Abstract
Background and Aims
Zenker’s diverticulum (ZD) is attributed to a poorly compliant cricopharyngeus muscle, and the mainstay of treatment is a cricopharyngeal myotomy. We present a video series summarizing endoscopic treatment options for ZD and related conditions.
Methods
We review the rationale and key technique for various endoscopic treatment modalities for ZD, cricopharyngeal bar, and other esophageal diverticula.
Results
Standard flexible endoscopic cricopharyngeal myotomy involves the division of the common wall or septum of the ZD, aiming for complete transection of the cricopharyngeus. However, recurrence rates are high, likely owing to incomplete myotomy. Zenker’s peroral endoscopic myotomy (Z-POEM) uses a proximal submucosal tunnel to provide direct visualization of the cricopharyngeus and septum, allowing confirmation of complete myotomy. We demonstrate an over-the-septum modification to simplify the technique. Submucosal fibrosis, commonly seen in patients with prior treatment, limits submucosal dissection. We present a hybrid technique to overcome this, whereby a traditional septotomy is performed until submucosal tissue is visualized. The intact mucosal flap after Z-POEM in a large ZD may contribute to residual dysphagia. We propose Z-POEM with mucosotomy for large ZD. Finally, we demonstrate modifications for treatment of other esophageal diseases, including cricopharyngeal bar and non-Zenker’s esophageal diverticula.
Conclusion
Endoscopic treatment options for ZD and related conditions are rapidly expanding. With careful tailoring to individual patient characteristics, our expanding arsenal of options allows effective and safe treatment of a broad spectrum of patients.
Abbreviations: FECM, flexible endoscopic cricopharyngeal myotomy; TTSC, through-the-scope clip; ZD, Zenker’s diverticulum; Z-POEM, Zenker’s peroral endoscopic myotomy
Introduction
Zenker’s diverticulum (ZD) is attributed to impaired cricopharyngeal muscle distensibility during swallowing1 and can result in symptoms including dysphagia, regurgitation, aspiration, cough, and weight loss. The mainstay of treatment is a cricopharyngeal myotomy. Traditional management options include open surgery (transcervical diverticulectomy, diverticulopexy, or diverticular inversion with or without cricopharyngeal myotomy) and rigid endoscopy (using stapling or CO2 laser treatment). However, these options are limited by significant morbidity and mortality, particularly in the elderly and often comorbid ZD population.2
Since its introduction, flexible endoscopic ZD treatment has rapidly gained traction and emerged as an excellent first-line treatment option, particularly for small to moderate diverticula.3 The past decade has seen multiple emerging techniques in flexible endoscopic ZD treatment (Table 1). This case series will review these advances in the treatment of ZD and related conditions (Video 1, available online at www.giejournal.org). We will detail the key steps and technical tips behind each procedure.
Table 1.
Summary of flexible endoscopic Zenker’s diverticulum treatment
| Procedure | Technique summary | Pros | Cons |
|---|---|---|---|
| Traditional FECM |
|
|
|
| Flexible endoscopic cricopharyngeal myectomy8† |
|
|
|
| Z-POEM |
|
|
|
| Modified over the septum Z-POEM |
|
|
|
| Modified Z-POEM with mucosotomy |
|
|
|
| Hybrid Z-POEM |
|
|
|
FECM, Flexible endoscopic cricopharyngeal myotomy; Z-POEM, Zenker’s peroral endoscopic myotomy.
Perceived theoretical benefit; no high-quality data available.
Not included in video case series.
Methods
Patients reporting typical symptoms as described earlier are comprehensively evaluated with a full clinical history, contrast swallow study, and diagnostic upper endoscopy. If there is any concern for impaired swallow initiation or coordination, patients are referred for a modified barium swallow and review by speech/language therapy. If there is concern for esophageal dysmotility, patients undergo high-resolution esophageal manometry. Symptomatic patients with ZD as confirmed on contrast swallow study and/or upper endoscopy are offered treatment. Procedures are performed with the patient under general anesthesia and in a supine position.
