Abstract
During the COVID‐19 pandemic, adolescents’ typical social support systems have been disrupted. The present study examined adolescent adjustment during the pandemic (summer, 2020) while controlling for pre‐pandemic adjustment (2017–2018) in 170 youth (ages 12–20) from Missouri and Florida. We also examined whether positive and negative relationship qualities with four close others (i.e., mothers, fathers, siblings, and best friends) interacted with COVID‐related stress to impact adolescent adjustment. In general, we found that close relationships impacted adolescent adjustment in expected directions (i.e., positive relationships better for adjustment, negative relationships more detrimental), but while mothers and fathers impacted adolescent adjustment in largely similar ways to pre‐pandemic studies, influences of relationships with best friends and sibling were more impacted by COVID‐related stress.
Even in the most typical and positive of contexts, adolescence can be a particularly stressful developmental period given the large number physical, social, and cognitive changes taking place simultaneously. Research also indicates that adolescents are more likely to be highly reactive to stress due to hormonal and brain development changes (Romeo, 2013). It should be no surprise, then, that research on the effects of previous pandemics, such as H1N1, reveal that adolescents are further negatively impacted by stressors and changes resulting from the pandemic (Murray, 2009). These negative outcomes include increased anxiety, depression, mood swings, anger, and involvement in risky and maladaptive coping behaviors (Murray, 2009). This is particularly concerning given that many behavioral and mood disorders also first emerge during adolescence (Kessler et al., 2001; Merikangas et al., 2010). Therefore, the combination of typical stressors with the additional stressors of COVID‐19 may interact with pre‐existing vulnerabilities to produce even higher levels of stress and reduced mental health for adolescents (Alloy & Abramson, 2007). Importantly, theorists identify social support as an important aspect of the stress process (Pearlin, Menaghan, Lieberman, & Mullan, 1981). Social support serves as a key buffer against stress and the subsequent development of emotional and behavioral problems during adolescence (Cheng et al., 2014; Possel et al., 2018). It does so both directly, as well as through promoting more adaptive coping responses (Calvete & Connor‐Smith, 2006; Holahan, Valentiner, & Moos, 1995). During the current COVID‐19 pandemic, however, adolescents’ schools and activities have been closed or significantly reduced, thus limiting adolescents’ social connections with peers, while family members became primary companions. Therefore, the present study examined whether relationship qualities with close others buffered or exacerbated behavioral and adjustment problems during the pandemic (while controlling for pre‐pandemic adjustment), and whether COVID‐19‐related stress moderated this association.
Importance of Close Relationships During Adolescence
Social relational theoretical models (Collins & Laursen, 1992; Hartup & Laursen, 1993) typically note that while there is fair degree of developmental continuity across close relationships, the functions and processes of these relationships typically change over the course of adolescence. While parents are considered primary socialization sources earlier in childhood (Maccoby, 1994), and siblings are typically youth’s primary out‐of‐school companions during childhood and often up through early adolescence (McHale & Crouter, 1996), adolescents begin to strive for greater independence from family members in an effort to assert their developing autonomy (Steinberg, 1990). Such autonomy assertion typically reveals itself in the form of increased conflict with parents (Laursen, Coy, & Collins, 1998) and siblings (Kim, McHale, Osgood, & Crouter, 2006). Additionally, adolescents start to seek‐out peers as their primary sources of social support; first, with close friends, and later, with romantic partners (Furman & Buhrmester, 1992). Across adolescence, however, mothers and best friends are similarly and consistently rated by adolescents as being the most frequent providers of social support, while mothers and siblings are engaged in the greatest amount of conflict (Furman & Buhrmester, 1992).
Despite these differences and transitions taking place throughout adolescence, all of these close, important relationships have been previously shown (1) to engage in both positive (e.g., affection, intimacy, support) and negative (e.g., conflict, criticism, antagonism) processes or qualities, and (2) show unique associations with adolescent adjustment and well‐being. Adams and Laursen (2007) found that negative relationship qualities with mothers and fathers were associated overtime with greater anxiety, depression, and delinquency, while positive relationship qualities with mothers and fathers were associated overtime with less anxiety, depression, and delinquency. Conflict and negativity with siblings have been found to negatively impact youth adjustment and psychopathology over and above similar relationships with parents (Dirks, Persram, Recchia, & Howe, 2015), while close and positive sibling relationships have found across several studies to be protective against internalizing and externalizing symptoms (Buist, Dekovic, & Prinzie, 2013). Similarly, recent meta‐analytic findings indicate that positive relationship quality with friends is related to lower symptoms of loneliness and depression, whereas negative features of friendship, such as conflict, are related to greater loneliness and depressive symptoms (Schwartz‐Mette, Shankman, Dueweke, Borowski, & Rose, 2020). While the research on direction of effects between positive and negative relationships qualities with these important close relationships is usually clear under typical contexts, what is less understood is how these relationships have functioned during the pandemic. Theorists have long noted the important role that social support plays in the stress process (Pearlin et al., 1981), but risk and resilience theorists also note that close relationships, such as those with family members, can be both protective or risky, depending on the context (Masten, 2018).
During the COVID‐19 pandemic, and particularly early‐on during stay‐at‐home orders, adolescents were typically less able to utilize their preferred sources of in‐person social support, namely peers. With this change, for many adolescents, family members became more central companions and sources of support for adolescents. Parents certainly play a crucial role in providing support during times of stress, and the way they respond to adolescent distress has been shown to affect adolescent adjustment following acute stressful situations like 9/11 (Gil‐Rivas, Silver, Holman, McIntosh, & Poulin, 2007) and more generally (Eisenberg et al., 1999). The role of siblings, though, should not be overlooked. Interactions with siblings may be particularly salient during the COVID‐19 pandemic. For many adolescents, siblings served as the only “peers” consistently present in‐person in their daily lives, and they may help one another cope with stress from the pandemic. Older siblings have been shown to serve as role models and significant sources of support and advice (Killoren & Roach, 2014; Tucker, Barber, & Eccles, 1997); however, as sibling relationships become more egalitarian and less hierarchical with age during adolescence, younger siblings also may be able to serve in a supportive role. Further, high‐quality sibling relationships have been found to be protective against family‐wide stressors and during stressful life events (Gass, Jenkins, & Dunn, 2007; Waite, Shanahan, Calkins, Keane, & O’Brien, 2011).
Although adolescents were much less likely to have in‐person interactions with friends during the early stages of the COVID‐19 pandemic, synchronous and asynchronous communication technologies can be useful in helping youth maintain relationships and provide outlets for disclosure when close relationship partners are not physically present (Lindell, Campione‐Barr, & Killoren, 2015). Therefore, friends may have continued to serve as important sources of support even when there was not face‐to‐face contact. This is important given that youth increasingly turn to friends for support during adolescence (Furman & Rose, 2015). Notably, though, there is likely considerable variation in youths’ virtual access to friends.
Pandemic Stress and Adolescent Adjustment
While research on youth emotional and behavioral adjustment during the pandemic is still emerging, recent research suggests that, on average, adjustment problems increased. Comparisons in China from pre‐pandemic rates of youth depression and anxiety, revealed higher rates of youth depression and anxiety during the pandemic than expected (Duan et al., 2020; Xie et al., 2020). Longitudinal studies of youth in Australia (Magson et al., 2021), as well as one examining youth from 12 different samples across the United States, Europe, and South America (Berendese et al., under review), have found increases in depression and anxiety in adolescents from pre‐pandemic to during the pandemic. Lacking in the literature so far, however, is the examination of factors that may protect against these increases in adjustment problems, as well as those that might exacerbate these difficulties. Positive and negative relationship qualities with close others are likely factors that could contribute.
