Abstract
Introduction and importance
Bariatric surgery is an evolving surgical field with increasing cases per year, as obesity is prevalent, especially in developed countries. Complication diagnosis and management can be challenging. Marginal ulcers and anastomosis perforation are rare, but their incidence is likely underestimated.
Case presentation
To the best of our knowledge, we present the first case with a two and a half years history of recurrent ischemia, marginal ulcers, and recurrent perforation after laparoscopic omega loop gastric bypass, most likely due to an abuse of an over-the-counter (OTC) sympathomimetic nasal spray. The complications (Clavien-Dindo classification IIIb) caused the necessity of recurrent hospitalizations and diagnostic interventions and an open conversion into Roux-Y gastric bypass in a damage control manner.
Clinical discussion and conclusion
Conclusively, we advocate evaluating drug abuse, including OTC medications that patients might not report on a daily-based medical history, as an etiology for marginal ulcers and anastomosis perforation, especially in late and recurrent cases.
Keywords: Bariatric surgery, Perforation, Gastrojejunal anastomosis, Complication, Drug abuse, Sympathomimetic
Highlights
-
•
Abuse of OTC sympathomimetic nasal spray can cause recurrent gastrojejunal anastomosis ischemia.
-
•
Re-Do surgery cannot prevent recurrence of ischemia in these cases.
-
•
In recurrence of ischemia, detailed medical history, including OTC drugs, is crucial.
1. Introduction
Obesity (BMI ≥ 30 kg/m2) with related comorbidities is gradually becoming one of the most frequent diseases, with a prevalence of 13.2% globally and 25.3% in Europe in 2016 [1], [2]. Since the introduction of surgical bariatric interventions, different procedures have evolved, and the number of modalities is increasing. According to the most recent survey of the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) in 2018, 696,191 surgical and endoluminal procedures were performed globally, with 55.4% being sleeve-gastrectomy (SG) and 29.3% Roux-en-Y gastric bypass (RYGB) as the two most frequently used procedures [3]. A Cochrane review (2014) could not find a consistent superiority between laparoscopic RYGB (LRYGB), open RYGB, and laparoscopic SG (LSG) about complications and mortality [4]. However, a study published in 2019 including >250,000 patients with significantly lower postoperative complication rates in LSG than in LRYGB was found [5]. Complications include bleeding, hemorrhage, staple line leaks, strictures, bile reflux, intussusception, and ulcer or perforation at the anastomosis [5], [6], [7], [8], [9].
To our knowledge, no data is available so far on recurrent ischemia and gastro-jejunal anastomosis (GJA) perforation after laparoscopic omega-loop gastric bypass (LOL-GB) or RYGB - caused by sympathomimetic nasal spray abuse. Given the lack of literature, we present the following patient with GJA ischemia after bariatric surgery, most likely caused by xylometazoline-based nasal spray abuse.
2. Presentation of case
A 53-year-old Caucasian female patient received LSG due to severe (WHO class III) obesity with a BMI of 48.6 kg/m2 at the University Hospital of Bern in Switzerland by a Swiss Society for the Study of Morbid Obesity and Metabolic Disorders certified surgeon. Relevant comorbidities were hypertension, dyslipidemia, severe obstructive sleep apnea, chronic obstructive pulmonary disease GOLD II (smoking [cumulative 40 packyears]), as well as bilateral symptomatic arthrosis of the lower extremities and spine. Patients Timetable, weight progression, and interventions are displayed in Table 1.
Table 1.
