Abstract
Context:
Throwing-related injuries occur commonly in softball players. Preventative programs can be implemented to assist in identifying and correcting risk factors that could potentially lead to injury and therefore time missed from both practice and games.
Objective:
The purpose of this study was to determine if position-specific injury prevention programs have been developed to decrease the risk of throwing-related injuries in softball players.
Data Sources:
A systematic review was performed using the PRISMA (Preferred Reporting Items of Systematic Reviews and Meta-Analyses) guidelines. PubMed, PMC, and EBSCO were searched for articles on injury prevention programs using the following key terms: softball, injury prevention, throwing injuries, pitcher, and shoulder.
Study Selection:
Studies that involved fast-pitch softball and included female participants as well as rehabilitation programs were included. Articles that highlighted slow-pitch softball or did not include female participants were excluded.
Level of Evidence:
Level 1.
Data Extraction:
The initial search identified 1605 articles. After implementing a filter, 131 articles remained. Thirteen articles were screened out as duplicates. After screening for inclusion criteria, 7 articles remained and were included in the systematic review.
Results:
Decreased range of motion (ROM) in both the upper and the lower extremities, unbalanced muscular strength, and fatigue were identified as risk factors for throwing injuries in softball players. Within the upper extremity, strength and ROM of the rotator cuff muscles, biceps, and extensors of the forearm were emphasized. The main focus of the lower extremity was the strength of the gluteal muscles and ROM of the lumbopelvic-hip complex. Only 1 study detailed an injury prevention program for softball players. The prevention program outlined was generalized for all softball players and was not position specific.
Conclusion:
There is a paucity of information about injury prevention programs for softball players. Of the evidence analyzed, balanced strengthening of the upper and lower extremities while maintaining dynamic range of motion was frequently utilized in developing an injury prevention program.
Keywords: injury prevention, softball, throwing injury
Softball is currently one of the largest team sports in the United States, with more than 2 million female athletes between the ages of 12 and 18 years participating. 13 Fast-pitch softball is a game dominated and controlled by the pitcher, similar to baseball, but with a few key differences. In softball, there is no mound, so athletes are throwing from a flat surface. This is opposed to baseball, where pitchers throw from an elevated mound. The second and most pivotal difference is in how each player is managed with regard to pitch count restrictions. Across all levels of baseball, there are restrictions limiting the number of pitches or innings played by an individual over the course of a week. According to the official Little League guidelines, youth baseball pitchers should not throw more than 95 pitches in a day with 4 days rest between. 8 A list of pitching restrictions for high school students outlined by the National Federation of State High School Association and highlighted in the Baseball America newsletter shows the variable state-specific restrictions on pitch count. However, most pitch count restrictions range between 105 and 120 pitches with 3 days of rest between. 4 Despite pitching guidelines for softball that resemble baseball pitching restrictions, there is no official pitch count limit; therefore, softball pitchers often throw a number of pitches substantially above the suggested limit in a very short time frame. In a blog article submitted to Shoulder Made Simple, the maximum pitch count for a softball player at the age of 15 years should be 140 pitches over a 2-day period, pitching 1 game each day. After these 140 pitches, 2 days of rest is suggested to allow recovery and prevent throwing-related injuries. 2 Additionally, general pitching guidelines for various age groups can be found in a blog post from the AOSSM in their Stop Sports Injuries campaign (Table 1). 7 A study by Werner et al 20 found that during a tournament, youth softball pitchers can throw upward of 2000 pitches in the span of 3 days, while pitching multiple games each day. This is worrisome, as a study by Patel et al 9 demonstrated that the rate of injury for pitchers increases by 5% with each additional 100 pitches thrown throughout the season.
Table 1.