In considering the impact of the pandemic on adolescent adjustment, taking into account pre‐pandemic adjustment is critical. Of course, prior to the COVID‐19 pandemic, adolescents ranged widely in terms of their emotional (e.g., depressive and anxiety symptoms) and behavioral (e.g., risky or problematic behaviors) adjustment. Accordingly, statistically controlling for pre‐pandemic adjustment was necessary in order to explore relative (residualized) changes in youth adjustment overtime (Castro‐Schilo & Grimm, 2017). Moreover, prevalence rates of some adjustment problems in adolescents, such as depression, have been increasing over the last couple of decades (Mojtabai, Olfson, & Han, 2016), even prior to the pandemic. Controlling for pre‐pandemic adjustment also is important for detecting changes in adjustment that are driven by experiencing the pandemic as opposed to more general cohort trends over time. In order to account for this in the present study, we followed up two samples of adolescents we had previously examined emotional and behavioral adjustment in 2017–2018.
The Present Study
Adolescents use their close relationships with mothers, fathers, siblings, and best friends, in different ways and for different functions. The COVID‐19 pandemic has caused some shifts in the frequency, opportunities, and ways that adolescents engage in positive and negative relationship processes with these close relationship partners. Additionally, the stress of the pandemic (e.g., economic instability, social isolation, fear of illness) appears to negatively impact the emotional and behavioral adjustment of adolescents (Berendese et al., under review; Magson et al., 2021) when compared to pre‐pandemic adjustment levels. Therefore, the present study had two primary goals: (1) to examine the associations between adolescents’ perceptions of positive and negative relationship qualities across four important close relationship partners on adolescent adjustment during the pandemic (controlling for pre‐pandemic adjustment), and (2) to examine the moderating role of COVID‐related stress on this association. Generally, we hypothesized that positive relationship qualities would be associated with better (more positive) adolescent adjustment and negative relationship qualities would be associated with worse (more problematic) adolescent adjustment. However, given the salience of friends during adolescence, and the enduring influence of mothers, particularly with regards to both serving as primary sources of social support (Furman & Buhrmester, 1992), we hypothesized that those relationships would be particularly influential on adolescent adjustment during this time. Additionally, we predicted that COVID‐related stress would moderate the association between relationship qualities and emotional and behavioral outcomes, such that there would be a stronger association for negative relationship qualities and poorer outcomes, and a weaker association for positive relationship qualities and better adjustment.
Method
Participants
Time 1 data (pre‐pandemic) were collected during 2017–2018 as part of two separate and larger studies in Central Missouri and Southern Florida, and in June and July of 2020 (Time 2; during pandemic), participants from these studies were contacted again to participate in a study of adolescent coping during the pandemic. The original (Time 1) sample consisted of 244 youth from Missouri (M age = 13.71, SD = 1.66, 48% female, 68% White, 17% African American, 11% Latinx, 4.9% American Indian/Alaska Native, 3.7% Asian, 2.9% Hawaiian/Pacific Islander, and 6.1% another race or multi‐racial; median family income range = $70,000–$84,999) and 123 youth from Florida (M age = 13.99, SD = 1.58, 54% female, 53% White, 29% African American, 12% Latinx; M family income = $55,000/year). At Time 2, 36% of the original Missouri sample and 42% of the original Florida sample agreed to participate (141 youth); an additional 29 siblings of youth in the original Florida sample also participated at Time 2 in order to make the number of sibling constellations more comparable across samples. Across both samples, non‐attritted participants were older and more likely to be White, with more well‐educated parents and a higher overall family income. The final sample of adolescents who participated at Time 2 consisted of 170 youth (89 from Missouri; 81 from Florida) who were approximately half female (n = 86) and half male (n = 82); two participants did not identify as female or male. At the time of data collection during the pandemic, participants ranged in age from 12 to 20 years, with a mean age of 16.21 years old (SD = 1.95). The sample was predominately European American (80%), with 14% African American and <5% each Asian American, American Indian/Alaskan Native, and Hawaiian/Pacific Islander. Approximately 10% of the sample identified as Latinx. Mean family income was $70,000–$79,000/year (15% made <$40,000/year; 34% made more than $100,000/year) and 80% of the sample had at least one parent with a four‐year college degree or more.
Some of the participants are siblings (67 pairs) because the original Missouri study involved families with multiple adolescents, and the Florida study was expanded to include siblings during COVID‐19 data collection. Another 36 participants did not have siblings in the sample. Siblings who participated were required to include the first‐born and a second‐born no more than 5 years younger. If more than two children were in the household (<25% of the original Missouri sample), only the oldest two siblings were included in the study and youth were only asked to report on the sibling who participated (or first‐born or second‐born in their family if their sibling did not participate). We controlled for non‐independence of data by clustering participants within families using the “Type = Complex” specification in Mplus, which computes standard errors and chi‐square tests of model fit taking into account non‐independence of observations due to cluster sampling (Muthén & Muthén, 2017). We did not specify separate models at the within‐ versus between‐family level, however, as adolescents in the sample were answering questions about a wide range of relationships both inside and outside of the family and predicting family‐level differences was not the study focus.
Procedures
Participants were originally part of two larger studies of adolescents (Campione‐Barr et al., 2019; Rote et al., 2021). Recruitment for the larger studies involved flyers, mailings, and school contacts. Youth adjustment measures were assessed as part of the larger studies (Time 1; collected between June 2017 and December 2018) as well as during the pandemic (Time 2; June/July 2020), while relationship measures and COVID‐19‐related stress measures were assessed only at Time 2. Original participants from the larger studies were invited to participate in the current research. Adolescents who agreed to participate and received electronic consent from parents (if under age 18), responded to surveys online via the Qualtrics platform.
Measures
Relationship quality
At Time 2 (during pandemic), all youth completed the Network of Relationships Inventory (NRI; Furman & Buhrmester, 1985) to assess relationship quality with mothers, fathers, siblings, and best friends. The entire measure consists of 39 items across 13 sub‐scales, although previous research has found that these sub‐scales best combine into three categories: positivity/support, negativity, and relative power (Adams & Laursen, 2007). For the present study, relationship positivity (18 items regarding affection, companionship, instrumental aid, intimacy, nurturance, reliable alliance, support, and admiration), and relationship negativity (nine items regarding conflict, criticism, and antagonism) were utilized for each of the close relationships assessed. All items were scored on a five‐point Likert scale from 1 (little or none) to 5 (the most). Mean scores for positivity and negativity with each relationship partner were utilized in analyses, and internal consistency was high among all relationships (α = .91–.96).
Anxiety symptoms
Before the pandemic (Time 1; 2017/2018), participants reported on their anxiety symptoms. However, different measures were used at the two different sites. Participants in the Missouri sample responded to the 28‐item Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1978), which is the same measure used for the combined sample during the pandemic (Time 2; June/July 2020). Items were rated on a Likert scale from 1 (not at all true of yourself) to 5 (really true of yourself). Mean scores at each time point were used, with higher scores indicating greater anxiety. Participants in the Florida sample responded to the Anxiety subscale of the Depression Anxiety Stress Scale (DASS; Lovibond & Lovibond, 1995) at Time 1. The seven items of the subscale were rated on a 0 (Did not apply to me at all) to 3 (Applied to me very much, or most of the time) scale. Scores were the average of these items (Time 1 α = .78). Of the full sample, 136 adolescents (80% of the sample) had pre‐pandemic anxiety data.
