Abstract
Introduction
As a local response to the COVID‐19 global pandemic, the University of Alabama at Birmingham (UAB) established the UAB COVID‐19 Collaborative Outcomes Research Enterprise (CORE), an institutional learning health system (LHS) to achieve an integrated health services outcomes and research response.
Methods
We developed a network of expertise and capabilities to rapidly develop and deploy an institutional‐level interdisciplinary LHS. Based upon a scoping review of the literature and the Knowledge to Action Framework, we adopted a LHS framework identifying contributors and components necessary to developing a system within and between the university academic and medical centers. We used social network analysis to examine the emergence of informal work patterns and diversified network capabilities based on the LHS framework.
Results
This experience report details three principal characteristics of the UAB COVID‐19 CORE LHS development: (a) identifying network contributors and components; (b) building the institutional network; and (c) diversifying network capabilities. Contributors and committees were identified from seven components of LHS: (a) collaborative and executive leadership committee, (b) research coordinating committee, (c) oversight and ethics committee, (d) thematic scientific working groups, (e) programmatic working groups, (f) informatics capabilities, and (g) patient advisory groups. Evolving from the topical interests of the initial CORE participants, scientific working groups emerged to support the learning system network. Programmatic working groups were charged with developing a comprehensive and mutually accessible COVID‐19 database.
Discussion
Our LHS framework allowed for effective integration of multiple academic and medical centers into a cohesive institutional‐level learning system. Network analysis indicated diversity of institutional disciplines, professional rank, and topical focus pertaining to COVID‐19, with each center leveraging existing institutional responsibilities to minimize gaps in network capabilities.
Conclusion
Incorporating an adapted LHS framework designed for academic medical centers served as a foundational resource supporting further institutional‐level efforts to develop agile and responsive learning networks.
Keywords: framework, interdisciplinary collaboration, learning healthcare system, network development, network diversity
1. INTRODUCTION
With global cases of coronavirus disease 2019 (COVID‐19) skyrocketing in the first quarter of 2020, a proclamation of national emergency was issued 13 March 2020 in the United States 1 , 2 , 3 , 4 ; the same date of the first reported COVID‐19 case in the state of Alabama. 5 Rapidly changing clinical recommendations and rapidly emerging data regarding therapeutic options highlighted the need for institutional‐level agility in responding to the pandemic. 6 Thus, University of Alabama at Birmingham (UAB) faculty, trainees, and staff established the UAB COVID‐19 Collaborative Outcomes Research Enterprise (CORE) to develop an institutional learning health system (LHS) as a coordinated response to the COVID‐19 pandemic, at a local level.
CORE membership initially included members from within the UAB Health System, School of Medicine, School of Public Health, School of Health Professions, School of Nursing, and the Birmingham community, with continual outreach efforts to recruit additional members focused on interdisciplinary solutions to COVID‐19. With growing popularity, leadership within CORE recognized the need for more formal organization and evidence‐based collaboratives capable of sustainably implementing the LHS across the institution. Thus, CORE established four guiding principal tenets including: (a) facilitating data access and providing research support to investigators, (b) avoiding duplication of efforts and undue burden on patients and participants, (c) fostering interdisciplinary collaborations, and (d) supporting rigorous and transparent research to rapidly produce COVID‐19 solutions. In addition, a LHS framework tailored to the unique characteristics of academic institutions and medical centers was adopted to guide CORE efforts, ensure inclusivity and integration, and minimize gaps throughout the system. This experience report details three characteristics of institutional‐level learning system development, derived from the experience of the UAB COVID‐19 CORE including: (a) identifying network contributors and components, (b) building the institutional network, and (c) diversifying network capabilities.
2. IDENTIFYING NETWORK CONTRIBUTORS AND COMPONENTS
Prior to the emergence of the COVID‐19 global pandemic, a UAB research team was actively developing a LHS framework characterizing components and features necessary to support system development within and between the university academic and medical centers. A scoping review of the literature was conducted to identify critical features, components, and contributors to LHS development specifically within academic medical settings. The purpose of the LHS framework was multifaceted including: simultaneously improving clinical care and contributing to scientific understanding, responding to emerging therapeutic recommendations, and developing institutional collaboratives with diverse capabilities within healthcare environments. 7 Using the results of the scoping review, the team adopted the LHS framework to identify core network contributors and components within the context of the COVID‐19 pandemic. Results of the scoping review and LHS framework are reported elsewhere. 8
The LHS framework includes seven organizational components driven by two dynamic and actionable engines, learning and research, derived from the Knowledge to Action Framework (KTA). 8 , 9 Each component identifies specific areas for expert contributions and each engine identifies the process of collecting, organizing, and disseminating evidence within the system. Applying the action cycles of the KTA within the institution's healthcare organization, the university medical system functions as the learning engine; incorporating analyses of patient and provider data derived from clinical practice to identify areas of disparity, low performance, or possible expansion. The university research infrastructure serves as the research engine, based upon institutional research capabilities and applied to specific clinical conditions or topics of interest. 9 , 10 Positioned upon these dynamic engines are seven structural components: (a) organization and collaborations, (b) performance, (c) ethics and security, (d) scientific, (e) data, (f) information technology, and (g) patient outcomes. Each component of the LHS framework serves a unique and essential purpose, collectively providing an organized and integrated system to achieve functionality as a LHS. 9 , 11 , 12 , 13 , 14 This overarching LHS framework provided the scaffolding upon which the rapidly emergent COVID‐19 CORE was organized (Figure 1).
