (Spearman coefficient =−0.68), and the number of contacts identified per patient prioritized for interview also decreased (Spearman coefficient = −0.60). The capacity to conduct timely contact tracing varied among health departments, largely driven by investigators’ caseloads (25).
Contact tracing applications
Person tracing in China was primarily provided by Alipay and WeChat mobile apps. These applications use user-reported data, travel history, health status, and government registers to assign colors green, yellow, and red. Color indicates whether the user is healthy (green), suspected (yellow), or confirmed COVID-19 patient (red) (26). The system is challenging as the color codes decide the user’s freedom of movement, and there are severe penalties for violators (27). Iran’s tracing application requires the user to register using their mobile phone number. The user uses unencrypted GPS data to determine its absolute location for person tracing. Moreover, the application is asking for permission to define a user’s activity. Security experts have discovered that the user also sends self-declared attributes, such as the user’s gender, name, height, and weight, to the developer’s server (28).
In Singapore, Trace Together official contact tracing app uses Bluetooth to identify people near the user. Location permission is used only to find the distance between users. Requires registration of the user’s phone number for fast communication. Each device periodically generates a random unique identifier to communicate with nearby devices. If someone is infected with COVID-19, their recorded data is uploaded and forwarded to other users to match. TraceTogether is relatively user privacy friendly because no identifiable information is shared between devices and the government only knows phone numbers (29). In Israel, “Hamagen” communication tracing application collects the user’s location history in the background. It compares the user’s movement with the health department’s data on the locations of confirmed COVID-19 cases. If a user has been in close contact with an infected person, a warning message is sent to the user and directed to a website containing the necessary precautions (30). In India, the ‘Aarogya Setu’ people tracing app requires additional information such as name, age, gender, occupation and countries visited in the last 30 d as well as phone number for registration. A unique identification number generated using a phone number is used to trace all people near a COVID-19 patient in the last 14 days (31).
“Covid Watch” and “CoEpi” applications in the USA use bluetooth for proximity-based person monitoring. Both applications measure the signal strength to estimate contact distance with other users. When a user is found to be infected, the unique “communication activity number” list on their personal device is made public. Other devices use this public list to find out if they have been in close contact with an infected person (32).
The Ministry of Health in Turkey as part of COVID-19 fight, citizens can see to the risk situation in the region and will be able to follow their own health “Hayat Eve Sığar” spent the mobile application to life. “Hayat Eve Sığar” means “Life is at Home”. Citizens who download the application for free can report a change in their health with a health test they can fill out every day. On the map in the application, besides the intensity of risk, the places to be known in emergency situations such as hospitals, pharmacies, markets, stops are also shown. Citizens can add their families and relatives to their lists in line with their approval. With the smart algorithms developed, it can be seen whether risky people are contacted or not (33). Citizens receive codes for plane and bus travel via the application or via text message. This code is shared with the travel company when buying tickets, so that the passengers are questioned whether they are at risk and the travel of risky people is not approved. Although the app was primarily used in travels, it became widespread in many areas such as workplace, clinic and institution visits in a short time (34).
Conclusion
The COVID-19 pandemic is the biggest health threat the world has seen in the last 100 years. The risk is high if there is at least 10–15 min within 1.5–2 m of the infected person. Individuals may be asked to self-isolate from newly infected presymptomatic people, and transmission to more people may be stopped. Mathematical models of the pandemic show that rapid contact tracing combined with a large-scale virus testing program can not only delay the outbreak but stop it completely. This will also mean that the isolation measures that are being applied can be gradually loosened. Effective, rapid contact tracing is the cornerstone of an effective public health response in outbreaks. Its success depends on quickly identifying cases, gathering information from them about their last contacts, and tracing and isolating those contacts. The common rationale for existing quarantines and other movement restrictions is to provide ‘physical distance’ to disrupt transmission of infection so that health systems can cope with estimated demand.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the author.
Acknowledgements
Not applicable.
Footnotes
Conflict of interest
The author has no conflicts of interest to declare.
