DISCLOSURES
The authors declare that they have no any potential conflict of interest regarding this submitted manuscript.
AUTHOR CONTRIBUTIONS
Yadong Wang and Haiyan Yang designed the study. Jie Xu, Ying Wang, Hongjie Hou and Li Shi performed literature search and data extraction. Jie Xu and Yadong Wang performed data analysis. Yadong Wang and Haiyan Yang wrote and reviewed the manuscript. All the authors approved the final manuscript.
Tuberculosis is reported to be associated with the severity and mortality amongst patients with coronavirus disease 2019 (COVID‐19). 1 However, the reported prevalence of comorbid tuberculosis amongst COVID‐19 patients varied greatly across the published studies. For example, the low prevalence of comorbid tuberculosis amongst COVID‐19 patients was reported in Tian et al’s study (0.4%) 2 and Yan et al’s study (0.2%) 3 and the relatively high prevalence of comorbid tuberculosis amongst COVID‐19 patients was reported in Hu et al’s study (4.5%) 4 and Zhang et al’s study (9.0%). 5 Therefore, it is needed to quantitatively estimate the pooled prevalence of comorbid tuberculosis amongst COVID‐19 patients using a meta‐analysis.
A systematic literature search was conducted independently by two investigators in PubMed, Web of Science, EMBASE, Springer, Elsevier‐ScienceDirect, Wiley Online Library, Scopus and Cochrane Library databases to select all eligible studies which were published from 1 January 2020 to 31 August 2021. The following keywords were used: “prevalence” or “incidence” or “rate” or “characteristics” and “tuberculosis” and “COVID‐19” or “SARS‐CoV‐2” or “2019‐nCoV” or “severe acute respiratory syndrome coronavirus 2” or “coronavirus disease 2019” or “2019 novel coronavirus”. All peer‐reviewed papers which were published in the English language were eligibly included if they provided the incidence rate of comorbid tuberculosis amongst COVID‐19 patients. Accordingly, we excluded case reports, review articles, duplicate publications, errata, comments and preprints. Reference lists of the retrieved articles were also screened to identify additional studies. This rapid systematic review and meta‐analysis was performed following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA). 6
The pooled prevalence of comorbid tuberculosis amongst COVID‐19 patients was estimated using a random effects meta‐analysis model. 7 , 8 The statistical heterogeneity across studies was assessed by I 2 statistic and Cochrane Q test. 9 , 10 The risk of publication bias was evaluated by Begg's rank correlation test. 11 , 12 All statistical analyses were carried out using the package “meta” on R version 3.6.3 (R Foundation for Statistical Computing). A two‐tailed P value <.05 was regarded statistically significant.
A total of 114 eligible studies 2 , 3 , 4 , 5 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 with 405 596 COVID‐19 patients were included in this meta‐analysis. Amongst the included studies, 77 studies 2 , 3 , 4 , 5 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 were reported in Asia, 15 studies 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 were conducted in Africa, nine studies 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 were conducted in South America, five studies 110 , 111 , 112 , 113 , 114 were performed in North America, seven studies 115 , 116 , 117 , 118 , 119 , 120 , 121 were conducted in Europe and one study 122 was from multicountries. The baseline characteristics of the included studies are summarised in Table 1. Overall, our findings demonstrated that the prevalence of comorbid tuberculosis amongst COVID‐19 patients in this pooled meta‐analysis was 1.6% with 95% confidence interval (CI): 1.3%–1.9% (Figure 1). The regional tuberculosis prevalence in COVID‐19 patients was estimated as follows: Africa (4.1%, 95% CI: 0.0%–5.8%), Asia (1.1%, 95% CI: 0.9%–1.3%), South America (0.5%, 95% CI: 0.0%–1.0%), Europe (0.4%, 95% CI: 0.0%–0.6%) and North America (0.2%, 95% CI: 0.0%–0.4%), which revealed great variability in the prevalence of comorbid tuberculosis amongst COVID‐19 patients in different regions. Begg's test revealed that there was potential publication bias (P = .0017).
TABLE 1.
General information of eligible studies included in this meta‐analysis
| Author | Country | Study design | Male (%) | Age a | Sample size | TB (%) |
|---|---|---|---|---|---|---|
| Hung IF | China | Randomised controlled trial | 53.5 | 48.27 | 127 | 2 (1.6%) |
| Pande D | India | NR | 48.1 | 50 | 27 | 1 (3.7%) |