FIGURE 1.

An adapted learning health system (LHS) framework for the UAB COVID‐19 Collaborative Outcomes Research Enterprise (CORE). 8 A LHS framework depicting seven interconnected structural components (depicted as rectangles). Learning and research engines (depicted as circles) include arrows indicating the flow of information and communication, as informed by the Knowledge to Action Framework (KTA)
3. BUILDING THE NETWORK
While interest in learning system development permeates many academic institutions, actualizing these systems oftentimes requires the cultivation of professional relationships and extensive networks over long timeframes. 8 Driven by national urgency from the COVID‐19 pandemic, the evolution of the UAB COVID‐19 CORE progressed rapidly, spanning approximately 6 weeks from initial development until the number of network contributors doubled (Figure 2). This growth was driven by targeted recruitment of key stakeholders as well as an open invitation for anyone interested to join this initiative. Contributors to the UAB COVID‐19 CORE are organized and recruited according to the engines and components of the LHS framework, ensuring that each component is well represented and providing diverse perspectives for larger contributions within the system.
FIGURE 2.
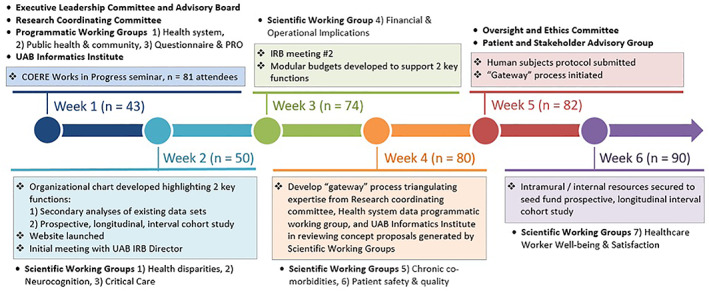
UAB COVID‐19 Collaborative Outcomes Research Enterprise (CORE) weekly milestones and progression. The early evolution of the UAB COVID‐19 CORE. Text boxes denote key milestones and achievements, with the weekly number of participants indicated parenthetically. The timeline denotes the evolution of the seven LHS structural components; increases in faculty, trainee, and staff participation following the inaugural meeting of healthcare providers and investigators spanning the health system and academic schools. COERE, Center for Outcomes and Effectiveness Research and Education; IRB, institutional review board; LHS, learning health system; PRO, patient reported outcomes
3.1. The learning engine: UAB Medicine
As the cornerstone of the UAB Health System, UAB Medicine provides comprehensive primary and subspecialty care services with over 90 000 hospital discharges and 1.6 million outpatient visits annually. 15 Established in 1945, UAB Hospital is a level 1 trauma center with over 1100 beds located in Birmingham, Alabama. From the outset of the pandemic, COVID‐19 CORE participation included front‐line providers and clinical leaders representing contributors within the learning engine. Thus, providers directly engaged in the provision of COVID‐19 testing and treatment serve as drivers of the UAB Medicine Learning Engine by contributing essential insights into variations of clinical practice associated with COVID‐19, highlighting high‐priority research questions, and suggesting options of data collection from within the clinical environment. 16
3.2. The research engine: Center for Outcomes and Effectiveness Research and Education and Center for Clinical and Translational Sciences
The UAB Center for Outcomes and Effectiveness Research and Education (COERE) and Center for Clinical and Translational Sciences (CCTS) afforded extant infrastructure and interdisciplinary expertise to support the UAB Research Engine. These research centers developed collaborative relationships between investigators within the university and health system representing medical informatics, regulation and compliance, biostatistics, epidemiology, and research design resources. The research engine allowed for dissemination and widespread communication of emerging evidence throughout the university.
3.3. Seven organizational components
3.3.1. Organization and collaborations component: Executive leadership committee
The COVID‐19 CORE Executive Leadership Committee is responsible for governance, management, and strategic decision‐making within the collaborative. Deputy directors from UAB Medicine, COERE, and CCTS comprise the executive committee and are responsible for day‐to‐day operations in steering the evolving enterprise, identifying budgetary needs, and communicating with an institutional but independent advisory committee. The advisory committee includes senior leadership from the UAB Health System, UAB President's office, centers, institutes, and academic schools providing critical feedback. The Executive Leadership Committee functions autonomously but with open lines of bidirectional communication with the advisory committee. While the reporting structures for COVID‐19 CORE to the advisory committee did not immediately provide scientific guidance on health system policies during the pandemic, planning and reorganization continues to better align the advisory committee capacities to inform health system policies from knowledge generated within the LHS.
