Abstract
Background & Aims:
The Ideal Body Weight (IBW) model has provided dietitians and researchers with a quick method of risk assessment but is known to be imperfect. IBW formulas were developed from anthropometric measurements of life-insurance policy holders obtained between 1885 and 1908, providing statistics of mortality, organized by sex and age. Actuaries of the U.S. life insurance companies published data on the impact of overweight/obese status and mortality risk. Research of the same era repeatedly revealed either no significance or an inverse relationship. The intent of this text is to draw attention to the complexity and overall discussion of utility of the IBW method.
Methods:
Reviewed relevant literature from the development of IBW through the recent findings in 2014.
Results:
Height, weight, and frame fail to consider comorbidities and genetics. IBW formulas assume that weight increases as a linear function of height. Weight has been shown to increase not just as a function of height, but also of volume: body width, trunk length, and musculature. Depending on standards of practice, several equations may be used.
Conclusions:
The IBW model is utilized but not limited to creating enteral and parenteral feeding plans, avoiding malnutrition, aiding weight management, identifying transplant eligibility, and determining inclusion or exclusion from research studies. Socially, the significance around “ideal” can impact a weight-centric mentality and negatively affect a large portion of the population. Every individual has a distinct “ideal” body weight based on genetics, environment and lifestyle, which could be represented and assessed effectively with new tools.
Keywords: Ideal body weight, BMI, predictive formulas, Met Life tables, nutrition assessment
I. Introduction
Ideal body weight (IBW) is defined as weight for height at the lowest risk of mortality. This definition results from a century’s research on the association between anatomical characteristics and health. Employing weight, height, and frame size, IBW is calculated via height-weight tables1,2,3,4,5,6. IBW can also be calculated using one of many predictive formulas4. The cost-effective and efficient nature of the IBW model has provided healthcare practitioners and researchers a practical method of risk assessment. The model is based on Metropolitan Life Insurance Company (MLIC) data and has persisted with scrutiny7. Opponents criticize the manner of data collection, validity of subsequent IBW formulas, and the strength of the alleged association between obesity and health4,5. To define the modern placement of the IBW model in healthcare and research, it is necessary to critically analyze former findings. The preceding article functions as an examination and commentary on the development and clinical utility of the IBW model. It is not the intent of this text to deprive healthcare practitioners and researchers of numerical domains for risk assessment, but instead to draw attention to the complexity and overall discussion of utility of the IBW method
II. Development of the Ideal Body Weight Model
Uncovering the association between obesity and health advanced during the twentieth century through a partnership between the Actuarial Society of America and the Association of Life Insurance Medical Directors of America4,8,9. The collaboration led to the publication of The Medico-Actuarial Mortality Investigation, providing statistics of mortality for weight and height of insured persons. Anthropometric measurements of life-insurance policy holders were obtained between 1885 and 1908. While these provided reference values for average weight, the inability of the average weight to exhibit the lowest risk of mortality ultimately failed to create standard values for “ideal” weight5. This publication defined standard values of weight, and thus the origin of “ideal” weight.
To assess and publish standard values of weight, the MLIC partnered with statistician L.I. Dublin8. Anthropometric measurements were taken from four million MLIC policy holders and longevity was established as the primary criteria for “ideal” weight8. The data failed to obey normal distribution which Dublin attributed to the idea of variability in skeletal frame size or breadth8. Frame size by elbow breadth was found to be the most accurate and consistent across 3,8,10 and was subsequently linked to total body fat and fat free mass11. To account for frame size, recorded heights were classified as having either a small, medium, or large frame3,12. Additionally, Dublin removed the age component of the standard values, arguing that weight should not vary after growth has ceased9. Dublin’s initiatives catalyzed publication of The National Standards for Weight by Sex and Body Frame MLIC 1942-438. Finally, standard values indicated for the assessment of excess weight in relation to health were available to practitioners and researchers.
In the middle of the twentieth century, the Society of Actuaries along with 26 insurance companies examined the impact of obesity and blood pressure on health via The Build and Blood Pressure Study8. Weights were recorded from policy holders between 1935 and 1953; subjects were then followed until 1954 and risk of mortality was determined. Subsequently, the Revised MLIC 1959 Standard Tables based on association with mortality incorporated the updated data.
