Abstract
Objectives
The closure of schools to prevent the spread of COVID-19 prompted concerns of deteriorating lifestyle behaviours, mental health, and wellbeing of children, particularly those in socioeconomically disadvantaged settings. We assessed changes in lifestyle behaviours (physical activity, screen time, eating habits and bed/wake-up times), mental health and wellbeing during the first lockdown in Spring 2020 as perceived by school children from disadvantaged settings, and examined determinants of these changes.
Study design
Cross-sectional study.
Methods
We surveyed 1095 grade 4 to 6 students (age 9–12 years) from 20 schools in socioeconomically disadvantaged communities in northern Canada. Students reported on changes in lifestyle behaviours, mental health and wellbeing during the lockdown. Determinants of these perceived changes were examined in multivariable regression models.
Results
A majority of students reported declines in physical activity, having late bed/wake-up times, and modest improvements in mental health and wellbeing. Many students reported increases rather than decreases in screen time and snacking. Positive attitudes toward being active, eating healthy, going to sleep on time and being healthy were strongly associated with maintaining healthy lifestyle behaviours during the lockdown. Positive attitudes toward active and healthy living and healthy lifestyle behaviours were associated with maintaining positive mental health and wellbeing during the lockdown.
Conclusions
The considerable changes in lifestyle behaviors, superimposed on the pre-existing burden of unhealthy lifestyle behaviours, put this generation of children at increased risk for future chronic disease. Findings call for effective health promotion of active and healthy lifestyles to benefit both physical and mental health.
Keywords: COVID-19, Children, Lifestyle behaviours, Mental health and wellbeing, School health, Public health
Introduction
The COVID-19 pandemic, declared by the World Health Organization on March 11, 2020,1 resulted in the implementation of drastic public health measures that affected large populations of school-aged children.2 , 3 While effective at reducing the viral spread, these measures prompted concerns regarding children's lifestyle behaviours (physical activity, screen time, eating habits and sleep patterns) and mental health and wellbeing.4
Healthy lifestyles, mental health and wellbeing are essential for physical, social and emotional development of children.5 Unhealthy lifestyles and psychological problems at a young age may be difficult to reverse and will track into adulthood,6, 7, 8, 9 thereby predisposing children to a range of chronic diseases and mental illness later in life.10 A recent survey of Canadian parents revealed that only 4.8% of children (5–11 years) and 0.6% of adolescents (12–17 years old) adhered to physical activity and sedentary behaviour recommendations during the early pandemic period, although 71.1% were meeting sleep recommendations.11 In addition, some emerging studies suggest, albeit not consistently, that mental health declined among children during the first COVID-19 lockdown.12, 13, 14
The health and wellbeing of socioeconomically disadvantaged children during the pandemic is of particular concern.15 The prevalence of poor lifestyles and mental illness is already high among these children, and studies report on low adherence to lifestyle recommendations during the lockdown in socioeconomically disadvantaged settings.16 In addition, the pandemic-caused stressors (household food insecurity, parental job loss,17 disruptive family dynamics18) may disproportionally affect the physical and mental health of vulnerable children. To date, existing evidence has come predominantly from online surveys in convenience samples of parents rather than children, and children's perspectives on their lifestyle behaviours, mental health and wellbeing have not yet been heard. Among elementary school children residing in socioeconomically disadvantages communities, we (1) examined the perceived changes in lifestyle behaviours, mental health and wellbeing and (2) assessed the role of attitudes toward active and healthy living and other determinants of these changes.
Methods
During in-person learning in November–December 2020 and January–February 2021, we invited 1340 students in grades 4 to 6 from 20 schools located in British Columbia, Alberta, Manitoba, and Northwest Territories to participate in the survey. All 20 schools are part of the Alberta Project Promoting healthy Living for Everyone (APPLE) in Schools project – an innovative, internationally recognized, not-for-profit health promotion program targeting children from socioeconomically disadvantaged communities. Grounded in a Comprehensive School Health approach, the program promotes healthy lifestyle behaviours, mental health and wellbeing by transforming the school's culture to “make the healthy choice the easy choice”.19 , 20
Data were collected in school during regular class time, with research assistants prompting the survey questions projected on the whiteboard through Zoom. A total of 1095 students completed the survey, with the participation rate of 81.6%. The Health Research Ethics Board of the University of Alberta (Pro00061528) and participating school boards approved all the procedures.
As part of the pandemic response in Canada, in-school learning in all participating schools (among others) was suspended mid-March 2020. Although school buildings were closed, online learning continued for the duration of the 2019/2020 school year. Grade K-6 students were permitted to attend in-person classes when the participating schools re-opened in September 2020 with enhanced public health measures in place (e.g. cohorting, masking, physical distancing)21, 22, 23 and an early and extended Christmas break.
Students were asked to compare their activity levels during the Spring 2020 lockdown with their activity levels before this lockdown with respect to 24 common physical activities derived from the PAQ-C.24 Response categories were adapted to reflect changes in activity levels, as perceived by the students, during the COVID-19 lockdown. Response categories (Less than/About the same/More than before schools got closed) were assigned a score of ‘-1’, ‘0’ and ‘1’, averaged and dichotomized using ‘0’ as the cut-off value, with lower values indicating less physical activity during the lockdown, and ‘0’ and above more physical activity. The same response categories were provided for the questions about perceived changes in time spent playing video games and using a cellphone, and in the number of meals and snacks. With respect to sleep, students reported their wake-up time and bedtime on weekdays. In accordance with the Canadian 24-h Movement Guidelines for children and youth,25 we coded responses for weekday wake-up time after 10:00 am or bedtime after 11:00 pm as having late bed/wake-up times. The surveys included 11 questions related to mental health and wellbeing (details described in our previous work26), with response categories adapted to capture perceived changes during the lockdown (More/About the same/Less than before schools got closed). The response categories were assigned a score of ‘-1’, ‘0’ and ‘1’ for positively stated items and reverse coded for negatively stated items. The cumulative score was created and dichotomized using ‘0’ as the cut-off value, with values above ‘0’ representing better mental health and wellbeing, and between ‘-12’ and ‘0’ (inclusive) worse mental health and wellbeing during the lockdown.
