Abstract
Objective
The objectives of this study were to identify community pharmacist (CP)‐led cognitive services and CPs’ precautions taken related to COVID‐19, perceived enablers and barriers related to pharmaceutical services and burnout levels during the COVID‐19 pandemic.
Method
In this descriptive study, the survey was administered online to CPs in all regions of Turkey. The frequency of their provision of patient counselling, provision of medication information and practices towards precautions during the pandemic were evaluated based on CP self‐reports. The Turkish version of the Burnout Measure Short Form was used, and a 30‐item questionnaire based on the 12‐domain Theoretical Domains Framework was developed to determine CPs’ perceived enablers of and barriers to pharmaceutical service delivery during the COVID‐19 pandemic. Data were collected using convenience sampling methods. Besides internal consistency reliability, principal component analysis, and correlation analysis, Mann‐Whitney U‐test was conducted in group comparisons.
Results
A total of 1098 complete responses were received, for a response rate of 4.11% among 26 747 CPs. The CPs’ median burnout score was 3.3 (2.5‐4.2). More than half of the CPs (54.5%) referred probable patients with COVID‐19 to the hospital. Commonly delivered cognitive CP‐led services included preventive health services (89.5%) and medication information services (86.3%). Perceived barriers to delivering pharmaceutical services were a lack of environmental resources and support and a lack of innovation in pharmaceutical services. Perceived enablers were CPs’ knowledge, skills, self‐confidence, actions, impacts, emotions and perceived behavioural control.
Conclusion
To increase the preparedness of pharmacists for future pandemics or disasters, this study highlighted CP‐led cognitive services, precautions taken related to COVID‐19, perceived enablers and barriers and burnout during the COVID‐19 pandemic. Pharmaceutical services guidelines that could be followed during a pandemic or other disaster should be designed by addressing these findings.
What’s known
As members of the primary healthcare team, community pharmacists have an essential role in delivering traditional and cognitive pharmaceutical services during the COVID‐19 pandemic.
What’s new
Community pharmacist‐led cognitive services during the COVID‐19 pandemic were mainly medication information services, preventive healthcare services, and patient counselling for those with chronic disease.
Community pharmacists reported insufficient environmental resources and support and a lack of innovation in pharmaceutical services as barriers during the COVID‐19 pandemic.
1. INTRODUCTION
The World Health Organization (WHO) announced the outbreak of a novel coronavirus disease (COVID‐19) as a Public Health Emergency of International Concern on 30 January 2020, after the disease first emerged in Wuhan, China, in December 2019. 1 More than 122 million people have been infected with COVID‐19, and more than 2.7 million deaths have occurred because of COVID‐19. 2
Community pharmacists (CPs) play a vital role in dispensing medicine and other medical devices and delivering cognitive services (non‐dispensing services such as pharmaceutical care, patient counselling, and the provision of medication information) during disasters. 3 Cognitive pharmaceutical services were defined as “the use of specialized knowledge by the pharmacist for the patient or health professionals for the purpose of promoting effective and safe drug therapy”. 4 Pharmacist‐led cognitive services promote the rational use of medication. In delivering these services (such as health promotion, medication therapy management and preventive healthcare services), pharmacists have a potential impact on the quality of medication therapy and the healthcare delivery system by using their specialist knowledge of medications. 4 , 5 , 6 , 7 , 8 , 9 These services delivered by CPs during disasters are within the scope of pharmacy practice and are usually an extension of the pharmacist's daily routine, which includes ensuring the supply of medicines and the provision of pharmaceutical care services. 3 During the COVID‐19 pandemic, community healthcare systems have been overwhelmed and interrupted due to the higher demands of patients. This pandemic has psychologically affected all healthcare workers, including CPs. 10 In these circumstances, CPs have had little knowledge of how to deliver pharmaceutical services to patients who may have COVID‐19 and those with chronic diseases. Pharmacists may contribute to the early detection and appropriate referral of COVID‐19 patients as well as the provision of patient‐oriented services, education about infection and prevention methods, psychological support and chronic disease management services during a disaster or pandemic. 11 , 12 , 13 , 14 According to guidance from the International Pharmaceutical Federation (FIP), to protect themselves from COVID‐19, CPs in Turkey have taken precautions, such as the regulation of opening hours; social distancing and identification of warning signs; the use of individual protective equipment, such as masks and goggles; the disinfection of pharmacies and the improvement of medical waste management. 15 , 16 However, delivering all these services may overload CPs and cause burnout. There are many definitions of burnout. 17 , 18 , 19 Pines and Aronson 19 defined burnout as a loss of energy, enthusiasm, perspective, idealism and purpose and suggested that it is a state of physical, emotional and mental exhaustion. 18 , 19 Burnout is more common in professionals who communicate directly with people, such as healthcare professionals. 17 Healthcare workers (physicians, nurses and pharmacists) have a high risk of stress, anxiety, depression, burnout, addiction and posttraumatic stress disorder due to the increase in stress and workload during the COVID‐19 pandemic. 20 , 21 , 22 , 23 During the COVID‐19 pandemic, pharmacy employees have been found to have high burnout scores related to many difficulties, such as job stress, a lack of staff and resources, general anxiety, a fear of infection and communication difficulties. 23 , 24 , 25 , 26 , 27 AlAteeq et al 28 showed that during the COVID‐19 pandemic, anxiety and depression were prevalent among healthcare workers in Saudi Arabia. Algunmeeyn et al 24 identified important COVID‐19 pandemic‐related factors, such as job stress, a lack of staff and resources, a fear of COVID‐19 infection and interprofessional relationships in healthcare practice. In a study in France, 35% of CPs reported psychological disturbances. 23 The majority of healthcare workers exposed to COVID‐19 have reported symptoms of depression, anxiety, insomnia and distress. 29 Although the continuity of pharmaceutical services provided by pharmacists is important, CPs’ role in disasters/pandemics has not been defined in detail. 3 The COVID‐19 pandemic is not the first disaster that humanity has faced, and it will not be the last. Thus, CPs’ perceived enablers of and barriers to the delivery of pharmaceutical services under such conditions should be investigated to develop and implement pharmaceutical services guidelines for use in future disasters.
1.1. Objectives of the study and research questions
The objectives of this study were to identify CP‐led cognitive services and CPs’ precautions taken related to COVID‐19, perceived enablers and barriers related to pharmaceutical services and burnout level during the COVID‐19 pandemic. The research questions were listed as follows: (1) Was there any difference in the median score of burnout level according to CPs’ gender and professional year during the COVID‐19 pandemic? (2) Was there any difference in the median score of perceived enablers and barriers components according to CPs’ gender, professional year and burnout status during the COVID‐19 pandemic?
2. METHODS
2.1. Design and sample size
In this descriptive study, a national online survey was conducted with CPs in all regions of Turkey between 21 and 29 May 2020. All Turkish CPs were included this study. A sample size of 379 was required within a 5% margin of error, confidence intervals (CI) of 95%, and expected rate of CPs’ high burnout level of 50% based on the study of Tiete et al. 30 Data were collected using convenience sampling methods. This study is reported according to the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) standards. 31
2.2. Survey distribution and data collection
The survey was uploaded onto the Marmara University web platform provided Lime Survey®. The invitation letter and survey were distributed online by the Turkish pharmacist chambers nationally. Turkish CPs were sent an e‐mail or WhatsApp message containing a link and information regarding the present study. To maximize the response rate, the survey link was posted on websites and social media accounts frequently visited by CPs during their daily professional work. CPs’ consent was obtained electronically. After giving their consent, the participants were directed to the questionnaire.
2.3. Online survey
The online survey consisted of the following five sections: characteristics of CPs (six questions), the Turkish version of the Burnout Measure Short Form, 18 , 32 CP‐led cognitive services during the COVID‐19 pandemic (nine questions), precautions taken by CPs during the COVID‐19 pandemic (four questions) and CPs’ perceived enablers of and barriers to delivering pharmaceutical services during the COVID‐19 pandemic (30 items). There was one open‐ended question that asked CPs for their comments/suggestions about delivering pharmaceutical services during the COVID‐19 pandemic.
Age, gender, duration since graduation (year), professional experience as a CP (year), the region where they lived and position at community pharmacy were collected.