It is necessary to observe the development of BMI when commenting on the IBW method as the two inevitably converge. BMI, the ratio between weight and height, was first proposed by Belgian mathematician Adolphe Quetelet. In the 1835 publication, A Treatise on Man and the Development of His Aptitudes, Quetelet concluded an individual’s weight increased as a function of their height squared4. This formula is expressed by dividing weight in kilograms by height in meters squared and offers a ratio, known as the Quetelet Index8.
This formula remained unvalidated for decades. In the late twentieth century, validity was considered using data from the fourth iteration of the Framingham Heart Study4. Resulting research led to the adoption and rebranding of the Quetelet Index as BMI. Convergence of these indices occurred through The Fogarty Center Conference on Obesity (FCCO) in 19738. The FCCO recommended acceptable ranges of weight for height. Employing Dublin’s frame sizes, the FCCO set acceptable weight from the lowest perimeter of the small frame to the highest perimeter of the large frame; weight for height was then converted into BMIs, culminating in acceptable BMI ranges. The FCCO’s acceptable ranges were later adopted by the USDA in the first edition of the Dietary Guidelines for Americans and by the National Health and Nutrition Survey 1976-80 (NHANES II).
IBW and BMI both address a relationship between health and mortality. Both are useful in large scale population studies due to the simplicity, low intensity and burden on the patients, and the information is readily available for anyone to use5,6. However, BMI is difficult to calculate without a calculator available. Both tools can be useful for generic target weight or weight loss goals but lack specificity in clinical care. They both fail to address body composition and overall nutritional status and cannot account for the metabolically healthy obese or the obesity paradox, where above-normal BMI can be protective in certain disease states5,6. During the second iteration of The Build and Blood Pressure Study in 1979, “desirable” weights were observed to have modestly increased8. Consequently, the Revised MLIC 1983 tables published slightly increased weights. Additionally, “ideal” and “desirable” were redacted from the tables due to misinterpretation of the terminology8,9.
For a timeline of the development of the IBW model see Figure 1.
Figure 1:
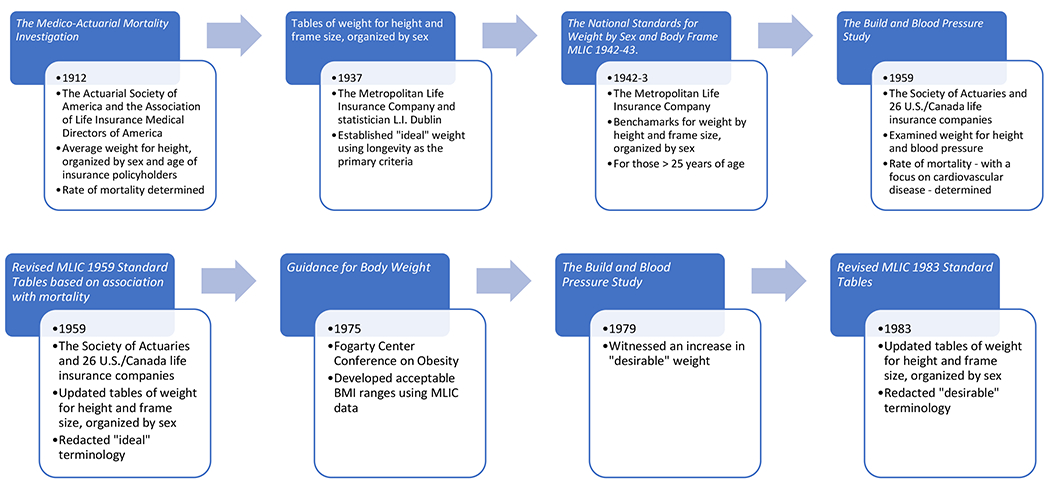
Timeline of the development of the IBW model
- Dark blue box represents the title of the publication (book, article, table)
- Blue outlined white box represents the year of publication, attribution and brief summary of publication results
- Top row, read from left to right, light blue arrows pointing in the direction of the progression. Bottom row, read from left to right, light blue arrows pointing in the direction of the progression.