The Executive Leadership Committee determines the primary functions of the COVID‐19 CORE initiative: (a) conducting secondary analyses of existing data related to testing, treatment, community, and population health outcomes and (b) developing a longitudinal, observational COVID‐19 cohort study to evaluate the long‐term sequelae and outcomes of COVID‐19 infections. The committee is also charged with identifying and securing intramural and extramural sources of funding; such that, the Executive Leadership Committee develops and maintains the LHS plan to leverage existing human and technological resources within the institution, increases institutional capacity for dedicated LHS human resources, and identifies areas of critical need for additional human or technological resources. While the initial LHS was largely volunteer‐driven, this committee also leveraged in kind support from the CCTS, COERE, and Informatics Institute to maximize efficiency with existing institutional resources.
A distributed leadership model was established with the Executive Leadership Committee providing overarching strategic vision, and empowering the Research Coordinating Committee, Scientific and Programmatic Working Groups, and other domains to make tactical decisions within their component's role as situated in the larger framework. For example, each Scientific Working Group leadership team was asked to identify two priority projects for their group, but given the flexibility to work with their membership to decide on these projects.
3.3.2. Performance component: Research coordinating committee
A Research Coordinating Committee was established to set short‐term objectives, define success, and establish processes to guide the activities of the Scientific and Data Components within the COVID‐19 CORE LHS framework. The committee defined three critical phases of activity: (a) foundational phase, (b) implementation phase, and (c) scientific phase. The foundational phase, focused upon building the team and COVID‐19 database, led to the formation of three programmatic working groups (PWG) charged with determining data elements for inclusion in a comprehensive, mutually shared COVID‐19 database. Initially incorporating UAB electronic health records and health system data, the implementation phase represents an ongoing process of building the shared database, with efforts to incorporate public health, community, novel patient‐level questionnaires, and patient‐reported outcome (PRO) data over time. Scientific working groups (SWG) emerged within the scientific phase to complement and support the PWG, driven by internal conflicts emanating from efforts to build a foundational database and platform but absent critical guidance from scientific and research questions. Thus, the SWG are designed to support topical interest areas of the network contributors and align study concepts with data collection and analysis.
3.3.3. Ethics and security component: Oversight and ethics committee
Engagement with leadership from the UAB Institutional Review Board served as a precursor to the establishment of a COVID‐19 CORE Oversight and Ethics Committee. The LHS framework describes an inherent tension between the Performance Component and the Ethics and Security Component 8 ; this tension is essential to safeguard human subjects and the UAB Medicine enterprise, ensuring COVID‐19 CORE research and clinical activities are conducted in alignment with ethical principles. The COVID‐19 pandemic highlighted the inherent pressures in academia to be first; with “under review” manuscripts regularly reported in the mainstream media as preprints prior to rigorous peer review and publication. 17 By emphasizing clinical and scientific rigor, ethics, reproducibility, and transparency the Oversight and Ethics Committee balanced the time pressure and aspirations within the Research Coordinating Committee. In addition, the Oversight and Ethics Committee also served to ensure diversified engagement of research participants, ethical research methods, and a variety of new studies to reduce health disparities based on prior research. 18 , 19 , 20 The ethics committee monitored participation of participants and clinical stakeholders to ensure inclusivity and representation relative to the large population of patients admitted with COVID‐19.
3.3.4. Scientific component: Scientific working groups
According to our LHS framework, the Scientific Component was charged with identifying relevant and priority research questions derived from the learning engine that were both context reflective and content specific. Thematic SWG, co‐led by two to three individuals, were established to serve this function and were open to participation from any interested student, faculty, or staff from the health system or academic schools of UAB. Initially, three working groups were formed, including health disparities, neurocognition, and critical care.
As other thematic areas of interest emerge, new working groups can be recommended via the COVID‐19 CORE website. The Executive Leadership Committee established approval guidelines for new SWG based upon alignment with the principal goals of the COVID‐19 CORE, overlap with existing working groups, and feasibility of accessing requisite data to meet their objectives. For example, based upon these principles, a proposal to establish a financial and operational implications SWG was approved, whereas the behavioral medicine interventions working group was not approved because prospectively enrolling participants for interventions was beyond the stated scope of the COVID‐19 CORE. Subsequent to the initial SWG, working groups focusing on chronic comorbidities, patient safety and quality, and healthcare worker wellness and satisfaction have been approved (Figure 2).
3.3.5. Data component: Programmatic working groups
Identifying available data elements, desired data elements, and sources of data access pertaining to COVID‐19 testing and treatment was a recognized challenge early in the LHS development. At the local level, these challenges included varying data structures from different sources, reporting lags, staffing, and resource constraints to address gaps in technical infrastructure and collection of new data elements. Within the public health level, inconsistent archiving procedures limited the potential sources of data. A key learning within this component was the need for focused attention and resources for data transformation and access.
