Abstract
Background
We examined the implementation of a brief, behavioural activation (BA) model, via telemedicine, for perinatal populations during a confluence of significant global events in 2020. We conducted a rigorous qualitative study to identify relevant barriers and facilitators from the perspectives of both perinatal participants and treatment providers. We also present two case studies where BA was used and adapted to provide patient-centered care.
Methods
Within the ongoing SUMMIT non-inferiority randomized controlled trial in Canada and USA, we interviewed a random selection of perinatal participants (n = 23) and all treatment providers (n = 28). A content analysis framework was developed to identify relevant barriers and facilitators and frequencies were calculated for each emergent theme within and across respondent groups.
Results
Key facilitators reported by participants receiving BA were that BA helped with support and social connection (73.9%), creative problem solving (26.1%) and attending to pandemic-related symptoms (21.7%). Key facilitators endorsed by providers delivering BA were the use of telemedicine (35.7%) and loosening of government restrictions (21.4%). Both participant groups reported similar barriers to BA during the pandemic such as a lack of privacy and limited activities due to pandemic restrictions. However, providers were more likely to endorse pandemic-related life stressors as a barrier to treatment delivery compared to participants (64.3% vs. 34.8%). Both participant groups experienced explicit discussion of race and the racial justice movements during sessions as beneficial and reported harms of not doing so to the therapeutic alliance.
Conclusions
BA offers a person-centered model to facilitate social connection through creative problem-solving for women with perinatal depressive and anxiety symptoms within the context of the COVID-19 pandemic. Explicit discussion of race and racial injustice during sessions is an important and helpful aspect in psychological treatments.
Keywords: Behavioral activation, Perinatal depression, Psychotherapy, COVID-19, Race, Ethnicity
1. Introduction
Since 2020, the novel coronavirus disease (COVID-19) has amplified the need to improve access to mental healthcare for patients, healthcare workforce and our communities at large (Xiang et al., 2020; Lai et al., 2020). Simultaneously, the Black Lives Matter movement and its contemporaneous global demonstrations for racial justice further highlighted that psychological interventions should be equitably accessible. However, the treatment gap for depression and anxiety—the most common psychiatric diagnoses likely to emerge during and after COVID-19 (Lai et al., 2020; Ettman et al., 2020)—may be as high as 80% (Thornicroft et al., 2017) and 90% (Alonso et al., 2018), respectively, in high-income countries such as the United States, and even worse for women of color (Jankovic et al., 2020).
Perinatal women are at heightened risk of depression and anxiety (Chen et al., 2020), with depression being the leading cause of disability among mothers worldwide (Ferrari et al., 2013). In the USA and Canada, as few as 20% of perinatal women suffering depression and anxiety have access to minimally-adequate treatments (Thornicroft et al., 2017; Byatt et al., 2016). Barriers to treatment include transportation, childcare, stigma, and insufficient trained professionals (Kazdin, 2017). While physical distancing has been required to curb the spread of COVID-19, the resultant social isolation is also a substantive risk factor of mental illness and suicide (Heinrich and Gullone, 2006), and the impact of social isolation for perinatal women is undeniable. Additional challenges during the COVID-19 pandemic include economic stress, housing and food insecurity, and reduced access to perinatal care—all of which were exacerbated for women of color (Morales et al., 2020; Purtle, 2020).
Women of color are less likely to access mental health services and have unmet mental health needs due to racialized barriers to access (Salameh et al., 2019; Wang et al., 2021), including experiences of discrimination and racial micro-aggressions while seeking care, mistrust of healthcare providers and in the mental healthcare system, and reduced quality of treatment for ethnic and minority groups (Wang et al., 2021; Watson et al., 2019; Mukherjee et al., 2016). Along with racialized barriers, additional challenges for women of color include cultural stigma about mental illness, beliefs about motherhood and women's roles, and a lack of language proficiency (Watson et al., 2019; Sambrook Smith et al., 2019).
In this manuscript, we present a behavioral activation (BA) model as one potential solution to address the mental healthcare challenges and disparities during the COVID-19 pandemic for perinatal women with depression and anxiety and movements against racial injustice. Within the ongoing Scaling Up Maternal Mental healthcare by Increasing access to Treatment (SUMMIT) trial (Singla et al., 2021), we conducted a qualitative study to identify relevant barriers and facilitators from the perspectives of participants receiving, and treatment providers delivering, BA. We also present two case studies where BA was used and adapted during COVID-19 and the racial justice movement to be responsive to disparities in access to needed, evidence-based psychological interventions derived from case notes of trial providers, and the results of qualitative interviews from a subset of the trial's patient participants and providers (Leitch et al., 2020).
2. Methods
2.1. Setting
The SUMMIT trial (www.thesummittrial.com) is currently taking place in academic hospitals across three hubs—Toronto, Chapel Hill, and Chicago. This non-inferiority randomized controlled trial includes adult women with perinatal depressive and anxiety symptoms, where participants receive an 8-session course of BA delivered by mental health specialists (psychiatrists, psychologists or social workers) or trained non-mental health specialist providers (e.g., registered nurses, midwives, with experience in perinatal care but not perinatal mental health care) using HIPPA/PHIPA-compliant telemedicine platforms. The SUMMIT trial is registered (NCT4153864) and ethical approvals were received at all sites. Details about the larger SUMMIT trial are available in the study protocol (Singla et al., 2021).
2.2. Participants
Participants for the current study included study participants and provider participants who, respectively, received and delivered the SUMMIT BA treatment between March 2020 and January 2021.
2.2.1. Perinatal participants
Perinatal participants (N = 23) were randomly-selected women from the larger SUMMIT trial across all the three hubs (see Table 1 for details). Eligible participants were adult women (aged 18 years or older), with depressive symptoms (EPDS≥10, (Cox et al., 1987)), pregnant up to 36 weeks or 4–30 weeks postpartum, and English or Spanish-speaking. Active suicidal intent; active substance abuse or dependence; psychosis or mania; a recent change in medication; ongoing psychotherapy or severe fetal anomalies, stillbirth or infant death at the time of enrollment represented the exclusion criteria. For the current study, we contacted a random subset of eligible participants who completed a minimum of 5 treatment sessions and recruited a representative sample of racially and ethnically diverse subjects. To capture participants across groups, our Data Coordinator identified a pool of potential participants using a maximum variance sample who were pregnant and postpartum, varying baseline symptom severity of mild, moderate and severe symptomatology, and key sociodemographic factors such as age and ethnicity.