| Du RH | China | NR | 54.2 | 57.6 ± 13.7 | 179 | 8 (4.5%) |
| Hu Y | China | Retrospective study | 47.1 | 53 (42‐62) | 308 | 14 (4.5%) |
| Mo P | China | Retrospective study | 55.5 | 54 (42‐66) | 155 | 3 (1.9%) |
| Zeng JH | China | Retrospective study | 47.6 | 46.58 | 416 | 8 (1.9%) |
| Sy KTL | Philippines | Cohort study | NR | NR | 12 513 | 113 (0.9%) |
| Joeng HE | Korea | Cohort study | 41.1 | 48.5 | 1824 | 7 (0.4%) |
| He G | China | Case series | NR | NR | 139 | 3 (2.2%) |
| Li X | China | Ambispective study | 50.9 | 60 (48‐69) | 548 | 9 (1.6%) |
| Durrani M | Pakistan | Retrospective study | 80 | 44 | 30 | 1 (3.3%) |
| Pachiega J | Brazil | NR | NR | NR | 14 737 | 4 (0.03%) |
| Souza CDF | Brazil | Observational study | 46.7 | NR | 197 | 1 (0.5%) |
| Panthee B | Nepal | NR | 72.1 | 49.7 ± 19.2 | 79 | 5 (10.4%) |
| Chen T | China | Case series | 53.2 | 54 (20‐91) | 203 | 4 (2.0%) |
| Zhang JJ | China | Retrospective study | 50.7 | 57 (25‐87) | 140 | 2 (1.4%) |
| Lee C | Korea | Retrospective study | 50 | 52.0 (37.5‐55.5) | 10 | 0 (0%) |
| Asghar MS | Pakistan | Retrospective study | 69 | 52.58 ± 15.68 | 100 | 1 (1%) |
| Pierrotti LC | Brazil | Retrospective study | 49 | 51.9 (17‐78) | 51 | 2 (3.9%) |
| Song J | China | Retrospective study | 52 | 63 (49‐70) | 961 | 20 (2.1%) |
| Borba MGS | Brazil | Randomised controlled trial | NR | NR | 55 | 2 (3.6%) |
| Lee JY | Korea | Retrospective study | 30.5 | 55.91 | 694 | 2 (0.3%) |
| Miciel EL | Brazil | Cross‐sectional study | NR | NR | 416 | 1 (0.2%) |
| Tian J | China | Retrospective study | 48.1 | 48.49 ± 14.36 | 721 | 3 (0.4%) |
| Kamal AF | Indonesia | Ambispective study | 42.9 | 32.89 ± 17.42 | 35 | 2 (5.7%) |
| Hong D | China | Retrospective study | 54.2 | 46.7 ± 17.7 | 168 | 8 (4.8%) |
| JeroniMo CMP | Brazil | Randomised controlled trial | NR | NR | 362 | 8 (2.2%) |
| Yan N | China | Retrospective study | 48.9 | 50 (39‐58) | 1682 | 3 (0.2%) |
| Panda S | India | Prospective study | 70.7 | 34.96 ± 13.4 | 225 | 1 (0.4%) |
| Wu Q | China | Retrospective study | 47.8 | 48.78 | 492 | 4 (0.8%) |
| Zhang J | China | Retrospective study | 48.3 | 60.0 (49.0‐69.0) | 901 | 13 (1.4%) |
| Liu J | China | Retrospective study | 53.4 | 57 (47‐67) | 1190 | 15 (1.3%) |
| Yu HH | China | Retrospective study | 50 | 62 (50‐70) | 1561 | 20 (1.3%) |
| Boulle A | South Africa | Cohort study | 31.6 | NR | 22 308 | 2128 (9.5%) |
| Yang C | China | Retrospective study | 61.5 | 44 (33‐55) | 104 | 2 (1.9%) |
| Barry M | Saudi Arabia | Case series | NR | NR | 99 | 10 (10.1%) |
| Nachega JB | Congo | Cohort study | 65.6 | 46 (34‐58) | 766 | 19 (2.5%) |
| AI Kuwari HM | Qatar | Case series | 88.9 | 35.8 ± 1.2 | 5685 | 13 (0.2%) |
| Ibrahim OR | Nigeria | Retrospective study | 86.7 | 43 ± 16.0 | 45 | 2 (4.4%) |
| Gupta N | India | Retrospective study | NR | NR | 1073 | 22 (2.1%) |
| Agarwal N | India | Observational study | 83.2 | 47.6 ± 15.9 | 95 | 2 (2.1%) |
| Dai M | China | Retrospective study | 59 | 51 ± 13 | 73 | 3 (4%) |
| Jin M | China | Retrospective study | 33.9 | 57.52 ± 14.71 | 121 | 1 (0.8%) |
| Zhang X | China | NR | 56.4 | 46.5 | 78 | 7 (9.0%) |
| Parker A | South Africa | Observational study | 38.9 | 48.5 | 113 | 13 (11.5%) |
| Luo Y | China | Retrospective study | 52.6 | 62 | 78 | 2 (2.56%) |
| Zhu J | China | Retrospective study | 54 | 45.04 ± 46.50 | 50 | 3 (6%) |
| Tahtasakal CA | Turkey | Retrospective study | 56.4 | 59 (19‐97) | 534 | 2 (0.4%) |
| Dev N | India | Retrospective study | 58 | 36 ± 13 | 55 | 0 (0%) |
| Li S | China | Retrospective study | 50.6 | 61.9 (49.7‐69.5) | 2924 | 52 (1.8%) |
| Sun C | China | Retrospective study | 46 | 45 (31‐56) | 129 | 1 (0.8%) |
| Feehan AK | USA | Cross‐sectional study | NR | NR | 311 | 0 (0%) |
| Porto LC | Brazil | Retrospective study | NR | 40.5 (34‐49) | 410 | 0 (0%) |
| Wang W | China | Retrospective study | 61.2 | 44 (33‐50) | 147 | 3 (2.1%) |
| Thiabaud A | Switzerland | Retrospective study | 59.5 | 68 (54‐79) | 3645 | 22 (0.9%) |
| Jeyaraman P | India | Retrospective study | 69.7 | 60 (18‐80) | 33 | 1 (3.0%) |
| Li C | China | Randomised controlled trial | 46.8 | 54.0 (39.8‐63.3) | 94 | 3 (3.2%) |
| Anaya JM | Colombia | Retrospective study | 70.8 | 57.5 (51.8‐66.3) | 120 | 0 (0%) |
| Yan B | China | Retrospective study | 53.7 | 59.5 (14‐86) | 190 | 1 (0.5%) |
| Patler C | USA | Cross‐sectional Study | 91.9 | 37.4 (18.6‐68.9) | 529 | 19 (3.6%) |
| Zheng B | China | Retrospective study | 40.4 | 49.5 | 198 | 1 (0.5%) |
| Fisman DN | Canada | Cohort study | 43 | 55 | 21 922 | 52 (0.2%) |