To include pre‐pandemic anxiety data from both samples in the same analyses, the proportion of maximum scaling (POMS) method was applied (Little, 2013). This scaling approach produces proportion scores for each participant ranging from 0 to 1 using the following method: (participant’s score – scale minimum) / (scale maximum – scale minimum). The POMS method is preferable to z‐scoring when combining data across different scales in longitudinal research because it does not obscure mean level differences between individuals across time points, allowing full examination of change overtime in rank order score differences (Moeller, 2015). As such, the use of POMS scoring for Time 1 adjustment measures should not be a limitation of the study.
Depressive symptoms
Adolescents in Missouri sample at Time 1 and in both samples at Time 2 completed the 20‐item Center for Epidemiological Studies Depression Scale (CES‐D; Radloff, 1977). Items were rated on a Likert scale from 1 (not at all true of yourself) to 5 (really true of yourself). Each item represented a depressive symptom. Items were rated on a 0‐3 point scale in terms of symptom frequency. Scores were the sum of the ratings across items and higher scores represented greater depressive symptoms. This scale was internally reliable (Time 1 α = .89; Time 2 α = .91). Participants in the Florida sample responded to the Depression subscale of the Depression Anxiety Stress Scale (DASS; Lovibond & Lovibond, 1995) at Time 1. The seven items of the subscale were also rated on 0‐3 point scale of symptom frequency, but scale scores were the average of these items (Time 1 α = .88). The POMS method was used to combine pre‐pandemic depression scores across samples. Of the full sample, 136 adolescents (80% of the sample) had pre‐pandemic depression data.
Problem behavior
Adolescent involvement in risky or problematic behavior was assessed using a 19‐item scale by Eccles and Barber (1990) in the Missouri sample at Time 1 and in both samples at Time 2. Items related to drug use, cheating at school, theft, etc. were assessed on a five‐point scale from 1 (never happens) to 5 (happens very often). Cronbach alphas were .91 for Time 1 and .88 for Time 2. Participants in the Florida sample responded to the 10‐item Problem Behavior Scale (PBS; Mason, Cauce, Gonzales, & Hiraga, 1996) at Time 1. These items assessed similar behaviors as the Hartup and Laursen (1993) scale and were also rated on a 5‐point “never” to “very often” scale. Scores were the average of these items (Time 1 α = .80). The POMS method was used to combine pre‐pandemic problem behavior scores across samples. Of the full sample, 136 adolescents (80% of the sample) had pre‐pandemic problem behavior data.
COVID‐19‐Related Stress (CASPE Questionnaire)
Participants responded to four items from the COVID‐19 Adolescent Symptom and Psychological Experience Questionnaire (CASPE, Ladouceur, 2020) to assess COVID‐19‐related stress. All items were rated on a five‐point Likert scale from 1 (not at all/very slightly) to 5 (Extremely). A sum score was created from responses to the following items such that higher scores indicated higher levels of experience stress due to the pandemic: “Overall, how much has the COVID‐19 outbreak, and the resulting changes to daily life, affected your life in a negative way?”, “COVID‐19 presents a lot of uncertainty about the future. In the past 7 days, including today, how stressful have you found this uncertainty to be?”, The COVID‐19 outbreak has changed and disrupted many existing plans. In the past 7 days, including today, how stressful do you find these disruptions to be?”, “How stressful have the restrictions on leaving home been for you?” The combined items displayed acceptable internal consistency (α = .77).
Analytic plan
Structural equation path analyses predicting anxiety symptoms, depressive symptoms, and problem behavior during COVID‐19, controlling for prior levels of each outcome, were examined in Mplus 8.4 (Muthén & Muthén, 2017). In each model, adjustment outcomes were regressed upon positive or negative relationship quality with relationship partners (mothers, fathers, siblings, and best friends), COVID‐19‐related stress, and interactions between COVID‐19‐related stress and relationship quality. Relationship partners were modeled simultaneously to better assess each relationship’s unique contribution to adolescent adjustment during COVID‐19. Positive and negative relationship quality were assessed separately, however, as our sample size precluded examination of all relationships and types of relationship qualities within a single model. Based on bivariate correlations between demographic and outcome variables (see Table 1), gender was controlled for in all models, but adolescent age, SES (family income, parent highest education), and race were not included (see Figure 1 for the general moderation model). Significant and marginal interaction terms were explored using Johnson‐Neyman regions of significance plots, which depict the association between the predictor and outcome variable surrounded by its 95% confidence interval (CI) across all levels of the moderator. The association between the predictor and outcome is significant across the range of moderator values at which the 95% CI does not include zero (Bauer & Curran, 2005). Only interactions producing regions of significance are discussed in the results.
Table 1.
Correlations and Descriptive Statistics for Main Study Variables and Demographics
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | Mean | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. M Rel Pos | 3.44 | 0.87 | |||||||||||||||
| 2. M Rel Neg | −.43** | 2.12 | 0.99 | ||||||||||||||
| 3. F Rel Pos | .45** | −.24** | 2.92 | 0.86 | |||||||||||||
| 4. F Rel Neg | .01 | .31** | −.28** | 1.89 | 0.84 | ||||||||||||
| 5. S Rel Pos | .40** | −.08 | .51** | −.08 | 2.9 | 0.85 | |||||||||||
| 6. S Rel Neg | −.03 | .25** | .03 | .27** | −.29** | 2.49 | 0.98 | ||||||||||
| 7. Rel Pos | .24** | .22** | .19* | .06 | .27** | −.02 | 3.52 | 0.71 | |||||||||
| 8. BF Rel Neg | .00 | .34** | −.15 | .19* | −.07 | .18* | −.02 | 1.56 | 0.66 | ||||||||
| 9. Covid Stress | .07 | .17* | −.13 | .20* | −.05 | .10 | .21* | .10 | 16.02 | 10.35 | |||||||
| 10. Anxiety | −.12 | .35** | −.29** | .23** | −.13 | .17* | .06 | .24** | .40** | 1.29 | 0.33 | ||||||
| 11. Depress | −.24** | .38** | −.31** | .21** | −.17* | .12 | .11 | .19* | .43** | .79** | 0.31 | 0.24 | |||||
| 12. Prob Beh | −.22** | .38** | −.29** | .30** | −.05 | .02 | .13 | .30** | .23** | .39** | .40** | 0.20 | 0.18 | ||||
| 13. Pre‐Anxiety | −.19* | .18* | −.11 | .13 | −.05 | −.01 | .09 | −.05 | .00 | .29** | .40** | .12 | 0.05 | 0.06 | |||
| 14. Pre‐Depress | −.27** | .29** | −.17 | .11 | −.07 | .09 | .22* | .04 | .12 | .34** | .43** | .14 | .71** | 3.44 | 0.87 | ||
| 15. Pre‐Prob Beh | −.14 | .27** | −.12 | .11 | −.06 | .02 | .10 | .18 | .12 | .05 | .17 | .37** | .31** | .37** | 2.12 | 0.99 | |
| 16. Gender | .10 | .21** | −.14 | .11 | .05 | .03 | .27** | .04 | .32** | .44** | .41** | .21** | .15 | .15 | .06 | 1.51 | 0.50 |
| 17. Age | .10 | .03 | −.01 | −.01 | .03 | −.20* | .09 | −.16 | .05 | −.06 | .08 | .09 | .11 | .16 | .17* | 16.21 | 1.95 |
| 18. Fam Income | .00 | −.10 | .14 | −.02 | −.04 | −.14 | −.03 | −.14 | .02 | −.04 | −.05 | −.03 | −.02 | −.09 | .03 | 2.76 | 1.08 |
| 19. Parent Ed | .10 | −.15 | .03 | −.01 | .00 | −.12 | −.01 | −.03 | .04 | −.01 | .09 | .08 | .05 | .01 | −.06 | 5.05 | 1.01 |
| 20. Race | −.02 | .01 | −.03 | −.00 | −.07 | .02 | .10 | −.04 | .12 | .14 | .04 | −.09 | .25** | .20** | .13 | 0.72 | 0.45 |
BF, Best Friend; Depress, Depressive Symptoms; F, Father; M, Mother; Neg, Negativity; Pos, Positivity; Prob Beh, Problem Behavior. Gender (1 = male, 2 = female); Rel, Relationship; S, Sibling.