Timetable, weight progression and interventions.
| Event | Weight |
BMI |
%TWL | %EWL | |
|---|---|---|---|---|---|
| [kg] | [kg/m2] | ||||
| Baseline | 126 | 48.6 | |||
| 28th December 2015 | Lap. sleeve gastrectomy | ||||
| 13th July 2017 | OPC | 88.5 | 34.1 | 29.8% | 61.3% |
| 21st June 2018 | OPC | 99 | 38.2 | ||
| 26th June 2018 | Lap. switch to omega loop | ||||
| 02nd August 2018 | OPC | 91 | 35.1 | 27.8% | 57.2% |
| 24th August 2018 | Lap. suture of perforated GJA | ||||
| 06th October 2018 | Hospitalization: acute gastroenteritis | ||||
| 09th October 2018 | Gastroscopy | ||||
| 17th October 2018 | OPC | 86 | 33.2 | 31.7% | 65.4% |
| 19th December 2018 | OPC | 85 | 32.8 | 32.5% | 67.0% |
| 28th January 2019 | Gastroscopy | ||||
| 30th January 2019 | Lactulose breath test | ||||
| 07th August 2019 | OPC | 85 | 32.8 | 32.5% | 67.0% |
| 28th August 2019 | Lactulose breath test | ||||
| 12th February 2020 | OPC | 92 | 35.5 | 27.0% | 55.6% |
| 04th February 2021 | Laparotomy, GJA resection | ||||
| 06th February 2021 | 2nd look, RYGB | ||||
| 08th February 2021 | 116 | 44.8 | 7.9% | 16.3% | |
| 18th February 2021 | 108 | 41.7 | 14.3% | 29.4% | |
| 13th March 2021 | Hospitalization: recurrent ischemic enteritis | ||||
| 14th March 2021 | Gastroscopy | ||||
| 15th March 2021 | 102 | 39.4 | 19.0% | 39.2% | |
| 07th April 2021 | Gastroscopy | ||||
| 26th May 2021 | Gastroscopy |
Abbreviations: ∆, delta; BMI, body mass index; %EWL, percentage of excess weight loss; GJA, gastro-jejunal anastomosis; Lap., laparoscopic; OPC, outpatient clinic; RYGB, Roux-Y gastric bypass; %TWL, percentage of total weight loss.
Two years after initial surgery, a weight loss of 37.5 kg was documented (BMI 34.1 kg/m2). At two and a half years after LSG, due to a weight regain of 10.5 kg (BMI 38.2 kg/m2), LOL-GB was performed, and the patient was uneventfully discharged on day three.
About two months after laparoscopic omega-loop, the patient presented to our emergency department (ED) with an acute onset of abdominal pain with computed tomography (CT) signs suggesting a possible intestinal perforation (perigastric, perisplenic, and perihepatic free air and liquid) (Fig. 1). Emergency diagnostic laparoscopy was performed. A biopsy of the 10 by 10 mm sized perforation of the GJA after LOL-GB was performed. The defect was closed using V-Loc© 3.0 continuous suture and covered with an omentum patch. Antibiotic therapy was established using piperacillin/tazobactam intravenously for nine days followed by a total of eight days of oral clavulanic acid/amoxicillin accompanied by proton pump inhibitors (PPI) therapy using pantoprazole 40 mg twice daily. Histopathological results yielded fibrinogen leukocyte exudate but no signs for malignancy. On the eleventh day after surgery, the patient was discharged home.
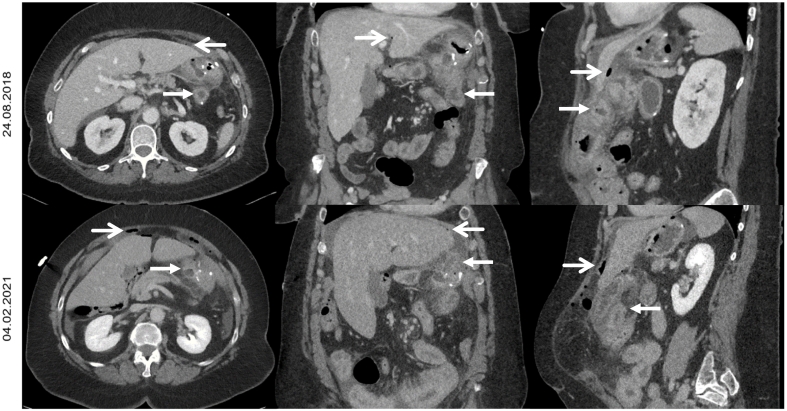
Fig. 1.
