Abstract
Pre-exposure prophylaxis (PrEP) is an important HIV prevention method for adolescent girls and young women (AGYW) in Africa, who are at heightened risk of HIV infection. HIV risk perception is generally a powerful motivator for adoption of HIV prevention behaviors, including PrEP use. While HIV risk perceptions have been evaluated using quantitative measures, these seldom capture how individuals conceptualize and understand risk within local frameworks of meaning. More nuanced understanding may come from qualitative approaches that map these perceptions across the trajectory of sexual histories. Between 2016 and 2018, we implemented a novel participatory method to investigate risk perceptions in interviews with 32 participants in HPTN 082, a study of AGYW’s use of PrEP in South Africa and Zimbabwe. Timelines were used to record narrative sexual histories and perceived HIV risk for each relationship. We found that women assessed HIV risk primarily based on their partners’ personal qualities and behavior (especially relating to infidelity); their subjective experience of being treated respectfully; and the practice of perceived ‘risk reduction’, including younger partners and condoms, even if used inconsistently. A narrative timeline approach grounded in an understanding of young women’s sexual histories may increase critical reflection about HIV risks and facilitate risk-reduction counselling with this group.
Keywords: PrEP, adolescent girls and young women, sexual histories, HIV risk perceptions, qualitative research, South Africa, Zimbabwe
Introduction
Access to oral pre-exposure prophylaxis (PrEP) to prevent HIV infection is being expanded across southern and East Africa, regions with the highest HIV incidence globally (1). PrEP use is not intended to be life-long but is limited instead to periods of heightened vulnerability to HIV (2, 3). Prevention-effective adherence – i.e. use during periods of high risk – may lead to more efficient PrEP use, with fewer side effects and lower costs (4, 5). HIV risk perception is generally a powerful motivator for adoption of HIV prevention behaviours, including PrEP use (6, 7). However, studies have shown that even where the likelihood of infection is high, people may underestimate their risk exposure (8–10).
Recognising one’s own vulnerability to HIV is complex. This typically requires considering oneself in a stigmatised category based on “risky” sexual behaviour (11, 12). Widespread stigma associated with illness, death and sexual transgression has been a feature of the AIDS pandemic from the outset (13). Understandably, people may be reluctant to self-stigmatise, which may explain why some deny or downplay their personal risk of HIV infection. Further causes of risk under-estimation may include ‘present bias’, where short-term rewards are prioritised over longer-term outcomes (14), and (among young people) ‘optimism bias’, the tendency to assume that one is invulnerable to danger and disease (15). Self-perception of HIV risk may also be dynamic. In the SEARCH study in Kenya and Uganda of PrEP uptake after population-level HIV testing, for example, approximately one-fifth of participants changed their self-assessment of risk between week 4 and week 24 of the study, and as risk perceptions fluctuated, so too did adherence to PrEP (1, 16).
These patterns suggest that HIV risk perceptions and decision-making about risk-reducing behaviours are not fully rational processes based purely on a cost-benefit analysis, as proposed by the Health Belief Model, for example (17). Innovative approaches are needed that are sensitive to the multi-dimensional, contingent nature of risk and how it is perceived (18). To date, the focus has been to develop validated tools for quantitatively measuring risk perceptions in sexual health and HIV studies (7, 19, 20). While these approaches have value, they often rely on static definitions of risk that may not have relevance across multiple settings. Additional and more nuanced understanding may come from qualitative and mixed-methods approaches to capture how individuals conceptualise and understand risk within local frameworks of meaning (3, 21, 22).
Drawing inspiration from visual methods and the use of a historical lens in qualitative health research (23, 24), we adapted a novel qualitative approach to risk perception measurement (25) and applied this in a study of adolescent girls and young women (AGYW) taking oral PrEP in South Africa and Zimbabwe (26). Our approach combined narrative sexual histories, a subjective numerical scoring of risk, and a visual timeline, with a focus on exploring how women viewed their historical HIV risk with different partners across the lifespan.
Methods
Study design and participants
Data are drawn from qualitative interviews with a subset of participants enrolled in HIV Prevention Trials Network (HPTN) 082, a randomised, open-label clinical trial assessing African AGYW’s acceptance of and adherence to daily oral emtricitabine/tenofovir (FTC/TDF) PrEP (26). Between 2016 and 2018, the trial enrolled 426 young women aged 16–25 years from Cape Town and Johannesburg, South Africa, and Harare, Zimbabwe. Women were eligible for enrolment if they were HIV-negative, literate in one or more of the study languages (English, isiXhosa, isiZulu, SeSotho, or Shona), sexually active in the month prior to screening, and scored ≥5 (out of a possible range of 0–10) on the VOICE risk score tool (27). Participants were enrolled irrespective of whether they accepted PrEP or not.
The study received ethical approval from research ethics committees at the University of the Witwatersrand, University of Zimbabwe, University of Cape Town, University of California - San Francisco, and University of Washington. All participants provided written informed consent in their preferred local language before participation. In the Johannesburg site, participants younger than 18 years provided assent with consent from a parent or legal guardian.
Study settings
Participants in all three study sites lived in high density, low-income settlements. In Cape Town, HPTN 082 participants were mainly recruited from areas surrounding the study clinic, encompassing the township communities of Crossroads, Nyanga, have high rates of crime and unemployment, and generally poor service delivery. Participants in the Johannesburg site were recruited from areas within the inner-city neighbourhoods of Hillbrow and Berea. A high proportion of residents in these areas are migrants seeking to gain a foothold in the city, and accommodation mostly takes the form of densely populated and neglected apartment blocks situated alongside small retail shops, brothels and entertainment venues (28). In Harare, women were recruited from clinics in high density suburbs on the outskirts of the city that are marked by poverty and crime. These clinics offer HIV screening, STI treatment and family planning to female sex workers. Additional participants were recruited from community gatherings for youth in liaison with youth Community Advisory Board (YCAB) members.
Qualitative study
Sampling and recruitment
For the qualitative study, we aimed to recruit up to 25 participants per site from the HPTN 082 cohort. Purposive sampling was used to recruit participants across a range of PrEP experiences, incorporating those who had accepted PrEP and were adhering well to it, those experiencing adherence challenges, and those who had declined PrEP altogether. At each site, we also sought out 2–4 participants who had been placed on product hold for protocol-specified safety reasons (e.g. pregnancy).
