Abstract
COVID‐19 lockdown measures have profoundly impacted adolescent’ daily life, with research suggesting an increase in irritability, stress, loneliness, and family conflict. A potential protective factor is parent–child relationship quality; however, no studies have investigated this. We used data from SIGMA, a longitudinal, experience sampling cohort study, in which N = 173 adolescents aged 11 to 20 were tested before and during COVID‐19. Multilevel analyses showed decreased daily‐life irritability and increased loneliness from pre‐ to mid‐pandemic. Daily‐life stress levels were unchanged. Relationship quality was negatively associated with irritability and loneliness and buffered against the increase in loneliness. Effect sizes were small and do not support a strong effect of the first lockdown on irritability, stress, loneliness, and family conflict in adolescents.
Keywords: COVID‐19, adolescence, daily life
The current spread of the novel SARS‐CoV‐2 (COVID‐19) virus is a major threat to physical and, along with the national lockdown measures imposed, also to mental health (WHO, 2020). Although there has been much media speculation about the adverse impact of this crisis on mental health and family life, there has been little empirical investigation of this. Moreover, emerging research on the impact of COVID‐19 on mental health (Moccia et al., 2020; Veer, Riepenhausen, Zerban, Wackerhagen, & Engen, 2020) is limited to adult studies, with a few notable exceptions (Green et al., 2021; Janssen et al., 2020; Magson et al., 2021; Widnall et al., 2020). However, adolescents are a population group who may be especially vulnerable to any mental health impacts of COVID‐19.
Adolescence is a developmental period where the vast majority of mental health conditions have their onset (Solmi et al., 2021). Large‐scale US research suggests that 75% of adults who report ever having a mental health condition indicate they experienced their first symptoms during adolescence (Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012). Along with significant physical and psychological changes, adolescence is a period of profound social transformation, where both peer and parent interactions are crucial for the development of adolescents into independent adults (Andrews, Ahmed, & Blakemore, 2020; Blakemore & Mills, 2014; Steinberg & Morris, 2001). During this period, adolescents strive to become independent and focus more on socializing and spending time with friends rather than with their families. Consequently, the drastic changes in daily social life due to the pandemic and associated lockdown measures may have particularly affected adolescents, as they are at a a critical stage of social development (Andrews et al., 2020; Orben, Tomova, & Blakemore, 2020). Adolescents’ enforced proximity to their families and the limitation of face‐to‐face contacts with peers may not allow their developmental needs to be met (Andrews et al., 2020; Grusec & Davidov, 2021; Orben et al., 2020; Steinberg & Morris, 2001). Findings from emerging research during the pandemic suggest an increased vulnerability for mental health problems in adolescents as compared to adults (Magson et al., 2021); however, some studies suggest a decrease in psychopathology symptoms (Widnall et al., 2020). To learn more about these conflicting findings on the impact of COVID‐19 on adolescent mental health, we may need to focus more on mental health symptoms at a subclinical level.
Several studies and viewpoint papers have suggested an increase in irritability, stress, and loneliness in adolescents due to the sudden global virus outbreak and government‐imposed lockdown regulations, which may be precursors to later mental health problems (Hasking et al., 2021; Loades et al., 2020; Panda et al., 2021). For example, previous studies found that irritability was fairly common among quarantined adolescents (Panda et al., 2021), possibly due to the increased parental involvement, reducing adolescents’ privacy and time alone (Hasking et al., 2021; Wang, Zhang, Zhao, Zhang, & Jiang, 2020). An increase in stress may also be expected, as adolescents worry about their own and loved ones’ safety during the pandemic, as well as their school education, given the swift transition to online learning from home (Ellis, Dumas, & Forbes, 2020; Hasking et al., 2021). Additionally, limitation of face‐to‐face contact with peers potentially increased concerns about maintaining close social connections during a period where these are crucial for adequate development and mental well‐being (Andrews et al., 2020; Grusec & Davidov, 2021; Smetana, Robinson, & Rote, 2015). Therefore, enforced physical distancing may have led adolescents to feel lonely during the COVID‐19 pandemic (Ellis et al., 2020; Loades et al., 2020). The broader literature emphasizes how these daily‐life outcomes, that is, irritability, stress, and loneliness, are related to negative physical and mental health outcomes, for example, anxiety disorders, depression, and suicidal behavior and mortality (Brotman, Kircanski, & Leibenluft, 2017; Hawkley & Cacioppo, 2010; McClelland, Evans, Nowland, Ferguson, & O'Connor, 2020; Romeo, 2017; Stringaris, Vidal‐Ribas, Brotman, & Leibenluft, 2018). As such, investigating proximal vulnerability and protective factors for irritability, stress, and loneliness could inform efforts to mitigate or prevent mental health problems in adolescents.
In addition to the potential impact of the COVID‐19 pandemic on adolescents’ levels of irritability, stress, and loneliness, several review papers suggest an impact on the family system as a whole (Campbell, 2020; Prime, Wade, & Browne, 2020). To understand this, we can draw upon the Family Resilience Model (FRM; Henry, Sheffield Morris, & Harrist, 2015): a theoretical framework describing how families as systems navigate unexpected adversity, such as the COVID‐19 pandemic, given certain pre‐existing protective and vulnerability factors. The FRM includes four basic elements that play a role in family resilience: family risk, protection, vulnerability, and adaptation. Families each have their own set of vulnerabilities and protective factors, which combine with certain risks (i.e., stressors) to produce a unique response to adversity. Both protection and adaptation occur within the Family Adaptive Systems (FAS) that are described in the FRM as arising from family interactions, which develop and regulate key domains of everyday family life. The five FAS within the FRM include, but are not limited to, meaning, emotion, control, maintenance, and stress response systems. For example, from the perspective of the FRM, the Stress Response System regulates the level of change and stability in the family equilibrium on a meta‐level. The other FAS influence how a family develops what is necessary to regulate family goals, structures, and interaction patterns, and adapt to the incoming adversity. For example, when the quality of parent–child relationships (an aspect of the Family Emotion Adaptative System) is poor before a new incoming challenge, this can limit family resilience and the adversity may further worsen the relationship. At the same time, when there is already a high level of conflict (an aspect of the Family Control Adaptative System), this may increase the distress during adversity and heighten the level of conflict in the family (Henry et al., 2015).
Emerging research suggests COVID‐19‐related stress, fear, uncertainty, limited support networks, and social isolation are risk factors for family conflict during the pandemic (Campbell, 2020; Guessoum et al., 2020). Another conceptual framework, recently proposed by Prime et al. (2020), posits that the social disruptions caused by the pandemic may heighten stress in parents, which in turn negatively affects parental, parent–child, and sibling relationships. Parents’ stress increases during the pandemic because they are searching for a new work‐family balance (e.g., shift in routines and structures), dealing with job insecurity/loss, as well as concerns about their safety and that of their loved ones. When parents’ mental and emotional resources are exhausted, ensuring the positive functioning of the family is difficult (Prime et al., 2020). This proposed cascading process suggests that family conflict is a particularly relevant risk factor for adolescent adjustment and well‐being (Browne, Plamondon, Prime, Puente‐Duran, & Wade, 2015). Therefore, it is of utmost importance to understand the consequences of the COVID‐19 pandemic on adolescents and their families. High‐quality parent–child relationships may buffer against the risk of negative outcomes in the context of COVID‐19 by promoting resilience (Prime et al., 2020), whereas poor parent–child relationships within families may create vulnerability to the negative effects of the pandemic on family life, for example, family conflict (Henry et al., 2015).
Previous research has shown that high‐quality parent–child relationships can protect adolescents against the impact of stressors (Dimitry, 2012; Kronenberg et al., 2010; Wickrama & Kaspar, 2007) as this can provide them with the opportunity to more easily identify, describe and share feelings with others (Cerutti, Zuffianò, & Spensieri, 2018; Gandhi et al., 2019). Conversely, adolescents with lower quality parent–child relationships might lack the skills to find support from others and share difficulties, meaning their strategies for dealing with adversity fall short (Brumariu & Kerns, 2010; Shpigel, Diamond, & Diamond, 2012). During adolescence, the need for (physical) proximity from the parental figure changes to the need for (emotional) availability, as self‐regulatory skills grow with age. Nevertheless, adolescents still need their parents to be available in times of need, because peer relationships are still developing and the intense emotions—inherent to adolescence—may be overwhelming (Bosmans & Kerns, 2015).
The broader literature has shown that low‐quality parent–child relationships are associated with more frequent and burdensome family conflict, whereas high‐quality parent–child relationships are associated with less frequent and less burdensome family conflict (Hannum & Dvorak, 2004; Shpigel et al., 2012). Therefore, children with poor parent–child relationships and their families are potentially more strongly impacted by stressors such as the pandemic. However, no published research in adolescents so far has investigated the presumed impact on irritability, stress, loneliness, and family conflict during this pandemic, and how the quality of paternal and maternal relationships may be associated with these outcomes. More specifically, how and to what extent the quality of paternal and maternal relationships can mitigate or exacerbate the pandemic’s potential impact on these daily‐life outcomes, and family conflict. Insights into these associations may help us to identify adolescents and families at risk of adverse mental health outcomes or experiencing heightened conflict and to develop effective strategies to support them.
Research on mental health and family dynamics during COVID‐19 faces two major challenges. First, in order to investigate dynamic processes such as irritability, stress, and loneliness in adolescents, it is necessary to look at these outcomes in an ecologically valid manner by targeting them in the context where they naturally occur: daily life. The Experience Sampling Method (ESM; Csikszentmihalyi & Larson, 1987; Myin‐Germeys et al., 2018) enables data on adolescents’ activities, thoughts, and experiences to be captured within the context of their natural daily life, by completing multiple brief questionnaires on a smartphone over a period of several days. The use of ESM to assess feelings of irritability, stress, and loneliness is expected to improve the accuracy of measurements by reducing recall bias and increasing ecological validity. Second, the vast majority of studies examining psychological and social effects of COVID‐19 are cross‐sectional. Consequently, we lack data on key predictors (and outcomes) from before the pandemic. Considering that prepandemic vulnerability factors may heighten risk of negative psychological outcomes and family conflict (Prime et al., 2020), longitudinal data which enables comparison of predictors and outcomes pre‐ and during‐pandemic is essential. To this end, the current study leverages pre‐COVID‐19 data from an ongoing adolescent cohort study including ESM (SIGMA; Kirtley, Achterhof, et al., 2021; Kirtley, et al., 2020; Kirtley, Achterhof, et al., 2021) in combination with data collected from a subgroup of these adolescents during the first COVID‐19 lockdown (Achterhof, Myin‐Germeys, et al., 2021).
Our study aims to investigate to what extent the quality of a parent–child relationship is associated with changes in adolescents’ levels of irritability, stress, and loneliness in daily life from before to during the COVID‐19 pandemic. We also examine whether the quality of the parent–child relationship is associated with adolescents’ experiences of COVID‐19‐related family conflict and its perceived burden. First, we hypothesize that there will be an increase in adolescents’ levels of irritability, stress, and loneliness in daily life from before to during the pandemic. Second, we predict that adolescents who report a lower quality of paternal and maternal relationships will be more likely to report higher levels of irritability, stress, and loneliness in daily life before and during the pandemic. Third, we expect that changes in adolescents’ daily life levels of irritability, stress, and loneliness from before to during the pandemic will be moderated by the quality of the paternal and maternal relationships, such that adolescents with a lower quality of relationships exhibit a larger increase in irritability, stress, and loneliness. Fourth, we hypothesize that adolescents who report a lower quality of paternal and maternal relationships will be more likely to experience more frequent and burdensome family conflict during the pandemic.
