ABSTRACT
Background
Data from the NHANES indicate that BMI has increased in some subgroups of children and adolescents in the United States over the past 20 y; however, BMI is an indirect measure of body fatness.
Objectives
We assessed changes in DXA-derived measures of adiposity in a nationally representative population of US children and adolescents aged 8–19 y from 1999–2006 to 2011–2018.
Methods
Using data from the NHANES, we compared the means and distributions of DXA-derived percentage body fat (%BF) and fat mass index (FMI; fat mass/height2 in kg/m2) between 1999–2006 (n = 10,231) and 2011–2018 (n = 6923) among males and females by age group, race and Hispanic origin, and BMI categories. Estimates were standardized by age and race and Hispanic origin.
Results
From 1999–2006 to 2011–2018, mean %BF increased from 25.6% to 26.3% (change in %BF: 0.7%; 95% CI: 0.2%, 1.2%; P < 0.01) among all males, whereas mean %BF increased from 33.0% to 33.7% (change in %BF: 0.7%; 95% CI: 0.2%, 1.2%; P = 0.01) and mean FMI increased from 7.7 to 8.0 fat mass kg/m2 (change in FMI: 0.3 fat mass kg/m2; 95% CI: 0.0, 0.6 fat mass kg/m2; P = 0.02) among all females. Changes were not consistent across all age, race and Hispanic origin, and BMI categories. Both %BF and FMI increased among Mexican-American children and adolescents, but not other race and Hispanic origin groups.
Conclusions
Among US children and adolescents, DXA-derived measures of adiposity increased from 1999–2006 to 2011–2018, albeit not consistently in every age, race and Hispanic origin, and BMI subgroup. These data reinforce the need to consider other measures, besides BMI categories, when studying adiposity in children and adolescents.
Keywords: US children and adolescents, adiposity, body fatness, percentage body fat, fat mass index, DXA, dual-energy X-ray absorptiometry, NHANES
See corresponding editorial on page 1275.
Introduction
Obesity among children and adolescents in the United States aged 2–19 y is defined by the CDC, based on expert committee recommendations, as a BMI (in kg/m2) ≥95th percentile of the 2000 CDC growth charts (1, 2). Obesity is prevalent among children and adolescents in the United States, affecting 19.3% of those aged 2–19 y in 2017–2018, an increase from 13.9% in 1999–2000 (3). Childhood obesity is associated with immediate health risks, including insulin resistance, cardiovascular disease risk factors, and sleep apnea, among others (4, 5). Children with obesity are also at risk of continued obesity as adults and consequent associated health risks (6, 7).
BMI is used as a noninvasive proxy measure of adiposity, utilizing weight relative to the square of height. However, because BMI is an indirect measure of adiposity not reflective of the distribution of fat and unable to distinguish between lean mass and fat mass, it is imperfect. Although children with obesity as defined by BMI generally have excess body fat, BMI is a poor estimator of percentage body fat (%BF) in children with lower BMI (8–11). Although some studies show that BMI and %BF have similar associations with cardiovascular disease risk factors, there is also some evidence that %BF may be associated with cardiovascular disease risk factors in children independently from BMI (12–14). In addition, there are differences in %BF by self-reported race and Hispanic origin groups within the same BMI category (15).
Several measures have been used to assess adiposity more directly, including %BF and fat mass index (FMI). FMI is calculated as fat mass divided by height-squared (fat mass kg/m2) (16). %BF gauges fat mass relative to total body mass. The FMI provides useful adjunctive information to %BF by giving an absolute measure of adiposity (16). Differences in FMI among individuals reflect differences in absolute fat mass, whereas differences in %BF among individuals could be due to differences in fat mass, lean mass, or both (16). DXA can assess total-body fat mass from which %BF and FMI can be calculated.
To assess changes in body composition over time, we compared DXA-derived %BF and FMI between 1999–2006 and 2011–2018 in children and adolescents aged 8–19 y, examining %BF and FMI in the entire group as well as according to sex, age, race and Hispanic origin, and by BMI categories, using data from the NHANES.
Methods
The NHANES is a nationally representative, cross-sectional survey designed to monitor the health and nutrition of the civilian, noninstitutionalized, resident US population (17). DXA examinations were included in the NHANES in 1999–2006 and again in 2011–2018. To improve the sample size in this analysis, data were combined from 1999–2006 and compared with data combined from 2011–2018. The NHANES was approved by the National Center for Health Statistics Research Ethics Review Board and signed consent from parents/guardians or participants aged ≥18 y, as well as assent from minor participants, were obtained. Demographic information was obtained during an in-home interview. Participants aged ≥16 y and emancipated minors were interviewed directly. An adult proxy provided information for participants aged <16 y. Measurements of weight, height, and total body fat from DXA scans were obtained in a mobile examination center (MEC). Unweighted NHANES examination response rates for children and adolescents aged 6–19 y during the NHANES cycles ranged from as low as 54.3% in 2017–2018 to as high as 86.1% in 2001–2002.
Examination methods
Standardized procedures were used to obtain weight and height to calculate BMI (17). Sex-specific BMI-for-age percentile values were calculated according to the 2000 CDC growth charts (18).
During 1999–2006, whole-body DXA scans were acquired with a Hologic QDR-4500A fan-beam densitometer (Hologic, Inc.). Each scan was reviewed and analyzed by the University of California, San Francisco, Department of Radiology using Hologic Discovery software, version 12.1 (1999–2004) or version 12.4 (2005–2006). The lean soft tissue mass was decreased by 5% and an equivalent kilogram weight of fat mass was added, maintaining the same total body mass, based on an analysis from 7 research laboratories that found the QDR-4500A algorithm underestimated fat mass and overestimated lean mass (19). DXA data available in the publicly released data sets for 1999–2006 that were used in this analysis included imputed data, using multiple imputation, for missing DXA values (19). Imputation was performed because of the high percentage of missing values and the missing data were related to age, BMI, weight, height, and possibly other characteristics (20). Part of this missingness is explained by weight and height limits of the DXA table, requiring exclusion of those with a self-reported weight >300 pounds (>136.1 kg) or height >6′5″ (>1.96 m). There was less missing information among children and adolescents than among adults. Other reasons for missingness included nonremovable objects, noise, arm/leg overlap, body parts out of the scan region, positioning problems, motion, missing limbs, and unknown artifacts, or forms of nonparticipation such as insufficient time to complete the examination, the pregnancy test not being completed, participant refusal, and other medical concerns. For those with any missing data, data were imputed. Of those children and adolescents included in this study from 1999–2006, 11.5% had imputed DXA data. Briefly, the multiple imputation procedures used sequential regression multivariate imputation and were constructed from both available DXA variables and non-DXA variables, such as demographic characteristics and body measurements (19). Further information on the DXA data, multiple imputation procedures, and evaluation of the imputed values is included in documentation for the data files (19, 20).
