Abstract
Mothers (n = 155) and their adolescent children (n = 146; aged 12–13 at pre‐COVID wave [Time 1, September 2019 to March 2020]) repeated measures of anxiety and depressive symptoms, and details about the impacts of the pandemic and social distancing at Time 2 (May‐June 2020). Average slopes of mother and adolescent depression increased but anxiety symptoms decreased from Time 1 to Time 2. Adolescent decreases in anxiety symptoms were driven by males, whereas depression increase was driven by females. Adolescents’ depression slopes were steeper for those who reported more negative changes. Implications are discussed relative to findings from other regions and later phases of the pandemic.
Keywords: COVID‐19, anxiety, depression, longitudinal change
The tragedy of the COVID‐19 pandemic and ensuing public health responses of social distancing, school closures, and staying home as much as possible “introduced a complex worldwide stressor” (Gruber et al., 2020, p. 6). Within weeks of the onset of the pandemic, developmental and clinical theorists warned that uncertainty and public health responses were ripe for enhancing mental health problems in parents and children (Fegert, Vitiello, Plener, & Clemens, 2020; Gruber et al., 2020; Lee, 2020; Loades et al., 2020; Masten & Motti‐Stefanidi, 2020; Osofsky, Osofsky, & Mamon, 2020; Pfefferbaum & North, 2020; Prime, Wade, & Browne, 2020; Wade et al., 2021). Specifically, risk factors known to exacerbate anxiety and depression (e.g., isolation, financial stress) were predicted to increase, consistent with early evidence (Breslau et al., 2021; Loades et al., 2020). Likewise, protective factors (e.g., school‐based supports, face‐to‐face social interactions) were expected to decrease, which has also been shown in early studies (Ellis, Dumas, & Forbes, 2020; Golberstein, Wen, & Miller, 2020). As a result, preliminary evidence aligned with expectations of risk, indicating that anxiety and depression rose in both youth (e.g., De France, Hancock, Stack, Serbin, & Hollenstein, 2021; Huang & Zhao, 2020) and parents (e.g., Benzeval et al., 2020; Perelli‐Harris & Walzenbach, 2020).
The picture of impact is far from complete, however. First, research so far has been mostly cross‐sectional and thus unable to situate levels of symptoms relative to prepandemic levels. Indeed, the impact may be especially potent for those who were already at risk (Gruber et al., 2020). Second, many of the stressors are family and/or region specific, such as localized remote schooling policies, social isolation protocols, number of cases, and deaths (Breslau et al., 2021). Thus, findings from one area may not map onto other areas. Third, while this pandemic is certainly a perturbation forming a natural experiment, it differs starkly from many of the large‐scale events that have been researched in the past. Terrorist attacks (Bonanno, Galea, Bucciarelli, & Vlahov, 2006), hurricanes (LaJoie, Sprang, & McKinney, 2010), and earthquakes (Harada et al., 2015) are localized, time‐bound events in comparison with the unfolding and truly global realities of the pandemic and public health responses that have persisted for over a year at this point. Moreover, the family‐ and region‐specific stressors mentioned above have also fluctuated over time, increasing and decreasing with seasons and waves of outbreak. Thus, the scope and timing of impact will differentiate COVID‐19 research findings, yet relatively few studies will capture the early impacts relative to later in the pandemic. With these considerations in mind, we rapidly adapted an ongoing longitudinal study of adolescents and their mothers for the purpose of understanding changes in both of their anxiety and depressive symptoms from just before to the first months of the pandemic. Our objectives were to identify trajectories of change and to examine person‐ and pandemic‐specific moderators of those trajectories.
Anxiety, Depression, and Covid‐19
By far, the most prevalent categories of mental health distress are anxiety and depression, with diagnostic point prevalence rates in excess of 10–15% and lifetime prevalence rates of 25–40% (Kessler, Berglund, Borges, Nock, & Wang, 2005; Schaefer et al., 2017). Youth begin to reach adult levels of these symptoms by mid‐adolescence with female rates rising to more than twice that of males (Breslau et al., 2017; Lewinsohn, Rohde, & Seeley, 1998). Rates for mothers of adolescents are also quite high, with prevalences up to 22% for depression and 11% for anxiety (Abel et al., 2019). For both parents and youth, symptoms can change due to myriad factors, including risk factors that exacerbate symptoms (e.g., stress) or protective factors that ameliorate symptoms (e.g., social support; Barlow, 2000; Calvete, Orue, & Hankin, 2013; Mezulis, Hyde, Simonson, & Charbonneau, 2011). The disruption to family circumstances during the early stages of the pandemic included the onset and removal of both risk and protective factors (Magson et al., 2021), as we consider next for anxiety and depression.
Anxiety
Anxiety is an emotional response driven by appraisals of uncertainty and potential threat (Lonigan, Vasey, Phillips, & Hazen, 2004; Micelli & Castelfranchi, 2005). The nature and domains of these uncertainties and threats can vary (e.g., social interactions, examinations) but only result in disorder when the symptoms reach excessive levels that interfere with functioning (American Psychiatric Association, 2013). During the first months of the pandemic, when relatively little was known, there were several characteristics that had the potential to exacerbate uncertainty and threat appraisals and therefore symptoms. First, the pandemic came with the addition of particular stressors. For example, the life‐threatening nature of the illness may drive individuals to contemplate their existence (Grasso et al., 2021). Public health measures introduced uncertainty in various ways as aspects of relationships, school, and work were novel and unpredictable (Mertens, Gerritsen, Duijndam, Salemink, & Engelhard, 2020; Sauer, Jungmann, & Witthöft, 2020). Second, the pandemic and public health responses also may have removed or limited previously relied upon protective factors. A sense of certainty and security is facilitated by the reliable repetition of events, schedules, and familiarity, yet the pandemic and ensuing measures tore away at these bulwarks and handholds of school, work, and familial consistency. Thus, the first few months of the pandemic in particular (i.e., the focus of the present study) have provided a suite of circumstances that may evoke appraisals of uncertainty and threat, and therefore potential increases in anxiety symptoms.
In contrast, there are aspects of the first wave of the pandemic that may have had the opposite effect and provided a relief to those who had elevated anxiety symptoms in the past (Bruining, Bartels, Polderman, & Popma, 2020; Shanahan et al., 2020). For parents, the stress of the work environment and/or their commute may have dissipated, providing less interpersonal agitation and more time for family (Benzeval et al., 2020; Perelli‐Harris & Walzenbach, 2020). Youth too may have experienced a relief from the stresses of school and other obligations (Cost et al., 2021). Peer victimization through bullying often happens in the school context, for example, and has strong ties to both anxiety and depression (Stapinski, Araya, Heron, Montgomery, & Stallard, 2015). At least initially, being under lockdown may have provided some relief for these youth (Shanahan et al., 2020). Moreover, some of the performative aspects of school, work, and socializing that were challenging in the past were diminished or eliminated in the first wave. Taken together, for at least some youth and families living through the pandemic, we might also expect decreases in anxiety and depressive symptoms.