The Burnout Scale Short Form developed by Pines and Aronson 19 , 32 was used to measure occupational burnout, including physical, mental and emotional exhaustion. The Turkish adaptation and validation of this scale was conducted by Capri. 18 Ten items rated on a scale ranging from 1 (never) to 7 (always). Higher scores indicated greater burnout. The threshold was 4, which indicated a critical level of burnout. 18 , 19
Questions related to CP‐led cognitive services during the COVID‐19 pandemic were developed based on a previous classification of cognitive pharmaceutical services. 33 The frequency of the provision of patient counselling (including the frequency compared with that before the pandemic) was evaluated both in general and in relation to the COVID‐19 pandemic based on CP self‐reports. A 5‐point Likert scale from 1 [very decreased or never] to 5 [very increased or always] was used. The frequency of the provision of medication information was evaluated in relation to the COVID‐19 pandemic based on CP self‐reports. Questions on medication information services were fixed items generated using the WHO MythBusters website (which was developed by the WHO to avoid an infodemic [the spread of false or misleading information] during the COVID‐19 pandemic), with slight modifications and additions based on the researchers’ knowledge and experience. 34
The frequency of CPs’ practices towards precautions (including personnel protection procedures and preventive alternative used against COVID‐19 and procedures followed by CP for their employees in COVID‐19 pandemic) were also assessed. These fixed items were generated from national and international guidelines and the researchers’ knowledge and experience.
To evaluate CPs’ perceived enablers of and barriers to delivering pharmaceutical services during the COVID‐19 pandemic, a Turkish version of a 30‐item questionnaire based on the 12‐domain Theoretical Domains Framework (TDF) was generated based on previous studies. 35 , 36 Items relating to behavioural determinants in the TDF were derived from the Determinants of Implementation Behaviour Questionnaire (DIBQ). The domains of the DIBQ are knowledge, skills, social/professional role and identity, beliefs about capabilities, optimism, beliefs about consequences, intentions, goals, innovation, socio‐political context, organization, patient, innovation strategy, social influences, positive emotions, negative emotions, behavioural regulation and nature of the behaviours. 35 The DIBQ uses a 5‐point Likert scale from 1 (strongly disagree/very difficult) to 5 (strongly agree/very easy). A Turkish translation and cultural adaption were conducted by following the World Health Organization process. 37 The expert panel (n = 5) assessed the understandability of the questionnaire. Convenience sampling was used to assess the test‐retest reliability. Thirty pharmacists (who were excluded from the study dataset) completed the questionnaire within a 2‐week interval. Completion of the survey took approximately 15‐20 minutes. CPs’ responses to open‐ended question were analysed according to domains of the questionnaire used.
2.4. Data analysis
Descriptive statistics (such as those used for demographic data and the frequency of cognitive services) are presented as frequencies and percentages. Data normality was assessed by a Kolmogorov‐Smirnov test. All continues variables were non‐normally distributed and represented as median (interquartile range [IQR]). Mann‐Whitney U‐test was used for testing unpaired sample of two groups (male vs. female, CPs with 20 years or less of professional experience vs. CPs with more than 20 years of professional experience, CPs with high level of burnout vs. CPs with low level of burnout) with non‐normally distributed variables. Spearman's rank correlation was used to determine the possible correlations between the continuous variables (such as those used in the test‐retest reliability assessment). The internal consistency of the questionnaire was assessed using Cronbach's alpha coefficient. A principal component analysis (PCA) with varimax rotation was conducted to evaluate the 30‐item questionnaire based on the 12‐domain TDF. The number of components was determined using the total variance explained, a scree plot, assumptions tests, factor loadings and component loadings according to a previous study. 38 The Kaiser‐Meyer‐Olkin (KMO) measure of sampling adequacy and Bartlett's test of sphericity were also used. The data were suitable for principal component analysis, as they met the following conditions: matrix coefficient ≥0.30, KMO sampling adequacy ≥0.60, and Bartlett's test of sphericity ≤0.05. The median and interquartile range of each item and each component of the behavioural determinant questionnaire were calculated. 39 Each item and component were scored from 1 to 5 as described previously. 40 , 41 Negatively phrased items were reverse scored. Based on a previous study, items with low median scores (<3) were considered barriers, and those with high median scores (≥3) were considered enablers. 40 , 42 A P value of less than .05 was considered statistically significant. SPSS version 11.0 was used for data analysis.
2.5. Ethical approval and informed consent
The study received ethical approval by the Uskudar University Non‐Interventional Research Ethics Board (approval number of 61351342‐2020/224 04.05.2020). Study permission was obtained from the Turkish Republic, Ministry of Health. Online informed consent was obtained from all individual participants included in the study.
3. RESULTS
3.1. Participants and demographics of the community pharmacists
A total of 1098 CPs were completed the online survey, for a response rate was 4.11% among 26 747 CPs (Figure 1). The characteristics of the participants are given in Table 1. The median age of the CPs was 41.0 (32.0‐50.0) years, and the majority of the participants (64.8%) were female.
FIGURE 1.
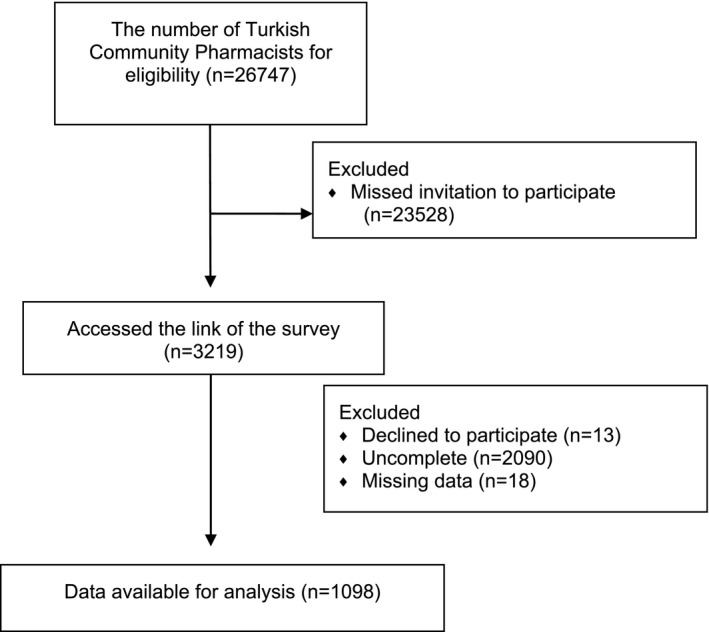
STROBE flow chart
TABLE 1.
Characteristics of community pharmacists (CPs) (N = 1098)
| N | % | |
|---|---|---|
| Age (median [interquartile range]) | 41.0 [32.0‐50.0] | |
| Gender | ||
| Male | 386 | 35.2 |
| Female | 712 | 64.8 |
| Duration since graduation (y) (median [interquartile range]) | 15.0 [5.0‐24.0] | |
| Professional experience as a CP (y) | ||
| ≤5 | 281 | 25.6 |
| 6‐10 | 138 | 12.6 |
| 11‐15 | 161 | 14.7 |
| 16‐20 | 161 | 14.7 |
| >20 | 357 | 32.5 |
| The region where CP lived | ||
| Marmara | 529 | 48.2 |
| Aegean | 126 | 11.5 |
| South‐eastern Anatolia | 124 | 11.3 |
| Black Sea | 108 | 9.8 |
| Mediterranean | 97 | 8.8 |
| Central Anatolia | 86 | 7.8 |
| Eastern Anatolia | 28 | 2.6 |
| Position at community pharmacy | ||
| Owner of community pharmacy | 1025 | 93.4 |
| Second Pharmacist | 26 | 2.4 |
| Assistant Pharmacist | 47 | 4.3 |
| The Burnout Measure, Short Form (BMSF) in COVID‐19 pandemic (median [interquartile range]) | 3.3 [2.5‐4.2] | |
| BMSF score ≥4 | 346 | 31.5 |
| BMSF score <4 | 752 | 68.5 |
3.2. Burnout levels of the community pharmacists
The median burnout score was 3.3 (2.5‐4.2) (Table 1). There were negative correlations between CPs’ burnout level and professional experience (r = −.245, P < .001), and age (r = −.255, P < .001). Female CPs had higher burnout scores than male CPs (3.5 [2.6‐4.3] vs 3.0 [2.2‐4.0], respectively; P < .001).