Funding
The author declared that this study has received no financial support
References
- 1.World Health Organization (2020). Statement on the second meeting of the International Health Regulations Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available from: https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 2.European Centre for Disease Prevention and Control (2020). Rapid risk assessment: Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK-eighth update 2020. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-eighth-update-8-april-2020.pdf
- 3.Adhikari SP, Meng S, Wu YJ, et al. (2020). Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty, 9:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shamseer L, Moher D, Clarke M, et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ, 350: g7647 doi: 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 5.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. (2019). Cochrane handbook for systematic reviews of interventions. 2nd ed. The Cochrane Collaboration and John Wiley & Sons Ltd, the United Kingdom. [Google Scholar]
- 6.COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention (2020). Contact transmission of COVID-19 in South Korea: Novel investigation techniques for tracing contacts. Osong Public Health Res Perspect, 11(1): 60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Africa Centres for Disease Control and Prevention (2020). Guidance on contact tracing for COVID-19 pandemic. Available from: https://africacdc.org/download/guidance-on-contact-tracing-for-covid-19-pandemic/
- 8.Fox M. (2020). ‘We need an army’: Hiring of coronavirus trackers seen as key to curbing disease spread. Available from: https://www.statnews.com/2020/04/13/coronavirus-health-agencies-need-army-of-contact-tracers/
- 9.Government of Canada (2020). COVID-19: How you can help. Available from: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/make-a-difference.html
- 10.COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention (2020). Coronavirus Disease-19: summary of 2,370 contact investigations of the first 30 cases in the Republic of Korea. Osong Public Health Res Perspect, 11(2): 81–84. doi: 10.24171/j.phrp.2020.11.2.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Habertakvimi (2020). Minister Koca: Except for Istanbul, there is no province whose number of cases has not decreased. Available from: https://habertakvimi.com/haber/5589551/bakan-koca-istanbul-haricinde-vaka-sayisi-azalmayan-il-yok
- 12.European Centre for Disease Prevention and Control (2020). Contact tracing for COVID-19: current evidence, options for scale-up and an assessment of resources needed. Available from: https://www.ecdc.europa.eu/en/publications-data/contact-tracing-covid-19-evidence-scale-up-assessment-resources
- 13.World Health Organization (2020). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- 14.Pung R, Chiew CJ, Young BE, et al. (2020). Investigation of three clusters of COVID-19 in Singapore: Implications for surveillance and response measures. Lancet, 395(10229): 1039–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen W, Wang Q, Li Y, et al. (2020). [Early containment strategies and core measures for prevention and control of novel coronavirus pneumonia in China]. Zhonghua Yu Fang Yi Xue Za Zhi, 54(3):239–44. [Article in Chinese] [DOI] [PubMed] [Google Scholar]
- 16.Moradi H, Vaezi A. (2020). Lessons learned from Korea: Covid-19 Pandemic. Infect Control Hosp Epidemiol, 41(7):873–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fang Y, Zhang S, Yu Z, Wang H, Deng Q. (2020). Shenzhen’ experience on containing 2019 novel coronavirus-infected pneumonia transmission. QJM, 113(6): 389–390. doi: 10.1093/qjmed/hcaa112.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. (2020). Presymptomatic transmission of SARS-CoV-2 - Singapore, January 23-March 16, 2020. CDC, Morbidity and Mortality Weekly Report, 69(14); 411–415. Available from: https://www.cdc.gov/mmwr/volumes/69/wr/mm6914e1.htm#suggestedcitation [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen THD, Vu DC. (2020). Summary of the COVID-19 outbreak in Vietnam - lessons and suggestions. Travel Med Infect Dis, 37:101651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker M, Kvalsvig A, Verrall A, Telfar-Barnard L, Wilson N. (2020). New Zealand’s elimination strategy for the COVID-19 pandemic and what is required to make it work. N Z Med J, 133(1512):10–14. [PubMed] [Google Scholar]
- 21.Hu Z, Cui Q, Han J, Wang X, Sha WEI, Teng Z. (2020). Evaluation and prediction of the COVID-19 variations at different input population and quarantine strategies, a case study in Guangdong province, China. Int J Infect Dis, 95:231–40. Available from: 10.1016/j.ijid.2020.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen M, Peng Z, Guo Y, et al. (2020). Assessing the effects of metropolitan-wide quarantine on the spread of COVID-19 in public space and households. International Journal of Infectious Diseases, 96:503–505. Available from: 10.1016/j.ijid.2020.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kucharski AJ, Klepac P, Conlan AJK, et al. (2020). Effectiveness of isolation, testing, contact tracing and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis, 20: 1151–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keeling MJ, Hollingsworth TD, Read JM. (2020). The efficacy of contact tracing for the containment of the 2019 novel coronavirus (COVID-19). J Epidemiol Community Health, 74(10): 861–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spencer KD, Chung CL, Stargel A, et al. (2021). COVID-19 case investigation and contact tracing efforts from health departments - United States. Morbidity and Mortality Weekly Report, 70(3): 83–87. Available from: https://www.cdc.gov/mmwr/volumes/70/wr/mm7003a3.htm?s_cid=mm7003a3_w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davidson H. (2020). China’s coronavirus health code apps raise concerns over privacy. Available from: https://www.theguardian.com/world/2020/apr/01/chinas-coronavirus-health-code-apps-raise-concerns-over-privacy
- 27.Knight W. (2020). Phones could track the spread of COVID-19. Is it a good ıdea? Available from: https://www.wired.com/story/phones-track-spread-covid19-good-idea/
- 28.Chrysaidos N. (2020). Iranian coronavirus app collecting sensitive information. Available from: https://blog.avast.com/iranian-coronavirus-app-collecting-sensitive-information-avast,
- 29.A Singapore Government Agency Website (2020). TraceTogether - behind the scenes look at its development process. Available from: https://www.tech.gov.sg/media/technews/tracetogether-behind-the-scenes-look-at-its-development-process
- 30.Winer S. (2021). Health Ministry launches phone app to help prevent spread of coronavirus. Available from: https://www.timesofisrael.com/health-ministry-launches-phone-app-to-help-prevent-spread-of-coronavirus/
- 31.Agrawal A. Madianama.com (2020). Indian Government releases COVID-19 contact tracing app. Available from: https://www.medianama.com/2020/04/223-aarogya-setu-coronavirus-contact-tracing-app-launched/
- 32.Berke A, Bakker M, Vepakomma P, Raskar R, Larson K, Pentland A. (2020). Assessing disease exposure risk with location histories and protecting privacy: a cryptographic approach in response to a global pandemic. arXiv preprint arXiv:2003.14412.
- 33.Anadolu Agency (2020). In the fight against COVID-19, the mobile application “Hayat Eve Sığar” was launched. Available from: https://www.aa.com.tr/tr/koronavirus/kovid-19-ile-mucadelede-hayat-eve-sigar-mobil-uygulamasi-hayata-gecirildi/1809714
- 34.Anadolu Agency (2020). Details of the HES code period in travels. Available from: https://www.aa.com.tr/tr/saglik/seyahatlerde-hes-kodu-doneminin-ayrintilari/1848773