METHOD
Socio‐Cultural Context
For the current study, we used data from two waves of the SIGMA study: Wave I and Wave COVID‐19. SIGMA is a large‐scale, accelerated longitudinal study that investigates the mental health and development of adolescents. Wave I of the SIGMA study included data from 1913 adolescents from 22 schools in Flanders, the Northern, Dutch‐speaking region of Belgium and took place between January 2018 and June 2019. Flanders counts approximately 6.6 million people (Statbel, 2020) of which 457,000 are in secondary education (Statistiek Vlaanderen, 2019). The sample was representative in terms of sex, education level, and geographical spread.
Wave COVID‐19 of the SIGMA study occurred during the first national lockdown from the 27th of April until the 10th of May. On the March 18, 2020, the Belgian government decided to impose restrictive measures to prevent the spread of COVID‐19. There was a stay‐at‐home order, and schools and nonessential shops were closed. In the week of the 4th of May, some measures were lifted (e.g., outdoor activities with a friend) and it was announced that other regulations (e.g., schools) would be lifted in the near future (Belgische Federale Overheidsdiensten, 2020).
Participants and Recruitment
For a detailed description of the measures and sample from the full SIGMA study, see Kirtley, Achterhof, et al. (2021), Kirtley, et al. (2020), and Kirtley, Lafit, et al. (2021). For an overview of the complete COVID‐19 Wave of SIGMA, see Achterhof, Myin‐Germeys, et al. (2021). See Appendix S1 for a full overview of the self‐report measures used for the full Wave I of the SIGMA study and Wave COVID‐19.
Wave I took place between January 2018 and June 2019 and includes data from 1913 adolescents, recruited via 22 mainstream secondary schools. The majority of the schools were recruited via their existing relationship with Te Gek!?, a Flemish nongovernmental organization that aims to break taboos surrounding discussion of mental health, and a partner organization of the SIGMA study. After the board of the secondary school had agreed with participation, the research team visited the school to explain the study and recruit potential participants. The parents/caregivers and potential participants were sent an information letter with further details. The majority of the sample were female (n = 1207; 63%), n = 695 were male (36%) and 11 participants indicated ‘Other’ (<1%). Within Wave I, age ranged from 11 to 20 years (M = 13.76 years, SD = 1.86 years). Inclusion criteria were being in the first, third, or fifth year of mainstream secondary education, having an adequate command of Dutch and having provided informed consent, both from themselves and their parent/caregiver. Within the current study, we only included adolescents that have participated in both Wave I and Wave COVID‐19.
Wave COVID‐19 occurred during the first national lockdown in Belgium due to COVID‐19 from the 27th of April until the 10th of May. From the full Wave I sample, it was possible to contact 1581 of 1913 adolescents via email (for n = 239, there was no contact information available and for n = 93 the contact information was erroneous). Of those, n = 173 took part in this second follow‐up wave, and n = 110 participated in the ESM part of the study. Regarding the family situation of this group, n = 146 indicated having both a father and a mother in their lives, n = 2 indicated having two fathers, while 2 other participants indicated having only one father or one mother. The other n = 17 indicated ‘Other’ (if none of the other options were relevant to them) or did not answer the question about their family situation. Inclusion criteria for the COVID‐19 measurement were having participated in Wave I of SIGMA, providing contact information for follow‐up contact at Wave I, being able to complete baseline questionnaires in REDCap (Harris et al., 2009), having provided informed consent and if younger than 18 years of age, providing informed consent from a parent/caregiver as well. Both SIGMA Wave I and COVID‐19 received full approval from the UZ/KU Leuven Medical Ethics Committee (S61395).
Procedure
Wave I
The full procedure for Wave I of the SIGMA study is described in detail in Kirtley, Achterhof, et al. (2021), Kirtley, et al. (2020), and Kirtley, Lafit, et al. (2021). During school hours (100 min), instructions were given to the participants by the research team where they received an explanation about the purpose of the study, as well as where they had the opportunity to ask questions and were guided through a demo of the full ESM questionnaire. Participants completed self‐report questionnaires in school on a tablet using the REDCap application (Harris et al., 2009). At the end of the testing session, all participants received a support sheet with contact details for relevant support services, including local and national crisis and advice phone lines.
Daily‐life data were collected using the ESM. To complete the ESM questionnaires via the MobileQ app (Meers, Dejonckheere, Kalokerinos, Rummens, & Kuppens, 2020), participants received a smartphone device (Motorola Moto E4) from the research team. The sampling scheme was semi‐random signal‐contingent with an ESM questionnaire 10 times a day, for six consecutive days. The questionnaire consisted of a minimum of 39 items and a maximum of 46 items with an average completion time of 162.8 s. The notification would buzz or beep for 90 s or until the participants opened the notification. To complete each item, they had 90 s. Participants were instructed to answer these items with the moment right before the notification in mind (e.g., ‘I feel irritated’). Compensation for participation was a 10‐euro gift voucher for a physical or online store. In addition, schools received mental health‐themed psychoeducation sessions, workshops or educational materials, delivered in cooperation with Te Gek!?. Participants received no feedback on their ESM compliance and were included irrespective of their rate. The average compliance during Wave I was 39.5% across all participants (N = 1913) and notifications. The MobileQ app did not allow partial responses to be saved until October 25, 2018.
Wave COVID‐19
The data collection procedure for Wave COVID‐19 was kept as similar as possible to that of Wave I, but was conducted completely remotely. Participants were invited to take part via email and received instructions via a prerecorded video made by the research team. The self‐report questionnaire battery was slightly adapted for this follow‐up (e.g., inclusion of a questionnaire assessing experiences of COVID‐19‐related stressors, such as family conflict).
As the MobileQ application used in Wave I, was not suited for remote data collection, participants installed another experience sampling application, SEMA3 (Koval et al., 2019) on their own smartphone device. The sampling scheme for Wave COVID‐19 was the same for Wave COVID‐19, but the momentary questionnaire consisted of 40–45 items (depending on conditional branching), as well as once‐a‐day morning (10 items) and evening questionnaires (21 items). The questionnaire expired after 10 min, even if participants were still completing items. All data until the moment of expiry were saved on the phone. If participants had not opened the questionnaire, a reminder was sent to the participants after five minutes. Compensation for participation in this wave was a 10‐euro gift voucher for an online store. For the group of 110 participants with ESM data in the COVID‐19 measurement, the compliance rate was 43.6%.
Measures
Self‐report questionnaires
Relationship quality (Wave I)
The quality of the parental relationship was assessed with a Dutch version of the Inventory of Parent and Peer Attachment (IPPA; Armsden & Greenberg, 1987; translated into Dutch by Noom, Deković, & Meeus 1999), a 36‐item self‐report questionnaire at baseline in Wave I of the SIGMA study. Both paternal and maternal relationship qualities was assessed on three dimensions: trust, communication, and alienation. To assess relationship quality, a sum score was used that added the Trust and Communication item scores and subtracted the Alienation item scores. Items were rated on a 4‐point Likert‐type scale (from 1 = Almost never to 4 = Almost always). For example, ‘My mother respects my feelings’ and ‘I feel angry with my mother’. As both one‐ and two‐factor models have been suggested for the IPPA (Gandhi et al., 2016; Murphy, Laible, & Augustine, 2017), we conducted a confirmatory factor analysis to test whether a two‐factor (separate father and mother relationship quality scores) or a one‐factor (composite parental relationship quality score) was most appropriate. The CFA in the present study showed that a two‐factor model (χ2 = 1404.3, AIC = 6479.7, BIC = 6597.0) was a better fit than the one‐factor model (χ2 = 1559.3, AIC = 6632.7, BIC = 6747.6). Paternal and maternal relationship qualities was weakly correlated (r = .17). Internal consistency was high (Cronbach’s ɑ = 0.90) for both the paternal and maternal relationship qualities scales.
Family conflict (Wave COVID‐19)
The experience and burden of family conflict during COVID‐19 were investigated with three items from the 22‐item COVID‐19‐related stressors questionnaire adapted from the DynaCORE survey on resilience, conducted as part of the DynaMORE project (https://dynamore‐project.eu/). Parental, parent–child, and sibling conflicts were assessed using the following three items: ‘In the following, some situations are listed that people may experience due to the current COVID‐19 pandemic. Please indicate if you are currently experiencing the following situations or have experienced these during the past 2 weeks in connection to the COVID‐19 pandemic, and how burdensome these are/were to you: (1) conflict between your parents, (2) conflict between you and your parents and (3) conflict between you and your siblings’. Presence vs. absence of family conflict in each of the three domains was measured using a binary ‘Yes’/‘No’ item. If participants indicated ‘Yes’ when asked about presence of family conflict, the follow‐up item was administered to assess the burden of the family conflict, with five response options ranging from ‘Not at all burdensome’ to ‘Very burdensome’. Cronbach’s ɑ for the family conflict scale was 0.54.
Age and sex (Wave I and Wave COVID‐19)
Given that previous research has highlighted differences in irritability, loneliness, and stress as a function of age (Friberg, Hagquist, & Osika, 2012; Van Roekel, Scholte, Verhagen, Goossens, & Engels, 2010) and sex (Friberg et al., 2012), we included these as covariates in the analysis.
Experience sampling
Irritability, stress and loneliness (Wave I and Wave COVID‐19)
To investigate momentary irritability, stress, and loneliness, the following items were used: ‘I feel irritated’, ‘I feel stressed’, and ‘I feel lonely’. These three items were rated on a 7‐point Likert scale ranging from 1 (Not at all) to 7 (Very much). All ESM items were presented in a fixed order.
Missing Data
From the 173 participants who took part in both waves, 22 were excluded due to completely missing data on their relationship quality scales and 75 had incomplete data for parental relationship quality (at least one item filled out for paternal or maternal relationship quality) assessed with the IPPA at baseline in Wave I of the SIGMA study. Therefore, these incomplete data (for n = 75) were imputed using multiple imputation by chained equations (MICE). This particular multiple imputation technique operates under the assumption that the missing data are Missing At Random and is recommended to address larger numbers of missing data in psychiatric research (Azur, Stuart, Frangakis, & Leaf, 2011). Within the current study, 20 imputed datasets were used to perform the analyses, and parameter estimates were pooled using Rubin’s rule (Eekhout, van de Wiel, & Heymans, 2019). All participants were asked to indicate whether they had: 1. ‘One father and one mother’, 2. ‘Two mothers’, 3. ‘Two fathers’, 4. ‘One father’, 5. ‘One mother’, or 6. ‘Other’. This provided us with information about the family situation of those who had incomplete data for parental relationship quality. Supplementary analyses showed that 63 of the 75 participants with incomplete data indicated to have both a mother and a father in their lives, 3 of them indicated ‘Other’ and 1 of them indicated having 2 fathers. These 67 participants received both questionnaires for paternal and maternal relationship qualities. The other eight participants (of the 75 with incomplete data) indicated having only one mother or one father, meaning they received only one questionnaire regarding relationship quality with their available parent. We only imputed data for paternal relationship quality if participants had completed at least one item for paternal relationship quality, and similarly for the imputation of maternal relationship quality data. Imputation was carried out in R studio (RStudio Team, 2020) with R version 4.0.3 (R Core Team, 2020) using the mice package (van Buuren & Groothuis‐Oudshoorn, 2011).