Data collection
Participants were invited to take part in individual in-depth interviews (IDIs) at two time-points, after the 13- and 26-week study visits. Interviews were carried out between March 2017 and October 2018 by trained social scientists and in participants’ preferred language. They took place in a quiet, private venue at the study sites and lasted on average 45 minutes. Written informed consent was obtained from all participants prior to the interviews. Interviewers followed semi-structured topic guides based on literature reviews and the study team’s prior experience of PrEP delivery and research. Key focal areas of the interviews included: women’s motivations to take PrEP; facilitators and barriers to PrEP adherence; the influence of sexual partners, friends and family on PrEP use; and, among those who did not initiate PrEP, their reasons for refusing PrEP.
Preliminary analysis after the week-13 interviews had been concluded and about a third of the way through the week-26 interviews showed that the data were somewhat superficial, suggesting limitations to the use of standard IDI techniques in exploring these topics with this age group. To collect richer data on women’s past and current sexual behaviour, the types of sexual partnerships formed, and how they conceptualised HIV risk within these partnerships, we introduced a novel method for inclusion in the remaining two-thirds of the week 26 interviews. This involved an adaptation of the life history calendar method (29), with the inclusion of a participatory element to encourage greater involvement of the women being interviewed. The interviewer asked participants to draw a horizontal line on a single page and treat this as a ‘relationship timeline’ (25), on which each sexual relationship was to be marked off, from sexual debut to the current partner, moving through time from left to right. Participants could assign pseudonyms or labels to individual partners based on their defining characteristics. The interviewer then probed about the circumstances and narrative arc of each relationship, and about factors perceived to impact on individual risk of HIV infection, including condom use, relationship power and conflict, substance use, and multiple concurrent partnerships. Participants were also asked to indicate in which past relationships they would have taken PrEP, had it been available. They were encouraged to add further descriptive notes to the timeline if they so wished.
After narrating their sexual histories in this way, participants were asked to assign a numerical risk score from 1 (least risk) to 5 (highest risk) to each relationship, and to note these scores on the timeline. Unlike the VOICE risk score tool (27) and other similar empirically validated risk scoring tools and algorithms (30, 31), our scoring system was not intended to objectively gauge the risk level of reported behaviour in relation to incident HIV infections. Instead, it was applied subjectively by participants, and was intended as a tool to support the construction and articulation of their sexual histories. The timeline exercise, inclusive of risk score allocation, took 15–20 minutes on average to complete.
Interviews (including the timeline exercise) were audio-recorded, transcribed, translated from local languages into English, and checked by site teams for accuracy. The original (hard copy) timelines were stored in a secure location, while electronic copies were made as back-up and password protected. Timelines were identified by participant ID number only and linked to the interview transcripts using this ID number.
Data analysis
From the completed timelines, we developed full descriptive narratives for each participant. A matrix was then developed to isolate participant-identified risk factors within these narratives, along with the risk scores they had assigned to each relationship. The matrix collated these details into a single framework for comparison of risk scores, descriptive data on risk perceptions, and related themes across the sample.
While the analysis presented here reports data only from the timeline exercise, to contextualise and interpret these data, we also drew on the larger dataset of interviews from all participants in the qualitative study. These transcripts were coded using a thematic, inductive approach (32). They were imported into NVivo (versions 11 and 12; QSR International, Melbourne, Australia) and an initial codebook containing key themes was created following open coding (33) by qualitative team members. Once the codebook was finalised, each transcript was then coded independently by a member of the qualitative study team, all eight of whom had prior experience in qualitative data coding. Three of the coders had also conducted interviews in the study sites. Coding was reviewed by FS on approximately 20% of the transcripts and disagreements in code application resolved through “reconciliation discussions” with individual coders (32). Additional in-depth discussion and analysis of key themes was undertaken during an in-person workshop involving qualitative team members from all three sites. Topic areas and themes from the coded interview data considered relevant to the analysis presented in this article are summarised in Table 1. Throughout the manuscript, we present representative quotations from participants using pseudonyms for all names.
Table 1.
Key themes from the IDIs of relevance to the analysis
| Topic area | Themes |
|---|---|
| Sexual and reproductive health | Contraceptive and condom use; STI history; HIV testing history; fertility desires |
| Sexual Relationships | Duration of relationships; quality of communication; decisionmaking about safe sex and contraception; conflict and violence; multiple partners, trust, and partner infidelity; transactional sex; HIV testing with partner |
| Knowledge and beliefs about PrEP | Beliefs about PrEP efficacy; understanding of dosing requirements; concerns about side effects; community awareness of PrEP; sources of information about PrEP; beliefs about the need for condom use with PrEP |
| HIV risk perceptions | Perceptions of risk from partner infidelity and alcohol use; risk as a sex worker; condom use and condom failure; risk from sexual violence; being part of a generation at risk; perceptions of high HIV prevalence in community; risk of infection with STIs other than HIV; impact of HIV risk perceptions on PrEP use; perceptions of ongoing HIV risk |
| PrEP adherence | Barriers and facilitators to adherence; self-reported adherence; reasons for initiating, discontinuing, and restarting PrEP |
| PrEP disclosure to partner | Informing vs seeking permission from partner for PrEP taking; partner response to PrEP disclosure; conflict following disclosure; concealing PrEP from partner |
| Changes in relationship with partner during the study | Intensification of inter-personal conflict; termination of relationships; reduction in sexual intimacy; condom disinhibition; partner reduction; acquisition of new partners; changes in perceptions of personal HIV risk; improved communication; no change in sexual behaviour |
Results
Sample characteristics
A total of 67 women were enrolled in the study, 56 of whom completed both interviews. Because the timeline exercise was introduced partway through the interviewing process, only 32 of the 56 participants who took part in the second (week 26) interview completed the timeline exercise (Johannesburg=11, Cape Town=7, Harare=14). Around two thirds of the timeline participants (22/32) had accepted PrEP and (based on self-report) were taking it by the time of the first (week 13) interview. They were a median of 22 years of age (IQR 17–25), and most (22/32) had completed secondary school or higher (see Table 2). At the Cape Town and Johannesburg sites, more than half were students at the time of the interviews, either in the final year of secondary school or in tertiary education. Three quarters of the sample (24/32) reported either dating or having at least one main partner, and 5 participants were married (the latter all in Harare). Just over half (18/32) said they were living with their parents, although in Harare this figure was lower (42%). A portion of the Harare sample included sex workers who worked in local bars and nightclubs.
Table 2.