3.3. Community pharmacist‐led cognitive services during the COVID‐19 pandemic
The CPs reported an increase in the frequency of patient counselling for products related to enhanced immunity (90.8%), dermatological problems (50.2%) and immunization (43.0%). The CPs stated that they frequently provided counselling to patients with chronic disease (71.7%) during the COVID‐19 pandemic. Regarding CP‐led cognitive services, the CPs reported that they responded to questions related to COVID‐19 (86.3%) and provided preventive health services (89.5%) during the COVID‐19 pandemic (Table 2). Overall, more than half of the CPs (54.5%) referred their patients to the hospital if they were suspected to have COVID‐19 (Table 3). The CPs received many questions on different subjects (Table 3). Almost all CPs (95.4%) were asked about the use of herbal and dietary supplements during the COVID‐19 pandemic. The CPs stated that patient resources related to these questions were television (84.8%), friends/neighbours (65.1%), WhatsApp groups (52.1%) and Facebook (50.6%).
TABLE 2.
Community pharmacists’ (CPs’) perceived frequency of cognitive pharmaceutical services during COVID‐19 pandemic (N = 1098)
| CPs’ perceived comparison of the frequency of patient counselling about the following conditions/products in COVID‐19 pandemic with their pre‐pandemic experience | Very decreased N (%) | Decreased N (%) | No change N (%) | Increased N (%) | Very increased N (%) |
|---|---|---|---|---|---|
| Symptoms related with upper respiratory tract infections (URIs) a | 207 (18.9) | 347 (31.6) | 243 (22.1) | 248 (22.6) | 53 (4.8) |
| Diarrhoea | 219 (19.9) | 288 (26.2) | 453 (41.3) | 135 (12.3) | 3 (0.3) |
| Constipation | 113 (10.3) | 180 (16.4) | 521 (47.4) | 258 (23.5) | 26 (2.4) |
| Pain | 66 (6.0) | 167 (15.2) | 464 (42.3) | 361 (32.9) | 40 (3.6) |
| Nausea and vomiting | 137 (12.5) | 266 (24.2) | 543 (49.5) | 146 (13.3) | 6 (0.5) |
| Dyspeptic complaints | 72 (6.6) | 139 (12.7) | 457 (41.6) | 374 (34.1) | 56 (5.1) |
| Minor injuries | 201 (18.3) | 308 (28.1) | 480 (43.7) | 105 (9.6) | 4 (0.4) |
| Dermatological problems (dermatitis, acne vulgaris, rash etc) | 86 (7.8) | 144 (13.1) | 317 (28.9) | 436 (39.7) | 115 (10.5) |
| Cosmetic problems (aging, skin care, moisturizer, sun protection etc) | 234 (21.3) | 262 (23.9) | 354 (32.2) | 207 (18.9) | 41 (3.7) |
| Blood pressure measurement | 471 (42.9) | 262 (23.9) | 269 (24.5) | 83 (7.6) | 13 (1.2) |
| Personal hygiene (mouth and teeth problems, etc) | 138 (12.6) | 277 (25.2) | 346 (31.5) | 257 (23.4) | 80 (7.3) |
| Immunization (flu/pneumonia vaccine) | 165 (15.0) | 137 (12.5) | 324 (29.5) | 364 (33.2) | 108 (9.8) |
| Products related to enhance immunity | 16 (1.5) | 29 (2.6) | 56 (5.1) | 377 (34.3) | 620 (56.5) |
| Medication‐related problems (side effects, toxicity, misuse, drug‐drug interaction etc) | 78 (7.1) | 149 (13.6) | 603 (54.9) | 218 (19.9) | 50 (4.6) |
| Cronbach's alpha: 0.812 |
| CPs’ perceived frequency of patient counselling in special patient population during COVID‐19 pandemic | Never n (%) | Seldom n (%) | Sometimes n (%) |
Often n (%) |
Always n (%) |
|---|---|---|---|---|---|
| Older (≥65 y old) | 31 (2.8) | 249 (22.7) | 225 (20.5) | 439 (40.0) | 154 (14.0) |
| Patients with chronic disease | 5 (0.5) | 110 (10.0) | 196 (17.9) | 573 (52.2) | 214 (19.5) |
| Children | 179 (16.3) | 416 (37.9) | 267 (24.3) | 185 (16.8) | 51 (4.6) |
| Pregnant | 69 (6.3) | 307 (28.0) | 368 (33.5) | 282 (25.7) | 72 (6.6) |
| Breastfeeding | 72 (6.6) | 350 (31.9) | 369 (33.6) | 238 (21.7) | 69 (6.3) |
| Adults | 9 (0.8) | 63 (5.7) | 217 (19.8) | 582 (53.0) | 227 (20.7) |
| Cronbach's alpha: 0.838 |
| CPs’ perceived frequency of cognitive pharmaceutical services during COVID‐19 |
Never n (%) |
Seldom n (%) |
Sometimes n (%) |
Often n (%) |
Always n (%) |
|---|---|---|---|---|---|
| Responding questions related to COVID‐19 | 9 (0.8) | 34 (3.1) | 107 (9.7) | 468 (42.6) | 480 (43.7) |
| Providing preventive health services | 9 (0.8) | 19 (1.7) | 87 (7.9) | 491 (44.7) | 492 (44.8) |
| Pharmaceutical care services in chronic diseases | 96 (8.7) | 164 (14.9) | 267 (24.3) | 326 (29.7) | 245 (22.3) |
| Pharmaceutical care services in minor illness | 88 (8.0) | 189 (17.2) | 298 (27.1) | 327 (29.8) | 196 (17.9) |
| Pharmaceutical care services in high‐risk population (such as older, cancer patients) | 176 (16.0) | 233 (21.2) | 251 (22.9) | 282 (25.7) | 156 (14.2) |
| Patients and/or relatives counselling regarding COVID‐19 | 218 (19.9) | 249 (22.7) | 262 (23.9) | 183 (16.7) | 186 (16.9) |
| Providing patient counselling to people applied to pharmacy | 61 (5.6) | 209 (19.0) | 276 (25.1) | 343 (31.2) | 209 (19.0) |
| Cronbach's alpha: 0.851 |
URI symptoms were considered such as fever, fatigue, cough.
TABLE 3.
Community pharmacists’ (CPs’) practices towards suspicion COVID‐19 patients and medication information services in COVID‐19 pandemic (N = 1098)
| N | % | |
|---|---|---|
| CPs’ practices towards patients with probable COVID‐19 | ||
| Referring the patients to the hospital with probable of COVID‐19 (n = 1098) | ||
| Yes | 598 | 54.5 |
| No | 500 | 45.5 |
| Procedure that CP followed a (n = 598) | ||
| Immediately suggesting them to go to hospital. | 573 | 95.8 |
| Calling Ministry of Health Communication Center | 31 | 5.2 |
| Disinfecting the pharmacy after patient left | 451 | 75.4 |
| Other | 35 | 5.9 |
| CPs’ medication information services in COVID‐19 pandemic | ||
| Questions gathered from individuals in COVID‐19 pandemic a | ||
| Hypertensive medication usage especially angiotensin‐converting inhibitors during COVID‐19 pandemic | 645 | 58.7 |
| Painkillers usage especially ibuprofen during COVID‐19 pandemic | 954 | 86.9 |
| Prophylactic effect of quinine containing beverages | 495 | 45.1 |
| Complementary and alternative medicine | 602 | 54.8 |
| Herbal/dietary supplements | 1047 | 95.4 |
| Clinical trials for COVID‐19 | 789 | 71.9 |
| Flu and pneumonia vaccination during COVID‐19 pandemic | 762 | 69.4 |
| None | 14 | 1.3 |
| Other | 155 | 14.1 |
| Resources of above questions mentioned by their patients a | ||
| Television | 931 | 84.8 |
| 556 | 50.6 | |
| 308 | 28.1 | |
| 405 | 36.9 | |
| Friend/Neighbour | 715 | 65.1 |
| WhatsApp Groups | 572 | 52.1 |
| Newspaper | 210 | 19.1 |
| Unknown | 223 | 20.3 |
| Other | 15 | 1.4 |
| Information resources of CPs regarding COVID‐19 a | ||
| Turkish Ministry of Health | 1006 | 91.6 |
| US Center for Disease Control and Prevention‐CDC | 86 | 7.8 |
| Turkish Pharmacists' Association‐TPA | 694 | 63.2 |
| World Health Organization‐WHO | 654 | 59.6 |
| Food and Drug Administration‐FDA | 151 | 13.8 |
| PubMed | 164 | 14.9 |
| Internet such as Google | 328 | 29.9 |
| Universities database on COVID‐19 | 397 | 36.2 |
| Physicians | 691 | 62.9 |
| Other Pharmacists | 722 | 65.8 |
| Social Media Groups | 522 | 47.5 |
| None | 2 | 0.2 |
| Other | 35 | 3.2 |
| CPs’ level of information based on their self‐evaluation and perceived information regarding the COVID‐19 pandemic | ||
| Sufficient | 803 | 73.1 |
| Insufficient | 295 | 26.9 |
Multiple choice would be selected.