| Lee SG | Korea | Retrospective study | 40.1 | 47.1 ± 19.0 | 7339 | 28 (0.4%) |
| Lu Y | China | Retrospective study | 65 | 59 (54‐63) | 77 | 1 (1.3%) |
| Bepouka BI | Congo | Retrospective study | 67.4 | 49.6 ± 16.5 | 141 | 1 (0.7%) |
| Zhou S | China | Retrospective study | 56 | 56.0 (45.3‐64.8) | 62 | 0 (0%) |
| Yitao Z | China | Retrospective study | 54 | 46 ± 17 | 257 | 3 (1.2%) |
| Li G | Multi‐country | NR | 54 | 66 (58‐74) | 399 | 6 (1.5%) |
| Zhang W | China | Retrospective study | 53.6 | 40.6 | 500 | 3 (0.6%) |
| Abraha HE | Ethiopia | Retrospective study | 63.3 | 29 (24‐38) | 2617 | 8 (0.3%) |
| Kumar S | India | Retrospective study | 87.1 | 64.5 (53.7‐70) | 31 | 0 (0%) |
| Sun J | China | Prospective clinical trial | 61.29 | 60.39 ± 10.20 | 31 | 1 (3.23%) |
| Hafiz M | Indonesia | Case series | 62.8 | 55.9 ± 15.7 | 42 | 5 (11.9%) |
| Riou C | South Africa | Cohort study | 57.9 | 52 (43‐57) | 95 | 15 (15.8) |
| Meng M | China | Retrospective study | 58.8 | 62.63 ± 13.49 | 415 | 8 (1.9%) |
| RECOVERY Collaborative Group | UK | Randomised controlled trial | 64.3 | 63.5 | 11 558 | 46 (0.4%) |
| African COVID‐19 Critical Care Outcomes Study (ACCCOS) Investigators | Ten African countries | Prospective study | 60.6 | 56 ± 16.11 | 3140 | 51 (1.7%) |
| Sahin B | Turkey | Prospective study | 55.2 | 63.2 ± 13.8 | 58 | 10 (18.2%) |
| Marimuthu Y | India | Longitudinal study | 56.6 | 45.3 ± 17.2 | 854 | 10 (1.2%) |
| Venturas J | South Africa | Retrospective study | 53 | 50 (39‐60) | 384 | 14 (4%) |
| Tsuchihashi Y | Japan | Retrospective study | 55 | 60 | 516 | 1 (0.3%) |
| Kridin K | Israel | Case–control study | 47.4 | 46.0 ± 19.3 | 6151 | 9 (0.29%) |
| Chanda D | Zambia | Retrospective study | 57.3 | 48.2 | 443 | 21 (4.74%) |
| Xu J | China | Retrospective study | 45.9 | 46.5 (34.3‐62.0) | 98 | 2 (2%) |
| Zhang Q | China | Retrospective study | 51.6 | 51.49 ± 17.39 | 157 | 1 (0.6%) |
| Dilogo IH | Indonesia | Randomised controlled trial | 75 | NR | 40 | 2 (5%) |
| Pakdel F | Iran | Cross‐sectional study | 66 | 52 | 15 | 1 (6.7%) |
| Agrupis KA | Philippines | Retrospective study | 55.8 | 48 ± 17 | 500 | 41 (8.2%) |
| Prasetya IB | Indonesia | Retrospective study | 62 | 43 (32‐54) | 391 | 4 (1.2%) |
| Dave JA | South Africa | Retrospective study | 38.3 | 40.0 (30.0‐52.0) | 64 476 | 4736 (7.3%) |
| Zhou K | China | Retrospective study | 53.5 | 47 | 144 | 4 (2.8%) |
| Meenakumari R | India | Retrospective study | 76.9 | 39.53 ± 13.4 | 204 | 1 (0.5%) |
| Sharif N | Bangladesh | Retrospective study | 65.8 | 39.8 ± 12.6 | 966 | 9 (0.9%) |
| Giubelan LI | Romania | Retrospective study | NR | NR | 100 | 1 (1%) |
| Ali MR | Bangladesh | Cross‐sectional study | 60.12 | 35 ± 14.90 | 326 | 27 (8.28%) |
| Kumar G | India | Prospective study | 64.8 | 50 | 18 961 | 138 (0.7%) |
| Aggarwal R | India | Retrospective study | 65.9 | 56 (41.5‐65) | 247 | 21 (8.5%) |
| Kirenga B | Uganda | Randomised clinical trial | 71.3 | 50 (38.5‐62.0) | 136 | 4 (2.9%) |
| Sang L | China | Retrospective study | 67.4 | 62.7 ± 13.3 | 190 | 1 (0.5%) |
| Bakamutumaho B | Uganda | Prospective study | NR | NR | 11 | 0 (0%) |
| Suryananda TD | Indonesia | Prospective study | 61.3 | 48.04 ± 11.66 | 75 | 5 (6.7%) |
| Fleitas PE | Argentina | Cross‐sectional study | 49.7 | 37 (26‐51) | 7968 | 84 (1.1%) |
| Ren P | China | Retrospective study | 62.3 | 57 (48‐66) | 80 | 1 (1.25%) |
| Badr OI | Saudi Arabia | Retrospective study | 69.8 | 52.8 | 159 | 2 (1.26%) |
| Lee SW | Korea | Cohort study | 37.3 | NR | 3882 | 51 (1.31%) |
| Maximiano Sousa F | Switzerland | Prospective study | 59.5 | 68 (55‐80) | 3590 | 21 (0.58%) |
| Sandoval M | USA | Retrospective study | 38 | 24 (21‐27) | 1853 | 1 (0.05%) |
| Munblit D | Russia | Cohort study | 48.9 | 56 (46‐66) | 2649 | 2 (0.08%) |
| Jassat W | South Africa | Cohort study | 45.5 | NR | 151 779 | 5173 (3.41%) |
| Bushman D | USA | Case–control study | 65.5 | 56 (23‐64) | 1029 | 1 (0.1%) |
| Wang J | China | Retrospective study | 59.2 | 57.0 (43.0‐66.0) | 436 | 6 (1.38%) |
| Wolday D | Ethiopia | Prospective study | 63.9 | 37 (28‐50) | 751 | 1 (0.13%) |
| El‐Battrawy I | Italy‐Spain‐Germany | NR | 58.6 | NR | 5810 | 15 (0.26%) |
| Arenas Jimenez MD | Spain | Retrospective study | 70.8 | 72.4 ± 12.6 | 288 | 5 (1.7%) |
Abbreviations: NR, Not clearly reported; TB, tuberculosis; UK, United Kingdom; USA, the United States of America.
Indicates age (years) was presented as mean ± standard deviation (SD) or median (interquartile range, IQR).
FIGURE 1.
