Abstract
Background
Multidisciplinary conference presentation may provide recommendations for diagnosis, monitoring and treatment for patients with inflammatory bowel disease.
Methods
A prospective observational study was completed evaluating if case presentation resulted in a direct change in management for patients presented over a 2-year period in a tertiary Canadian centre. Change in management was defined as hospital admission, surgery or surgical referral, start/change in biologic therapy or other medication or initiation of parenteral nutrition. Secondary outcomes included the involvement of specialists and other referrals. Data were analyzed using frequencies and means with standard deviations.
Results
In 63 multidisciplinary conferences, 181 patients were presented, of whom 136 patients met the inclusion criteria of inflammatory bowel disease (Crohn’s n = 45, ulcerative colitis n = 88, undifferentiated n = 3). The majority were outpatient cases 110 (81%). Indications included 71 (52%) patients presented for IBD management with diagnosis > 1 year, 37 (27%) with an acute IBD flare in a chronic patient (>1 year since diagnosis) and 24 (18%) with new diagnosis of IBD. Change in management was recommended in 35 (26%) patients. The most common change was referral to surgery in 17 (13%), surgery in 12 (9%) or change in biologic therapy 11 (8%). Compliance with the recommendations was 85%. There was frequent specialist involvement in case discussions (gastroenterologist 100%, surgeon 60%, radiologist 68% and pathologist 32%).
Conclusions
Presentation of complex inflammatory bowel disease cases at multidisciplinary conference leads to a direct change in treatment in one quarter of cases, with surgical referral as the most frequent outcome.
Keywords: Crohn’s disease, Inflammatory bowel disease, Management, Treatment, Ulcerative colitis
Background
Inflammatory bowel disease (IBD), comprised of ulcerative colitis (UC) and Crohn’s disease (CD), is a complex disorder affecting 0.5% of North Americans with variations in clinical practice and access to specialist care (1). Patients with IBD typically experience a relapsing and remitting disease course, necessitating life-long medical treatment and recurrent monitoring to prevent disease related complications. Despite the availability of several advanced medical therapies, 10-year risk of colectomy in patients with UC is 13% and 10-year risk of bowel resection in patients with CD is 40% (2).
Increased availability of therapeutic agents has resulted in challenges in terms of drug selection and sequencing, in addition to monitoring and management of the disease and integrating surgery at the right time. These complexities have highlighted the necessity of multidisciplinary management. Composition of the multidisciplinary team for IBD has been described by expert consensus panels and includes IBD-focused gastroenterologists, colorectal surgeons, radiologists, gastrointestinal pathologists and allied health care such as IBD nurse specialists, dietitians and psychologists (3).
The benefits of regular multidisciplinary team meetings (MDTMs) are widely acknowledged in oncology and other chronic diseases. They are pivotal as a mechanism for communication and coordination of care, bringing complementary diagnostic and therapeutic skills together in one venue (4,5). They also bring reassurances to patients of wider consultation when complex decision making is needed. Literature from MDTM in cancer patients has also demonstrated cost-effectiveness, improved outcomes, increased compliance with guidelines and potentially survival benefits (4–8).
With advocacy for multidisciplinary management, MDTMs have been introduced in many IBD centres. The UK National IBD audit reported 75% of participating institutions had a weekly MDTM for IBD patients (9). Although there have been retrospective audits and expert consensus opinions published, there is a paucity of prospective data on the impact of an IBD MDTM at an academic centre and the effect it may have on treatment plans (9–11).
The goals of this study were to (1) examine a prospective cohort of IBD patients presented at MDTMs over 2 years and assess changes to the initial treatment plan; (2) to determine if an IBD MDTM consensus leads to compliance with recommendations and (3) to describe the implementation, composition and other benefits or barriers to IBD MDTMs.
METHODS
This was a prospective observational study conducted over 2 years (July 1, 2017 to June 30, 2019), 3 months after inception of dedicated IBD MDTMs at our centre. The MDTMs were held at a single academic centre which encompassed three academic hospitals (London Health Sciences Centre [LHSC] hospitals and St. Joseph’s Health Care Centre), where approximately 5000 IBD patients receive diagnostic and therapeutic care in London, Ontario, Canada. The Strengthening the Reporting of Observation studies in Epidemiology (STROBE) guidelines were followed (12). Ethics approval was obtained through the Health Sciences Research Ethics Board at Western University (HSREB# 116004).