The traditional method of flexible endoscopic cricopharyngeal myotomy (FECM) involves the division of the entire common wall or septum of the ZD, aiming for a complete myotomy of the cricopharyngeus. Zenker’s peroral endoscopic myotomy (Z-POEM) uses a proximal submucosal tunnel to provide direct visualization and exposure of the cricopharyngeus and septum. Because the mucosa is kept intact, aggressive myotomy can then be performed. We demonstrate a modification to simplify the technique by performing submucosal injection and mucosal incision directly over the septum. Proposed advantages of this technique include shorter procedure time and potentially decreased risk, although this remains to be proven in prospective comparative studies.
Submucosal fibrosis, commonly seen in patients who have undergone prior treatment, limits submucosal dissection. In this setting, a hybrid technique can be adopted, whereby a traditional septotomy is performed until submucosal tissue is visualized. Submucosal tunneling then allows exposure of the base of the septum for a full-thickness myotomy. A major difference between Z-POEM and standard FECM is that the mucosal flap is left intact after Z-POEM. For management of large ZD, where persistence of the mucosal flap may contribute to residual dysphagia, we propose Z-POEM with mucosotomy. The added tunneling technique in Z-POEM with mucosotomy allows exposure of the muscular layer at the critical point (ie, at the base of the diverticulum). This helps to ensure that a complete myotomy is achieved, theoretically reducing the risk of recurrence, although comparative trials are awaited to confirm this. Finally, the demonstrated techniques can be adapted to treatment of other esophageal diseases. For example, despite the absence of a diverticular pouch or septum in cricopharyngeal bar, a modified Z-POEM can be performed. Furthermore, concurrent cricopharyngeal bar and distal esophageal diverticulum can be treated in a single session.
Patients
Flexible endoscopic cricopharyngeal myotomy
The rationale behind FECM is a complete division of the septum, including the cricopharyngeus muscle (Fig. 1). The aim is for a complete myotomy; however, this can be difficult to gauge endoscopically, and an incomplete myotomy is believed to be a large contributor to reported recurrence rates of 11%.4 Multiple variations in technique exist between institutions, including cutting device, use of a diverticuloscope or other accessory, and whether a prophylactic clip is placed at the apex of the incision.
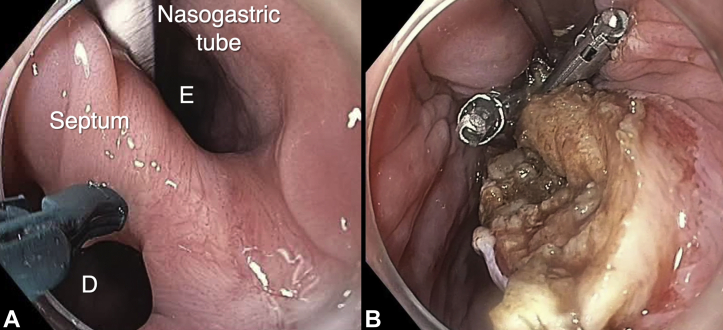
Figure 1.
Traditional flexible endoscopic cricopharyngeal myotomy. A, The septum separates the Zenker’s diverticulum (D) from the esophageal lumen (E). A nasogastric tube is placed to delineate the true esophageal lumen. B, After transection of the septum including the cricopharyngeal muscle, through-the-scope clips are placed at the apex of the defect.
A septal exposure device, including a diverticuloscope or a transparent distal attachment, is often used. The diverticuloscope is specifically designed to straddle the cricopharyngeus between 2 flaps. In the absence of a diverticuloscope, nasogastric tube placement can be used to delineate the esophagus. This is often placed under endoscopic visualization or over a guidewire to prevent inadvertent injury to the ZD during passage. We prefer the use of a transparent distal attachment, which improves visualization, increases working space, and optimizes equipment positioning. In our first case, a nasogastric tube was used to delineate the true esophageal lumen. A stag beetle knife (Olympus America, Center Valley, Pa, USA) was used to transect the septum until the most inferior aspect of the diverticulum was reached. Through-the-scope clips (TTSCs) then were placed at the apex of the incision to prevent perforation. There is controversy regarding the need for a prophylactic clip at the base of the defect, and this practice differs among institutions.