Open Science Practices
Hypotheses and planned analyses were postregistered on the Open Science Framework (OSF) after data collection but before data were accessed and analyses were conducted (Benning, Bachrach, Smith, Freeman, & Wright, 2019), using the registration template for ESM research (Kirtley, Achterhof, et al., 2021; Kirtley, et al., 2020; Kirtley, Lafit, et al., 2021). The postregistration is available at https://osf.io/83evy/?view_only=8cd6772e331c4b2595158186f70bdaf7. Please see Appendix S2 for changes that were made to the registration along with the full description of CFA results, list of ESM items, missing data procedure, R codes for all main and power analyses at https://osf.io/wdkxz/?view_only=661b8a0c433747e68aacfdb1d85b5ffe. ESM items used in Wave I of the SIGMA study are also publicly available in the ESM Item Repository (Kirtley, et al., 2020).
Data Analyses
For the research questions on the associations between relationship quality at Wave I and daily‐life irritability, stress, and loneliness at Wave I and Wave COVID‐19, we estimated linear mixed effects models, as these data have a multilevel structure with repeated measurements (i.e., observations) nested within persons. Multilevel models, that is, linear mixed effects models, enable us to analyze data that are organized at more than one level (i.e., nested data) by taking into account that observations within any given cluster at any level (e.g., observations nested within a person) can be expected to be more similar to each other than to observations within other clusters. In all multilevel models, we accounted for autocorrelation with the corAR1() component. For the analyses on relationship quality and family conflict, we used logistic regressions as the variables included were all time‐invariant. All analyses were carried out in R Studio (RStudio Team, 2020) with R version 4.0.3 (R Core Team, 2020).
Sensitivity power analysis
As there were no data available from a pilot study nor information in the literature on effect sizes, we conducted a sensitivity power analysis to calculate the effect size that could be detected within the COVID‐19 sample (N = 173). For full details on the sensitivity power analysis, see https://osf.io/83evy/?view_only=8cd6772e331c4b2595158186f70bdaf7. For the sensitivity power analysis, the following packages were used: future.apply (Bengtsson, 2020), r2glmm (Jaeger, 2017) and nlme (Pinheiro, Bates, DebRoy, & Sarkar, 2020).
For the hypotheses regarding the increase in irritability, stress, and loneliness, the results show that the standard linear mixed models are sufficiently powered (>.99). For the hypotheses regarding relationship quality and irritability, stress, and loneliness at T0, the results show that the standard linear mixed models are sufficiently powered (□.88) in the case of partial R 2 > .02. For the hypotheses relationship quality and irritability, stress, and loneliness at T1, the results show that the standard linear mixed models have sufficient power (□.82) in the case of an effect size of partial R 2 > .03. For the moderation hypotheses regarding the change in irritability, stress, and loneliness from T0 to T1 and how this is associated with parent–child relationship quality, the standard linear mixed models perform with sufficient power (≥ .80) in the case of partial R 2 > .06. For the hypotheses regarding the experience of family conflict, the results show that the binary logistic regression is underpowered (0.07–0.77). For the hypotheses regarding the burden of family conflict, power could not be calculated because of convergence issues arising due to the small sample size.
Relationship quality and irritability, stress, and loneliness
To estimate the change in levels of irritability, stress, and loneliness in daily life from Wave I to Wave COVID‐19, a standard linear mixed model was performed on each outcome variable (irritability, stress, and loneliness), allowing for varying intercepts. The timepoint (0 = ‘Wave I’, 1 = ‘Wave COVID‐19’) was set as the predictor, while age and sex were included as covariates in separate models for each outcome variable. Of the N = 173 participants, N = 110 had ESM data during Wave I and Wave COVID‐19 and were therefore included in these three standard linear mixed models.
The associations between the relationship quality (paternal and maternal) and the levels of irritability, stress, and loneliness at Wave I were estimated with standard linear mixed models with the levels of irritability, stress, and loneliness at Wave I all set as a separate outcome variable, allowing for varying intercepts. Paternal and maternal relationship qualities were both simultaneously set as the predictor variables in each of the three standard linear mixed models, while age and sex were included as covariates. N = 151 participants had both relationship quality and ESM data during Wave I, and were therefore included in this analysis.
The same analyses with relationship quality (paternal and maternal) as predictors simultaneously in each model were conducted for Wave COVID‐19 data for each of the three outcome variables (irritability at Wave COVID‐19; stress at Wave COVID‐19; and loneliness at Wave COVID‐19). Age and sex were included as covariates in all three standard linear mixed models, and intercepts were allowed to vary. For these three standard linear mixed models, N = 88 participants were included because they had relationship quality data at Wave I and ESM data during Wave COVID‐19.
The moderation of relationship quality (paternal and maternal) in the change in irritability, stress, and loneliness from Wave I to Wave COVID‐19 was estimated with three standard linear mixed models with the levels of irritability, stress, and loneliness all set as the outcome in separate models. The timepoint (0 = ‘Wave I’, 1 = ‘Wave COVID‐19’), paternal and maternal relationship qualities and the interaction terms (timepoint × paternal relationship quality; timepoint × maternal relationship quality) were entered simultaneously as the predictor variables with random intercepts for persons. In all three models, we included age and sex as covariates. For these moderation analyses, N = 88 participants were included. For these ESM‐based analyses, the following packages were used: r2glmm (Jaeger, 2017), readxl (Wickham & Bryan, 2019), mice (van Buuren & Groothuis‐Oudshoorn, 2011), mitml (Grund, Robitzsch, & Luedtke, 2019), and nlme (Pinheiro et al., 2020). For more details on how the models are expressed, see the postregistration: https://osf.io/83evy/?view_only=8cd6772e331c4b2595158186f70bdaf7.
Relationship quality and family conflict
To investigate the association between relationship quality (paternal and maternal) and the experience of family conflict, a binary logistic regression with the presence/absence of family conflict (0 = ‘Absence of family conflict’, 1 = ‘Presence of family conflict’) was performed for each outcome variable (parental conflict; parent–child; and sibling). Paternal and maternal relationship qualities were both set simultaneously as the predictor variables in each of the three models. In all three binary logistic regressions, N = 151 adolescents were included, and age and sex were included as covariates.
Finally, an ordinal logistic regression with the burden of family conflict (0 = ‘No burden at all’, 1 = ‘Hardly burdensome’, 2 = ‘Somewhat burdensome’, 3 = ‘Quite burdensome’, and 4 = ‘Very burdensome’) was performed for each outcome variable (parental conflict burden; parent–child conflict burden; and sibling conflict burden) to investigate the association between relationship quality (paternal and maternal) and the burden of each type of family conflict. Paternal and maternal relationship qualities were both set as the predictor variables simultaneously in each of the three models. In all three ordinal logistic regressions, N = 151 adolescents were included, and age and sex were included as covariates. Analyses from these six models were carried out in R Studio (RStudio Team, 2020) with R version 4.0.3 (R Core Team, 2020) using the following packages: r2glmm (Jaeger, 2017), readxl (Wickham & Bryan, 2019), mice (van Buuren & Groothuis‐Oudshoorn, 2011), mitools (Lumley, 2019), ordinal (Christensen, 2019), and miceadds (Robitzsch & Grund, 2021). For more details on how the models are expressed, see the postregistration: https://osf.io/83evy/?view_only=8cd6772e331c4b2595158186f70bdaf7.
RESULTS
Descriptive statistics for demographics, family conflict, relationship quality, and ESM variables in Wave I and Wave COVID‐19 are provided in Table 1.
Table 1.
Descriptives of Wave I and Wave COVID‐19 (N = 173)
| Variables | Wave I | Wave COVID‐19 | ||||||
|---|---|---|---|---|---|---|---|---|
| Available n | M (SD) | Mdn | Range | Available n | M (SD) | Mdn | Range | |
| Demographics | ||||||||
| Age (years) | 173 | 14.2 (1.8) | 14 | 11 to 18 | 173 | 16.0 (1.9) | 16 | 13–20 |
| Sex, % Females | 173 | 89 | 173 | 89 | ||||
| Number of completed beeps | 110 | 32.3 (13.7) | 33 | 0 to 59 | 110 | 27.5 (16.2) | 27 | 1–59 |
| ESM | ||||||||
| Irritability | 168 | 2.4 (1.9) | 1 | 1 to 7 | 110 | 2.1 (1.6) | 1 | 1–7 |
| Stress | 168 | 2.5 (1.9) | 2 | 1 to 7 | 110 | 2.5 (1.8) | 2 | 1–7 |
| Loneliness | 168 | 1.6 (1.3) | 1 | 1 to 7 | 110 | 1.8 (1.4) | 1 | 1–7 |
| Family conflict | ||||||||
| Parental | ||||||||
| Experience, % Yes | 171 | 36.8 | ||||||
| Burden | 63 | 3.3 (1.1) | 3 | 1–5 | ||||
| Parent–child | ||||||||
| Experience, % Yes | 171 | 61.4 | ||||||
| Burden | 105 | 3.2 (0.9) | 3 | 2–5 | ||||
| Sibling | ||||||||
| Experience, % Yes | 171 | 57.9 | ||||||
| Burden | 99 | 3 (1.1) | 3 | 1–5 | ||||
| Relationship quality | ||||||||
| Paternal | 147 | 6.8 (7.6) | 7 | −18 to 19 | ||||
| Maternal | 145 | 9.9 (6.5) | 12 | −14 to 18 | ||||
Relationship Quality and Irritability, Stress, and Loneliness
Results for irritability, stress, and loneliness in daily life in Wave I compared to Wave COVID‐19 are presented in Table 2. Analyses revealed a significant decrease in daily‐life irritability scores, and a significant increase in daily‐life loneliness scores from Wave I to Wave COVID‐19. Results showed no significant change in daily‐life stress scores from Wave I to Wave COVID‐19.
Table 2.
Standard Linear Mixed Model, Predicting the Change in Irritability, Stress, and Loneliness From Wave I to Wave COVID‐19
| Timepoint | Age | Sex | Correlation | |||||
|---|---|---|---|---|---|---|---|---|
| β (SE) | R 2 | p | β (SE) | p | β (SE) | p | r | |
| Irritability | −.31 (.08) | .01 | <.001 | .08 (.04) | .03 | .24 (.24) | .31 | .62 |
| Stress | −.16 (.09) | .001 | .07 | .17 (.04) | <.001 | .68 (.26) | .008 | .57 |
| Loneliness | .19 (.07) | .004 | .003 | .05 (.03) | .10 | .16 (.18) | .38 | .40 |
p‐values <.05 are displayed in bold; R 2 = partial R 2; Correlations reflect between pre‐ and during‐pandemic levels of irritability, stress, and loneliness.