Complex cases IBD were identified by the treating physician, who submitted patient identifiers, as well as a current and proposed management plan to the MDTM coordinator. The coordinator compiled and distributed the patient list for each meeting. For this study, eligible participants were adult patients aged 18 years or older, presented at IBD MDTMs with a diagnosis of UC, CD or undifferentiated colitis. The decision to present a patient was left to the treating physician. Once patients were included after initial presentation at IBD MDTMs, any subsequent presentation was excluded to avoid duplicates.
IBD MDTMs were conducted weekly and attended by gastroenterologists, surgeons, radiologists, histopathologists, IBD nurses and IBD fellows who were present in person or virtually. A MDTM chair facilitated the meeting and the treating physician would present the clinical history, physical, diagnostic findings and their current and proposed management plan. Radiologists and pathologists reviewed relevant imaging and pathology, and treatment recommendations would be made following multidisciplinary discussion. The responsibility to accept or decline the group recommendations rested with the responsible physician. Patients could be added again to future MDTMs by any treating physician or specialist to update or discuss a disagreement with the MDTM treatment plan.
Data Collection
A dedicated IBD nurse prospectively recorded case data during each IBD MDTM on an electronic or paper abstraction form. Demographics included age at time of MDTM, gender, inpatient/outpatient and disease subtype further classified as follows: (1) new diagnosis of IBD, (2) IBD management in patients with a diagnosis > than 1 year and (3) acute IBD flare in a chronic patient (>1 year since diagnosis e.g., obstruction, bleeding).
Statistical Analysis
The primary outcome was defined as a change in final management plan as recommended by the multidisciplinary group discussion, and included admission to hospital, surgery, surgical referral, start or change of biologic therapy, change in dose or frequency of biologic therapy, start or change in IV/PO steroids, or addition of another medication (methotrexate, azathioprine, 5-ASA) or initiation of total parenteral nutrition [TPN]). A change in the final management plan was documented by the IBD nurse and reviewed by study personnel. Secondary outcomes included specialist involvement in the MDTMs and referrals (within and outside of MDTM participant specialities) occurring as a result of the MDTMs.