Attitudes toward active and healthy living were assessed by a series of questions: “How much do you care about being healthy? Being physically active? Eating healthy foods? Going to sleep on time?” The response categories were ‘very much’, ‘quite a lot’, ‘a little bit’, and ‘not at all.’ We considered these attitudes as potential determinants of changes in lifestyle behaviours, mental health and wellbeing based on their utility to help prioritize future prevention intervention efforts. Given existing differences in lifestyle behaviours by gender, grade,27 race/ethnicity, and socioeconomical status,28 we considered the student's gender (girl, boy), grade level (4, 5, 6), languages spoken (English only, English and Indigenous language(s), and English and other language(s)), region of residence (rural, small population centre, medium, and large population centre29) as potential confounders. In addition, we adjusted for social and material deprivation indices that were derived from Canada Census 2016 data based on postal codes of APPLE Schools included in the analysis (detailed description of and procedures for calculating these indices can be found elsewhere30). Higher quintiles for both indices indicate more deprived areas.31 , 32 Finally, we considered the length of time since school reopening in September 2020 (<3 months, ≥3 months) as a confounder to account for the possibility that student's lifestyle behaviours and mental health and wellbeing three or more months after reopening could have returned to the pre-pandemic levels.
Statistical analyses
First, multivariable logistic regression models were used to examine the association of the attitudes toward being healthy with perceived changes in physical activity, playing video games, cellphone use, maintaining and adopting good meal and snack routines, not having late bed/wake-up times, and maintaining positive mental health and wellbeing while adjusting for potential confounders. Gender-stratified exploratory factor analysis with varimax (orthogonal) rotation was employed to extract latent factors that maximized the explained variance. After examination of the scree plot and based on the Kaiser criterion (i.e. eigenvalue >1), three clusters were identified separately for girls and boys to reflect gender differences in clustering of the responses (Table S1). Factor scores were then calculated for each of the clusters using the Bartlett's test of sphericity,33 dichotomized and considered as outcomes in the multivariable logistic regression models. Before analyses, missing values were imputed for lifestyle behaviors and mental health and wellbeing based on ‘multivariate imputation by chain equation (MICE)’.34 Approximately 80% of students provided responses to each of the 20 questions (11 questions on mental health and wellbeing, five on screen time, two on eating habits, and two on sleep), and 90% completed at least 19 of the items. Data from 31 students who did not respond to 10 or more of the 20 questions were excluded from analyses. Fixed effects regression modeling was applied instead of mixed effects models since the intra-class correlation was below 0.02 for all models.35 In addition, we considered changes in lifestyle behaviours as potential correlates of changes in mental health and wellbeing.
Results
Table 1 shows the characteristics of the 1095 participants and their schools. There were more girls (n = 557) than boys (n = 538) and more grade 6 (n = 400) relative to grade 4 (n = 312) and 5 (n = 383) students participating. Twenty percent of students reported speaking one or more Indigenous languages and 11% speaking another language in addition to English. In terms of students' attitudes toward active and healthy living, the majority of girls and boys cared ‘very much’ or ‘quite a lot’ about being healthy, physically active and eating healthy, although less than half reported they cared about good sleep.
Table 1.
Characteristics of students and schools that participated in the study, Canada, 2020/21.
| Student Characteristics | Girls (n = 557) |
Boys (n = 538) |
Total (n = 1095) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Grade Level | |||
| Grade 4 | 161 (29) | 151 (28) | 312 (28) |
| Grade 5 | 180 (32) | 203 (38) | 383 (35) |
| Grade 6 | 216 (39) | 184 (34) | 400 (37) |
| Attitudes toward being healthy | |||
| Carea about being healthy | 486 (87) | 460 (85) | 926 (86) |
| Carea about being physically active | 429 (77) | 409 (76) | 838 (77) |
| Carea about eating healthy | 416 (75) | 376 (69) | 792 (72) |
| Carea about good sleep | 268 (49) | 235 (44) | 503 (46) |
| Language(s) spoken | |||
| English only | 387 (69) | 374 (70) | 761 (69) |
| English and Indigenous | 109 (20) | 110 (20) | 219 (20) |
| English and other |
61 (11) |
54 (10) |
115 (11) |
| School characteristics | Schools (n = 20) |
Students (n = 1095) |
|
| n (%) |
n (%) |
||
| Time since reopening | |||
| ≤3 months | 13 (65) | 672 (61) | |
| >3 months | 7 (35) | 423 (39) | |
| Region of residenceb | |||
| Rural | 8 (40) | 165 (15) | |
| Small PC | 7 (35) | 583 (53) | |
| Medium PC | 2 (10) | 188 (17) | |
| Large PC | 3 (15) | 159 (15) | |
| Material deprivation quintile | |||
| 1 (least deprived) | 2 (10) | 66 (6) | |
| 2 | 4 (20) | 222 (20) | |
| 3 | 5 (25) | 447 (41) | |
| 4 | 5 (25) | 291 (27) | |
| 5 (most deprived) | 4 (20) | 69 (6) | |
| Social deprivation quintile | |||
| 1 (least deprived) | 5 (25) | 224 (20) | |
| 2 | 6 (30) | 402 (37) | |
| 3 | 4 (20) | 197 (18) | |
| 4 | 3 (15) | 164 (15) | |
| 5 (most deprived) | 2 (10) | 108 (10) | |
PC: population centre.