Depression
While factors underlying depression include anxiety (Van den Bergh, Marchetti, & Koster, 2020), diminished social connection is more specifically salient for the onset and maintenance of depressive symptoms (Hames, Hagan, & Joiner, 2013; Rudolph, 2009). The social isolation that has resulted from quarantines, remote schooling, working from home, and other social distancing measures may have limited access to social supports that had historically protected against depressive symptoms (Erzen & Çikrikci, 2018; Ge, Yap, Ong, & Heng, 2017). Although the effects of diminished social supports are expected to have affected both parents and youth (Prime et al., 2020), the impact on youth may have been greater due to their greater age‐related reliance on peers and social interactions (Blakemore, 2019; Steinberg, 2008), as well as adolescents’ developmental vulnerability for the emergence of depression (Allen & Sheeber, 2008). Thus, like anxiety, the pandemic provided many circumstances that may have facilitated greater depressive symptoms in parents but particularly in youth.
For some of the same reasons, it is possible that staying at home and spending more time with family was a protective factor. This extended period of less harried and scheduled time combined with more opportunity to talk, play, create, or support each other may also have alleviated symptoms and promoted resilience (Masten, 2001). For example, during the early phase of the pandemic, depression was lower for youth who felt more socially connected (Magson et al., 2021) and who spent more time with family, both in‐person and via video chat (Ellis et al., 2020). Thus, early in the unfolding of the COVID‐19 pandemic, the direction that anxiety and depressive symptoms may have changed for youth and parents is still uncertain, as some may have experienced improvements even while others did not (Cost et al., 2021). We conducted the present study as a way to discover these individual differences in symptom changes as well as pandemic‐related factors that might explain the magnitude and/or direction of such changes.
The Present Study
As more studies are conducted over the next few years that measure the impact of COVID‐19, it is imperative that cultural, regional, and impact‐specific individual differences contextualize interpretations. The present study was conducted in Ontario, Canada, in a small city that experienced a relatively minimal impact in terms of number of cases and deaths. The timeline within which the present study was conducted is displayed in Figure 1. There are several features of the public health system response that bear noting in comparison with COVID‐19 studies conducted elsewhere. First, following the SARS outbreak in 2003, Canada mounted an investigation into where the health system failed and developed a commission that created a pandemic response plan (Government of Canada, 2018). This plan was at the ready and implemented early in the COVID outbreak. Second, unlike the severe and widespread impact in the United States, Canada’s impact on vulnerable populations was minimized through its universal healthcare system (e.g., no cost barriers to care). Third, in the region in which the current sample lives, there were 78 confirmed cases and no deaths by the end of data collection, just over 3 months after schools were shut down and the state of emergency was declared. Thus, the infection‐related impact on these participants was comparatively minimal, yet they still experienced the hardships of social isolation and remote learning, as well as the awareness of the tragic global pandemic shared by youth and families around the world. This study, therefore, afforded less confounded interpretations about the mental health impact of social restrictions than in regions where the number of cases and death toll was high as well.
Figure 1.
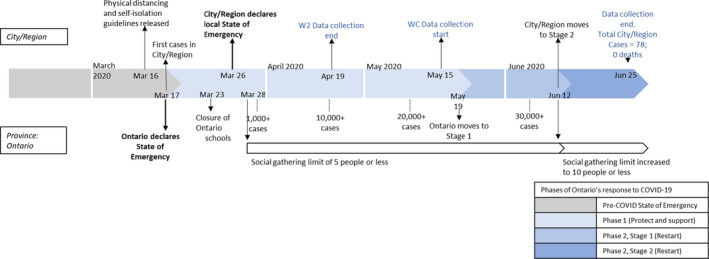
Timeline outlining the sequence of events of the study in relation to the city and province’s COVID‐19 responses and cases.
The present research comes from a longitudinal study of normative adolescent socioemotional development that had just completed data collection of an annual wave prior to the onset of the pandemic. We followed up with an impromptu “wave” of data collection in May and June of 2020, approximately 2–3 months into lockdown. Mothers and their adolescent children provided measures of anxiety and depressive symptoms at both waves as well as details about the impact of the pandemic and social distancing on their personal lives. Our primary research questions were (1) how did symptoms change over this period and (2) what predicted individual differences in these changes? For this second question, we assessed two key factors. First, we examined whether pre‐existing levels of anxiety or depression accounted for the pandemic‐related changes. Second, we wanted to assess individual differences in the pandemic and lockdown impacts on families and youth (Prime et al., 2020). As these impacts may have been different for adolescents and their mothers, they were measured in different ways. For the mothers, we assessed their personal hardship across 9 domains (work, education, home life, social, economic, emotional, physical health, physical distancing, and infection). With this approach, we could assess differences between mothers’ cumulative hardship as a broad index of how stressful the first wave might have been. For the youth, we were able to capture both negative and positive impacts from a checklist of possible changes that correspond to risk and protective factors, respectively. Thus, for youth, we had the opportunity to account for the heterogeneity of symptom change trajectories in either direction.
In addition, because of well‐known age‐related sex differences in anxiety and depressive symptoms in adolescence (Zahn‐Waxler, Shirtcliff, & Marceau, 2008), we also sought to differentiate changes by sex. Specifically, because females are consistently found to be at higher levels of both anxiety and depressive symptoms, we included sex as a predictor of their changes. Early indications from the pandemic have also highlighted that the negative impacts may have been more substantial for females (De France et al., 2021).
In adolescent models, we predicted before to during COVID slopes of anxiety and depressive symptoms from adolescents’ initial symptom levels, sex, and positive and negative changes due to social distancing protocols and school shutdown. In mother models, we predicted before to during COVID slopes of anxiety and depressive symptoms from mothers’ initial symptom levels and hardship due to pandemic restrictions. For all models, we included the number of days since school shutdown as a covariate to control for the growth in worldwide cases and concerns across the 2‐month period.
Method
Participants
At Time 1, there were 178 adolescents (77 girls, 98 boys, 1 nonbinary, and 2 “prefer not to disclose”) aged 12–13 years old (M age = 12.49) and 179 mothers 35.5–56.5 years old (M age = 45.2). Time 2 included 146 adolescents and mothers, plus 9 mothers whose adolescent did not participate. Adolescents reported being Caucasian (79.7%), mixed (13.3%), First Nation (1.4%), South Asian (1.4%), or other (4.2%) ethnicities. Mothers reported being Caucasian (87.7%), mixed (5.6%), or other (6.7%) ethnicities. Participants were originally recruited using a database of families who indicated interest in studies in the past, maintained by the developmental researchers in the department. Consent was obtained at each time point and, because the Time 2 COVID wave data were collected online, mothers had to provide consent first before youth were able to consider their assent.
Procedure
Time 1
Participants visited the laboratory for an interaction task as part of the 5‐year annual Second Decade study between September 2019 and March 2020. Prior to the tasks, participants completed questionnaires using computers provided in the laboratory. At the end of the laboratory session, participants received $45 CAD.