- Each publication in the timeline a catalyst for the next project/development in the ideal body weight timeline
References:
Medico-Actuarial Mortality Investigation. Vol. 1. New York, NY, USA: Association of Life Insurance Medical Directors; The Actuarial Society of America; 1912.
Dublin L. I, Lotha A. J. Twenty-Five Years of Health Progress: A Study of the Mortality Experience among the Industrial Policyholders of the Metropolitan Life Insurance Company, 1911 to 1935. New York, NY, USA: Metropolitan Life Insurance; 1937
Ideal weight for women. Statistical bulletin of the Metropolitan Life Insurance Company, 1943.
Metropolitan Life Insurance Company. Ideal weights for men. Statistical Bulletin of the Metropolitan Life Insurance Company. 1942;23:6–8.
Metropolitan Life Insurance Company. New weight standards for men and women. Statistical Bulletin-Metropolitan Life Insurance Company. 1959;40:1–4
Build and Blood Pressure Study. Vol. 1. Chicago, Ill, USA: Society of Actuaries; 1959
Build Study 1979. Chicago, Ill, USA: Society of Actuaries and Associations of Life Insurance Medical Directors; 1980
Metropolitan Life Insurance Company. Metropolitan height and weight tables. Statistical Bulletin (Metropolitan Life Insurance Company) 1983;64:1–19
Bray G., editor. Obesity in perspective. (DHEW Publication no (NIH) 75-708).Fogarty International Center. Series on Preventive Medicine. 1975;2(part 1) https://searchworks.stanford.edu/view/2520869
III. Clinical Utility of the Ideal Body Weight Model
Depending on the setting or healthcare center standards of practice, several different equations may be used. Access to Indirect Calorimetry to determine Resting Energy Expenditure is limited in acute care settings, and the use of standard predictive equations without stress factors may not be appropriate. Despite inconsistency, the potential options available may not be enough. As outlined in the history of predictive equations, it is known that not all demographics and comorbidities are considered for the most common and supported predictive equations. In the clinical setting, it is important to assess what additional benchmarks can be interwoven into predictive equations and tables that determine IBW. Demographic information, including sex/gender, age, and race/ethnicity are all important factors. The disease state of patients could also factor into the formulas used in identifying ideal needs.
Accompanying clinical judgement, the IBW model is utilized but not limited to creating enteral and parenteral feeding plans in obese populations, avoiding malnutrition in pediatric populations, aiding in development of goals for weight management, identifying transplant eligibility in cases of increased adiposity in the abdominal region, and determining inclusion or exclusion from research studies. Bariatric surgery prerequisites are also based on these equations, as are certain dosing requirements during parenteral nutrition in any population. IBW may be used in driving mechanical ventilation settings, thereby increasing the importance of a specified personal assessment of what an IBW should be. Additionally, exclusion criteria for research studies often include narrow weight parameters, and while exceptions can be made with the necessary approvals, there is theoretically no room for clinical judgement when working within these criteria and statistical analysis. These equations are used throughout the patient care process and assessment of needs constantly requires updating based on patient response. While this begs for simplicity in equations for fast application, the level of nuance per patient demands a more complex approach. The more complex a needs assessment becomes, the more likely the diagnostic process could be delayed.
IV. Criticism of the Ideal Body Weight Model
During the twentieth century, actuaries of the U.S. life insurance companies collected, analyzed, and published data on the impact of overweight/obese status and mortality risk 6,8. Prior to this analysis, underweight policyholders were charged higher premiums due to the correlation between low weight and tuberculosis7. The overt bias and monetary incentives of U.S. life insurance actuaries was in part enabled by the subjective, inconsistent methods used in collecting measurements. Approximately 20% and 10% of weight and height data were self-reported for the Revised MLIC 1959 Standard Tables based on association with mortality, and Revised MLIC 1983 tables, respectively.
Furthermore, all MLIC tables failed to obtain anthropometric measurements without garments and utilized inconsistent factors to account for these variables7. Aside from weight and height data, frame size has also been under scrutiny. Without any evidence to guide the theory, frame size was defined, measured, and reported arbitrarily by the MLIC and Dublin.