Z-POEM
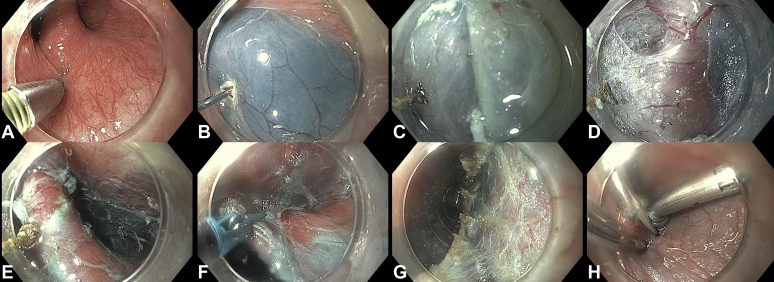
Z-POEM follows a principle similar to that for treatment of achalasia by standard esophageal POEM. That is, submucosal tunneling starting proximal to the diverticular septum allows full exposure of the muscular layer, thereby allowing a complete myotomy (Fig. 2). Because an incomplete myotomy is believed to be a large contributor to recurrence after standard septotomy, this theoretically reduces the risk of recurrence. In case 2, a submucosal injection using a premixed solution of indigo carmine and normal saline solution was performed 1.5 cm proximal to the Zenker’s septum to create a mucosal bleb. A mucosal incision was then made along the axis of the septum. The submucosal space was then entered and tunneling was performed to the septum. Intraprocedural bleeding was treated using coagulation graspers (Coagrasper, Olympus America) and soft coagulation (ERBE Medical, Marietta, Ga, USA). Submucosal dissection was continued until the septum was completely exposed on both sides. A complete myotomy was then performed, transecting through the cricopharyngeal muscle and extending a few centimeters into esophageal muscle. Mucosal closure was attained using TTSCs placed sequentially in close approximation across the entire defect. Short-stemmed clips are preferred in this proximal location, because this decreases the foreign body sensation for patients.
Figure 2.
Standard Zenker’s peroral endoscopic myotomy (Z-POEM). A, Submucosal injection is performed a short distance proximal to the septum. B, Mucosal incision is performed. C, The submucosal space is entered. D, Submucosal tunneling is performed until the septum is reached. E, Submucosal dissection is performed on either side of the muscular septum. F, A stag beetle knife is used to transect the septum. G, Myotomy of the entire cricopharyngeus and extending a short distance distally. H, Mucosal closure using through-the-scope clips.
Notably, despite the positive outcomes, Z-POEM has not attained widespread uptake, being a technically challenging procedure. Long-term outcomes and comparative trials are awaited. Pending this, the only guideline so far considers Z-POEM and other tunneling techniques to be experimental.5
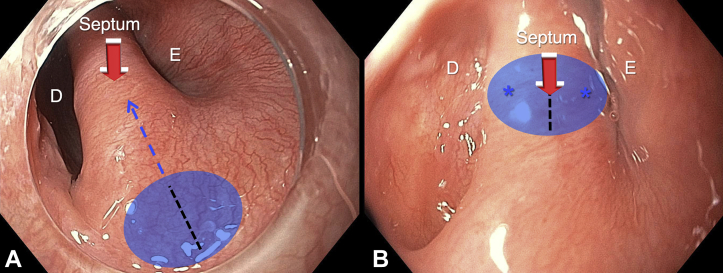
Modified over-the-septum Z-POEM
In a modified Z-POEM, submucosal injection followed by mucosal incision is performed directly over the septum (Fig. 3). In contrast to achalasia, visualization of the Zenker’s septum negates the need for proximal tunneling. In the third case, a submucosal injection was performed directly over the septum, followed by a mucosal incision along the axis of the septum. Subsequent steps, including dissection to expose the septum and full-thickness myotomy through the cricopharyngeus into esophageal muscle, are as per the prior iteration. Notably, the modification negates the need for proximal tunneling, improves working space during mucosal closure, and improves visualization of closure adequacy. This theoretically reduces the risk of leak and is now the preferred technique at our institution.