Associations between parent–child relationship quality and the levels of irritability, stress, and loneliness are presented in Table 3. Results showed that paternal relationship quality was significantly associated with irritability at Wave I and Wave COVID‐19; lower paternal relationship quality was linked to higher daily‐life irritability. In addition, results showed that both paternal and maternal relationship qualities was significantly associated with loneliness at Wave I; lower paternal and maternal relationship qualities was linked to higher daily‐life loneliness.
Table 3.
Standard Linear Mixed Model, Predicting Levels of Irritability, Stress, and Loneliness at Wave I and Wave COVID‐19 From Low Paternal/Maternal Relationship Qualities (RQs)
| Low Paternal RQ | Low Maternal RQ | Age | Sex | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β (SE) | R 2 | p | β (SE) | R 2 | p | β (SE) | p | β (SE) | p | |
| Wave I | ||||||||||
| Irritability | −.03 (.01) | .01 | .04 | −.02 (.02) | .003 | .25 | .09 (.05) | .08 | .24 (.26) | .35 |
| Stress | −.02 (.01) | .002 | .10 | −.02 (.02) | .003 | .27 | .13 (.05) | .01 | .72 (.26) | .01 |
| Loneliness | −.02 (.01) | .01 | .03 | −.02 (.01) | .01 | .05 | .06 (.03) | .07 | .18 (.17) | .29 |
| Wave COVID‐19 | ||||||||||
| Irritability | −.03 (.02) | .02 | .03 | −.01 (.02) | .003 | .44 | −.03 (.06) | .66 | .08 (.38) | .83 |
| Stress | −.03 (.02) | .02 | .09 | −.02 (.02) | .01 | .26 | .07 (.07) | .36 | .59 (.47) | .22 |
| Loneliness | −.02 (.02) | .01 | .25 | −.03 (.02) | .02 | .07 | −.01 (.06) | .89 | .07 (.42) | .87 |
p‐values <.05 are displayed in bold; R 2 = partial R 2; parameter estimates were pooled using the Rubin’s rule (Eekhout, van de Wiel, & Heymans, 2019).
Changes in irritability, stress, and loneliness from Wave I to Wave COVID‐19 as a function of paternal and maternal relationship qualities are presented in Table 4. The interaction effect of timepoint with paternal and maternal relationship qualities was significant for loneliness; the increase in loneliness scores from Wave I to Wave COVID‐19 was greatest when paternal and maternal relationship qualities was low. Figures 1, 2, 3 visualize all associations between relationship quality (paternal and maternal) and irritability, stress, and loneliness.
Table 4.
Standard Linear Mixed Model, Predicting the Change in Levels of Irritability, Stress, and Loneliness From Wave I to Wave COVID‐19 With Low Paternal and Maternal Relationship Qualities (RQs) as Moderators
| Timepoint | Low Paternal RQ | Low Maternal RQ | Timepoint × Low paternal RQ | Timepoint × Low maternal RQ | Age | Sex | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β (SE) | R 2 | p | β (SE) | R 2 | p | β (SE) | R 2 | p | β (SE) | R 2 | p | β (SE) | R 2 | p | β (SE) | p | β (SE) | p | |
| Irritability | −.34 (.13) |
.000 |
.01 | −.03 (.01) | .01 | .01 | .03 (.01) | .004 | .07 | −.001 (.01) | .000 | .88 | .01 (.01) | .000 | .19 | .03 (.04) | .43 | .22 (.23) | .33 |
| Stress | −.13 (.24) | .000 | .54 | −.02 (.01) | .001 | .13 | −.02 (.02) | .004 | .16 | −.02 (.01) | .01 | .08 | .02 (.01) | .001 | .08 | .12 (.04) | .01 | .66 (.25) | .01 |
| Loneliness | .21 (.11) | .001 | .05 | −.02 (.01) | .01 | .04 | −.03 (.01) | .01 | .01 | −.02 (.01) | .002 | .01 | −.02 (.01) | .003 | .003 | −.003 (.03) | .92 | .14 (.17) | .42 |
p‐values <.05 are displayed in bold; R 2 = partial R 2; parameter estimates were pooled using the Rubin’s rule (Eekhout, van de Wiel, & Heymans, 2019).
Figure 1.
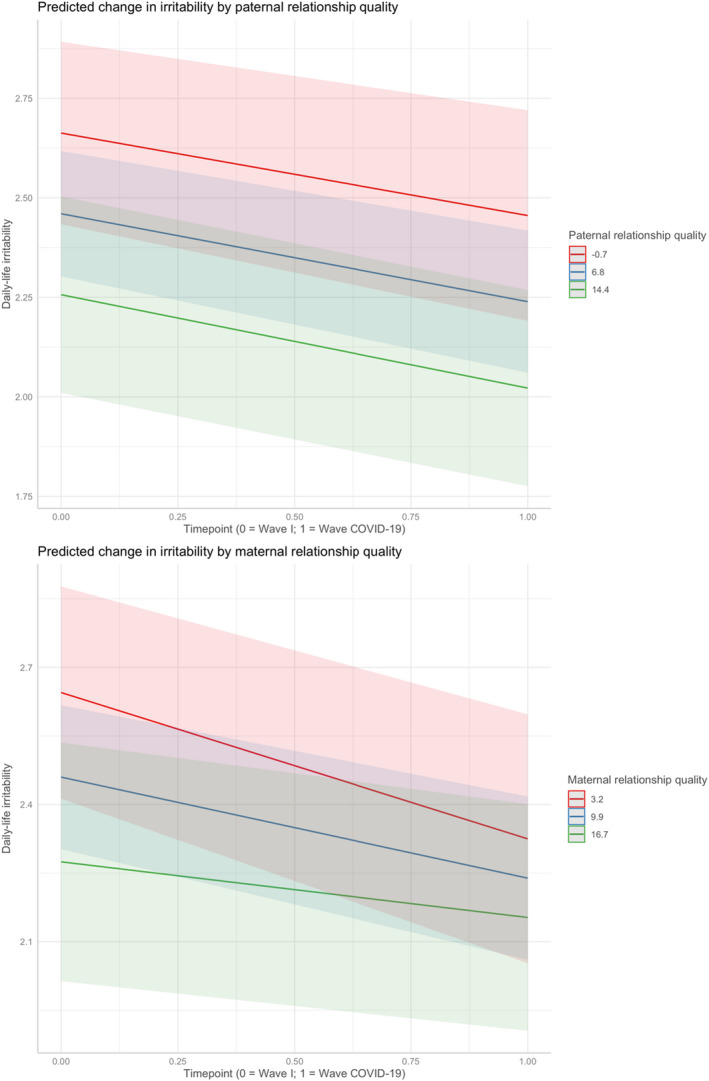
Changes in daily‐life irritability from Wave I to Wave COVID‐19 with relationship quality as a moderator.
Figure 2.
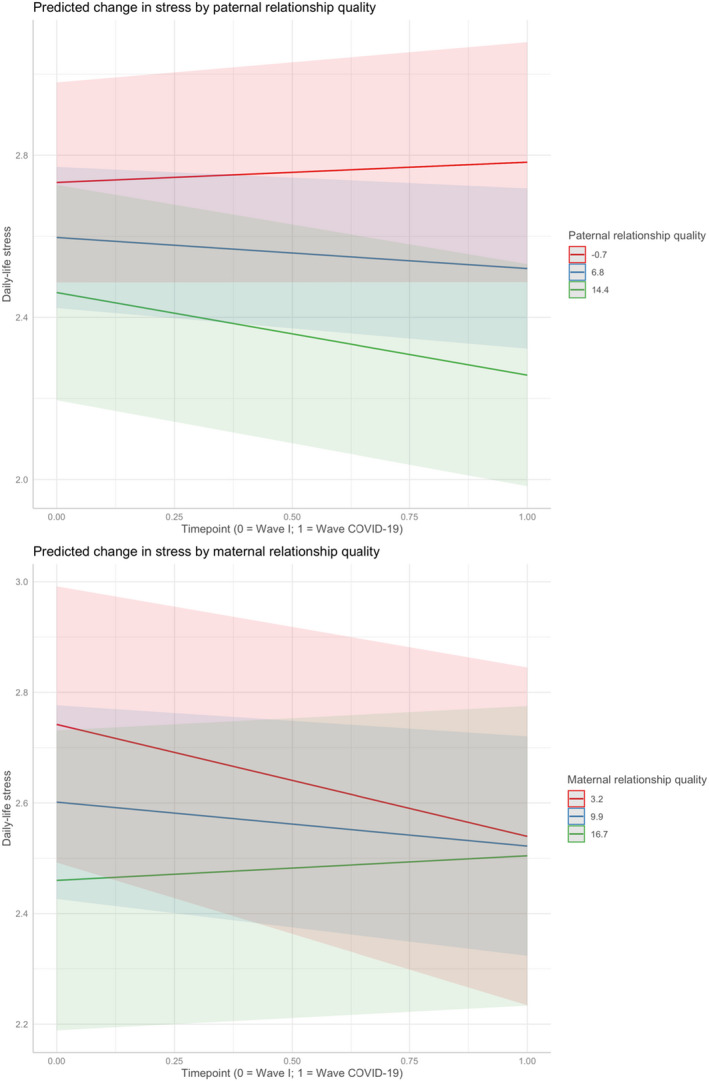
Changes in Daily‐life Stress from Wave I to Wave COVID‐19 with relationship quality as a moderator.
Figure 3.
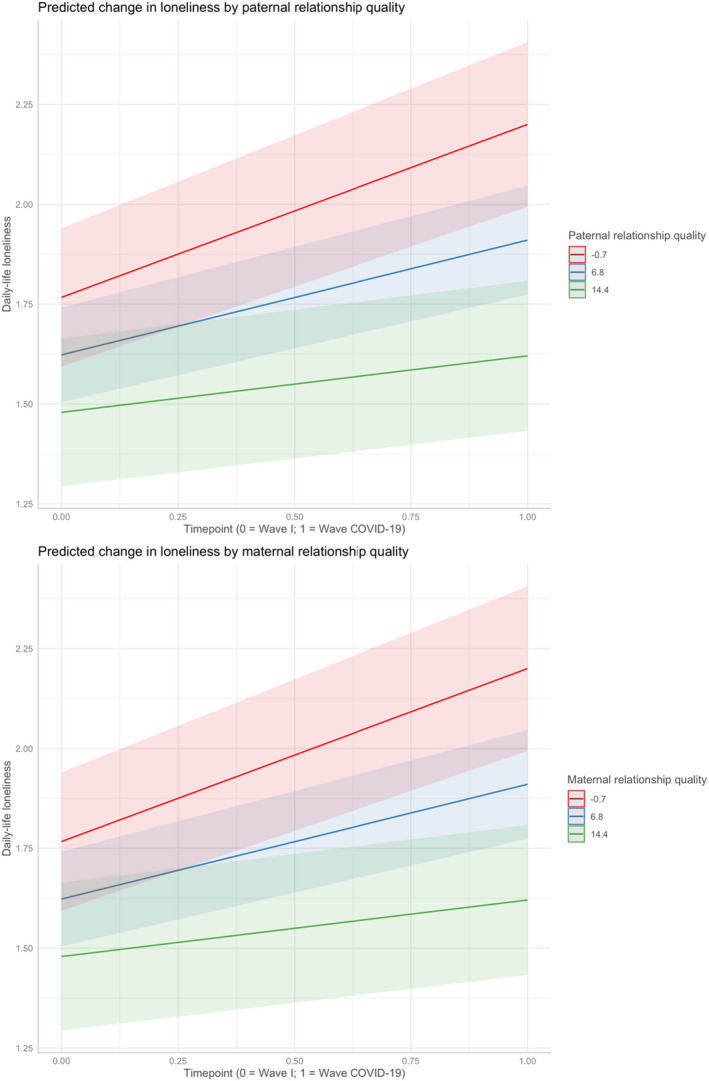
Changes in Daily‐life Loneliness from Wave I to Wave COVID‐19 with relationship quality as a moderator.
