Abstract
Background
COVID‐19 is generating clinical challenges, lifestyle changes, economic consequences. The pandemic imposes to familiarize with concepts as prevention, vulnerability and resilience.
Methods
We analysed and reviewed the most relevant papers in the MEDLINE database on syndemic, noncommunicable diseases, pandemic, climate changes, pollution, resilience, vulnerability, health costs, COVID‐19.
Results
We discuss that comprehensive strategies must face multifactorial consequences since the pandemic becomes syndemic due to interactions with noncommunicable diseases, climate changes and iniquities. The lockdown experience, on the other hand, demonstrates that it is rapidly possible to reverse epidemiologic trends and to reduce pollution. The worst outcome is evident in eight highly industrialized nations, where 12% of the world population experienced about one‐third of all COVID‐19‐deaths worldwide. Thus, a great economic power has not been fully protective, and a change of policy is obviously needed to avoid irreversible consequences.
Conclusions
We are accumulating unhealthy populations living in unhealthy environments and generating unhealthy offspring. The winning policy should tackle structural inequities through a syndemic approach, to protect vulnerable populations from present and future harms.
Keywords: climate changes, COVID‐19, noncommunicable diseases, pandemic, pollution, resilience, SARS‐CoV‐2, syndemic, vulnerability
1. THE START
At the end of 2019, a novel coronavirus was reported to World Health Organization as the cause of a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China. The name severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) was ultimately adopted. On March 11, 2020, COVID‐19, the disease caused by SARS‐CoV‐2 was identified as a global pandemic spreading worldwide. 1 , 2 , 3 , 4 To date and globally, we are counting over 230 million confirmed cases, over 4.7 million deaths, and over 5.8 billion vaccine doses administered (WHO COVID‐19 Dashboard accessed 24 September 2021 5 ). The SARS‐CoV‐2 pandemic is definitively changing our lives because of several simultaneous events including infectious and clinical aspects (ie, spread of SARS‐CoV‐2 variants, respiratory and non‐respiratory manifestations, immune response and reinfection, need of vaccine prophylaxis), marked changes in lifestyle and habits (ie, prophylaxis by frequent handwashing, mask‐wearing, social distancing, quarantine, increased use of digital media and smart‐work implementation) and many socio‐economic implications. 6
Independently from own specific and usual area of interest, each health professional should fill huge knowledge gaps about virology, epidemiology, variable clinical manifestations, prevention and therapy of SARS‐CoV‐2. The overlapping effects of this new disease are studied in fragile patients, and in a rapidly evolving scenario.
Besides the clinical implications of the pandemic, the new fields of actions impose to build specific strategies to dissect the multifactorial, medical and non‐medical consequences. In addition, we should learn how to avoid future harms. As health professionals, we are directly facing the individual and global effects of COVID‐19 in a complex scenario, where COVID‐19 interacts with other severe criticalities.
In that follow‐ups, we discuss how COVID‐19 challenges the capacity of resilience of health professionals and of large communities worldwide. We explore the complex relationships existing, mainly in western countries, between the viral pandemic and factors, which increase vulnerability. Aspects include the growing incidence of noncommunicable diseases (NCD), the alarming effects of climate change and of environmental pollution, and the spread of iniquities and inequalities.
2. SEARCH STRATEGY AND SELECTION CRITERIA
We searched the MEDLINE database and included the terms syndemic, noncommunicable diseases, pandemic, climate changes, pollution, resilience, vulnerability, health costs, COVID‐19 and SARS‐CoV‐2. No language restrictions were applied. Abstracts and potentially relevant full texts were reviewed independently by authors (ADC, MK and PP) with any conflict resolved by consensus. Reporting of the study conforms to broad EQUATOR guidelines. 7
3. THE HEALTH PROFESSIONALS HAVE BEEN OBLIGED TO FAMILIARIZE THEMSELVES WITH THE CONCEPT OF RESILIENCE.
The word resilience is defined as ‘an ability to recover from or adjust easily to a misfortune or change’. 8 This word arises from the present participle of the Latin verb resilire, meaning ‘to jump back’ or ‘to recoil’. We learn from ongoing events, that indeed we can oppose the sudden changes in our societies and life. In last year, we firstly published a paper to focus on the role of internists and resilience, 9 in accordance with the mission of the Italian Society of Internal Medicine (SIMI), the oldest Scientific Society in Italy, dated 1887. We reported the striking difference and gap existing between the ongoing COVID‐19 outbreaks in Northern compared to Southern Italy, hoping that the incidence of disease could stay lower in the southern regions. That was not the case, unfortunately, and we had to adopt fast, effective ethical and technical decisions to govern the process. We had to quickly discuss issues related to patients (both COVID‐19 and non‐COVID‐19), emergency rooms and overcrowding, waiting lists, organization of grey areas, role of intensive care units, death rates and later policies related to long‐COVID syndromes. Additional issues concerned the needs arising out of conditions such as critical, frail, cancer patients, elderly isolation and non‐COVID communities. 10 Overall, these events initiated a period of huge challenge for the Public Health Systems locally, at a national level, and worldwide. We had to rearrange clinical and academic activities, and we are now adopting methodologies designed for distance learning/teaching and remote working of personnel at any level. Deeply affected aspects concern personal interactions, research stages, access to available funding, participation in meetings/congresses and webinar methodologies. 11 In addition, COVID‐19 substantially affects the quality of life of healthcare professionals. 12 Eventually, for many researchers the overall profile of scientific output is deeply affected by the COVID‐19 pandemic, by shifting the field of interest towards still unexplored territories, 9 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 as also documented by the global number of publications (more than 190,000 from 2019 to date) available so far in PubMed (PubMed (nih.gov)).
4. THE PANDEMIC AND THE GROWING INCIDENCE OF NONCOMMUNICABLE DISEASES
We are currently interacting with two types of pandemics, which are overwhelming the populations, that is, the SARS‐CoV‐2 pandemic is spreading acutely on the wide background of NCD pandemic. There is an evidence of a close relationship between these two widely diffused threats for the human health.