Time 2
To capture the early effects of the pandemic and lockdown, we inserted an unplanned “COVID wave” during May and June of 2020. Participants were e‐mailed a survey link on May 15th during Phase 1 of the province’s response to COVID‐19 (see Figure 1). Upon completion of the questionnaires, each participant received $15 CAD, which was sent via e‐transfer.
Measures
Anxiety symptoms
Mother and adolescent self‐reported anxiety symptoms were measured using the Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988). Participants indicated on a 4‐point scale (0 = not at all; 3 = severely—it bothered me a lot) the extent to which 21 anxiety symptoms have bothered them in the past month. The scale showed high internal consistency across respondents and time points (Cronbach’s alphas = .90–.96). The participants’ total scores were calculated by taking the average of the 21 items, with higher means indicating more symptoms of anxiety.
Adolescent depressive symptoms
The Child Depression Inventory, Second Edition (CDI‐2; Kovacs, 1992) is a 26‐item questionnaire for which youth self‐reported the degree to which sentences best described their feelings and ideas over the past two weeks (e.g., I am sad once in a while, I am sad many times, and I am sad all of the time). Reliability was high at both time points, .90 and .92, respectively. Higher mean scores indicated more severe depressive symptoms.
Mother depressive symptoms
The Beck Depression Inventory, Second Edition (BDI‐II; Beck, Steer, & Brown, 1996) is a 19‐item questionnaire for which mothers self‐reported the degree to which sentences best described their feelings over the past two weeks (e.g., I do not feel sad, I feel sad much of the time, I am sad all of the time, and I am so sad or unhappy that I can’t stand it). Reliability was high at both time points, .88 and .92, respectively. Higher mean scores indicated more severe depressive symptoms.
Child positive and negative changes (Time 2 only)
Mothers reported on their child’s positive and negative changes due to the pandemic using the COVID‐19 Adolescent Symptom & Psychological Experience Questionnaire (CASPE; Ladouceur, 2020). Using a “select all that apply” prompt, mothers indicated which changes were the most positive (12 items; e.g., more sleep, less school pressure, more time with family) and which were the most negative (8 items; e.g., not seeing friends, stress, worry about illness) for their child. These were summed to create positive change and negative change scores.
Mother hardship (Time 2 only)
Mothers self‐reported the degree of their own hardship using the Epidemic–Pandemic Impacts Inventory (EPII; Grasso, Briggs‐Gowan, Carter, Goldstein, & Ford, 2020a). Mothers indicated whether they experienced hardship (Yes or No) due to the pandemic across 92 items in nine domains: work, education, home life, social, economic, emotional, physical health, physical distancing, and infection. Mother hardship was calculated as the sum across all domains.
Number of days since lockdown (Time 2 Only)
We calculated a count of the number of days between local school closures (March 23rd, 2020) and the date that the Time 2 surveys were completed (May 15th–June 25th; see Figure 1). Because the details and subsequent public health measures were unfolding week by week, this days’ variable was used as a statistical control for potential variation in impact over those weeks.
Analytic Plan
First, we conducted missing data analyses to determine whether there were any differences along the core study variables between those who did vs. did not complete both waves of the study. We also ran preliminary correlations and descriptive statistics for the study variables, including t tests exploring mean‐level gender differences for adolescents. We used latent difference score (LDS) modeling (McArdle, 2009) in Mplus 8.4 (Muthén & Muthén, 1998‐2017) to estimate adolescents’ and mothers’ anxiety and depression symptom intercepts (i.e., initial levels) and slopes (i.e., changes from before to during COVID). The LDS technique allowed us to assess inter‐individual differences in intra‐individual change and, when such differences were significant, relate them to individual‐ and COVID‐specific predictors. We accounted for the measurement error of our observed indicators at each time point by fixing their residual variances to (1 – reliability) * variance of the scale in question (see McArdle, 2001). For models that were not fully saturated, we proceeded when the following indicators of acceptable fit were met: a standardized root mean square residual (SRMR) < .08, a root mean square error of approximation (RMSEA) < .08 with 90% confidence intervals (CI), and a comparative fit index (CFI) > .90. All focal models employed maximum likelihood estimation with standard errors robust to nonnormality (MLR) and full information maximum likelihood estimation (FIML) to handle missing data. We first ran four unconditional univariate base models assessing the intercepts and slopes of adolescents’ and mothers’ anxiety and depressive symptoms (separate models for each symptom within each informant). We then ran conditional LDS models for adolescents predicting the slope factors from initial symptom levels, sex, positive changes, and negative changes. We also ran conditional models for mothers with initial symptom levels and hardship as predictors. All conditional models controlled for number of days since school closure.
Since this was an exploratory study contingent on the sample of a previous longitudinal study and the timing of COVID‐19, we did not conduct an a priori power analysis. We selected the present sample‐analysis combination based on previous recommendations of 100–200 participants (depending on measurement quality) for latent statistical modeling similar to that used here (e.g., Kievit et al., 2018; Wolf, Harrington, Clark, & Miller, 2013). We conducted post hoc power analyses using the WebPower online tool (Zhang & Liu, 2019) for latent change score models with 2 measurement occasions, the unconditional parameter estimates obtained from the present analyses, and one “open” parameter predicting the slope. For each model, the parameter predicting the slope was varied to gauge the threshold at which 80% power could be achieved for estimates similar to those testing core hypotheses in the present investigation. Results indicated that a power of at least .80 could be achieved with approximate unstandardized estimates as low as .07, .04, .04, and .03 for the adolescent anxiety, adolescent depression, mother anxiety, and mother depression models, respectively.
Results
Preliminary tests for attrition effects using a dichotomous missing indicator as a predictor of anxiety and depression symptoms from the pre‐COVID wave yielded no significant differences with the exception of a small effect on mothers’ depression, F(1, 177) = 4.44, p = .04. The 33 mothers who did not participate in the COVID wave reported greater depressive symptoms (M = .54, SD = .38) than the 146 mothers who participated in both waves (M = .40, SD = .33). Of the 41 youth who did not participate in the COVID wave, the sex distribution was equal (49% female). Table 1 displays descriptive statistics and correlations among all continuous variables. It also shows the results of t tests exploring sex differences in the adolescent‐specific variables. Females reported greater anxiety symptoms than males at both time points and greater depression symptoms at Time 2.
Table 1.