Percent of students who responded ‘very much’ or ‘quite a lot’.
Rural refers to a community with <1000 population, small PC to 1000–29,999 population, medium PC to 30,000–99,999, large PC refers to population of 100,000 or more.29
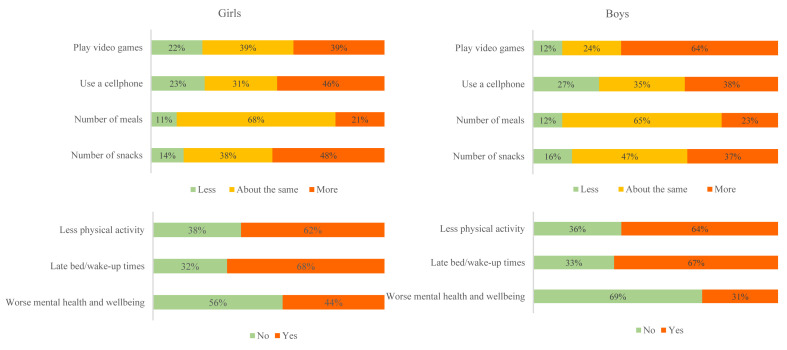
About two-thirds of girls and boys (62% and 64%, respectively) recalled their physical activity levels to be lower during the lockdown than before the lockdown (Fig. 1 ). Almost two-thirds of boys (64%) reported they spent more time playing video games during the lockdown, whereas about one-quarter (24%) reported this to be about the same and 12% spent less time playing video games during the lockdown. Almost half the girls (46%) and more than a third of boys (38%) reported using a cellphone more, 23% and 27% of girls and boys reported using it less than before, and the rest of the students reported no change. Almost half of girls (48%) and 37% of boys reported snacking more than 14% and 16% of girls and boys who reported snacking less during the lockdown. Sixty-eight percent of girls and 67% of boys reported late bed/wake-up times (Fig. 1).
Fig. 1.
Changes in physical activity, time playing video games, time using the cellphones, meal and snack frequency, bed/wake-up times, and mental health and wellbeing during vs before the lockdown.
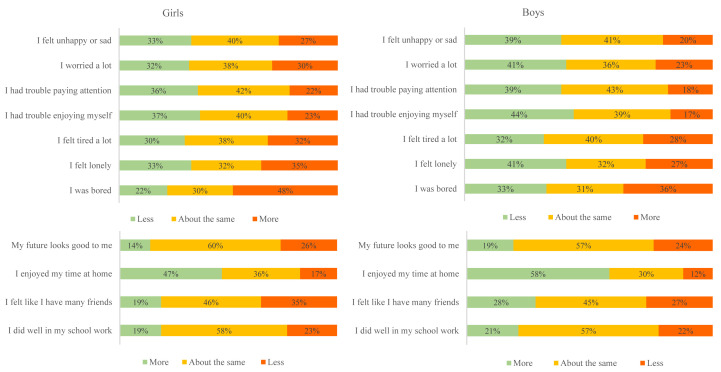
While 44% and 31% of girls and boys perceived, on average, their mental health and wellbeing to be worse, the majority perceived their mental health and wellbeing to be better during the lockdown (Fig. 1). However, responses to the individual questions were mixed (Fig. 2 ). For example, 35% of girls and 27% of boys indicated they felt lonely more often compared to 33% and 41% of girls and boys who felt lonely less often during the lockdown than before the schools got closed. Thirty-two percent of students reported feeling lonely the same as before the lockdown. Almost half of girls (48%) and 36% of boys indicated they were more bored than 22% and 33% of girls and boys reporting they were less bored during the lockdown than before the schools got closed. At the same time, most of girls (47%) and boys (58%) reported enjoying their time at home more than before the lockdown, while the rest enjoyed their time at home less and about the same (Fig. 2).
Fig. 2.
Changes in mental health and wellbeing during vs before the lockdown.
Students who cared about being physically active were more likely to report no increases in time playing video games and using a cellphone and were more likely to maintain positive mental health (Table 2 ). Similarly, those who cared about eating healthy were more likely to report no increases in snacking during the lockdown and were likely to consume same amount or fewer snacks, while those who cared about their sleep and being healthy were less likely to report late bed/wake-up times during the lockdown. Gender-stratified associations are presented in Tables S2 and S3.
Table 2.
Associationsa of attitudes toward active and healthy living with changes in physical activity, sedentary behaviours, healthy eating, sleep, mental health and wellbeing during vs before the lockdown, Canada, 2020/21.
| More physical activity (vs less) |
Same/less time playing video games (vs more) |
Same/less time on cell phone (vs more) |
Same/more meals (vs less) |
Same/fewer snacks (vs more) |
No late bed/wake-up times (vs late) |
Better mental health and wellbeing (vs worse) |
|
|---|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Care about being healthy | |||||||
| A little/not at all | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Very much/quite a lot | 1.12 (0.72, 1.78) | 1.20 (0.77, 1.87) | 0.94 (0.61, 1.42) | 1.39 (0.70, 2.65) | 0.83 (0.53, 1.28) | 1.69 (1.13, 2.51) | 1.13 (0.71, 1.79) |
| Care about being active | |||||||
| A little/not at all | Ref | Ref | Ref | Ref | |||
| Very much/quite a lot | 1.18 (0.83, 1.68) | 2.12 (1.5, 3.00) | 1.86 (1.35, 2.59) | 1.39 (1.06, 1.82) | |||
| Care about eating healthy | |||||||
| A little/not at all | Ref | Ref | Ref | ||||
| Very much/quite a lot | 0.67 (0.39, 1.12) | 1.44 (1.05, 1.98) | 1.29 (0.91, 1.81) | ||||
| Care about good sleep | |||||||
| A little/not at all | Ref | Ref | |||||
| Very much/quite a lot | 2.15 (1.63, 2.84) | 0.85 (0.60, 1.19) | |||||
OR: odds ratio; 95% CI: 95% confidence interval; Ref: reference category.