During 2011–2018, whole-body DXA scans were acquired with Hologic Discovery A densitometers (Hologic, Inc.). Each scan was reviewed and analyzed by the University of California, San Francisco, Department of Radiology using Hologic APEX version 4.0 software with the NHANES Body Composition Analysis option. The NHANES Body Composition Analysis option was added in 2011 and utilizes the same correction factor as in 1999–2006, subtracting 5% of lean mass and adding this to the fat mass, to correct for underestimated fat mass and overestimated lean mass. No publicly released DXA data from 2011–2018 were imputed given there was less concern about missingness related to age, BMI, and other characteristics. The weight limit for the Hologic Discovery model A densitometer table (450 pounds; 204 kg) used in 2011–2018 was higher than for the Hologic QDR fan-beam densitometer used in 1999–2006 as explained in the accompanying technical documentation released along with the data files (21, 22). During 2011–2018, 16.3% of children and adolescents were missing DXA data; however, sex-specific distributions of age group, race and Hispanic origin, and BMI category were not meaningfully different among all participants and those with DXA data available. Missing data can be related to invalid scans due to the presence of removable or nonremovable objects, noise, arm/leg overlap, body parts out of the scan region, positioning problems, motion, missing limbs, unknown artifacts, or other issues or due to forms of nonparticipation such as insufficient time to complete the examination, the pregnancy test not being completed, participant refusal, and other medical concerns. Those with any missing data during 2011–2018 did not have total-body adiposity measures calculated and were excluded.
%BF was calculated as the DXA-derived fat mass divided by the DXA-derived total body mass. FMI was calculated as the DXA-derived fat mass (kg) divided by height (m) squared.
Definitions
Age was calculated in months at the time of examination. Age categories were defined as 8–11 y, 12–15 y, and 16–19 y. Race and Hispanic origin were separately self-identified by participants. Race and Hispanic origin responses were combined into categories, as provided in NHANES public-use files: 1) Mexican-American, 2) other Hispanic origin, 3) non-Hispanic white, 4) non-Hispanic black, and 5) other non-Hispanic race including non-Hispanic multiracial (23). Persons reporting other Hispanic origin or other non-Hispanic race were included for the total estimates but not shown separately. Sex-specific BMI-for-age was divided into 3 categories: <85th percentile, 85th to <95th percentile, and ≥95th percentile.
Statistical analyses
Analyses were performed using R version 3.6.0 (R Foundation for Statistical Computing), including the R survey package (24). All analyses used examination sample weights, encompassing those who participated in an examination in the MEC. Weighting procedures reflected the survey's complex, multistage probability design and accounted for the differential probabilities of selection, nonresponse, and noncoverage. The use of weights allows for the production of estimates of statistics reflective of the civilian, noninstitutionalized, resident US population (23). Variances were calculated using Taylor series linearization (23). The 1999–2006 study population was standardized to the 2011–2018 study population by sex-specific race and Hispanic origin, and 6-mo age interval, in order to control for changes in these demographic characteristics when comparing body composition between these 2 periods. Crude (unstandardized) estimates are also presented in the supplementary data.
Given some data were imputed for 1999–2006, effect estimates and SEs were initially obtained separately for each imputed data set. Calculated effect estimates for %BF and FMI included means and mean differences between 1999–2006 and 2011–2018. These means and mean differences were averaged across imputations. SEs were pooled across imputations using within-imputation and between-imputation variances as proposed by Rubin and Schenker (25).
Significance testing was performed by comparing mean differences to a null hypothesis of 0 (no change) using a t-distribution with adjusted df calculated as suggested by Barnard and Rubin (26). Similar to the approach of Flegal and Troiano, changes to the distribution of %BF and FMI between 1999–2006 and 2011–2018 were explored visually using Tukey mean-difference plots (27). To create these plots, weighted quantiles of %BF and FMI were calculated at even quantile values (2nd, 4th, 6th, etc., up to the 98th percentile) for each imputed data set and then combined by averaging across the imputed data sets. Each data point on the mean-difference plots represents a separate quantile. To obtain the x-axis values, the %BF or FMI for each quantile was averaged across 1999–2006 and 2011–2018. Y-axis values were calculated by subtracting the %BF or FMI in 1999–2006 from 2011–2018 for each quantile. The resulting plots give a graphical representation of how the distributions changed over time.
Analytic sample
Children and adolescents aged 8–19 y who participated in the NHANES in 1999–2006 or 2011–2018 and had DXA, BMI, and age at examination data available were included in the analysis (Supplemental Figure 1). Given important known differences in body composition by sex in children and adolescents, such as higher %BF in females than in males and differential changes in body fat during adolescence (28), results are presented separately for males and females. Pregnant females did not have DXA examinations and were excluded from this analysis. In 1999, females aged 8–17 y did not have Ethics Review Board approval for DXA examinations, so all data were imputed and combined with data from females in 2000 in a restricted-use data set. Given the high percentage of imputed data, females in 1999–2000 (n = 1427) were excluded from the main analysis. An exploratory analysis including these data was performed and reported separately within the results. In 1999–2006, a total of 10,427 children and adolescents aged 8–19 y (excluding females from 1999–2000 and pregnant females) were examined in the MEC among whom 10,231 had both BMI and DXA data available (98.1%) and were included in this analysis. Data from 1999–2006 are available in imputed data sets, and a total of 1178 participants of these 10,231 participants (11.5%) in the included sample had at least some missing DXA data that required imputation (19). Adiposity estimates from the data during 1999–2004 have previously been reported along with a description of the imputation process (15, 19, 28). In 2011–2018, a total of 8289 children and adolescents aged 8–19 y were examined in the MEC among whom 6923 (83.5%) had both BMI and DXA data available and were not pregnant. Exclusion of children and adolescents with missing BMI and DXA data did not significantly change the sex-specific weighted distributions of age, race and Hispanic origin, or BMI category.
Results
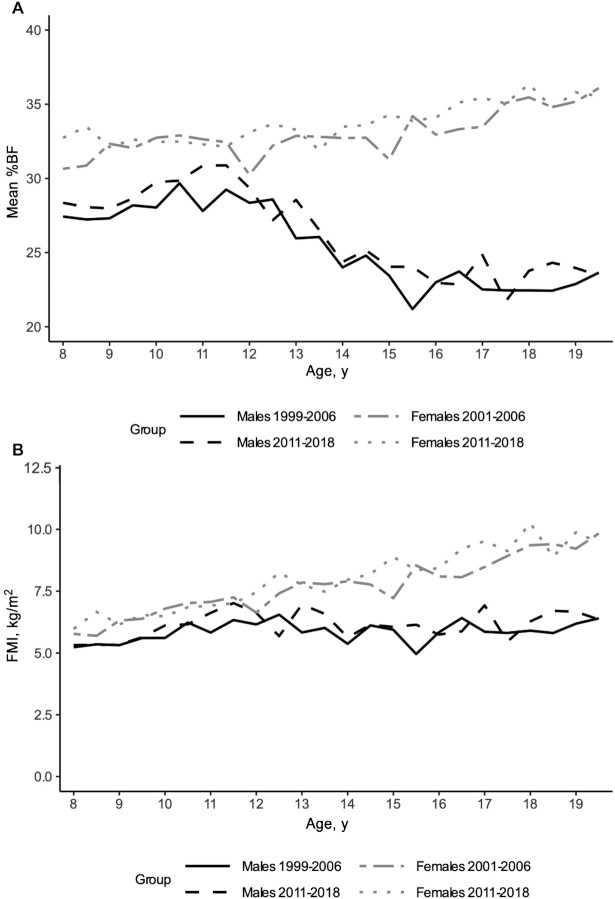
Table 1 reports sample sizes and weighted percentages of age, race and Hispanic origin, and BMI status groups by sex and survey period. In both 1999–2006 and 2011–2018, %BF appeared higher among females than among males, and sex-specific differences in mean %BF appeared larger starting above approximately age 12 y (Figure 1A). FMI appeared higher in females than in males in both 1999–2006 and 2011–2018 and, as seen with %BF, sex-specific differences were larger above approximately age 12 y (Figure 1B).