3.4. Precautions taken by the community pharmacists during the COVID‐19 pandemic
The most common personal protection measures used by the CPs were avoiding direct contact (93.7%), more frequently washing their hands (93.2%) and using masks (92.8%). Of all CPs studied, 19.1% took hydroxychloroquine tablets as an unproven preventive agent against COVID‐19 (Table 4).
TABLE 4.
Community pharmacists’ (CPs’) practices towards precautions in COVID‐19 pandemic (N = 1098)
| CPs’ precautions in COVID‐19 pandemic | n | % |
|---|---|---|
| Precautions followed by CPs a | ||
| Allowing limited number of people in community pharmacy at the same time | 786 | 71.6 |
| Dispensing in front of the door at community pharmacy | 324 | 29.5 |
| Restriction of the areas that patients could enter | 776 | 70.7 |
| Making protective materials within the community pharmacy | 593 | 54.0 |
| Increasing the frequency of disinfection and sterilization | 996 | 90.8 |
| Setting up a UV sterilization lamps | 97 | 8.8 |
| None | 4 | 0.4 |
| Other | 33 | 3.0 |
| Personnel protection procedures used by CPs a | ||
| Avoiding direct contact | 1029 | 93.7 |
| Washing their hands with soap for at least 20 s | 1023 | 93.2 |
| Frequently used hand sanitizers | 988 | 90.0 |
| Using mask | 1019 | 92.8 |
| Wearing Gloves | 302 | 27.5 |
| Wearing safety googles | 429 | 39.1 |
| Using whole body protective suits | 97 | 8.8 |
| None | 4 | 0.4 |
| Other | 36 | 3.3 |
| Uncertain preventive alternative used against COVID‐19 a | ||
| Hydroxychloroquine tablet | 210 | 19.1 |
| Diosmin + hesperidin | 40 | 3.6 |
| Lugol solution | 29 | 2.6 |
| Povidone iodine mouthwash | 45 | 4.1 |
| Pneumococcal vaccine | 47 | 4.3 |
| Flu vaccine | 51 | 4.6 |
| None | 705 | 64.2 |
| Other | 116 | 10.6 |
| Procedures followed by CP for their employees in COVID‐19 pandemic a | ||
| Rearranging working shifts | 606 | 55.2 |
| Providing pharmacy personal protective gears and equipment | 1006 | 91.6 |
| Allowing their staff with chronic illness or advanced age to stay home. | 110 | 10.0 |
| Suggesting to their staff with symptoms of URI (upper respiratory tract infection) stay in quarantine for 14 d | 88 | 8.0 |
| None | 39 | 3.6 |
| Other | 117 | 10.7 |
Multiple choice would be selected.
3.5. Community pharmacists’ perceived enablers of and barriers to delivering pharmaceutical services during the COVID‐19 pandemic
The CPs reported more enablers of than barriers to the delivery of pharmaceutical services during the COVID‐19 pandemic. Of the 30 TDF items, the CPs rated nine items as barriers (items with a median score <3) to the delivery of pharmaceutical services during the COVID‐19 pandemic; however, they rated 21 items as enablers (items with a median score ≥3; Tables 5, 6, 7, 8, 9).
TABLE 5.
Community pharmacists’ (CPs’) perceived enablers of and barriers related with knowledge, skills and self‐confidence in delivering pharmaceutical services during the COVID‐19 pandemic (N = 1098)
| Median [IQR] | Strongly disagreed (%) | Disagree (%) | Neither agree nor disagree (%) | Agree (%) | Strongly agree (%) | |
|---|---|---|---|---|---|---|
| Component 1‐Knowledge, skills and self‐confidence | ||||||
| I know how to deliver pharmaceutical services in the COVID‐19 pandemic | 4.0 [4.0‐5.0] | 28 (2.6) | 50 (4.6) | 143 (13.0) | 585 (53.3) | 292 (26.6) |
| My role as a pharmacist in the COVID‐19 pandemic is clearly defined for me | 3.0 [2.0‐4.0] | 159 (14.5) | 290 (26.4) | 276 (25.1) | 277 (25.2) | 96 (8.7) |
| I have been trained to deliver pharmaceutical services in the COVID‐19 pandemic | 2.0 [1.0‐3.0] | 308 (28.1) | 379 (34.5) | 176 (16.0) | 182 (16.6) | 53 (4.8) |
| I am confident about how to deliver pharmaceutical services in the COVID‐19 pandemic | 4.0 [4.0‐5.0] | 10 (0.9) | 28 (2.6) | 128 (11.7) | 561 (51.1) | 371 (33.8) |
| I have long‐term goals related to delivering pharmaceutical services in the COVID‐19 pandemic | 3.0 [3.0‐4.0] | 34 (3.1) | 171 (15.6) | 439 (40.0) | 316 (28.8) | 138 (12.6) |
| I have a clear plan how I will deliver pharmaceutical services in the COVID‐19 pandemic | 4.0 [3.0‐4.0] | 32 (2.9) | 155 (14.1) | 343 (31.2) | 487 (44.4) | 81 (7.4) |
| I have a clear plan when I will deliver pharmaceutical services in the COVID‐19 pandemic | 4.0 [3.0‐4.0] | 36 (3.3) | 166 (15.1) | 345 (31.4) | 468 (42.6) | 83 (7.6) |
| Delivering pharmaceutical services in the COVID‐19 pandemic is something I do routinely | 4.0 [2.0‐4.0] | 80 (7.3) | 227 (20.7) | 193 (17.6) | 487 (44.4) | 111 (10.1) |
|
Cronbach's alpha: 0.812 Median: 3.38 IQR (interquartile range): 3.0‐3.8 |
||||||
TABLE 6.