Maximum pitch counts 7
| Age, y | Pitches/Game | Pitches/Day (Days 1-2) | Pitches/Day (Day 3) |
|---|---|---|---|
| 8-9 | 50 | 80 | 0 |
| 10-12 | 65 | 95 | 0 |
| 13-14 | 80 | 115 | 80 |
| ≥15 | 100 | 140 | 100 |
The differences in pitching mechanics between softball and baseball have been largely responsible for the lack of pitching restrictions implemented for softball players. Although the pitching mechanisms are different, similar forces are placed on the throwing arm. 1 In baseball’s overhead pitch, the greatest resistance to force is generated during the deceleration phase, after the ball has left the pitcher’s hand, as opposed to the windmill pitch, which generates the majority of its resistance during the delivery phase, as the pitcher is releasing the ball. 1 Although the forces were slightly higher with the overhead pitching mechanism, the windmill pitch generated much more torque, particularly during abduction and extension. 1
The perception that the windmill pitch has a lower risk of injury has caused throwing-related injuries in softball, particularly affecting pitchers. A study found that among 48 pitchers, there were 18 injuries (37.5%) directly attributed to pitching. 17 Eleven of the 18 injuries (61%) involved the shoulder. Pitchers had a 2.1 (95% CI, 0.94-4.6) times higher risk of injury lasting longer than 2 weeks as compared with position players. 18 To further challenge this perception, the incidence of injury was higher in youth softball players (5.6/1000 athlete-exposures) than in baseball players (4.0/1000 athlete-exposures), with the majority of injuries manifesting in pitchers (37.3%) compared with position players (15.3%). 15
In adolescent softball players ranging from ages 11 to 15 years, anterior shoulder pain related to rotator cuff/biceps pathology and labral pathology were the most common in 13- to 15-year-old softball windmill pitchers, when compared among all adolescent high school softball players. 17 Epicondylar injuries in softball position players also commonly occur (incidence of up to 39%) with the highest percentage of injury occurring in high school players between the ages of 14 and 18 years. 16 Softball position players commonly present with reduced range of motion, increased glenohumeral joint laxity, and anterior shoulder pain. 17
As softball players progress in age, technique, and competition difficulty, pitchers and position players display different injury patterns. In a web-based injury surveillance study focusing on the epidemiology of high school and collegiate softball injuries, it was found that high school softball pitchers were most at risk for upper leg and thigh injuries and collegiate softball pitchers were most at risk for trunk and shoulder strains when assessed for noncontact injuries. 19 In National Professional Fast-Pitch Softball teams, it was found that the majority of position players suffered injuries acutely (59%), while the majority of pitching injuries occurred from overuse injuries that may or may not be related to other chronic injuries (62%). 9
Coaches, athletic trainers, physicians, and physical therapists should maintain a multifocal and individualized injury prevention program. 17 The purpose of this systematic review was to determine if position-specific injury prevention programs have been developed to decrease the risk of throwing-related injuries in softball players.
Methods
A systematic review of the literature was performed in accordance with the guidelines set by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses). A complete initial search of PubMed, PMC, and EBSCO databases was conducted June 28 through July 1, 2019, using various combinations of the keywords softball injury, shoulder, and throwing. This was performed under a specific filter adjusted as follows: ((“injury”[All Fields] AND prevention”[All Fields]) OR “injury prevention”[All Fields]) AND (“baseball”[Medical Subject Headings Terms] OR “baseball”[All Fields] OR “softball”[All Fields]).
Studies were included if they were published in the English language and contained female softball players. The titles were screened, and duplicates were removed. The remaining abstracts were then evaluated for inclusion. Full text of all relevant articles meeting the inclusion criteria were reviewed. Articles included in the systematic review described prevention programs for pitchers and position players in fast-pitch softball of various levels. Studies included clearly proposed preventative measures to help limit the frequency of throwing-related injuries in softball players. Studies that referenced rehabilitation programs were also included if a “return to play” criterion was outlined showing risk factors for both healthy and previously injured softball players. Articles ranging from level 2 to level 4 evidence were included in the review. 3 The 7 studies selected were then assessed for their internal validity using the Newcastle-Ottawa Quality Assessment Scale. This scale measures selection bias, comparability, and outcomes assessing retention and follow-up time. The 7 studies averaged a score of 6.86 out of 9 total points. Studies were excluded if they focused on slow-pitch softball, had a study population mainly consisting of male participants, or exclusively focused on overhead athletes that were not in a mixed study of baseball and softball players.
Results
The initial search of all 3 databases identified a total of 1605 articles. After applying the search term filter, a total of 131 articles remained. Of the 131 articles, 13 were removed for being duplicates. Another 108 articles were screened out based on title, abstract, and inclusion criteria, leaving 10 articles eligible for a full-text review. After a thorough review, 6 articles remained eligible and 1 was added from the reference section, for a total of 7 studies that were included in this review (Figure 1). The eligible articles focused on preventative and rehabilitative programs for throwing-related injuries that manifested in both the lower and the upper extremities of softball pitchers and position players. Range of motion (ROM) and strength were found to be the most important risk factors for potential injury in the shoulder complex, gluteal muscles, and lumbopelvic hip complex. Target muscle groups that would increase prevention of throwing-related injury were referenced in all the studies; however, only 1 article described a full injury prevention program.