Table 1.
Interview participants across sites.
| Interview Participants | Toronto | UNC | Northshore | Total N |
|---|---|---|---|---|
| Study Participants | 14 | 3 | 6 | 23 |
| Treatment Providers | 12 | 6 | 10 | 28 |
| Specialist Providers | 6 | 2 | 5 | 13 |
| NSPs | 6 | 4 | 5 | 15 |
2.2.2. Provider participants
Data from all treatment providers (n = 28) were used (see Table 1 for details), including both non-specialist providers (NSPs, n = 15), such as nurses and midwives with no formal experience delivering mental healthcare, and specialist providers (SPs, n = 13), including social workers, psychologists, and psychiatrists.
2.3. Behavioral activation treatment
Behavioral Activation (BA) proposes that the key to reducing depression and anxiety is to increase enjoyable or fulfilling activities that align with one's values (Dimidjian et al., 2011; Jacobson et al., 2001), targeting key mechanisms of patient activation and avoidant coping. A key BA-specific principle involves teaching both participants and treatment providers to act according to their values, rather than their emotions. Acting according to values can foster a sense of well-being and agency (Kanter et al., 2010), particularly during times of crisis. The content of our model expands on core principles of behavioural activation by identifying key values through a values card sort, a focus on interpersonal mechanisms (Singla et al., 2021) by improving communication skills and relaxation techniques. A handout was provided to all treatment providers about the delivery of BA in the context of the pandemic (see Appendix A).
In the SUMMIT trial, we use an 8-session manualized BA model (Patel et al., 2017) that has been adapted for perinatal populations. Treatment sessions are delivered to an individual participant, on a weekly basis, by a trained treatment provider using a secure, telehealth server such as Zoom™ or WebEx™. BA was selected for the SUMMIT trial because of its strong evidence base in treating depression in the general population (Cuijpers et al., 2007; Mazzucchelli et al., 2009) and perinatal populations (O'mahen et al., 2014; Dimidjian et al., 2017), and because it is easy to understand and implement as demonstrated in its effective delivery by NSPs worldwide (Patel et al., 2017; Jordans et al., 2019; Richards et al., 2016). All treatment providers were trained and supervised by a clinical lead—an expert in psychological interventions and perinatal mental health. Treatment fidelity is assessed among for adherence to treatment-specific and general skills by independent fidelity raters (described elsewhere (Singla et al., 2021).
2.4. Data collection
Case study data were extracted by clinical leads (PR and CES) from study treatment log notes, audio recordings of sessions, and clinical supervision with treating providers. Case study data were not from the same individuals who consented to participate in the interviews.
Individual semi structured interviews were conducted with consenting study participants, and focus groups were conducted with BA treatment providers to capture a range of perspectives using a HIPPA/PHIPA-compliant version of Zoom™. All qualitative interviews and focus groups were audio-recorded and transcribed, with random quality checks conducted by independent research volunteers (see Appendix B for sample questions). Self-reported demographic characteristics (age, ethnicity, martial and employment status) for patient participants were also collected.
2.5. Data analysis
Qualitative data were analyzed using NVivo™. Content analysis (Hsieh and Shannon, 2005) was conducted by two co-authors (SH and NA), who engaged in an iterative coding process to identify patterns across participants and providers’ responses to questions about their experiences receiving and delivering BA during COVID-19. A coding index was developed using the interview question index to organize emergent codes into themes and identify the most frequently endorsed barriers and facilitators reported by participants and providers, respectively. The index was updated iteratively in the second stage of coding to reflect the broader qualitative themes and subthemes that arose during the coding process. Coding was done through a 2-step process using NVIVO™: an initial, line by line coding stage was conducted using the initial coding index, followed by a more focused, selective coding stage, where the initial codes were sorted, synthesized, and integrated to reflect recurring patterns and, themes and subthemes that arose in the coded data. Data were collected from all three study sites to aim for saturation and sufficiently capture the unique experiences of participants and providers. Inter-rater reliability between coders was calculated using Cohen's Kappa (κ) coefficient, demonstrating excellent agreement (κ=0.95). In addition, the frequency of barriers and facilitators for each of the emergent subthemes was calculated to determine the most salient themes endorsed by participants.
3. Results
3.1. Case studies
We present the case studies followed by the participant-level data because the former showcase the consistent intersection between perinatal mood disorders, the interpersonal consequences of the pandemic and public health responses and the heightened awareness of racial injustice; while the latter develop the barriers and facilitators relevant to this moment in time. Pseudonyms and other identifying information has been modified to secure the anonymity of participants.
3.1.1. Case study 1
Identifying Data. Sidra was a 42-year-old pregnant married Canadian woman of South Asian descent and mother of a 3-year son. At the time of assessment, she was in her third pregnancy, and had suffered a late pregnancy loss with miscarriage two years previously.
History of Presenting Illness. Sidra had been struggling with perinatal depression for the past 6 weeks with symptoms of low mood, disrupted sleep and anhedonia. She did not have suicidal thoughts or intentions, and there was no history of current or past substance misuse, bipolar or psychotic symptoms. She had a past history of episodic depression, with no hospitalizations and was not taking any medications.
Sidra had recently lost her job as an Early Childhood Educator. Due to the COVID-19 pandemic and restrictions imposed by public health, her spouse—a teacher—was working from home and overwhelmed with adjusting to online teaching. Their son's daycare was closed, and they were both no longer seeing their family members, friends, neighbors or colleagues to maintain isolation. Because Sidra's parents and in-laws were older and had health problems, she didn't ask them for help with childcare nor did she wish to breach public health guidelines or expose any of them in case she or her family members may be asymptomatic carriers of COVID-19. Tensions with her husband were heightened, and they were avoiding conflict and speaking little to one another around issues of childcare, household responsibilities, and financial worries. In addition, Sidra was worried about the potential to miscarry in light of her recent history of late pregnancy loss.