Socio-demographic characteristics of HPTN 082 participants in the timeline exercise
| Characteristic | Harare (n=14) | Cape Town (n=7) | Johannesburg (n=11) | Total (n=32) |
|---|---|---|---|---|
| Age, in years | ||||
| Median (IQR) | 21.5 (17–24) | 20 (18–22) | 24 (21–25) | 22 (17–25) |
|
| ||||
| Education | ||||
| Some secondary school | 3 | 6 | 1 | 10 |
| Completed secondary school or higher | 11 | 1 | 10 | 22 |
|
| ||||
| Employment status | ||||
| Employed | 4 | 1 | 1 | 6 |
| Unemployed | 6 | 1 | 4 | 11 |
| Current student (secondary or tertiary education) | 4 | 5 | 6 | 15 |
|
| ||||
| Relationship status | ||||
| Single, no sexual partners | 3 | 0 | 0 | 3 |
| Dating (at least one sexual partner but casual) | 0 | 0 | 3 | 3 |
| In a relationship (at least one main serious partner) | 6 | 7 | 8 | 21 |
| Married | 5 | 0 | 0 | 5 |
|
| ||||
| Living with: | ||||
| Parents | 6 | 6 | 7 | 19 |
| Partner | 6 | 0 | 0 | 6 |
| Other (e.g. other family members, roommates, children) | 2 | 1 | 3 | 6 |
| Alone | 0 | 0 | 1 | 1 |
|
| ||||
| HIV risk scores assigned (n=142 relationships) (%)* | ||||
| Low risk (0–2) | 27 (48.2) | 13 (50.0) | 28 (46.7) | 68 (47.9) |
| Medium risk (3) | 7 (12.5) | 5 (19.2) | 6 (10.0) | 18 (12.7) |
| High risk (4–5) | 18 (32.2) | 8 (30.8) | 18 (30.0) | 44 (31.0) |
| No score given | 4 (7.1) | 0 (0.0) | 8 (13.3) | 12 (8.4) |
column percentages
Key Patterns in the Timelines
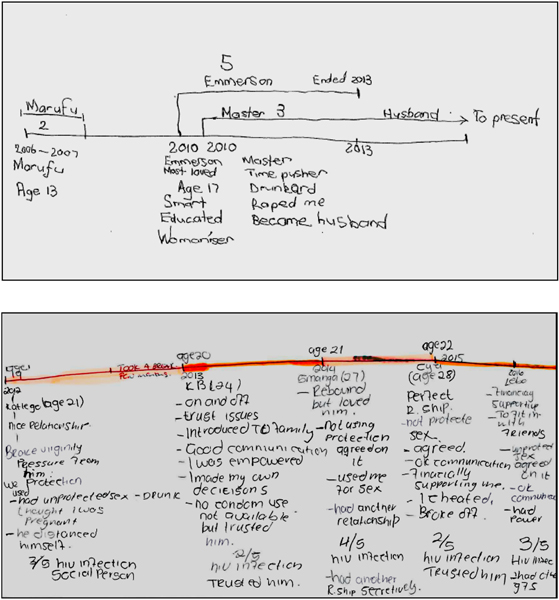
The 32 timelines collected from participants encapsulated 142 discrete sexual relationships (See Figure 1 for examples). Women in Johannesburg recorded a mean of 5.5 partners, while women in Cape Town and Harare recorded a mean of 3.8 partners each. The kinds of relationships narrated by the young women took many forms, from those involving a deep emotional commitment, to casual relationships embarked on to alleviate boredom, and from brief ‘one-night stands’ to long-term transactional sex relationships. There were women who had had only one sexual partner in their lives, while others claimed to have had so many partners, together they would “fill a bus”.
Figure 1.
Two examples of sexual history timelines produced by participants in HPTN 082
Just over half (56%) of the women who completed the timeline exercise reported sexual debut under the age of 18; women in the Harare and Johannesburg sites reported first sexual intercourse at an average of 17.6 and 17.4 years respectively, while in Cape Town this was lower, at 15.9 years. About a third (10/32) of participants described their first sexual experience as unwanted. In Harare, three women reported this as being forced or tricked into sex; one subsequently married her partner after he had raped her, following social pressure to do so. Sexual violence by an intimate partner featured also in the narratives of a few women in the Johannesburg and Cape Town sites, but more frequent was the mention of physical violence and controlling behaviour by partners in these sites. Across all sites, physical, sexual, or emotional violence was explicitly mentioned in a quarter of all relationships depicted in the timelines (36/142).
Some participants chose to list romantic relationships prior to sexual debut on their timelines, for example, high school “flings” or relationships that were simply too new for sexual intimacy. This was especially the case in Harare, where some women listed as many as 6 or 7 such relationships (which we included in our tally of 142 ‘sexual relationships’ above). Since the interviewers’ instructions for completing the timelines were similar across all three sites, the prominence of these romantic, nonsexual relationships among Harare participants may reflect local gendered norms around dating behaviour, since pre-marital sex is frowned upon in this setting.
Transactional sex was described in roughly a quarter of all timeline relationships in Harare (23%) and just under a third (30%) of those in Johannesburg and Cape Town. A subset of these transactional relationships occurred with men known as “blessers”. These are typically older, well-resourced men who support young women with cash, gifts, and luxury goods in exchange for multiple sexual encounters, and with whom there is initially little emotional connection or commitment (34). Short-term relationships with casual partners also featured strongly across the women’s narratives; these tended to be peers rather than older men. In Harare these were referred to as “ghetto boys”, “pain easers” (new partners to ease the emotional pain of a break-up) or “time pushers” (partners to alleviate boredom). A handful of participants in this site described regularly attending “dance hall bashes”, where they got drunk and found casual partners. In Johannesburg, casual partners were “fuck boys” or “players”, and in Cape Town, they were “side men”, nomenclature suggesting the co-existence of a main partner. Only a handful of women documented their own concurrent partners on their timelines (typically marked as multiple overlapping lines or segments), however, although these were mentioned more frequently during interviews. The Harare participants who were sex workers reported multiple sexual encounters with clients but did not list these in their timelines.
Assessing risk
Most of the 142 relationships featured in the timelines were rated using the 1–5 risk scale (91%). Relationships not rated in this way were mostly those where no sex had occurred or where participants chose instead to simply use the labels “high risk” or “low risk”. Below, we describe participants’ assessment of the relative risk profiles of their relationships, isolating the key factors that women considered to be determinants of risk. Four main themes emerged. Firstly, there was an emphasis on the personal qualities of male partners and an assessment of their behaviour against a set of moral ideals. Secondly, participants attributed risk to a partner based on the depth of trust and respect in the relationship, a judgement directly related to experiences of partner infidelity. Thirdly, many women interpreted the presence of risk reduction behaviours as protective and as signs that a relationship was relatively safe. Finally, in the face of stark evidence of likely HIV risk exposure, such as contracting an STI in a relationship, most women’s awareness of risk became more acute and the emphasis on protective factors fell away.