Figure 1.
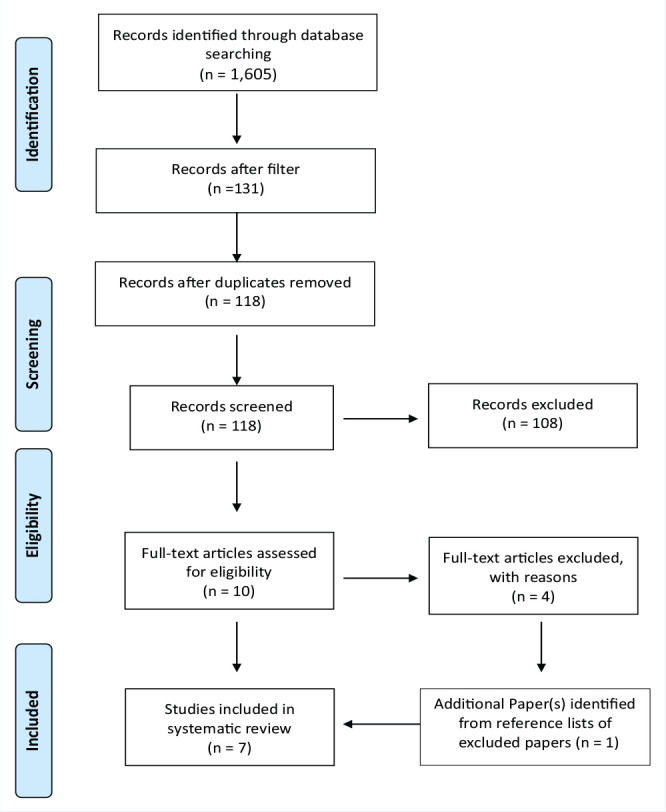
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for article review.
Patient Demographics
The 7 articles included a total of 264 female softball players between the ages of 9 and 26 years (Table 2). It is important to note that 179 of 264 softball players (67.8%) were from a single study. 6 Mean age was assessed in 2 (28.5%) of the 7 articles with an average age of 14.5 years.13,14 Participants in 2 studies ranged in age from 18 to 26 years.5,6 In another 2 studies, age of the athletes was not specified.10,12 Finally, in 1 study, the age ranged from 11 to 21 years. 13 Two studies (28.5%) focused on youth recreational softball,13,14 2 studies (28.5%) focused strictly on collegiate or semiprofessional softball players,5,6 2 studies (28.5%) focused on all ages (ranging from ages 11-26 years),10,11 and 1 study (14%) did not specify level of play. 12 Six of the articles (86%) focused primarily on softball pitchers,6,10-14 and 1 article (14%) focused on softball position players. 5
Table 2.
Results from the 7 articles included in the systematic review
| Study | No. of Athletes | Age Range, y | Mean Age, y | Level of Play | Position | ROM Studied | Target Muscles for Strength and ROM |
|---|---|---|---|---|---|---|---|
| Hibberd et al 5 | 35 | 18-26 | N/A | Collegiate | Position players | Upper extremity | Shoulder complex |
| Hill et al 6 | 179 | 18-26 | N/A | Collegiate | Pitchers | Upper extremity | Shoulder complex |
| Oliver 10 | N/A | N/A | N/A | All levels | Pitchers | Lower extremity | Gluteal muscles, core, and postural muscles |
| Oliver et al 11 | 17 | 11-21 | N/A | All levels | Pitchers | Upper extremity | Entire arm segment |
| Oliver and McKeon 12 | N/A | N/A | N/A | N/A | Pitchers | N/A | Gluteal muscles and lumbopelvic-hip complex |
| Oliver and Plummer 13 | 10 | 14-21 | 17.6 | Youth recreation | Pitchers | Lower extremity | Gluteal muscles, lumbopelvic-hip complex |
| Oliver et al 14 | 23 | 9-12 | 11.4 | Youth recreation | Pitchers | Lower extremity | Lumbopelvic-hip complex and trunk |
N/A, not available; ROM, range of motion.
Overview of the Kinetic Chain
It is important to note the significance of the kinetic chain as it explains the sequential distribution of kinematic forces that are similar in both the overhand throw and the windmill pitch. 13 These forces display a proximal-to-distal neuromuscular pattern initiated by the lower extremities and are followed by activation of the upper extremity. 13 Proper transfer of kinematic force, starting with the activation of the gluteal muscles controlling the pelvis through the trunk, shoulder, elbow, and wrist, is essential in the prevention of throwing-related injury. 13 The kinetic chain in both overhand throwing and windmill pitching demonstrates the necessary relationship between the upper and lower extremities needed to create a balanced throwing-related injury prevention program for softball players.