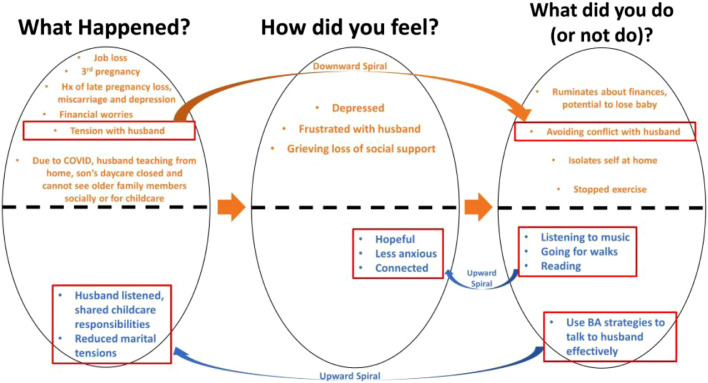
Course of Treatment. Over the 8-sessions of BA, she formed a therapeutic alliance with agreement on the goals to improve depression symptoms and found ways to engage in values-based activities. The provider empathically validated Sidra's concerns and highlighted links between stressors, feelings, activities that she was doing, or not doing. Sidra identified some activities she had stopped doing that had prior given her a sense of pleasure and connection such as getting together with friends and family, singing in a choir, exercising, listening to music, going for walks, and reading. They collaboratively mapped an understanding of what was contributing to downward mood spirals and identified important relationships in her circle of supports. Sidra began to track hourly activities and mood states shedding further light on problems to target in the stressful, upsetting moments of her days including marital tensions.
Using communication strategies, she was able to confide in her spouse, improve their relationship and find ways to better support one another, and share child-care responsibilities. She noticed how her mood worsened during periods of inaction when ruminating with worries about miscarrying. She made efforts during these periods to deliberately shift her attention to engage in values-based antidepressant activities such as listening to music, and playing with their son. This was in keeping with her efforts to select, plan and schedule values-based activities that provided a sense of connection, accomplishment, or enjoyment – finding creative ways to celebrate occasions and maintain safe physical distancing. Drawing from the BA approaches to problem solving, communication, and engaging in values-based activities, Sidra's depressive and anxiety symptoms remitted.
Fig. 1 depicts a map of a patient's life, tracking current patterns between the situation, her feelings and behaviours. feeling and doing.
Fig. 1.
Mapping for case study 1.
3.1.2. Case study 2
Identifying Data. Alicia was a 37-year-old postpartum, married, Black woman living in the United States who identified as African American. She had a graduate degree, was currently employed and working remotely. She had four children, ranging from 2 months to 11 years. She had experienced ptyalism and hyperemesis gravidarum with each of her previous pregnancies.
History of Presenting Illness. For her current pregnancy, she gave birth in the hospital under strict COVID-19 precautions and described going to the hospital for delivery as “driving into the belly of the storm.” Two weeks following childbirth, the patient woke up in a pool of blood. Her husband rushed her to the hospital, and because she believed she would die, she described her wishes for her will and care for her children to her husband during the drive. She underwent dilation and curettage and spent two nights alone in the hospital. On the third day of admission, her blood pressure was unstable and she had a blood transfusion. Upon meeting her provider, 2 months after her hospitalization, she expressed concerns about the effects of the blood transfusion on her mood.
At the outset of treatment, Alicia endorsed depressed mood, excessive anxiety and worry, anger, and insomnia. She denied suicidal thoughts or intentions, and while there was no history of current or past substance misuse, bipolar or psychotic symptoms, she reported drinking a glass or two of wine each evening in order to fall asleep. She had a past history of depression and anxiety, which was never diagnosed or treated, and she was not taking any medications.
With both schools and daycares closed, Alicia and her husband were sharing childcare responsibilities while trying to work. The family was not seeing anyone outside of their home because of state-wide, stay-at-home orders. Her children were especially disappointed that they could not see their grandparents. At the initial session, Alicia described difficulty balancing her recently recovery with the fear of dying, working full-time, and childcare. After the first session, George Floyd was killed by police officers. The killing highlighted racial injustice on both a local and global scale and was followed by increasing police violence in response to social justice demonstrations in the city where Alicia lived. The patient began experiencing increased sadness and anxiety in the wake of the killing. She reported difficulty sleeping, with early morning insomnia. She often awoke at 4:30AM and just started working by sending emails and planning her day.
Course of Treatment. Over the 8-sessions of BA with her trained non-specialist provider (NSP), they formed a therapeutic alliance with agreement on the goal of reducing depression symptoms by 1) tracking activities to gain insight into activities that affect mood, and 2) increasing engagement in mood-promoting and value-consistent behaviors.
Alicia and the provider developed a shared understanding of what was contributing to downward mood spirals, including the traumatic health event, ongoing pandemic and social isolation, racial injustice, returning to work at 8 weeks postpartum, and childcare responsibilities. Alicia and the NSP worked together to clarify these stressors, identify and validate her emotional response, and discover patterns of behavior in which Alicia engages in response to her emotions. By tracking her activities and mood throughout the day, Alicia noticed that her mood was worst in the morning after waking too early and engaging in a busy work schedule with deadlines and meetings. Communication concerns with her husband also emerged as a significant stressor that was identified through tracking. Communication with her husband became a central treatment goal to reduce marital discord and negotiate a better morning routine that would allow the patient to feel less busy. In later sessions, the patient used communication and problem-solving skills at work to negotiate a better work schedule that felt less stressful. She also began planning and scheduling pleasurable activities throughout the week, which elevated her mood, despite ongoing global stressors related to the pandemic and racial injustice.