Implementation of the multidisciplinary consensus recommendation was subsequently assessed by reviewing the electronic medical record for verifiable evidence that it had been acted on within 6 months of the MDTM.
Data were evaluated using frequencies and means with standard deviations. All analyses were performed using SPSS Version 24 (IBM Corp., SAS Institute, Cary, NC).
RESULTS
Demographics
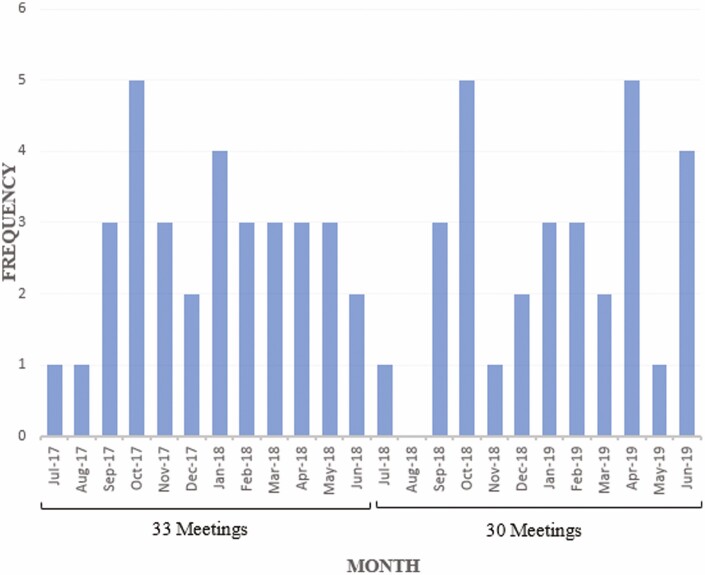
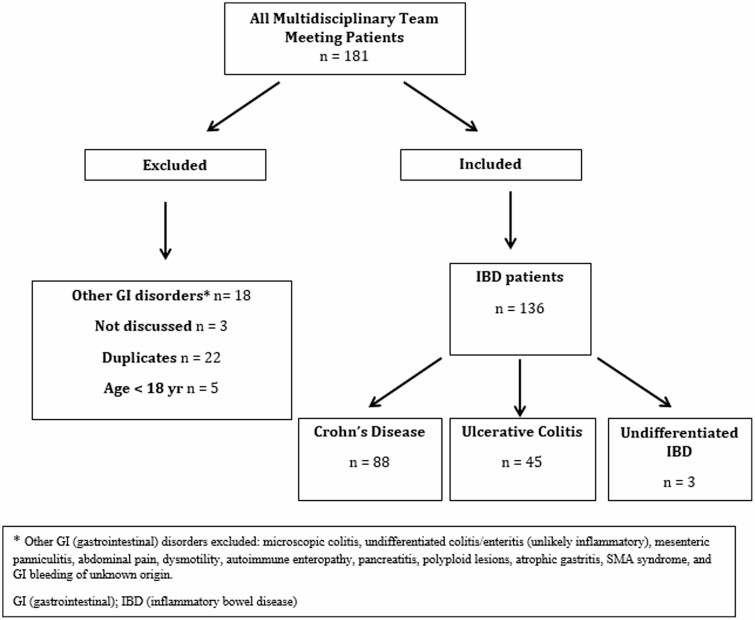
Sixty-three IBD MDTMs were held during the 2-year study period. One hundred and eighty-one patients were submitted for MTDM presentation, and 136 were included in the study. Forty-five patients were excluded due to age, duplicates or other GI disorders, or were listed and then not discussed at the MDTM (Figures 1 and 2).
Figure 1.
Frequency of IBD MDTM. IBD, Inflammatory bowel disease; MDTM, Multidisciplinary treatment meeting.
Figure 2.
Flow chart of included patients. *Other GI disorders excluded: microscopic colitis, undifferentiated colitis/enteritis (unlikely inflammatory), mesenteric panniculitis, abdominal pain, dysmotility, autoimmune enteropathy, pancreatitis, polyploid lesions, atrophic gastritis, SMA syndrome and GI bleeding of unknown origin. GI, Gastrointestinal; IBD, Inflammatory bowel disease.
Study Population
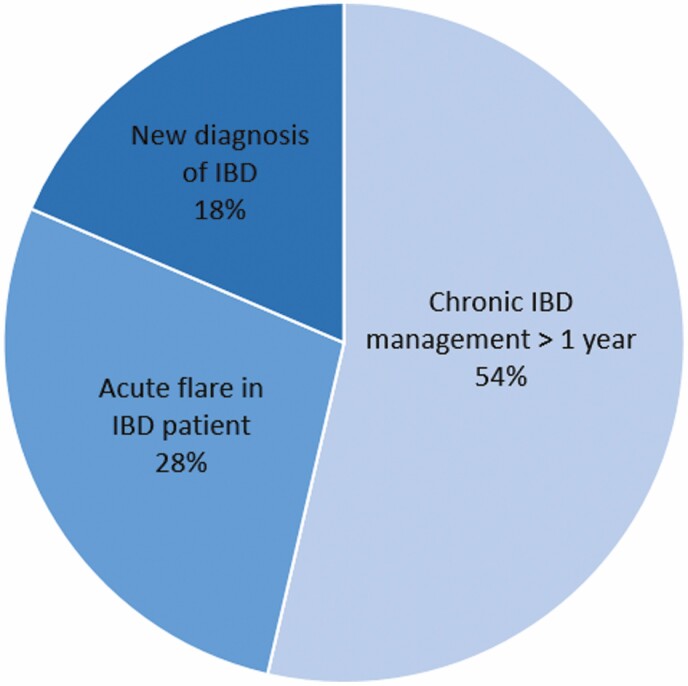
The study population of 136 patients comprised 59 males and 77 females, mean age of 46 years. There were 110 (81%) outpatient versus 26 (19%) inpatient cases presented. Indications for presentation included 71 (52%) patients with chronic IBD management potentially needing change in management, 37 (27%) with an acute flare in a chronic IBD patient and 24 (18%) with a new diagnosis of IBD. The disease process was classified into CD 88 (65%), UC 45 (33%) and undifferentiated IBD 3 (2%) (Table 1, Figure 3).
Table 1.
Patient demographics
| Patient demographics | Patients |
|---|---|
| Study population after exclusion (n) | 136 |
| Crohn’s disease n (%) | 88 (65) |
| Ulcerative colitis n (%) | 45 (33) |
| Undifferentiated IBD n (%) | 3 (2) |
| Inpatient n (%) | 26 (19) |
| Outpatient n (%) | 110 (81) |
| Age in years, mean (SD) | 46 (17) |
| Female sex n (%) | 77 (56) |
IBD, Inflammatory bowel disease.