TABLE 1.
Unweighted sample sizes and weighted percentages of the total among children and adolescents aged 8–19 y by sex, survey years, age group, race and Hispanic origin, and BMI category—United States, 1999–2006 and 2011–20181
| Males | Females | |||
|---|---|---|---|---|
| 1999–2006 | 2011–2018 | 2001–2006 | 2011–2018 | |
| All | 5933 | 3584 | 4298 | 3339 |
| Age group, y | ||||
| 8–11 | 1389 (32.6) | 1387 (32.7) | 1089 (32.7) | 1347 (34.0) |
| 12–15 | 2234 (34.4) | 1164 (35.1) | 1694 (34.6) | 998 (33.5) |
| 16–19 | 2310 (33.1) | 1033 (32.3) | 1515 (32.6) | 994 (32.5) |
| Race and Hispanic origin group2 | ||||
| Non-Hispanic white | 1525 (61.1) | 987 (52.9) | 1191 (62.1) | 880 (54.3) |
| Non-Hispanic black | 1952 (14.7) | 897 (13.7) | 1392 (14.7) | 788 (12.8) |
| Mexican-American | 2004 (11.7) | 717 (15.6) | 1372 (10.9) | 745 (15.5) |
| BMI category | ||||
| <85th percentile | 3800 (66.1) | 2223 (63.7) | 2699 (66.6) | 2049 (63.1) |
| 85th–<95th percentile | 925 (15.9) | 582 (16.0) | 729 (16.6) | 603 (17.5) |
| ≥95th percentile | 1208 (18.0) | 779 (20.3) | 870 (16.8) | 687 (19.3) |
Values are unweighted sample sizes (weighted percentages of the total). For the 1999–2006 time period, female data include only 2001–2006. Source: National Center for Health Statistics, NHANES.
Those with race and Hispanic origin defined as “other” were included in the total estimates but are not reported separately here.
FIGURE 1.
Crude means of adiposity measures by sex, survey years, and 6-mo age intervals—United States, 1999–2006 and 2011–2018. (A) Mean %BF, (B) mean FMI. Estimates were calculated using examination sample weights and accounted for the survey's complex, multistage probability design. For 1999–2006, imputed data were included; means were averaged across imputations. Overall sample sizes: males during 1999–2006, n = 5933; males during 2011–2018, n = 3584; females during 2001–2006, n = 4298; females during 2011–2018, n = 3339. Source: National Center for Health Statistics, NHANES. For the 1999–2006 time period, female data include only 2001–2006. FMI, fat mass index; %BF, percentage body fat.
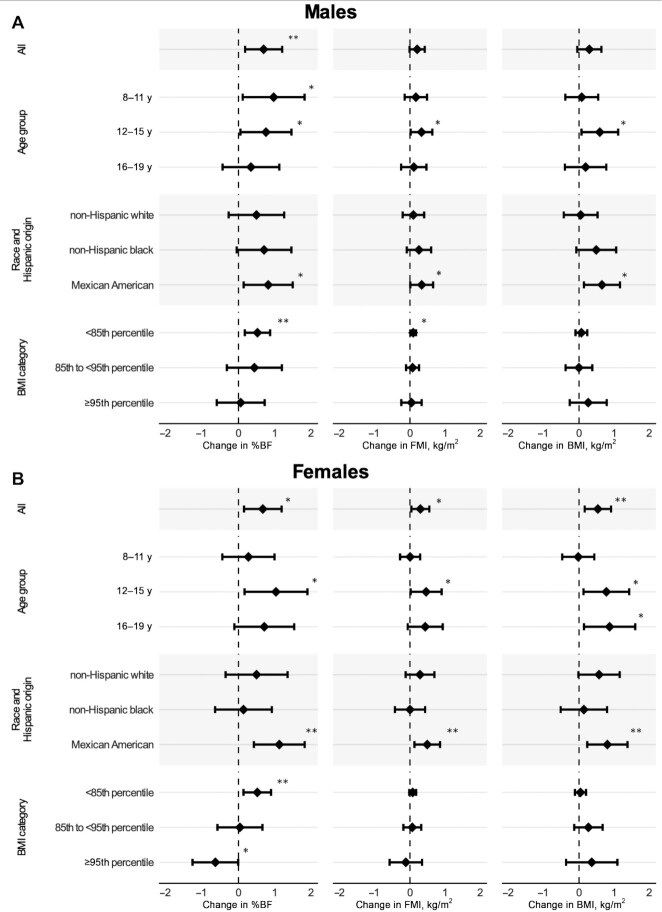
Table 2 shows mean %BF, FMI, and BMI during 1999–2006 (standardized to 2011–2018) and 2011–2018 (crude) by age group, race and Hispanic origin, and BMI categories. Crude values for 1999–2006 were generally similar to standardized values for 1999–2006 (Supplemental Table 1). Figure 2 shows the change in these values over time (underlying values shown in Supplemental Table 2). Among all males, mean %BF increased, from 25.6% to 26.3% (change in %BF: 0.7%; 95% CI: 0.2, 1.2%; P < 0.01), but mean FMI and BMI did not. Among all females, increases were seen in mean %BF from 33.0% to 33.7% (change in %BF: 0.7%; 95% CI: 0.2%, 1.2%; P = 0.01), FMI from 7.7 to 8.0 kg/m2 (change in FMI: 0.3 kg/m2; 95% CI: 0.0, 0.6 kg/m2; P = 0.02), and BMI from 22.1 to 22.6 (change in BMI: 0.5; 95% CI: 0.2, 0.9; P < 0.01).
TABLE 2.