Evidence of self-selection also exists within the samples from which data were collected7. Approximately two to three percent of policy holders were of overweight/obese status (defined as 20% to 30% above their “ideal” weight for height) and were made to pay higher premiums. However, the actual national occurrence of overweight/obese status at the time was between six and seven percent. This implies that policyholders paying higher premiums acquiesced due to additional health risks that were not disclosed to insurers, a behavior known as “selecting against the insurer.”
While the U.S. life insurance companies dominated much of the discussion, there has been no lack of research on obesity and health7. Research of the same era repeatedly revealed either no significance or an inverse relationship between obesity and mortality, most of which was ignored by the U.S. life insurance companies.
V. Ideal Body Weight Predictive Formulas
Memorization of the IBW tables is cumbersome, and healthcare practitioners realistically prefer simple formulas that can be quickly employed5. Numerous IBW formulas have been developed to suit this purpose: Devine, Robinson et al, Miller et al, Broca, Hamwi, and Hammond4,7. While many of the formulas were derived from the MLIC Standard tables, some evolved from unknown origins.
Refinement of the IBW predictive formulas grew from the need to determine best practices for pharmacological dosing of patients. In the Revised MLIC 1959 Standard Tables, Robinson et al replaced the Devine IBW predictive formula4 as the latter relied on anecdotal observation, the former deployed regression analysis of median weight for height at three frame sizes, offering a more validated approach.
When the MLIC tables were later updated, Miller et al – through the same methods as Robinson et al – developed an updated IBW predictive formula4. To account for anthropometric measurements including apparel, Miller et al subtracted five and three pounds for men and women, respectively. Additional predictive formulas include Broca, Hamwi, and Hammond; however, no method of development for these predictive formulas have been reported. Analysis has revealed significant similarities; likely due to the use of weight for height tables as source data4,9. Consequently, researchers have concluded them to be comparable4,9.
Statistical comparison of predictive formulas has revealed variation between “ideal” weights at different heights4. IBW predictive formulas have failed to produce consistent BMIs across heights.
For a table of IBW predictive formulas see Table 1.
Table 1:
IBW predictive formulas
| Author(s) | Year | Predictive Formula |
|---|---|---|
| Devine | 1974 | IBW (men) = 50 kg + (2.3 kg per inch over 5’) |
| IBW (women) = 45.5 kg + (2.3 kg per inch over 5’) | ||
| Robinson et al | 1983 | IBW (men) = 52 kg + (1.9 kg per inch over 5’) |
| IBW (women) = 49 kg + (1.7 kg per inch over 5’) | ||
| Miller et al | 1983 | IBW (men) = 55.7 kg + (1.39 kg per inch over 5’) |
| IBW (women) = 53 kg + (1.33 kg per inch over 5’) | ||
| Broca | 1871 | IBW (kg) = height (cm) − 100 |
| Hamwi | 1964 | IBW (men) = 106 lb + (6 lb per inch over 5’) |
| IBW (women) = 100 lb + (5 lb per inch over 5’) | ||
| Hammond | 2000 | IBW (men) = 48 kg + (1.1 kg per cm over 150) |
| IBW (women) = 45 kg + (0.9 kg per cm over 150) |
VI. Criticism of the Predictive Formulas: Ideal Body Weight and Body Mass Index
Despite flaws within the methods employed for the IBW tables, they have been central to development of the IBW predictive formulas and acceptable BMI. Consequently, regardless of whether the formulas are reliable, the standard used to determine validity (i.e., IBW tables) may itself lack the ability to measure what it intends to4,7,8,9. While frame size has been shown to possess a stronger correlation than stature to weight, researchers have found a significant variation in frame sizes between Caucasians and African Americans13. Additionally, the WHO found that some Asian populations with a BMI between 22-25 kg/m2 still had higher risk for comorbidities like DM2 and CVD14 despite frame. Such findings may warrant further investigation and stratification of frame size, IBW, and BMI by race.