Community pharmacists’ (CPs’) perceived enablers of and barriers related with action and impact of delivering pharmaceutical services during COVID‐19 pandemic (N = 1098)
| Median [IQR] | Strongly disagreed (%) | Disagree (%) | Neither agree nor disagree (%) | Agree (%) | Strongly agree (%) | |
|---|---|---|---|---|---|---|
| Component 2‐Action and impact | ||||||
| It is part of my work to deliver pharmaceutical services in the COVID‐19 pandemic | 5.0 [4.0‐5.0] | 19 (1.7) | 9 (0.8) | 31 (2.8) | 400 (36.4) | 639 (58.2) |
| If I deliver pharmaceutical services in the COVID‐19 pandemic, my patients will appreciate this | 4.0 [3.0‐4.0] | 109 (9.9) | 154 (14.0) | 261 (23.8) | 358 (32.6) | 216 (19.7) |
| If I deliver pharmaceutical services in the COVID‐19 pandemic, I will get professional satisfaction | 4.0 [4.0‐5.0] | 38 (3.5) | 66 (6.0) | 118 (10.7) | 480 (43.7) | 396 (36.1) |
| If I deliver pharmaceutical services in the COVID‐19 pandemic, it will benefit public health | 5.0 [4.0‐5.0] | 8 (0.7) | 7 (0.6) | 22 (2.0) | 426 (38.8) | 635 (57.8) |
| I have short‐term goals to delivering pharmaceutical services in the COVID‐19 pandemic | 3.0 [3.0‐4.0] | 48 (4.4) | 184 (16.8) | 393 (35.8) | 394 (35.9) | 79 (7.2) |
| Most people who are important to me think that I should deliver pharmaceutical services in the COVID‐19 pandemic | 4.0 [3.0‐4.0] | 34 (3.1) | 96 (8.7) | 218 (19.9) | 549 (50.0) | 201 (18.3) |
| Other pharmacists I know influence me to deliver pharmaceutical services in the COVID‐19 pandemic | 3.0 [2.0‐4.0] | 94 (8.6) | 293 (26.7) | 237 (21.6) | 407 (37.1) | 67 (6.1) |
| Other health professionals think I should deliver pharmaceutical services in the COVID‐19 pandemic | 4.0 [3.0‐4.0] | 32 (2.9) | 90 (8.2) | 207 (18.9) | 627 (57.1) | 142 (12.9) |
| Other health professionals are helpful in delivering pharmaceutical services in the COVID‐19 pandemic | 3.0 [3.0‐4.0] | 78 (7.1) | 182 (16.6) | 336 (30.6) | 425 (38.7) | 77 (7.0) |
| When I deliver pharmaceutical services in COVID‐19 pandemic, I feel optimistic | 4.0 [3.0‐5.0] | 44 (4.0) | 76 (6.9) | 186 (16.9) | 513 (46.7) | 279 (25.4) |
| For me, delivering pharmaceutical services in COVID‐19 pandemic is (not worthwhile at all— very worthwhile) | 4.0 [4.0‐5.0] | 35 (3.2) | 47 (4.3) | 116 (10.6) | 415 (37.8) | 485 (44.2) |
|
Cronbach's alpha: 0.821 Median:3.8 IQR (interquartile range): 3.4‐4.2 |
||||||
TABLE 7.
Community pharmacists (CPs’) perceived enablers of and barriers related with innovation characteristic of delivering pharmaceutical services during the COVID‐19 pandemic (N = 1098)
| Median [IQR] | Strongly disagreed (%) | Disagree (%) | Neither agree nor disagree (%) | Agree (%) | Strongly agree (%) | |
|---|---|---|---|---|---|---|
| Component 3‐Innovation characteristic | ||||||
| Pharmaceutical services in the COVID‐19 pandemic cost little time to perform | 2.0 [1.0‐2.0] | 390 (35.5) | 453 (41.3) | 115 (10.5) | 111 (10.1) | 29 (2.6) |
| Pharmaceutical services in the COVID‐19 are simple to perform | 2.0 [1.0‐2.0] | 486 (44.3) | 439 (40.0) | 76 (6.9) | 78 (7.1) | 19 (1.7) |
| Pharmaceutical services in the COVID‐19 are compatible with routine pharmacy practice | 2.0 [1.0‐2.0] | 405 (36.9) | 440 (40.1) | 110 (10.0) | 121 (11.0) | 22 (2.0) |
|
Cronbach's alpha: 0.743 Median: 2.0 IQR (interquartile range): 1.3‐2.3 |
||||||
TABLE 8.
Community pharmacists (CPs’) perceived enablers of and barriers related with environmental resources and support in delivering pharmaceutical services during the COVID‐19 pandemic (N = 1098)
| Median [IQR] | Strongly disagree (%) | Disagree (%) | Neither agree nor disagree (%) | Agree (%) | Strongly agree (%) | |
|---|---|---|---|---|---|---|
| Component 4‐Environmental resources and support | ||||||
| The government and local authorities provide sufficient support to deliver pharmaceutical services in the COVID‐19 pandemic | 2.0 [1.0‐2.0] | 548 (49.9) | 337 (30.7) | 136 (12.4) | 59 (5.4) | 18 (1.6) |
| The Turkish Pharmacists Association and the pharmacists chamber of which I’m a member make it easy to reach all necessary resources to deliver pharmaceutical services in the COVID‐19 pandemic | 2.0 [1.0‐3.0] | 399 (36.3) | 282 (25.7) | 205 (18.7) | 167 (15.2) | 45 (4.1) |
| The Turkish Pharmacists Association and the pharmacists chamber of which I’m a member provides sufficient materials to deliver pharmaceutical services in the COVID‐19 pandemic | 2.0 [1.0‐3.0] | 396 (36.1) | 294 (26.8) | 191 (17.4) | 168 (15.3) | 49 (4.5) |
| The Turkish Pharmacists Association and the pharmacists chamber of which I’m a member help me regarding delivering pharmaceutical services in the COVID‐19 pandemic | 2.0 [1.0‐3.0] | 333 (30.3) | 280 (25.5) | 231 (21.0) | 203 (18.5) | 51 (4.6) |
|
Cronbach's alpha: 0.874 Median: 2.0 IQR (interquartile range): 1.2‐3.0 |
||||||
TABLE 9.
Community pharmacists (CPs’) perceived enablers of and barriers related with emotions and perceived behavioural control in delivering pharmaceutical services during the COVID‐19 pandemic (N = 1098)
| Median [IQR] | Strongly disagree (%) | Disagree (%) | Neither agree nor disagree (%) | Agree (%) | Strongly agree (%) | |
|---|---|---|---|---|---|---|
| Component 5‐Emotions and perceived behavioural control | ||||||
| When I deliver pharmaceutical services in the COVID‐19 pandemic, I feel comfortable | 3.0 [2.0‐4.0] | 98 (8.9) | 289 (26.3) | 288 (26.2) | 298 (27.1) | 125 (11.4) |
| When I deliver pharmaceutical services in the COVID‐19 pandemic, I feel nervous a | 3.0 [2.0‐4.0] | 92 (8.4) | 371 (33.8) | 279 (25.4) | 279 (25.4) | 77 (7.0) |
| I worry about delivering pharmaceutical services in the COVID‐19 pandemic a | 3.0 [2.0‐4.0] | 131 (11.9) | 405 (36.9) | 227 (20.7) | 285 (26.0) | 50 (4.6) |
| For me, delivering pharmaceutical services in the COVID‐19 pandemic is (very difficult‐ very easy) | 2.0 [2.0‐2.0] | 266 (24.2) | 588 (53.6) | 96 (8.7) | 131 (11.9) | 17 (1.5) |
|
Cronbach's alpha: 0.721 Median: 3.0 IQR (interquartile range): 2.2‐3.5 |
||||||
Reversed items.
According to PCA, the KMO measure of sampling adequacy was 0.890, and Bartlett's test was significant (P < .001). The extracted five‐factor model accounted for 53.0% of the total variance. The Cronbach's alpha coefficients of each component ranged from 0.721 to 0.874. The test‐retest reliability was confirmed by a positive correlation between the findings within a 2‐week interval (r = .828; P < .001).
Component 1 (CPs’ knowledge, skills, and self‐confidence) and Component 2 (CPs’ actions and impacts following the delivery of pharmaceutical services during the COVID‐19 pandemic) were enablers, as they had high median scores (3.38 [3.0‐3.8] and 3.8 [3.4‐4.2], respectively). Regarding Component 1, most CPs (79.9%) reported that they knew how to deliver pharmaceutical services during the COVID‐19 pandemic (4.0 [4.0‐5.0]). However, in response to another item related to knowledge about their roles as pharmacists during the COVID‐19 pandemic, 40.9% reported that the pharmacist role was not clearly defined (3.0 [2.0‐4.0]). More than half (62.6%) reported that they had not been trained with the necessary skills on how to act as pharmacists during the COVID‐19 pandemic (2.0 [1.0‐3.0]). However, most participants (84.9%) reported that they were confident about how to act as pharmacists during the COVID‐19 pandemic (4.0 [4.0‐5.0]). Regarding Component 2, items related to outcome expectancies and attitudes had higher median scores, meaning that they enabled the delivery of pharmaceutical services during the COVID‐19 pandemic.