Upper Extremity
Three articles (43%) focused on the upper extremity, specifically the rotator cuff muscles, biceps, extensors of the forearm, and associated ROM of the shoulder (Table 2).5,6,12 A study by Oliver and McKeon 12 in 2010 evaluated the risk of throwing-related injuries in recreational, competitive, and elite softball pitchers. The authors found that novice pitchers rely more on their upper arm segment (ie, muscles from the shoulder to the elbow) during the pitching motion. This was in comparison with their intermediate and elite counterparts, who relied more on the distal arm segment, which consists of the muscles from the elbow to the wrist and lower extremities to generate throwing power. 12 This was postulated to increase the risk of potential throwing-related injuries for novice softball pitchers. The study emphasized improper throwing technique as a major risk factor for shoulder injury. Two articles (67%) found that biceps and rotator cuff weakness or fatigue and shoulder ROM deficits were common risk factors for throwing-related injuries in both position players and pitchers at the collegiate level.5,6 A 2014 study by Hibberd et al 5 focused on dominant limb range of motion and humeral-retrotorsion adaptation in baseball and softball players. 5 This study highlighted risk factors for throwing-related injuries in softball position players at the collegiate level that utilize the overhead throwing motion similarly to baseball pitchers and position players. The authors found that glenohumeral joint internal rotation in uninjured softball position players did not significantly differ from their female, nonoverhead athlete control counterparts. 5
Lower Extremity
Three articles (43%) concentrated on how the lower extremities can contribute to the risk for throwing-related injuries (Table 2). All 3 studies focused particularly on the risk of injury associated with the gluteal muscles of the leg used to lunge while in the pitching motion, ROM of the hips and pelvis, and trunk stabilization.10,13,14 Each of these articles highlighted gluteal muscle activation in phase 3, or the lunge component of the pitching motion, as a risk factor for potential throwing-related injuries in softball pitchers.10,13,14 Two articles (67%) focused on trunk and core activation and shoulder ROM as major stabilizers of the lower extremities in all 3 phases of the throwing motion.10,14 Fatigue and lack of balanced muscular strength in the gluteal muscles and trunk were found to increase the risk of potential throwing-related injury, and it was recommended that these components be the main focus of injury prevention programs.10,13,14
Injury Prevention Programs for Softball Players
Articles specifically mentioned neither the amount of time that should be devoted to rehabilitative or prevention programs nor the time when injury prevention exercises should be incorporated (eg, in-season/off-season). All 7 articles (100%) agreed that injury prevention programs need to be individualized to the player by considering the athlete’s baseline strength, ROM, and playing position.5,6,10-14 Although each of the articles mentioned specific exercises that could increase ROM and strength in the upper or lower extremities, only 1 article described an injury prevention program for softball players, specifically pitchers (Table 3). 10 This article focused on dynamic stretches to increase flexibility as well as exercises to specifically strengthen the gluteal muscles and lumbopelvic-hip complex. 10
Table 3.
Softball-specific exercise information for injury prevention and rehabilitation
| Study | Specific Exercise Program | Exercises | Training Focus |
|---|---|---|---|
| Hibberd et al 5 | No | N/A | Using specific injury mechanisms to guide injury prevention programs, specifically in the shoulder complex |
| Hill et al 6 | No | N/A | • Position specific • Muscle groups that will prevent muscular imbalance such as the rotator cuff |
| Oliver 10 | Yes | • Front-plank isometric exercises with contralateral leg and arm extension • “Bird-dog” exercise—coactivation of hip extensors, longissimus muscles, scapular stabilizers, and shoulder flexors • Side-lying resisted hip abduction |
• Entire kinetic chain of the windmill pitching motion • Pitching specific • Dynamic strengthening |
| Oliver et al 11 | No | N/A | • Entire kinetic chain of throwing motion, specifically the forearm, shoulder, and wrist • Begin with strengthening the trunk and move outward |
| Oliver and McKeon 12 | No | Gluteal extension with core stabilization | • Entire kinetic chain of the throwing motion, specifically on pelvic and scapular stability • Start with strengthening the lumbopelvic complex, specifically the abdominal muscles, holding the pelvis in the neutral position • After the core is engaged, work on gluteal muscle strengthening, prioritizing dynamic gluteal extension |
| Oliver and Plummer 13 | No | N/A | Strength and functionality of the lumbopelvic hip complex |
| Oliver et al 14 | No | N/A | Overhead movements while stabilizing the lumbopelvic complex |
N/A, not available.