Means, Standard Deviations, Correlations among Study Variables, and Sex Differences
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | M(SD) | M(SD)male | M(SD)female | t | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. A anx T1 | 1 | .73(.63) | .63(.55) | .84(.66) | −2.00* | ||||||||||||
| 2. A dep T1 | .56*** | 1 | 1.31(.28) | 1.30(.26) | 1.33(.26) | −.78 | |||||||||||
| 3. M anx T1 | .02 | .07 | 1 | .54(.43) | |||||||||||||
| 4. M dep T1 | .05 | .14 | .44*** | 1 | .40(.33) | ||||||||||||
| 5. A anx T2 | .52*** | .39*** | .03 | .13 | 1 | .52(.59) | .32(.45) | .77(.64) | −4.80*** | ||||||||
| 6. A dep T2 | .46*** | .56*** | .03 | .20* | .75*** | 1 | 1.39(.33) | 1.29(.26) | 1.52(.37) | −4.40*** | |||||||
| 7. M anx T2 | .01 | .08 | .47*** | .39*** | .14 | .06 | 1 | .36(.34) | |||||||||
| 8. M dep T2 | .01 | .05 | .25*** | .52*** | .20* | .11 | .63*** | 1 | .50(.40) | ||||||||
| 9. A pos | .09 | .00 | −.06 | .05 | .11 | −.02 | .04 | −.02 | 1 | 4.57(2.19) | 4.71(2.10) | 4.40(2.32) | .83 | ||||
| 10. A neg | .06 | .05 | .13 | .16 | .20* | .21* | .13 | .21* | −.13 | 1 | 6.15(1.88) | 5.99(1.91) | 6.34(1.81) | −1.13 | |||
| 11. A days | −.05 | −.04 | .11 | .13 | −.02 | .14 | .07 | .11 | −.09 | .12 | 1 | 70.00(12.12) | 69.14(12.03) | 70.83(12.08) | −.83 | ||
| 12. M hard | .08 | .08 | .06 | .16 | .11 | .16 | .15 | .19* | .04 | .11 | −.02 | 1 | 6.04(1.15) | ||||
| 13. M days | −.06 | −.09 | .14 | .03 | −.03 | −.01 | .14 | .05 | .003 | .12 | .83*** | .01 | 1 | 65.57(10.77) |
T1 = time 1. T2 = time 2. A = adolescent. M = Mother. Anx = anxiety symptoms. Dep = depressive symptoms. Pos = positive changes. Neg = negative changes Hard = Hardship. Days = days since lockdown that participant completed time 2 questionnaires. ***p < .001. *p < .05.
Unconditional Univariate LDS Models of Symptom Change from Before to During COVID‐19
The four unconditional univariate LDS base models are depicted in Figure 2. All slope means were significantly different from zero. In line with expectations of COVID‐related risk, adolescents and mothers reported average increases in depressive symptoms (estimates = .09, .09, ps ≤ .003, 95% CIs [.04, .14], [.03, .14], respectively). However, contrary to such expectations, anxiety symptoms for adolescents and mothers declined on average (estimates = −.19, −.19, ps < .001, 95% CIs [−.29, −.09], [−.26, −.13], respectively). Despite these mean‐level trends, adolescents and mothers varied considerably in their symptom change relative to their counterparts—all slope variances were significant (estimates = .07–.32, ps < .001).
Figure 2.
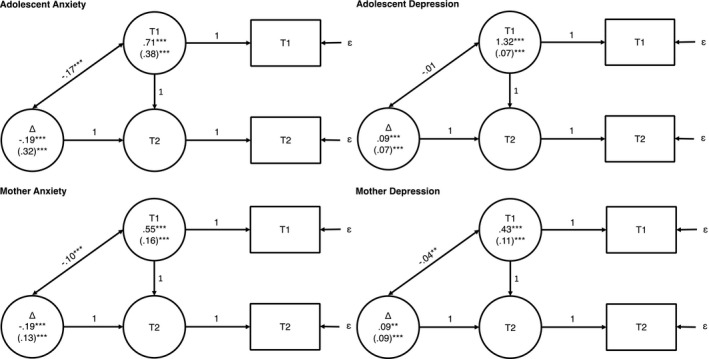
Unconditional univariate LDS models of change in adolescents’ and mothers’ anxiety and depression symptoms from before to during COVID‐19 lockdown.
Note: Squares denote observed scores. Circles denote latent scores. T1 = time 1. T2 = time 2. Δ = time 2 – time 1. Intercept and slope means, (variances), and covariances between T1 and slope scores depicted. ɛ = error term fixed to (1 – reliability) * variance. ***p < .001. **p < .01.
We saved the latent slope factor scores from unconditional models (nonestimated to ensure precise raw frequencies) and plotted them in histograms to visualize between‐participant variability in rates of change for each symptom type and informant. As seen in Figure 3, anxiety symptom slopes showed more dispersion and higher magnitudes of change in comparison with depressive symptom slopes. Bearing in mind that both symptoms were assessed on a 4‐point scale, 21% and 14% of adolescents and mothers, respectively, showed at least a 0.5‐point decrease in anxiety symptoms, whereas only 5% and 7% of adolescents and mothers, respectively, showed a 0.5‐point increase in depression symptoms from before to during COVID.
Figure 3.
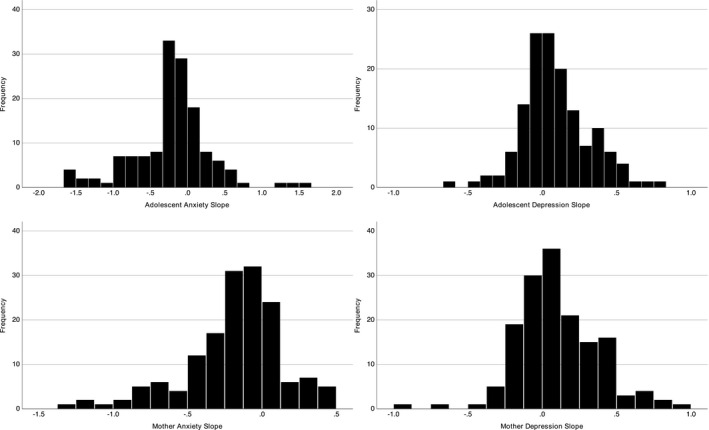
Distributions of adolescents’ and mothers’ anxiety and depression symptoms slope estimates.
Conditional Univariate LDS Models Predicting Symptom Change
Given the significant inter‐individual variability in all four slopes, we added our predictors to each model. As depicted in Table 2, adolescent sex (0 = male, 1 = female) significantly and positively predicted the anxiety and depressive symptom slopes. Probing these effects with separate unconditional models for males and females, males had a significant, negative anxiety symptom slope (b = −.31, p < .001, 95% CI [−.45, −.18]), whereas females did not (b = −.04, p = .54, 95% CI [−.17,.09]). In contrast, females had a significant, positive depressive symptoms slope (b = .19, p < .001, 95% CI [.12,.26]), whereas males did not (b = −.01, p = .88, 95% CI [−.07,.06]). Thus, the sample‐wide decrease in anxiety symptoms identified in the base model was driven by males whereas the sample‐wide increase in depressive symptoms was driven by females. Also, more negative changes due to COVID‐19 lockdown predicted steeper increases in depressive symptoms and higher initial levels of anxiety predicted steeper reported declines from before to during lockdown (see Table 2).
Table 2.