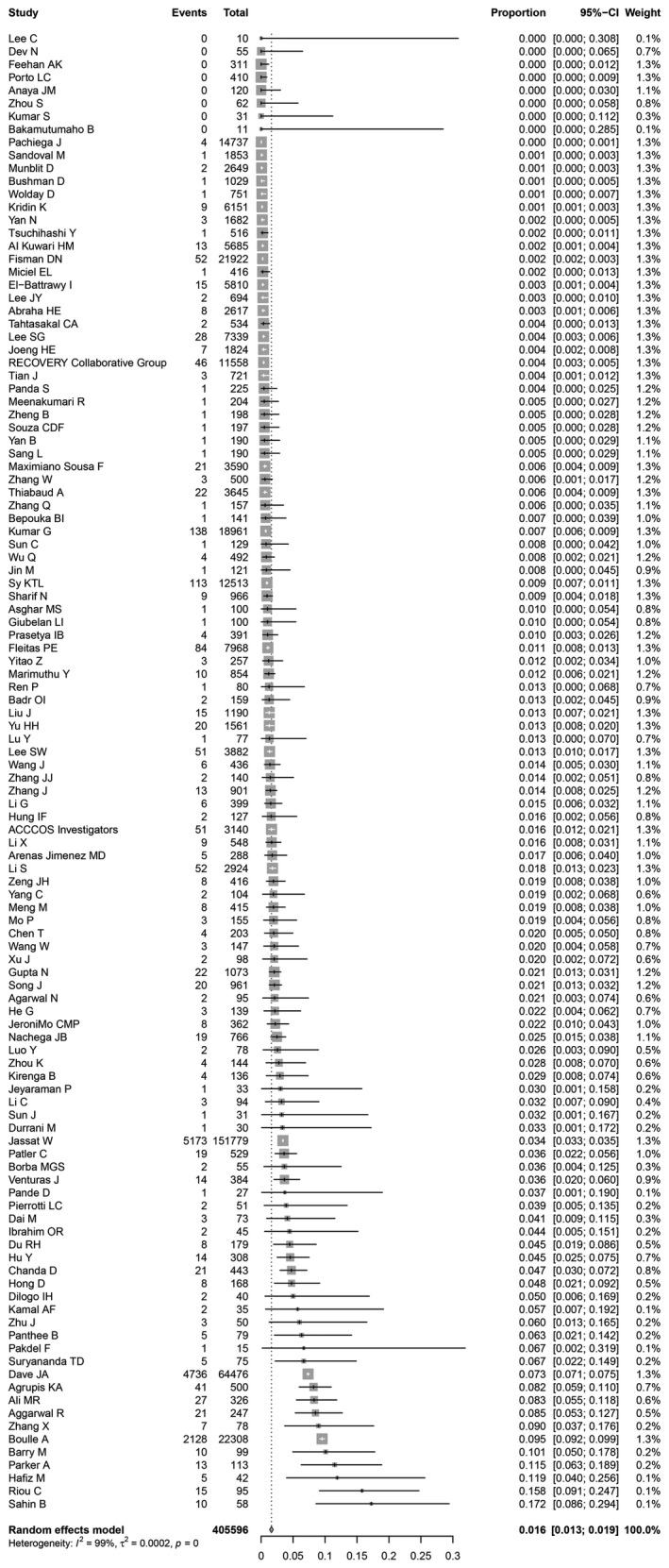
The forest plot demonstrating the prevalence of comorbid tuberculosis amongst coronavirus disease 2019 (COVID‐19) patients on the basis of 114 studies with 405 596 cases
In conclusion, our findings demonstrated that the prevalence of comorbid tuberculosis amongst COVID‐19 patients was 1.6%, which varied greatly in different regions.
ACKNOWLEDGEMENTS
We would like to thank Wenwei Xiao, Xuan Liang, Peihua Zhang, Yang Li and Jian Wu (All are from Department of Epidemiology, School of Public Health, Zhengzhou University) for their kind help in searching articles and collecting data.
Funding information
This study was supported by grants from Joint Construction Project of Henan Medical Science and Technology Research Plan (grant number LHGJ20190679), National Natural Science Foundation of China (grant number 81973105) and Key Scientific Research Project of Henan Institution of Higher Education (grant number 21A330008). The funders have no role in the data collection, data analysis, preparation of manuscript and decision to submission.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable request.
REFERENCES
- 1. Wang Y, Feng R, Xu J, Hou H, Feng H, Yang H. An updated meta‐analysis on the association between tuberculosis and COVID‐19 severity and mortality. J Med Virol. 2021;93(10):5682‐5686. doi: 10.1002/jmv.27119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tian J, Yan S, Wang H, et al. Hanshiyi formula, a medicine for Sars‐CoV2 infection in China, reduced the proportion of mild and moderate COVID‐19 patients turning to severe status: a cohort study. Pharmacol Res. 2020;161:105127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID‐19 pneumonia caused by SARS‐CoV‐2: a prospective cohort study. Eur Res J. 2020;55(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hu Y, Wang T, Hu Z, et al. Clinical efficacy of glucocorticoid on the treatment of patients with COVID‐19 pneumonia: a single‐center experience. Biomed Pharmacother. 2020;130:110529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory COVID‐19 pneumonia in Wuhan, China. Clin Infect Dis. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Balduzzi S, Rucker G, Schwarzer G. How to perform a meta‐analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shi LI, Xu J, Xiao W, et al. Asthma in patients with coronavirus disease 2019: a systematic review and meta‐analysis. Ann Allergy, Asthma Immunol. 2021;126(5):524‐534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327(7414):557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. DerSimonian R, Laird N. Meta‐analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088‐1101. [PubMed] [Google Scholar]
- 12. Wang Y, Shi L, Yang H, Duan G, Wang Y. Pooled prevalence of deep vein thrombosis among coronavirus disease 2019 patients. Crit Care. 2020;24(1):466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Agarwal N, Biswas B, Lohani P. Epidemiological determinants of COVID‐19 infection and mortality: a study among patients presenting with severe acute respiratory illness during the pandemic in Bihar, India. Niger Postgrad Med J. 2020;27(4):293‐301. [DOI] [PubMed] [Google Scholar]
- 14. Kumar R, Malhotra R, Guleria R, et al. Clinicoepidemiological features and mortality analysis of deceased patients with COVID‐19 in a tertiary care center. Indian J Crit Care Med. 2021;25(6):622‐628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Agrupis KA, Smith C, Suzuki S, et al. Epidemiological and clinical characteristics of the first 500 confirmed COVID‐19 inpatients in a tertiary infectious disease referral hospital in Manila, Philippines. Trop Med Health. 2021;49(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Al Kuwari HM, Abdul Rahim HF, Abu‐Raddad LJ, et al. Epidemiological investigation of the first 5685 cases of SARS‐CoV‐2 infection in Qatar, 28 February‐18 April 2020. BMJ Open. 2020;10(10):e040428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ali MR, Hasan MA, Rahman MS, et al. Clinical manifestations and socio‐demographic status of COVID‐19 patients during the second‐wave of pandemic: a Bangladeshi experience. J Infect Public Health. 2021; 10.1016/j.jiph.2021.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Asghar MS, Haider Kazmi SJ, Ahmed Khan N, et al. Clinical profiles, characteristics, and outcomes of the first 100 admitted COVID‐19 patients in Pakistan: a single‐center retrospective study in a tertiary care hospital of Karachi. Cureus. 2020;12(6):e8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Badr OI, Alwafi H, Elrefaey WA, et al. Incidence and outcomes of pulmonary embolism among hospitalized COVID‐19 patients. Int J Environ Res Public Health. 2021;18(14):7645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barry M, AlMohaya A, AlHijji A, et al. Clinical characteristics and outcome of hospitalized COVID‐19 patients in a MERS‐CoV endemic area. J Epidemiol Glob Health. 2020;10(3):214‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen TieLong, Dai Z, Mo P, et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID‐19) in Wuhan, China: a single‐centered, retrospective study. J Gerontol A Biol Sci Med Sci. 2020;75(9):1788‐1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dai M, Liu X, Zhu X, et al. Temporal changes of CT findings between non‐severe and severe cases of COVID‐19 pneumonia: a multi‐center, retrospective, longitudinal Study. Int J Med Sci. 2020;17(17):2653‐2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dev N, Sankar J, Gupta N, et al. COVID‐19 with and without anosmia or dysgeusia: a case‐control study. J Med Virol. 2021;93(4):2499‐2504. [DOI] [PubMed] [Google Scholar]