Figure 3.
Standard Zenker’s peroral endoscopic myotomy (Z-POEM) versus modified over-the-septum Z-POEM. A, Standard Z-POEM with submucosal injection (blue circle) proximal to the septum to allow mucosal incision (black dotted line) and submucosal tunnelling (blue dotted line). Once the septum is exposed, dissection is performed on either side, before a myotomy is performed (red arrow) to transect the septum including the cricopharyngeal muscle. B, Over-the-septum Z-POEM with submucosal injection (blue circle) directly over the septum and mucosal incision (black dotted line) along the axis of the septum. Submucosal dissection is performed on either side of the septum (blue asterisks) to expose it before full-thickness myotomy (red arrow). D, Diverticulum; E, esophageal lumen.
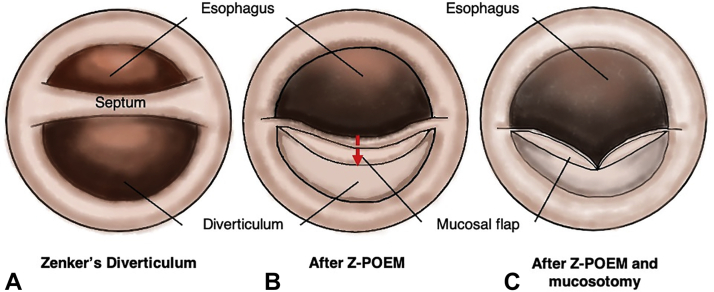
Z-POEM with mucosotomy
Importantly, during FECM or Z-POEM, diverticulectomy is not performed. However, particularly because the mucosa is left intact during Z-POEM, a large mucosal flap can contribute to residual symptoms (Fig. 4). In case 4, we demonstrate the addition of a mucosotomy in a large ZD (Fig. 5). After completion of myotomy as part of an over-the-septum Z-POEM, the residual mucosal flap was stabilized with placement of TTSCs at either end of the mucosal incision. The mucosa between the 2 clips was then transected sequentially until the most inferior aspect of the diverticulum was reached. This technique allows a wider communication between the diverticulum and esophageal lumen, thereby improving preferential passage of food contents to the true esophageal lumen. Complete closure is vital and was achieved by sequential clip placement in our patient, although this could be tailored to the endoscopist’s technical skill set and preference.
Figure 4.
Zenker’s peroral endoscopic myotomy (Z-POEM) with mucosotomy. A, The septum separates the Zenker’s diverticulum from the true esophageal lumen. B, After Z-POEM, a large residual mucosal flap can contribute to persistent symptoms. C, Transection of the mucosal flap to the most inferior aspect of the diverticulum widens the communication between the diverticulum and the esophagus, thereby favoring preferential passage into the true esophageal lumen.
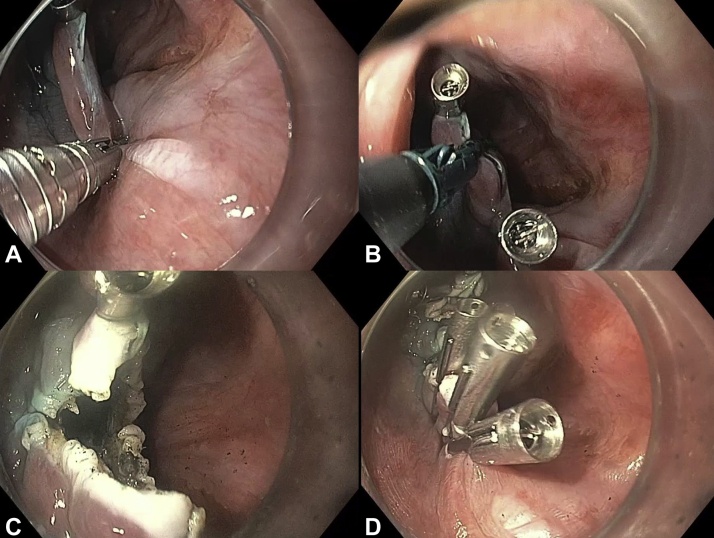
Figure 5.