“A good person”: Risk and the ideal partner
Across all sites, where a partner was portrayed in positive, somewhat idealised ways, the relationship tended to be rated low risk (0–2 on the risk scale; see Table 2). Women used terms such as “decent and respectful”, “fun”, “kind” and “with a good heart”, “a good person” and “perfect” to describe these partners. To a large extent, what mattered when it came to assessing partners’ personal qualities was how the women remembered being treated by them. Some participants recalled that they had “felt loved and respected” by these men and loved them in return. In Johannesburg, relationships that featured shared decision-making and positive partner communication, and where women recalled feeling “empowered”, were considered low risk, as were men with a “gentle” disposition. These were partners who displayed little aggression, tended to “not quarrel”, and did not make sexual demands on women or force them to have sex when they were not yet ready. This was how Tafadzwa from Harare, aged 21 years, described her first partner, who was “humble, loving and caring”, and earned a risk score of zero:
Amongst all my boyfriends, he was the best … he never touched my body or done anything…[yet] he was that person who could have taken advantage of me because I was still naive.
Men who were shy or religious were also considered low risk because they were deemed unlikely to be deceitful or engaged in other relationships.
The flip side of this pattern was that exuberant, over-confident personalities – such as men who were said to be “full of themselves”, “immature”, or “talkative” – were automatically regarded as higher risk. A common way of framing this was a reference to men as ‘busy’: their multiple social engagements, frequent absences, and consequent inattentiveness pointed to an unwillingness to invest emotionally in the relationship and suggested, perhaps, the presence of other sexual liaisons.
Meeting the financial needs of women and their dependants was often seen as demonstrating a man’s personal integrity and commitment to a relationship. Framed as being “taken care of” by men, this quality was highly valued across the three sites. However, it obscured some of the vulnerability faced by women in these relationships, evidenced by the fact that as much as half of all relationships involving transactional sex were rated with a zero or 1 on the risk scale. This normative valorisation of men as ‘providers’ emerged in a number of participant narratives. Danai from Harare, for example, recalled her first partner embodying the provider role in both his actions and appearance. Explaining why she had rated him low risk (‘1’ on the scale), she said:
With that care he had in that he covered for the boys’ [her older brothers’] responsibilities at our house, that’s why I loved him…Plus he was handsome. Plus, he dressed well. Plus, he was someone who worked.
Even partners living on the wrong side of the law were valued for their ability and willingness to provide financial support to women. Explaining why many of the partners she had dated over the years had been criminals, or (in her own words) “thugs”, who made a living from armed robbery, Kabelo from Johannesburg observed that “they take really good care of you”. Yet there was some ambiguity in interpreting relationships with men who were materially well-off or financially stable. ‘Busy’ men who conspicuously flaunted their wealth were seen as higher risk partners because they were said to “lure” other women with the promise of gifts and material support. And when men were no longer able or willing to ‘take care of’ women and their dependents, they appeared to diminish in women’s esteem and be regarded as less-than-ideal partners who potentially posed a greater than average HIV risk.
“Womanisers”, “Smooth talkers” and “Cheats”: Infidelity, trust, and respect
While the personal qualities and material wealth of a partner were important aspects of defining risk, they were not the only considerations. A second theme that dominated our analysis involved the question of how much women believed they could trust a partner. This was appraised almost entirely within the narrow context of partner fidelity. Relationships where participants suspected or knew there was partner infidelity tended to be rated “3” or higher on the risk scale. Unfaithful partners were described in strong terms, evident in the pseudonyms chosen by participants to label them on their timelines. They were “womanisers” (Harare), “smooth talkers”, “players” (Johannesburg), “a woman’s man” (Cape Town), and “cheats” (all sites). One woman spoke of a partner as “a dog” and the “the most cheating [man] on earth…a shit human being” (Dikeledi, 21 years, Johannesburg).
For many participants, the default was to assume men were fundamentally untrustworthy, given that it was their ‘nature’ to have more than one sexual partner at a time. The comment on this of seventeen-year old Tariro from Harare was typical:
The rule that I stand by is never to trust anyone. I cannot trust my boyfriend to the extent of saying I can never get HIV. For example, right now I am here, I don’t know what he is up to. He can tell me that he is at work when he is not there.
At the age of 17, Ntokozo met and started a relationship with a 19-year-old man in Johannesburg. After four months of dating, they had sex. It was around this time that she discovered that he was seeing other partners.
You see men always want to have two girlfriends. They will date the other one in secret and the other, meanwhile you have no idea what’s going on. You will find that ja, when he’s with you, he treats you right, like his queen, like, everything is fine. Wow, and next thing you go visit him, yoh! This I will never forget…When I arrived at his place, I knocked, and he answered the door. Wow, and then I noticed that this guy is avoiding eye contact and I’m like, ‘what is going on here? …Only to find out he is with another girl…and so when I saw her, I just left and went straight home.
Ntokozo rated him a 4 on the scale and regarded her risk from this relationship the highest of all three relationships depicted on her timeline. The experience affected her deeply and shaped her interactions with other men in the months to come. Following the break-up, Ntokozo recalls, “I didn’t want a boyfriend, and then I was single for an entire year in 2014. I chose to remain single yoh. I just couldn’t.”
Not living with a partner was a situation thought to encourage partner infidelity, thereby making women more vulnerable to HIV infection. Nwabisa from Cape Town saw the fifth partner in her timeline (whom she dated when 21 years old) as high risk for STI exposure, explaining, “he stays far from me – so wherever he is, I don’t know what he is doing because I don’t see him.” Similarly, migrant workers or those whose jobs required travel were high-risk partners. This was aptly described by 23-year-old Kudzai, herself a migrant worker who travelled regularly between her rural home and the suburbs of Harare, where she was employed as a domestic worker. In her timeline, her first partner at the age of 18 years was “a good person”: the father of her two children, who eventually became her husband. When they were first married, he worked as a bus driver on local routes. Then he began to travel further afield, driving outside of Harare as far as the South African border. Over time, his financial contributions to cover household expenses ceased and visits home became less frequent. Three years later, they separated. Unable to suggest condom use in the later stages of the relationship, she ranked him a ‘5’ on the risk scale because of his lengthy absences from home. Kudzai explained, “ You may have sex with him once a month. Where will he be having sex all the other time?” She expressed that had PrEP been available at the time, she would have taken it, recalling that “life was painful…you would notice that you are really at risk for sure”.