- 24. Dilogo IH, Aditianingsih D, Sugiarto A, et al. Umbilical cord mesenchymal stromal cells as critical COVID‐19 adjuvant therapy: a randomized controlled trial. Stem Cells Transl Med. 2021;10(9):1279‐1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Durrani M, Haq IU, Kalsoom U, Yousaf A. Chest X‐rays findings in COVID 19 patients at a University Teaching Hospital ‐ A descriptive study. Pak J Med Sci. 2020;36(COVID19‐S4):S22–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gupta N, Ish P, Gupta A, et al. A profile of a retrospective cohort of 22 patients with COVID‐19 and active/treated tuberculosis. Eur Res J. 2020;56(5):2003408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hafiz M, Icksan AG, Harlivasari AD, Andarini S, Susanti F, Yuliana ME. Association between clinical, laboratory findings and chest CT in COVID‐19 in a secondary hospital in Jakarta. Indonesia. Germs. 2021;11(1):32‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. He G, Wu J, Shi J, et al. COVID‐19 in tuberculosis patients: a report of three cases. J Med Virol. 2020;92(10):1802‐1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hong D, Long L, Wang AY, et al. Kidney manifestations of mild, moderate and severe coronavirus disease 2019: a retrospective cohort study. Clin Kidney J. 2020;13(3):340‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hung I‐N, Lung K‐C, Tso E‐K, et al. Triple combination of interferon beta‐1b, lopinavir‐ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID‐19: an open‐label, randomised, phase 2 trial. Lancet. 2020;395(10238):1695‐1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jeong HE, Lee H, Shin HJ, Choe YJ, Filion KB, Shin JY. Association between NSAIDs use and adverse clinical outcomes among adults hospitalized with COVID‐19 in South Korea: a nationwide study. Clin Infect Dis. 2020;ciaa1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jeyaraman P, Agrawal N, Bhargava R, et al. Convalescent plasma therapy for severe Covid‐19 in patients with hematological malignancies. Transfus Apher Sci. 2021;60(3):103075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jin M, Chen C, Huang J, et al. Clinical characteristics of COVID‐19 patients with asthma in Wuhan, China: a retrospective cohort study. J Asthma. 2020;1–9. 10.1080/02770903.2020.1850768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kamal AF, Widodo W, Kuncoro MW, et al. Does elective orthopaedic surgery in pandemic era increase risk of developing COVID‐19? A combined analysis of retrospective and prospective study at Cipto Mangunkusumo Hospital, Jakarta. Indonesia. Ann Med Surg. 2020;60:87‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kridin K, Schonmann Y, Tzur Bitan D, et al. Coronavirus Disease 2019 (COVID‐19)‐associated hospitalization and mortality in patients with psoriasis: a population‐based study. Am J Clin Dermatol. 2021;22(5):709‐718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kumar G, Mukherjee A, Sharma RK, et al. Clinical profile of hospitalized COVID‐19 patients in first & second wave of the pandemic: insights from an Indian registry based observational study. Indian J Med Res. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kumar S, Pujari VS, Kotak SD, Yadav SP, Someshwar VR, Raut AA. CT chest analysis of 2019 novel coronavirus pneumonia: an Indian perspective. Indian J Radiol Imaging. 2021;31(Suppl 1):S154‐S160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lee C, Ahn MY, Byeon K, et al. Clinical experience with use of Remdesivir in the treatment of severe acute respiratory syndrome coronavirus 2: a case series. Infect Chemother. 2020;52(3):369‐380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lee JY, Hong SW, Hyun M, et al. Epidemiological and clinical characteristics of coronavirus disease 2019 in Daegu, South Korea. Int J Infect Dis. 2020;98:462‐466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lee SG, Park GU, Moon YR, Sung K. Clinical characteristics and risk factors for fatality and severity in patients with coronavirus disease in korea: a nationwide population‐based retrospective study using the Korean Health Insurance Review and Assessment Service (HIRA) Database. Int J Environ Res Public health. 2020;17(22):8559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lee SW, Lee J, Moon SY, et al. Physical activity and the risk of SARS‐CoV‐2 infection, severe COVID‐19 illness and COVID‐19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. 2021. 10.1136/bjsports-2021-104203 [DOI] [PubMed] [Google Scholar]
- 42. Li C, Luo F, Liu C, et al. Effect of a genetically engineered interferon‐alpha versus traditional interferon‐alpha in the treatment of moderate‐to‐severe COVID‐19: a randomised clinical trial. Ann Med. 2021;53(1):391‐401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Li S, Lin Y, Zhu T, et al. Development and external evaluation of predictions models for mortality of COVID‐19 patients using machine learning method. Neural Comput Appl. 2021;1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Li X, Xu S, Yu M, et al. Risk factors for severity and mortality in adult COVID‐19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146(1):110‐118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Liu J, Zhang S, Wu Z, et al. Clinical outcomes of COVID‐19 in Wuhan, China: a large cohort study. Ann Intensive Care. 2020;10(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lu Y, Huang Z, Wang M, et al. Clinical characteristics and predictors of mortality in young adults with severe COVID‐19: a retrospective observational study. Ann Clin Microbiol Antimicrob. 2021;20(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Luo Y, Li J, Liu Z, Yu H, Peng X, Cao C. Characteristics and outcomes of hemodialysis patients with COVID‐19: a retrospective single center study. PeerJ. 2020;8:e10459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Marimuthu Y, Kunnavil R, Anil NS, et al. Clinical profile and risk factors for mortality among COVID‐19 inpatients at a tertiary care centre in Bengaluru, India. Monaldi Arch Chest Dis. 2021; 10.4081/monaldi.2021.1724 [DOI] [PubMed] [Google Scholar]