Mean %BF, mean FMI, and mean BMI among male and female adolescents aged 8–19 y by survey years, age group, race and Hispanic origin, and BMI category—United States, 1999–2006 and 2011–20181
| %BF | FMI, kg/m2 | BMI, kg/m2 | ||||
|---|---|---|---|---|---|---|
| 1999–20062 | 2011–20183 | 1999–20062 | 2011–20183 | 1999–20062 | 2011–20183 | |
| Males4 | ||||||
| All | 25.6 (25.2, 26.0) | 26.3 (25.9, 26.7) | 5.9 (5.8, 6.1) | 6.1 (5.9, 6.3) | 21.8 (21.6, 22.1) | 22.1 (21.8, 22.4) |
| Age group, y | ||||||
| 8–11 | 28.3 (27.6, 28.9) | 29.2 (28.6, 29.8) | 5.7 (5.5, 6.0) | 5.9 (5.7, 6.1) | 19.1 (18.7, 19.4) | 19.2 (18.8, 19.5) |
| 12–15 | 25.5 (25.0, 25.9) | 26.2 (25.6, 26.8) | 5.9 (5.7, 6.1) | 6.2 (6.0, 6.5) | 21.8 (21.5, 22.1) | 22.4 (22.0, 22.8) |
| 16–19 | 23.0 (22.6, 23.5) | 23.4 (22.8, 24.0) | 6.1 (5.9, 6.3) | 6.2 (5.9, 6.5) | 24.6 (24.2, 25.0) | 24.8 (24.4, 25.3) |
| Race and Hispanic origin group | ||||||
| Non-Hispanic white | 25.5 (24.9, 26.0) | 26.0 (25.4, 26.5) | 5.8 (5.6, 6.0) | 5.9 (5.6, 6.1) | 21.5 (21.2, 21.9) | 21.6 (21.2, 22.0) |
| Non-Hispanic black | 23.2 (22.7, 23.6) | 23.9 (23.2, 24.6) | 5.5 (5.3, 5.7) | 5.8 (5.5, 6.1) | 22.1 (21.9, 22.4) | 22.6 (22.1, 23.2) |
| Mexican-American | 27.7 (27.3, 28.1) | 28.5 (27.9, 29.2) | 6.7 (6.5, 6.9) | 7.0 (6.7, 7.3) | 22.8 (22.5, 23.1) | 23.5 (22.9, 24.0) |
| BMI category | ||||||
| <85th percentile | 21.4 (21.2, 21.7) | 22.0 (21.7, 22.2) | 4.1 (4.1, 4.2) | 4.2 (4.1, 4.3) | 19.0 (18.9, 19.1) | 19.1 (18.9, 19.3) |
| 85th–<95th percentile | 29.8 (29.3, 30.2) | 30.2 (29.6, 30.8) | 7.1 (7.0, 7.3) | 7.2 (7.0, 7.4) | 23.9 (23.6, 24.1) | 23.9 (23.5, 24.2) |
| ≥95th percentile | 36.7 (36.3, 37.2) | 36.8 (36.3, 37.3) | 11.2 (11.0, 11.4) | 11.2 (11.0, 11.5) | 30.0 (29.7, 30.4) | 30.3 (29.9, 30.7) |
| Females5 | ||||||
| All | 33.0 (32.7, 33.4) | 33.7 (33.3, 34.1) | 7.7 (7.5, 7.8) | 8.0 (7.8, 8.2) | 22.1 (21.8, 22.3) | 22.6 (22.3, 22.9) |
| Age group, y | ||||||
| 8–11 | 32.2 (31.7, 32.8) | 32.5 (32.0, 33.0) | 6.6 (6.4, 6.8) | 6.6 (6.4, 6.8) | 19.5 (19.2, 19.9) | 19.5 (19.2, 19.8) |
| 12–15 | 32.4 (31.9, 33.0) | 33.5 (32.8, 34.2) | 7.6 (7.4, 7.9) | 8.1 (7.7, 8.5) | 22.4 (22.0, 22.7) | 23.2 (22.6, 23.7) |
| 16–19 | 34.5 (34.0, 35.0) | 35.2 (34.5, 35.9) | 8.9 (8.5, 9.2) | 9.3 (8.9, 9.7) | 24.4 (24.0, 24.9) | 25.3 (24.7, 25.9) |
| Race and Hispanic origin group | ||||||
| Non-Hispanic white | 32.6 (32.1, 33.2) | 33.1 (32.5, 33.8) | 7.4 (7.2, 7.7) | 7.7 (7.4, 8.1) | 21.7 (21.3, 22.1) | 22.3 (21.8, 22.8) |
| Non-Hispanic black | 32.6 (32.2, 33.0) | 32.7 (32.0, 33.4) | 8.3 (8.1, 8.5) | 8.3 (7.9, 8.7) | 23.8 (23.4, 24.1) | 23.9 (23.2, 24.6) |
| Mexican-American | 34.8 (34.3, 35.3) | 35.9 (35.4, 36.4) | 8.2 (8.0, 8.5) | 8.7 (8.4, 9.0) | 22.5 (22.1, 22.9) | 23.3 (22.8, 23.9) |
| BMI category | ||||||
| <85th percentile | 29.5 (29.3, 29.8) | 30.1 (29.7, 30.4) | 5.8 (5.7, 5.9) | 5.9 (5.8, 6.0) | 19.2 (19.1, 19.4) | 19.3 (19.1, 19.4) |
| 85th–<95th percentile | 37.2 (36.7, 37.6) | 37.2 (36.8, 37.7) | 9.2 (9.0, 9.4) | 9.3 (9.1, 9.5) | 24.5 (24.2, 24.8) | 24.7 (24.4, 25.0) |
| ≥95th percentile | 43.0 (42.6, 43.5) | 42.4 (41.9, 42.8) | 13.7 (13.3, 14.0) | 13.6 (13.2, 13.9) | 31.2 (30.7, 31.8) | 31.6 (31.0, 32.1) |
Values are means (95% CIs). Estimates were calculated using examination sample weights and accounted for the survey's complex, multistage probability design. Variances used to compute 95% CIs were calculated using Taylor series linearization. For 1999–2006, imputed data were included; means were averaged across imputations and SEs were pooled across imputations using within-imputation and between-imputation variances. Source: National Center for Health Statistics, NHANES. FMI, fat mass index; %BF, percentage body fat.
For the 1999–2006 time period, female data include only 2001–2006. Data for 1999–2006 (2001–2006 in females) are standardized to the sex-specific, race and Hispanic origin–specific, and 6-mo age–specific distributions of 2011–2018 to allow for comparison across time frames.
Data for 2011–2018 are crude values.
Overall sample size for males for 1999–2006: n = 5933. Overall sample size for males for 2011–2018: n = 3584.
Overall sample size for females for 2001–2006: n = 4298. Overall sample size for females for 2011–2018: n = 3339.
FIGURE 2.