Some have argued against the robustness of the predictive formulas4,5. IBW formulas assume that weight increases as a linear function of height. However, weight has been shown to increase not just as a function of height, but also of volume: body width, trunk length, and musculature. BMI attempts to account for this issue through squaring of the height. However, some have claimed this does not entirely repair the concern of weight as a function of height since there are still flaws with the upper and lower extremes of stature.
Overall, researchers have argued that IBW and BMI are too general, and the predictive formulas’ intention is to measure lean body mass4,5. Additionally, height, weight, and frame fail to consider comorbidities and genetics4,5,14.More refined technologies exist to do so: bio-electrical impedance (BIA), dual-energy x-ray absorptiometry (DXA), and Air Displacement Plethysmograph (ADP) which can be costly and time-consuming. In addition to IBW and BMI, there are several other body weight metrics available: Lean body weight (LBW), predicted normal weight (PNW), adjusted body weight (ABW), and fat free mass to name a few (FFM)15. LBW and PNW are predictive equations that both utilize sex and BMI in the calculations. These equations aim to represent the expected fat free weight and normal weight of an obese person. Both equations employ BMI and are subject to similar limitations. ABW was intended for better medication dosing in obese populations, but similarly utilize IBW and is subject to similar limitations. The FFM equation has potential. The data was produced from total body water, bone density, and body potassium measurements to determine if BMI could estimate FFM but was developed from an animal model and validated in one small study. IBW and LBW are important options when calculating medication, nutrition, or ventilation prescriptions in obese or critical care populations. Obesity and critical care status can impact certain medications’ ability to metabolize properly in the body. Using actual weight may be more beneficial in obese populations when hydrophobic drugs are given in intervals, but LBW would be preferred for long infusions. The higher fat mass may cause medication to accumulate in slow dosing setups. Low weight patients (under 18.5 BMI) are also complicated based on critical care status. Depending on the reason for their low weight, some clinicians will use pediatric calculations using actual weight, however medication metabolism still varies in adults.
VII. Conclusion
The discussion regarding the dichotomy of exactness and flexibility is highlighted in this commentary. The IBW model has provided healthcare practitioners and researchers a quick and mostly effective method of risk assessment but is known to be imperfect. Practitioners have found ways to manipulate the predictive equations to help them provide recommendations in acute care situations. Feed patients to meet their needs at goal weight but understand it is approximate. Assess and treat quickly, but also be thoughtful and consider all angles. Consider all disease states, track your thought process and math, and use clinical judgement.
Ambulatory and research use the same predictive numbers, but not always in the same way. Clinical judgement also applies to the outpatient setting, but when working with numbers and diagnostic definitions, there is typically less flexibility. In research settings, all patients in a study should be compared to the same standards for statistical significance, but those standards may not be appropriate for a diverse demographic. A researcher might be able to correct for the variations in equations if the equations were appropriately manipulated, otherwise they could be stranded with unintended cohorts. Research volunteers are included or excluded from participation based on hard cutoff points in tables that fail to reflect important demographic characteristics. Depending on the patient care scenario, it is necessary to use clinical judgement with regards to IBW estimates. It is an ever-evolving attempt to better the care delivered.
On the social level, the significance around “ideal” can impact a weight-centric mentality and unintentionally negatively affect a large portion of the population. Every person has a different “ideal” body weight based on their genetics, environment, and lifestyle, and not every person can fit into a neat mathematical table. Most of the tables don’t address demographics other than simple black or white races, and there are several important people who are not represented; mixed race, nonbinary, transgender, intersex, little people, disabled, or any number of co-morbidities.
Additionally, is race an appropriate demographic to use for differentiation at all? Race is a social construct and not biologically significant according to the Human Genome project, suggesting race may not be a necessary factor in determining IBW and overall health status. However, equal representation is important. Should the IBW tables/equations be updated? Should they be differentiated by more representative demographics? How many tables is too many? Should there be a shift in terminology from “ideal body weight” to “realistic body weight” or “functional body weight”? Can a universal calculator/app be developed to plug in basic demographics and health considerations to decrease the reliance on physical tables and improve speed of assessments? How can we use technology to our advantage with clinical assessments?
Further exploration into these questions is needed to learn about how we can move forward in research and clinical care.