Three unique areas were selected, with the formation of PWG, to identify data elements including: health system data, public health and community data, questionnaire and PRO data. The health system data group compiled currently available data, classified as discrete elements in the electronic health record (EHR), amenable to data query vs unstructured elements requiring manual abstraction; the latter of which were abstracted following a coordinated gateway process (Figure 3). Data derived from this process were used in local level decision‐making, informing the implementation of inpatient telehealth approaches to facilitate remote clinician rounds within the UAB hospital system and support conservation efforts for personal protective equipment during national shortages throughout the pandemic. 21
FIGURE 3.
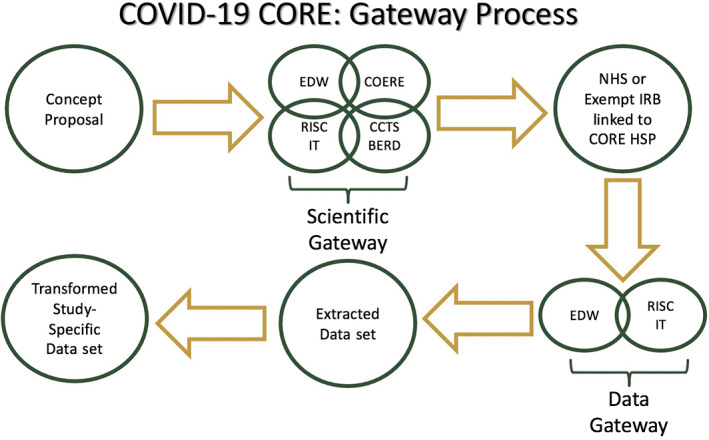
UAB COVID‐19 Collaborative Outcomes Research Enterprise (CORE): Gateway process. The workflow to generate data sets providing transformed study specific data sets from extracted health system data. Beginning with submissions of study concept proposals, this process is followed by a scientific gateway meeting with lead study investigators including representatives from the EDW of the Informatics Institute, along with clinical informatics, biostatistics, epidemiology, and research design (BERD), and outcomes research experts from the Research Coordinating Committee (RCC) of COVID‐19 CORE. CCTS BERD, Center for Clinical and Translational Science Biostatistics, Epidemiology, and Research Design; COERE, Center for Outcomes and Effectiveness Research and Education; EDW, Enterprise Data Warehouse; HSP, human subjects protocol; IRB, institutional review board; NHS, not human subjects; RISC IT, Research and Informatics Service Center—Information Technology
The public health and community group determined local and state health department individual‐level surveillance data related to COVID‐19. These data were not immediately available for research purposes and were identified through community testing venues that might augment data captured via UAB Medicine. The questionnaire and selected PRO, informed by National Institutes of Health (NIH) guidance, represented validated instruments for data capture and synthesis during index encounters for COVID‐19 related medical services and/or via longitudinal follow‐up in a convalescent phase. 22
3.3.6. Information technology component: UAB Informatics Institute
The UAB Informatics Institute's Enterprise Data Warehouse (EDW), i2B2 framework, and data query tool contributed an existing infrastructure for the extraction and management of UAB Medicine health system data within the LHS framework. 23 The need emerged for qualified personnel to group raw diagnostic, procedural, and other codes housed in i2B2 into composite clinical variables needed for statistical analysis. A team within the Research and Informatics Service Center—Information Technology (RISC), with substantial data transformation experience for HIV health system research, filled this role for the COVID‐19 CORE, establishing a novel process to engage investigators interested in conducting secondary analyses utilizing health system data (Figure 3).
By reorganizing the use of existing institutional resources into new scientific and data gateway processes, the information technology component provided a refined platform for investigators to access and evaluate health system data. For example, these data were used by UAB researchers within the Quality and Safety SWG to quickly produce a retrospective analysis of hospital‐acquired pressure injuries during the early stages of the pandemic, determining if the newly adopted inpatient telehealth approaches were able to simultaneously minimize the onset of pressure injuries and reduce the risk of COVID‐19 exposure among nursing staff. 24 Results from this analysis were used to inform and alter the operations of UAB Wound, Ostomy, and Continence (WOC) nursing staff and direct resources within the UAB nursing administration to produce a hospital‐acquired pressure injury root cause analysis. 24
3.3.7. Patient outcomes component: Patient and stakeholder advisory group
The Patient Outcomes Component is a mechanism for stakeholder perspectives and experiences to be captured while informing operations within the Organization and Collaborations, Performance, and Ethics and Security Components. The importance of this component is exemplified both in the prominence of stakeholder partnerships in patient‐centered outcomes research and increased focus on patient experience by health systems (Figure 1). Social distancing restrictions and the speed at which research and patient care pathways developed in response to COVID‐19 represented a challenge to traditional stakeholder engagement processes. 16 Thus, the patient and stakeholder engagement committee included five members selected for inclusivity and diversity relative to the larger population of patients and caregivers in the health system. 25 Because of the prioritization of patient care and strain on the healthcare system, this committee largely represented a convenience sample of patients and stakeholders connected to the hospital and institution. Strategic planning for a larger UAB LHS initiative, catalyzed by COVID‐19 CORE, includes prioritization of recruitment of a broader swath of patients and stakeholders to maximize inclusivity and representation.