All estimates are adjusted for the student characteristics (gender, grade level, language(s) spoken) and school/community characteristics (social deprivation, material deprivation, region of residence, and time since reopening of schools).
Table 3, Table 4 report on the associations of changes in lifestyle behaviours with changes in mental health and wellbeing in girls and boys, respectively. Girls who were more physically active during than before the lockdown were less likely to experience ‘internalizing and functioning problems, tiredness and loneliness’ and more likely to have a ‘positive outlook on future and time during lockdown’ relative to those who were less physically active (Table 3). In girls, spending less or the same amount of time playing video games was associated with a higher likelihood of maintaining positive mental health and wellbeing during the lockdown and being bored and lonely. In addition, having more meals was associated with having a ‘positive outlook on future and time during the lockdown’. Similar to girls, boys who were physically active during the lockdown were more likely to have a ‘positive outlook on future and time during the lockdown’. Boys who reported having more meals and fewer snacks were more likely to experience positive mental health and wellbeing during the lockdown (Table 4).
Table 3.
Associations of changes in lifestyle behaviours with changes in mental health and wellbeing and its subgrouping during vs before the lockdown among girls, Canada, 2020/21.
| Better mental health and wellbeing (vs worse) |
Internalizing and functioning problems, tired and lonely (vs not) |
Positive outlook (vs not) |
Bored and lonely (vs not) |
|
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Physical activity | ||||
| Less than before | Ref | Ref | Ref | Ref |
| More than before | 0.66 (0.45, 0.97) | 0.52 (0.36, 0.76) | 1.69 (1.13, 2.55) | 0.81 (0.55, 1.18) |
| Video games | ||||
| Less than/same as before | 1.61 (1.09, 2.37) | 1.25 (0.85, 1.83) | 1.16 (0.78, 1.72) | 1.54 (1.04, 2.27) |
| More than before | Ref | Ref | Ref | Ref |
| Cellphone use | ||||
| Less than/same as before | 1.18 (0.8, 1.73) | 1.01 (0.69, 1.47) | 1.47 (0.99, 2.18) | 1.86 (1.27, 2.73) |
| More than before | Ref | Ref | Ref | Ref |
| Number of meals | ||||
| Less than/same as before | Ref | Ref | Ref | Ref |
| More than before | 1.66 (0.93, 2.99) | 1.02 (0.57, 1.81) | 1.78 (1, 3.18) | 1.42 (0.79, 2.58) |
| Number of snacks | ||||
| Less than/same as before | 1.32 (0.9, 1.94) | 1.3 (0.89, 1.89) | 1.19 (0.81, 1.77) | 1.06 (0.72, 1.54) |
| More than before | Ref | Ref | Ref | Ref |
| Late bed/wake-up times | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 0.74 (0.5, 1.09) | 0.77 (0.52, 1.14) | 0.83 (0.56, 1.24) | 0.67 (0.45, 0.99) |
OR: odds ratio; 95% CI: 95% confidence interval; Ref: reference category.
All estimates are adjusted for the following student characteristics (grade level, language(s) spoken) and school/community characteristics (social deprivation, material deprivation, region of residence, and time since reopening of schools).
Table 4.
Associations of changes in lifestyle behaviours with changes in mental health and wellbeing and its subgrouping during vs before the lockdown among boys, Canada, 2020/21.
| Better mental health and wellbeing (vs worse) |
Bored, tired and lonely (vs not) |
Internalizing and functioning problems (vs not) |
Positive outlook (vs not) |
|
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Physical activity | ||||
| Less than before | Ref | Ref | Ref | Ref |
| More than before | 1.18 (0.77, 1.82) | 1.05 (0.71, 1.54) | 0.69 (0.47, 1.02) | 2.06 (1.39, 3.06) |
| Video games | ||||
| Less than/same as before | 0.82 (0.53, 1.27) | 0.86 (0.57, 1.29) | 1.04 (0.7, 1.56) | 0.65 (0.43, 0.97) |
| More than before | Ref | Ref | Ref | Ref |
| Cellphone use | ||||
| Less than/same as before | 1.2 (0.78, 1.85) | 1.2 (0.81, 1.78) | 1.08 (0.73, 1.59) | 0.8 (0.54, 1.19) |
| More than before | Ref | Ref | Ref | Ref |
| Number of meals | ||||
| Less than/same as before | Ref | Ref | Ref | Ref |
| More than before | 1.92 (1.08, 3.39) | 1.38 (0.8, 2.39) | 1.11 (0.64, 1.92) | 0.9 (0.52, 1.57) |
| Number of snacks | ||||
| Less than/same as before | 1.83 (1.2, 2.78) | 1.31 (0.9, 1.92) | 1.22 (0.83, 1.78) | 1.08 (0.73, 1.59) |
| More than before | Ref | Ref | Ref | Ref |
| Late bed/wake-up times | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 1.44 (0.93, 2.26) | 1.16 (0.78, 1.73) | 1.04 (0.71, 1.55) | 1.11 (0.75, 1.66) |
OR: odds ratio; 95% CI: 95% confidence interval; Ref: reference category.