The progression of NCD can negatively affect the outcome of the SARS‐CoV‐2 infection. 21 , 22 , 23 On the other hand, social containment measures taken to reduce the spread of the infection promoted unhealthy lifestyles and, in turn, increased health risk in patients with NCD. 16 , 24 Future studies need to clarify if and to which extent the acute SARS‐CoV‐2 infection will affect the progression of the pre‐existing NCD in COVID‐19 survivors. 16 , 25 This possibility exists mainly for selected conditions as chronic pulmonary, 26 , 27 cardiovascular, 28 , 29 neurologic, 30 psychiatric, 31 and metabolic disorders. 13 , 14 , 16
The mortality risk secondary to a SARS‐CoV‐2 infection, however, could be non‐specific, since NCD have been associated with an increased risk of death due to infectious diseases even before the COVID‐19 pandemic began. 32 This evidence underscores the role of NCD as factors increasing individual vulnerability in the pandemic era, and of the pandemic as an amplifier of previously existing risk factors.
About 22% of the global population (from subjects younger than 20 years to subjects aged 70 or older) suffer from at least one chronic disease able to increase the risk of a severe course of disease after a SARS‐CoV‐2 infection. This risk is highest in countries with the larger proportion of elderly subjects. 33 Ageing and multi‐morbidity negatively influence the course of COVID‐19. 34 However, the increased vulnerability in aged people is mainly related to the degree of frailty, rather than to age per se. 34 , 35 Frailty, in turn, depends on complex relationships linking environmental factors to NCD, finally leading to disabilities and reduced health span. 36
Notably, the environmental factors leading to NCD and frailty act during the whole life, and frequently start during the period in‐utero. 36 On the other hand, NCD affects people of any age, and the epidemiologic trend is continuously rising. The four main NCD, namely cardiovascular diseases, cancer, chronic respiratory diseases and diabetes, cause an enormous burden of premature deaths. 37 Moreover, the risk of mortality due to NCD between 30 and 70 years of age is inversely related with the income, being lowest in high‐income countries, and highest in low‐ and middle‐income countries. 37 Rather than simply pointing to increased lifespan, we should implement measures leading to a successful ageing and pointing to increased healthspan. 36 This approach could significantly reduce, at one time, the incidence of NCD in all age classes, the related health costs and the individual vulnerability, also increasing the possibility of resilience at a population level. As a result, the intersection of NCD with COVID‐19 pandemic is negatively affecting the well‐being of world population and generating imbalance and disruption of essential national public health services. Such detrimental effects are particularly severe in the case of socio‐economic iniquities, 38 highlighting the role of socio‐economic deprivation in NCD 39 , 40 and of increased individual vulnerability to COVID‐19. 41
Virtually, all factors generating detrimental effects on the quality of ageing (ie, dietary habits, unhealthy lifestyle, economic deprivation, iniquities and inequalities, environmental pollution) are modifiable. This observation paves the way to possible primary prevention measures, likely reducing long‐term vulnerability.
Of note, although individual behaviours (ie, unhealthy diet, smoking, inadequate alcohol consumption, sedentary life) have a marked and well‐known causal role in the onset and progression of NCD, individuals do not have full responsibility in terms of public health. External drivers, in fact, can strongly and negatively influence individual choices. At least three aspects must be considered: i) amid policies generally adopted for tackling wrong individual behaviours, the commercial determinants of health and unsustainable industrial productions largely driving unhealthy behaviours are usually ignored; ii) the detrimental role of the private sector producing harmful commodities remains unconsidered or obscured; iii) policies really useful to reduce health inequalities are lacking. 42 , 43 , 44
5. THE ROLE OF CLIMATE CHANGE AND ENVIRONMENTAL POLLUTION
The complexity of climate change and the related environmental and social consequences can generate a variety of health risks and high economic costs. 45 , 46 , 47 , 48 , 49 NCD are a major part of this scenario since the main drivers of climate change also act as environmental risk factors for NCD. 50 , 51 Data from the Global Burden of Disease reveal that the burden of NCD related to climate progressively increased in the period 1990–2019. 48
Conversely, unhealthy dietary habits, which fuel the global rise in obesity, can contribute per se to the observed climate change. Excessive consumption of energy‐dense foods promotes obesity and generates a huge cost for the world's health system and a substantial ecological cost in relation to the environment. 52 In this respect, the waste of resources, which includes food eaten above physiological can be labelled as ‘metabolic food waste’. Thus, ‘obesogen’ food consumption must be included into practical assessments of ecological impacts of Western lifestyle in the future, since these unnecessary greenhouse emissions have been mostly ignored, so far. When dietary intake corresponding to metabolic food waste is transformed into ecological indexes, animal products display the highest values for carbon emissions. 52 Among the different regions, Europe is responsible for the greatest amount of metabolic food waste (39.2 million tonnes of food), followed by North America—Oceania (32.5 million tonnes), figures, which are around 14 times more than the amount in Sub‐Saharan Africa. 53
The Paris agreement in 2015 aimed to reduce global warming to ‘well below 2°C’, as compared to the pre‐industrial level. However, after 2015 global carbon dioxide emissions continued to increase, with an average rise, at a world level, of +1,23 billion tonnes (+3%) from 2015 to 2019 (source: https://ourworldindata.org). This trend will further worsen the global public health, will increase individual vulnerability in subjects at risk, and will generate a high cost in terms of excess morbidity and mortality. 45
Most of the health risks depend on climatic influences on global food security, on the trend of infectious diseases, on the integrity of the defences against natural disasters (forests, windbreaks, dams, water drainage systems in urban areas), and on the adverse consequences of socio‐economic status, altered social cohesion, migrations and conflicts. 47
As NCD, COVID‐19 pandemic is also linked with environmental harms and with the progressive rise in global temperature. The negative effects of climate change are amplified by the interaction between NCD and socio‐economic factors. The climate suitability for infectious disease transmission has been growing since the 1950s, 45 and the rapid spread of SARS‐CoV‐2 might be secondary to this trend. In fact, SARS‐CoV‐2 is a novel zoonotic coronavirus with a possible origin in bats and a following inter‐species transmission from bats to humans. 54 Climate change might have had a critical role in this process 55 and in the spread of the infection, which could be facilitated by unsustainable urbanization, reduced biodiversity, lack of green areas, habitat destruction, live animal trade, and global hypermobility. 56 , 57 , 58 , 59
Besides the greenhouse gas emissions causing global warming and direct effects on health, the burden of other environmental toxic chemicals released into the environment represents a serious risk factor for NCD. NCD correlate with the concentration of air pollutants 60 , 61 , 62 , 63 and with endocrine‐disrupting chemicals (EDC), 64 , 65 and both factors promote an unhealthy environment, increased individual vulnerability at all age classes, and ultimately generate high health costs.