Discussion
There is currently no well-defined injury prevention program for softball pitchers or position players. Based on the articles in this study, it is unclear whether focusing on the upper body or lower body is more effective in preventing throwing-related injuries in softball players. Six of the articles (86%) cited decreased ROM of the lumbopelvic-hip complex and shoulder complex in relation to internal/external rotation and abduction, as potential risk factors attributed to injury during the season.5,6,10,11,13,14 The lack of regulations regarding pitch count, season duration, and athletes transitioning to year-round play have all contributed to the injuries most commonly seen in softball players. According to Shanley et al 16 and Shanley and Thigpen, 17 the most common injury for both adolescent pitchers and position players is strains to either the leg (unspecified region) or the shoulder complex. A study by Wasserman et al 19 demonstrated that in high school softball pitchers, upper leg and thigh strains are the predominant injury with an incidence of 9.4% of all injuries. This is in contrast to collegiate softball pitchers, where common injuries were trunk and shoulder strains that accounted for 9.5% of total injuries. Noncontact throwing injuries were also analyzed for both high school and collegiate softball position players. The incidence of noncontact throwing injury in high school position players was 13.8% in practice and 4.2% in games. This is in contrast to the incidence of collegiate throwing injury in position players that was 14.8% in practice and 4.7% in games. 19 These injury patterns further emphasize the importance of an injury prevention program that focuses on improving strength and maintaining ROM in the upper and lower extremities to decrease the risk of potential throwing-related injuries.
Another important factor to note was the balance between increasing the strength of particular muscle groups and maintaining ROM with passive and dynamic stretching. Wilk et al 21 agree that maintaining balanced muscular conditioning and ROM can largely decrease the common injuries seen in overhead athletes and are necessary for an effective preventative or rehabilitative program. 21 These conditioning combinations can limit potential rotator cuff tears by decreasing muscular tightness that may lead to muscular imbalance because of the high tensile load during the throwing phase. 21 Maintaining muscular strength and ROM can also help prevent superior labral tear from anterior to posterior lesions and lumbopelvic-hip complex strains that also include the gluteal muscles. 21 The previously mentioned injuries are associated with a greater loss of time from practice, ranging from 15 to 45 more days, and greater loss of time from games, which ranged from 5 to 24 more games, depending on the severity of the injury. 12 Generally, these injuries occur within the first few months of the season. If they occur later in the season, these injuries are attributed to overuse.16,21 These factors underscore the importance of having an off-season injury prevention program that incorporates strength training and maintenance of ROM as an essential factor in limiting throwing injuries in fast-pitch softball players. None of the articles included in this study clearly defined the time when the prevention program should be implemented, either in season or out of season.
While the information regarding what muscles should be targeted within a prevention program is important for decreasing the risk of potential injury, we cannot ignore the fact that overuse injuries (eg, rotator cuff tendinitis/tendinopathy/bursitis) will be difficult to avoid because of the lack of pitching regulation in the sport.16,21 Wilk et al 21 and Shanley et al 16 ascertain that without pitching regulations for softball players, the preventative exercises that increase strength and maintain ROM will have limited success. These recommendations have been outlined by the AOSSM: Stop Sports Injuries Campaign (Table 1). 7
Limitations
There are several limitations to this systematic review. First, the evidence level of the included articles ranged from levels 2 to 4. This limits the conclusions drawn from studies without controls. The second and most important limitation is the lack of information regarding a program that details specific exercises and stretches, time frame (in-season and off-season), and position-based modality that can be used for injury prevention. Finally, there were only 7 articles eligible for this systematic review.
Conclusion
There is a paucity of information about injury prevention programs for softball players. Increasing strength and maintaining ROM in both the upper and lower extremities is important to prevent throwing injuries in softball pitchers and position players. The numerous ways softball players sustain throwing-related injuries suggests that prevention programs should be tailored individually to address specific deficits in muscle balance or strength. Further research is needed to clearly define an injury prevention program with optimal exercises, recommended duration, and timing of program implementation to decrease the risk of throwing-related injuries in softball players.
Footnotes
The following author declared potential conflicts of interest: M.K.M. reports personal fees from AAOS, ACSM Transitional Journal, American Orthopaedic Society for Sports Medicine, Arthrex Inc, Arthroscopy Association of North America, Ortho Info, Ruth Jackson Orthopaedic Society, and The Forum.