* p < .05. ** p < .01.
Figure 1.
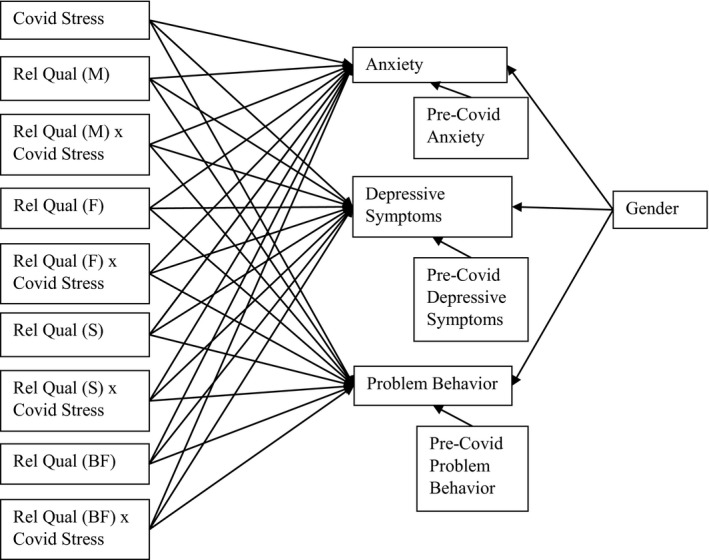
Moderation model.
Note. Correlations among relationship quality in each relationship and among adjustment variables at each wave were modeled but not depicted to improve visual clarity. Correlations were also included between pre‐covid anxiety and Covid depression and between pre‐Covid depression and Covid anxiety to improve model fit. BF, Best Friend; F, Father; Rel Qual, Relationship Quality; M, Mother; S, Sibling.
Model fit was evaluated using traditional fit indices (non‐significant χ2 values, RMSEA < .05 to .08, CFI > .90 to .95, SRMR < .05 to 08; Kline, 2005). Across variables in all models, approximately 7.7% of data were missing completely at random, Little’s MCAR test χ2 (121) = 127.56, p = .324. Missing data were multiply imputed using 10 datasets with product terms based on centered variables created prior to imputation (von Hippel, 2009), then models were analyzed using a maximum likelihood estimator. Participants were clustered within families to control for non‐independence during both multiple imputation and model estimation (Muthén & Muthén, 2017). For both positive and negative relationship quality models, a main effects model (with path coefficients from the interaction terms to the outcomes constrained at 0) was examined prior to a moderation model (in which these interaction paths were freely estimated). Model fit comparisons were conducted using χ2 difference tests.
Results
Descriptive Information
Correlations and descriptive statistics of all study variables can be found in Table 1. Adolescents reported moderate‐to‐high relationship positivity and moderate‐to‐low relationship negativity across relationship types. Relationships were generally most positive and least negative with best friends. Relationship quality was moderately correlated among relationship types, with the strongest associations appearing for relationship positivity among family members.
Adolescents reported low levels of problem behavior during COVID‐19, but quite high levels of depression and anxiety for a community sample, with 38% of participants reporting depression levels above the clinical cut‐off (16.0; Radloff, 1977). Average levels of COVID‐19‐related stress were at the midpoint of the scale. All adjustment measures were significantly correlated with one another within time points and with themselves over time; anxiety and depressive symptoms had particularly high associations. COVID‐19‐related stress was significantly associated with concurrent, but not prior, adjustment measures.
Compared to males, female adolescents reported more negative relationship quality with mothers and more positive relationship quality with best friends; they also reported greater COVID‐19‐related stress and all forms of adjustment problems during COVID‐19. Older adolescents reported less negative relationship quality with siblings and higher levels of pre‐pandemic problem behavior. White, non‐Hispanic adolescents reported higher levels of pre‐pandemic depressive symptoms and anxiety. No other significant correlations emerged with demographic variables.
Path Analyses
Fit indices and path coefficients are presented in Table 2 for main effect models and in Table 3 for models including interaction terms. The data fit the models well for positive and negative relationship quality. Because all predictor variables were centered prior to computing interaction terms, no meaningful differences emerged between the main effects observed in the models with and without interactions included. Findings will therefore be discussed based on the interaction models. Notably, the addition of interaction terms significantly improved model fit for the positive relationships model (Δχ2 (12) = 26.93, p = .008), but not for the negative relationships model (Δχ2 (12) = 15.48, p = .22). Significant interactions in the negative relationships model should therefore be interpreted with caution, given the possibility of an inflated family‐wise error rate.
Table 2.
Main Effects Model Results
| Fit Indexes | Positive Relationship Quality | Negative Relationship Quality | ||||
|---|---|---|---|---|---|---|
| χ2(46) = 76.99, p = .003, RMSEA = .062, CFI = .889, SRMR = .075 | χ2(46) = 62.91, p = .049, RMSEA = .045, CFI = .939, SRMR = .074 | |||||
| Predictors | Anxiety | Depression | Problem Behavior | Anxiety | Depression | Problem Behavior |
| Prior adjust | .20* (.08) | .26** (.08) | .26** (.08) | .20** (08) | .26** (.08) | .22** (.08) |
| Gender | .31*** (.07) | .27*** (.08) | .13 (.08) | .28*** (.07) | .23** (.07) | .10 (.07) |
| Covid stress | .31*** (.06) | .34*** (.07) | .14 † (.07) | .28*** (.06) | .32*** (.07) | .11 † (.06) |
| Rel qual (M) | −.03 (.09) | −.16* (.08) | −.19 † (.10) | .14 (.10) | .19* (.08) | .24* (.09) |
| Rel qual (F) | −.12 (.08) | −.10 (.08) | −.20* (.09) | .04 (.07) | .01 (.06) | .17* (.08) |
| Rel qual (S) | −.04 (.08) | −.05 (.07) | .10 (.10) | .08 (.07) | .02 (.07) | −.12 (.08) |
| Rel qual (BF) | −.07 (.08) | .00 (.07) | .09 (.08) | .11 (.09) | .09 (.07) | .14 (.10) |
Standardized path coefficients presented, SE in parentheses. Gender: 1 = male, 2 = female.
p < .10, *p < .05, **p < .01, ***p < .001.
Table 3.
Moderation Model Results
| Fit Indexes | Positive Relationship Quality | Negative Relationship Quality | ||||
|---|---|---|---|---|---|---|
| χ2(34) = 50.06, p = .037; RMSEA = .050, CFI = .941, SRMR = .069 | χ2(34) = 47.43, p = .063, RMSEA = .045, CFI = .95, SRMR = .071 | |||||
| Predictors | Anxiety | Depression | Problem Behavior | Anxiety | Depression | Problem Behavior |
| Prior adjust | .19* (.08) | .28*** (.08) | .26** (.08) | .20** (.08) | .26** (.08) | .21* (.08) |
| Gender | .31*** (.07) | .26*** (.07) | .13 † (.08) | .28*** (.07) | .23** (.07) | .10 (.07) |
| Covid stress (CS) | .31*** (.06) | .34*** (.06) | .14** (.07) | .26*** (.06) | .33*** (.08) | .11 † (.07) |
| Rel qual (M) | .01 (.09) | −.18* (.08) | −.11 (.10) | .14 (.10) | .18* (.06) | .21* (.09) |
| Rel qual (F) | −.12 (.07) | −.09 (.07) | −.20* (.09) | .05 (.07) | .01 (.07) | .17* (.08) |
| Rel qual (S) | −.07 (.09) | −.00 (.08) | .06 (.11) | .09 (.07) | .03 (.07) | −.10 (.08) |
| Rel qual (BF) | −.04 (.08) | .01 (.07) | .12 (.08) | .12 (.09) | .09 (.07) | .16 (.10) |
| Rel qual (M) × CS | −.01 (.09) | .11 (.08) | −.07 (.09) | −.02 (.07) | .05 (.06) | .08 (.07) |
| Rel qual (F) × CS | −.03 (.08) | .07 (.09) | .03 (.09) | −.02 (.07) | −.04 (.07) | −.04 (.07) |
| Rel qual (S) × CS | .14 † (.08) | −.07 (.07) | .17 † (.09) | −.13 † (.07) | .02 (.07) | −.04 (.06) |
| Rel qual (BF) × CS | .08 (.07) | .08 (.07) | .15* (.07) | .05 (.09) | −.08 (.08) | −.06 (.10) |
Standardized path coefficients presented, SE in parentheses.
p < .10, *p < .05, **p < .01, ***p < .001.