In the period of 1991–2010, in Europe, NCD represented the 29% of the total contribution to premature mortality linked with the exposure to fine particular matters in the order of 2.5 micrometres—PM2.5 (263,000 premature deaths per year, 95% CI 144,600–386,600). 60 About the 70% of the diseases caused by pollution are NCD, and the burden of disease attributable to environmental pollution is maximal in the presence of socio‐economic deprivation and high vulnerability, as in children, among minorities and marginalized, and in low‐ and middle‐income countries. 62
Endocrine‐disrupting chemicals, on the other hand, generate elevated health costs, which are higher in the USA (more than 2% of gross domestic product) than in Europe (1.28% of gross domestic product). 66 Unequal exposures to toxic chemicals secondary to racial, ethnic and socio‐economic disparities might account for the elevated EDCs‐related burden of disease in the case of socio‐economic deprivation. 67 , 68
In both the short‐ and long term, preliminary evidence indicates that the concentration of air pollutants can negatively affect the clinical outcome in COVID‐19 patients, 69 , 70 , 71 recapitulating close correlations between air quality and COVID‐19 incidence. A Chinese time‐series study showed, in the short term, a direct correlation between COVID‐19 incidence, nitrogen dioxide (NO2), PM2.5 and coarse particular matter in the order of 10 micrometres (PM10) air concentration. 72 Daily concentrations of NO2 and PM2.5 also influence, in the short term, the mortality risk from COVID‐19, in particular in elderly. 73 A study exploring data from 33 European countries showed significant correlations between the air concentration of several pollutants (PM10, PM2.5, ammonia, sulphur dioxide, non‐methane volatile organic compounds, NO2 and greenhouse gas elements) and the cumulative number of COVID‐19 deaths, with strongest correlations showed, in particular, for PM2.5 and nitrogen oxides (NOx). 74 Long‐term exposures to critical air pollution (in particular PM2.5 and Nox) are also linked with morbidity and mortality rates from COVID‐19. 75 , 76 In New York City, a poorer prognosis of COVID‐19 has been shown in subjects living in neighbourhoods with higher ozone (O3) levels. In this case, the link was also present at O3 air levels below Environmental Protection Agency regulatory standards. 77
High concentrations of atmospheric pollutants as PM2,5, PM10, SO2, NO2 can induce inflammation in the lungs, possibly leading to an increased risk of SARS‐CoV‐2 infection. The rapid spread of the pandemic in some Italian regions as Lombardy and Veneto may have depended on air pollution in these areas. 71 , 78 Similar findings have also been reported in Poland. In particular, the Silesian agglomeration, Mazavia and Lesser Poland were highly impacted in the very early phase of COVID‐19 79
The results of previous studies suggest that reducing air pollution might contribute to a decreased burden of disease of COVID‐19 and likely, of future pandemics. On the other hand, the COVID‐19 pandemic has demonstrated that it is concretely possible to obtain a fast reduction of pollution, which is also the main goal of policies aimed to counteract climate change. Notably, the pandemic was associated with a historic drop in greenhouse gas emission during the year 2020, with a significant decrease in global carbon dioxide (CO2) emissions (−8.8%, −1,551 million metric tonnes CO2) in the first half of 2020, as compared to the same period in 2019. 80 Evidence mainly from USA, 81 Europe, 82 , 83 , 84 India 85 and China 86 show that a marked decrease in the concentration of air pollutants has been recorded during the lockdown imposed to contain the spread of the pandemic.
We could not exclude the climate impact and higher temperatures during the pandemic progress. The higher temperature limits transmission of the virus since it promotes aerosol droplets’ drying on which the virus can spread or the sunlight radiation is more important, even. Indeed, mortality due to COVID‐19 decreases in warmer air temperature. 87 The pandemic development from February to May during the first wave of the pandemic inversely correlates with the amount of UVA and UVB radiation. It may suggest a lower number of SARS‐CoV‐2 infections in the northern hemisphere during the summer, with the increased incidence of COVID‐19 in the southern hemisphere during the summer in the southern hemisphere (Brazil). However, even in hot temperatures, monsoon clouds block solar radiation in high humidity tropical countries.
Not everything is, therefore, yet understood, but the lesson from COVID‐19 pandemic clearly demonstrates that nations (especially in developed countries) can, to some extent, successfully and rapidly face a major threat for the humankind, that a fast reduction of air pollution is concretely possible. To reach these goals, improved environmental health, marked abetment in greenhouse emissions and effective international cooperation are achievable in the short term, despite the elevated economic costs.
6. THE SYNDEMIC AS THE OUTCOME
The spread of COVID‐19 pandemic confirms that NCD, climate and environmental threats and socio‐economic inequities and inequalities are not distinct problems. It is logical to address these problems as a unique challenge, which is characterized by multiple and strong inter‐relations, which ultimately increase the individual vulnerability, decrease resilience and raise health and economic costs.
The ongoing pandemic is showing that the major factors characterizing vulnerable groups and markedly affecting public health in the short and in the long term include unhealthy ageing (and not merely the number of aged people), the burden of NCD, the burden of toxic chemicals released into the environment, socio‐economic deprivation, the scarce efficacy of policies to improve public health, and the lack of primary prevention measures. In addition, the spread of SARS‐CoV‐2 infection shows how the pandemic is amplifying pre‐existing criticalities and is rapidly worsening public health worldwide, a kind of ‘Tsunami‐like’ effect.
During the COVID‐19 pandemic, we are insistently reminded that iniquities and inequalities do exist and can further emerge, decreasing the efficiency and the efficacy of all policies and the goals of ameliorating public health. Figure 1 depicts a metropolis in the world characterized by two totally different social areas. COVID‐19 pandemic can hit each area in a totally different way and violence, depending on pre‐existing factors regulating individual vulnerability and possibility of recovery.