All estimates are adjusted for the following student characteristics (grade level, language(s) spoken) and school/community characteristics (social deprivation, material deprivation, region of residence, and time since reopening of schools).
Discussion
The present study reported on changes in the lifestyle behaviours and mental health and wellbeing, as perceived by elementary school–aged children living in socioeconomically disadvantaged communities, during the Spring 2020 COVID-19 lockdown. Children reported to be less physically active, to spend more time playing video games (boys) and using cellphones (girls), and to snack more. The majority of students reported having late bed or wake-up times on weekdays during the lockdown. In contrast, the majority of students found their mental health and wellbeing to be better during the lockdown. Moreover, positive attitudes toward being active, eating healthy, going to sleep on time and being healthy were strongly associated with maintaining healthy lifestyle behaviours during the lockdown. Last, positive attitudes were also associated with maintaining positive mental health and wellbeing during the lockdown.
Several studies reported on a considerable disengagement in physical activity during the lockdown.36, 37, 38, 39, 40 While this appears true for most of our respondents, it is noteworthy that changes for the better were reported by more than one-third of girls and boys. In a study of lifestyle behaviours in Irish adolescents (12–18 years old) during the first lockdown,41 20% and 30% of students reported exercising more and about the same, respectively, than 50% exercising less than pre-pandemic. The majority of boys and girls reported an increase in time playing video games and using cellphones, respectively. The decrease in physical activity combined with an increase in screen time is concerning. However, in the context of the pandemic where physical distancing is paramount, and multiple and repeat lockdowns are enforced; sedentary activities that involve peer/social interaction might have favourable effects on emotional wellbeing because students might use video gaming to connect with peers.42 Health promotion messages should seek a balance between encouraging active lifestyles while affording children the opportunities for social interaction through online mediums, particularly those that encourage physical activity (e.g. exergaming).
Participants reported snacking more during the lockdown, which is consistent with emerging literature.43 , 44 Despite the substantial increase in the consumption of processed foods since the start of the pandemic,45 there are also reports that many families used the lockdown as an opportunity to steer their eating habits toward healthier options.46 This underlines the importance of the health promotion initiatives focusing on healthy eating habits in the family setting.
Our findings of late bed/wake-up times during the lockdown are consistent with emerging literature,47 but are not necessarily alarming. Most schools provided flexible school hours during the lockdown, and a shift toward later bedtime among children was shown to be accompanied by longer sleep duration, improved sleep quality and less daytime sleepiness during the lockdown.48 Adopting a flexible school time schedule during the lockdown may help ensure children meet the recommended number of hours of sleep.49
Evidence on the impact of the COVID-19 pandemic on mental health and wellbeing in children is equivocal, and our study also reports mixed findings. While some children reported their mental health and wellbeing to worsen during the lockdown, most students reported positive changes. These results are seemingly not consistent with studies showing modest adverse impact of the pandemic on children and youth's mental health and wellbeing.50 , 51 For example, in a survey of 166 grade 4 students in South Korea, Choi et al.52 reported an increase in stress levels along with unchanged life satisfaction, underscoring the importance of high quality parent–child relationship in supporting children's mental health and wellbeing during the pandemic. Cultural and contextual factors, such as resiliency in small communities in Canada,53 , 54 may also underlie the findings in the current study. All participating schools are part of the APPLE Schools program that takes a Comprehensive School Health approach to promoting healthy lifestyle behaviours and mental wellness. Pre-pandemic research had shown that this program was effective in increasing physical activity levels,55, 56, 57 reducing screen time, improving vegetables and fruit consumption, and preventing excess body weight.58 APPLE Schools continued the delivery of their programming when school buildings were closed, connecting directly with students and parents, sharing resource/activities promoting healthy lifestyle, distributing exercise equipment, providing healthy food hampers, offering online activities (e.g. guided meditations), support from mental health therapists, among others. These activities could have helped students to weather the adverse effects of the lockdown, particularly on mental health and wellbeing given the emphasis of the APPLE Schools programming on promotion of mental health and wellbeing. Moreover, APPLE Schools programming also targets the attitudes of students. In this study, we revealed that students with positive attitudes toward active and healthy living, were more likely to maintain healthy lifestyle behaviors and mental health and wellbeing.
Most of the emerging literature on lifestyle behaviours and mental health and wellbeing of children is based on parental reports, while our study gathered information directly from students. Grade 4 to 6 students have appropriate literacy level to complete surveys and may be better at responding to questions on changes in lifestyle behaviours and mental health and wellbeing than their parents.59 Another strength of this study is a very high response rate achieved by providing flexibility to teachers in scheduling the survey administration and coordinating on the day when most of the students were available. However, there are several limitations, including the cross-sectional design of the study. Longitudinal studies are required to study long-term health impacts that might result from the negative lifestyle changes associated with the pandemic-related public health measures.60 Particular attention should be paid to socioeconomically disadvantaged groups and communities because the pandemic has exacerbated pre-existing inequalities, with evidence emerging that a range of adversities (e.g. financial burden, access to basic necessities) are maintained over time.61 In addition, the surveys were administered several months after the lockdown, which may have affected participants’ recall of the changes in lifestyle behaviours and mental health and wellbeing.