Mucosotomy. A, After over-the-septum Z-POEM, the mucosal flap is stabilized with placement of one through-the-scope clip at either end. B, The stag beetle knife is used to transect the mucosal flap. C, The mucosal flap is incised down to the most inferior aspect of the diverticulum. D, The entire mucosal defect is closed with through-the-scope clips. Z-POEM, Zenker’s peroral endoscopic myotomy.
Hybrid technique for treatment of recurrent ZD
Recurrence of ZD after treatment is not uncommon, and patients increasingly present after prior surgical or endoscopic treatment. In case 5, a patient with prior surgical ZD treatment presented with recurrent symptoms. At endoscopy, surgical staples were seen, consistent with prior therapy. Submucosal injection resulted in minimal lift, and the submucosal plane was not readily identifiable. Thus, a standard septotomy was commenced. The septotomy was continued through fibrotic tissue until submucosal tissue was visualized. Injection of the premixed indigo carmine and normal saline solution into the submucosal tissue was then able to delineate the submucosal plane, allowing a submucosal tunnel to be created. The benefit of this procedure over standard FECM is that tunneling can be performed at the crucial point—the base of the diverticulum—to allow direct visualization and confirmation of a complete myotomy, again theoretically reducing the risk of recurrence.
Treatment of other upper esophageal disorders
The submucosal tunneling technique is highly modifiable and can be tailored for the management of other upper esophageal disorders.
In a cricopharyngeal bar, there is no diverticulum or septum; however, a similar technique can still be adopted. Case 6 demonstrates a patient with a prominent cricopha-ryngeal bar. In this setting, mucosal incision and tunneling was commenced proximal to the cricopharyngeus, which allowed clear identification of the thickened cricopharyngeus. This allowed a full-thickness myotomy of the cricopharyngeus, extending a short distance distally.
The final case demonstrates treatment of a combination of prominent cricopharyngeus and an upper esophageal diverticulum distally. The submucosal tunnel was commenced proximal to the cricopharyngeus and extended beyond the diverticular septum to normal esophageal muscle. This exposed both the cricopharyngeus and the muscular diverticular septum, allowing full-thickness myotomy of both. Closure was then attained with TTSCs. This case demonstrates that the technique can be extrapolated for treatment of other esophageal diverticula, so-called diverticular POEM, or D-POEM.6
Prevention and management of adverse events
Case 2 demonstrated the management of intraprocedural bleeding. The cutting knife with the tip retracted can be used to treat small vessels; however, there should be a low threshold to use coagulation graspers for treatment of larger vessels. Treatment should be applied away from the mucosa where possible. Any active bleeding should be promptly addressed because even a small amount of blood within the tight submucosal tunnel can rapidly obscure views, making not only hemostasis but also the remainder of the procedure more difficult. The bleeding point should be identified, and the clear cap should be carefully but firmly pressed against the area to provide tamponade should there be any delay in obtaining the necessary equipment.
Another adverse event that can cause significant morbidity is perforation. Before closure, the entire treated area, particularly the mucosa on both the diverticular and esophageal sides, should be closely inspected for inadvertent injuries. Intraprocedural identification of inadvertent mucosotomies can usually be successfully closed with TTSCs and/or suturing. Secure closure of the mucosal incision site is key. TTSCs are commonly used; however, equipment choice can depend on endoscopist experience and preference. Clip loss in edematous mucosa in the setting of peroral endoscopic myotomy for achalasia is a significant predictor of closure site dehiscence.7 Accordingly, we recommend delaying the procedure, if possible, if significant mucosal inflammation is encountered. If the procedure cannot be postponed, we recommend consideration of an alternate closure modality such as suturing. Routine postprocedure contrast swallow study is frequently used for early detection of leaks, although no studies have specifically addressed its utility.