FIGURE 1.

Impact of pre‐existing social differences on the outcome of COVID‐19 pandemic. (A) In a given metropolis, the initial event of pandemic can hit two geographical areas, which segregate intrinsic social, economic, structural, health and medical differences. (B) COVID‐19 pandemic has the chance to hit each area in a totally different way and violence since the above‐mentioned differences are important predisposing; (C) the consequences of the pandemic will ultimately depend on the underlying capacity of resilience, which is weaker below ‘the line of poverty’. The ultimate outcome of the pandemic (bringing the concept of ‘syndemic’) will increase the burden of inequalities between the two social realities Source: Mumbai, India (2017), Extreme wealth and opulence exist side by side in India's financial capital, Mumbai. With permission from J. Miller, Unequal Scenes ‐ Mumbai.
The definition of syndemic is ‘an outbreak of disease that spreads quickly and affects many individuals at the same time: an outbreak of epidemic disease’, while pandemic is ‘an outbreak of a disease that occurs over a wide geographic area (such as multiple countries or continents) and typically affects a significant proportion of the population’ (Merriam‐Webster). Thus, the epidemic is a more limited phenomenon, as compared to a pandemic, and COVID‐19 is, therefore, closer to the concept of pandemic than epidemic. For many reasons, therefore, COVID‐19 is not simply a pandemic. 6 Rather, it can be considered one of the possible, multiple expressions of a pre‐existing syndemic. This word was first coined in 2009 by the Anthropologist Merril Singer working at the University of Connecticut, USA. 88 The syndemic or the synergistic epidemic requires the study of both biological and social processes. 89 The research, therefore, develops as a complex, multilevel phenomenon, with aggregation of two or more concurrent or sequential epidemics or disease clusters in a population and with biological interactions. The events related to the syndemic will greatly exacerbate the prognosis and burden of disease. Thus, research on the COVID‐19 pandemic can benefit from a syndemic approach, which is particularly useful to understand vulnerability and the unequal impacts of this public health crisis. 90
Judging COVID‐19 as a syndemic requires a syndemic approach not only to provide an appropriate response to the pandemic but also to limit the risk of further pandemics. In fact, we must consider that NCD as obesity, hypertension, cardiovascular diseases, chronic respiratory diseases and cancer have been spreading across poorer and most vulnerable countries. 6 , 91 Since 2019, the same populations have also become the target of COVID‐19. 91
We must not forget that the effects of COVID‐19 persist beyond the resolution of infection, resulting in a reduced health‐related quality of life (HRQoL). 92 Already the early analyses of groups of individuals with COVID‐19 demonstrated that older age is the main risk factor of mortality, 93 and this was also reported in Germany. 94 Older patients with COVID‐19 need longer time to recover. A recent analysis of patients from Tübingen, one of the districts in Germany that was affected as one of the first ones with COVID‐19, showed that, in patients older than 70 years, almost 30% were not able to return to their home environment, although they were fully sufficient before the infection. 95 Hence, elderly individuals represent a particularly vulnerable group of patients who require a special attention not only during the disease itself but also during the convalescence period, with a special emphasis on rehabilitation.
We ultimately require an integrated approach besides simple basic, clinical and epidemiological interpretations. We must look for cost‐effective interventions, primary prevention measures, social inequalities, environmental health and of course existing NCD.
The COVID‐19 pandemic is showing the worst outcome in the group of the eight highly industrialized nations, in which the 12% of the world population has experienced about one‐third of all COVID‐19 related deaths at a world level. This evidence demonstrates that a great economic power does not fully protect against the health risk linked with the spread of the SARS‐CoV‐2, and points to the need for a decisive change of course in actions and strategies.
To date, the major fuels for the inaction to a global economic transformation have been the fear about a decrease in the Gross Domestic Product (GDP), and the subsequent absence of a convincing and firm exit strategy from fossil fuels. From an economic point of view, what happened during the lockdown confirmed this fear.
Initially (February 1, 2020 ‐ March 15, 2020) only China implemented lockdown measures. According to data collected by Wikipedia (‘national responses to the 2019–20 coronavirus pandemic’), in March 2020 about 1.7 billion people worldwide started a lockdown. In April 2020, this number involved more than half of the world population (3.9 billion people). Starting from these data, it is calculated that the impact of the lockdowns at the peak of the crisis amounts to 9.4% of annual GDP. 96 It is quite important, as the publicly available data from the European Centre for Disease Prevention and Control (ECDC) show a close correlation between GDP per capita and the number of deaths per COVID‐19 per million population in each country. Data indicate that higher GDP, not impacted by COVID‐19, could help fighting COVID‐19 probably by testing more, identifying more cases, offering better treatment options, better healthcare system, and better qualifying COVID‐19 related deaths.
Nevertheless, the spread of the SARS‐CoV‐2 is generating elevated and still uncalculated health costs worldwide. Similarly, an accurate financial analysis revealed that climate change is able to hardly affect the stability of the global banking system, causing an additional fiscal burden of about 5–15% of GDP per year and increasing the public debt/GDP ratio by a factor of 2. 97 Using a syndemic point of view, such high costs must be added to the enormous health costs generated by environmental pollution and by the increasing epidemic of NCD and related disabilities.
Intersection of human rights that comprise the overarching right to well‐being has been well depicted in the framework of Figure 2. The Lancet Commission identifies five interrelated human rights recognised by international law. There is a right to health, food, culture, cultural rights, child rights, and rights to healthy environments ultimately leading to the right to well‐being. 98
FIGURE 2.