Results of LDS Models Predicting Changes in Anxiety and Depression Symptoms
| Predictor | Outcome | |||||||
|---|---|---|---|---|---|---|---|---|
| Adolescent Anxiety Slope | Adolescent Depression Slope | Mother Anxiety Slope | Mother Depression Slope | |||||
| b | β | b | β | b | β | b | β | |
| Anxiety Intercept | −.53*** (−.70, −.37) | −.57*** (−.73, −.41) | – | – | −.62*** (−.75, −.49) | −.69*** (−.81, −.58) | – | – |
| Depression Intercept | – | – | −.19 (−.43,.06) | −.19 (−.43,.05) | – | – | −.37*** (−.59, −.15) | −.39*** (−.59, −.20) |
| Days Since Lockdown | −.001 (−.008,.005) | −.03 (−.16,.10) | .001 (−.003,.005) | .05 (−.14,.24) | .001 (−.003,.006) | .04 (−.08,.16) | .00 (−.004,.005) | .01 (−.14,.15) |
| Hardship | – | – | – | – | .04 (−.01,.08) | .12 (−.03,.27) | .04 (−.01,.09) | .15 (−.02,.31) |
| Sex | .37*** (.20,.54) | .32*** (.17,.48) | .19*** (.10,.28) | .36*** (.21,.52) | – | – | – | – |
| Positive Change | −.01 (−.08,.06) | −.04 (−.29,.22) | .01 (−.02,.03) | .06 (−.15,.26) | – | – | – | – |
| Negative Change | .05 (−.01,.11) | .17 (−.01,.35) | .05*** (.02,.07) | .34*** (.15,.52) | – | – | – | – |
| Positive Change x Sex | .08 (−.02,.17) | .20 (−.04,.44) | .002 (−.04,.04) | .01 (−.21,.23) | – | – | – | – |
| Negative Change x Sex | −.02 (−.11,.07) | −.04 (−.23,.15) | −.04 (−.08,.01) | −.18 (−.40,.04) | – | – | – | – |
95% CIs. Sex (0 = male, 1 = female). ***p ≤ .001.
For mothers, hardship did not significantly predict anxiety symptom change. However, similar to adolescents, higher initial levels of anxiety symptoms significantly predicted steeper declines in anxiety over time. Hardship also did not significantly predict mothers’ depression symptom change, although mothers who reported higher initial levels of depression also tended to report steeper decreases/lesser increases in depression from before to during COVID‐19 lockdown.
Discussion
Understanding the impact of pandemic‐related measures on the well‐being of youth and their families is of paramount importance. The present study contributes to the fast‐growing literature documenting these impacts across the world. Our results indicated that, at least in the early months of the pandemic in a modest‐sized Canadian city, mean‐level anxiety symptoms decreased and depressive symptoms increased for both mothers and youth. Moreover, the decreases in anxiety symptoms were greatest for those who had higher prepandemic anxiety symptoms. For adolescents, the steepest decreases in anxiety symptoms were for males and the increases in depressive symptoms were greater for females. Youth who experienced more negative COVID‐related impacts (e.g., not seeing friends, stress, worry about illness) showed steeper increases in depressive symptoms.
Anxiety Symptoms and COVID‐19
Our findings on anxiety symptoms were the most surprising, given the dire predictions at the onset of the pandemic (e.g., Loades et al., 2020; Wade et al., 2021) and our own a priori hypotheses. Since then, longitudinal studies have mostly shown stable rates of anxiety symptoms for youth from before to the early months of the pandemic (Barendse et al., 2021; De France et al., 2021), as well as symptom decreases in both peer‐reviewed (Shanahan et al., 2020) and nonpeer‐reviewed (Widnall, Kidger, Winstone, Mars, & Haworth, 2020) studies. In a study conducted in New York City, arguably one of the hardest hit areas at the time, youth depressive and anxiety symptoms rose from April into early May but then decreased into July 2020 (Hawes, Szenczy, Olino, Nelson, & Klein, 2021).
That symptoms decreased in general and more steeply for the most pre‐COVID anxious participants in our study suggest at least two possibilities. First, the positive experiences that typically provide relief from anxiety were suddenly present or more available (e.g., more family time). Second, negative experiences that supported anxiety symptoms prior to the pandemic were no longer present or as strong (e.g., select work and academic stressors). However, the youth positive and negative change indicators we had available for this study did not predict changes in anxiety symptoms. As these measures were reported by mothers, it is possible that they did not fully reflect the subjective impact felt by the youth. Moreover, mothers’ hardship, which was expected to elevate anxiety, did not predict changes in mothers’ anxiety through COVID. Thus, it remains unclear from these findings what pandemic‐related factors may have supported anxiety symptom decreases.
The drop in anxiety symptoms was more pronounced for boys. As with the overall trend, there may have been sex‐specific changes in positive and negative factors that influenced this change pattern. Boys at this age may have had a greater appreciation for the interactions and activities at home compared to girls. Among the longitudinal studies completed to date, those that showed increases in anxiety symptoms did so for girls but not for boys (e.g., Magson et al., 2021). It may be that girls, who tend to be more physically and socially mature at this age (van der Graaff et al., 2014), did not experience the same relief as boys. For example, mother–daughter conflict increases in early adolescence (Lichtwarck‐Aschoff, Kunnen, & van Geert, 2009; Montemayor, Eberly, & Flannery, 1993) and this could have countered or canceled out other anxiolytic effects.
Depressive Symptoms and COVID‐19
In contrast to anxiety, depressive symptoms increased overall, particularly for girls. It is likely that social isolation and distancing measures diminished the connection and support that were previously available to these participants. Depressive symptoms are known to be elevated when relationships are poor or limited, especially for adolescent girls (Hammen, 2009). It is also possible that diminished activity in the first few months of lockdown included a decrease in exercise and weight gain, further factors that contribute to feelings of depression (Mikkelsen, Stojanovska, Polenakovic, Bosevski, & Apostolopoulos, 2017). However, initial results from pandemic studies have not shown this same pattern. For example, a recent report found that feelings associated with depression (e.g., hopelessness, feeling “down”) decreased for youth during COVID and this was associated with getting more sleep and more family connection (Twenge, Coyne, Carroll, & Wilcox, 2020). Thus, as with any developmental account of emotions, moods, and symptoms, the results of COVID studies are likely to be inconsistent at first until more generalizable patterns and clearer mechanisms of variability emerge.
Generalizability
It cannot be emphasized enough that the specifics of the geographic region’s illness‐related impact must contextualize corresponding findings. The present study helps to understand the changes related to public health protections in the relative absence of cases. In that sense, this and other studies conducted in such areas can provide insights into those specific features (e.g., school closings, work changes, limited face‐to‐face interaction). Other samples from larger urban centers where the number of cases and deaths were much higher (e.g., Hawes et al., 2021) are less able to separate preventive lockdown impacts from overall illness impacts. In such samples, it is more likely that youth and families knew someone infected or witnessed more severe public health events. Thus, it will be vital to accentuate these differences in our academic communication, and perhaps even more so in our public communication, about findings across studies.