- 49. Meenakumari R, Thangaraj K, Sundaram A, et al. Clinical outcomes among COVID‐19 patients managed with modern and traditional Siddha medicine ‐A retrospective cohort study, Chennai, Tamil Nadu, India, 2020. J Ayurveda Integr Med. 2021. 10.1016/j.jaim.2021.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Meng M, Chen L, Zhang S, et al. Risk factors for secondary hemophagocytic lymphohistiocytosis in severe coronavirus disease 2019 adult patients. BMC Infect Dis. 2021;21(1):398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pakdel F, Ahmadikia K, Salehi M, et al. Mucormycosis in patients with COVID‐19: a cross‐sectional descriptive multicentre study from Iran. Mycoses. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Panda S, Mohamed A, Sikka K, et al. Otolaryngologic Manifestation and Long‐Term Outcome in Mild COVID‐19: experience from a tertiary care centre in India. Indian J otolaryngol head and neck surgery. 2020:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Pande D, Kochhar A, Saini S, Ganapathy U, Gogia AR. An update on initial epidemiological profile, clinical course, and outcome of COVID‐19 patients at a tertiary care center in India. Indian J Palliat Care. 2020;26(Suppl 1):S36‐S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Panthee B, Dhungana S, Panthee N, Gyawali S, Paudel A, Panthee S. Clinical and epidemiological features of COVID‐19 deaths in Nepal. New Microbes New Infect. 2020;38:100797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Prasetya IB, Cucunawangsih , Lorens JO, Sungono V, El‐Khobar KE, Wijaya RS. Prognostic value of inflammatory markers in patients with COVID‐19 in Indonesia. Clin Epidemiol Glob Health. 2021;11:100803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Ren P, Zhu C, He Y, Jiang H, Chen J. Analysis of the dynamic relationship between immune profiles and the clinical features of patients with COVID‐19. Ann Transl Med. 2021;9(14):1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Sahin B, Kose S, Eren G, Yoruk G. Clinical features, management, and outcome of hemodialysis patients with SARS‐CoV‐2. Ther Apher Dial. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Sang L, Xi Y, Lin Z, et al. Secondary infection in severe and critical COVID‐19 patients in China: a multicenter retrospective study. Annals of Palliat Med. 2021;10(8):8557–8570. [DOI] [PubMed] [Google Scholar]
- 59. Sharif N, Opu RR, Ahmed SN, et al. Prevalence and impact of comorbidities on disease prognosis among patients with COVID‐19 in Bangladesh: a nationwide study amid the second wave. Diabetes Metab Syndr. 2021;15(4):102148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Song J, Zeng M, Wang H, et al. Distinct effects of asthma and COPD comorbidity on disease expression and outcome in patients with COVID‐19. Allergy. 2021;76(2):483‐496. [DOI] [PubMed] [Google Scholar]
- 61. Sun C, Liu P, Cui Y, et al. Retrospective cohort study comparing the epidemiological and clinical characteristics between imported and local COVID‐19 inpatients in Nanyang, China. J Invest Med. 2021;69(3):704‐709. [DOI] [PubMed] [Google Scholar]
- 62. Sun J, Liu J, Li H, et al. Pulmonary rehabilitation focusing on the regulation of respiratory movement can improve prognosis of severe patients with COVID‐19. Ann Palliat Med. 2021;10(4):4262‐4272. [DOI] [PubMed] [Google Scholar]
- 63. Suryananda TD, Yudhawati R. Association of serum KL‐6 levels on COVID‐19 severity: a cross‐sectional study design with purposive sampling. Ann Med Surg. 2021;69:102673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Sy KTL, Haw NJL, Uy J. Previous and active tuberculosis increases risk of death and prolongs recovery in patients with COVID‐19. Infect Dis. 2020;52(12):902‐907. [DOI] [PubMed] [Google Scholar]
- 65. Tahtasakal CA, Oncul A, Sevgi DY, et al. Could we predict the prognosis of the COVID‐19 disease? J Med Virol. 2021;93(4):2420‐2430. [DOI] [PubMed] [Google Scholar]
- 66. Tsuchihashi Y, Arima Y, Takahashi T, et al. Clinical characteristics and risk factors for severe outcomes of novel coronavirus infection, january‐march 2020, Japan. J Epidemiol. 2021;31(8):487‐494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wang J, Lu Z, Jin M, et al. Clinical characteristics and risk factors of COVID‐19 patients with chronic hepatitis B: a multi‐center retrospective cohort study. Front Med. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wang W, Chen L, He Q, et al. Clinical characteristics of inpatients with coronavirus disease 2019 (COVID‐19) in Sichuan province. BMC Infect Dis. 2021;21(1):155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wu Q, Wang S, Li L, et al. Radiomics analysis of computed tomography helps predict poor prognostic outcome in COVID‐19. Theranostics. 2020;10(16):7231‐7244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Xu J, Wang W, Ye H, et al. A predictive score for progression of COVID‐19 in hospitalized persons: a cohort study. NPJ Prim Care Respiry Med. 2021;31(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Yan B, Yang J, Xie Y, Tang X. Relationship between blood eosinophil levels and COVID‐19 mortality. World Allergy Organ J. 2021;14(3):100521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Yan N, Xu Z, Mei B, Gao Y, Lv D, Zhang J. Neurological implications of non‐critically Ill patients with Coronavirus Disease 2019 in a Fangcang Shelter Hospital in Wuhan, China. Front Neurol. 2020;11:895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Yang C, Ma X, Wu J, et al. Low serum calcium and phosphorus and their clinical performance in detecting COVID‐19 patients. J Med Virol. 2021;93(3):1639‐1651. [DOI] [PubMed] [Google Scholar]