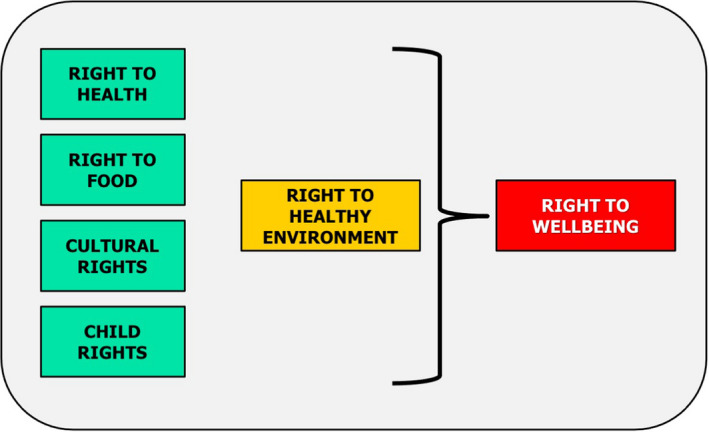
Framework showing the intersection of human rights. The overarching right to well‐being comprises five rights, which contribute to the right to well‐being Adapted from Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, Brinsden H, Calvillo A, De Schutter O, Devarajan R. The global syndemic of obesity, undernutrition and climate change: The Lancet Commission report. 98
Health is the result of a broader prospectus that includes the quality of education (primary to tertiary), economic growth, gender equality and migration policy. 99 According to international human rights standards, the populations have an equal right to the highest attainable standard of physical and mental health. This goal includes access not only to health care, but also to the underlying determinants of good health. 100 The mission is, therefore, to provide health in all policies. By improving health, enhancing living conditions, strengthening the people's capacity, we should increase the mass of healthy people, improve healthy environments, and promote primary prevention. This approach will contribute to prevent the complications related to several diseases, which are highly costly in our population.
Thus, COVID‐19 is a syndemic of viral infection combined with an epidemic of NCD, and both interact on a social substrate of poverty and inequality and in a scenario strongly characterized by an unhealthy environment.
The winning policy is to tackle such structural criticalities to protect fragile populations from future infectious outbreaks 99 but also to guarantee the respect of fundamental human rights.
At a higher level, we need to face COVID‐19 syndemic by holistic approach encompassing education, employment, housing, food, environmental health and economical issues looking at inequalities and poverty.
In the framework of health sciences, we have to move up from individuals to population 101 to depict a complex, multilevel phenomenon, which ultimately must help policymakers and program implementers in their endeavours to improve the global health. In this respect, different levels of interaction include governance (with policies, economics, and social norms), systems (which include food, transport, land use and urban design, environments, social determinants), and outcomes. The latter step includes the box of global syndemic grouping aspects related to climate changes, food supply, malnutrition, developmental Origins of Health and Disease, obesity (Figure 3). 98
FIGURE 3.
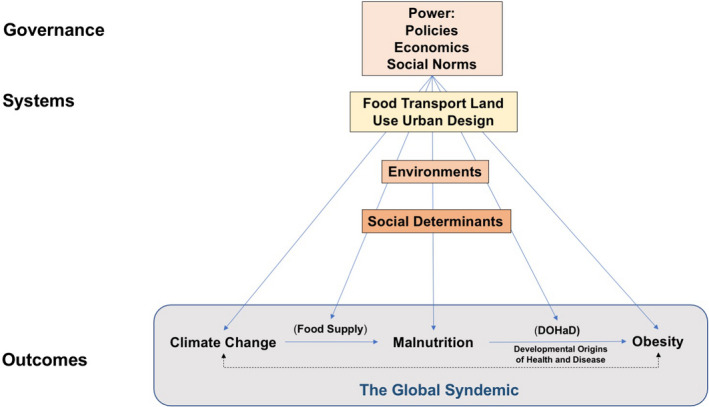
Factors contributing to the modulation of global syndemic. The factors group under three essential steps, which involve governance, systems, and outcomes Adapted from Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, Brinsden H, Calvillo A, De Schutter O, Devarajan R. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. 98
Following the COVID‐19 syndemic, we shall not contribute to generate a society poorer in economics, environment and overall health. Recent observations suggest that socio‐economic inequalities in severe COVID‐19 are largely avoidable, as documented by the Hong Kong case. In that area, there was no significant association between the area‐level income‐poverty rate with severe COVID‐19. Thus, the socio‐economic patterning of severe COVID‐19 was mild in Hong Kong. 102
7. CONCLUSIONS
Since 2019, the SARS‐CoV‐2 pandemic is spreading across the world on the top of ongoing NCD. This tragic combination of events has made us discover the capacity of resilience, the syndemic aspects occurring worldwide, emphasizing the role of existing inequalities and of environmental criticalities. In this scenario, there is a high risk of accumulating unhealthy populations living in unhealthy environments and generating unhealthy offspring.
We urge to awake the conscience about the global themes, and the concepts of resilience and syndemic, approaching appropriate policies. This mission must reach the soul of young doctors and scientists as well and must start now because it will soon be too late. We must be prepared to face emerging global medical aspects, against the background of environmental and social factors.
CONFLICT OF INTEREST
None to declare.
ACKNOWLEDGEMENT
This review is partly based on the lecture given to the 55th Annual Scientific Meeting of European Society for Clinical Investigation, Webinar edition, 9‐11 June 2021. P. Portincasa is member of the Apulian Academy of Sciences and recipient of the "Albert Struyvenberg" ESCI Medal (2018). A. Di Ciaula is member of the International Society of Doctors for Environment (ISDE), Arezzo, Italy.
Di Ciaula A, Krawczyk M, Filipiak KJ, Geier A, Bonfrate L, Portincasa P. Noncommunicable diseases, climate change and iniquities: What COVID‐19 has taught us about syndemic. Eur J Clin Invest. 2021;51:e13682. doi: 10.1111/eci.13682
REFERENCES
- 1. World Health Organization . Coronavirus Disease 2019 (COVID 19). Situation Report. World Health Organization; 2020. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/situation‐reports [Google Scholar]
- 2. World Health Organization . Coronavirus disease (COVID‐19) Pandemic, Vol. 2020. World Health Organization; 2020. https://www.who.int/publications/m/item/weekly‐epidemiological‐update‐on‐covid‐19‐‐‐21‐september‐2021 [Google Scholar]
- 3. European Centre for Disease Prevention and Control . Novel Coronavirus in China. European Centre for Disease Prevention and Control; 2020. https://www.ecdc.europa.eu/en/covid‐19 [Google Scholar]
- 4. NCD Risk Factor Collaboration (NCD‐RisC) . Worldwide trends in body‐mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population‐based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017;390:2627‐2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. WHO Coronavirus (COVID‐19) Dashboard. https://covid19.who.int/. 2021. [Google Scholar]
- 6. Horton R. Offline: COVID‐19 is not a pandemic. Lancet (London, England). 2020;396:874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Simera I, Moher D, Hoey J, Schulz KF, Altman DG. A catalogue of reporting guidelines for health research. Eur J Clin Invest. 2010;40:35‐53. [DOI] [PubMed] [Google Scholar]
- 8. Merriam‐Webster Dictionary . Definition of resilience. 2021. https://www.merriam‐webster.com/dictionary/resilience Accessed September 26, 2021.