Component 3 (innovative characteristics of pharmaceutical services) and Component 4 (environmental resources and support) were barriers to service delivery during the COVID‐19 pandemic, as they had low median scores (2.0 [1.3‐2.3] and 2.0 [1.2‐3.0], respectively). Regarding Component 3, 84.3% of the CPs described pharmaceutical services during the COVID‐19 pandemic as complex to perform (2.0 [1.0‐2.0]). Almost three‐quarters of the CPs disagreed that pharmaceutical services during the COVID‐19 pandemic took little time (2.0 [1.0‐2.0]) and were compatible with routine pharmacy practice (2.0 [1.0‐2.0]). Regarding Component 4, the socio‐political domain of environmental resources and support received the lowest median scores (2.0 [1.2‐3.0]). The CPs indicated that the government and local authorities provided insufficient support to them during the COVID‐19 pandemic. Table 8 show that four items relating to environmental resources and support constituted barriers. The CPs reported a lack of organizational resources and support from the Turkish Pharmacists Association and their pharmacist chambers. Finally, Component 5 (CPs’ emotions and perceived behavioural control) was an enabler, as it had a high median score (3.0 [2.2‐3.5]). Of all CPs, 77.8% stated that delivering pharmaceutical services during the COVID‐19 pandemic was “difficult” or “very difficult”; this finding was related to the beliefs about the capability domains of the TDF (2.0 [2.0‐2.0]).
3.6. Factors related to the community pharmacists’ perceived enabler and barrier determinants during the COVID‐19 pandemic
The median score for Component 3 (innovative characteristics of pharmaceutical services; female CPs = 2.0 [1.3‐2.3], male CPs = 2.0 [1.3‐2.7]; P < .05) and Component 5 (CPs’ emotions and perceived behavioural control; female CPs = 2.8 [2.2‐3.5], male CPs = 3.0 [2.5‐3.5]) showed that there were significant differences between female and male CPs (P < .05). CPs with more than 20 years of professional experience had a higher median score of the components than CPs with 20 years or less of professional experience (Component 1 = 3.50 [3.1‐3.9] vs 3.2 [2.9‐3.6], Component 2 = 3.9 [3.6‐4.3] vs 3.7 [3.4‐4.1], Component 4 = 2.2 [1.8‐3.0] vs 2.0 [1.0‐2.8] and Component 5 = 3.0 [2.5‐3.5] vs 2.8 [2.2‐3.5], respectively; P < .05). The median score of Component 3 (CPs with more than 20 years of professional experience: 2.0 [1.3‐2.7] vs CPs with 20 years or less of professional experience: 2.0 [1.3‐2.3]) showed that there was a significant difference between according to professional experience of the CPs (P < .05). CPs with high burnout levels had a significantly lower median score for all components than CPs with low burnout levels (Component 1 = 3.1 [2.6‐3.5] vs 3.5 [3.1‐0.39], Component 2 = 3.5 [3.1‐4.0] vs 3.9 [3.6‐4.2], Component 3 = 1.7 [1.0‐2.0] vs 2.0 [1.3‐2.7], Component 4 = 1.8 [1.0‐2.5] vs 2.2 [1.5‐3.0] and Component 5 = 2.2 [2.0‐3.0] vs 3.0 [2.5‐3.5], respectively; P < .05).
3.7. Community pharmacists’ comments and suggestions about delivering pharmaceutical services during the COVID‐19 pandemic
Among the 1098 CPs, 321 responded to the open‐ended questions. They reported that they understood their professional responsibilities and the importance of their roles as health counsellors and that they were pleased with the services they provided during the pandemic. These findings corresponded with the enablers identified in the questionnaire. The CPs thought that they should be informed earlier and that they needed more education and training about the COVID‐19 pandemic. The CPs suggested the preparation of an emergency action plan in such situations. They noted that they could not obtain sufficient support from public authorities, the Turkish Pharmacists Association, their pharmacist chambers, or pharmacy faculty/academics. Most of the CPs who completed this part of the survey mentioned the problems they experienced with the supply and distribution of masks in Turkey, which had a negative impact on their professional reputations and relationships with their patients. They thought this process could be appropriately and feasibly designed with their involvement. They reported that they expected to receive appreciation and financial support, especially for the provision of masks and disinfectant, from professional organizations or the government. Such expectations could be considered to reinforce the provision of pharmaceutical services during the COVID‐19 pandemic as well as to be an outcome of the provision of such services.
4. DISCUSSION
This study highlighted CP‐led cognitive services, precautions taken related to COVID‐19, perceived enablers and barriers, and burnout during the COVID‐19 pandemic. The cognitive services delivered by the CPs mainly included medication information services, preventive healthcare services and patient counselling for patients with chronic disease. During the COVID‐19 pandemic, the CPs had high burnout levels. More than half of the CPs referred probable COVID‐19 patients to the hospital. The most common personal protection measures used by the CPs were avoiding direct contact, more frequently washing their hands, and using masks. Future disaster work plans should consider the barriers (a lack of innovative characteristics and insufficient of environmental resources and support) and enablers (knowledge, skills and self‐confidence, actions and impacts and preparedness, emotions and perceived behavioural control) to pharmaceutical service delivery identified in this study.
In the present study, higher levels of burnout were associated with the female gender, younger age and less professional experience at the time of the COVID‐19 pandemic. Barello et al 43 showed a high level of burnout in Italian health care professionals at the beginning of the COVID‐19 pandemic. Lange et al found high burnout symptoms in French CPs (approximately one‐third) during the first wave of COVID‐19. 23 This study showed that in Turkey, 2 months after the first COVID‐19 case was confirmed, almost one‐third of CPs experienced burnout. Female health care providers were previously found to be more likely to experience burnout during the COVID‐19 pandemic. 43 , 44 This finding was in line with the results of the present study. Burnout in health care professionals has been associated with job stress, time pressure, workload and a lack of organizational support. 45 According to the job demands‐resources model, 46 Gaither et al 47 suggested that high job demands were associated with emotional exhaustion in pharmacists. Similar to our findings, the findings of Calgan et al 48 showed that Turkish CPs’ burnout levels were associated with age and duration of professional experience.
The CPs in this study reported an increase in the frequency of patient counselling for products related to enhanced immunity, dermatological problems and immunization during the COVID‐19 pandemic. Regarding CP‐led cognitive services, the CPs responded to patients’ questions related to COVID‐19 and provided preventive health services during the COVID‐19 pandemic. Almost all CPs were asked about the use of herbal and dietary supplements during the COVID‐19 pandemic. These findings were line with those of a previous study. 49 Hoti et al 50 noted the beneficial impact of pharmacy chamber‐led dissemination of related information regarding COVID‐19.
Unexpectedly, 51 , 52 CPs’ provision of patient counselling regarding minor ailments decreased during the COVID‐19 pandemic. More than half of the CPs stated that they immediately referred patients they suspected to have COVID‐19 to the hospital. This finding was similar to that of a previous study, in which most CPs reported that they knew what to do when encountering patients with suspected COVID‐19. 53 This finding highlighted CPs' public health services during the COVID‐19 pandemic. Most patients asked CPs questions related to COVID‐19 to confirm uncertain information and insufficient evidence. This finding showed that CPs should advise and instruct their patients regarding COVID‐19 after reviewing the evidence. Although there is no evidence of the protective effect of hydroxychloroquine against COVID‐19, almost one‐fifth of the pharmacists used it prophylactically. In line with previous studies, 50 , 53 , 54 , 55 most CPs followed precautions, including avoiding direct contact, washing their hands and using masks.