References
- 1. Barrentine S, Fleisig G, Whiteside J, Escamila R, Andrews J. Biomechanics of windmill softball pitching with implications about injury mechanisms at the shoulder and elbow. J Orthop Sports Phys Ther. 1998;28:405-415. [DOI] [PubMed] [Google Scholar]
- 2. Buchberger E. Why no pitch counts for softball. Accessed December 29, 2019. https://www.shouldermadesimple.com/whyh-no-pitch-counts-for-softball/
- 3. Burns P, Rohrich R, Chung K. The levels of evidence and their role in evidence-based medicine. Plast Reconstr Surg. 2011;128:305-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cooper JJ. (2017). High school pitch count rules by state. Accessed January 1, 2020. https://www.baseballamerica.com/stories/high-school-pitch-count-rules-by-state/
- 5. Hibberd EE, Oyama S, Tatman J, Myers JB. Dominant-limb range-of-motion and humeral-retrotorsion adaptation in collegiate baseball and softball position players. J Athl. 2014;49:507-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hill JL, Humphries B, Weidner T, Newton RU. Female collegiate windmill pitchers: influences to injury incidence. J Strength Cond Res. 2004;18:426-431. [DOI] [PubMed] [Google Scholar]
- 7. Ireland M, Snyder-Mackler L, Ferguson B. Softball injury prevention. Accessed August 23, 2020. https://www.sportsmed.org/aossmimis/STOP/Prevent_Injuries/Revised/Sports/Softball%20Injuries.pdf
- 8. Little League. Regular season pitching rules. Accessed January 6, 2020. https://www.littleleague.org/playing-rules/pitch-count
- 9. Patel N, Bhatia A, Mullen C, Bosman E, Lear A. Professional women’s softball injuries: an epidemiological cohort study. Clin J Sports Med. Published online June 19, 2019. doi: 10.1097/JSM.0000000000000698 [DOI] [PubMed] [Google Scholar]
- 10. Oliver GD. The windmill softball pitch, part 2: injury prevention. Int J Athl Ther Train. 2011;16:27-31. [Google Scholar]
- 11. Oliver GD, Dwelly P, Kwon YH. Kinematic motion of the windmill softball pitch in prepubescent and pubescent girls. J Strength Cond Res. 2010;24:2400-2407. [DOI] [PubMed] [Google Scholar]
- 12. Oliver GD, McKeon JM. The windmill softball pitch: optimal mechanics and pathomechanics of injury. Athl Ther Today. 2010;15(6):28-31. [Google Scholar]
- 13. Oliver GD, Plummer H. Ground reaction forces, kinematics, and muscle activations during the windmill softball pitch. J Sports Sci. 2010;29:1071-1077. [DOI] [PubMed] [Google Scholar]
- 14. Oliver GD, Washington JK, Plummer HA, Saper MG, Andrews JR, Dugas JR. Pitching mechanics in female youth fastpitch softball. Int J Sports Phys Ther. 2018;13:493-500. [PMC free article] [PubMed] [Google Scholar]
- 15. Shanely E, Rauh MJ, Michener LA, Elenbecker T. Incidence of injuries in high school softball and baseball players. J Athl Train. 2011;46:648-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med. 2011;39:1997-2006. [DOI] [PubMed] [Google Scholar]
- 17. Shanley E, Thigpen C. Throwing injuries in the adolescent athlete. Int J Sports Phys Ther. 2013;8:630-640. [PMC free article] [PubMed] [Google Scholar]
- 18. Smith M, Davis R, Brophy R, Prather H, Garbutt J, Wright R. Prospective player-reported injuries in female youth fast-pitch softball players. Sports Health. 2015;7:497-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wasserman EB, Register-Mihalik JK, Sauers EL, et al. The first decade of web-based sports injury surveillance: descriptive epidemiology of injuries in US high school girls’ softball (2005-2006 through 2013-2014) and National Collegiate Athletic Association Women’s Softball (2004-2005 through 2013-2014). J Athl Train. 2019;54:212-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Werner SL, Jones DG, Guido JA, Jr, Brunet ME. Kinematics and kinetics of elite windmill softball pitching. Am J Sports Med. 2006;34:597-603. [DOI] [PubMed] [Google Scholar]
- 21. Wilk KE, Obma P, Simpson CD, Cain EL, Dugas JR, Andrews JR. Shoulder injuries in the overhead athlete. J Orthop Sports Phys Ther. 2009;39:38-54. [DOI] [PubMed] [Google Scholar]