- 9. Di Ciaula A, Palmieri VO, Migliore G, Portincasa P and Group IMC . COVID‐19, internists and resilience: the north‐south Italy outbreak. Eur J Clin Invest. 2020;50:e13299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Armitage R, Nellums LB. COVID‐19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5:e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Armstrong K. Covid‐19 and the investigator pipeline. N Engl J Med. 2021;385:7‐9. [DOI] [PubMed] [Google Scholar]
- 12. Zhu W, Fang Y, Bai ZL, Li NN, Zhao JY, Hu Z. Effect of emerging major infectious diseases on sleep quality of medical workers: findings from medical workers providing support during the COVID‐19 pandemic. Med Sci Monit. 2021;27:e931881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Portincasa P, Krawczyk M, Machill A, Lammert F, Di Ciaula A. Hepatic consequences of COVID‐19 infection. lapping or biting? Eur J Intern Med. 2020;77:18‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Portincasa P, Krawczyk M, Smyk W, Lammert F, Di Ciaula A. COVID‐19 and non‐alcoholic fatty liver disease: Two intersecting pandemics. Eur J Clin Invest. 2020;50:e13338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smyk W, Janik MK, Portincasa P, Milkiewicz P, Lammert F, Krawczyk M. COVID‐19: focus on the lungs but do not forget the gastrointestinal tract. Eur J Clin Invest. 2020;50:e13276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shanmugam H, Di Ciaula A, Di Palo DM, et al. Multiplying effects of COVID‐19 lockdown on metabolic risk and fatty liver. Eur J Clin Invest. 2021;51:e13597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Loconsole D, Passerini F, Palmieri VO, et al. Recurrence of COVID‐19 after recovery: a case report from Italy. Infection. 2020;48:965‐967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baj J, Karakula‐Juchnowicz H, Teresinski G, et al. COVID‐19: Specific and non‐specific clinical manifestations and symptoms: the current state of knowledge. J Clin Med. 2020;9:1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stella A, Lamkanfi M, Portincasa P. Familial Mediterranean fever and COVID‐19: friends or foes? Front Immunol. 2020;11: 574593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Iannuzzi L, Salzo AE, Angarano G, et al. Gaining back what is lost: recovering the sense of smell in mild to moderate patients after COVID‐19. Chem Senses. 2020;45:875‐881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen YY, Assefa Y. The heterogeneity of the COVID‐19 pandemic and national responses: an explanatory mixed‐methods study. BMC Public Health. 2021;21:835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Buicu AL, Cernea S, Benedek I, Buicu CF, Benedek T. Systemic inflammation and COVID‐19 mortality in patients with major noncommunicable diseases: chronic coronary syndromes, diabetes and obesity. J Clin Med. 2021;10:1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Murillo‐Zamora E, Hernandez‐Suarez CM. Survival in adult inpatients with COVID‐19. Public Health. 2021;190:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Paltrinieri S, Bressi B, Costi S, et al. Beyond lockdown: the potential side effects of the SARS‐CoV‐2 pandemic on public health. Nutrients. 2021;13:1600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Palmer K, Monaco A, Kivipelto M, et al. The potential long‐term impact of the COVID‐19 outbreak on patients with non‐communicable diseases in Europe: consequences for healthy ageing. Aging Clin Exp Res. 2020;32:1189‐1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McDonald LT. Healing after COVID‐19: are survivors at risk for pulmonary fibrosis? Am J Physiol Lung Cell Mol Physiol. 2021;320:L257‐L265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Maniscalco M, Ambrosino P, Fuschillo S, et al. Bronchodilator reversibility testing in post‐COVID‐19 patients undergoing pulmonary rehabilitation. Respir Med. 2021;182:106401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Saeed S, Tadic M, Larsen TH, Grassi G, Mancia G. Coronavirus disease 2019 and cardiovascular complications: focused clinical review. J Hypertens. 2021;39:1282‐1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mitrani RD, Dabas N, Goldberger JJ. COVID‐19 cardiac injury: implications for long‐term surveillance and outcomes in survivors. Heart Rhythm. 2020;17:1984‐1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Miners S, Kehoe PG, Love S. Cognitive impact of COVID‐19: looking beyond the short term. Alzheimers Res Ther. 2020;12:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Park HY, Park WB, Lee SH, et al. Posttraumatic stress disorder and depression of survivors 12 months after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health. 2020;20:605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Drozd M, Pujades‐Rodriguez M, Lillie PJ, et al. Non‐communicable disease, sociodemographic factors, and risk of death from infection: a UK Biobank observational cohort study. Lancet Infect Dis. 2021;21:1184–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Clark A, Jit M, Warren‐Gash C, et al. Global, regional, and national estimates of the population at increased risk of severe COVID‐19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8:e1003‐e1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wyper GMA, Assuncao R, Cuschieri S, et al. Population vulnerability to COVID‐19 in Europe: a burden of disease analysis. Arch Public Health. 2020;78:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pranata R, Henrina J, Lim MA, et al. Clinical frailty scale and mortality in COVID‐19: A systematic review and dose‐response meta‐analysis. Arch Gerontol Geriatr. 2021;93:104324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Di Ciaula A, Portincasa P. The environment as a determinant of successful aging or frailty. Mech Ageing Dev. 2020;188:111244. [DOI] [PubMed] [Google Scholar]
- 37. NCD Countdown collaborators . NCD Countdown 2030: pathways to achieving Sustainable Development Goal target 3.4. Lancet. 2020;396:918‐934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gutierrez JP, Bertozzi SM. Non‐communicable diseases and inequalities increase risk of death among COVID‐19 patients in Mexico. PLoS One. 2020;15:e0240394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mendenhall E, Kohrt BA, Norris SA, Ndetei D, Prabhakaran D. Non‐communicable disease syndemics: poverty, depression, and diabetes among low‐income populations. Lancet. 2017;389:951‐963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. NCD Countdown collaborators . NCD Countdown 2030: worldwide trends in non‐communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392:1072‐1088. [DOI] [PubMed] [Google Scholar]