Across the three sites, women spoke openly about the shame and embarrassment they felt when a partner’s infidelity became public knowledge. Whereas an unfaithful partner might still be rated of ‘medium risk’ (a ‘3’ on the scale), if his infidelities were openly flaunted, their risk was usually elevated to a ‘5’. Twenty-five-year-old Karabo from Johannesburg listed 8 relationships on her timeline and explained why she rated the fourth of these and the father of her child the highest risk of all her partners:
[He would] humiliate me in front of his girlfriends…I arrived at his place once, and his girlfriend was there, and then there was drama, he slapped me…
Several women in Johannesburg and Cape Town described feeling “used for sex” and “not respected” in these high-risk relationships. Asiphe from Cape Town recalled that her first partner, whom she dated when she was 18, was open about the numerous other sexual partners he was seeing at the same time. This left its mark on her; she remembered, “I felt useless because he didn’t see me as a person”. Of the four relationships on her timeline, 24-year-old Nompumelelo from Johannesburg regarded the man who had fathered her child as the one who had exposed her to the highest risk of HIV infection. Named as “Baby Daddy” (lit. the father of her baby) on her timeline, he had supported her financially, but was abusive and violent, at times attempting to strangle her when they argued. For Nompumelelo, however, the elevated risk he posed stemmed not from his violent nature or the practice of unsafe sex, but from the fact that “…most of the time he didn’t have respect. [Other] people used to call me to say, ‘I am with your boyfriend’, this and that.”
Such was the importance of ‘respect’ in a relationship, that infidelity could even be tolerated, provided it was done discreetly. Twenty-year-old Phumza from Cape Town, whose current partner would regularly go to parties and “come back with a different woman”, said, “I don’t mind, I know that guys cheat. But at least he shouldn’t do it for me to see, at least try to respect me.” In spite of clear evidence of his infidelity, another woman memorably described her high-risk partner as her “joyful ride”, someone she felt she could “explore the world with” (Refiloe, 23 year old, Johannesburg). Overall, however, in relationships marked by disrespect and betrayal, the high risk scores showed that women felt at their most vulnerable to HIV, with an emotional impact that remained long after these relationships had come to an end.
Being “responsible”: practising risk reduction
Occasionally, participants’ narratives gestured towards the broader social context in which HIV risk was constructed, as they referenced the heightened vulnerability to HIV infection faced in particular by young women in these settings. In part, this awareness came from personal experience of friends, neighbours, classmates, and colleagues who were living with HIV. Women overall, but especially in the two South African sites, also noted the potential risk from sexual assault, which was experienced – and feared – as widespread in their communities. For participants in Harare who were sex workers, the workplace was permeated by risk, with very few options for attenuating it.
Against this background of high awareness of the ubiquity of HIV in the environment, perhaps it is not surprising that participants highlighted risk-reduction practices that were at times ways to mitigate concerns about risk. Condom use was one such practice, and it seemed to matter little if this was erratic or short-lived. A Johannesburg participant, Nompumelelo, described her current partner as six years older than her, supporting her financially, and someone who drinks “a lot of alcohol”. Yet she rated him as posing only “medium” risk (‘3’) – lower than her other partners – because although he was dating another woman at the same time, he had used condoms with Nompumelelo in the first year of their three-year relationship, which she saw as a sign that he was “responsible”.
Other protective factors included HIV testing together with a partner, shorter relationship duration, and having infrequent sex in a relationship. Ntokozo (24-year old, Johannesburg) and her current partner went together to test for HIV. When their results came back negative, they decided it was safe to stop condom use. Over time, they experienced intermittent periods of arguing and breaking up, which in turn brought the spectre of HIV into the relationship.
I would say that maybe there is a risk, especially around the time where we broke up quite a bit... Ja then that’s when we use it [condom]. And a [HIV] test is a given. So, we would go for a test ‘cos I don’t know where he’s been…Like I told him that you can separate with your partner on a healthy note. But you won’t know for sure the other person’s status. That’s what I told him ‘cos I don’t know what he does when we break up.
Male youth was also considered protective, in that younger men were assumed to have less sexual experience than older men and were, therefore, less likely to be living with HIV. The experience of Rufaro (22-year old, Harare) illustrates this dynamic well. She marked off three relationships on her timeline, two of which were concurrent. These were with “time-pushers”, whom she also described as “drunkards”. Even though she had had unprotected sex with both men, Rufaro rated one a ‘5’ on the risk scale on account of him being a “womaniser” and being five years older than her, but rated the other low risk (‘1’) because she believed that at 21 years old, “…he was still young, I don’t think he has a lot that he did”.
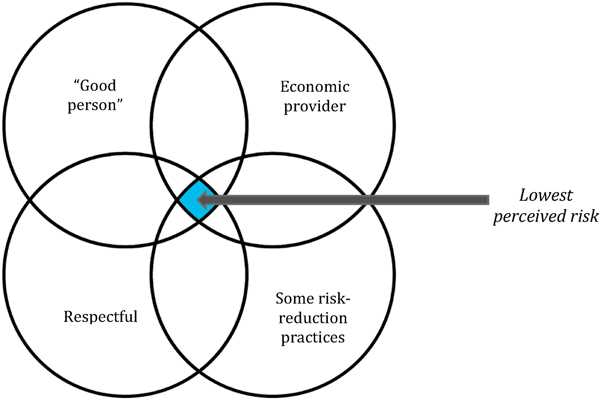
Overall, then, the foregrounding of these apparently protective features and practices, in turn, created ‘blind spots’, in which the risk potential of other behaviours could be overlooked or minimised. Figure 2 illustrates one possible way to think about such blind spots, as a nexus of lowest perceived risk where different partner characteristics and behaviours intersect.
Figure 2.
A nexus of partner and relationship characteristics considered to reduce HIV risk
In relationships with “good” partners and with whom a positive emotional connection had been established, the practice of some risk-reduction practices could make HIV risk invisible altogether. Twenty-year-old Tendai in Harare described the first man she had had sex with, at 17, as someone who had made her “feel loved” and who still made her “heart skip” when seeing him now. Condoms had been used, although sparsely, and later she discovered that he had cheated on her with other women. In the interview, Tendai reflected on the reasons why she had not felt at risk when dating him all those years ago, “… because I was so much in love with him that I did not see anything wrong with him.” This tendency to downplay obvious sources of risk, such as partner infidelity, appeared to be more common in earlier relationships when participants were younger. The risk assessment exercise became, for many participants, an opportunity to reflect on the vulnerability of their younger selves. With time and experience, their ability to discern and manage risk appeared to improve, for example through insisting on condom-use or terminating wholly unsafe relationships altogether.