Based on the patient's values, she was able to identify activities that promoted creativity and pleasure (going hiking with her children instead of their usual indoor activities) and addressing issues of racial injustice (prioritizing self-care in addition to advocacy and saying “no” to requests at work). Drawing from the BA approaches to problem solving, communication, and engaging in values-based activities, Alicia's depressive and anxiety symptoms diminished. In the ending phase of treatment, she connected her recent stressors and triggers of earlier life traumas she hadn't processed before. She requested a referral for specialized therapy to address these traumas.
3.2. Qualitative study
Our qualitative findings illustrate the barriers and facilitators that were most frequently endorsed by perinatal participants (Table 2 ) and treatment providers while receiving and delivering BA. The key themes and their frequencies are summarized in Table 3 and are described below.
Table 2.
Study participant characteristics (N = 23).
| Participants | Frequency (%) unless otherwise indicated |
|---|---|
| Age (range) | 32.0 (20 to 40) |
| Ethnicity | |
| White | 12 (52.2) |
| Black/African American | 2 (8.7) |
| Hispanic | 2 (8.7) |
| Multi-race | 2 (8.7) |
| Asian | 2 (8.7) |
| Do not wish to answer | 2 (8.7) |
| Other | 1 (4.3) |
| Marial Status | |
| Married | 19 (82.6) |
| Single | 4 (23.5) |
| Do not wish to answer | 2 (8.7) |
| Dating | 1 (4.3) |
| Employment | |
| Maternity Leave | 8 (34.8) |
| Full-time employment | 6 (26.1) |
| Part-time employment | 3 (13.0) |
| Unemployed | 3 (13.0) |
| Student | 2 (8.7) |
| Homemaker | 1 (4.3) |
Table 3.
Barriers and facilitators endorsed by participants and providers in receiving or delivering BA during COVID-19.
| Key Themes | N (%) |
|---|---|
| Participants Receiving BA During COVID-19 (n = 23) | |
| Facilitators | |
| BA provides support and social connection during COVID-19 pandemic | 17 (73.9) |
| Creative problem solving to address barriers to attending BA | 6 (26.1) |
| BA helps with management of pandemic related symptoms | 5 (21.7) |
| Barriers | |
| Privacy and work/family interruptions during BA sessions | 8 (34.8) |
| Pandemic induced/exacerbated life stressors | 8 (34.8) |
| Limited activities due to regional COVID-19 restrictions | 7 (30.4) |
| Providers Delivering BA During COVID-19 (n = 28) | |
| Facilitators | |
| Telemedicine has been a facilitator particularly during COVID-19 | 10 (35.7) |
| Loosening of government and institutional restrictions | 6 (21.4) |
| Barriers | |
| Pandemic induced/exacerbated life stressors | 18 (64.3) |
| Limited activities due to regional COVID-19 restrictions | 9 (32.1) |
| Privacy and work/family interruptions during BA sessions | 6 (21.4) |
3.2.1. Facilitators to receiving and delivering BA during the COVID-19 pandemic
Perinatal Participant Perspectives. Almost all participants reported that receiving BA during the COVID-19 pandemic was helpful (n = 21 of 23, 91.3%). Participants identified three key facilitators while receiving weekly treatment sessions. First, many (n = 17 or 73.9%) participants reported that receiving BA sessions during this time provided consistent social connection and support.
“I don't think anybody ever plans to bring a baby into the world during a pandemic… It was beneficial for me to reflect on my feelings and not everybody else's feelings [during BA sessions]. It was nice to be able to learn how to cope with how I'm feeling, that it's normal.... to be able to express myself and not just compress my feelings… [the treatment] helped me a lot.” (Participant _Northshore_02)
Second, more than one-fourth of participants (6 of 23, 26.1%) reported that planning creative strategies with their provider to do values-based activities were. Problem solving helped to address barriers related to attending sessions and doing BA homework that arose due to regional COVID-19 restrictions and family interruptions.
“And then when it came to me actually stepping out [for activities], I had planned things in places where I knew no one else would be there so it was all secluded and full of fresh air, open-air and like basically the parks and stuff that are less visited. And that way it was good, no anxiety at all whatsoever and that's part of the planning.” (Participant_Toronto_12)
Finally, when asked what they found helpful about participating in the BA treatment during COVID-19, some participants (5 of 23, 21.7%) reported that receiving BA helped them discover ways to cope with their depression and or anxiety symptoms that were specifically related to the pandemic.
“My anxiety was through the roof between COVID, even all post-partum. I always had this pit in the bottom in my stomach of something is going to go wrong with my son. COVID made it that much worse….[The BA provider] helped me work through how we were going to manage that, and what was realistic and what wasn't, and helped me come out of it with a game plan.” (Participant_ Toronto _11)
Treatment Provider Perspectives. Half of providers (14 of 24, 50.0%) specified that BA was particularly helpful for their patients who experienced exacerbated stressors during the pandemic. The other half of providers (14 of 28, 67.8%) reported that BA was helpful irrespective of the pandemic, because BA can facilitate patients’ skill building, such as problem solving, communication skills, and activity scheduling. The most common facilitator reported by BA treatment providers was the use of telemedicine while delivering BA during the pandemic. Telemedicine allowed for flexibility and convenience in both providers’ and participants’ work-family-life (n = 18 of 28, 64.2%) and the continued delivery of treatment despite restrictions on in-person care. Telemedicine also enabled participants to receive treatment that they normally would not have been able to access if it were only offered in-person.
“For me, as a parent, I work full time and I have kids and I will say that telemedicine has allowed me to be able to provide [care] … [and] to be much more available and flexible…. Because in-person [BA] is just not an option. I don't feel safe with that right now, either…. I'm really grateful that we have the telemedicine platform.” (SP_Northshore_04)
There was a loosening of regional COVID-19 restrictions in late Spring and Summer of 2020 in some cities like Toronto, which had previously been under a strict stay-at-home order. Approximately one-fifth (n = 6 or 21.4%) of providers reported that this enabled participants to increase social interactions, activities, and perceived support.