- 41. Patel JA, Nielsen FBH, Badiani AA, et al. Poverty, inequality and COVID‐19: the forgotten vulnerable. Public Health. 2020;183:110‐111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kriznik NM, Kinmonth AL, Ling T, Kelly MP. Moving beyond individual choice in policies to reduce health inequalities: the integration of dynamic with individual explanations. J Public Health (Oxf). 2018;40:764‐775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Medicine. 2012;9:e1001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Maani N, Collin J, Friel S, et al. Bringing the commercial determinants of health out of the shadows: a review of how the commercial determinants are represented in conceptual frameworks. Eur J Public Health. 2020;30:660‐664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Butler CD, Harley D. Primary, secondary and tertiary effects of eco‐climatic change: the medical response. Postgrad Med J. 2010;86:230‐234. [DOI] [PubMed] [Google Scholar]
- 47. McMichael AJ. Globalization, climate change, and human health. N Engl J Med. 2013;369:96. [DOI] [PubMed] [Google Scholar]
- 48. Song J, Pan R, Yi W, et al. Ambient high temperature exposure and global disease burden during 1990–2019: an analysis of the Global Burden of Disease Study 2019. Sci Total Environ. 2021;787:147540. [DOI] [PubMed] [Google Scholar]
- 49. Watts N, Amann M, Arnell N, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836‐1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Frumkin H, Haines A. Global environmental change and noncommunicable disease risks. Annu Rev Public Health. 2019;40:261‐282. [DOI] [PubMed] [Google Scholar]
- 51. Lancet Oncology . Climate change and non‐communicable diseases. Lancet Oncol. 2016;17:1. 10.1016/S470-2045(15)00568-9. [DOI] [PubMed] [Google Scholar]
- 52. Serafini M, Toti E. Unsustainability of obesity: metabolic food waste. Front Nutr. 2016;3:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Toti E, Di Mattia C, Serafini M. Metabolic food waste and ecological impact of obesity in FAO World's region. Front Nutr. 2019;6:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270‐273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Beyer RM, Manica A, Mora C. Shifts in global bat diversity suggest a possible role of climate change in the emergence of SARS‐CoV‐1 and SARS‐CoV‐2. Sci Total Environ. 2021;767:145413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lorenz C, de Oliveira LM, Chiaravalloti‐Neto F. Deforestation hotspots, climate crisis, and the perfect scenario for the next epidemic: The Amazon time bomb. Sci Total Environ. 2021;783:147090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Wu X, Yin J, Li C, Xiang H, Lv M, Guo Z. Natural and human environment interactively drive spread pattern of COVID‐19: A city‐level modeling study in China. Sci Total Environ. 2021;756:143343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Barouki R, Kogevinas M, Audouze K, et al. The COVID‐19 pandemic and global environmental change: emerging research needs. Environ Int. 2021;146:106272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Lin S, Fu Y, Jia X, Ding S, Wu Y, Huang Z. Discovering correlations between the COVID‐19 epidemic spread and climate. Int J Environ Res Public Health. 2020;17(21):7958‐7971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tarin‐Carrasco P, Im U, Geels C, Palacios‐Pena L, Jimenez‐Guerrero P. Contribution of fine particulate matter to present and future premature mortality over Europe: a non‐linear response. Environ Int. 2021;153:106517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Schraufnagel DE, Balmes JR, Cowl CT, et al. Air pollution and noncommunicable diseases: a review by the forum of International Respiratory Societies’ Environmental Committee, Part 2: Air Pollution and Organ Systems. Chest. 2019;155:417‐426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Landrigan PJ, Fuller R, Acosta NJR, et al. The Lancet Commission on pollution and health. Lancet. 2018;391:462‐512. [DOI] [PubMed] [Google Scholar]
- 63. Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204‐1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. EDCs: regulation still lagging behind evidence. Lancet Diabetes Endocrinol. 2019;7:325. 10.1016/S2213-8587(19)30114-7. [DOI] [PubMed] [Google Scholar]
- 65. Zarean M, Poursafa P. The role of environmental disruptor chemicals in the development of non communicable disease. Adv Exp Med Biol. 2019;1121:21‐31. [DOI] [PubMed] [Google Scholar]
- 66. Attina TM, Hauser R, Sathyanarayana S, et al. Exposure to endocrine‐disrupting chemicals in the USA: a population‐based disease burden and cost analysis. Lancet Diabetes Endocrinol. 2016;4:996‐1003. [DOI] [PubMed] [Google Scholar]
- 67. Attina TM, Malits J, Naidu M, Trasande L. Racial/ethnic disparities in disease burden and costs related to exposure to endocrine‐disrupting chemicals in the United States: an exploratory analysis. J Clin Epidemiol. 2019;108:34‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ruiz D, Becerra M, Jagai JS, Ard K, Sargis RM. Disparities in environmental exposures to endocrine‐disrupting chemicals and diabetes risk in vulnerable populations. Diabetes Care. 2018;41:193‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Woodby B, Arnold MM, Valacchi G. SARS‐CoV‐2 infection, COVID‐19 pathogenesis, and exposure to air pollution: What is the connection? Ann N Y Acad Sci. 2021;1486:15‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Bowe B, Xie Y, Gibson AK, et al. Ambient fine particulate matter air pollution and the risk of hospitalization among COVID‐19 positive individuals: cohort study. Environ Int. 2021;154:106564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ho CC, Hung SC, Ho WC. Effects of short‐ and long‐term exposure to atmospheric pollution on COVID‐19 risk and fatality: analysis of the first epidemic wave in northern Italy. Environ Res. 2021;199:111293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Li H, Xu XL, Dai DW, Huang ZY, Ma Z, Guan YJ. Air pollution and temperature are associated with increased COVID‐19 incidence: a time series study. Int J Infect Dis. 2020;97:278‐282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Dales R, Blanco‐Vidal C, Romero‐Meza R, Schoen S, Lukina A, Cakmak S. The association between air pollution and COVID‐19 related mortality in Santiago, Chile: a daily time series analysis. Environ Res. 2021;198:111284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lembo R, Landoni G, Cianfanelli L, Frontera A. Air pollutants and SARS‐CoV‐2 in 33 European countries. Acta Biomed. 