Across all models, higher pre‐pandemic anxiety, depressive symptoms, and problem behavior were associated with higher levels of the same adjustment problems during COVID‐19. Controlling for prior adjustment, greater reported COVID‐19‐related stress was also associated with poorer adjustment on all outcomes, although this effect was smaller for problem behavior. Likewise, controlling for prior adjustment, female adolescents reported higher levels of anxiety and depressive symptoms during COVID‐19, but not significantly more problem behavior.
Relationship Positivity
Controlling for prior adjustment, gender, and COVID‐19‐related stress, more positivity in relationships with mothers was associated with lower depressive symptoms during COVID‐19 and more positivity in relationships with fathers was associated with less problem behavior during COVID‐19. Relationship positivity with best friends, and marginally (p = .07) siblings, interacted with COVID‐related stress in predicting problem behavior. More positive relationships with best friends (Figure 2) and siblings (Figure 3) were significantly associated with greater problem behavior when COVID‐19‐related stress was relatively high (>0.2 SD for best friends, >1.3 SD for siblings), but not when it was average or low.
Figure 2.
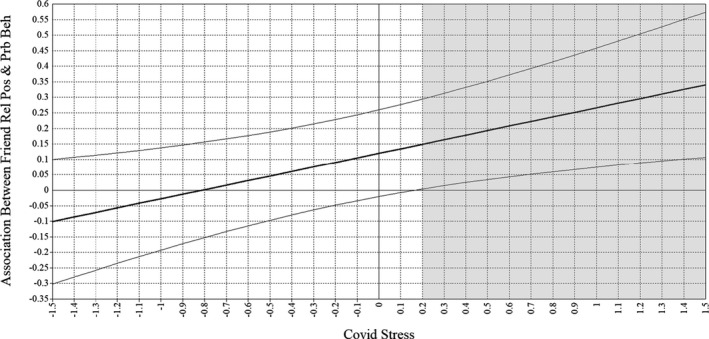
Johnson‐Neyman Plot of the interaction between best friend relationship positivity × covid stress on problem behavior.
Note. All variables standardized. Thick black line represents the association between best friend relationship positivity and problem behavior; light black lines represent the upper and lower bounds of a 95% CI around this association. Region within the gray rectangle depicts values of Covid Stress at which the association between best friend relationship positivity and problem behavior is significantly positive. Rel Pos, Relationship Positivity.
Figure 3.
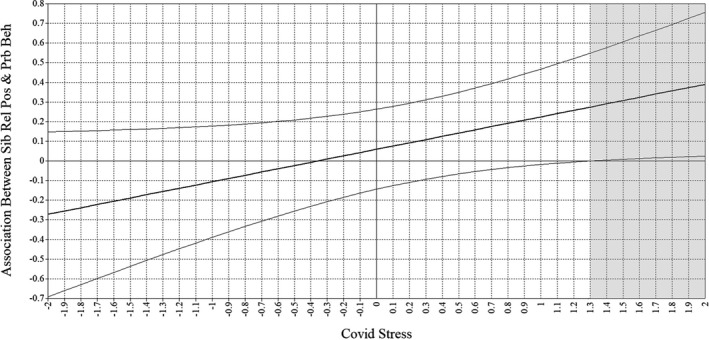
Johnson‐Neyman Plot of the interaction between sibling relationship positivity × covid stress on problem behavior.
Note. All variables standardized. Thick black line represents association between sibling relationship positivity and problem behavior; light black lines represent the upper and lower bounds of a 95% CI around this association. Region within the gray rectangle depicts values of Covid Stress at which the association between sibling relationship positivity and problem behavior is significantly positive. Sib Rel Pos, Sibling Relationship Positivity.
Relationship Negativity
Controlling for prior adjustment, gender, and COVID‐19‐related stress, more negativity in relationships with mothers was associated with more depressive symptoms and problem behavior during COVID‐19 and more negativity in relationships with fathers was associated with more problem behavior during COVID‐19. Negativity in sibling relationships marginally (p = .07) interacted with COVID‐related stress in predicting anxiety; more relationship negativity with siblings was significantly associated with more anxiety only when COVID‐related stress was low (<−.67 SD; see Figure 4).
Figure 4.
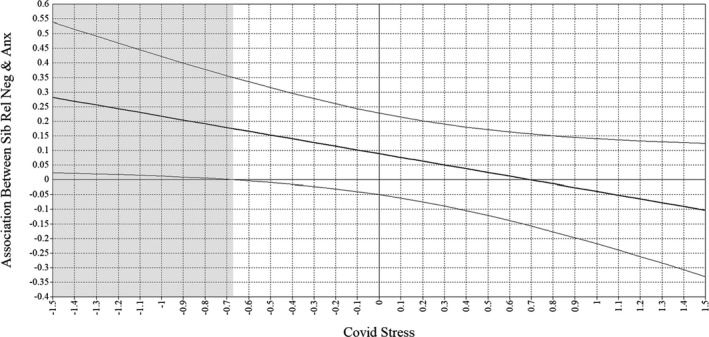
Johnson‐Neyman plot of the interaction between sibling relationship negativity × covid stress on anxiety symptoms.
Note. All variables standardized. Thick black line represents association between sibling relationship negativity and anxiety; light black lines represent the upper and lower bounds of a 95% CI around this association. Region within the gray rectangle depicts values of Covid Stress at which the association between sibling relationship negativity and anxiety is significantly positive. Sib Rel Neg, Sibling Relationship Negativity.
Discussion
The COVID‐19 pandemic has impacted the ways that youth interact with close others. While adolescents often seek social support from peers in typical contexts (Furman & Rose, 2015), stay‐at‐home orders and safety regulations have made face‐to‐face interaction with peers less accessible, while also forcing greater time spent with family members. The present study aimed to examine the unique role of relationship qualities (i.e., positive and negative) with four important close relationships in adolescents’ lives (i.e., mothers, fathers, siblings, and best friends) and in adolescents’ emotional and behavioral adjustment during the pandemic. Additionally, we sought information about whether these relationship qualities were moderated by COVID‐19‐related stress levels. In general, we found that adolescents’ close relationships with parents predicted their adjustment in expected directions (i.e., positive relationships were better for adjustment, negative relationships were detrimental for adjustment) regardless of COVID‐19‐related stress, while the effects on adjustment of positive egalitarian relationships with siblings and friends, and negative relationships with siblings, depended more on COVID‐19‐related stress.