Figure 3.
Patients presented at IBD MDTMs. IBD, Inflammatory bowel disease; MDTM, Multidisciplinary treatment meeting.
MDTM Management Recommendations
A change in the final treatment plan recommendation based on IBD MDTM consensus occurred in 35 (26%) of patients, representing 57 recommendations. The most common changes were recommendation for a surgical referral 17 (13%) or surgery 12 (9%), followed by the initiation of a new or different biologic therapy 11 (8%). Other consensus recommendations included the start or change in IV/PO steroids 5 (4%), initiation of TPN 4 (3%), start of other medications (azathioprine, methotrexate, 5-ASA) 3 (2%) and admission to hospital 2 (1%) (Table 2).
Table 2.
MDTM consensus change to initial treatment plan
| Change in management | Patients |
|---|---|
| Change in final management plan n (%) | 35 (26) |
| Surgical referral | 17 (13) |
| Surgery | 12 (9) |
| Start/change biologic therapy | 11 (8) |
| Start/change in IV/PO steroids | 5 (4) |
| Initiation of TPN | 4 (3) |
| Start of other medications* | 3 (2) |
| Admission to hospital | 2 (1) |
IV, Intravenous; MDTM, Multidisciplinary treatment meeting; PO, Per os; TPN, Total parenteral nutrition.
*Azathioprine, methotrexate, 5-ASA.
Implementation of IBD Recommendations
Of the 35 patients who had a recommended change to their treatment plan, 28 of 33 (85%) had this recommendation implemented within 6 months of IBD MDTMs. One patient did not have the recommendation implemented after further discussion with the surgeon due to minimal symptoms. Another two patients had a start/change of medications not recommended by the MDTM based on the patients’ responses to treatment and discussion between the patient and gastroenterologist. Follow up compliance information was not available for two patients due to the absence of provider documentation.
Specialist IBD MDTM Involvement and Referrals
Gastroenterologists submitted 132 (97%) of the cases for IBD MDTMs. A radiology opinion was obtained in 93 (68%), surgical opinion in 82 (60%) and pathology reviewed in 44 (32%) of patients. IBD MDTMs facilitated 33 surgical referrals, 6 gastroenterology referrals and 5 referrals to other specialists (genetics, hepatology, hematology, gynecology and dietitian) (Table 3).
Table 3.
Specialist involvement at MDTMs and referrals
| Specialists and referrals | Patients |
|---|---|
| Specialist involvement n (%) | |
| Gastroenterology | 136 (100) |
| Colorectal surgery | 82 (60) |
| Radiology | 93 (68) |
| Pathology | 44 (32) |
| Referrals n (%) | |
| General surgery | 33 (24) |
| Gastroenterology | 6 (4) |
| Other referrals* | 5 (4) |
MDTM, Multidisciplinary treatment meeting.
*Genetics, hepatology, hematology, gynecology, dietitian.
Discussion
Regular MDTMs were successfully implemented for IBD patients at a single academic centre. As a result, a change in patient management was recommended by the IBD MDTM group in more than 25% of patients, with a high rate of treating physician compliance of the recommendations. Gastroenterologists, surgeons, radiologists, pathologists and an IBD nurse were all integral to the composition of IBD MDTMs as evidenced by their frequent opinions and involvement. Our results support current literature which also concludes IBD MDTMs may lead to a change in treatment for a significant number of patients (11). The level of recommendations are in keeping with cancer MDTMs which have been observed to lead to changes in the treatment plan for breast, esophageal, gastric and colon cancers in 30% to 50% of patients, with the highest impact in patients who require multiple modalities of treatment (13–18).
It was notable that the most common management change recommendation was surgery or a surgical referral. Only 11 of 136 (8%) had an initiation or change of biologic therapy. This may be due to informal ongoing discussions between the gastroenterologists that occurred outside of the MDTMs, especially by those with a high volume of IBD patients. Concurrent with other literature, we identified eligible cases for discussion in the IBD MDTM including those with a new diagnoses, patients on biological agents, those who have undergone recent IBD surgery, or complex cases requiring surgery (9).