2021;92:e2021166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Barnett‐Itzhaki Z, Levi A. Effects of chronic exposure to ambient air pollutants on COVID‐19 morbidity and mortality – a lesson from OECD countries. Environ Res. 2021;195:110723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Hou CK, Qin YF, Wang G, Liu QL, Yang XY, Wang H. Impact of a long‐term air pollution exposure on the case fatality rate of COVID‐19 patients‐A multicity study. J Med Virol. 2021;93:2938‐2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Kim H, Bell ML. Air pollution and COVID‐19 mortality in New York City. Am J Respir Crit Care Med. 2021;204:97‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Stufano A, Lisco S, Bartolomeo N, et al. COVID19 outbreak in Lombardy, Italy: An analysis on the short‐term relationship between air pollution, climatic factors and the susceptibility to SARS‐CoV‐2 infection. Environ Res. 2021;198:111197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Jurgiel J, Dzieciątkowski T, Szarpak Ł, Filipiak KJ. What have we learned about COVID‐19 in 2020? 10 hypotheses explaining the differences in ncidence and mortality from COVID‐19 between countries. Folia Cardiologica. 2021;16:1‐19. [Google Scholar]
- 80. Liu Z, Ciais P, Deng Z, et al. Near‐real‐time monitoring of global CO2 emissions reveals the effects of the COVID‐19 pandemic. Nat Commun. 2020;11:5172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Berman JD, Ebisu K. Changes in U.S. air pollution during the COVID‐19 pandemic. Sci Total Environ. 2020;739:139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Baldasano JM. COVID‐19 lockdown effects on air quality by NO2 in the cities of Barcelona and Madrid (Spain). Sci Total Environ. 2020;741: 140353. [DOI] [PubMed] [Google Scholar]
- 83. Collivignarelli MC, De Rose C, Abba A, et al. Analysis of lockdown for CoViD‐19 impact on NO2 in London, Milan and Paris: What lesson can be learnt? Process Saf Environ Prot. 2021;146:952‐960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Giani P, Castruccio S, Anav A, Howard D, Hu W, Crippa P. Short‐term and long‐term health impacts of air pollution reductions from COVID‐19 lockdowns in China and Europe: a modelling study. Lancet Planet Health. 2020;4:e474‐e482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Singh V, Singh S, Biswal A, Kesarkar AP, Mor S, Ravindra K. Diurnal and temporal changes in air pollution during COVID‐19 strict lockdown over different regions of India. Environ Pollut. 2020;266:115368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Fan Z, Zhan Q, Yang C, Liu H, Zhan M. How did distribution patterns of particulate matter air pollution (PM2.5 and PM10) change in China during the COVID‐19 outbreak: a spatiotemporal investigation at Chinese city‐level. Int J Environ Res Public Health. 2020;17:6274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Quilodran CS, Currat M, Montoya‐Burgos JI. Air temperature influences early Covid‐19 outbreak as indicated by worldwide mortality. Sci Total Environ. 2021;792:148312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Singer M. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health. Jossey‐Bass, San Francisco; 1990. [Google Scholar]
- 89. Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio‐social context. Med Anthropol Q. 2003;17:423‐441. [DOI] [PubMed] [Google Scholar]
- 90. Pirrone I, Dieleman M, Reis R, Pell C. Syndemic contexts: findings from a review of research on non‐communicable diseases and interviews with experts. Glob Health Action. 2021;14:1927332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Huizar MI, Arena R, Laddu DR. The global food syndemic: the impact of food insecurity, Malnutrition and obesity on the healthspan amid the COVID‐19 pandemic. Prog Cardiovasc Dis. 2021;64:105‐107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Rajkumar K, Klingshorn P, Chedrese PJ, Murphy BD. Prolactin, LH, and estradiol‐17 beta in utilization of lipoprotein substrate by porcine granulosa cells in vitro. Can J Physiol Pharmacol. 1988;66:561‐566. [DOI] [PubMed] [Google Scholar]
- 93. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934‐943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Karagiannidis C, Mostert C, Hentschker C, et al. Case characteristics, resource use, and outcomes of 10 021 patients with COVID‐19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8:853‐862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Herrmann ML, Hahn JM, Walter‐Frank B, et al. COVID‐19 in persons aged 70+ in an early affected German district: risk factors, mortality and post‐COVID care needs‐A retrospective observational study of hospitalized and non‐hospitalized patients. PLoS One. 2021;16:e0253154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Mandel A, Veetil V. The economic cost of COVID lockdowns: an out‐of‐equilibrium analysis. Econ Disaster Clim Chang. 2020;1‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Lamperti F, Bosetti V, Roventini A, Tavoni M. The public costs of climate‐induced financial instability. Nat Clim Chang. 2019;9:829‐833. [Google Scholar]
- 98. Swinburn BA, Kraak VI, Allender S, et al. The global syndemic of obesity, undernutrition, and climate change: the lancet commission report. Lancet. 2019;393:791‐846. [DOI] [PubMed] [Google Scholar]
- 99. Lancet T. Global health: time for radical change? Lancet (London, England). 2020;396:1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Willen SS, Knipper M, Abadia‐Barrero CE, Davidovitch N. Syndemic vulnerability and the right to health. Lancet. 2017;389(10072):964‐977. [DOI] [PubMed] [Google Scholar]
- 101. Tsai AC, Mendenhall E, Trostle JA, Kawachi I. Co‐occurring epidemics, syndemics, and population health. Lancet. 2017;389:978‐982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Chung GK, Chan SM, Chan YH, et al. Differential impacts of multimorbidity on COVID‐19 severity across the socioeconomic ladder in Hong Kong: a syndemic perspective. Int J Environ Res Public Health. 2021;18:8168. [DOI] [PMC free article] [PubMed] [Google Scholar]