ACKNOWLEDGEMENTS
We thank the 2018-2019 dietetic interns at Massachusetts General Hospital for their participation and contributions to this study. We have received permission from the groups mentioned above.
FUNDING/FINANCIAL DISCLOSURES
This work was supported in part by Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences) National Institutes of Health Award 1UL1TR002541-01 and financial contributions from Harvard University and its affiliated academic health care centers.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Credit Statement
Tara M. Holmes: Conceptualization, Methodology, Resources, Writing – Original Draft, Writing – Review & Editing, Supervision, Project administration
Sierra Chichester: Resources, Writing – Original Draft, Writing – Review & Editing,
Jane Hubbard: Conceptualization, Methodology, Resources, Writing – Review & Editing, Supervision, Project administration
CONFLICT OF INTEREST DISCLOSURES
All authors report no conflicts of interest.
Contributor Information
Sierra Chichester, MGH Dietetic Intern (previous), Department of Nutrition and Food Services, 55 Fruit Street, Boston, MA 02114; Clinical Dietitian (current), Aramark Healthcare, 170 Morton Street, Jamaica Plain, MA 02130.
Tara M. Holmes, Senior Research Dietitian, Translational & Clinical Research Centers, Massachusetts General Hospital, 55 Fruit Street, Boston, MA 02114.
Jane Hubbard, Director of Metabolism and Nutrition Research, Translational & Clinical Research Centers, Massachusetts General Hospital, 55 Fruit Street, Boston, MA 02114.
References
- 1).Metropolitan Life Insurance Company. New weight standards for men and women. Stat Bull Metrop Insur Co. 1959;40:1–4. [Google Scholar]
- 2).Metropolitan Life Insurance Company. New weight standards for men and women. Stat Bull Metrop Insur Co. 1983;64:1–9. [Google Scholar]
- 3).Mitchell MC Comparison of determinants of frame size in older adults. Journal of the American Dietetic Association. 1993; 93:53–57. [DOI] [PubMed] [Google Scholar]
- 4).Shah B, Sucher K, Hollenbeck CB. Comparison of ideal body weight equations and published height-weight tables with body mass index tables for healthy adults in the United States. Nutr Clin Pract. 2006;21:312–319. [DOI] [PubMed] [Google Scholar]
- 5).Muller MJ. Ideal body weight or BMI: So, what’s it to be? Am J Clin Nutr. 2016;103:1193–1194. [DOI] [PubMed] [Google Scholar]
- 6).Peterson CM, Thomas DM, Blackburn GL, Heymsfield SB. Universal equation for estimating ideal body weight and body weight at any BMI. Am J Clin Nutr. 2016;103:1197–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Keys A Is there an ideal body weight? BMJ. 1986;293:1023–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Komaroff M For researchers on obesity: Historical review of extra body weight definitions. J Obes. 2016;1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Pai MP, Paloucek FP. The orgin of the “ideal” body weight equations. Ann Pharmacother. 2000;34:1066–1069 [DOI] [PubMed] [Google Scholar]
- 10).Lohman TG, Roche AF, Martorelli R (eds) Anthropometric Standardization Reference manual. Champaign, IL: Human Kinetics Books, 1988. [Google Scholar]
- 11).Chumlea WC, Wisemandle W, Guo SS, Siervogel RM. Relations between frame size and body composition and bone mineral status. Am J Clin Nutr. 2002; 75:1012–1016. [DOI] [PubMed] [Google Scholar]
- 12).Eknoyan G Adolphe Quetelet (1976-1874) – the average man and indices of obesity. Nephrol Dial Transplant. 2008;23:47–51. [DOI] [PubMed] [Google Scholar]
- 13).Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM. Why are there race/ethnic differences in adult body mass index‱adiposity relationships? A quantitative critical review. Obes Rev. 2016; 17(3): 262–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).The WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363: 157–163. [DOI] [PubMed] [Google Scholar]
- 15).MacDonald JJ, Moore J, Davey V, Pickering S, Dunne T The weight debate, .Jics. 2015; 16(3): 234–238. [DOI] [PMC free article] [PubMed] [Google Scholar]