A second factor that narrows the generalizability of these findings is the timing. Experiences of the pandemic in May and June of 2020 may have differed considerably from later in the pandemic. One reason is seasonal; as the pandemic wore on at this time, the weather improved and being outdoors was increasingly possible. The spike in cases in the autumn of 2020, for example, may have had the opposite pattern—just as restrictions were being put back in place, the outdoors was less feasible for recreation and socializing. Another difference in the early months of the pandemic was that the adaptations were still novel and in general more accommodating. Going back to school in September came with more potential issues as well as the anticipation that COVID‐related restrictions would probably continue for the entire school year.
Finally, as most of the studies documenting pandemic impacts on development and mental health are likely to come from the United States, it is important to highlight that the present study was conducted in Canada. Canada’s universal healthcare system significantly reduces limitations to access. Thus, these and other societal differences will be important factors to consider when assessing the net impact of the pandemic on youth and families.
Limitations and Future Directions
The longitudinal design of the present study is an important strength, as only comparisons to the months and years prior to the pandemic will help us understand the impacts of the pandemic on development. Nonetheless, there are several limitations that should be considered. As the COVID assessment wave was designed and implemented very quickly and early in the pandemic, few measurement options were available. Our measures tapped into several of the key aspects that we anticipated would have an impact, yet we failed to capture other possible factors. Most notably, we did not obtain sufficient self‐reported impacts from the youth. More details would have helped differentiate for whom symptoms increased or decreased. A second limitation is the diversity of our sample. While the sample roughly represents the composition of the city it was drawn from, these results may not generalize to larger cities or other regions with greater diversity. Finally, the limitations of timing, outbreak severity, and region discussed earlier certainly constrain the interpretations of our findings. However, we also see this as a strength given that studies will ultimately be compared and contrasted with respect to these characteristics in the future.
Conclusions
The circumstances surrounding the pandemic in the first half of 2020 inspired the expectation that the impact on the emotional functioning of youth and families would be devastating (Gruber et al., 2020). Indeed, for many around the world, these circumstances included death, severe illness, financial hardships, interpersonal conflict, isolation, and a great deal of uncertainty about the future. Any of these are well‐known factors that compromise mental health. At the same time, some of these pandemic changes included well‐known factors that improve mental health. Families have been spending more time together, some work and school stresses have been alleviated, new hobbies or activities have begun as ways to deal with public health restrictions, and technology has afforded ways to bridge physical distance. Thus, like most all socioemotional phenomena, the impacts of COVID‐19 on well‐being are diverse.
The present study highlights some broader issues that should be taken into account over the next few years as we strive to integrate findings across studies. First, youth are resilient (Zimmerman et al., 2013). Second, the rapid societal changes implemented to minimize the spread of the virus have exposed some of the more chronic and systemic problems that challenge the well‐being of youth and their families. The unexpected drops in anxiety symptoms in the present study and other COVID studies (e.g., Shanahan et al., 2020; Widnall et al., 2020) are perhaps reflections of these underlying, extant issues. Third, one of the messages of mental health anti‐stigma campaigns over the last decade is that those who suffer are not alone (Chen et al., 2016). The mechanism being targeted is the problematic sense, especially for youth, that they are uniquely broken or misunderstood. The pandemic has likely had an impact on most people to at least some degree; the uncertainty and concerns for safety are shared by the majority of one’s collective. Like a natural disaster or a war, this common purpose can be a balm against the existential angst and challenges to meaning in the modern world. Thus, there is a great deal to be learned about human development from this historical period. Finally, all researchers will need to approach the study of the pandemic impacts with open questioning to discover how, when, and for whom pandemic experiences have been beneficial or deleterious. Insights gained from such inquiries will go a long way to improve postpandemic society and the lives of youth and families.
Research was supported by funding from Queen’s University and the Social Sciences and Humanities Research Council of Canada.
References
- Abel, K. M. , Hope, H. , Swift, E. , Parisi, R. , Ashcroft, D. M. , Kosidou, K. , … Pierce, M. (2019). Prevalence of maternal mental illness among children and adolescents in the UK between 2005 and 2017: a national retrospective cohort analysis. The Lancet Public Health, 4(6), e291–e300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen, N. B. , & Sheeber L. B. (Eds.) (2008). Adolescent emotional development and the emergence of depressive disorders. Cambridge, UK: Cambridge University Press. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM‐5®). Arlington, Texas: American Psychiatric Pub. [Google Scholar]
- Barendse, M. , Flannery, J. E. , Cavanagh, C. , Aristizabal, M. , Becker, S. P. , Berger, E. , & Pfeifer, J. H. (2021). Longitudinal change in adolescent depression and anxiety symptoms from before to during the COVID‐19 pandemic: An international collaborative of 12 samples. PsyArXiv. 10.31234/osf.io/hn7us [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow, D. H. (2000). Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist, 55(11), 1247–1263. [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Epstein, N. , Brown, G. , & Steer, R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Steer, R. A. , & Brown, G. K. (1996). Beck depression inventory manual (2nd ed.). San Antonion, TX: Psychological Corporation. [Google Scholar]
- Benzeval, M. , Burton, J. , Crossley, T. F. , Fisher, P. , Jäckle, A. , Perelli‐Harris, B. , & Walzenbach, S. (2020). Understanding Society COVID‐19 Survey May Briefing Note: Family relationships (No. 13, pp. 5). Understanding Society Working Paper. [Google Scholar]
- Blakemore, S. J. (2019). Adolescence and mental health. The Lancet, 393(10185), 2030–2031. [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. , Galea, S. , Bucciarelli, A. , & Vlahov, D. (2006). Psychological resilience after disaster: New York City in the aftermath of the September 11th terrorist attack. Psychological Science, 17(3), 181–186. 10.1111/j.1467-9280.2006.01682.x [DOI] [PubMed] [Google Scholar]