Pre‐pandemic adjustment levels, as well as COVID‐19‐related stress, were consistently associated with higher levels of depression, anxiety, and problem behavior during the pandemic. Over and above these findings, unique associations with the four different close relationship were revealed. Positive relationship qualities with both mothers and fathers were uniquely predictive of better youth adjustment, but while positive relationships with mothers were more protective against depressive symptoms, more positive relationships with fathers were protective against problem behavior. Conversely, more negative relationships with mothers were associated with greater depressive symptoms and problem behavior, and more negative relationships with fathers were only associated with greater problem behavior. These findings appear to be consistent with previous research prior to the pandemic which has found that conflict with fathers is associated with higher levels of risky behavior, rather than emotional adjustment problems, which was more the case for conflict with mothers (Adams & Laursen, 2007). Mothers are more likely than fathers to be turned to as significant sources of social support throughout childhood and adolescence (Furman & Buhrmester, 1992), and often thought societally as more in‐tuned to and responsible for their children’s emotional well‐being than are fathers. Interestingly, while negative relationships with either parent were associated with greater problem behavior, only positive relationships with fathers were uniquely protective against problem behavior with adolescents in this study. Previous research on father involvement has found that it is particularly protective against adolescent delinquency, and that greater involvement in risky and delinquent behaviors actually increases fathers’ involvement (Coley & Medeiros, 2007). In the context of the pandemic and the added health risks involved with adolescents engaging in problematic behaviors outside the home, and in combination with the fact that fathers may have been more involved and engaged with their adolescents than is typical due to stay‐at‐home orders, positive relationship qualities with fathers may have been particularly beneficial to teens.
While the more hierarchical nature of the parent–child relationship lends itself to relationships with mothers and fathers being similar, the more egalitarian nature of relationships with both siblings and best friends also revealed some similarities in the ways that those relationships impacted adolescent adjustment. Interestingly, for both siblings and best friends, higher relationship positivity in the context of high levels of COVID‐related stress, was associated with greater adolescent problem behavior. Previous research suggests that deviancy training processes, a form of peer socialization in which friends or siblings encourage and exacerbate each other’s behavior problems by responding positively to deviant talk, are especially strong when these relationships and interactions are positive (Piehler & Dishion, 2007; Whiteman, Jensen, & McHale, 2017). However, whether deviancy training processes might help to explain the current findings is unclear. On one hand, if the friends are not seeing each other in person, the effects of deviancy training processes (e.g., over video chat) may be weaker, but siblings were seeing each other regularly while “stuck at home” together. Alternatively, if deviancy training processes (virtual or in‐person) are related to youth breaking rules related to social distancing and engaging in problematic behavior together outside the home without the parents’ knowledge, then considering deviancy training may help to explain the current findings.
In terms of unique findings between siblings and best friends, we found that the combination of higher negative sibling relationship qualities (but not with best friends) with low levels of COVID‐related stress was associated with greater adolescent anxiety. It is not particularly surprising that high levels of conflict and negativity with siblings would be associated with greater anxiety as this has been found in pre‐pandemic studies (e.g., Campione‐Barr, Greer, & Kruse, 2013; Dirks et al., 2015). Sibling relationships are known to be the quintessential “love‐hate” relationship with high levels of ambivalence particularly common during adolescence (Buist & Vermande, 2014; Killoren, Rodríguez de Jesús, Updegraff, & Wheeler, 2017). It is interesting, however, that this would only be evident under conditions of low COVID‐related stress. It is likely that in households experiencing high levels of COVID‐related stress, sibling conflict is pretty low on the hierarchy of concerns. Alternatively, families experiencing low levels of COVID‐related stress may have experienced more business‐as‐usual style of family interactions, but with the added time together and boredom, sibling conflict likely rose to higher‐than‐usual levels, to some detrimental effects.
Our study is the first we are aware of to examine the potential protective and exacerbating effects of various relationship qualities on adolescent adjustment during the COVID‐19 pandemic. Despite the interesting results, the examination is not without limitations. First, despite the fact that the study used adolescents from multiple areas of the United States (Midwest and South), the ethnic/racial and socioeconomic diversity of the larger sample was limited, consisting primarily of White, middle‐class families. Given that the COVID‐19 pandemic disproportionately impacted families with fewer financial means and families from minoritized groups (Tai, Shah, Doubeni, Sia, & Wieland, 2021), the generalizability of these results is likely limited. It is also important to note that compliance with COVID‐19 public health regulations, as well as the viral burden of the pandemic, were not consistent across the United States, and thus our samples from Missouri and Florida may not be consistent with those from the East‐ or West‐coast. However, we did not assess beliefs or compliance in our study, only the influence of COVID‐19‐related stress; therefore, it is difficult to know how much these findings would have varied.
Second, given that we studied adolescents, a potential fifth important close relationship that was missing from this examination was romantic relationships. While we did assess the positivity and negativity of adolescents’ romantic relationships, only approximately 25% of our sample reported on such a relationship, which was too much missing data to be useful. While romantic partners are increasingly important to youth over the course of adolescence (Furman & Rose, 2015), it is difficult for us to know how much they were able to stay in contact or see each other in‐person during this time and this likely ranged widely across families. Some parents may have allowed romantic partners to essentially be a part of their “family bubble,” while others may have had strict rules against seeing romantic partners due to health concerns.
Finally, the sample size for our analyses provides reasonable power (80%) to detect moderately small sized path coefficients (f 2 = .05, as calculated in G*Power; Faul, Erdfelder, Lang, & Buchner, 2007). However, the sample is somewhat small for the number of parameters in our models, which may have resulted in less precise results (Kline, 2005). Examination of the same models with each relationship considered independently (thus greatly reducing model parameters) provided generally similar findings, however, bolstering confidence in our results (see Tables S1 and S2).
Despite these limitations, our findings suggest not only the ways in which adolescents were uniquely utilizing mothers, fathers, siblings, and best friends as sources of coping during the pandemic, but also have further implications beyond the pandemic. It appears as though relationship qualities with mothers and fathers during the pandemic were similarly impactful on adolescent adjustment to the ways in which they were typically during pre‐pandemic (and likely post‐pandemic) times. Alternatively, the associations between relationships with siblings and best friends and adolescents’ adjustment were more impacted by the stress of the COVID‐19 pandemic. This is likely because the amount of time they spent together and the ways in which they interacted. Siblings were likely spending more time together than usual due to outside‐of‐household contact being limited, and they were likely to serve as a substitute for more preferred peers given the limitations. Best friends, on the other hand, were more likely relegated to online or virtual communication (e.g., texting, social media, video chat, online gaming). In the aftermath of the pandemic, it is likely that adolescents will return more of their time to socializing with peers and utilizing their social support as is developmentally appropriate, but it will be interesting for future research to examine whether this experience has improved or changed the ways in which adolescents utilize their siblings as sources of support and companionship even when they are not the only alternative.
Supporting information
Table S1. Path Analyses for Each Relationship Separately – Positive Relationship Quality.
Table S2. Path Analyses for Each Relationship Separately – Negative Relationship Quality.
We would like to thank the Columbia Public School District, Pinellas County School District, and the many families who participated in this research, as well as our undergraduate research assistants for their participation with family recruitment and data entry. We are grateful to the recruitment efforts of Yue Guo (University of Missouri) and Savannah Flak (University of South Florida). Finally, we thank the National Science Foundation (#1451757, Campione‐Barr, PI), USF Women in Leadership Funds (Rote, PI), and MU College of Human Environmental Science Research Funds (Killoren, PI) for funding the data collection.