This study identified several barriers perceived by CPs during the COVID‐19 pandemic. Insufficient environmental resources and support and a lack of innovative characteristics of pharmaceutical services during the COVID‐19 pandemic were the most common barriers reported by CPs. These findings were line with previous study. 56 The CPs’ lack of knowledge about their roles and skills needed during the COVID‐19 pandemic were also indicated as barriers. Behaviour change strategies could be used to develop and implement interventions targeting these barriers, which were identified using the TDF. Michie et al 57 first described the 12 domains of the TDF, which are relevant to behaviour change processes and could be used to develop and implement evidence‐based services. Cane et al 58 identified a relationship between the TDF and Michie et al’s behaviour changes technique taxonomy. 59 According to these studies, 58 , 59 instructions on how to perform behaviours, problem solving, the demonstration of behaviours, behavioural practice or rehearsal and graded tasks could be effective in overcoming barriers related to knowledge, skills and beliefs about capabilities. This is consistent with a previous study that determined that training had a significant positive impact on the knowledge, skills, professional role, beliefs about capabilities and goal domains of the TDF in relation to CP‐led services for patients requiring urgent care. 60 Barriers related to environmental resources and support might be addressed through social support (practical), prompts/cues and the addition of tools and resources to the environment. 58 , 59 Changes at the organizational and health system levels could be required to cope with barriers related to environmental resources and support during a pandemic. The development and implementation of interventions targeting these domains could be more effective for such situations. 61
4.1. Limitations of the study
This study was a national survey with an adequate sample size. However, there could be sampling bias (selection and response bias) because CPs who frequently used the Internet and/or more interest in cognitive pharmaceutical services may have been more likely to participate in the survey. This could impact the generalizability of the results to all CPs in Turkey. Another strength was the theory‐based approach using the TDF taken in this study to determine enablers of and barriers to the delivery of pharmaceutical services (both traditional and cognitive services) during the COVID‐19 pandemic. However, changes in the frequency of traditional services were not evaluated in this study. Although each domain could have been represented by a larger number of items, this approach could have resulted in a longer time to complete the questionnaire, and the questionnaire acceptability to the participants may then have been decreased. The open‐ended question provided additional qualitative information about the CPs’ perceptions, opinions, suggestions, expectations, and perceived barriers related to delivering pharmaceutical services during the COVID‐19 pandemic. This knowledge clarified potential factors related to pharmaceutical activities during the COVID‐19 pandemic. An analysis of the qualitative data may highlight other potential factors that could influence the behaviour of CPs. The burnout levels of the CPs were measured according to their self‐reported data approximately 2 months after the COVID‐19 pandemic started in Turkey. This strategy did not allow a comparison with baseline data. Many other factors (such as the workload in the pharmacy and the presence of pharmacy staff) could have impacted CP burnout.
4.2. Conclusion
The COVID‐19 pandemic has impacted every aspect of life. In primary care, CPs have an important role in referring probable COVID‐19 patients to the hospital and delivering cognitive services, such as providing medication information in response to patients’ questions about using medication during the COVID‐19 pandemic and providing patient counselling, especially for patients with noncommunicable diseases with or without COVID‐19. To increase the preparedness of pharmacists for future pandemics or disasters, we determined the impact of the pandemic on CPs by assessing their burnout levels, the precautions they took, and their perceived enablers of and barriers to service delivery. Through the theory‐based examination conducted in this study, we identified barriers related to TDF domains that could be used to develop and implement complex interventions to promote and maintain pharmaceutical service delivery during a pandemic or other disaster. To our knowledge, this is the first study investigating CP‐led cognitive services, burnout, precautions taken and perceived enablers of and barriers to delivering pharmaceutical services during the COVID‐19 pandemic.
DISCLOSURES
The authors declare that there is no conflict of interest.
ACKNOWLEDGEMENT
We would like to thank all CPs who completed the survey, all healthcare workers who have been working on the frontline and those who lost their lives during the COVID‐19 pandemic.
Okuyan B, Bektay MY, Kingir ZB, Save D, Sancar M. Community pharmacy cognitive services during the COVID‐19 pandemic: A descriptive study of practices, precautions taken, perceived enablers and barriers and burnout. Int J Clin Pract. 2021;75:e14834. 10.1111/ijcp.14834
Funding information
None.
DATA AVAILABILITY STATEMENT
Author elects to not share data.
REFERENCES
- 1. World Health Organisation WHO. WHO Director‐General's statement on IHR Emergency Committee on Novel Coronavirus (2019‐nCoV). https://www.who.int/director‐general/speeches/detail/who‐director‐general‐s‐statement‐on‐ihr‐emergency‐committee‐on‐novel‐coronavirus‐(2019‐ncov). Accessed March 23, 2021.
- 2. World Health Organisation WHO . Coronavirus disease (COVID‐19) pandemic Weekly operational update on COVID‐19 ‐ 22 March 2021; 2021. https://www.who.int/publications/m/item/weekly‐operational‐update‐on‐covid‐19‐‐‐22‐march‐2021. Accessed March 23, 2021.
- 3. Watson KE, Singleton JA, Tippett V, Nissen LM. Defining pharmacists’ roles in disasters: a Delphi study. PLoS One. 2019;14:e0227132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cipolee RJ, Strand LM. Pharmaceutical Care Practice. The Patient‐Centered Approach to Medication Management. McGraw‐Hill Companies; 1998. [Google Scholar]
- 5. Sáez‐Benito L, Fernandez‐Llimos F, Feletto E, et al. Evidence of the clinical effectiveness of cognitive pharmaceutical services for aged patients. Age Ageing. 2013;42:442‐449. [DOI] [PubMed] [Google Scholar]
- 6. Nkansah N, Mostovetsky O, Yu C, et al. Effect of outpatient pharmacists' non‐dispensing roles on patient outcomes and prescribing patterns. Cochrane Database Syst Rev. 2010;2010:CD000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Beney J, Bero LA, Bond C. Expanding the roles of outpatient pharmacists: effects on health services utilisation, costs, and patient outcomes. Cochrane Database Syst Rev. 2000;3:CD000336. [DOI] [PubMed] [Google Scholar]
- 8. Mohammed MA, Moles RJ, Chen TF. Impact of pharmaceutical care interventions on health‐related quality‐of‐life outcomes: a systematic review and meta‐analysis. Ann Pharmacother. 2016;50:862‐881. [DOI] [PubMed] [Google Scholar]
- 9. Milosavljevic A, Aspden T, Harrison J. Community pharmacist‐led interventions and their impact on patients' medication adherence and other health outcomes: a systematic review. Int J Pharm Pract. 2018;26:387‐397. [DOI] [PubMed] [Google Scholar]
- 10. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID‐19) on medical staff and general public ‐ a systematic review and meta‐analysis. Psychiatry Res. 2020;291:113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cadogan CA, Hughes CM. On the frontline against COVID‐19: community pharmacists’ contribution during a public health crisis. Res Social Adm Pharm. 2021;17:2032‐2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zheng S‐Q, Yang L, Zhou P‐X, Li H‐B, Liu F, Zhao R‐S. Recommendations and guidance for providing pharmaceutical care services during COVID‐19 pandemic: a China perspective. Res Social Adm Pharm. 2021;17:1819‐1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ung COL. Community pharmacist in public health emergencies: quick to action against the coronavirus 2019‐nCoV outbreak. Res Social Adm Pharm. 2020;16:583‐586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Paudyal V, Cadogan C, Fialová D, et al. Provision of clinical pharmacy services during the COVID‐19 pandemic: Experiences of pharmacists from 16 European countries. Res Social Adm Pharm. 2021;17:1507‐1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. International Pharmaceutical Federation FIP . Coronavirus SARS‐CoV‐2 / COVID‐19 Pandemic: Information and interim guidelines for pharmacists and the pharmacy workforce. 2020;29. https://www.fip.org/files/content/priority‐areas/coronavirus/COVID‐19‐Guidelines‐for‐pharmacists‐and‐the‐pharmacy‐workforce.pdf. Accessed March 23, 2021.
- 16. T.C. Sağlık Bakanlığı Türkiye İlaç ve Tıbbi Cihaz Kurumu. Serbest Eczaneler İçin Alınması Gereken Pandemi Tedbirleri Hakkında [Turkish]. 2020. https://titck.gov.tr/storage/Archive/2020/announcement/PandemiTedbirleri_28c0b97b‐827d‐44fe‐ad4b‐48438060a34c.pdf. Accessed March 23, 2021.