Change in mean %BF, mean FMI, and mean BMI among children and adolescents aged 8–19 y from 1999–2006 to 2011–2018 by age group, race and Hispanic origin, and BMI category—United States. (A) Among males, (B) among females. Estimates were calculated using examination sample weights and accounted for the survey's complex, multistage probability design. Mean differences were averaged across imputations. SEs were pooled across imputations using within-imputation and between-imputation variances. Significance testing was performed using a t-distribution with adjusted df. 95% CIs are provided. Overall sample sizes: males during 1999–2006, n = 5933; males during 2011–2018, n = 3584; females during 2001–2006, n = 4298; females during 2011–2018, n = 3339. Source: National Center for Health Statistics, NHANES. For the 1999–2006 time period, female data include only 2001–2006. Data for 1999–2006 (2001–2006 in females) are standardized to the sex-specific, race and Hispanic origin–specific, and 6-mo age–specific distributions of 2011–2018 to allow for comparison across time frames. *,**Significant change: *P < 0.05; **P < 0.01. FMI, fat mass index; %BF, percentage body fat.
Among males aged 8–11 y, there was a significant increase in mean %BF (28.3% to 29.2%; P = 0.03) but not in mean FMI or BMI. Significant increases among males aged 12–15 y occurred in mean %BF (25.5% to 26.2%; P = 0.04), FMI (5.9 to 6.2 kg/m2; P = 0.04), and BMI (21.8 to 22.4; P = 0.03). Among Mexican-American males, mean %BF (27.7% to 28.5%; P = 0.02), FMI (6.7 to 7.0 kg/m2; P = 0.04), and BMI (22.8 to 23.5, P = 0.01) increased. Increases in mean %BF (23.2% to 23.9%), FMI (5.5 to 5.8 kg/m2), and BMI (22.1 to 22.6) among non-Hispanic black males were similar in magnitude to those among Mexican-American males but were not significant. Among males with BMI <85th percentile, mean %BF (21.4% to 22.0%; P < 0.01) and FMI (4.1 to 4.2 kg/m2; P = 0.03) increased but not mean BMI.
Among females aged 12–15 y, mean %BF (32.4% to 33.5%; P = 0.02), FMI (7.6 to 8.1 kg/m2; P = 0.04), and BMI (22.4 to 23.2; P = 0.02) increased. Mean BMI increased among females aged 16–19 y (24.4 to 25.3; P = 0.02), but not mean %BF or FMI. Among Mexican-American females, mean %BF (34.8% to 35.9%; P < 0.01), FMI (8.2 to 8.7 kg/m2; P < 0.01), and BMI (22.5 to 23.3; P < 0.01) increased. Mean %BF increased among females with BMI <85th percentile (29.5% to 30.1%; P < 0.01) and decreased among females with BMI ≥ 95th percentile (43.0% to 42.4%; P < 0.05), whereas mean FMI and BMI remained stable among these groups.
In exploratory analyses including data from females in 1999–2000, FMI did not significantly increase among females aged 12–15 y and BMI significantly increased among non-Hispanic white females. Other significant findings remained similar to the analyses without females from 1999–2000.
As shown in the mean-difference plot in Figure 3A, differences in %BF and FMI from 1999–2006 to 2011–2018 among all males were not consistent throughout their distributions. Although increases in %BF and FMI over time were seen across most of the distributions, these increases were generally largest between the 50th and 90th percentiles. Changes in %BF and FMI differed above the 90th percentile. Patterns within age groups and race and Hispanic origin groups were generally similar to those for all males, except for changes seen in FMI above the 90th percentile which varied across subgroups (Supplemental Figures 2, 3). As with males, differences from 2001–2006 to 2011–2018 in %BF and FMI among females did not appear consistent throughout their distributions, with differences in changes in %BF and FMI most apparent above the 90th percentile (Figure 3B). Increases in %BF over time were highest between the 30th and 50th percentiles and decreases in %BF over time were observed above the 90th percentile. Increases in FMI over time generally increased with increasing quantiles. Patterns within age groups and race and Hispanic origin groups were variable (Supplemental Figures 4, 5). Of note, %BF decreased over time above the 90th percentile in all groups except females aged 8–11 y.
FIGURE 3.
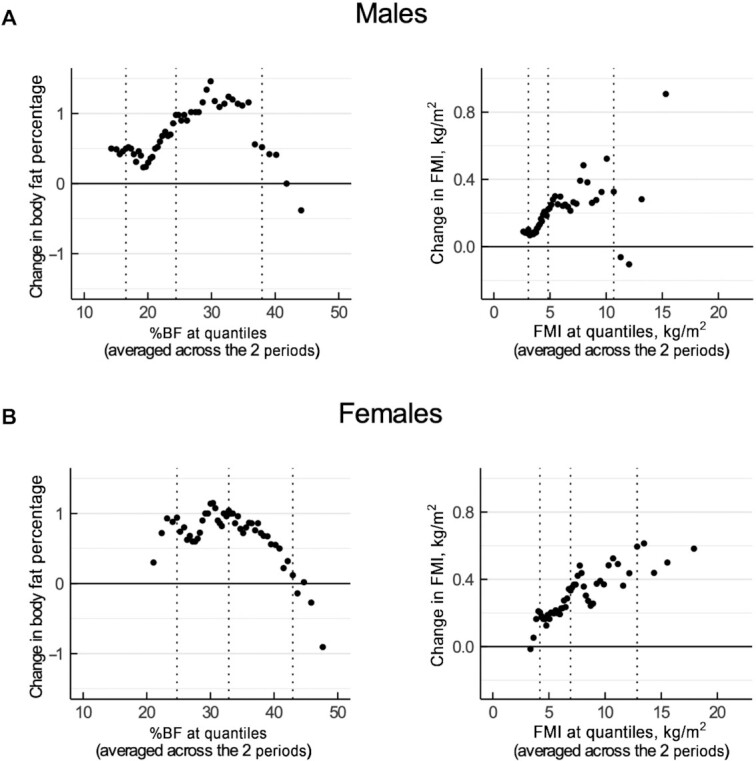
Mean-difference plots for the differences in distribution of %BF and FMI among children and adolescents aged 8–19 y between 1999–2006 and 2011–2018—United States. (A) Among males, (B) among females. Plots show the difference for each quantile across time periods compared with the average of each quantile across time periods. For 1999–2006, imputed data were included; quantiles were averaged across imputations. Estimates were calculated using examination sample weights and accounted for the survey's complex, multistage probability design. The 10th, 50th, and 90th percentiles are marked by dotted lines. Overall sample sizes: males during 1999–2006, n = 5933; males during 2011–2018, n = 3584; females during 2001–2006, n = 4298; females during 2011–2018, n = 3339. Source: National Center for Health Statistics, NHANES. For the 1999–2006 time period, female data include only 2001–2006. Data for 1999–2006 (2001–2006 in females) are standardized to the sex-specific, race and Hispanic origin–specific, and 6-mo age–specific distributions of 2011–2018 to allow for comparison across time frames. FMI, fat mass index; %BF, percentage body fat.
Discussion
To our knowledge, this is the first study to report how direct measures of adiposity have changed over time in a nationally representative sample of US children and adolescents. Recent estimates from 1999–2000 to 2017–2018 showed increases in obesity in US children aged 6–11 y and aged 12–19 y (29). In this study, mean %BF increased among male and mean %BF and FMI increased among female children and adolescents aged 8–19 y from 1999–2006 to 2011–2018. Across most age, race and Hispanic origin, and BMI subgroups, changes in %BF and FMI were in the direction of increase. Although changes were generally small and statistically significant among only some subgroups, small changes can have an important impact on population health.