- Breslau, J. , Finucane, M. L. , Locker, A. R. , Baird, M. D. , Roth, E. A. , & Collins, R. L. (2021). A longitudinal study of psychological distress in the United States before and during the COVID‐19 pandemic. Preventive Medicine, 143, 106362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau, J. , Gilman, S. E. , Stein, B. D. , Ruder, T. , Gmelin, T. , & Miller, E. (2017). Sex differences in recent first‐onset depression in an epidemiological sample of adolescents. Translational Psychiatry, 7(5), e1139. 10.1038/tp.2017.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruining, H. , Bartels, M. , Polderman, T. J. , & Popma, A. (2020). COVID‐19 and child and adolescent psychiatry: An unexpected blessing for part of our population? European Child & Adolescent Psychiatry, 1–2. 10.1007/s00787-020-01578-5. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvete, E. , Orue, I. , & Hankin, B. L. (2013). Transactional relationships among cognitive vulnerabilities, stressors, and depressive symptoms in adolescence. Journal of Abnormal Child Psychology, 41(3), 399–410. 10.1007/s10802-012-9691-y [DOI] [PubMed] [Google Scholar]
- Chen, S.‐P. , Chen, S.‐P. , Koller, M. , Koller, M. , Krupa, T. , Krupa, T. , … Stuart, H. (2016). Contact in the classroom: Developing a program model for youth mental health contact‐based anti‐stigma education. Community Mental Health Journal, 52(3), 281–293. 10.1007/s10597-015-9944-7 [DOI] [PubMed] [Google Scholar]
- Cost, K. T. , Crosbie, J. , Anagnostou, E. , Birken, C. S. , Charach, A. , Monga, S. , … Korczak, D. J. (2021). Mostly worse, occasionally better: Impact of COVID‐19 pandemic on the mental health of Canadian children and adolescents. European Child & Adolescent Psychiatry, 1–14. 10.1007/s00787-021-01744-3. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De France, K. , Hancock, G. , Stack, D. M. , Serbin, L. A. , & Hollenstein, T. (2021). The mental health implications of COVID‐19 for adolescents: Follow‐up of a four‐wave longitudinal study during the pandemic. American Psychologist, 1–15. 10.1037/amp0000838. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Ellis, W. E. , Dumas, T. M. , & Forbes, L. M. (2020). Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID‐19 crisis. Canadian Journal of Behavioural Science, 52(3), 177–187. [Google Scholar]
- Erzen, E. , & Çikrikci, Ö. (2018). The effect of loneliness on depression: A meta‐analysis. International Journal of Social Psychiatry, 64(5), 427–435. [DOI] [PubMed] [Google Scholar]
- Fegert, J. M. , Vitiello, B. , Plener, P. L. , & Clemens, V. (2020). Challenges and burden of the Coronavirus 2019 (COVID‐19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge, L. , Yap, C. W. , Ong, R. , & Heng, B. H. (2017). Social isolation, loneliness and their relationships with depressive symptoms: A population‐based study. PLoS One, 12(8), e0182145. 10.1371/journal.pone.0182145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein, E. , Wen, H. , & Miller, B. F. (2020). Coronavirus disease 2019 (COVID‐19) and mental health for children and adolescents. JAMA Pediatrics, 174(9), 819–820. [DOI] [PubMed] [Google Scholar]
- Government of Canada (2018). Canadian pandemic influenza preparedness: Planning guidance for the health sector. https://www.canada.ca/en/public‐health/services/flu‐influenza/canadian‐pandemic‐influenza‐preparedness‐planning‐guidance‐health‐sector.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso, D. J. , Briggs‐Gowan, M. J. , Carter, A. S. , Goldstein, B. , & Ford, J. D. (2020). A person‐centered approach to profiling COVID‐related experiences in the United States: Preliminary findings from the epidemic‐pandemic impacts inventory (EPII). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso, M. , Klicperová‐Baker, M. , Koos, S. , Kosyakova, Y. , Petrillo, A. , & Vlase, I. (2021). The impact of the coronavirus crisis on European societies. What have we learnt and where do we go from here? ‐ Introduction to the COVID volume. European Societies, 23(S1), S2–S32. 10.1080/14616696.2020.1869283 [DOI] [Google Scholar]
- Gruber, J. , Prinstein, M. J. , Clark, L. A. , Rottenberg, J. , Abramowitz, J. S. , Albano, A. M. , … Weinstock, L. M. (2020). Mental health and clinical psychological science in the time of COVID‐19: Challenges, opportunities, and a call to action. The American Psychologist, 76(3), 409–426. 10.1037/amp0000707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hames, J. L. , Hagan, C. R. , & Joiner, T. E. (2013). Interpersonal processes in depression. Annual Review of Clinical Psychology, 9, 355–377. [DOI] [PubMed] [Google Scholar]
- Hammen, C. (2009). Adolescent depression: Stressful interpersonal contexts and risk for recurrence. Current Directions in Psychological Science, 18(4), 200–204. 10.1111/j.1467-8721.2009.01636.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada, N. , Shigemura, J. , Tanichi, M. , Kawaida, K. , Takahashi, S. , & Yasukata, F. (2015). Mental health and psychological impacts from the 2011 Great East Japan earthquake disaster: A systematic literature review. Disaster and Military Medicine, 1(1), 17. 10.1186/s40696-015-0008-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawes, M. T. , Szenczy, A. K. , Olino, T. M. , Nelson, B. D. , & Klein, D. N. (2021). Trajectories of depression, anxiety and pandemic experiences: A longitudinal study of youth in New York during the spring‐summer of 2020. Psychiatry Research, 298, 113778. 10.1016/j.psychres.2021.113778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y. , & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: A web‐based cross‐sectional survey. Psychiatry Research, 288, 112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Berglund, P. , Borges, G. , Nock, M. , & Wang, P. S. (2005). Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. The Journal of the American Medical Association, 293(20), 2487–2495. 10.1001/jama.293.20.2487 [DOI] [PubMed] [Google Scholar]
- Kievit, R. A. , Brandmaier, A. M. , Ziegler, G. , van Harmelen, A. , de Mooij, S. M. M. , Moutoussis, M. , … Dolan, R. J. (2018). Developmental cognitive neuroscience using latent change score models: A tutorial and applications. Developmental Cognitive Neuroscience, 33, 99–117. 10.1016/j.dcn.2017.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs, M. (1992). Children’s Depression Inventory (CDI): Technical manual update. Multi‐Health Systems. [Google Scholar]
- Ladouceur, C. (2020). COVID‐19 adolescent symptom and psychological experience questionnaire (CASPE). Pittsburgh, PA: Author. [Google Scholar]
- LaJoie, A. S. , Sprang, G. , & McKinney, W. P. (2010). Long‐term effects of Hurricane Katrina on the psychological well‐being of evacuees. Disasters, 34(4), 1031–1044. 10.1111/j.1467-7717.2010.01181.x [DOI] [PubMed] [Google Scholar]
- Lee, J. (2020). Mental health effects of school closures during COVID‐19. The Lancet Child & Adolescent Health, 4, 421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn, P. M. , Rohde, P. , & Seeley, J. R. (1998). Major depressive disorder in older adolescents: Prevalence, risk factors, and clinical implications. Clinical Psychology Review, 18(7), 765–794. 10.1016/S0272-7358(98)00010-5 [DOI] [PubMed] [Google Scholar]
- Lichtwarck‐Aschoff, A. , Kunnen, S. E. , & van Geert, P. L. (2009). Here we go again: A dynamic systems perspective on emotional rigidity across parent–adolescent conflicts. Developmental Psychology, 45(5), 1364–1375. [DOI] [PubMed] [Google Scholar]