The stakeholder network of the UAB COVID‐19 CORE was further developed with active participation, defined as participation within biweekly or monthly meetings, of frontline healthcare providers. Ongoing outreach to Birmingham city and Alabama state communities, through social media and weekly online events related to COVID‐19, and established relationships with community partners predating the COVID‐19 pandemic are supporting further developments of the network. 26
4. DIVERSIFYING NETWORK CAPABILITIES
Diversifying network capabilities is essential to ensuring an agile LHS, a system capable of responding to the dynamic and uncertain healthcare environment related to the COVID‐19 pandemic and sustainably advancing learning capabilities beyond the pandemic. 27 To assess interdisciplinary functionality of COVID‐19 CORE, the team used social network analysis examining emergent informal work patterns. We created a list of members in PWG and SWG. These data were used to create an affiliation‐based interdisciplinary network representing individual connections within each of the PWG and SWG. Attribute data, based on an individual's professional rank, was used to determine multilevel functionality (Figure 4a). UCINET 6 software for social network analysis was used to calculate the degree centrality of individuals and working groups. 28 Degree centrality, created with NetDraw graph visualization software's layout with node repulsion and equal edge length bias, is the sum of the number of ties a node has with other nodes, larger nodes have a greater number of connections to working groups and members (Figure 4b). 29
FIGURE 4.
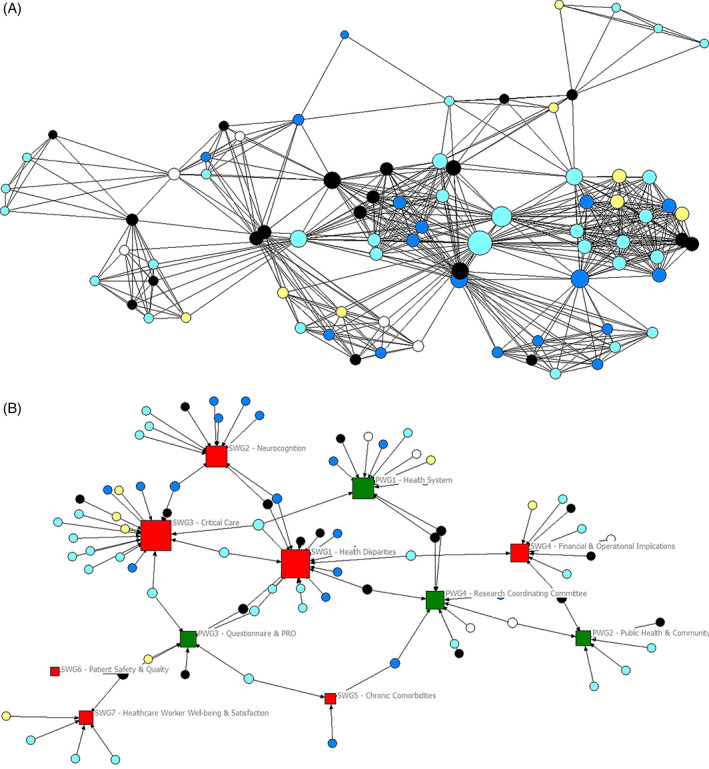
(A) UAB COVID‐19 Collaborative Outcomes Research Enterprise (CORE) diversity by rank. Diversity of professional rank within the COVID‐19 CORE. The size of each circle corresponds to the number of representatives of each rank within each school or center supporting the CORE. Professional rank is indicated by circles: white = staff, yellow = trainee, light blue = assistant professor, dark blue = associate professor, black = full professor. (B) UAB COVID‐19 Collaborative Outcomes Research Enterprise (CORE) degree centrality network diagram. The network diagram was created using NetDraw graph visualization software's layout with node repulsion and equal edge length bias. This is a two‐mode network with individual nodes indicated by circles, Programmatic Working Groups indicated by green squares, and Scientific Working Groups indicated by red squares. Professional rank is indicated by circles: white = staff, yellow = trainee, light blue = assistant professor, dark blue = associate professor, black = full professor
The interdisciplinary approach to the UAB COVID‐19 CORE development was both intentional and instrumental to the success of the efforts. The benefits of team science are noted within a growing body of research indicating that interdisciplinary teams are critical to maximize innovation and support high‐impact research endeavors. 30 , 31 In addition, institutions supporting intradepartmental and interuniversity collaborations can produce long‐term engagement within the system by ensuring equitable access to information, providing time and opportunities to collaborate, and maintaining an institutional culture for knowledge sharing. 32 , 33 Considering the unique culture and diversity of expertise within UAB, interdisciplinary teams flourished within the SWG of the COVID‐19 CORE; such that, diversity in career level and expertise provided a rich environment for scientific collaborations while fostering innovation and providing a unique institutional environment for knowledge sharing. 32 As an academic medical center, education and mentorship are essential components of UAB's institutional mission. Thus, as SWG evolved with diversity of career levels and potential for career development in mind, early stage investigators and trainees were linked with more senior investigators to build sustainable mentoring relationships. This creative approach to career development ensures the continual progress and emergence of interdisciplinary researchers committed to LHS development. 33
In addition, the leadership within the Executive Committee cultivated and currently maintains a collaborative mindset that is representative of the overall organizational culture found within UAB. Organizational culture includes the values and behaviors that drive the policies, practices, and guiding philosophies of an institution. 34 Recently listed by Forbes as one of the best employers for diversity in America, UAB is a nationally recognized leader in diversity, equity, and inclusion; perspectives and values that foster collaborative endeavors and support sustainable interdisciplinary system development. 35 While this culture existed prior to the pandemic, the COVID‐19 CORE provided a tangible structure organized by a rigorous framework to bring this culture to life within a functional LHS.