“I'd say that when the whole social bubbles came into being, I found that two of my participants finally were able to meet up with their family and that just seemed to bring such a sense of relief and support and connection that I really noticed a change… It was just such a dramatic change to see.” (NSP_Toronto_04)
3.2.2. Barriers to receiving and delivering BA during the COVID-19 pandemic
Perinatal Patient and Provider Perspectives. The most common challenge that participants reported was work or family interruptions during their BA sessions (n = 8 of 23 or 34.8%). With COVID-19 restrictions resulting in children and spouses learning and working remotely, these participants stated the need to overcome a lack of the privacy to participate, especially while needing to homeschool children, or while living in a small space.
“The only challenge that I can identify is being at home when there are other people in my household. You know, finding a private space can sometimes be challenging. I have a very supportive husband, but one week we had his parents visiting, and finding a way to be able to do this session in a way that was private was a little bit harder but still manageable.” (Participant_ UNC_01)
Likewise, a number of treatment providers (6 of 28, 21.4%) also endorsed that work and family interruptions were a challenge while delivering BA during the pandemic. Providers reported that with daycares and schools closed and spouses often working remotely, participants struggled to find the time, and physical and mental privacy to participate in BA sessions without distractions.
“I had a patient [that we had] some challenges rescheduling appointments… because she's doing homeschooling. So I think that having kids, doing the homeschooling, and having to help them to navigate through the process…And also… I have other patients that [are] not doing homeschooling, but the kids are around. Not having necessarily the privacy to talk or having a lot of interruptions during the session.” (SP_UNC_02)
Equally, participants reported the experience of additional COVID-19 related life stressors (n = 8 of 23, 34.8%) that interfered with the potential benefits of the BA treatment. These challenges related to childcare and finances, with increased anxiety symptoms.
“A lot of the anxiety and stuff that I was experiencing was probably doubled because of the pandemic…. if it was normal life… the therapy would have been maybe more effective or more, just easier to do, like the tasks and things.” (Participant_ Toronto_ 02)
However, more than two-thirds of the treatment providers (n = 18 of 28, 64.3%) reported that delivering BA during COVID-19 was challenging for providers and participants alike due to pandemic-related life stressors including fears of exposure, family and childcare challenges, healthcare-related stressors and financial stressors. Providers also reported that participants’ COVID-19 related stressors became prominent topics of discussion while delivering BA.
“The current pandemic brings up so many more stressors for our patients, and so a lot of my sessions have been related to patients having difficulty with what's going on in the current environment, and so not quite as focused on some of the maternal perinatal and postpartum concerns.” (NSP_UNC_05)
Finally, a number of participants reported limitations on the choice of safe activities that they could engage in due to regional COVID-19 restrictions as a barrier (7 of 23, 30.4%). Participants stated that the activities that they would engage in to help them feel better, such as meeting friends, going outside to exercise, or going to a mall was significantly limited in compliance with public health restrictions. This barrier was also endorsed by treatment providers (n = 9 of 28,32.1%). Providers described challenges in collaboratively generating activities with participants, as the mood-enhancing activities they would normally recommend such as social interactions and outings were not possible due to pandemic restrictions, or because participants were fearful of exposure to COVID-19.
Some of the activities that we would write down that would be helpful towards changing the behavior… or your feelings… [were limited]. That probably would be the only thing I would say [is a challenge]… Just the lack of being able to go places and do certain things. (Participant_ NorthShore_04)
“Another challenge that I had is… my go-to encouragements or my go ‘to dos’ are not really available. So like, delegating care, getting outside, connecting with other people in-person, like that has been a massive [change]…. We had to create something else… The way that we worked on that was really getting that patient to scale down and to look within their home or their bubble [to find activities they enjoy], but I did find that very limiting.” (SP_NorthShore_01)
We noted no notable differences between study sites or between provider type (NSP vs. specialist).
3.2.3. BA in the aftermath of the George Floyd murder and the Black Lives Matter protests
The murder of George Floyd that spurred demonstrations across the United States and globally against racial injustice, led to unique challenges related to these events that arose spontaneously during the interview sessions. One provider (3.5%) noted that the dual impact of the pandemic and protests on her patient:
With one of my patients, it wasn't just COVID that added a lot to her experience, but it was also the state of the police brutality in the United States and the protests and the social injustice…So that's just another thing I want to point out that's been a challenge [while delivering BA in the context of COVID-19 and social unrest].” (NSP_UNC_04)
Another provider (3.5%) reported that explicitly discussing the protests and racial injustice movements served to facilitate their therapeutic alliance:
“When we started, there was a pandemic, and then by session 3 is when the murder of George Floyd happened. And so, to be able to connect just for a few minutes on that, I think made her feel more connected with me. And I think in the long run, it did help with our being able to have a positive relationship, a therapeutic relationship. So, yeah, I think that was important [for patients to receive BA during this time of COVID-19 and social unrest].” (NSP_UNC_02)
One participant (4.3%) wondered if her SUMMIT provider would be able to understand the stressors that she was experiencing related to the Black Lives Matter movement and racial injustices while she received BA:
“Another thing is he [treatment provider] was a white guy. I was like…I'm Black [and] the Black Lives Matters movement was kind of a big stressor for me. I found myself kind of wondering, ‘does he get it?’ ‘Will he get it?’ And like so I think for me…it wouldn't have been my choice of care provider.” (Participant_Toronto_16)
In clinical supervision, NSPs at each site were encouraged to talk about their own emotional responses to police brutality and the widespread demonstrations. Some providers expressed concern that it would be too overtly “political,” and felt unprepared to have such fraught and complicated conversations. Supervisors coached them on the importance of bringing up race, discrimination, and racial injustice directly. Didactic instruction and experiential role plays were employed in the context of supervision to prepare the NSPs for such conversations.
4. Discussion
In this study, we presented two case studies where BA was used and adapted during COVID-19 and the racial justice movements to address disparities in access to needed, evidence-based psychological interventions (Leitch et al., 2020). We also identified relevant barriers and facilitators from both participant and provider perspectives of receiving and delivering one treatment modality of behavioral activation (BA) within the context of the COVID-19 pandemic and heightened awareness of racial injustice.