Relationship Quality and Family Conflict
Associations between paternal/maternal relationship quality and the experience and burden of family conflict are provided in Table 5. The analyses showed that the associations between paternal/maternal relationship quality and the experience of family conflict were not significant. However, results showed significant associations between relationship quality and the extent to which family conflict was experienced as a burden; lower paternal relationship quality was associated with experiencing parental and sibling conflict as more of a burden and lower maternal relationship quality was associated with adolescents experiencing parent–child conflict as more of a burden.
Table 5.
Binary and Ordinal Logistic Regression Model, Predicting Family Conflict and Its Perceived Burden From Low Paternal and Maternal Relationship Qualities (RQs; n = 151)
| Low Paternal RQ | Low Maternal RQ | Age | Sex | |||||
|---|---|---|---|---|---|---|---|---|
| β (SE) | p | β (SE) | p | β (SE) | p | β (SE) | p | |
| Parental conflict | ||||||||
| Experience a | −.02 (.03) | .46 | −.04 (.03) | .19 | −.04 (.09) | .67 | 0.19 (.53) | .72 |
| Burden b | −.07 (.04) | .04 | .01 (.04) | .89 | −.13 (.15) | .40 | 1.10 (.78) | .17 |
| Parent–child conflict | ||||||||
| Experience a | −.00 (.03) | .94 | −.01 (.03) | .85 | −.08 (.09) | .40 | 0.54 (.50) | .29 |
| Burden b | −.05 (.03) | .11 | −.07 (.03) | .03 | .13 (.11) | .22 | 0.90 (.65) | .17 |
| Sibling conflict | ||||||||
| Experience a | .03 (.02) | .19 | −.03 (.03) | .28 | −.09 (.09) | .33 | 0.69 (.51) | .18 |
| Burden b | −.11 (.03) | .00 | .02 (.04) | .53 | .02 (.11) | .88 | −0.02 (.73) | .98 |
p‐values <.05 are displayed in bold.
Logistic regression.
Ordinal logistic regression.
DISCUSSION
In line with the hypotheses, the current study found an increase in daily‐life loneliness from before to during COVID‐19. However, the results showed no change in daily‐life stress scores and a decrease in daily‐life irritability scores from before to during COVID‐19. In addition, we found that low paternal relationship quality was associated with irritability scores in daily life during Wave I and Wave COVID‐19. Both low paternal and maternal relationship qualities was associated with loneliness scores during Wave I. Results confirmed the expected buffering effect of paternal and maternal relationship qualities for loneliness. Nevertheless, while associations between relationship quality and these outcomes were statistically significant, the amount of variance explained by relationship quality was small. Given the small effect sizes, not all of our models had sufficient power to reliably detect these effects. Therefore, results should be interpreted with caution and require replication in more highly‐powered studies. Regarding the expected associations of father and mother relationship quality with experiences of COVID‐19‐related family conflict and its perceived burden, our results showed that low paternal relationship quality was positively associated with experiencing parental and sibling conflict as a burden, while low maternal relationship quality was positively associated with experiencing parent–child conflict as a burden.
Irritability, Stress, and Loneliness
The finding that adolescents reported feeling lonelier during the COVID‐19 pandemic, in comparison with before the pandemic, is in line with emerging literature and suggests that adolescents are vulnerable to the detrimental effects of the COVID‐19 pandemic and its associated physical distancing measures (Van Bavel et al., 2020; Brooks et al., 2020; Gunnell et al., 2020; Nelson, Pettitt, Flannery, & Allen, 2020). However, the effect size for the increase in loneliness was small. Coupled with our results showing no significant increase in stress and decreased irritability during COVID‐19 relative to before the pandemic, this may suggest that increases in psychological distress during the early phase of the pandemic were minimal and specific. While this may bring some relief, we must be careful not to be complacent—our results only reflect the situation in the early phase of the pandemic and the small observed increase in loneliness may have grown as the pandemic progressed. Previous research in adolescents showed that loneliness is associated with negative mental health outcomes months or even years in the future (Hawkley & Cacioppo, 2010; McClelland et al., 2020) and as many of the pandemic’s potential negative consequences are anticipated to follow later, after the initial acute phase of the pandemic (Brooks et al., 2020; Gunnell et al., 2020), continued monitoring of loneliness and other indicators of psychological distress is essential.
The lack of an increase in stress and the decrease in irritability is consistent with Achterhof, Myin‐Germeys, et al.s’ (2021) findings that indicate a decrease in anxiety symptoms in adolescents from Wave I to Wave COVID‐19, within the same sample used in the current study. This may indicate a ‘positive’ side‐effect of the national lockdown, as this eliminated two well‐known triggers for stress and irritability in adolescents, that is, school and social contact. For example, adolescent studies show that the pressure of high demands at school—much more than those at home—is a major source of stress in their lives (Modin, Östberg, Toivanen, & Sundell, 2011; Wiklund, Malmgren‐Olsson, Öhman, Bergström, & Fjellman‐Wiklund, 2012). Another study showed that adolescents’ irritability is mainly triggered in a social environment (Toohey & DiGiuseppe, 2017). Consequently, while some aspects of the pandemic might have increased stress (i.e., worrying about their own and others’ safety, as well as their education ), others might have decreased stress (i.e., not being at school and reduced social interaction), resulting in stress scores remaining stable between Wave I and Wave COVID‐19. Additionally, this finding, along with the increase in loneliness and decrease in irritability, highlights the complexity of social interactions and experiences during adolescence. During this age period, social contact is indispensable, but at the same time, these interactions are accompanied by stress and irritability in growing adolescents (Steinberg & Morris, 2001). Consequently, lockdown measures could increase loneliness in adolescents because their social needs are not being met, but on the other hand, may bring some relief due to reducing the stress and irritability that come with school and social interaction.
However, this should not be interpreted as indicating that closing schools and limiting social contact benefits adolescents by eliminating stress. In fact, both ‘stressors’ are important for adolescents’ development and the stress they elicit is adaptive for the development of social and stress‐regulating skills (Andrews et al., 2020; Steinberg & Morris, 2001). The timing of our study should also be considered when interpreting the results; it took place during the first national lockdown, and at the time, there was the prospect of relaxation in the restrictions. While adolescents who were feeling more stressed and irritable may have felt unable to participate in the COVID‐19 wave of this study, our results suggest this was not the case. Adolescents from the COVID‐19 sample did not significantly differ in terms of irritability and loneliness from adolescents in the full Wave 1 sample who did not take part in the COVID‐19 study—they even felt less stressed at Wave I in comparison with adolescents who did not participate in the COVID‐19 wave. See the OSF project page for the study for these supplementary analyses: https://osf.io/wdkxz/?view_only=661b8a0c433747e68aacfdb1d85b5ffe. Although another study found that adolescents in the COVID‐19 sample scored significantly higher on psychopathology at Wave 1 compared to participants who did not take part in the COVID‐19 study, once age and sex were taken into account, this was no longer the case (Achterhof, Myin‐Germeys, et al., 2021).
Relationship Quality and Irritability, Stress, and Loneliness
Our finding that adolescents with a lower‐quality relationship with their father reported higher levels of irritability in daily life during Wave I and Wave COVID‐19, converges with findings from previous cross‐sectional literature (Brumariu & Kerns, 2010; Shpigel et al., 2012). Given that irritability may be a precursor symptom of developing mental health problems (Brotman et al., 2017; Stringaris et al., 2018), these findings may point toward low paternal relationship quality as a vulnerability factor for psychopathology, as it may increase feelings of irritability in adolescent daily life. However, we found no significant association between maternal relationship quality and irritability.
We also found that adolescents with a lower quality relationship with their father or mother reported higher levels of loneliness during Wave I, which is consistent with previous research that suggests a negative effect of low parental relationship quality on loneliness in middle and late childhood (de Minzi, 2006). Conversely, the perception of acceptance from both parents, as well as trust in their love, protects children against loneliness (de Minzi et al., 2006).
In addition, our findings suggest a small buffering effect of high paternal and maternal relationship qualities for the increase in loneliness scores from Wave I to Wave COVID‐19. This indicates that adolescents with higher quality paternal and maternal relationships were slightly more protected against an increase in loneliness during the first national lockdown in comparison with adolescents with a lower paternal and maternal relationship qualities.
These findings may add to a growing body of literature on the association between relationship quality and emotional experiences in everyday life (Sheinbaum et al., 2015; Torquati & Raffaelli, 2004) and on the buffering effect of high‐quality relationships on the mental well‐being of adolescents (Bowlby, 1973; Shpigel et al., 2012). This increases insights into the vulnerability and protective factors for prediagnostic precursors of actual psychopathology, that is, loneliness. Moreover, these results seem to support the importance of a high‐quality relationship with parents to help adolescents weather personal adversity.
Relationship Quality and Family Conflict
Results within this sample show no significant associations between parental relationship quality and the experience of COVID‐19‐related family conflict. However, the amount of reported family conflict appeared high in this sample: 36.8% of adolescents reported parental, 61.4% parent–child and 57.9% sibling COVID‐19‐related conflict. Therefore, it is possible that the pandemic has increased the conflict in all families irrespective of relationship quality. Unfortunately, as there was no measure of family conflict at Wave 1, we could not investigate whether family conflict had increased from pre‐ to mid‐pandemic. This hypothesis should be addressed in future studies with family conflict data across multiple time points.
On the other hand, results showed significant associations between parental relationship quality and the burden of COVID‐19‐related family conflict. Low paternal relationship quality was associated with greater experienced burden of parental (between‐parents) and sibling conflict, while low maternal relationship quality was associated with higher burden of parent–child conflict. These findings converge with recent research on parenting and the experience of social interactions in the SIGMA Wave I sample (N = 1913) that showed that paternal autonomy support, which is related to higher paternal relationship quality, was linked to the experience of nonparent social interactions, that is, interactions with individuals other than their parents (Achterhof, Myin‐Germeys, et al., 2021). Additionally, maternal responsiveness, a parenting style that increases maternal relationship quality, was related to adolescents’ experiences of interacting with their parents. As a consequence, our findings fall in line with this as also in the present study the paternal relationship is associated with the experience (i.e., the burden) of nonparent interactions, namely sibling and between‐parent interactions (i.e., conflict), while the maternal relationship is associated with parent–child interactions (i.e., conflict). Our findings may be explained by the distinct but complementary caregiving roles that fathers and mothers often adopt (Kerns, Mathews, Koehn, Williams, & Siener‐Ciesla, 2015), which may influence different domains—and interactions—of adolescents’ life (Palm, 2014). Whereas mothers generally function as a safe haven (i.e., listens, comforts, and shows availability) that the child seeks in times of need, fathers are generally experienced as a play mate that functions as a secure base (i.e., sets boundaries, gives trust and supports autonomy) from which the child explores the world and engages in social relationships and interactions outside the parent–child relationship. These findings support the importance of both paternal and maternal relationship qualities for the extent to which family conflict is experienced as burdensome (Hannum & Dvorak, 2004; Shpigel et al., 2012). This highlights the relevance of improving both the quality of the paternal and maternal relationships (i.e., holistic family approaches) when family conflict occurs and is experienced as burdensome in adolescents.