Results
All patients were successfully managed with no postprocedure adverse events or residual dysphagia at time of last follow-up.
Conclusion
Endoscopic treatment options for ZD and similar esophageal diseases are rapidly expanding. There is heterogeneity in techniques and equipment used. However, the techniques are highly modifiable, and with careful tailoring to individual patient characteristics, our expanding arsenal of options has resulted in the ability to treat a broader spectrum of patients and conditions.
Disclosure
Dr Nieto is a consultant for Boston Scientific. Dr Repici is a consultant for Boston Scientific and ERBE; is on the advisory board for Medtronic, NEC, Linkverse, EndoKey, and EndoStart; has received speaker fees from Medtronic, Fujifilm, Olympus, Boston Scientific, and Norgine; and has research grants from Medtronic, Fujifilm, Pentax, Cosmo Pharma, Boston Scientific, ERBE, Norgine, and Endostart. Dr Ngamruengphong is a consultant for Boston Scientific. Dr Khashab is a consultant for Boston Scientific, Olympus, Medtronic, and GI Supply and receives royalties from UpToDate and Elsevier.
Supplementary data
Zenker’s diverticulum: advancing beyond the tunnel.
References
- 1.Zhang L.Y., Iung-Chiang Wu P., Szczesniak M.M., et al. Clinical utility of cricopharyngeal distensibility measurements during endoscopic myotomy for Zenker’s diverticulum. Gastrointest Endosc. 2021;93:390–397. doi: 10.1016/j.gie.2020.05.064. [DOI] [PubMed] [Google Scholar]
- 2.Dzeletovic I., Ekbom D.C., Baron T.H. Flexible endoscopic and surgical management of Zenker’s diverticulum. Expert Rev Gastroenterol Hepatol. 2012;6:449–465. doi: 10.1586/egh.12.25. quiz 466. [DOI] [PubMed] [Google Scholar]
- 3.Yang J., Novak S., Ujiki M., et al. An international study on the use of peroral endoscopic myotomy in the management of Zenker’s diverticulum. Gastrointest Endosc. 2020;91:163–168. doi: 10.1016/j.gie.2019.04.249. [DOI] [PubMed] [Google Scholar]
- 4.Ishaq S., Hassan C., Antonello A., et al. Flexible endoscopic treatment for Zenker’s diverticulum: a systematic review and meta-analysis. Gastrointest Endosc. 2016;83:1076–1089.e5. doi: 10.1016/j.gie.2016.01.039. [DOI] [PubMed] [Google Scholar]
- 5.Weusten B.L.A.M., Barret M., Bredenoord A.J., et al. Endoscopic management of gastrointestinal motility disorders - part 2: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:600–614. doi: 10.1055/a-1171-3174. [DOI] [PubMed] [Google Scholar]
- 6.Yang J., Zeng X., Yuan X., et al. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy. 2019;51:346–349. doi: 10.1055/a-0759-1428. [DOI] [PubMed] [Google Scholar]
- 7.Zhang X.C., Li Q.L., Xu M.D., et al. Major perioperative adverse events of peroral endoscopic myotomy: a systematic 5-year analysis. Endoscopy. 2016;48:967–978. doi: 10.1055/s-0042-110397. [DOI] [PubMed] [Google Scholar]
- 8.Pang M., Koop A., Brahmbhatt B., et al. Comparison of flexible endoscopic cricopharyngeal myectomy and myotomy approaches for Zenker diverticulum repair. Gastrointest Endosc. 2019;89:880–886. doi: 10.1016/j.gie.2018.09.043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Zenker’s diverticulum: advancing beyond the tunnel.