Studies that look exclusively at changes in BMI and obesity prevalence over time do not account for the potential for changes in adiposity independent of BMI. In this study, we found that changes in mean %BF and FMI differed by BMI category and were not always consistent with changes in mean BMI. Significant increases in %BF were seen in males and females with BMI <85th percentile. FMI increased significantly in females with BMI <85th percentile. Conversely, %BF decreased significantly in females with BMI ≥95th percentile. Given this decrease in %BF was not accompanied by a significant decrease in FMI, increases in other components of total body mass (i.e., lean mass index) likely contributed to the change. In addition, changes in %BF were not equal across quantiles, with the greatest increases generally closest to the middle of the distribution. This suggests that there are changes to adiposity in children and adolescents over time not captured by cutoffs in BMI or adiposity alone, such as standard BMI categories. Such variable changes across the whole distribution may have important implications for population health. For instance, several studies have found that among adults with normal weight, higher %BF is associated with increased risk of cardiometabolic disease, suggesting that BMI categories alone can miss important information about body composition that influences disease risk (30–32). Less is known about such findings in children and adolescents. One study showed significant differences in visceral fat, trunk fat, and waist circumference, but not %BF, in metabolically unhealthy compared with metabolically healthy adolescents with obesity (33).
The largest and statistically significant increases in mean %BF and mean FMI among age groups in males and females were for those aged 12–15 y. %BF also significantly increased in males aged 8–11 y. The 12- to 15-y age group is notable for generally having the most overlap with the ages of puberty (34). As seen in Figure 1 as well as prior studies, body composition notably changes during puberty, with males often reducing or stabilizing body fat during mid-puberty and females continuing to accrue adiposity steadily throughout puberty (28, 35, 36). In addition, some evidence indicates that obesity may be causally related to earlier onset of thelarche in girls (37, 38). A decrease in the age of onset of puberty since the early 1900s has been noted in both males and females with changes in the early to mid-1900s presumed to be attributable largely to better nutrition that would be expected to manifest as changes in body composition within the population over time (39, 40). If there were any changes in the age of puberty from 1999–2006 to 2011–2018, this may explain some of the increases in %BF and mean FMI in females. One study showed that the proportion of women aged 15–44 y who reported having reached menarche between ages 8 and 12 y increased from 1995 to 2013–2017, providing evidence that this may be a possible explanation (41).
Mexican-American males and females had the largest increase in mean %BF and FMI among the race and Hispanic origin groups analyzed. This is consistent with changes among children and adolescents in the United States by race and Hispanic origin in previously reported obesity estimates from 1999–2000 to 2017–2018 (29) as well as mean BMI from 1999–2006 to 2011–2018 in this study. Disparities in the prevalence of overweight/obesity have increased over time among foreign-born Mexican-American children and have remained elevated among US-born Mexican-American children compared with non-Hispanic white children (42). Increases in mean %BF and FMI among non-Hispanic black males were similar to those seen in Mexican-American males, although they were not statistically significant. In contrast, there were no changes in mean %BF and FMI among non-Hispanic black females. A previous study showed an increase in obesity prevalence among combined male and female non-Hispanic black children and adolescents aged 12–19 y from 1999–2000 to 2017–2018 (29).
Significant changes in %BF were not always accompanied by changes in FMI, which suggests that differences in the fat-free mass index (FFMI) contributed, in part, to changes in %BF. Fat-free mass consists of appendicular muscle mass, internal organ mass, and bone mineral content. Changes to FFMI over time could reflect any of these components. Lean body mass may be associated with cardiometabolic risk factors independently from fat mass in children and adolescents (43), suggesting changes to FMI and FFMI may both be important considerations for population health. There are significant race- and sex-specific differences in FFMI that may potentially affect the relations of such risk factors to FFMI (44).
The effect of these changes in adiposity on health outcomes at the population level are unclear. In contrast to these small increases in adiposity measures, 1 study showed a decrease in the prevalence of dyslipidemia and stable prevalence of high or borderline high blood pressure between 1999–2000 and 2011–2012 for children and adolescents aged 8–17 y (45).
This analysis is subject to several limitations. First, response rates for NHANES have declined over time since the inception of the continuous NHANES in 1999. NHANES weights are adjusted for nonresponse to mitigate this concern. Second, the NHANES did not oversample all Hispanic persons or non-Hispanic Asian persons in 1999–2006, so estimates could not be calculated for these populations during these years and race and Hispanic origin categorization is limited to non-Hispanic black, non-Hispanic white, and Mexican-American populations in this analysis. Third, the 1999–2006 DXA data had missingness related to age, BMI, weight, height, and possibly other characteristics and thus relied on imputed data. During 2011–2018, there was less concern for missingness related to age, BMI, weight, and height, and therefore data were not imputed. In this study, analyses were stratified by sex and weights were standardized by age and race and Hispanic origin to improve comparability across time, further limiting the impact of missingness. Fourth, analysis is currently limited to whole-body measures of adiposity and does not distinguish how adipose tissue is distributed in the body. Significant evidence suggests that the distribution of body fat may be more important to health outcomes than the amount or proportion of total body fat. In adults, visceral adipose tissue (VAT) has a stronger association with negative health outcomes than total body fat or abdominal subcutaneous adipose tissue (SAT) (46–48). In children and adolescents, this relation is less clearly defined, with varying associations with health outcomes seen for both VAT and abdominal SAT (49–52). VAT and abdominal SAT vary by age, maturational status, race and ethnicity, and sex, further complicating comparisons (50). Fifth, the DXA data were captured using different machines in 1999–2006 than in 2011–2018, which could lead to variability, although the use of quality control scans should have kept such variability to a minimum (19, 21–24).
In conclusion, DXA-derived measures of adiposity, including %BF and FMI, generally increased in children and adolescents aged 8–19 y in the United States from 1999–2006 to 2011–2018, although the magnitude of such changes was small. These changes were largest among Mexican-American males and females and non-Hispanic black males had similar but nonsignificant increases. Changes also varied by sex, age group, and BMI category and were not always consistent with observed changes in BMI. Because BMI does not always reflect underlying adiposity, these findings reinforce the need to consider other measures, besides BMI categories, when studying adiposity in children and adolescents.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—NS: prepared the data; BS: analyzed the data, wrote the paper, and has primary responsibility for the final content; and all authors: designed the research, participated in critical revision of the manuscript, and read and approved the final manuscript. The authors report no conflicts of interest.
Notes
The authors reported no funding received for this study.
The findings and conclusions in this report are those of the authors and not necessarily the official position of the CDC or the NIH.
Supplemental Figures 1–5 and Supplemental Tables 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Abbreviations used: FFMI, fat-free mass index; FMI, fat mass index; MEC, mobile examination center; SAT, subcutaneous adipose tissue; VAT, visceral adipose tissue; %BF, percentage body fat.