Strengths and Limitations
The current study has several strengths. First, the data used within this study originate from an ongoing longitudinal cohort study with unique data from a subgroup of adolescents from before and during the COVID‐19 pandemic, which enables the delineation of pre‐existing (i.e., prepandemic) vulnerabilities for irritability, stress, loneliness, and family conflict during COVID‐19. Second, using ESM to assess daily life levels of irritability, stress, and loneliness in adolescents increases ecological validity and reduces recall bias. We did not assess family conflict in daily life, primarily in order to minimize participant burden due to an already long ESM questionnaire. While momentary assessments of family conflict may have yielded different results, research by Chung, Flook, and Fuligni (2009) suggests that episodes of family conflict are rather rare events in adolescents’ daily life, and may not be best captured by momentary assessments. Third, the study was postregistered, a form of preregistration occurring after data collection (Benning et al., 2019). All research questions, hypotheses, and analysis plans were determined and documented prior to data access, reducing the chances of data‐dependent decision‐making and as such, researcher degrees of freedom. Additionally, all analysis code has been made available on the OSF, further increasing the transparency of this research. Given that routine use of open science practices in clinical psychology and developmental psychology is still the exception rather than the rule (e.g., Tackett, Brandes, & Reardon, 2019), we feel the open science approaches used in the current study are a major strength.
Although the current study has several strengths, the findings should be interpreted within the context of its limitations. First, parent–child relationship quality was only assessed during Wave I and not during Wave COVID‐19. Although, traditionally, parent–child relationship quality is hypothesized to be a stable characteristic in children (Bowlby, 1973), more recent research on this topic challenges the stability of relationship quality (Davila & Sargent, 2003). This raises the possibility that parent–child relationship quality may have changed between Wave I and Wave COVID‐19. Therefore, it might be fruitful to assess the dynamic nature of the relationship quality over both the long term (using longitudinal studies) and the short term (using Experience Sampling or daily diaries). Additionally, the analyses involving relationship quality were somewhat underpowered, due to a moderate level of missing data for this variable at Wave I.
Second, family conflict was measured by asking participants about the presence or absence of family conflict in relation to the COVID‐19 pandemic. As a result, participants may have interpreted the question differently and assumed that questions were about conflicts about or directly related to the pandemic. This narrows our measurement of family conflict, and therefore, the level of family conflict reported may be an underestimation. Also, the items used to assess family conflict were only included in Wave COVID‐19, precluding comparison with family conflict in Wave 1. Further, the family conflict items were taken from a larger scale assessing COVID‐related stressors and internal consistency for these items was low. Future research would benefit from employing well‐validated measures of family conflict, which assess the construct more fully.
Third, although it is common in ESM research to use single items to minimize participant burden (Wright & Zimmermann, 2019), irritability, stress, and loneliness may be better captured with multiple items. Optimal items and combinations of items for assessing these constructs should be substantively investigated in future research. Fourth, the ESM compliance rates were lower in both studies (39.5% in Wave I with N = 1913 and 43.6% in Wave COVID‐19, with N = 110) than would be expected from previous ESM studies conducted with adults, in both general and clinical samples (Rintala, Wampers, Myin‐Germeys, & Viechtbauer, 2019). There may be several reasons for this, including the short time in which ESM questionnaires were available to participants (questionnaires had to be started within 90 s of the notification). The length of the questionnaire may also have played a role, as recent research by Eisele et al. (2020) in young adults demonstrated that questionnaire length negatively impacts compliance. Moreover, participants were also asked to complete ESM during school hours, and even though schools agreed to this, there may still have been barriers to completion of ESM questionnaires during lessons. We also did not incentivize compliance which may result in lower ESM compliance rates, but—in comparison with other ESM studies—we believe it enhanced our data quality. Last, nonsignificant results should be interpreted within the context of the effect sizes, as some hypotheses were not sufficiently powered to detect small effects while these may have been detected in a larger sample.
FUTURE RESEARCH
Given that the current study is limited only to the period of the first national lockdown and the COVID‐19 pandemic appears to be not only invasive but also long‐lasting, understanding how this crisis affects adolescents’ mental health and family relationships over time is important. Further insights into the impact of COVID‐19 on adolescents’ daily life outcomes and family conflict, and the specific roles of father and mother relationship quality, require well‐powered, longitudinal studies, with multimethod approaches, to investigate whether adolescent and family well‐being worsens or recovers from this global crisis, for example, large ongoing cohort studies of youth mental health, for example, SIGMA (Kirtley, Achterhof, et al., 2021; Kirtley, et al., 2020; Kirtley, Lafit, et al., 2021). ALSPAC (ALSPAC Study Team, 2001; Kwong et al., 2021) and ABCD (Karcher & Barch, 2021) can provide opportunities to look at the evolution of psychosocial distress over time.
IMPLICATIONS
Findings from the current study can provide researchers, clinicians, parents, adolescents and policy makers with insights into the impact of the COVID‐19 pandemic and its measures on adolescents’ daily life experiences and their families during the first national lockdown. Even though during this first lockdown, adolescents were not as affected as we would have expected, we caution against complacence regarding young people’s mental health and well‐being, given that the most deleterious effects of the pandemic may only emerge much later (Brooks et al., 2020; Gunnell et al., 2020). Our findings indicated a small but statistically significant contribution of both paternal and maternal relationship qualities to adolescents’ daily‐life experiences, and we emphasize the need for holistic family therapy approaches—including both fathers and mothers—to improve relationship quality in adolescents facing adversity. Before these findings are translated into practice, further replication is essential.
CONCLUSIONS
The current study provides small, but positive support for the prediction of an increase in daily‐life levels of loneliness from before to during COVID‐19 and for the role of both paternal and maternal relationship qualities as a moderator in this relationship. In addition, the current study provides no evidence for change in daily‐life stress and finds a decrease in daily‐life irritability from before to during COVID‐19. Also, an association between paternal relationship quality and irritability is demonstrated as well as an association between both paternal and maternal relationship qualities and daily‐life loneliness. No significant associations were found between parental relationship quality and the frequency of family conflict; however, findings from the study do provide evidence for a link between both paternal and maternal relationship qualities and how burdensome family conflict was experienced. The findings of this study may suggest that the impact of the pandemic on the daily lives of adolescents during the first national lockdown is not as bleak as what was expected. However, continued monitoring of young people’s well‐being and mental health is still warranted, as our results only reflect the situation during the early phase of the pandemic, which may have changed as the pandemic progressed. Future research on the link between relationship quality and adolescent’ daily life experiences and family conflict in large cohort studies is needed to see how this evolves as the pandemic progresses.
Supporting information
Appendix S1. Overview of self‐report questionnaire measures used in the full SIGMA Wave I and Wave COVID‐19 studies.
Appendix S2. Deviations from post‐registration.
Olivia J. Kirtley is supported by a Senior Postdoctoral Fellowship from Research Foundation Flanders (FWO 1257821N). Inez Myin‐Germeys is supported by a Research Foundation—Flanders Odysseus grant (FWO GOF8416N), which also includes the PhD fellowships of Julie J. Janssens, Robin Achterhof, Eva Bamps, Noëmi Hagemann, Anu P. Hiekkaranta, and Karlijn S. F. M. Hermans. Noëmi Hagemann is also supported by a doctoral grant of the Stiftung Begabtenförderung Cusanuswerk. Aleksandra Lecei is supported by the Research Foundation Flanders (FWO) (Doctoral Grant 1104219N).
Contributor Information
Julie J. Janssens, Email: julie.janssens2@kuleuven.be.
Ginette Lafit, Email: ginette.lafit@kuleuven.be.