“I dodged a bullet”: STIs and the embodiment of risk
At times, there were situations in which concrete, objective evidence of the proximity of HIV simply could not be ignored, such as when a partner was discovered to be actually living with HIV. Participants who recalled unprotected sex with these partners expressed some alarm at having narrowly escaped the same fate. Kabelo (23 years) narrated her experiences with several men who were active in the drug and criminal underworlds of the city; these were often violent relationships, and Kabelo had herself struggled for many years with substance abuse. When joining the study, she was in a relationship with an unemployed man who made a living from stealing electricity. She ended the relationship upon hearing from a friend that he was living with HIV. Although they had “used condoms all the time”, Kabelo reflected “…geez, he had HIV. I dodged the bullet, hey. It almost had me. Seriously.”
Also from the Johannesburg cohort, 25-year-old Palesa discovered sero-discordance in one relationship only after it had ended. In her first sexual experience at 16, a man 9 years her senior had pursued her for some time and eventually forced her to have sex with him. She remained in a relationship with him for some months afterwards, charmed by the attention he lavished on her, and the frequent declarations of love, which continued even as it became apparent that he was engaging in other relationships:
After school, I would see him with other girls, older girls. And I’m sitting there, and I’m thinking, like, ‘what about me? If he is chasing them, where does that leave me?’ …And I was so stupid, and I ended up getting an STI with him. When I discovered that I have an STI, from there, I stopped [the relationship]. I was like, at least it came early, imagine if I had stayed.
The hypothetical future with this partner (“imagine if I had stayed”) was a reference to a life that would have unfolded with HIV at its centre. For she later discovered that he had died of AIDS shortly after their relationship had come to an end. At the time, however, it was the STI diagnosis that had served as a warning of imminent HIV risk, which in turn prompted Palesa to terminate the relationship.
Infection with other STIs was in fact seen as a potential harbinger of a future HIV diagnosis in several narratives. In Cape Town, three participants recounted stories of contracting an STI and receiving treatment and a partner-referral letter from their local clinic. In all three instances, the partners were rated as ‘5’ on the risk scale, and the participants were convinced that without condoms, they would almost certainly have been infected with HIV. This experience appeared to have shaped how the women responded to threats of HIV exposure in later relationships, as they had a sharper awareness of the proximity of risk and were more willing to take steps to reduce that risk, even terminating relationships if necessary. In Johannesburg, participants spoke of how the embodied experience of having an STI had brought a new urgency to the need for self-protection. Dikeledi was diagnosed with an STI soon after entering the study. She reflected:
I have learned to listen to my body…. Eh I think it was a second week or something; I tested for an STI, right. Like, I had Chlamydia… And then that has made me, I don’t know, like I have that thing when it comes to sex, like, I’m more like no, I don’t want that [STI] inside of me because like, yoh, and I have become more observant.
Taking PrEP was her main strategy to avoid future brushes with HIV, as it was for many participants in the study. The emphasis on greater consciousness of the body’s exposure to risk was evident, too, in other women’s characterisations of PrEP-taking as a form of self-care. When asked why she had accepted PrEP in the study, for example, 19-year old Gugu from Cape Town responded, “so that I can take care of a huge part of myself, like, have the responsibility that I have to take care about my body.”
Although not as prominent as the response to STIs, unplanned pregnancies and the fear of pregnancy also featured in the risk narratives of women in Johannesburg and Cape Town. An unplanned pregnancy – a more socially desirable event than an STI – was seldom interpreted as a sign of possible exposure to HIV in a relationship, however. In the narrative of one participant, the prospect of an unplanned pregnancy with her second partner (rated a ‘2’ on the risk scale) even overshadowed awareness of HIV risk altogether. Twenty-two year old Akhona from Cape Town explained ““the risk I felt with him was that I was not on family planning, you see, and when I sleep with him without a condom I thought I would fall pregnant.” When asked whether she ever feared HIV or other STIs, she responded, simply, “I never thought of those things”.
Discussion
Our study made use of a participatory, visual storytelling approach with young women in HPTN 082, to generate rich descriptive data on sexual histories and self-perceptions of HIV risk. The approach actively involved participants in the creation of meaning in the interviews (35), facilitating detailed narratives about their relationships with men over time. The timelines they sketched served as an anchoring device that helped guide the narration of complex experiences in a coherent form, while the act of comparing risk assessments across multiple relationships threw into relief the underlying mechanics of decision-making around HIV risk.
Overall, study participants’ calibration of personal risk of HIV acquisition diverged from or had little to do with conventional public health messaging on the avoidance of HIV infection. Women’s narratives revealed a wish for a type of sexual companionship defined principally by respect, love and financial security (8), with risk scores largely reflecting this ideal. A key deciding factor in the weighing of risk was how women remembered how they had been treated by their partner in each relationship. Where the relationship overall had been a positive, affirming, or egalitarian one for women, they tended to rate their risk as low, even in the face of other signs of apparent risk, such as partner infidelity. This underestimation of risk seemed more likely when women were younger, less experienced, and possibly influenced by romantic aspirations.
Importantly, material considerations were central to the perceived morality of sexual partners. In a demonstration of the continued appeal of ‘provider masculinity’ (36), men who provided financially for women’s needs – and especially those who financed the needs of children – were generally seen as ‘good’ (less risky) partners to have. This echoes an observation previously noted in other research in the region (12), namely, that when men fulfill their expected role as economic providers, women in these settings tend to feel less vulnerable to HIV infection. Clearly, HIV risk is shaped by competing rationalities – among them, the “rationalities that influence economic survival” (37) – and not only by an individual intention or commitment to practice safe sex.
The patterns relating to idealised sexual partners illustrate how risk tends to be assessed on the basis of an ‘affect heuristic’, in which feelings are the primary basis for this judgement (21). Our study provides evidence of both rational (cognitive, analytical reasoning) and experiential (intuitive, emotion and affect) systems operating in parallel (38), but demonstrates how both are contingent upon social and structural forces that are often beyond individual control. These diverse influences on risk perception frequently produce a form of cognitive dissonance, in which, for example, women may underestimate the HIV risk of a relationship with a man who displays positive personal qualities, is respectful, and meets their emotional and financial needs, and yet overestimate the risk posed by a man simply because he lives or works far away from her. This cognitive dissonance may skew young women’s decision-making around PrEP uptake and even affect their adherence to PrEP in practice.
Among a portion of our participants, particularly in the two South African sites, the narratives contained elements of the ‘ABCs’ of safe sex that have historically dominated messaging around HIV prevention. Many women saw condom use and partner reduction as two forms of behaviour change with the potential to reduce one’s risk, even if practiced imperfectly. Overwhelmingly, partner infidelity was emphasised as a predictor of high HIV risk, which has been reported in other studies in the region (9, 19). And relationships where the male partner was substantially older, for example, were believed to bring greater risk than relationships with younger male peers.