Outpatients were more likely to be submitted for presentation than inpatients. Inpatients may be more likely to have their treatment plan expedited by virtue of the acute nature of presentation as the gastroenterologist will likely approach the surgeon through the normal inpatient consultation route, without waiting for the next MDTM. This would be in adherence to previous literature by Nichols et al., suggesting outpatients are more likely to benefit from a MDTM (19). However, in contrast to cancer MDTMs, decision making with the chronic IBD outpatient may be less objective as the symptomatology and perception of the patient’s needs are integral to the decisions, and must be considered in management (19).
Aside from direct change to patient care, the IBD MDTM provides an source of interdisciplinary education through promoting best practice, integrating research updates, discouraging opinion- or experience-based decisions and expediting care (19). As IBD patients may have an unpredictable course with multiple relapses, this may result in both physician and patient frustration. The support of colleagues, second opinions and documentation of the MDTM discussion is likely beneficial to the treating physician and patient even if no change in management was recommended, and could be measured in future studies.
IBD MDTMs require an administrative structure and require time that physicians must devote to attend meetings, often making it difficult for every person to be present. While multidisciplinary care may be obtained through multiple consultations, our results corroborate with other studies the inherent value of a meeting involving multiple disciplines in a single setting (11,19). This was demonstrated not only through a consensus management change recommendation, but also the through the collaboration of diagnostics, clinical decision making, and planning in a single setting facilitating patient care. While a thorough economic analysis was not completed in our study, administrative time to facilitate IBD MDTMs was 3 to 4 hours/week and physician time was 1 hour/week of uncompensated time per attending physician. There were no room rental costs and coffee and tea were provided to attendees. Fader et al. demonstrated a cost savings benefit in oncology MDTMs compared to conventional treatment (8). Governments and hospitals may require more objective evidence of benefit prior to covering these expenses for IBD MDTMs.
Although IBD MDTMs were implemented weekly, on average they occurred two to three times per month for 1 hour (Figure 1). This was likely a consequence of the number of IBD patients submitted, and availability of multiple disciplines throughout various times of the year. The number of patients presented, and frequency of IBD MDTMs suggests that a centre providing care to approximately 5000 IBD patients per year could institute similar MDTMs biweekly. A more formal MDTM template outlining the presenting complaint, clinical history, current and proposed treatment plan, discussion during MDMT, as well as clear consensus recommendations which would remain in the patient’s clinical records may reinforce the value of IBD MDTMs to different stakeholders, including a copy sent to the primary care physician (9). Organizational recognition of IBD MDTM and implementation into the job plan for core members would also likely encourage attendance.(9) Care needs to be taken that an MDT for IBD does not become a burden for those physicians who already may also be committed to attend other MDTMs, such as for gastrointestinal oncology.
The strengths of this study include its prospective nature over a prolonged time period with direct assessment of each case to assessment of each case for implementation of the MDT recommendation. Limitations should be acknowledged. It is a prospective cohort study and therefore has inherent bias with the observational design and opportunity for selection bias as treating physicians may not have forwarded all eligible patients to the MDTM. Informal discussion between specialists is difficult to quantify, which is likely to have underestimated the referrals or communication that occurred between stakeholders. While 26% of patients had a treatment recommendation change, there was no control group for comparison, therefore a sample size and probability values could not be calculated, and the results may not reflect any improvement over standard practice. Compared to the MDTM for cancer, the broad variability of IBD severity and lack of concrete end-points such as survival, make it difficult to quantify whether MDT result in improved individual patient outcomes.
Conclusion
Presentation of patients with inflammatory bowel disease at multidisciplinary conference lead to direct changes in patient management in one quarter of cases, most notably recommendation for surgery or surgical referral, followed by change in biological therapy In addition, they promoted collaboration and support among specialists, improving education and promoting best practice, and discouraging idiosyncratic decision-making. Further prospective studies or large data-base studies are needed to determine if an IBD MDTM consensus recommendation translates to improved patient outcomes over standard practice.
Work performed at London Health Sciences Centre and Western University.
Funding
None declared.
The contents of this manuscript are not copyrighted, published previously or under consideration for publication elsewhere.
Conflict of Interest
None declared.