REFERENCES
- Achterhof, R. , Kirtley, O. , Schneider, M. , Lafit, H. , Hagemann, N. , Hermans, K. , … Myin‐Germeys, I. (2021). Interrelationships between parenting styles, daily life social experiences and psychopathology in adolescence. 10.31234/osf.io/bczdg [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achterhof, R. , Myin‐Germeys, I. , Bamps, E. , Hagemann, N. , Hermans, K. S. F. M. , Hiekkaranta, A. P. , … Kirtley, O. J. (2021). Changes in daily‐life social processes and psychopathology symptoms in Flemish youth from before to during the COVID‐19 pandemic. 10.31234/osf.io/5nfp2 [DOI] [Google Scholar]
- ALSPAC Study Team (2001). ALSPAC – The Avon longitudinal study of parents and children. Paediatric and Perinatal Epidemiology, 15(1), 74–87. 10.1046/j.1365-3016.2001.00325.x [DOI] [PubMed] [Google Scholar]
- Andrews, J. L. , Ahmed, S. , & Blakemore, S. J. (2020). Navigating the social environment in adolescence: The role of social brain development. Biological Psychiatry, 89(2), 109–118. 10.1016/j.biopsych.2020.09.012 [DOI] [PubMed] [Google Scholar]
- Armsden, G. C. , & Greenberg, M. T. (1987). The inventory of parent and peer attachment: Relationships to well‐being in adolescence. Journal of Youth and Adolescence, 16, 427–454. [DOI] [PubMed] [Google Scholar]
- Azur, M. J. , Stuart, E. A. , Frangakis, C. , & Leaf, P. J. (2011). Multiple imputation by chained equations: What is it and how does it work? International Journal of Methods in Psychiatric Research, 20(1), 40–49. 10.1002/mpr.329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bavel, J. J. V. , Baicker, K. , Boggio, P. S. , Capraro, V. , Cichocka, A. , Cikara, M. , … Willer, R. (2020). Using social and behavioural science to support COVID‐19 pandemic response. Nature Human Behaviour, , 4(5), 460–471. 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- Belgische Federale Overheidsdiensten (2020, 24 maart). Coronavirus: versterkte maatregelen. Belgium.be. https://www.belgium.be/nl/nieuws/2020/coronavirus_versterkte_maatregelen
- Bengtsson, H. (2020). future.apply: Apply Function to Elements in Parallel using Futures. R package version 1.6.0. https://CRAN.R‐project.org/package=future.apply
- Benning, S. D. , Bachrach, R. L. , Smith, E. A. , Freeman, A. J. , & Wright, A. G. (2019). The registration continuum in clinical science: A guide toward transparent practices. Journal of Abnormal Psychology, 128(6), 528. 10.1037/abn0000451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore, S. J. , & Mills, K. L. (2014). Is adolescence a sensitive period for sociocultural processing? Annual Review of Psychology, 65, 187–207. 10.1146/annurev-psych-010213-115202 [DOI] [PubMed] [Google Scholar]
- Bosmans, G. , & Kerns, K. A. (2015). Attachment in middle childhood: Progress and prospects. New Directions for Child and Adolescent Development, 2015(148), 1–14. 10.1002/cad.20100 [DOI] [PubMed] [Google Scholar]
- Bowlby, J. (1973). Attachment and loss: Volume II: Separation, anxiety and anger (pp. 1–429). London, UK: The Hogarth Press and the Institute of Psycho‐Analysis. [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotman, M. A. , Kircanski, K. , & Leibenluft, E. (2017). Irritability in children and adolescents. Annual Review of Clinical Psychology, 13, 317–341. 10.1146/annurev-clinpsy-032816-044941 [DOI] [PubMed] [Google Scholar]
- Browne, D. T. , Plamondon, A. , Prime, H. , Puente‐Duran, S. , & Wade, M. (2015). Cumulative risk and developmental health: An argument for the importance of a family‐wide science. Wiley Interdisciplinary Reviews: Cognitive Science, 6(4), 397–407. 10.1002/wcs.1349 [DOI] [PubMed] [Google Scholar]
- Brumariu, L. E. , & Kerns, K. A. (2010). Parent–child attachment and internalizing symptoms in childhood and adolescence: A review of empirical findings and future directions. Development and Psychopathology, 22(1), 177–203. 10.1017/S0954579409990344 [DOI] [PubMed] [Google Scholar]
- Campbell, A. M. (2020). An increasing risk of family violence during the Covid‐19 pandemic: Strengthening community collaborations to save lives. Forensic Science International: Reports, 2, 100089. 10.1016/j.fsir.2020.100089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerutti, R. , Zuffianò, A. , & Spensieri, V. (2018). The role of difficulty in identifying and describing feelings in non‐suicidal self‐injury behavior (NSSI): Associations with perceived attachment quality, stressful life events, and suicidal ideation. Frontiers in Psychology, 9. 10.3389/fpsyg.2018.00318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen, R. H. B. (2019). ordinal – Regression Models for Ordinal Data. R package version 2019.12‐10. https://CRAN.R‐project.org/package=ordinal
- Chung, G. H. , Flook, L. , & Fuligni, A. J. (2009). Daily family conflict and emotional distress among adolescents from Latin American, Asian, and European backgrounds. Developmental Psychology, 45(5), 1406. 10.1037/a0014163 [DOI] [PubMed] [Google Scholar]
- Csikszentmihalyi, M. , & Larson, R. (1987). Validity and reliability of the Experience‐Sampling Method. The Journal of Nervous and Mental Disease, 175(9), 526–536. 10.1097/00005053-198709000-00004 [DOI] [PubMed] [Google Scholar]
- Davila, J. , & Sargent, E. (2003). The meaning of life (events) predicts changes in attachment security. Personality and Social Psychology Bulletin, 29(11), 1383–1395. 10.1177/0146167203256374 [DOI] [PubMed] [Google Scholar]
- de Minzi, M. A. (2006). Loneliness and depression in middle and late childhood: The relationship to attachment and parental styles. The Journal of Genetic Psychology, 167(2), 189–210. 10.3200/gntp.167.2.189-210 [DOI] [PubMed] [Google Scholar]
- Dimitry, L. (2012). A systematic review on the mental health of children and adolescents in areas of armed conflict in the Middle East. Child: Care, Health and Development, 38(2), 153–161. 10.1111/j.1365-2214.2011.01246.x [DOI] [PubMed] [Google Scholar]
- Eekhout, I. , van de Wiel, M. A. , & Heymans, M. W. (2017). Methods for significance testing of categorical covariates in logistic regression models after multiple imputation: power and applicability analysis. BMC Medical Research Methodology, 17(1), 129. 10.1186/s12874-017-0404-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisele, G. , Vachon, H. , Lafit, G. , Kuppens, P. , Houben, M. , Myin‐Germeys, I. , & Viechtbauer, W. (2020). The effects of sampling frequency and questionnaire length on perceived burden, compliance, and careless responding in experience sampling data in a student population. Assessment, 107319112095710. 10.1177/1073191120957102 [DOI] [PubMed] [Google Scholar]
- Ellis, W. E. , Dumas, T. M. , & Forbes, L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID‐19 crisis. Canadian Journal of Behavioural Science/Revue Canadienne des sciences du comportement, 52(3), 177. 10.1037/cbs0000215 [DOI] [Google Scholar]
- Friberg, P. , Hagquist, C. , & Osika, W. (2012). Self‐perceived psychosomatic health in Swedish children, adolescents and young adults: An internet‐based survey over time. British Medical Journal Open, 2(4), e000681. 10.1136/bmjopen-2011-000681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi, A. , Claes, L. , Bosmans, G. , Baetens, I. , Wilderjans, T. F. , Maitra, S. , … Luyckx, K. (2016). Non‐suicidal self‐injury and adolescents attachment with peers and mother: The mediating role of identity synthesis and confusion. Journal of Child and Family Studies, 25(6), 1735–1745. 10.1007/s10826-015-0350-0 [DOI] [Google Scholar]
- Gandhi, A. , Luyckx, K. , Molenberghs, G. , Baetens, I. , Goossens, L. , Maitra, S. , & Claes, L. (2019). Maternal and peer attachment, identity formation, and non‐suicidal self‐injury: A longitudinal mediation study. Child and Adolescent Psychiatry and Mental Health, 13(1), 1–11. 10.1186/s13034-019-0267-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green, K. H. , van de Groep, S. , Sweijen, S. W. , Becht, A. I. , Buijzen, M. , de Leeuw, R. N. H. , … Crone, E. A. (2021). Mood and emotional reactivity of adolescents during the COVID‐19 pandemic: Short‐term and long‐term effects and the impact of social and socioeconomic stressors. Scientific Reports, 11, 11563. 10.1038/s41598-021-90851-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grund, S. , Robitzsch, A. , & Luedtke, O. (2019). mitml: Tools for Multiple Imputation in Multilevel Modeling. R package version 0.3‐7. https://CRAN.R‐project.org/package=mitml
- Grusec, J. E. , & Davidov, M. (2021). Socializing children. Elements in child development. [Google Scholar]
- Guessoum, S. B. , Lachal, J. , Radjack, R. , Carretier, E. , Minassian, S. , Benoit, L. , & Moro, M. R. (2020). Adolescent psychiatric disorders during the COVID‐19 pandemic and lockdown. Psychiatry Research, 291, 113264. 10.1016/j.psychres.2020.113264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell, D. , Appleby, L. , Arensman, E. , Hawton, K. , John, A. , Kapur, N. , … Yip, P. S. F. (2020). Suicide risk and prevention during the COVID‐19 pandemic. The Lancet Psychiatry, 7(6), 468–471. 10.1016/S2215-0366(20)30171-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannum, J. W. , & Dvorak, D. M. (2004). Effects of family conflict, divorce, and attachment patterns on the psychological distress and social adjustment of college freshmen. Journal of College Student Development, 45(1), 27–42. 10.1353/csd.2004.0008 [DOI] [Google Scholar]
- Harris, P. A. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata‐driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasking, P. , Lewis, S. P. , Bloom, E. , Brausch, A. , Kaess, M. , & Robinson, K. (2021). Impact of the COVID‐19 pandemic on students at elevated risk of self‐injury: The importance of virtual and online resources. School Psychology International, 42(1), 57–78. 10.1177/0143034320974414 [DOI] [Google Scholar]
- Hawkley, L. C. , & Cacioppo, J. T. (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annuals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry, C. S. , Sheffield Morris, A. , & Harrist, A. W. (2015). Family resilience: Moving into the third wave. Family Relations, 64(1), 22–43. 10.1111/fare.12106 [DOI] [Google Scholar]
- Jaeger, B. (2017). r2glmm: Computes R Squared for Mixed (Multilevel) Models. R package version 0.1.2. https://CRAN.R‐project.org/package=r2glmm
- Janssen, L. H. C. , Kullberg, M.‐L. , Verkuil, B. , van Zwieten, N. , Wever, M. C. M. , van Houtum, L. A. E. M. , … Elzinga, B. M. (2020). Does the COVID‐19 pandemic impact parents’ and adolescents’ well‐being? An EMA‐study on daily affect and parenting. PLoS One, 15(10), e0240962. 10.1371/journal.pone.0240962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karcher, N. R. , & Barch, D. M. (2021). The ABCD study: Understanding the development of risk for mental and physical health outcomes. Neuropsychopharmacology, 46(1), 131–142. 10.1038/s41386-020-0736-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns, K. A. , Mathews, B. L. , Koehn, A. J. , Williams, C. T. , & Siener‐Ciesla, S. (2015). Assessing both safe haven and secure base support in parent–child relationships. Attachment & Human Development, 17(4), 337–353. 10.1080/14616734.2015.1042487 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Petukhova, M. , Sampson, N. A. , Zaslavsky, A. M. , & Wittchen, H. U. (2012). Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research, 21(3), 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirtley, O. J. , Achterhof, R. , Hagemann, N. , Hermans, K. S. F. M. , Hiekkaranta, A. P. , Lecei, A. , … Myin‐Germeys, I. (2021). Initial cohort characteristics and protocol for SIGMA: An accelerated longitudinal study of environmental factors, inter‐ and intrapersonal processes, and mental health in adolescence. 10.31234/osf.io/jp2fk [DOI] [Google Scholar]
- Kirtley, O. J. , Hiekkaranta, A. P. , Kunkels, Y. K. , Eisele, G. , Verhoeven, D. , Van Nierop, M. , & Myin‐Germeys, I. (2020). The Experience Sampling Method (ESM) Item Repository. 10.17605/OSF.IO/KG376 [DOI] [Google Scholar]