Computed tomography scans, demonstrating perforation of gastrojejunal anastomosis with free air and liquid in horizontal, coronal and sagittal views. White open rounded arrow displays free air, white closed arrow highlights thickened gastric and jejunal walls.
About one month after discharge, the patient presented to our ED with diarrhea for three days, accompanied by one episode of melena and hematemesis. CT demonstrated thickened gastric wall without signs of perforation. After 24 h of uneventful monitoring, the patient was discharged. The further diagnostic was planned and performed in the outpatient clinic using gastroscopy, which demonstrated a large ulcer of the GJA and a smaller ulcer distally to the anastomosis. The highly dosed regimen of proton pump inhibitors (PPI) was established for four weeks. Regular check-ups in our outpatient clinic followed, where rarely intermittent epigastric patient and diarrhea were reported. Re-gastroscopy (no ulcer, bile reflux and suspected discrete reactive gastropathy; histopathologically discrete chronic type c gastritis) and a lactulose breath test (H2-concentration 60 min >20 ppm and CH4-concentration always <8 ppm) were performed, and an antibiotic (Gentamycin) decontamination for suspected small intestinal bacterial overgrowth (SIBO) was prescribed. At following check-ups patient's complaints improved but re-occurred with intermittent abdominal pain, vomiting, diarrhea, and constipation. Complaints slightly decreased by the use of laxatives. The lactulose breath test was repeated after seven months (H2-concentration 90 min >20 ppm and CH4-concentration 150 min >8 ppm), suggesting possible SIBO. PPI therapy was continued (pantoprazole 20 mg three times daily).
Thirty months after LOL-GB, the patient presented to our ED with persisting abdominal pain for three days, recurrent vomiting, and diarrhea. The patient was hemodynamically stable, had a quick sepsis-related organ failure assessment score (qSOFA) of 0/3 points, and had a flat abdomen. Laboratory testing showed an elevated CRP 39 mg/L and normal lactate (1.20 mmol/L). CT scan showed free air and liquids in the epigastrium with a thickened wall of the omega loop but no signs of relevant vascular pathology (Fig. 1). Empirical antibiotic therapy with piperacillin/tazobactam was established. Explorative laparotomy presented four-quadrant peritonitis with a perforation of the anterior wall of the GJA. The omega loop was heavily inflamed. After adhesiolysis, the GJA was resected, followed by peritoneal lavage and closure of the abdomen using a vacuum-assisted closure therapy in a damage-control manner. The second look was done 54 h later with reconstruction in a Roux-en-Y way. Histopathology of the GJ-resection demonstrated ischemic transformation as well as acute, chronic inflammation of the anastomosis and again no signs of malignancy. Antibiotic therapy was continued for ten days after surgery, and the patient was transferred in a good general state of health to a rehabilitation clinic on day twelve.
Three days after discharge from the rehabilitation center, the patient presented to our ED with a 12-hour history of vomiting and slight epigastric pain. Tenderness on palpation of the left hemiabdomen was noted with a discrete increase of CRP (10 mg/L). CT scan yielded an edematous thickening of the jejunal wall just distally to the GJA after RYGB without any free liquid or air. The patient was admitted to our ward for monitoring. The gastroscopy demonstrated multiple fibrinous defects (marginal ulcer) of the GJA as well as punctiform ischemic lesions of the jejunum just distally to the GJA (Fig. 2). Histopathology revealed active focal erosive inflammation of the lamina propria. Anticoagulation with intravenously heparin 15′000 IE per 24 h was given with suspected underlying ischemic cause for the recurrent complaints. Duplex sonography was performed by an angiologist where no relevant stenosis of the mesenteric blood vessels was found. In further medical history, the patient reported using an over-the-counter (OTC) xylometazoline-based (alpha-adrenergic sympathomimetic) nasal spray >15–20 blows/day (recommended maximum three blows/d for max. 7 days) for nasal congestion. Timely coherence of recurrent abdominal complaints and intestinal perforation with increased xylometazoline use was found. The patient was advised to cease the use of alpha-adrenergic sympathomimetic nasal spray and smoking. She was discharged home on day five.