5. DISCUSSION
This experience report details three principal characteristics of institutional learning health system development, derived from the experience of the UAB COVID‐19 CORE, including: (a) identifying network contributors, (b) building the institutional network, and (c) diversifying network capabilities. We suggest this framework could support academic health systems interested in LHS development but not currently engaged in LHS initiatives. In particular, the LHS framework supported critical evaluation of governance and organizational structures in alignment with the proposed seven structural components, dynamic learning and research engines. From our experience, the COVID‐19 CORE, grounded in the LHS framework, is a key catalyst for larger institutional LHS initiatives extending beyond the original purpose and focus on COVID‐19.
For example, in March 2021, we launched a LHS month featuring UAB and national speakers to discuss developing and advancing learning systems across a variety of topics within the institution; these lectures were highly attended with 70 to 100 participants per weekly session over a 5‐week period. 36 A LHS task force was also developed, comprised of academic and health system leadership, and charged with implementing subsequent LHS efforts at UAB. Based on the recommendations from this committee, the UAB Health System is sponsoring a LHS predoctoral fellow to engage in the dissemination of findings from improvement programs and fostering embedded research and scholarship initiatives at UAB Medicine. Finally, the health system has tentatively agreed to financially sponsor the scientific gateway that will connect frontline healthcare leaders with researchers in a process linking the learning and research engines that were initially designed for the COVID‐19 CORE.
5.1. Mobilization and sustained engagement of individuals and resources
Faced with adversity, as imposed by the global COVID‐19 pandemic, we learned three critical lessons for sustainable mobilization and engagement of individuals and resources within a learning system: (a) identify a common issue or concern that many individuals within the organization can be energized to consider, (b) identify areas for increased efficiency within existing resources and personnel, and (c) estimate the costs, resources, and labor required to meet the demands of the system. While the COVID‐19 pandemic was clearly an extraordinary concern for everyone within the organization, the pandemic experience varied drastically across departments within UAB. As an academic medical center, UAB strove to maintain high quality clinical care while simultaneously ensuring safety among faculty, staff, and students. Thus, many clinical and academic departments operated as polar opposites, with clinical programs treating COVID‐19 patients at maximum capacity but many academic programs working from home and minimizing interpersonal contact. This unprecedented situation highlighted opportunities to engage and collaborate across departments within the shared experience of COVID‐19. For example, reorganizing human resources within the CCTS, COERE, and Informatics Institute supported the development of the scientific and data gateway processes. The results from these processes where then used to inform clinical practices on campus at the UAB hospital. 21 , 24
Situating and structuring the COVID‐19 CORE initiative according to the LHS framework was essential for purposeful mobilization and engagement of individuals and groups, ensuring financial resources aligned with increasing the capacity of the LHS across the institution. Initially generated by volunteer effort, we leveraged in kind support through the existing CCTS, COERE, and Informatics Institute for the development of the LHS and reorganized human resources via the scientific and data gateways to create new efficiencies with existing personnel and resources. Grounding the COVID‐19 CORE within the LHS framework provided clear connectivity, highlighting specific functions for sustained participation and presenting opportunities to estimate costs, identify required resources, and minimize gaps in personnel to support the system. The importance of such a framework became apparent early within the formation of COVID‐19 CORE when initial focus on the Data Component and PWG left many individuals feeling scientifically concerned. The rapid deployment of SWG, representing the Scientific Component, addressed these considerations with priority scientific questions that informed the establishment of the COVID‐19 shared database (Figure 4). The seven emergent SWG remain active as of August 2021 with monthly meetings of members, generation of peer review manuscripts, and development of grant applications extending into non‐COVID‐19 questions aligned with the thematic focus of each group.
Beyond engagement of individuals, the framework allowed for effective integration of several UAB centers and institutes by leveraging existing resources to catalyze this initiative. Led by UAB COERE, pre‐existing and ongoing discussions with UAB Medicine leadership about LHS were vital to engendering support for COVID‐19 CORE. Moreover, collaborative initiatives and resources afforded by the CCTS and Informatics Institute were essential. For example, the Patient‐Reported Outcomes Measurement Information System, CCTS, Biostatistics Epidemiology and Research Design (BERD), and COERE programs were in existence prior to the pandemic; investigators were able to leverage these programs to collect COVID‐19 related data and to support the organization and development of the COVID‐19 CORE. Notably, the existence of these research‐oriented entities allowed for rapid restructuring and alignment of human resources within the LHS framework via the scientific and data gateways, providing a platform and process to conduct COVID‐19 health system studies.