Conclusion
This study in the general population of elementary school–aged children from socioeconomically disadvantaged communities demonstrated considerable changes in physical activity, screen time, eating habits and bed/wake-up times, albeit modest changes in mental health and wellbeing. Considering multiple and repeat lockdowns and the negative changes in lifestyles observed in this study population despite the ongoing APPLE Schools programming, investments in health promotion are critical to avoid a cascade of negative health consequences in the decades ahead.
Author statements
Acknowledgments
The authors thank the students, parents/guardians, and school principals for their participation in the research. They further thank teachers, school health facilitators and champions, project assistants, the APPLE Schools staff for facilitating the research, and specifically Tina Skakun, Katherine Dekker and Landra Walker for their major roles in coordinating and conducting the data collection.
Ethical approval
The Health Research Ethics Board of the University of Alberta (Pro00061528) and participating school boards approved all the procedures.
Funding
The Public Health Agency of Canada (grant #1516-HQ-000071) along with other partners (for details see20) funded the APPLE Schools programming in the Northern communities. The present study was supported by operating funds from the Canadian Institutes for Health Research to KM and PJV (grant #172685). KM holds the Murphy Family Foundation Chair in Early Life Interventions.
Competing interests
The authors have no real or perceived competing interests to disclose.
Authors’ contributions
All listed authors contributed to study design, drafted and revised the article, and gave their final approval of the version submitted for publication. KM and PJV conceptualized the study and methodology, and secured funding and resources. MKAK, KM, and PJV developed a statistical analysis plan, and MKAK conducted all data analyses. JD and PJV accessed and verified the data and wrote the original draft. All authors reviewed and approved the final manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2021.10.007.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization . 11 March 2020. WHO Director-General’s opening remarks at the media briefing on COVID-19.https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available from: [Google Scholar]
- 2.Public Health Agency of Canada . 2021. Community-based measures to mitigate the spread of coronavirus disease (COVID-19) in Canada.https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html Available from: [Google Scholar]
- 3.United Nations . 2020 Aug. Policy brief: education during COVID-19 and beyond.https://www.un.org/development/desa/dspd/wp-content/uploads/sites/22/2020/08/sg_policy_brief_covid-19_and_education_august_2020.pdf Available from: [Google Scholar]
- 4.Zemrani B., Gehri M., Masserey E., Knob C., Pellaton R. A hidden side of the COVID-19 pandemic in children: the double burden of undernutrition and overnutrition. Int J Equity Health. 2021 Jan 22;20(1):44. doi: 10.1186/s12939-021-01390-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macera C.A. Promoting healthy eating and physical activity for a healthier nation. Cent Dis Control Prev. 2005:1–22. [Google Scholar]
- 6.Biddle S.J.H., Pearson N., Ross G.M., Braithwaite R. Tracking of sedentary behaviours of young people: a systematic review. Prev Med. 2010 Nov 1;51(5):345–351. doi: 10.1016/j.ypmed.2010.07.018. [DOI] [PubMed] [Google Scholar]
- 7.Lake A.A., Mathers J.C., Rugg-Gunn A.J., Adamson A.J. Longitudinal change in food habits between adolescence (11–12 years) and adulthood (32–33 years): the ASH30 Study. J Public Health. 2006 Mar 1;28(1):10–16. doi: 10.1093/pubmed/fdi082. [DOI] [PubMed] [Google Scholar]
- 8.Lien N., Lytle L.A., Klepp K.-I. Stability in consumption of fruit, vegetables, and sugary foods in a cohort from age 14 to age 21. Prev Med. 2001 Sep 1;33(3):217–226. doi: 10.1006/pmed.2001.0874. [DOI] [PubMed] [Google Scholar]
- 9.Telama R. Tracking of physical activity from childhood to adulthood: a review. Obes Facts. 2009;2(3):187–195. doi: 10.1159/000222244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loewen O.K., Maximova K., Ekwaru J.P., Faught E.L., Asbridge M., Ohinmaa A., et al. Lifestyle behavior and mental health in early adolescence. Pediatrics. 2019;143(5) doi: 10.1542/peds.2018-3307. [DOI] [PubMed] [Google Scholar]
- 11.Moore S.A., Faulkner G., Rhodes R.E., Brussoni M., Chulak-Bozzer T., Ferguson L.J., et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. J Behav Nutr. 2020;17(1):85. doi: 10.1186/s12966-020-00987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bignardi G., Dalmaijer E.S., Anwyl-Irvine A.L., Smith T.A., Siugzdaite R., Uh S., et al. Longitudinal increases in childhood depression symptoms during the COVID-19 lockdown. Arch Dis Child. 2020 Dec 9:1–7. doi: 10.1136/archdischild-2020-320372. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cost K.T., Crosbie J., Anagnostou E., Birken C.S., Charach A., Monga S., et al. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatr. 2021 Feb 26:1–14. doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ravens-Sieberer U., Kaman A., Erhart M., Devine J., Schlack R., Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatr. 2021 Jan:1–11. doi: 10.1007/s00787-021-01726-5. https://doi: 10.1007/s00787-021-01726-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bambra C., Riordan R., Ford J., Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020 Nov 1;74(11):964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guerrero M.D., Vanderloo L.M., Rhodes R.E., Faulkner G., Moore S.A., Tremblay M.S. Canadian children's and youth's adherence to the 24-h movement guidelines during the COVID-19 pandemic: a decision tree analysis. J Sport. 2020;9(4):313–321. doi: 10.1016/j.jshs.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Statistica Canada . 2020. Labour market impacts of COVID-19 on Indigenous people: March to August 2020.https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00085-eng.htm Available from: [Google Scholar]
- 18.Gassman-Pines A., Ananat E.O., Fitz-Henley J., 2nd COVID-19 and parent-child psychological well-being. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-007294. e2020007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan-Canadian Joint Consortium for School Health . 2016. Comprehensive school health framework.http://www.jcsh-cces.ca/images/What_is_Comprehensive_School_Health_-_2-pager_-_July_2016.pdf Available from: [Google Scholar]
- 20.APPLE Schools . 2021. APPLE Schools is an innovative school-focused health promotion initiative.https://www.appleschools.ca/ Available from: [Google Scholar]
- 21.Alberta Government . 2020 Aug. School re-entry plan.https://open.alberta.ca/dataset/a3910dd5-d52f-4a7d-821f-a381002419e9/resource/03c07743-31bc-46d1-9c65-b39335c4f3ad/download/edu-2020-2021-school-re-entry-plan-2020-0827.pdf Available from: [Google Scholar]
- 22.Manitoba Government . 2020 Jun. Welcoming our students back: restoring safe schools.https://www.gov.mb.ca/asset_library/en/covid/k-12-reopeningplan.pdf Available from: [Google Scholar]
- 23.Government of Northwest Territories. Reopening NWT schools safely. Available from: https://www.gov.nt.ca/covid-19/sites/covid/files/resources/reopening_nwt_schools_safely_plan_for_2020-21_eng.pdf.