Our findings highlighted that the selection of BA to use in our SUMMIT trial was fortuitous because it is both flexible and context neutral. BA can address participant-specific challenges along those that arose over the course of treatment related to the context of the ongoing pandemic and racial justice movements. BA is highly adaptable because its target is each participant's unique behavioral response pattern to their own stressors and emotions. Providers collaborate with participants to identify the participant's behavioral response patterns that contribute to both positive and negative mood states. As a result, BA is adaptable to most contexts or stressors.
In the context of the pandemic, a key question that arose was how to select or plan activities that were no longer permitted or safe. Both participants and providers were encouraged to differentiate safe activities in which they have some control from those that are unsafe and which they are unable to control. Similarly, the task of setting behavioral goals to manage racial injustice can risk trivializing participants’ concerns by focusing on individual stress and depression. However, by making behavioral choices that aligned with their value system; and taking small steps to engage in modified activities that continued to provide a sense of purpose, connection, accomplishment, and pleasure helped participants and providers to better cope. Like the core elements of many evidence-based psychotherapies (Anderson et al., 2016; Wampold, 2015; Singla et al., 2017), being attentive to therapeutic alliances and empathically validating emotions during COVID-19 and racial injustice such as sadness, anxiety, and fear is essential.
4.1. Barriers and facilitators of BA in the context of COVID
Participants and providers reported several key facilitators and barriers that were critical to understanding the application of BA during the pandemic. Specific barriers, namely work and family interruptions during BA sessions, along with exacerbated life stressors due to the pandemic and limited activities—overlapped between perinatal participants and treatment providers; however, providers were almost twice as likely to report the pandemic exacerbating life stressors and symptomatology as a barrier to treatment delivery compared to participants (34.8%). In the context of COVID-19, treatment providers may find themselves facing many of the same stressors as their participants. Participants’’ lack of privacy and family interruptions have also been highlighted in recent studies exploring patient and psychotherapists’ perspectives using telemedicine during the pandemic (Crowe et al., 2020; Boldrini et al., 2020).
There were also differences in perceived facilitators between participants and providers. From the participant perspective, key facilitators of receiving BA included a focus on facilitating social connection and the use of creative problem solving. From the provider perspective, telemedicine and the use of specific activities (i.e., problem solving, communication skills, activity scheduling) in compliance with restrictions facilitated their delivery of this treatment modality. For participants, the percentage of facilitators outweighed the barriers and previous evaluations have found that facilitators—rather than barriers—are related to behavior change (Singla and Kumbakumba, 2015). Within the SUMMIT trial, recognizing what works and what requires additional attention or revision when delivering BA during the pandemic can be addressed by the clinical team during supervision.
4.1.1. Being explicit about race
While we did not systematically examine the roles of race or racial injustice on participant and provider perspectives, both participant groups spontaneously reported relevant themes. Our findings align with previous studies that highlight the benefits of explicitly discussing race to facilitate therapeutic alliance between provider and participant, along with and the harms of not doing so (Chang and Berk, 2009). In particular, and reflective of other studies (Zane et al., 2005), our findings suggest that clients may be mistrustful of therapists who do not acknowledge that racial/cultural differences may influence the therapeutic relationship. Given the extant literature has no demonstrated benefit to treatment benefits of matching participants and therapists (Cabral and Smith, 2011), guidelines on how race can be explicitly recognized in cross-racial therapeutic contexts, should be considered an essential component when training and credentialing all therapists. Additional studies are needed to explore how psychotherapy can be delivered in a culturally sensitive manner to successfully address topics of race, racial injustice and culture, from the perspective of ethnically diverse patients and therapy providers.
4.2. Implications
There are several implications to the findings mentioned above. First, and similar to other process evaluations of intervention contexts (Saunders et al., 2005), the systematic examination of challenges and facilitators are critical to identify in order to achieve optimal implementation (Evans-Lacko et al., 2010). Second, we found no significant differences between study sites, highlighting the external validity of our study Singla et al., 2021 .
5. Limitations and strengths
We note several limitations. First, we did not collect demographic information (including ethnicity) among providers. Second, we did not systematically collect qualitative data to examine the impact of race and racial injustice on participants and providers and were thus unable to discern either positive or negative interactions within the treatment dyads. This raises questions about where conversations about racial injustice are likely to the most benefits and the ways in which these discussions may fit into the BA framework. Future studies among ethnically-diverse patients and providers are required to discern whether race and racial injustice come up during treatment sessions and whether these conversations are helpful. This information is needed in clinical psychotherapy trials to inform patient-centered care among ethnically-diverse participants. Third, and given all study data were collected during the pandemic, additional studies are required to determine whether reported facilitators (e.g., BA facilitating social support) and barriers (e.g., family interruptions during telemedicine-delivered treatment sessions) are specific to the COVID-19 pandemic, or whether these would occur beyond the pandemic context.
A strength of the current study is its rigorous and systematic use of qualitative methods to examine practical questions related to the delivery of psychotherapy via telemedicine. Few studies have examined the delivery of psychotherapy from multiple perspectives during the pandemic and these findings are important to ensure that we can improve access and quality of evidence-based talk therapies to individuals suffering from depression and anxiety symptoms. This approach, which is referred to as integrative data analysis, allows for the pooling of data from numerous sources to examine information from multiple perspectives. In addition, we highlight the receipt and delivery of care as it relates to vulnerable populations—namely perinatal populations and women of color.
In sum, BA offers one person-centered model that can help women with perinatal depression even in the context of the COVID-19 pandemic and racial justice. It is aligned with stress-coping frameworks with problem-solving, connecting to social supports, and engaging in values-based activities (Folkman and Greer, 2000). Given COVID-19 disproportionately affects ethnically diverse populations (Laster Pirtle, 2020), there is the need for adaptable and person-centered care to address the growing number of individuals suffering from depressive and anxiety symptoms.
Author contributions
Authors DRS, PR and CES designed the study. DRS, SH, PR and CES wrote the initial version of the manuscript, with inputs from all co-authors. Authors SH and NA conducted the qualitative analyses. All authors have contributed to and approved the final manuscript.