6. CONCLUSION
By design, components of the LHS framework were populated by interdisciplinary individuals who had not previously worked together, drawing from the health system learning and academic research engines. Speaking to the value of these new collaborations, on the initial call, a frontline provider commented, “I am not a researcher, but I have a lot of questions.” This provider led the implementation of inpatient telehealth approaches to facilitate remote clinician rounds within the UAB hospital system and support conservation efforts for personal protective equipment during national shortages throughout the pandemic. 21 Evaluation of this inpatient telehealth approach, facilitated by the COVID‐19 CORE, answered the provider's questions on the effectiveness, safety, and outcomes of this approach. 21 As representation of frontline providers within the LHS increases, we anticipate greater agility within the LHS to prioritize their questions and to formulate a response that is representative and inclusive of their voices, questions, and concerns.
6.1. LHS framework as a foundational cornerstone to catalyze and critically assess LHS form and functions
Prior to the COVID‐19 pandemic, some LHS components were in place within UAB; several clinical areas had effectively localized LHS implementation fostering ongoing discussion about healthcare delivery and research connections. Applications of these existing programs within the LHS framework provided concrete structure to guide the COVID‐19 CORE in conducting rigorous high‐quality research studies, aligned with the form and functions attributed to LHS. Providing proof‐of‐concept, aligned with other ongoing initiatives, there is potential for the COVID‐19 CORE experience to accelerate learning system development in other areas of UAB Medicine. The foundational role of the LHS framework in mobilizing, organizing, and catalyzing such efforts is clear in the case of the UAB COVID‐19 CORE. The framework holds potential to sustain engagement and fulfill the functions of LHS more broadly, but the effectiveness of expansion to other areas beyond COVID‐19 remains to be seen and represents a future opportunity for systematic evaluation. Moreover, application of the LHS framework as a catalyst for other health systems to achieve the promise and potential of the LHS represents an opportunity for future implementation and investigation. Finally, critical appraisal of existing UAB programs and collaborative networks relative to the seven structural components of the LHS framework, and dynamic learning and research engines, may identify opportunities for institutional enhancement and purposeful interdisciplinary engagement.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
The authors would like to thank the members of the University of Alabama at Birmingham (UAB) COVID‐19 CORE, the UAB Center for Outcomes and Effectiveness Research and Education (COERE), and UAB Center for Clinical and Translational Science (CCTS). The learning health system scoping review, used as a foundation for this manuscript, was presented at the Translational Science Conference 2019 in Washington D.C. on 6 March 2019. The results of this experience report were presented at the Virtual Translational Science Conference 2021 on 30 March 2021.
Anderson JL, Reamey RA, Levitan EB, et al. The University of Alabama at Birmingham COVID‐19 Collaborative Outcomes Research Enterprise: Developing an institutional learning health system in response to the global pandemic. Learn Health Sys. 2022;6(2):e10292. doi: 10.1002/lrh2.10292
REFERENCES
- 1. Lescure FX, Bouadma L, Nguyen D, et al. Clinical and virological data of the first cases of COVID‐19 in Europe: a case series. Lancet Infect Dis. 2020;20(6):697‐706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City area. JAMA. 2020;323(20):2052‐2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patel A, Jernigan DB, 2019‐nCoV CDC Response Team . Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak‐United States, December 31, 2019‐February 4, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(5):140‐146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Trump D. Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID‐19) Outbreak 2020. Washington, D.C.: White House Press Office; 2020. https://www.govinfo.gov/content/pkg/FR-2020-03-18/pdf/2020-05794.pdf [Google Scholar]
- 5. WBRC Staff ADPH confirms first case of coronavirus in Alabama. https://www.wbrc.com/2020/03/13/adph-confirms-first-confirmed-case-coronavirus-alabama/. Accessed April 22, 2021.
- 6. Guo G, Ye L, Pan K, et al. New insights of emerging SARS‐CoV‐2: epidemiology, etiology, clinical features, clinical treatment, and prevention. Front Cell Dev Biol. 2020;8:410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McLachlan S, Potts HWW, Dube K, et al. The Heimdall framework for supporting characterisation of learning health systems. J Innov Health Inform. 2018;25(2):77‐87. [DOI] [PubMed] [Google Scholar]
- 8. Anderson JL, Mugavero MJ, Ivankova NV, Reamey RA, Varley A, Cherrington A. Adapting an interdisciplinary learning health system framework for academic hospitals and medical centers: a scoping review. Under Review. [DOI] [PubMed]
- 9. Field B, Booth A, Ilott I, Gerrish K. Using the knowledge to action framework in practice: a citation analysis and systematic review. Implement Sci. 2014;9:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Spooner A, Aitken L, Chaboyer W. Implementation of an evidence‐based practive nursing handover tool in intensive care using the knowledge‐to‐action framework. Worldviews Evid Based Nurs. 2018;15(2):88‐96. [DOI] [PubMed] [Google Scholar]
- 11. Keshavjee K, Morrison D, Mohammed S, Guergachi A. IT for bending the healthcare cost curve: the high needs, high cost approach. Stud Health Technol Inform. 2017;243:178‐182. [PubMed] [Google Scholar]
- 12. Lessard L, Michalowski W, Fung‐Kee‐Fung M, Jones L, Grudniewicz A. Architectural frameworks: defining the structures for implementing learning health systems. Implement Sci. 2017;12:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Prokosch HU, Acker T, Bernarding J, et al. MIRACUM: medical informatics in research and care in university medicine. Methods Inf Med. 2018;57(S 01):e82‐e91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. U.S. White House . Federal enterprise architectural framework II. https://obamawhitehouse.archives.gov/sites/default/files/omb/assets/egov_docs/fea_v2.pdf. Accessed November 10, 2018.