References
- Adams, R. E. , & Laursen, B. (2007). The correlates of conflict: Disagreement is not necessarily detrimental. Journal of Family Psychology, 21(3), 445–458. 10.1037/0893-3200.21.3.445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alloy, L. B. , & Abramson, L. Y. (2007). The adolescent surge in depression and emergence of gender differences: A biocognitive vulnerability‐stress model in developmental context. In Romer D., & Walker E. F. (Eds.), Adolescent psychopathology and the developing brain: Integrating brain and prevention science (pp. 284–312). Oxford, UK: Oxford University Press. [Google Scholar]
- Barendese, M. A. , Flannery, J. , Cavanagh, C. , Arstizabal, M. , Becker, S. P. , Berger, E. , … Pfeifer, J. H. (under review). Longitudinal change in adolescent depression and anxiety symptoms from before to during the COVID‐19 pandemic: An international collaborative of 12 samples. Retreived from https://psyarxiv.com/hn7us/ [DOI] [PMC free article] [PubMed]
- Bauer, D. J. , & Curran, P. J. (2005). Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research, 40, 373–400. 10.1207/s15327906mbr4003_5 [DOI] [PubMed] [Google Scholar]
- Buist, K. L. , Dekovic, M. , & Prinzie, P. (2013). Sibling relationship quality and psychopathology of children and adolescents: A meta‐analysis. Clinical Psychology Review, 33, 97–106. 10.1016/j.cpr.2012.10.007 [DOI] [PubMed] [Google Scholar]
- Buist, K. L. , & Vermande, M. (2014). Sibling relationship patterns and their associations with child competence and problem behavior. Journal of Family Psychology, 28, 529–537. 10.1037/a0036990 [DOI] [PubMed] [Google Scholar]
- Calvete, E. , & Connor‐Smith, J. K. (2006). Perceived social support, coping, and symptoms of distress in American and Spanish students. Anxiety, Stress & Coping, 19, 47–65. 10.1080/10615800500472963 [DOI] [Google Scholar]
- Campione‐Barr, N. , Greer, K. B. , & Kruse, A. (2013). Differential associations between domains of sibling conflict and adolescent emotional adjustment. Child Development, 84, 938–954. 10.1111/cdev.12022 [DOI] [PubMed] [Google Scholar]
- Campione‐Barr, N. , Odudu, C. , Giron, S. E. , & Killoren, S. E. (March, 2019). Associations between subjective ratings of parent and adolescent behaviors during interactions and adolescent disclosure. Paper presented at the Biennial Meetings of the Society for Research on Child Development. Baltimore, MD. [Google Scholar]
- Castro‐Schilo, L. , & Grimm, K. J. (2017). Using residualized change versus difference scores for longitudinal research. Journal of Social and Personal Relationships, 35, 32–58. 10.1177/0265407517718387 [DOI] [Google Scholar]
- Cheng, Y. , Li, X. , Lou, C. , Sonenstein, F. L. , Kalamar, A. , … Ojengbede, O. (2014). The association between social support and mental health among vulnerable adolescents in five cities: Findings from the study of the well‐being of adolescents in vulnerable environments. Journal of Adolescent Health, 55, 531–538. 10.1016/j.adohealth.2014.08.020 [DOI] [PubMed] [Google Scholar]
- Coley, R. L. , & Medeiros, B. L. (2007). Reciprocal longitudinal relations between nonresident father involvement and adolescent delinquency. Child Development, 78, 132–147. 10.1111/j.1467-8624.2007.00989.x [DOI] [PubMed] [Google Scholar]
- Collins, W. A. , & Laursen, B. (1992). Conflict and relationships during adolescence. In Shantz C. U., & Hartup W. W. (Eds.), Cambridge studies in social and emotional development. Conflict in child and adolescent development (pp. 216–241). New York, NY: Cambridge University Press. [Google Scholar]
- Dirks, M. A. , Persram, R. , Recchia, H. E. , & Howe, N. (2015). Sibling relationships as sources of risk and resilience in the development and maintenance of internalizing and externalizing problems during childhood and adolescence. Clinical Psychology Review, 42, 145–155. 10.1016/j.cpr.2015.07.003 [DOI] [PubMed] [Google Scholar]
- Duan, L. , Shao, X. , Wang, Y. , Huang, Y. , Miao, J. , Yang, X. , & Zhu, G. (2020). An investigation of mental health status of children and adolescents in China during the outbreak of COVID‐19. Journal of Affective Disorders, 275, 112–118. 10.1016/j.jad.2020.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccles, J. S. , & Barber, B. (1990). Risky behavior measure. Unpublished scale, University of Michigan.
- Eisenberg, N. , Fabes, R. A. , Shepard, S. A. , Guthrie, I. K. , Murphy, B. C. , & Reiser, M. (1999). Parental reactions to children’s negative emotions: Longitudinal relations to quality of children’s social functioning. Child Development, 70, 513–534. 10.1111/1467-8624.00037 [DOI] [PubMed] [Google Scholar]
- Faul, F. , Erdfelder, E. , Lang, A.‐G. , & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavioral Research Methods, 39, 175–191 [DOI] [PubMed] [Google Scholar]
- Furman, W. , & Buhrmester, D. (1985). Children’s perceptions of the personal relationships in their social networks. Developmental Psychology, 21, 1016–1024. 10.1037/0012-1649.21.6.1016 [DOI] [Google Scholar]
- Furman, W. , & Buhrmester, D. (1992). Age and sex differences in perceptions of networks of personal relationships. Child Development, 63, 103–115. 10.2307/1130905 [DOI] [PubMed] [Google Scholar]
- Furman, W. , & Rose, A. J. (2015). Friendships, romantic relationships, and peer relationships. In Lamb M. E., & Lerner R. M. (Eds.), Handbook of child psychology and developmental science: Socioemotional processes (pp. 932–974). Hoboken, NJ: John Wiley & Sons, Inc. 10.1002/9781118963418.childpsy322 [DOI] [Google Scholar]
- Gass, K. , Jenkins, J. , & Dunn, J. (2007). Are sibling relationships protective? A longitudinal study. Journal of Child Psychology and Psychiatry, 48, 167–175. 10.1111/j.1469-7610.2006.01699.x [DOI] [PubMed] [Google Scholar]
- Gil‐Rivas, V. , Silver, R. C. , Holman, E. A. , McIntosh, D. N. , & Poulin, M. (2007). Parental response and adolescent adjustment to the September 11, 2001 terrorist attacks. Journal of Traumatic Stress, 20, 1063–1068. 10.1002/jts.20277 [DOI] [PubMed] [Google Scholar]
- Hartup, W. W. , & Laursen, B. (1993). Conflict and context in peer relations. In Hart C. H. (Ed.), Children on playgrounds: Research perspectives and applications (pp. 44–84). Albany, NY: State University of New York Press. [Google Scholar]
- Holahan, C. J. , Valentiner, D. P. , & Moos, R. H. (1995). Parental support, coping strategies, and psychological adjustment: An integrative model with late adolescents. Journal of Youth & Adolescence, 24, 633–648. 10.1007/BF01536948 [DOI] [Google Scholar]
- Kessler, R. C. , Avenevoli, S. , & Merikangas, K. R. (2001). Mood disorders in children and adolescents: An epidemiologic perspective. Biological Psychiatry, 49, 1002–1014. 10.1016/50006-3223(01)01129-5 [DOI] [PubMed] [Google Scholar]
- Killoren, S. E. , & Roach, A. L. (2014). Sibling conversations about dating and sexuality: Sisters as confidants, sources of support, and mentors. Family Relations, 63, 232–243. 10.1111/fare.12057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killoren, S. E. , Rodríguez de Jesús, S. A. , Updegraff, K. A. , & Wheeler, L. A. (2017). Sibling relationship quality and Mexican‐origin adolescents’ and young adults’ familism values and adjustment. International Journal of Behavioral Development, 41, 155–164. 10.1177/0165025415607084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, R. (2005). Principles and practices of structural equation modeling 2nd edn. New York, NY: Guilford Press. [Google Scholar]