It is significant that the experience of having an STI diagnosis or learning that a partner was living with HIV had a profound impact on participants, often moving them to decisively exit these high-risk partnerships. This suggests that in STI treatment settings the heightened awareness of HIV risk may make them opportune spaces for productive conversations about risk-reduction with young people. Even where personal risk of HIV acquisition was recognised, however, women in our study often had limited capacity to reduce their risk. As other studies have shown, socio-cultural, economic, and other structural factors created trade-offs in which managing personal risk had to be balanced against other needs, such as appeasing an aggressive partner or securing material and emotional support (8, 39, 40).
There were limitations to the study, and to the narrative timeline method described here. We asked participants to remember experiences from their first sexual relationship onwards, and our findings may have been biased by challenges around recall and social desirability. At times, participants found it difficult to delineate a clear beginning or ending to a relationship, especially in cases where they had restarted a relationship with an ex-partner or where multiple relationships overlapped in time. These patterns were a reminder of the circularity and ‘messiness’ of life, and of the limitations of using a conceptually simple timeline to organise a complex trajectory of experiences that cannot easily be presented as discrete, book-ended relationships. Furthermore, women’s own concurrent relationships were likely under-represented in the timelines, possibly because the use of a linear timeline may have inadvertently encouraged the depiction of relationships as sequential rather than concurrent, and focused attention on risk derived from partners rather than on risk associated with own behaviour. Further refinement of the method in future studies with this population might benefit from experimenting with alternative visual formats that capture AGYW’s perceptions of both external sources of risk and their own decision-making in situations of heightened HIV vulnerability.
Conclusion
For many participants in this study, the exercise of creating the timelines appeared to encourage critical reflection in a non-threatening manner, giving participants new and valuable insights into their lifetime exposure to HIV risk. Study participants recognised patterns in their sexual histories that they had not previously registered, with some even observing that the risk assessment undertaken in the timeline exercise differed from the way they had viewed their risk at the time of the relationship, when they were younger, perhaps more naïve, and still enmeshed in its emotional hold.
The narrative timeline method may lend itself to being used in risk-reduction counselling with young women to improve the accuracy of risk perceptions, and in PrEP recruitment to increase PrEP uptake in this population. Since we applied the method in a research context, our interviewers naturally refrained from using goal-directed questioning or offering advice, but in a counselling setting, there is clearly scope for the method to incorporate such elements, while remaining open-ended in orientation. Additional adaptations could involve shortening the time period to improve accuracy of recall, and using alternative, less linear visual formats.
In conclusion, our findings provide important insights for the framing and shaping of conversations around sexual risk when promoting PrEP. To enhance the success of PrEP programmes with young women, individuals need to be engaged in assessments of risk that go beyond simple constructs of risk perception that have traditionally been used in quantitative measurement surveys. In addition, more direct methods are needed to assist women in recognising when their subjective risk assumptions do not necessarily align with objectively defined risk exposures. The timeline method may ultimately help women build a habit of self-reflection about sexual risk that can potentially undergird prevention-effective adherence to PrEP – and other, emerging HIV prevention methods – in the long term.
Supplementary Material
Research Highlights.
Young women vulnerable to HIV infection may not consider themselves to be at risk
We tested a new method to explore women’s sexual histories and perceptions of HIV risk
HIV risk was often overlooked in the search for respect, love and financial security
The method may be useful in risk-reduction counselling with young women
Acknowledgements
We thank study participants for trusting us with the information presented here. We are grateful to the teams at the study sites in Johannesburg and Cape Town, South Africa, and Harare, Zimbabwe, and the HIV Prevention Trials Network that supported data collection and management for this work. We also thank Miria Chitukuta, Lumka Nobula, Sanele Gumede, Michelle Bulterys, and Nomaswazi Mthombeni, for their contributions to data collection, coding, and analysis. The HIV Prevention Trials Network is funded by the National Institute of Allergy and Infectious Diseases (UM1AI068619, UM1AI068613, UM1AI1068617), with co-funding from the National Institute of Mental Health, and the National Institute on Drug Abuse, all components of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The sponsors of this research were not involved in study design; collection, analysis and interpretation of data; writing of the article; and in the decision to submit it for publication.
Footnotes
Declarations of interest
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Koss CA, Charlebois ED, Ayieko J, et al. Uptake, engagement, and adherence to pre-exposure prophylaxis offered after population HIV testing in rural Kenya and Uganda: 72-week interim analysis of observational data from the SEARCH study. The Lancet HIV. 2020;7(4):e249–e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mugo NR, Ngure K, Kiragu M, Irungu E, Kilonzo N. The preexposure prophylaxis revolution; from clinical trials to programmatic implementation. Curr Opin HIV AIDS. 2016;11(1):80–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Namey E, Agot K, Ahmed K, et al. When and why women might suspend PrEP use according to perceived seasons of risk: implications for PrEP-specific risk-reduction counselling. Culture, health & sexuality. 2016;18(9):1081–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haberer JE, Bangsberg DR, Baeten JM, et al. Defining success with HIV preexposure prophylaxis: a prevention-effective adherence paradigm. AIDS. 2015;29(11):1277–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haberer JE, Kidoguchi L, Heffron R, et al. Alignment of adherence and risk for HIV acquisition in a demonstration project of pre-exposure prophylaxis among HIV serodiscordant couples in Kenya and Uganda: a prospective analysis of prevention-effective adherence. Journal of the International AIDS Society. 2017;20(1):21842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaefer R, Thomas R, Nyamukapa C, et al. Accuracy of HIV Risk Perception in East Zimbabwe 2003–2013. AIDS and behavior. 