- 15. UAB Medicine . Facts and figures. https://www.uabmedicine.org/facts-and-figures. Accessed April 22, 2021.
- 16. Boyer AP, Fair AM, Joosten YA, et al. A multilevel approach to stakeholder engagement in the formulation of a clinical data research network. Med Care. 2018;56(10 suppl 1):S22‐S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Flier J. COVID‐19 is reshaping the world of bioscience publishing. STAT. https://www.statnews.com/2020/03/23/bioscience‐publishing‐reshaped‐covid‐19/. Accessed April 21, 2021.
- 18. Braithwaite R, Warren R. The African American petri dish. J Health Care Poor Underserved. 2020;31(2):1‐12. [DOI] [PubMed] [Google Scholar]
- 19. Yancy CW. COVID‐19 and African Americans. JAMA. 2020;323(19):1891‐1892. [DOI] [PubMed] [Google Scholar]
- 20. Gamble VN. A legacy of distrust: African Americans and medical research. Am J Prev Med. 1993;9(6):35‐38. [PubMed] [Google Scholar]
- 21. Kennedy KC, Hearld KR, May B, et al. Inpatient telehealth and coronavirus disease 2019 outcomes: experiences in Alabama. Telemed Rep. 2021;2(1):148‐155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. RTI International . PhenX Toolkit. https://www.phenxtoolkit.org/covid19/. Accessed June 18, 2020.
- 23. i2b2 . Informatics for integrating biology and the bedside. https://www.i2b2.org. Accessed June 18, 2020.
- 24. Polancich S, Hall AG, Miltner R, et al. Learning during crisis: the impact of COVID‐19 on hospital‐acquired pressure injury incidence. J Healthc Qual. 2021;43(3):137‐144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res. 2014;14:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. UAB School of Public Health COVID‐19's impact on the Black community. https://www.youtube.com/watch?v=yd982c1-_X8XX. Accessed June 18, 2020.
- 27. Potts J, Thompson R, Merchant R, et al. Learning: contemplating the unexamined core of learning health systems. Learn Health Syst. 2017;1(4):e10036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Borgatti SP, Everett MG, Freeman LC. UCINET 6 for Windows: Software for Social Network Analysis. Harvard, MA: Analytic Technologies; 2002. [Google Scholar]
- 29. Borgatti SP. NetDraw: Graph Visualization Software. Harvard, MA: Analytic Technologies; 2002. [Google Scholar]
- 30. Bridle H, Vrieling A, Cardillo M, Araya Y, Hinojosa L. Preparing for an interdisciplinary future: a perspective from early‐career researchers. Futures. 2013;53:22‐32. [Google Scholar]
- 31. Lyall C, Meagher LR. A Masterclass in interdisciplinarity: research into practice in training the next generation of interdisciplinary researchers. Futures. 2012;44(6):608‐617. [Google Scholar]
- 32. Stokols D, Misra S, Moser RP, Hall KL, Taylor BK. The ecology of team science: understanding contextual influences on transdisciplinary collaboration. Am J Prev Med. 2008;35(2 suppl):S96‐S115. [DOI] [PubMed] [Google Scholar]
- 33. Hall KL, Feng AX, Moser RP, Stokols D, Taylor BK. Moving the science of team science forward: collaboration and creativity. Am J Prev Med. 2008;35(2 suppl):S243‐S249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Trudel J. Organizational culture in higher educational institutions: link to sustainability initiatives. In: Leal Filho W, Azul A, Brandli L, Özuyar P, Wall T, eds. Quality Education. Encyclopedia of the UN Sustainable Development Goals. Cham, Switzerland: Springer. 2020:600–610. [Google Scholar]
- 35. Rohan A. Forbes names UAB one of America's best employers for diversity. https://www.uab.edu/news/campus/item/11983-forbes-names-uab-one-of-america-s-best-employers-for-diversity. Accessed August 29, 2021.
- 36. UAB Center for Outcomes and Effectiveness Research and Education . https://www.uab.edu/medicine/coere/news-events/uab-s-learning-health-system-month. Accessed April 22, 2021.