- Kim, J. , McHale, S. M. , Osgood, D. W. , & Crouter, A. C. (2006). Longitudinal course and family correlates of sibling relationships from childhood through adolescence. Child Development, 77, 1746–1761. 10.1111/j.1467-8624.2006.00971.x [DOI] [PubMed] [Google Scholar]
- Ladouceur, C. D. (2020). COVID‐19 Adolescent Symptom & Psychological Experience Questionnaire (CASPE). Unpublished scale. Retrieved from https://osf.io/mzrjg/ [Google Scholar]
- Laursen, B. , Coy, K. C. , & Collins, W. A. (1998). Reconsidering changes in parent‐child conflict across adolescence: A meta‐analysis. Child Development, 69, 817–832. 10.1111/j.1467-8624.1998.tb06245.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindell, A. K. , Campione‐Barr, N. , & Killoren, S. E. (2015). Technology‐mediated communication with siblings during the transition to college: Associations with relationship positivity and self‐disclosure. Family Relations, 64, 563–578. 10.1111/fare.12133 [DOI] [Google Scholar]
- Little, T. D. (2013). Longitudinal structural equation modeling. New York, NY: Guilford Press. [Google Scholar]
- Lovibond, S. H. , & Lovibond, P. F. (1995). Manual for the depression anxiety stress scales (2nd ed.). Psychology Foundation. [Google Scholar]
- Maccoby, E. E. (1994). The role of parents in the socialization of children: An historical overview. In Parke R. D., Ornstein P. A., Rieser J. J., & Zahn‐Waxler C. (Eds.), A century of developmental psychology (pp. 589–615). Washington, DC: American Psychological Association. 10.1037/10155-021 [DOI] [Google Scholar]
- Magson, N. R. , Freeman, J. Y. A. , Rapee, R. M. , Richardson, C. E. , Oar, E. L. , & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID‐19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason, C. A. , Cauce, A. M. , Gonzales, N. , & Hiraga, Y. (1996). Neither too sweet nor too sour: Problem peers, maternal control, and problem behavior in african american adolescents. Child Development, 67, 2115. 10.2307/1131613 [DOI] [PubMed] [Google Scholar]
- Masten, A. S. (2018). Resilience theory and research on children and families: Past, present, and promise. Journal of Family Theory & Review, 10, 12–31. 10.1111/jftr.12255 [DOI] [Google Scholar]
- McHale, S. M. , & Crouter, A. C. (1996). The family contexts of children’s sibling relationships. In Brody G. H. (Ed.), Advances in applied developmental psychology, 10. Sibling relationships: Their causes and consequences (pp. 173–195). Norwood, NJ: Ablex Publishing. [Google Scholar]
- Merikangas, K. R. , He, J. , Burstein, M. , Swanson, S. A. , Aveneovoli, S. , … Swendsen, J. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the national comorbidity survey replication‐adolescent supplement. American Academy of Child and Adolescent Psychiatry, 49, 980–989. 10.1016/j.jacc.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller, J. (2015). A word on standardization in longitudinal studies: Don't. Frontiers in Psychology, 6, 1389. 10.3389/fpsyg.2015.01389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai, R. , Olfson, M. , & Han, B. (2016). National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics, 138(6), e20161878. 10.1542/peds.2016-1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray, J. S. (2009). A collaborative approach to meeting the psychosocial needs of children during an influenza pandemic. Journal for Specialists in Pediatric Nursing, 15, 135–143. 10.1111/j.1744-6155.2009.00229.x [DOI] [PubMed] [Google Scholar]
- Muthén, L. K. , & Muthén, B. O. (2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Pearlin, L. I. , Menaghan, E. G. , Lieberman, M. A. , & Mullan, J. T. (1981). The stress process. Journal of Health and Social Behavior, 22, 337. 10.2307/2136676 [DOI] [PubMed] [Google Scholar]
- Piehler, T. F. , & Dishion, T. J. (2007). Interpersonal dynamics within adolescent friendships: Dyadic mutuality, deviant talk, and pattersn of antisocial behavior. Child Development, 78, 1611–1624. 10.1111/j.1467-8624.2007.01086.x [DOI] [PubMed] [Google Scholar]
- Possel, P. , Burton, S. M. , Cauley, B. , Sawyer, M. G. , Spence, S. H. , & Sheffield, J. (2018). Associations between social support from family, friends, and teachers, and depressive symptoms in adolescents. Journal of Youth and Adolescence, 47, 398–412. 10.1007/s10964-017-0712-6 [DOI] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES‐D Scale. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Reynolds, C. R. , & Richmond, B. O. (1978). Revised children’s manifest anxiety scale. APA PsycTests. 10.1037/t00514-000 [DOI] [PubMed] [Google Scholar]
- Romeo, R. D. (2013). The teenage brain. Current Directions in Psychological Science, 22, 140–145. 10.1177/0963721413475445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rote, W. M. , Flak, S. R. , & Ellison, C. (2021). “That’s not what I heard!”: Adolescent internalizing, negative perceptions of maternal communication, and felt shame and guilt. Journal of Youth and Adolescence. Advance Online Publication. 10.1007/s10964-021-01458-4 [DOI] [PubMed] [Google Scholar]
- Schwartz‐Mette, R. A. , Shankman, J. , Dueweke, A. R. , Borowski, S. , & Rose, A. J. (2020). Relations of friendship experiences with depressive symptoms and loneliness in childhood and adolescence: A meta‐analytic review. Psychological Bulletin, 146, 664–700. 10.1037/bul0000239 [DOI] [PubMed] [Google Scholar]
- Steinberg, L. (1990). Autonomy, conflict, and harmony in the family relationship. In Feldman S. S., & Elliott G. R. (Eds.), At the threshold: The developing adolescent (pp. 255–276). Cambridge, MA: Harvard University Press. [Google Scholar]
- Tai, D. B. G. , Shah, A. , Doubeni, C. A. , Sia, I. G. , & Wieland, M. L. (2021). The disproportionate impact of COVID‐19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases, 72, 703–706. 10.1093/cid/ciaa815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker, C. J. , Barber, B. L. , & Eccles, J. S. (1997). Advice about life plans and personal problems in late adolescent sibling relationships. Journal of Youth and Adolescence, 26, 63–76. 10.1023/A:1024540228946 [DOI] [Google Scholar]
- von Hippel, P. T. (2009). How to impute interactions, squares, and other transformed variables. Sociological Methodology, 39, 265–291. 10.1111/j.1467-9531.2009.01215.x [DOI] [Google Scholar]
- Waite, E. B. , Shanahan, L. , Calkins, S. D. , Keane, S. P. , & O’Brien, M. (2011). Life events, sibling warmth, and youths’ adjustment. Journal of Marriage and Family, 73, 902–912. 10.1111/j.1741-3737.2011.00857.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteman, S. D. , Jensen, A. C. , & McHale, S. M. (2017). Sibling influences on risky behaviors from adolescence to young adulthood: Vertical socialization or bidirectional effects? In N. Campione‐Barr (Ed.), Power, control, and influence in sibling relationships across development. New Directions for Child and Adolescent Development, 156, 67–85. 10.1002/cad.20197 [DOI] [PubMed] [Google Scholar]
- Xie, X. , Xue, Q. I. , Zhou, Y. U. , Zhu, K. , Liu, Q. I. , Zhang, J. , & Song, R. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics, 174, 898–900. 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Path Analyses for Each Relationship Separately – Positive Relationship Quality.
Table S2. Path Analyses for Each Relationship Separately – Negative Relationship Quality.