- Kirtley, O. J. , Lafit, G. , Achterhof, R. , Hiekkaranta, A. P. , & Myin‐Germeys, I. (2021). Making the black box transparent: A template and tutorial for registration of studies using experience‐sampling methods. Advances in Methods and Practices in Psychological Science, 4(1), 251524592092468. 10.1177/2515245920924686 [DOI] [Google Scholar]
- Koval, P. , Hinton, J. , Dozo, N. , Gleeson, J. , Alvarez, M. , Harrison, A. , … Sinnott, R. (2019). SEMA3: Smartphone Ecological Momentary Assessment, Version 3. [Computer software]. [Google Scholar]
- Kronenberg, M. E. , Hansel, T. C. , Brennan, A. M. , Osofsky, H. J. , Osofsky, J. D. , & Lawrason, B. (2010). Children of Katrina: Lessons learned about postdisaster symptoms and recovery patterns. Child Development, 81(4), 1241–1259. 10.1111/j.1467-8624.2010.01465.x [DOI] [PubMed] [Google Scholar]
- Kwong, A. S. F. , Pearson, R. M. , Adams, M. J. , Northstone, K. , Tilling, K. , Smith, D. , Fawns‐Ritchie, C. , Bould, H. , Warne, N. , Zammit, S. , Gunnell, D. J. , Moran, P. A. , Micali, N. , Reichenberg, A. , Hickman, M. , Rai, D. , Haworth, S. , Campbell, A. , Altschul, D. , … Timpson, N. J. (2021). Mental health before and during the COVID‐19 pandemic in two longitudinal UK population cohorts. The British Journal of Psychiatry, 218(6), 334–343. 10.1192/bjp.2020.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades, M. E. , Chatburn, E. , Higson‐Sweeney, N. , Reynolds, S. , Shafran, R. , Brigden, A. , … Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. Journal of the American Academy of Child & Adolescent Psychiatry, 59(11), 1218–1239.e3. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley, T. (2019). mitools: Tools for Multiple Imputation of Missing Data. R package version 2.4. https://CRAN.R‐project.org/package=mitools
- Magson, N. R. , Freeman, J. Y. A. , Rapee, R. M. , Richardson, C. E. , Oar, E. L. , & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID‐19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland, H. , Evans, J. J. , Nowland, R. , Ferguson, E. , & O'Connor, R. C. (2020). Loneliness as a predictor of suicidal ideation and behaviour: A systematic review and meta‐analysis of prospective studies. Journal of Affective Disorders, 274, 880–896. 10.1016/j.jad.2020.05.004 [DOI] [PubMed] [Google Scholar]
- Meers, K. , Dejonckheere, E. , Kalokerinos, E. K. , Rummens, K. , & Kuppens, P. (2020). mobileQ: A free user‐friendly application for collecting experience sampling data. Behavior Research Methods, 52(4), 1510–1515. 10.3758/s13428-019-01330-1 [DOI] [PubMed] [Google Scholar]
- Moccia, L. , Janiri, D. , Pepe, M. , Dattoli, L. , Molinaro, M. , De Martin, V. , … Di Nicola, M. (2020). Affective temperament, attachment style, and the psychological impact of the COVID‐19 outbreak: An early report on the Italian general population. Brain, Behavior, and Immunity, 87, 75–79. 10.1016/j.bbi.2020.04.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modin, B. , Östberg, V. , Toivanen, S. , & Sundell, K. (2011). Psychosocial working conditions, school sense of coherence and subjective health complaints. A multilevel analysis of ninth grade pupils in the Stockholm area. Journal of Adolescence, 34(1), 129–139. 10.1016/j.adolescence.2010.01.004 [DOI] [PubMed] [Google Scholar]
- Murphy, T. P. , Laible, D. , & Augustine, M. (2017). The influences of parent and peer attachment on bullying. Journal of Child and Family Studies, 26(5), 1388–1397. 10.1007/s10826-017-0663-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myin‐Germeys, I. , Kasanova, Z. , Vaessen, T. , Vachon, H. , Kirtley, O. , Viechtbauer, W. , & Reininghaus, U. (2018). Experience sampling methodology in mental health research: New insights and technical developments. World Psychiatry, 17(2), 123–132. 10.1002/wps.20513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, B. W. , Adam, P. , Flannery, J. E. , & Allen, N. B. (2020). Rapid assessment of psychological and epidemiological correlates of COVID‐19 concern, financial strain, and health‐related behavior change in a large online sample. PLoS One, 15(11), e0241990. 10.1371/journal.pone.0241990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noom, M. J. , Deković, M. , & Meeus, W. H. (1999). Autonomy, attachment and psychosocial adjustment during adolescence: A double‐edged sword? Journal of Adolescence, 22(6), 771–783. 10.1006/jado.1999.0269 [DOI] [PubMed] [Google Scholar]
- Orben, A. , Tomova, L. , & Blakemore, S. J. (2020). The effects of social deprivation on adolescent development and mental health. The Lancet Child & Adolescent Health, 4(8), 634–640. 10.1016/S2352-4642(20)30186-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palm, G. (2014). Attachment theory and fathers: Moving from “being there” to “being with”. Journal of Family Theory & Review, 6(4), 282–297. 10.1111/jftr.12045 [DOI] [Google Scholar]
- Panda, P. K. , Gupta, J. , Chowdhury, S. R. , Kumar, R. , Meena, A. K. , Madaan, P. , … Gulati, S. (2021). Psychological and behavioral impact of lockdown and quarantine measures for COVID‐19 pandemic on children, adolescents and caregivers: A systematic review and meta‐analysis. Journal of Tropical Pediatrics, 67(1), fmaa122. 10.1093/tropej/fmaa122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro, J. , Bates, D. , DebRoy, S. , Sarkar, D. , & R Core Team (2020). _nlme: Linear and Nonlinear Mixed Effects Models_. R package version 3.1‐149, https://CRAN.R‐project.org/package=nlme
- Prime, H. , Wade, M. , & Browne, D. T. (2020). Risk and resilience in family well‐being during the COVID‐19 pandemic. American Psychologist, 75(5), 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R‐project.org/ [Google Scholar]
- Rintala, A. , Wampers, M. , Myin‐Germeys, I. , & Viechtbauer, W. (2019). Response compliance and predictors thereof in studies using the experience sampling method. Psychological Assessment, 31(2), 226. 10.1037/pas0000662 [DOI] [PubMed] [Google Scholar]
- Robitzsch, A. , & Grund, S. (2021). miceadds: Some additional multiple imputation functions, especially for 'mice'. R package version 3.11‐6. https://CRAN.R‐project.org/package=miceadds
- Romeo, R. D. (2017). The impact of stress on the structure of the adolescent brain: Implications for adolescent mental health. Brain Research, 1654, 185–191. 10.1016/j.brainres.2016.03.021 [DOI] [PubMed] [Google Scholar]
- RStudio Team (2020). RStudio: Integrated Development for R. Boston, MA: PBC, RStudio. [Google Scholar]
- Sheinbaum, T. , Kwapil, T. R. , Ballespí, S. , Mitjavila, M. , Chun, C. A. , Silvia, P. J. , & Barrantes‐Vidal, N. (2015). Attachment style predicts affect, cognitive appraisals, and social functioning in daily life. Frontiers in Psychology, 6, 296. 10.3389/fpsyg.2015.00296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shpigel, M. S. , Diamond, G. M. , & Diamond, G. S. (2012). Changes in parenting behaviors, attachment, depressive symptoms, and suicidal ideation in attachment‐based family therapy for depressive and suicidal adolescents. Journal of Marital and Family Therapy, 38, 271–283. 10.1111/j.1752-0606.2012.00295.x [DOI] [PubMed] [Google Scholar]
- Smetana, J. G. , Robinson, J. , & Rote, W. M. (2015). Socialization in adolescence. In Grusec J. E., & Hastings P. D. (Eds.), Handbook of socialization: Theory and research (pp. 60–84). The Guilford Press. [Google Scholar]
- Solmi, M. , Radua, J. , Olivola, M. , Croce, E. , Soardo, L. , Salazar de Pablo, G. , Il Shin, J. , Kirkbride, J. B. , Jones, P. , Kim, J. H. , Kim, J. Y. , Carvalho, A. F. , Seeman, M. V. , Correll, C. U. , … Fusar‐Poli, P. (2021). Age at onset of mental disorders worldwide: large‐scale meta‐analysis of 192 epidemiological studies. Molecular Psychiatry. 10.1038/s41380-021-01161-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statbel . Structure of the Population 2020 [updated 26 May, 2020. https://statbel.fgov.be/en/themes/population/structure‐population
- Statistiek Vlaanderen . Schoolbevolking basis‐ en secundair onderwijs 2019 [updated 26 August, 2019. https://www.statistiekvlaanderen.be/nl/schoolbevolking‐basis‐en‐secundair‐onderwijs
- Steinberg, L. , & Morris, A. S. (2001). Adolescent development. Annual Review of Psychology, 52(1), 83–110. 10.1146/annurev.psych.52.1.83 [DOI] [PubMed] [Google Scholar]
- Stringaris, A. , Vidal‐Ribas, P. , Brotman, M. A. , & Leibenluft, E. (2018). Practitioner Review: Definition, recognition, and treatment challenges of irritability in young people. Journal of Child Psychology and Psychiatry, 59(7), 721–739. 10.1111/jcpp.12823 [DOI] [PubMed] [Google Scholar]
- Tackett, J. L. , Brandes, C. M. , & Reardon, K. W. (2019). Leveraging the Open Science Framework in clinical psychological assessment research. Psychological Assessment, 31(12), 1386. 10.1037/pas0000583 [DOI] [PubMed] [Google Scholar]
- Toohey, M. J. , & DiGiuseppe, R. (2017). Defining and measuring irritability: Construct clarification and differentiation. Clinical Psychology Review, 53, 93–108. 10.1016/j.cpr.2017.01.009 [DOI] [PubMed] [Google Scholar]
- Torquati, J. C. , & Raffaelli, M. (2004). Daily experiences of emotions and social contexts of securely and insecurely attached young adults. Journal of Adolescent Research, 19(6), 740–758. 10.1177/0743558403260023 [DOI] [Google Scholar]
- van Buuren, S. , & Groothuis‐Oudshoorn, K. (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. [Google Scholar]
- Van Roekel, E. , Scholte, R. H. J. , Verhagen, M. , Goossens, L. , & Engels, R. C. M. E. (2010). Loneliness in adolescence: Gene × environment interactions involving the serotonin transporter gene. Journal of Child Psychology and Psychiatry, 51(7), 747–754. 10.1111/j.1469-7610.2010.02225.x [DOI] [PubMed] [Google Scholar]
- Veer, I. M. , Riepenhausen, A. , Zerban, M. , Wackerhagen, C. , Puhlmann, L. M. C. , Engen, H. , … Kalisch, R. (2021). Psycho‐social factors associated with mental resilience in the Corona lockdown. Translational Psychiatry, 11(1), 67. 10.1038/s41398-020-01150-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, G. , Zhang, Y. , Zhao, J. , Zhang, J. , & Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID‐19 outbreak. The Lancet, 395(10228), 945–947. 10.1016/s0140-6736(20)30547-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2020). World Health Organization: WHO announces COVID‐19 outbreak a pandemic. http://www.euro.WHO.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/news/news/2020/3/who‐announces‐covid‐19‐outbreak‐a‐pandemic
- Wickham, H. , & Bryan, J. (2019). readxl: Read Excel Files. R package version 1.3.1. https://CRAN.R‐project.org/package=readxl
- Wickrama, K. A. S. , & Kaspar, V. (2007). Family context of mental health risk in Tsunami‐exposed adolescents: Findings from a pilot study in Sri Lanka. Social Science & Medicine, 64(3), 713–723. 10.1016/j.socscimed.2006.09.031 [DOI] [PubMed] [Google Scholar]
- Widnall, E. , Grant, C. E. , Wang, T. , Cross, L. , Velupillai, S. , Roberts, A. , … Downs, J. (2020). User perspectives of mood‐monitoring apps available to young people: Qualitative Content Analysis. JMIR mHealth and uHealth, 8(10), e18140. 10.2196/18140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiklund, M. , Malmgren‐Olsson, E. B. , Öhman, A. , Bergström, E. , & Fjellman‐Wiklund, A. (2012). Subjective health complaints in older adolescents are related to perceived stress, anxiety and gender – a cross‐sectional school study in Northern Sweden. BMC Public Health, 12(1). 10.1186/1471-2458-12-993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, A. G. , & Zimmermann, J. (2019). Applied ambulatory assessment: Integrating idiographic and nomothetic principles of measurement. Psychological Assessment, 31(12), 1467. 10.1037/pas0000685 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Overview of self‐report questionnaire measures used in the full SIGMA Wave I and Wave COVID‐19 studies.
Appendix S2. Deviations from post‐registration.