- Loades, M. E. , Chatburn, E. , Higson‐Sweeney, N. , Reynolds, S. , Shafran, R. , Brigden, A. , … Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. Journal of the American Academy of Child and Adolescent Psychiatry, 59(11), 1218–1239.e3. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonigan, C. J. , Vasey, M. W. , Phillips, B. M. , & Hazen, R. A. (2004). Temperament, anxiety, and the processing of threat‐relevant stimuli. Journal of Clinical Child & Adolescent Psychology, 33(1), 8–20. 10.1207/S15374424JCCP3301_2 [DOI] [PubMed] [Google Scholar]
- Magson, N. R. , Freeman, J. Y. A. , Rapee, R. M. , Richardson, C. E. , Oar, E. L. , & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID‐19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten, A. S. , & Motti‐Stefanidi, F. (2020). Multisystem resilience for children and youth in disaster: Reflections in the context of COVID‐19. Adversity and Resilience Science, 1(2), 95–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle, J. J. (2001). A latent difference score approach to longitudinal dynamic structural analysis. In Cudeck R., du Toit S., & Sorbom D. (Eds.), Structural equation modeling: Present and future (pp. 341–380). Lincolnwood, IL: Scientific Software International. [Google Scholar]
- McArdle, J. J. (2009). Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology, 60(1), 577–605. 10.1146/annurev.psych.60.110707.163612 [DOI] [PubMed] [Google Scholar]
- Mertens, G. , Gerritsen, L. , Duijndam, S. , Salemink, E. , & Engelhard, I. M. (2020). Fear of the coronavirus (COVID‐19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders, 74, 102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezulis, A. H. , Hyde, J. S. , Simonson, J. , & Charbonneau, A. M. (2011). Integrating affective, biological, and cognitive vulnerability models to explain the gender difference in depression: The ABC Model and its implications for intervention. [Google Scholar]
- Miceli, M. , & Castelfranchi, C. (2005). Anxiety as an “epistemic” emotion: An uncertainty theory of anxiety. Anxiety, Stress, and Coping, 18(4), 291–319. [Google Scholar]
- Mikkelsen, K. , Stojanovska, L. , Polenakovic, M. , Bosevski, M. , & Apostolopoulos, V. (2017). Exercise and mental health. Maturitas, 106, 48–56. 10.1016/j.maturitas.2017.09.003 [DOI] [PubMed] [Google Scholar]
- Montemayor, R. , Eberly, M. , & Flannery, D. J. (1993). Effects of pubertal status and conversation topic on parent and adolescent affective expression. The Journal of Early Adolescence, 13(4), 431–447. [Google Scholar]
- Muthén, L. , & Muthén, B. (1998–2017). Mplus user’s guide. Muthén & Muthén. [Google Scholar]
- Osofsky, J. D. , Osofsky, H. J. , & Mamon, L. Y. (2020). Psychological and social impact of COVID‐19. Psychological Trauma, 12(5), 468–469. 10.1037/tra0000656 [DOI] [PubMed] [Google Scholar]
- Perelli‐Harris, B. , & Walzenbach, S. (2020). How has the Covid‐19 crisis impacted parents relationships with their children?. [Google Scholar]
- Pfefferbaum, B. , & North, C. S. (2020). Mental health and the Covid‐19 pandemic. The New England Journal of Medicine, 383(6), 510–512. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Prime, H. , Wade, M. , & Browne, D. T. (2020). Risk and resilience in family well‐being during the COVID‐19 pandemic. American Psychologist, 75(5), 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Rudolph, K. D. (2009). The interpersonal context of adolescent depression. In Nolen‐Hoeksema S., & Hilt L. M. (Eds.), Handbook of depression in adolescents (pp. 377–418). Routledge/Taylor & Francis Group. [Google Scholar]
- Sauer, K. S. , Jungmann, S. M. , & Witthöft, M. (2020). Emotional and behavioral consequences of the COVID‐19 pandemic: The role of health anxiety, intolerance of uncertainty, and distress (in) tolerance. International Journal of Environmental Research and Public Health, 17(19), 7241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer, J. D. , Scult, M. A. , Caspi, A. , Arseneault, L. , Belsky, D. W. , Hariri, A. R. , … Moffitt, T. E. (2017). Is low cognitive functioning a predictor or consequence of major depressive disorder? A test in two longitudinal birth cohorts. Development and Psychopathology, Journal Article, 126, 1–15. 10.1017/S095457941700164X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan, L. , Steinhoff, A. , Bechtiger, L. , Murray, A. L. , Nivette, A. , Hepp, U. , … Eisner, M. (2020). Emotional distress in young adults during the COVID‐19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine, 1–10. 10.1017/S003329172000241X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapinski, L. A. , Araya, R. , Heron, J. , Montgomery, A. A. , & Stallard, P. (2015). Peer victimization during adolescence: Concurrent and prospective impact on symptoms of depression and anxiety. Anxiety, Stress, and Coping, 28(1), 105–120. 10.1080/10615806.2014.962023 [DOI] [PubMed] [Google Scholar]
- Twenge, J. , Coyne, S. , Carroll, J. , & Wilcox, W. (2020). Teens in quarantine: Mental health, screen time, and family connection. Institute for Family Studies: The Wheatley Institution. [Google Scholar]
- van den Bergh, N. , Marchetti, I. , & Koster, E. H. W. (2020). Bridges over troubled waters: Mapping the interplay between anxiety, depression and stress through network analysis of the DASS‐21. Cognitive Therapy and Research, 45(1), 46–60. 10.1007/s10608-020-10153-w [DOI] [Google Scholar]
- van der Graaff, J. , Branje, S. , De Wied, M. , Hawk, S. , Van Lier, P. , & Meeus, W. (2014). Perspective taking and empathic concern in adolescence: Gender differences in developmental changes. Developmental Psychology, 50(3), 881–888. 10.1037/a0034325 [DOI] [PubMed] [Google Scholar]
- Wade, M. , Prime, H. , Johnson, D. , May, S. S. , Jenkins, J. M. , & Browne, D. T. (2021). The disparate impact of COVID‐19 on the mental health of female and male caregivers. Social Science & Medicine, 275, 113801. 10.1016/j.socscimed.2021.113801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widnall, E. , Kidger, J. , Winstone, L. , Mars, B. , & Haworth, C. (2020). Young people’s mental health during the COVID‐19 pandemic. National Institute of Health Research, School of Public Health. https://sphr.nihr.ac.uk/research/young‐peoples‐mental‐health‐during‐the‐covid‐19‐pandemic/ [Google Scholar]
- Wolf, E. J. , Harrington, K. M. , Clark, S. L. , & Miller, M. W. (2013). Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educational and Psychological Measurement, 73(6), 913–934. 10.1177/0013164413495237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahn‐Waxler, C. , Shirtcliff, E. A. , & Marceau, K. (2008). Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology, 4, 275–303. [DOI] [PubMed] [Google Scholar]
- Zhang, Z. , & Liu, H. (2019). Sample size and measurement occasion planning for latent change score models through Monte Carlo simulation. In Ferrer E., Boker S. M., & Grimm K. J. (Eds.), Longitudinal multivariate psychology (pp. 189–211). Taylor & Francis. [Google Scholar]
- Zimmerman, M. A. , Stoddard, S. A. , Eisman, A. B. , Caldwell, C. H. , Aiyer, S. M. , & Miller, A. (2013). Adolescent resilience: Promotive factors that inform prevention. Child Development Perspectives, 7(4), 215–220. 10.1111/cdep.12042 [DOI] [PMC free article] [PubMed] [Google Scholar]