- 17. Maslach C. Burnout: The Cost of Caring. Prentice‐Hall; 1982. [Google Scholar]
- 18. Capri B. The Turkish Adaptation of the Burnout Measure‐Short Version (BMS) and Couple Burnout Measure‐Short Version (CBMS) and the Relationship between Career and Couple Burnout Based on Psychoanalytic‐Existential Perspective. Educ Sci Theory Pract. 2013;13:1408‐1417. [Google Scholar]
- 19. Pines A, Aronson E. Career Burnout: Causes and Cures. Free Press; 1988. [Google Scholar]
- 20. Yıldırım M, Solmaz F. COVID‐19 burnout, COVID‐19 stress and resilience: initial psychometric properties of COVID‐19 Burnout Scale. Death Stud. 2020:1‐9. doi: 10.1080/07481187.2020.1818885 [DOI] [PubMed] [Google Scholar]
- 21. Shah K, Chaudhari G, Kamrai D, Lail A, Patel RS. How essential is to focus on physician's health and burnout in coronavirus (COVID‐19) pandemic? Cureus. 2020;4:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wu Y, Wang J, Luo C, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID‐19 epidemic in Wuhan, China. J Pain Symptom Manage. 2020;60:e60‐e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lange M, Joo S, Couette PA, de Jaegher S, Joly F, Humbert X. Impact on mental health of the COVID‐19 outbreak among community pharmacists during the sanitary lockdown period. Ann Pharm Fr. 2020;78:459‐463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Algunmeeyn A, El‐Dahiyat F, Altakhineh M, Azab M, Babar Z‐U‐D. Understanding the factors influencing healthcare providers' burnout during the outbreak of COVID‐19 in Jordanian hospitals. J Pharm Policy Pract. 2020;53:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ashiru‐Oredope D, Chan AHY, Olaoye O, Rutter V, Babar Z. Needs assessment and impact of COVID‐19 on pharmacy professionals in 31 commonwealth countries. J Pharm Policy Pract. 2020;13:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Johnston K, O’Reilly CL, Cooper G, Mitchell I. The burden of COVID‐19 on pharmacists. J Am Pharm Assoc (2003). 2021;61:e61‐e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Patel SK, Kelm MJ, Bush PW, Lee HJ, Ball AM. Prevalence and risk factors of burnout in community pharmacists. J Am Pharm Assoc (2003). 2021;61:145‐150. [DOI] [PubMed] [Google Scholar]
- 28. AlAteeq DA, Aljhani S, Althiyabi I, Majzoub S. Mental health among healthcare providers during coronavirus disease (COVID‐19) outbreak in Saudi Arabia. J Infect Public Health [Internet]. 2020;13:1432‐1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tiete J, Guatteri M, Lachaux A, et al. Mental health outcomes in healthcare workers in COVID‐19 and non‐COVID‐19 care units: a cross‐sectional survey in Belgium. Front Psychol. 2021;11:612241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:1623‐1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Malach‐Pines A. The burnout measure, short version. Int J Stress Manage. 2005;12:78‐88. [Google Scholar]
- 33. van de Pol JM, Koster ES, Hövels AM, Bouvy ML. How community pharmacists prioritize cognitive pharmaceutical services. Res Social Adm Pharm. 2019;15:1088‐1094. [DOI] [PubMed] [Google Scholar]
- 34. World Health Organisation W . Coronavirus disease (COVID‐19) advice for the public: Mythbusters. 2020. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/advice‐for‐public/myth‐busters. Accessed November 7, 2020.
- 35. Huijg JM, Gebhardt WA, Dusseldorp E, et al. Measuring determinants of implementation behavior: psychometric properties of a questionnaire based on the theoretical domains framework. Implement Sci. 2014;9:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Seward K, Wolfenden L, Wiggers J, et al. Measuring implementation behaviour of menu guidelines in the childcare setting: confirmatory factor analysis of a theoretical domains framework questionnaire (TDFQ). Int J Behav Nutr Phys Act. 2017;14:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. World Health Organisation W . Process of translation and adaptation of instruments. 2020. https://www.who.int/substance_abuse/research_tools/translation/en/. Accessed July 2, 2020.
- 38. Alqubaisi M, Tonna A, Strath A, Stewart D. Quantifying behavioural determinants relating to health professional reporting of medication errors: a cross‐sectional survey using the Theoretical Domains Framework. Eur J Clin Pharmacol. 2016;72:1401‐1411. [DOI] [PubMed] [Google Scholar]
- 39. Jamieson S. Likert scales: how to (ab)use them. Med Educ. 2004;38:1217‐1218. [DOI] [PubMed] [Google Scholar]
- 40. Arnold H, Wallace SJ, Ryan B, Finch E, Shrubsole K. Current practice and barriers and facilitators to outcome measurement in aphasia rehabilitation: a cross‐sectional study using the theoretical domains framework. Aphasiology. 2020;34:47‐69. [Google Scholar]
- 41. Grady A, Seward K, Finch M, et al. Barriers and enablers to implementation of dietary guidelines in early childhood education centers in Australia: application of the theoretical domains framework. J Nutr Educ Behav. 2018;50:229‐237.e1. [DOI] [PubMed] [Google Scholar]
- 42. Okuyan B, Balta E, Ozcan V, Durak Albayrak O, Turker M, Sancar M. Turkish community pharmacists' behavioral determinants in provision of pharmaceutical care to elderly patients. Int J Clin Pharm. 2021;43:1024‐1035. [DOI] [PubMed] [Google Scholar]
- 43. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID‐19 pandemic. Psychiatry Res. 2020;290:113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Civantos AA‐O, Byrnes Y, Chang C, et al. Mental health among otolaryngology resident and attending physicians during the COVID‐19 pandemic: national study. Head Neck. 2020;42:1597‐1609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dugani S, Afari H, Hirschhorn LR, et al. Prevalence and factors associated with burnout among frontline primary health care providers in low‐and middle‐income countries: a systematic review. Gates open Res. 2018;2:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands‐resources model of burnout. J Appl Psychol. 2001;86:499. [PubMed] [Google Scholar]
- 47. Gaither CA, Nadkarni A. Interpersonal interactions, job demands and work‐related outcomes in pharmacy. Int J Pharm Pract. 2012;20:80‐89. [DOI] [PubMed] [Google Scholar]
- 48. Calgan Z, Aslan D, Yegenoglu S. Community pharmacists’ burnout levels and related factors: an example from Turkey. Int J Clin Pharm. 2011;33:92‐100. [DOI] [PubMed] [Google Scholar]
- 49. ElGeed H, Owusu Y, Abdulrhim S, et al. Evidence of community pharmacists' response preparedness during COVID‐19 public health crisis: a cross‐sectional study. J Infect Dev Ctries. 2021;15:40‐50. [DOI] [PubMed] [Google Scholar]
- 50. Hoti K, Jakupi A, Hetemi D, et al. Provision of community pharmacy services during COVID‐19 pandemic: a cross sectional study of community pharmacists' experiences with preventative measures and sources of information. Int J Clin Pharm. 2020;42:1197‐1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Alkhalili M, Ma J, Grenier S. Defining Roles for pharmacy personnel in disaster response and emergency preparedness. Disaster Med Public Health Prep. 2017;11:496‐504. [DOI] [PubMed] [Google Scholar]
- 52. Al‐Quteimat OM, Amer AM. SARS‐CoV‐2 outbreak: how can pharmacists help? Res Social Adm Pharm. 2021;17:480‐482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bahlol M, Dewey RS. Pandemic preparedness of community pharmacies for COVID‐19: a cross‐sectional survey. Res Soc Adm Pharm. 2021;17:1888‐1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hasan SS, Kow CS, Zaidi STR. Social distancing and the use of PPE by community pharmacy personnel: Does evidence support these measures? Res Social Adm Pharm. 2021;17:456‐459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sum ZZ, Ow CJW. Community pharmacy response to infection control during COVID‐19. A cross‐sectional survey. Res Social Adm Pharm. 2021;17:1845‐1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Mohammed E, Khanal S, Jalal Z, Cheema E, Abutaleb MH, Paudyal V. Perceived barriers and facilitators to uptake of non‐traditional roles by pharmacists in Saudi Arabia and implications for COVID‐19 pandemic and beyond: a qualitative study using Theoretical Domain Framework. J Pharm Policy Pract. 2021;14:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14:26‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cane J, Richardson M, Johnston M, Ladha R, Michie S. From lists of behaviour change techniques (BCTs) to structured hierarchies: comparison of two methods of developing a hierarchy of BCT s. Br J Health Psychol. 2015;20:130‐150. [DOI] [PubMed] [Google Scholar]
- 59. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81‐95. [DOI] [PubMed] [Google Scholar]
- 60. Willis SC, Seston EM, Family H, White S, Cutts C. Extending the scope of community pharmacists’ practice to patients requiring urgent care–an evaluation of a training programme using the Theoretical Domains Framework. Health Soc Care Community. 2019;27:999‐1010. [DOI] [PubMed] [Google Scholar]
- 61. Stewart D, Klein S. The use of theory in research. Int J Clin Pharm. 2016;38:615‐619. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Author elects to not share data.