Fig. 2.
Gastroscopy images demonstrating multiple punctiform ischemic lesions (left) and marginal ulcer at gastrojejunal anastomosis (right; highlighted by the black stealth arrow).
Control gastroscopy two weeks after discharge documented a partial and at six weeks a complete resolution of the ischemic lesions.
3. Discussion and conclusion
To our knowledge, we present the first case of a 3.5 years follow-up period of a bariatric surgical intervention with recurrent complications (Clavien-Dindo Classification IIIb) most likely caused by an OTC nasal spray abuse, which has been reported according to the SCARE 2020 Guidelines [10].
In this case, the first onset of perforation of anastomosis occurred two months after LOL-GB leading to revisional surgery. Retrospectively, the acute gastroenteritis approximately 1.5 months after surgery was most likely a less severe case of ischemia leading to admission to our clinic. In the following months, recurrent, less intense symptoms occurred, and several different diagnostically interventions were performed. Two and a half years after LOL-GB, perforation of the GJA necessitated the switch into RYGB in a two-staged damage control manner.
Complication occurrence, adequate diagnostics as well as treatment modalities are ongoing topics of research interest. In a single-surgeon experience in the US, marginal ulcers (MU) occurred in 5.3% (122/2282) of which 68% (83/122) were successfully treated without surgery, whereas only one case (0.8%, 1/122) suffered from perforation [7]. The authors argued that the incidence (0.6%–16.0%) remains likely underestimated as symptoms of MU are variable and might be confounded with complaints of overeating [7]. Moreover, the etiology of MU incl. Perforation remains a matter of debate.
Cervin et al. were able to demonstrate a decreased blood flow in the nasal septal mucosal tissue in humans 20 min after administration of xylometazoline by 61% [11]. In a review (2018), the use of intranasal vasoconstrictors has been discussed as a possible etiology of nasoseptal perforation [12]. In rats, nasal application of oxymetazoline has shown significant systemic (rats' tail tissue) ischemic changes, necrosis, and ulceration accompanied by a possible trend of arterial thrombosis [13]. Preclinical data displays evidence of active metabolites of oxymetazoline in human, rat, and rabbit liver tissue [14]. However, the authors argued that safety concerns of systemic changes and toxicity are unlikely due to the short application period and lower dosages [14]. In literature, case reports or minor case series report stroke and non-ST-elevation myocardial infarction in use of nasal oxymetazoline and acute ischemia of the hand as a consequence of intra-arterial oxymetazoline injection, displaying rare systemic effects and resulting complications in oxymetazoline use [15], [16], [17].
Currently, as data is sparse, no recommendations are available on diagnostics and treatment for recurrent MU. Derived from the presented case, we advocate the evaluation of drug abuse, including OTC medications - which patients might not report - on a daily-based medical history, as well as possible medical interactions leading to a reduced blood perfusion as a cause for marginal ulcers and anastomosis perforation, especially in late and recurrent cases.
Sources of funding
No funding received.
Ethical approval
General consent as well as signed ‘International Journal of Surgery Patient Consent Form’ was obtained from the patient. The 1964 Helsinki declaration and its lateramendments and comparable ethical standards were obeyed. There were no animal studies performed by any of the authors for this study. Single case report with n = 1 is exempted for ethnical approval seeking in Switzerland from the national ethical committee (swissethics; Swiss Association of Research Ethics Committees).
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authorship and contributorship
CTJM: investigation, manuscript drafting, writing, literature search.
GAP: writing, editing, critical review.
PCN: critical review, supervision, final approval.
Research registration
None.
Guarantor
Philipp C Nett.
Declaration of competing interest
No financial or other conflicts of interest to report.
Acknowledgments
Acknowledgements
Nihil.