References
- 1. Mowat C, Cole A, Windsor A, et al. ; IBD Section of the British Society of Gastroenterology . Guidelines for the management of inflammatory bowel disease in adults. Gut 2011;60(5):571–607. [DOI] [PubMed] [Google Scholar]
- 2. Tsai L, Ma C, Dulai PS, et al. Contemporary risk of surgery in patients with ulcerative colitis and Crohn’s disease: A meta-analysis of population-based cohorts. Clin Gastroenterol Hepatol 2020. doi: 10.1016/j.cgh.2020.10.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Morar P, Read J, Arora S, et al. PWE-094 setting standards by defining the aims and optimal design of the inflammatory bowel disease (IBD) Multidisciplinary Team (MDT) Meeting. Gut 2014;63(Suppl 1):A165.1–A165. [Google Scholar]
- 4. Snelgrove RC, Subendran J, Jhaveri K, et al. Effect of multidisciplinary cancer conference on treatment plan for patients with primary rectal cancer. Dis Colon Rectum 2015;58(7):653–8. [DOI] [PubMed] [Google Scholar]
- 5. De Ieso PB, Coward JI, Letsa I, et al. A study of the decision outcomes and financial costs of multidisciplinary team meetings (MDMs) in oncology. Br J Cancer 2013;109(9):2295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stephens MR, Lewis WG, Brewster AE, et al. Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer. Dis Esophagus 2006;19(3):164–71. [DOI] [PubMed] [Google Scholar]
- 7. Burton S, Brown G, Daniels IR, et al. ; Royal Marsden Hospital, Colorectal Cancer Network . MRI directed multidisciplinary team preoperative treatment strategy: The way to eliminate positive circumferential margins? Br J Cancer 2006;94(3):351–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fader DJ, Wise CG, Normolle DP, Johnson TM. The multidisciplinary melanoma clinic: A cost outcomes analysis of specialty care. J Am Acad Dermatol 1998;38(5 I):742–51. [DOI] [PubMed] [Google Scholar]
- 9. Morar PS, Sevdalis N, Warusavitarne J, et al. Establishing the aims, format and function for multidisciplinary team-driven care within an inflammatory bowel disease service: A multicentre qualitative specialist-based consensus study. Frontline Gastroenterol 2018;9(1):29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ricci C, Lanzarotto F, Lanzini A. The multidisciplinary team for management of inflammatory bowel diseases. Dig Liver Dis 2008;40(SUPPL. 2):S285–8. [DOI] [PubMed] [Google Scholar]
- 11. Ferman M, Lim AH, Hossain M, et al. Multidisciplinary team meetings appear to be effective in inflammatory bowel disease management: An audit of process and outcomes. Intern Med J 2018;48(9):1102–8. [DOI] [PubMed] [Google Scholar]
- 12. STROBE Statement-Checklist of Items That Should Be Included in Reports of Cohort Studies. http://www.epidem.com/ (Accessed May 10, 2020). [DOI] [PubMed]
- 13. van Hagen P, Spaander MC, van der Gaast A, et al. ; Rotterdam Oesophageal Tumour Study Group . Impact of a multidisciplinary tumour board meeting for upper-GI malignancies on clinical decision making: A prospective cohort study. Int J Clin Oncol 2013;18(2):214–9. [DOI] [PubMed] [Google Scholar]
- 14. Kaifi JT, Gusani NJ, Jiang Y, et al. Multidisciplinary management of early and locally advanced esophageal cancer. J Clin Gastroenterol 2011;45(5):391–9. [DOI] [PubMed] [Google Scholar]
- 15. Newman EA, Guest AB, Helvie MA, et al. Changes in surgical management resulting from case review at a breast cancer multidisciplinary tumor board. Cancer 2006;107(10):2346–51. [DOI] [PubMed] [Google Scholar]
- 16. Davison AG, Eraut CD, Haque AS, et al. Telemedicine for multidisciplinary lung cancer meetings. J Telemed Telecare 2004;10(3):140–3. [DOI] [PubMed] [Google Scholar]
- 17. Wheless SA, McKinney KA, Zanation AM. A prospective study of the clinical impact of a multidisciplinary head and neck tumor board. Otolaryngol Head Neck Surg 2010;143(5):650–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Junor EJ, Hole DJ, Gillis CR. Management of ovarian cancer: Referral to a multidisciplinary team matters. Br J Cancer 1994;70(2):363–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nicholls J. The inflammatory bowel disease unit and the multidisciplinary team meeting. Colorectal Dis 2007;9(6):477. [DOI] [PubMed] [Google Scholar]