- 24.Kowalski K.C., Crocker P.R.E., Donen R.M. College of Kinesiology, University of Saskatchewan; Saskatoon: 2004. The physical activity questionnaire for older children (PAQ-C) and adolescents (PAQ-A) manual. Saskatoon, Saskatchewan, Canada; pp. 1–37. [Google Scholar]
- 25.Tremblay M.S., Carson V., Chaput J.-P., Connor Gorber S., Dinh T., Duggan M., et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metabol. 2016 Jun;41(6):S311–S327. doi: 10.1139/apnm-2016-0151. Suppl. 3. [DOI] [PubMed] [Google Scholar]
- 26.Maximova K., Khan M.K.A., Austin S.B., Kirk S.F.L., Veugelers P.J. The role of underestimating body size for self-esteem and self-efficacy among grade five children in Canada. Ann Epidemiol. 2015 Oct 1;25(10):753–759. doi: 10.1016/j.annepidem.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 27.Public Health Agency of Canada . 2016 Mar. Health behaviour in school-aged children in Canada: focus on relationships.https://healthycanadians.gc.ca/publications/science-research-sciences-recherches/health-behaviour-children-canada-2015-comportements-sante-jeunes/index-eng.php#c6 Available from: [Google Scholar]
- 28.Armstrong S., Wong C.A., Perrin E., Page S., Sibley L., Skinner A. Association of physical activity with income, race/ethnicity, and sex among adolescents and young adults in the United States: findings from the National Health and Nutrition Examination Survey, 2007-2016. JAMA Pediatr. 2018 Aug 1;172(8):732–740. doi: 10.1001/jamapediatrics.2018.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Statistics Canada . 2017. Population centre and rural area classification 2016.https://www.statcan.gc.ca/eng/subjects/standard/pcrac/2016/introduction Available from: [Google Scholar]
- 30.Institut National de Santé Publique du Québec . 2019. Material and social deprivation index.https://www.inspq.qc.ca/en/deprivation/material-and-social-deprivation-index Available from: [Google Scholar]
- 31.Pampalon R., Raymond G. A deprivation index for health and welfare planning in Quebec. Chron Dis Can. 2000;21(3):104–113. [PubMed] [Google Scholar]
- 32.Pampalon R., Hamel D., Gamache P., Simpson A., Philibert M.D. Validation of a deprivation index for public health: a complex exercise illustrated by the Quebec index. CDIC. 2014;34(1) https://www.canada.ca/en/public-health/services/reports-publications/health-promotion-chronic-disease-prevention-canada-research-policy-practice/vol-34-no-1-2014/validation-deprivation-public-health-complex-exercise-illustrated-quebec.html Available from: [PubMed] [Google Scholar]
- 33.Bartholomew D.J., Deary I.J., Lawn M. The origin of factor scores: Spearman, Thomson and Bartlett. Br J Math Stat Psychol. 2009;62(3):569–582. doi: 10.1348/000711008X365676. [DOI] [PubMed] [Google Scholar]
- 34.van Buuren S., Groothuis-Oudshoorn K. MICE: multivariate imputation by chained equations in R. J Stat Software. 2011;45(3):1–67. [Google Scholar]
- 35.Clark T.S., Linzer D.A. Should I use fixed or random effects? Polit Sci Res Methods. 2015;3(2):399–408. [Google Scholar]
- 36.Zhang X., Zhu W., Kang S., Qiu L., Lu Z., Sun Y. Association between physical activity and mood states of children and adolescents in social isolation during the COVID-19 epidemic. J Environ Res. 2020;17(20):7666. doi: 10.3390/ijerph17207666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reece L.J., Owen K., Foley B., Rose C., Bellew B., Bauman A. Understanding the impact of COVID-19 on children's physical activity levels in NSW, Australia. J Aust. 2020 Nov doi: 10.1002/hpja.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tulchin-Francis K., Stevens W.J., Gu X., Zhang T., Roberts H., Keller J., et al. The impact of the coronavirus disease 2019 pandemic on physical activity in US children. J Sport Health Sci. 2021 May;10(3):323–332. doi: 10.1016/j.jshs.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Medrano M., Cadenas-Sanchez C., Oses M., Arenaza L., Amasene M., Labayen I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: a longitudinal analysis from the MUGI project. Pediatr Obes. 2021;16(4):e12731. doi: 10.1111/ijpo.12731. [DOI] [PubMed] [Google Scholar]
- 40.Xiang M., Zhang Z., Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020 Aug;63(4):531–532. doi: 10.1016/j.pcad.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ng K., Cooper J., McHale F., Clifford J., Woods C. Barriers and facilitators to changes in adolescent physical activity during COVID-19. BMJ Open Sport Exerc Med. 2020;6(1):e000919. doi: 10.1136/bmjsem-2020-000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maunula L. Canadian Public Health Association Forum; 2021 Apr 22. Doing research in schools during the COVID-19 pandemic. What did we hear from students and parents in semi-structured interviews?https://www.cpha.ca/publichealth2021-program Online. Available from: [Google Scholar]