Funding
The SUMMIT trial is funded as a Pragmatic Clinical Study (PCS) by the Patient-Centered Outcomes Research Institute (PCORI), PCS-2018C1–10,621. The funder was not involved in the design of the study, and is not involved in the collection, analysis, and interpretation of data, nor in writing the current manuscript. DRS is also partly funded through an Academic Scholars Award from the Department of Psychiatry at the University of Toronto.
Author statement
Authors DRS, PR and CES designed the study. DRS, SH, PR and CES wrote the initial version of the manuscript, with inputs from all co-authors. Authors SH and NA conducted the qualitative analyses. All authors have contributed to and approved the final manuscript.
Declaration of Competing Interest
The authors report no conflicts of interest.
Acknowledgements
We would like to thank the women and providers who have participated in the current study. The authors would also like to thank additional clinical and research staff, and a range of stakeholders who have informed the development and implementation of the SUMMIT trial.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.12.006.
Appendix. Supplementary materials
References
- Alonso J., Liu Z., Evans-Lacko S., et al. Treatment gap for anxiety disorders is global: Results of the World Mental Health Surveys in 21 countries. Depress. Anxiety. 2018;35(3):195–208. doi: 10.1002/da.22711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson T., McClintock A.S., Himawan L., Song X.X., Patterson C.L. A Prospective Study of Therapist Facilitative Interpersonal Skills as a Predictor of Treatment Outcome. J. Consult. Clin. Psychol. 2016;84(1):57–66. doi: 10.1037/ccp0000060. [DOI] [PubMed] [Google Scholar]
- Boldrini T., Schiano Lomoriello A., Del Corno F., Lingiardi V., Salcuni S. Psychotherapy during COVID-19: How the clinical practice of Italian psychotherapists changed during the pandemic. Front. Psychol. 2020;11:2716. doi: 10.3389/fpsyg.2020.591170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byatt N., Xiao R.S., Dinh K.H., Waring M.E. Mental health care use in relation to depressive symptoms among pregnant women in the USA. Arch. Women’s Ment. Health. 2016;19(1):187–191. doi: 10.1007/s00737-015-0524-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabral R.R., Smith T.B. Racial/ethnic matching of clients and therapists in mental health services: a meta-analytic review of preferences, perceptions, and outcomes. J. Counsel. Psychol. 2011;58(4):537. doi: 10.1037/a0025266. [DOI] [PubMed] [Google Scholar]
- Chang D.F., Berk A. Making cross-racial therapy work: A phenomenological study of clients’ experiences of cross-racial therapy. J. Counsel. Psychol. 2009;56(4):521. doi: 10.1037/a0016905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Selix N., Nosek M. Perinatal anxiety and depression during Covid-19. The Journal for Nurse Practitioners. 2020. [DOI] [PMC free article] [PubMed]
- Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Crowe M., Inder M., Farmar R., Carlyle D. Delivering psychotherapy by video conference in the time of COVID-19: some considerations. J. Psychiatr. Ment. Health Nurs. 2020 doi: 10.1111/jpm.12659. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Van Straten A., Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clin. Psychol. Rev. 2007;27(3):318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- Dimidjian S., Barrera M., Jr., Martell C., Muñoz R.F., Lewinsohn P.M. The origins and current status of behavioral activation treatments for depression. Ann. Rev. Clin. Psychol. 2011;7:1–38. doi: 10.1146/annurev-clinpsy-032210-104535. [DOI] [PubMed] [Google Scholar]
- Dimidjian S., Goodman S.H., Sherwood N.E., et al. A pragmatic randomized clinical trial of behavioral activation for depressed pregnant women. J. Consult. Clin. Psychol. 2017;85(1):26. doi: 10.1037/ccp0000151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. -e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Lacko S., Jarrett M., McCrone P., Thornicroft G. Facilitators and barriers to implementing clinical care pathways. BMC Health Serv. Res. 2010;10(1):1–6. doi: 10.1186/1472-6963-10-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari A.J., Charlson F.J., Norman R.E., et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11) doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S., Greer S. Promoting psychological well-being in the face of serious illness: When theory, research and practice inform each other. Psycho-Oncol. 2000;9(1):11–19. doi: 10.1002/(sici)1099-1611(200001/02)9:1<11::aid-pon424>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Heinrich L.M., Gullone E. The clinical significance of loneliness: A literature review. Clin. Psychol. Rev. 2006;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Hsieh H.-.F., Shannon S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Jacobson N.S., Martell C.R., Dimidjian S. Behavioral activation treatment for depression: Returning to contextual roots. Clin. Psychol. Sci. Pract. 2001;8(3):255–270. [Google Scholar]
- Jankovic J., Parsons J., Jovanović N., et al. Differences in access and utilisation of mental health services in the perinatal period for women from ethnic minorities—A population-based study. BMC Med. 2020;18(1):1–12. doi: 10.1186/s12916-020-01711-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans M.J., Luitel N.P., Garman E., et al. Effectiveness of psychological treatments for depression and alcohol use disorder delivered by community-based counsellors: two pragmatic randomised controlled trials within primary healthcare in Nepal. Br. J. Psychiatry. 2019;215(2):485–493. doi: 10.1192/bjp.2018.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanter J.W., Manos R.C., Bowe W.M., Baruch D.E., Busch A.M., Rusch L.C. What is behavioral activation?: A review of the empirical literature. Clin. Psychol. Rev. 2010;30(6):608–620. doi: 10.1016/j.cpr.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Kazdin A.E. Addressing the treatment gap: A key challenge for extending evidence-based psychosocial interventions. Behav. Res. Ther. 2017;88:7–18. doi: 10.1016/j.brat.2016.06.004. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. -e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laster Pirtle W.N. <? covid19?>Racial Capitalism: A Fundamental Cause of Novel Coronavirus (COVID-19) Pandemic Inequities in the United States. Health Educ. Behav. 2020;47(4):504–508. doi: 10.1177/1090198120922942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitch S., Corbin J.H., Boston-Fisher N., et al. Black lives matter in health promotion: moving from unspoken to outspoken. Health Promot. Int. 2020 doi: 10.1093/heapro/daaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzucchelli T., Kane R., Rees C. Behavioral activation treatments for depression in adults: a meta-analysis and review. Clin. Psychol. Sci. Pract. 2009;16(4):383–411. [Google Scholar]