Contributor Information
Bryan Stierman, Division of Health and Nutrition Examination Surveys, National Center for Health Statistics, CDC, Hyattsville, MD, USA; Epidemic Intelligence Service, CDC, Atlanta, GA, USA.
Cynthia L Ogden, Division of Health and Nutrition Examination Surveys, National Center for Health Statistics, CDC, Hyattsville, MD, USA.
Jack A Yanovski, Section on Growth and Obesity, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, Rockville, MD, USA.
Crescent B Martin, Division of Health and Nutrition Examination Surveys, National Center for Health Statistics, CDC, Hyattsville, MD, USA.
Neda Sarafrazi, Division of Health and Nutrition Examination Surveys, National Center for Health Statistics, CDC, Hyattsville, MD, USA.
Craig M Hales, Division of Health and Nutrition Examination Surveys, National Center for Health Statistics, CDC, Hyattsville, MD, USA; United States Public Health Service, Rockville, MD, USA.
Data Availability
Data described in the article are publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm.
References
- 1. Barlow SE, Expert Committee. Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Supplement 4):S164–92. [DOI] [PubMed] [Google Scholar]
- 2. CDC National Center for Chronic Disease Prevention and Health Promotion.. Defining childhood obesity. [Internet]. Atlanta (GA): CDC; [cited 2021 Feb 1]. Available from: https://www.cdc.gov/obesity/childhood/defining.html. [Google Scholar]
- 3. QuickStats: prevalence of obesity and severe obesity among persons aged 2–19 years — National Health and Nutrition Examination Survey, 1999–2000 through 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69(13):390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes. 1999;23(S2):S2–S11. [DOI] [PubMed] [Google Scholar]
- 5. Han JC, Lawlor DA, Kimm SYS. Childhood obesity. Lancet. 2010;375(9727):1737–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gordon-Larsen P, The NS, Adair LS. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity. 2010;18(9):1801–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Umer A, Kelley GA, Cottrell LE, Giacobbi P Jr, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta-analysis. BMC Public Health. 2017;17(1):683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bray GA, DeLany JP, Volaufova J, Harsha DW, Champagne C. Prediction of body fat in 12-y-old African American and white children: evaluation of methods. Am J Clin Nutr. 2002;76(5):980–90. [DOI] [PubMed] [Google Scholar]
- 9. Freedman DS, Butte NF, Taveras EM, Lundeen EA, Blanck HM, Goodman AB, Ogden CL. BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–2014. Obesity. 2017;25(4):739–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Demerath EW, Schubert CM, Maynard LM, Sun SS, Chumlea WC, Pickoff A, Czerwinski SA, Towne B, Siervogel RM. Do changes in body mass index percentile reflect changes in body composition in children? Data from the Fels Longitudinal Study. Pediatrics. 2006;117(3):e487–95. [DOI] [PubMed] [Google Scholar]
- 11. Freedman DS, Ogden CL, Blanck HM, Borrud LG, Dietz WH. The abilities of body mass index and skinfold thicknesses to identify children with low or elevated levels of dual-energy X-ray absorptiometry–determined body fatness. J Pediatr. 2013;163(1):160–6.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Steinberger J, Jacobs DR, Raatz S, Moran A, Hong CP, Sinaiko AR. Comparison of body fatness measurements by BMI and skinfolds vs dual energy X-ray absorptiometry and their relation to cardiovascular risk factors in adolescents. Int J Obes. 2005;29(11):1346–52. [DOI] [PubMed] [Google Scholar]
- 13. Freedman DS, Ogden CL, Kit BK. Interrelationships between BMI, skinfold thicknesses, percent body fat, and cardiovascular disease risk factors among U.S. children and adolescents. BMC Pediatr. 2015;15(1):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gishti O, Gaillard R, Durmus B, Abrahamse M, van der Beek EM, Hofman A, Franco OH, de Jonge LL, Jaddoe VW. BMI, total and abdominal fat distribution, and cardiovascular risk factors in school-age children. Pediatr Res. 2015;77(5):710–8. [DOI] [PubMed] [Google Scholar]
- 15. Flegal KM, Ogden CL, Yanovski JA, Freedman DS, Shepherd JA, Graubard BI, Borrud LG. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. Am J Clin Nutr. 2010;91(4):1020–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Weber DR, Moore RH, Leonard MB, Zemel BS. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am J Clin Nutr. 2013;98(1):49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. CDC National Center for Health Statistics (NCHS).. National Health and Nutrition Examination Survey. [Internet]. Hyattsville (MD): NCHS; 2021[cited 2021 Feb 2]. Available from: https://www.cdc.gov/nchs/nhanes/index.htm. [Google Scholar]
- 18. CDC National Center for Health Statistics (NCHS).. Clinical growth charts. [Internet]. Hyattsville (MD): NCHS; 2017[cited 2021 Feb 2]. Available from: https://www.cdc.gov/growthcharts/clinical_charts.htm. [Google Scholar]
- 19. CDC National Center for Health Statistics (NCHS).. The 1999–2006 dual energy X-ray absorptiometry (DXA) multiple imputation data files and technical documentation. [Internet]. Hyattsville (MD): NCHS; 2013; [cited 2021 Feb 2]. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/Dxa/Dxa.aspx. [Google Scholar]
- 20. Schenker N, Borrud LG, Burt VL, Curtin LR, Flegal KM, Hughes J, Johnson CL, Looker AC, Mirel L. Multiple imputation of missing dual-energy X-ray absorptiometry data in the National Health and Nutrition Examination Survey. Stat Med. 2011;30(3):260–76. [DOI] [PubMed] [Google Scholar]
- 21. CDC National Center for Health Statistics (NCHS).. Dual-energy X-ray absorptiometry—whole body, 2017–2018, data documentation, codebook, and frequencies. [Internet]. Hyattsville (MD): NCHS; 2020[cited 2021 Feb 2]. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/DXX_J.htm. [Google Scholar]
- 22. CDC National Center for Health Statistics (NCHS).. National Health and Nutrition Examination Survey: body composition procedures manual[Internet]. Hyattsville (MD): NCHS; 2018[cited 2021 May 13]. Available from: https://wwwn.cdc.gov/nchs/data/nhanes/2017-2018/manuals/Body_Composition_Procedures_Manual_2018.pdf. [Google Scholar]
- 23. CDC National Center for Health Statistics (NCHS).. National Health and Nutrition Examination Survey: analytic guidelines, 2011–2014 and 2015–2016. [Internet]. Hyattsville (MD): NCHS; 2018[cited 2021 May 13]. Available from: https://wwwn.cdc.gov/nchs/data/nhanes/analyticguidelines/11-16-analytic-guidelines.pdf. [Google Scholar]