- 74. Yitao Z, Mu C, Ling Z, et al. Predictors of clinical deterioration in non‐severe patients with COVID‐19: a retrospective cohort study. Curr Med Res Opin. 2021;37(3):385‐391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Yu HH, Qin C, Chen M, Wang W, Tian DS. D‐dimer level is associated with the severity of COVID‐19. Thromb Res. 2020;195:219‐225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zeng JH, Wu WB, Qu JX, et al. Cardiac manifestations of COVID‐19 in Shenzhen, China. Infection. 2020;48(6):861‐870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zhang J, Hao Y, Ou W, et al. Serum interleukin‐6 is an indicator for severity in 901 patients with SARS‐CoV‐2 infection: a cohort study. J Transl Med. 2020;18(1):406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Zhang J‐J, Dong X, Cao Y‐Y, et al. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan. China. Allergy. 2020;75(7):1730‐1741. [DOI] [PubMed] [Google Scholar]
- 79. Zhang Q, Li J, Zhang Y, et al. Differences in clinical characteristics and liver injury between suspected and confirmed COVID‐19 patients in Jingzhou, Hubei Province of China. Medicine. 2021;100(19):e25913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Zhang W, Zhang C, Bi Y, et al. Analysis of COVID‐19 epidemic and clinical risk factors of patients under epidemiological Markov model. Results Phys. 2021;22:103881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Zhang X, Wang H, Wang Y, et al. Epidemiological and clinical based study on four passages of COVID‐19 patients: intervention at asymptomatic period contributes to early recovery. BMC Infect Dis. 2020;20(1):855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Zheng B, Cai Y, Zeng F, et al. An interpretable model‐based prediction of severity and crucial factors in patients with COVID‐19. Biomed Res Int. 2021;2021:8840835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Zhou K, Sun Y, Li LU, et al. Eleven routine clinical features predict COVID‐19 severity uncovered by machine learning of longitudinal measurements. Comput Struct Biotechnol J. 2021;19:3640‐3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Zhou S, Xu J, Sun W, et al. Clinical features for severely and critically Ill patients with COVID‐19 in Shandong: a retrospective cohort study. Ther Clin Risk Manag. 2021;17:9‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Zhu J, Huang WC, Huang B, et al. Clinical characteristics and prognosis of COVID‐19 patients with initial presentation of lung lesions confined to a single pulmonary lobe. Am J Transl Res. 2020;12(11):7501‐7509. [PMC free article] [PubMed] [Google Scholar]
- 86. Abraha HE, Gessesse Z, Gebrecherkos T, et al. Clinical features and risk factors associated with morbidity and mortality among patients with COVID‐19 in northern Ethiopia. Int J Infect Dis. 2021;105:776‐783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Biccard BM, Gopalan PD, Miller M, et al. Patient care and clinical outcomes for patients with COVID‐19 infection admitted to African high‐care or intensive care units (ACCCOS): a multicentre, prospective, observational cohort study. Lancet. 2021;397(10288):1885‐1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Bakamutumaho B, Cummings MJ, Owor N, et al. Severe COVID‐19 in uganda across two epidemic phases: a prospective cohort study. Am J Trop Med Hygiene. 2021;105(3):740–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Bepouka BI, Mandina M, Makulo JR, et al. Predictors of mortality in COVID‐19 patients at Kinshasa University Hospital, Democratic Republic of the Congo, from March to June 2020. Pan Afr Med J. 2020;37:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Boulle A, Davies MA, Hussey H, et al. Risk factors for COVID‐19 death in a population cohort study from the Western Cape Province, South Africa. Clin Infect Dis. 2020;ciaa1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Chanda D, Minchella PA, Kampamba D, et al. COVID‐19 severity and COVID‐19‐associated deaths among hospitalized patients with HIV infection ‐ Zambia, March‐December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(22):807‐810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Dave JA, Tamuhla T, Tiffin N, et al. Risk factors for COVID‐19 hospitalisation and death in people living with diabetes: a virtual cohort study from the Western Cape Province, South Africa. Diabetes Res Clin Pract. 2021;177:108925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Ibrahim OR, Suleiman BM, Abdullahi SB, et al. Epidemiology of COVID‐19 and predictors of outcome in Nigeria: a single‐center study. Am J Trop Med Hyg. 2020;103(6):2376‐2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Jassat W, Cohen C, Tempia S, et al. Risk factors for COVID‐19‐related in‐hospital mortality in a high HIV and tuberculosis prevalence setting in South Africa: a cohort study. Lancet HIV. 2021;8(9):e554‐e567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Kirenga B, Byakika‐Kibwika P, Muttamba W, et al. Efficacy of convalescent plasma for treatment of COVID‐19 in Uganda. BMJ Open Respir Res. 2021;8(1):e001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Nachega JB, Ishoso DK, Otokoye JO, et al. Clinical characteristics and outcomes of patients hospitalized for COVID‐19 in Africa: early insights from the democratic republic of the Congo. Am J Tropical Med Hyg. 2020;103(6):2419‐2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Parker A, Koegelenberg CFN, Moolla MS, et al. High HIV prevalence in an early cohort of hospital admissions with COVID‐19 in Cape Town, South Africa. S Afr Med J. 2020;110(10):982‐987. [DOI] [PubMed] [Google Scholar]