2019;23(8):2199–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Napper LE, Fisher DG, Reynolds GL. Development of the perceived risk of HIV scale. AIDS and behavior. 2012;16(4):1075–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warren EA, Paterson P, Schulz WS, et al. Risk perception and the influence on uptake and use of biomedical prevention interventions for HIV in sub-Saharan Africa: A systematic literature review. PloS one. 2018;13(6):e0198680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maughan-Brown B, Venkataramani AS. Accuracy and determinants of perceived HIV risk among young women in South Africa. BMC Public Health. 2017;18(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corneli AL, McKenna K, Headley J, et al. A descriptive analysis of perceptions of HIV risk and worry about acquiring HIV among FEM-PrEP participants who seroconverted in Bondo, Kenya, and Pretoria, South Africa. Journal of the International AIDS Society. 2014;17(3 Suppl 2):19152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macintyre K, Rutenberg N, Brown L, Karim A. Understanding perceptions of HIV risk among adolescents in KwaZulu-Natal. AIDS and behavior. 2004;8(3):237–50. [DOI] [PubMed] [Google Scholar]
- 12.Severy LJ, Tolley E, Woodsong C, Guest G. A framework for examining the sustained acceptability of microbicides. AIDS and behavior. 2005;9(1):121–31. [DOI] [PubMed] [Google Scholar]
- 13.Holzemer WL, Uys L, Makoae L, et al. A conceptual model of HIV/AIDS stigma from five African countries. J Adv Nurs. 2007;58(6):541–51. [DOI] [PubMed] [Google Scholar]
- 14.Linnemayr S, Stecher C. Behavioral Economics Matters for HIV Research: The Impact of Behavioral Biases on Adherence to Antiretrovirals (ARVs). AIDS and behavior. 2015;19(11):2069–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chapin J. It Won’t Happen to Me: The Role of Optimistic Bias in African American Teens’ Risky Sexual Practices. Howard Journal of Communications. 2001;12(1):49–59. [Google Scholar]
- 16.Celum C, Baeten JM. Lessons on PrEP from the SEARCH study in east Africa. The Lancet HIV. 2020;7(4):e219–e20. [DOI] [PubMed] [Google Scholar]
- 17.Khumsaen N, Stephenson R. Beliefs and Perception About HIV/AIDS, Self-Efficacy, and HIV Sexual Risk Behaviors Among Young Thai Men Who Have Sex With Men. AIDS Educ Prev. 2017;29(2):175–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bajos N. Social factors and the process of risk construction in HIV sexual transmission. AIDS care. 1997;9(2):227–37. [DOI] [PubMed] [Google Scholar]
- 19.Corneli A, Wang M, Agot K, et al. Perception of HIV risk and adherence to a daily, investigational pill for HIV prevention in FEM-PrEP. J Acquir Immune Defic Syndr. 2014;67(5):555–63. [DOI] [PubMed] [Google Scholar]
- 20.Smith KP, Watkins SC. Perceptions of risk and strategies for prevention: responses to HIV/AIDS in rural Malawi. Soc Sci Med. 2005;60(3):649–60. [DOI] [PubMed] [Google Scholar]
- 21.Hartmann M, McConnell M, Bekker LG, et al. Motivated Reasoning and HIV Risk? Views on Relationships, Trust, and Risk from Young Women in Cape Town, South Africa, and Implications for Oral PrEP. AIDS and behavior. 2018;22(11):3468–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corneli A, Field S, Namey E, et al. Preparing for the Rollout of Pre-Exposure Prophylaxis (PrEP): A Vignette Survey to Identify Intended Sexual Behaviors among Women in Kenya and South Africa if Using PrEP. PloS one. 2015;10(6):e0129177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cornwall A. Body mapping in health RRA/PRA. RRA Notes. 1992;16:69–76. [Google Scholar]
- 24.Stadler J, Dugmore C, Venables E, MacPhail C, Delany-Moretlwe S. Cognitive mapping: using local knowledge for planning health research. BMC Medical Research Methodology. 2013;13:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldenberg T, Finneran C, Andes KL, Stephenson R. Using participant-empowered visual relationship timelines in a qualitative study of sexual behaviour. Global public health. 2016;11(5–6):699–718. [DOI] [PubMed] [Google Scholar]
- 26.Celum C, Mgodi N, Bekker L-G, Hosek S, Donnell D, Anderson PL, Dye BJ, Pathak S, Agyei Y, Fogel JM, Marzinke MA, Makgamathe K, Kassim S, Mukaka S, Noble H, Adeyeye A, Delany-Moretlwe S, on behalf of the HPTN 082 Study Team, 2019. PrEP adherence and effect of drug level feedback among young African women in HPTN 082. In: Abstract TUAC0301 IAS 2019: 10th IAS Conference on HIV Science, July 21–24 2019, Mexico City (2019). Available at. http://programme.ias2019.org/Abstract/Abstract/2328. [Google Scholar]
- 27.Balkus JE, Brown E, Palanee T, et al. An Empiric HIV Risk Scoring Tool to Predict HIV-1 Acquisition in African Women. J Acquir Immune Defic Syndr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rees H, Delany-Moretlwe S, Scorgie F, Luchters S, Chersich MF. At the Heart of the Problem: Health in Johannesburg’s Inner-City. BMC Public Health. 2017;17(Suppl 3):554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luke N, Clark S, Zulu EM. The relationship history calendar: improving the scope and quality of data on youth sexual behavior. Demography. 2011;48(3):115–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kahle EM, Hughes JP, Lingappa JR, et al. An empiric risk scoring tool for identifying high-risk heterosexual HIV-1-serodiscordant couples for targeted HIV-1 prevention. J Acquir Immune Defic Syndr. 2013;62(3):339–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wand H, Reddy T, Naidoo S, et al. A Simple Risk Prediction Algorithm for HIV Transmission: Results from HIV Prevention Trials in KwaZulu Natal, South Africa (2002–2012). AIDS and behavior. 2018;22(1):325–36. [DOI] [PubMed] [Google Scholar]
- 32.Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. London: Sage; 1998. [Google Scholar]
- 33.Glaser BG Open Coding Descriptions. The Grounded Theory Review. 2016;15(2):108–10. [Google Scholar]
- 34.Moodley P, Ebrahim S. #Blesser: A critical evaluation of conceptual antecedents and the allure of a transactional relationship. Acta Academica. 2019;51(2):21–40. [Google Scholar]
- 35.Holstein J, Gubrium JF. The active interview. Thousand Oaks, CA: SAGE Publications; 1995. [Google Scholar]
- 36.Bhana D, Pattman R. Girls want money, boys want virgins: the materiality of love amongst South African township youth in the context of HIV and AIDS. Culture, health & sexuality. 2011;13(8):961–72. [DOI] [PubMed] [Google Scholar]
- 37.Tenkorang EY, Rajulton F, Maticka-Tyndale E. Perceived risks of HIV/AIDS and first sexual intercourse among youth in Cape Town, South Africa. AIDS and behavior. 2009;13(2):234–45. [DOI] [PubMed] [Google Scholar]
- 38.Slovic P, Finucane ML, Peters E, DG M. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Anal. 2004;24(2):311–22. [DOI] [PubMed] [Google Scholar]
- 39.Tenkorang EY, Maticka-Tyndale E, Rajulton F. A multi-level analysis of risk perception, poverty and sexual risk-taking among young people in Cape Town, South Africa. Health Place. 2011;17(2):525–35. [DOI] [PubMed] [Google Scholar]
- 40.Aggleton P, O’Reilly K, Slutkin G, Davies P. Risking everything? Risk behavior, behavior change, and AIDS. Science. 1994;265(5170):341–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.