- 24. Lumley T. Survey: analysis of complex survey samples. R package version 3.36. 2019. [Internet]. [Accessed 2019 Aug 15]. Available from: https://CRAN.R-project.org/package=survey. [Google Scholar]
- 25. Rubin DB, Schenker N. Multiple imputation for interval estimation from simple random samples with ignorable nonresponse. J Am Statist Assoc. 1986;81(394):366–74. [Google Scholar]
- 26. Barnard J, Rubin DB. Miscellanea. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86(4):948–55. [Google Scholar]
- 27. Flegal KM, Troiano RP. Changes in the distribution of body mass index of adults and children in the US population. Int J Obes. 2000;24(7):807–18. [DOI] [PubMed] [Google Scholar]
- 28. Ogden CL, Li Y, Freedman DS, Borrud LG, Flegal KM. Smoothed percentage body fat percentiles for U.S. children and adolescents, 1999–2004. Natl Health Stat Report. 2011;(43):1–7. [PubMed] [Google Scholar]
- 29. Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, Hales CM. Trends in obesity prevalence by race and Hispanic origin—1999–2000 to 2017–2018. JAMA. 2020;324(12):1208–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lu Y-C, Lin YC, Yen AM-F, Chan WP. Dual-energy X-ray absorptiometry-assessed adipose tissues in metabolically unhealthy normal weight Asians. Sci Rep. 2019;9(1):17698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shea JL, King MT, Yi Y, Gulliver W, Sun G. Body fat percentage is associated with cardiometabolic dysregulation in BMI-defined normal weight subjects. Nutr Metab Cardiovasc Dis. 2012;22(9):741–7. [DOI] [PubMed] [Google Scholar]
- 32. Gómez-Ambrosi J, Silva C, Galofré JC, Escalada J, Santos S, Gil MJ, Valentí V, Rotellar F, Ramírez B, Salvador Jet al. . Body adiposity and type 2 diabetes: increased risk with a high body fat percentage even having a normal BMI. Obesity. 2011;19(7):1439–44. [DOI] [PubMed] [Google Scholar]
- 33. Lee S, Arslanian S. Body composition and cardiorespiratory fitness between metabolically healthy versus metabolically unhealthy obese black and white adolescents. J Adolesc Health. 2019;64(3):327–32. [DOI] [PubMed] [Google Scholar]
- 34. Sun SS, Schubert CM, Chumlea WC, Roche AF, Kulin HE, Lee PA, Himes JH, Ryan AS. National estimates of the timing of sexual maturation and racial differences among US children. Pediatrics. 2002;110(5):911–9. [DOI] [PubMed] [Google Scholar]
- 35. Siervogel RM, Demerath EW, Schubert C, Remsberg KE, Chumlea WC, Sun S, Czerwinski SA, Towne B. Puberty and body composition. Horm Res. 2003;60(Suppl 1):36–45. [DOI] [PubMed] [Google Scholar]
- 36. Garn SM, Clark DC, Ad Hoc Committee to Review the Ten-State Nutrition Survey. Trends in fatness and the origins of obesity. Pediatrics. 1976;57(4):443–56. [PubMed] [Google Scholar]
- 37. Kaplowitz PB. Link between body fat and the timing of puberty. Pediatrics. 2008;121(Supplement 3):S208–17. [DOI] [PubMed] [Google Scholar]
- 38. Crocker MK, Stern EA, Sedaka NM, Shomaker LB, Brady SM, Ali AH, Shawker TH, Hubbard VS, Yanovski JA. Sexual dimorphisms in the associations of BMI and body fat with indices of pubertal development in girls and boys. J Clin Endocrinol Metab. 2014;99(8):E1519–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Herman-Giddens ME, Steffes J, Harris D, Slora E, Hussey M, Dowshen SA, Wasserman R, Serwint JR, Smitherman L, Reiter EO. Secondary sexual characteristics in boys: data from the Pediatric Research in Office Settings Network. Pediatrics. 2012;130(5):e1058–68. [DOI] [PubMed] [Google Scholar]
- 40. Euling SY, Herman-Giddens ME, Lee PA, Selevan SG, Juul A, Sørensen TIA, Dunkel L, Himes JH, Teilmann G, Swan SH. Examination of US puberty-timing data from 1940 to 1994 for secular trends: panel findings. Pediatrics. 2008;121(Supplement 3):S172–91. [DOI] [PubMed] [Google Scholar]
- 41. Martinez GM. Trends and patterns in menarche in the United States: 1995 through 2013–2017. Natl Health Stat Report. 2020;(146):1–12. [PubMed] [Google Scholar]
- 42. Maldonado LE, Albrecht SS. Does the immigrant advantage in overweight/obesity persist over time in Mexican American youth? NHANES 1988–1994 to 2005–2014. Obesity. 2018;26(6):1057–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Weber DR, Leonard MB, Shults J, Zemel BS. A comparison of fat and lean body mass index to BMI for the identification of metabolic syndrome in children and adolescents. J Clin Endocrinol Metab. 2014;99(9):3208–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shypailo RJ, Wong WW. Fat and fat-free mass index references in children and young adults: assessments along racial and ethnic lines. Am J Clin Nutr. 2020;112(3):566–75. [DOI] [PubMed] [Google Scholar]
- 45. Kit BK, Kuklina E, Carroll MD, Ostchega Y, Freedman DS, Ogden CL. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999–2012. JAMA Pediatrics. 2015;169(3):272–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Malden D, Lacey B, Emberson J, Karpe F, Allen N, Bennett D, Lewington S. Body fat distribution and systolic blood pressure in 10,000 adults with whole-body imaging: UK Biobank and Oxford BioBank. Obesity. 2019;27(7):1200–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Britton KA, Massaro JM, Murabito JM, Kreger BE, Hoffmann U, Fox CS. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol. 2013;62(10):921–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Neeland IJ, Turer AT, Ayers CR, Powell-Wiley TM, Vega GL, Farzaneh-Far R, Grundy SM, Khera A, McGuire DK, de Lemos JA. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA. 2012;308(11):1150–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kjellberg E, Roswall J, Andersson J, Bergman S, Karlsson AK, Svensson PA, Kullberg J, Dahlgren J. Metabolic risk factors associated with visceral and subcutaneous adipose tissue in a sex-specific manner in seven-year-olds. Obesity. 2019;27(6):982–8. [DOI] [PubMed] [Google Scholar]
- 50. Staiano AE, Katzmarzyk PT. Ethnic and sex differences in body fat and visceral and subcutaneous adiposity in children and adolescents. Int J Obes. 2012;36(10):1261–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hübers M, Geisler C, Plachta-Danielzik S, Müller MJ. Association between individual fat depots and cardio-metabolic traits in normal- and overweight children, adolescents and adults. Nutr Diabetes. 2017;7(5):e267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kelly AS, Dengel DR, Hodges J, Zhang L, Moran A, Chow L, Sinaiko AR, Steinberger J. The relative contributions of the abdominal visceral and subcutaneous fat depots to cardiometabolic risk in youth. Clin Obes. 2014;4(2):101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the article are publicly and freely available without restriction at https://www.cdc.gov/nchs/nhanes/index.htm.