Availability of data and materials
On request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.WHO GHO | By category | Prevalence of obesity among adults, BMI ≥ 30, crude - Estimates by WHO region. https://apps.who.int/gho/data/view.main.BMI30CREGv?lang=en
- 2.Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- 3.Angrisani L., Santonicola A., Iovino P., Ramos A., Shikora S., Kow L. Bariatric surgery survey 2018: similarities and disparities among the 5 IFSO chapters. Obes. Surg. 2021;31(5):1937–1948. doi: 10.1007/s11695-020-05207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colquitt J.L., Pickett K., Loveman E., Frampton G.K. Surgery for weight loss in adults. Cochrane Database Syst. Rev. 2014;8:2014. doi: 10.1002/14651858.CD003641.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chung A.Y., Strassle P.D., Schlottmann F., Patti M.G., Duke M.C., Farrell T.M. Trends in utilization and relative complication rates of bariatric procedures. J. Gastrointest. Surg. 2019;23(7):1362–1372. doi: 10.1007/s11605-018-3951-2. [DOI] [PubMed] [Google Scholar]
- 6.Robinson T.D., Sheehan J.C., Patel P.B., Marthy A.G., Zaman J.A., Singh T.P. Emergent robotic versus laparoscopic surgery for perforated gastrojejunal ulcers: a retrospective cohort study of 44 patients. Surg. Endosc. 2021;1:3. doi: 10.1007/s00464-021-08447-5. [DOI] [PubMed] [Google Scholar]
- 7.Patel R.A., Brolin R.E., Gandhi A. Revisional operations for marginal ulcer after Roux-en-Y gastric bypass. Surg. Obes. Relat. Dis. 2009;5(3):317–322. doi: 10.1016/j.soard.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Della Penna A., Lange J., Archid R., Hönes F., Königsrainer A., Quante M. Impact of resection volume/stapler firings-ratio on perioperative complications and weight loss after laparoscopic sleeve gastrectomy. Obes. Surg. 2021;31(1):207–214. doi: 10.1007/s11695-020-04870-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Springer International Publishing; 2020. The ASMBS Textbook of Bariatric Surgery. [Google Scholar]
- 10.Agha R.A., et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. Dec. 2020;84:226–230. doi: 10.1016/J.IJSU.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Cervin A., Åkerlund A., Greiff L., Andersson M. The effect of intranasal budesonide spray on mucosal blood flow measured with laser doppler flowmetry. Rhinology. 2001;39(1):13–16. [PubMed] [Google Scholar]
- 12.Pereira C., Santamaría A., Langdon C., López-Chacón M., Hernández-Rodríguez J., Alobid I. Nasoseptal perforation: from etiology to treatment. Curr. Allergy Asthma Rep. 2018;18(1) doi: 10.1007/s11882-018-0754-1. [DOI] [PubMed] [Google Scholar]
- 13.Dokuyucu R., et al. Systemic side effects of locally used oxymetazoline. Int. J. Clin. Exp. Med. 2015;8(2):2674–2678. [PMC free article] [PubMed] [Google Scholar]
- 14.Mahajan M.K., Uttamsingh V., Daniels J.S., Gan L.S., LeDuc B.W., Williams D.A. In vitro metabolism of oxymetazoline: evidence for bioactivation to a reactive metabolite. Drug Metab. Dispos. Apr. 2011;39(4):693–702. doi: 10.1124/dmd.110.036004. [DOI] [PubMed] [Google Scholar]
- 15.Cantu C., Arauz A., Murillo-Bonilla L.M., López M., Barinagarrementeria F. Stroke associated with sympathomimetics contained in over-the-counter cough and cold drugs. Stroke. Jul. 2003;34(7):1667–1672. doi: 10.1161/01.STR.0000075293.45936.FA. [DOI] [PubMed] [Google Scholar]
- 16.Shukla P.C. Acute ischemia of the hand following intra-arterial oxymetazoline injection. J. Emerg. Med. Jan. 1995;13(1):65–70. doi: 10.1016/0736-4679(94)00124-3. [DOI] [PubMed] [Google Scholar]
- 17.Rajpal S., Morris L.A., Akkus N.I. Non-ST-elevation myocardial infarction with the use of oxymetazoline nasal spray. Rev. Port. Cardiol. 2014;33(1):51.e1–51.e4. doi: 10.1016/j.repc.2013.07.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
On request.