- 43.Adams E.L., Caccavale L.J., Smith D., Bean M.K. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity. 2020;28(11):2056–2063. doi: 10.1002/oby.22996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ruiz-Roso M.B., de Carvalho Padilha P., Matilla-Escalante D.C., Brun P., Ulloa N., Acevedo-Correa D., et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during Covid-19 pandemic: an observational study. Nutrients. 2020 Jul;12(8):2289. doi: 10.3390/nu12082289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Janssen M., Chang B.P.I., Hristov H., Pravst I., Profeta A., Millard J. Changes in food consumption during the COVID-19 pandemic: analysis of consumer survey data from the first lockdown period in Denmark, Germany, and Slovenia. Front Nutr. 2021;1:635859. doi: 10.3389/fnut.2021.635859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carroll N., Sadowski A., Laila A., Hruska V., Nixon M., Ma D.W.L., et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020 Aug;12(8):2352. doi: 10.3390/nu12082352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou S.-J., Wang L.-L., Yang R., Yang X.-J., Zhang L.-G., Guo Z.-C., et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020;1:39–47. doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gruber R., Saha S., Somerville G., Boursier J., Wise M.S. The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. 2020;1:33–35. doi: 10.1016/j.sleep.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lim M.T.C., Ramamurthy M.B., Aishworiya R., Rajgor D.D., Tran A.P., Hiriyur P., et al. School closure during the coronavirus disease 2019 (COVID-19) pandemic – impact on children's sleep. Sleep Med. 2021 Feb 1;78:108–114. doi: 10.1016/j.sleep.2020.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bélanger R.E., Patte K.A., Leatherdale S.T., Gansaonré R.J., Haddad S. An impact analysis of the early months of the COVID-19 pandemic on mental health in a prospective cohort of Canadian adolescents. J Adolesc Health. 2021 doi: 10.1016/j.jadohealth.2021.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Penner F., Ortiz J.H., Sharp C. Change in youth mental health during the COVID-19 pandemic in a majority Hispanic/Latinx US sample. J Am Acad Child Adolesc Psychiatry. 2021 Apr;60(4):513–523. doi: 10.1016/j.jaac.2020.12.027. [DOI] [PubMed] [Google Scholar]
- 52.Choi J., Park Y., Kim H.-E., Song J., Lee D., Lee E., et al. Daily life changes and life satisfaction among Korean school-aged children in the COVID-19 pandemic. Int J Environ Res Publ Health. 2021 Mar 23;18:3324. doi: 10.3390/ijerph18063324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kirmayer L., Sehdev M., Whitley R., Dandeneau S., Isaac C. Community resilience: models, metaphors and measures. J Aborig Health. 2009:62–117. [Google Scholar]
- 54.Peters P.A. Broadening the narrative on rural health: from disadvantage to resilience. Univ Toronto Med J. 2019;96(2):41–43. [Google Scholar]
- 55.Vander Ploeg K.A., McGavock J., Maximova K., Veugelers P.J. School-based health promotion and physical activity during and after school hours. Pediatrics. 2014 Feb 1;133(2):e371–e378. doi: 10.1542/peds.2013-2383. [DOI] [PubMed] [Google Scholar]
- 56.Vander Ploeg K.A., Maximova K., McGavock J., Davis W., Veugelers P. Do school-based physical activity interventions increase or reduce inequalities in health? Soc Sci Med. 2014 Jul;112:80–87. doi: 10.1016/j.socscimed.2014.04.032. [DOI] [PubMed] [Google Scholar]
- 57.Bastian K.A., Maximova K., McGavock J., Veugelers P. Does school-based health promotion affect physical activity on weekends? And, does it reach those students most in need of health promotion? Ozakinci G, editor. PLOS ONE. 2015 Oct 21;10(10) doi: 10.1371/journal.pone.0137987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fung C., Kuhle S., Lu C., Purcell M., Schwartz M., Storey K., et al. From “best practice” to “next practice”: the effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity. Int J Behav Nutr Phys Act. 2012;9(1):27. doi: 10.1186/1479-5868-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sithole F., Veugelers P. 2015. Health reports: parent and child reports of children’s activity.https://www150.statcan.gc.ca/n1/pub/82-003-x/2008003/article/10662-eng.htm Available from: [PubMed] [Google Scholar]
- 60.Munasinghe S., Sperandei S., Freebairn L., Conroy E., Jani H., Marjanovic S., et al. The impact of physical distancing policies during the COVID-19 pandemic on health and well-being among Australian adolescents. J Adolesc Health. 2020 Nov;67(5):653–661. doi: 10.1016/j.jadohealth.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wright L., Steptoe A., Fancourt D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J Epidemiol. 2020;74(9):683–688. doi: 10.1136/jech-2020-214475. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.