- 98. Riou C, du Bruyn E, Stek C, et al. Relationship of SARS‐CoV‐2‐specific CD4 response to COVID‐19 severity and impact of HIV‐1 and tuberculosis coinfection. J Clin Investig. 2021;131(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Venturas J, Zamparini J, Shaddock E, et al. Comparison of outcomes in HIV‐positive and HIV‐negative patients with COVID‐19. J Infect. 2021;83(2):217‐227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Wolday D, Gebrecherkos T, Arefaine ZG, et al. Effect of co‐infection with intestinal parasites on COVID‐19 severity: a prospective observational cohort study. EClinicalMedicine. 2021;39:101054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Anaya J‐M, Monsalve DM, Rojas M, et al. Latent rheumatic, thyroid and phospholipid autoimmunity in hospitalized patients with COVID‐19. J Transl Autoimmun. 2021;4:100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Borba MGS, Val FFA, Sampaio VS, et al. Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infection: a randomized clinical trial. JAMA Network Open. 2020;3(4):e208857. [DOI] [PubMed] [Google Scholar]
- 103. Fleitas PE, Paz JA, Simoy MI, et al. Clinical diagnosis of COVID‐19. A multivariate logistic regression analysis of symptoms of COVID‐19 at presentation. Germs. 2021;11(2):221‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Jeronimo CMP, Farias MEL, Val FFA, et al. Methylprednisolone as adjunctive therapy for patients hospitalized with coronavirus disease 2019 (COVID‐19; Metcovid): a randomized, double‐blind, phase IIb, Placebo‐controlled Trial. Clin Infect Dis. 2021;72(9):e373‐e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Maciel EL, Jabor P, Goncalves Junior E, et al. Factors associated with COVID‐19 hospital deaths in Espirito Santo, Brazil, 2020. Epidemiologia E Servicos De Saude : Revista do Sistema Unico De Saude do Brasil. 2020;29(4):e2020413. [DOI] [PubMed] [Google Scholar]
- 106. Pachiega J, Afonso A, Sinhorin GT, et al. Chronic heart diseases as the most prevalent comorbidities among deaths by COVID‐19 in Brazil. Rev Inst Med Trop Sao Paulo. 2020;62:e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Pierrotti LC, Reusing Junior JO, Freire MP, et al. COVID‐19 among kidney‐transplant recipients requiring hospitalization: preliminary data and outcomes from a single‐center in Brazil. Transpl Int. 2020;33(12):1837‐1842. [DOI] [PubMed] [Google Scholar]
- 108. Porto LC, Costa CH, Nunes AS, et al. Clinical and laboratory characteristics in outpatient diagnosis of COVID‐19 in healthcare professionals in Rio de Janeiro, Brazil. J Clin Pathol. 2021. [DOI] [PubMed] [Google Scholar]
- 109. Souza CDF, Leal TC, Santos LG. Circulatory system diseases in patients with COVID‐19: description of clinical and epidemiological profile of 197 deaths. Arq Bras Cardiol. 2020;115(2):281‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Bushman D, Davidson A, Pathela P, et al. Risk factors for death among hospitalized patients aged 21–64 years diagnosed with COVID‐19‐New York City. J Racial Ethn Health Disparities, 2021;1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Feehan AK, Fort D, Velasco C, et al. The importance of anosmia, ageusia and age in community presentation of symptomatic and asymptomatic SARS‐CoV‐2 infection in Louisiana, USA; a cross‐sectional prevalence study. Clin Microbiol Infect. 2021;27(4):633 e639‐633 e616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Fisman DN, Greer AL, Hillmer M, Tuite R. Derivation and validation of clinical prediction rules for COVID‐19 mortality in Ontario, Canada. Open Forum Infect Dis. 2020;7(11):ofaa463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Patler C, Saadi A. Risk of poor outcomes with COVID‐19 among U.S. detained immigrants: a cross‐sectional study. J Immigr Minor Health. 2021;23(4):863‐866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Sandoval M, Nguyen DT, Vahidy FS, Graviss EA. Risk factors for severity of COVID‐19 in hospital patients age 18–29 years. PLoS One. 2021;16(7):e0255544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Arenas Jimenez MD, Gonzalez‐Parra E, Riera M, et al. Mortality in hemodialysis patients with COVID‐19, the effect of paricalcitol or calcimimetics. Nutrients. 2021;13(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. El‐Battrawy I, Nunez‐Gil IJ, Abumayyaleh M, et al. COVID‐19 and the impact of arterial hypertension‐An analysis of the international HOPE COVID‐19 Registry (Italy‐Spain‐Germany). Eur J Clin Invest. 2021:e13582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Giubelan LI, Dumitrescu F, Stoian AC, Dragonu L. Analysis of the first 300 Cases of SARS CoV2 infection from the infection disease clinic of Craiova, Romania. Curr Health Sci J. 2021;47(1):28‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Group RC . Convalescent plasma in patients admitted to hospital with COVID‐19 (RECOVERY): a randomised controlled, open‐label, platform trial. Lancet. 2021;397(10289):2049‐2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Maximiano Sousa F, Roelens M, Fricker B, et al. Risk factors for severe outcomes for COVID‐19 patients hospitalised in Switzerland during the first pandemic wave, February to August 2020: prospective observational cohort study. Swiss Med Wkly. 2021;151:w20547. [DOI] [PubMed] [Google Scholar]
- 120. Munblit D, Bobkova P, Spiridonova E, et al. Incidence and risk factors for persistent symptoms in adults previously hospitalized for COVID‐19. Clin Exp Allergy. 2021;51(9):1107‐1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Thiabaud A, Iten A, Balmelli C, et al. Cohort profile: SARS‐CoV‐2/COVID‐19 hospitalised patients in Switzerland. Swiss Med Wkly. 2021;151:w20475. [DOI] [PubMed] [Google Scholar]
- 122. Li G, Liu Y, Jing X, et al. Mortality risk of COVID‐19 in elderly males with comorbidities: a multi‐country study. Aging. 2020;13(1):27‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are included in this article and available from the corresponding author upon reasonable request.