- Morales D.X., Morales S.A., Beltran T.F. Racial/ethnic disparities in household food insecurity during the covid-19 pandemic: a nationally representative study. J. Rac. Ethnic Health Dispar. 2020:1–15. doi: 10.1007/s40615-020-00892-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee S., Trepka M.J., Pierre-Victor D., Bahelah R., Avent T. Racial/Ethnic Disparities in Antenatal Depression in the United States: A Systematic Review. Matern. Child. Health J. 2016;20(9):1780–1797. doi: 10.1007/s10995-016-1989-x. [DOI] [PubMed] [Google Scholar]
- O’mahen H., Richards D., Woodford J., et al. Netmums: a phase II randomized controlled trial of a guided Internet behavioural activation treatment for postpartum depression. Psychol. Med. 2014;44(08):1675–1689. doi: 10.1017/S0033291713002092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Weobong B., Weiss H.A., Anand A., Bhat B., Katti B.…Fairburn C.G. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. The Lancet. 2017;389(10065):176–185. doi: 10.1016/S0140-6736(16)31589-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purtle J. COVID-19 and mental health equity in the United States. Soc. Psychiatry Psychiatr. Epidemiol. 2020;55(8):969–971. doi: 10.1007/s00127-020-01896-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards D.A., Ekers D., McMillan D., et al. Cost and Outcome of Behavioural Activation versus Cognitive Behavioural Therapy for Depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet North Am. Ed. 2016;388(10047):871–880. doi: 10.1016/S0140-6736(16)31140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salameh T.N., Hall L.A., Crawford T.N., Staten R.R., Hall M.T. Racial/ethnic differences in mental health treatment among a national sample of pregnant women with mental health and/or substance use disorders in the United States. J. Psychosom. Res. 2019;121:74–80. doi: 10.1016/j.jpsychores.2019.03.015. [DOI] [PubMed] [Google Scholar]
- Sambrook Smith M., Lawrence V., Sadler E., Easter A. Barriers to accessing mental health services for women with perinatal mental illness: systematic review and meta-synthesis of qualitative studies in the UK. BMJ Open. 2019;9(1) doi: 10.1136/bmjopen-2018-024803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders R.P., Evans M.H., Joshi P. Developing a process-evaluation plan for assessing health promotion program implementation: a how-to guide. Health Promot. Pract. 2005;6(2):134–147. doi: 10.1177/1524839904273387. [DOI] [PubMed] [Google Scholar]
- Singla D.R., Kohrt B.A., Murray L.K., Anand A., Chorpita B.F., Patel V. Psychological Treatments for the World: Lessons from Low- and Middle-Income Countries. Annu. Rev. Clin. Psychol. 2017;13:149–181. doi: 10.1146/annurev-clinpsy-032816-045217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla D.R., Kumbakumba E. The development and implementation of a theory-informed, integrated mother-child intervention in rural Uganda. Soc. Sci. Med. 2015;147:242–251. doi: 10.1016/j.socscimed.2015.10.069. [DOI] [PubMed] [Google Scholar]
- Singla D.R., Lawson A., Kohrt B., et al. The implementation and effectiveness of non-specialist delivered interventions for perinatal mental health in high-income countries: A systematic review and meta-analysis. JAMA Psychiatry. 2021 doi: 10.1001/jamapsychiatry.2020.4556. accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla D.R., MacKinnon D.P., Fuhr D.C., Sikander S., Rahman A., Patel V. Multiple mediation analysis of the peer-delivered Thinking Healthy Programme for perinatal depression: findings from two parallel, randomised controlled trials. Br. J. Psychiatry. 2021;218(3):143–150. doi: 10.1192/bjp.2019.184. [DOI] [PubMed] [Google Scholar]
- Singla D.R., Meltzer-Brody S.E., Silver R.K., Vigod S.N., Kim J.J., La Porte L.M., Ravitz P., Schiller C.E., Schoueri-Mychasiw N., Hollon S.D., Kiss A., Clark D., Dalfen A.K., Dimidjian S., Gaynes B.N., Katz S.R., Lawson A., Leszcz M., Maunder R.G., Mulsant B.H., Naslund J.A., Reyes-Rodriquez M.L., Stuebe A.M., Dennis C-L., Patel V. Scaling Up Maternal Mental healthcare by Increasing access to Treatment (SUMMIT) through non-specialist providers and telemedicine: a study protocol for a non-inferiority randomized controlled trial. Trials. 2021;22(1):186. doi: 10.1186/s13063-021-05075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G., Chatterji S., Evans-Lacko S., et al. Undertreatment of people with major depressive disorder in 21 countries. Br. J. Psychiatry. 2017;210(2):119–124. doi: 10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold B.E. How important are the common factors in psychotherapy? An update. World Psychiatry. 2015;14(3):270–277. doi: 10.1002/wps.20238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang E., Glazer K.B., Sofaer S., Balbierz A., Howell E.A. Racial and Ethnic Disparities in Severe Maternal Morbidity: A Qualitative Study of Women’s Experiences of Peripartum Care. Womens Health Issues. 2021;31(1):75–81. doi: 10.1016/j.whi.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson H., Harrop D., Walton E., Young A., Soltani H. A systematic review of ethnic minority women’s experiences of perinatal mental health conditions and services in Europe. PLoS One. 2019;14(1) doi: 10.1371/journal.pone.0210587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.-.T., Yang Y., Li W., et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zane N., Sue S., Chang J., et al. Beyond ethnic match: Effects of client–therapist cognitive match in problem perception, coping orientation, and therapy goals on treatment outcomes. J. Community Psychol. 2005;33(5):569–585. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.