Abstract
Background
This longitudinal cohort study aimed to examine the impact of the first wave of the COVID‐19 pandemic in Ireland on parents of children with externalising difficulties, in comparison to parents of children without such difficulties.
Method
Parents of 159 children completed online self‐report measures at three time points during the first wave of the COVID‐19 pandemic; (a) Delay and Mitigation Phase (March 2020 to May 2020), (b) Reopening of Society Phase (June 2020 to July 2020) and (c) Wave 2 Case Acceleration Phase (September 2020 to October 2020). Participants were allocated to the clinical group if they met the clinical cut off point on the Conduct or Hyperactivity/Inattention subscales of the Strengths and Difficulties Questionnaire at Time 1.
Results
Parents of children with externalising difficulties experienced significantly higher levels of stress, lower levels of wellbeing and engaged in higher levels of avoidant‐focused coping strategies longitudinally. There was a significant difference between outcomes at the different phases of the COVID‐19 pandemic, for stress related to parenting, personal/family stress related to the impact of the COVID‐19 and type of coping strategies employed. Children with externalising difficulties, in comparison to children without externalising difficulties, showed significantly greater adjustment over time for behavioural and emotional difficulties, as reported by their parents.
Conclusions
Results provide important information regarding the trajectory of psychological outcomes in parents of children with externalising difficulties over the first wave of the COVID‐19 pandemic, highlighting the need for increased parental supports during, and after, the COVID‐19 pandemic.
What's known
The COVID‐19 pandemic has been associated with negative psychological outcomes in the general population. Parents of children with externalising difficulties experience poorer outcomes than parents of children without such difficulties, in pre‐pandemic circumstances.
What's new
Over the first wave of the COVID‐19 pandemic, parents of children with externalising difficulties experienced significantly higher levels of stress, lower levels of wellbeing and engaged in higher levels of avoidant‐focused coping strategies. Children with externalising difficulties showed significantly greater adjustment over time for parent‐reported behavioural and emotional difficulties. Results provide important information regarding the trajectory of psychological outcomes in parents of children with externalising difficulties, and their perception of their children's emotional and behavioural difficulties, during the COVID‐19 pandemic.
1. INTRODUCTION
The first case of COVID‐19 was detected in the Republic of Ireland on 26 February 2020, 1 with nationwide public health containment measures announced on 12 March 2020, marking the country's move from the Containment Phase to the Delay Phase, of virus management. Public health measures implemented included closure of schools, colleges, and childcare facilities, 2 with further restrictions instigated in late March and April 2020, as confirmed cases of COVID‐19 increased. 3 On 1 May 2020, a Five Phase Roadmap 4 was introduced following a decline in COVID‐19 cases, which outlined the easing of restrictions. A second surge of COVID‐19 cases began in August 2020, resulting in the reimplementation of restrictions in selected regions of the country, with a five level “Framework for Restrictive Measures” 5 introduced in September 2020. Ireland has since been subjected to second and third waves of surges in COVID‐19 cases, which have resulted in the easing and tightening of containment measures based on this framework. 5
Meta‐analytic data from various countries 6 , 7 , 8 , 9 suggest the prevalence of depression to be from 22.6% to 33.7%, anxiety to be from 22.4% to 32.6%, and insomnia to be from 23.0% to 37.9%, during the COVID‐19 pandemic. There is difficulty in accurately comparing these prevalence rates to pre‐pandemic data, considering the use of varied outcomes measures and methodological factors. Longitudinal data from the UK suggests an overall increase in mental distress during the COVID‐19 pandemic, in comparison with the year prior to the COVID‐19 pandemic, in individuals aged 16 years and older, 10 however, a longitudinal study conducted in the Netherlands suggests no significant change in anxiety and depression occurred between prior to and during the COVID‐19 pandemic. 11
Available evidence in an Irish population suggests that during the first week of the implementation of stay‐at‐home measures in March 2020, 27.7% of adults met the clinical cut off point on screening measures for GAD or depression, 12 with 17.7% of this sample also meeting diagnostic requirements for COVID‐19‐related Post Traumatic Stress Disorder (PTSD). 13 A cross‐sectional study, which involved retrospective report prior to the quarantine period, suggests the COVID‐19 pandemic to be associated with statistically significant increases in levels of depression, anxiety and stress, 14 with the rate of depression increasing from 30% to 46.3%, the rate of anxiety increasing from 30.7% to 32.5%, and the rate of stress increasing from 27.7% to 34%. People with an ongoing chronic health condition were also shown to have elevated psychological distress, and reduced wellbeing indices. 15 A longitudinal study, however, suggested there to be a significant reduction in major depression in an Irish population from a year prior to the COVID‐19 pandemic and the early phases of the COVID‐19 pandemic. 16 A cross‐sectional study considering the relational path between COVID‐19 distress and depression in the general population, in which a large proportion of respondents were living in Ireland, suggested the traumatic distress of COVID‐19 to have a strong positive effect on depression, which was mediated by resilience, anxiety and hope. 17
With the closure of schools and child‐care facilities, and implementation of stay‐at‐home orders in Ireland in March 2020, many parents had to adjust to increased levels of responsibility in supporting their children to access education through remote learning, and in many cases, simultaneously manage the demands of working from home. Longitudinal international data highlights the negative impact which the COVID‐19 pandemic has had on parents. In a study conducted in the US, levels of parent depression and child externalising and internalising problems were significantly worse during the pandemic in comparison to pre‐pandemic levels, to large effect. 18 Another US study reported that parent psychological well‐being decreased during the post‐COVID‐19 restrictions period, with the number of COVID‐19‐related hardships found to be strongly associated with all psychological well‐being measures. 19 When compared with pre‐pandemic estimates, parents in Australia reported higher rates of parent depression, anxiety and stress, higher parenting irritability and lower family positive expressiveness. 20 In Singapore, 21 levels of parental stress were found to mediate the impact of COVID‐19 on harsh parenting and parent‐child relationship closeness during a period of stay‐at‐home orders, highlighting the importance of considering parental stress during periods of public health restrictions.
Caring for a child with an externalising difficulty, such as the behavioural difficulties often exhibited by children with Attention Deficit Hyperactivity Disorder (ADHD), in pre‐pandemic circumstances, has been associated with higher levels of parental stress, depression, and anxiety. 22 , 23 This is of heightened concern during the COVID‐19 pandemic, as there is a risk that additional stressors imposed by the COVID‐19 pandemic may exacerbate pre‐pandemic mental health difficulties. 24 As a bidirectional relationship has been proposed between parental stress and child behaviour difficulties, 25 the impact which the COVID‐19 pandemic may have on both parents and their children with externalising difficulties must be considered.
Externalising difficulties are often prevalent for children who have autism, 26 , 27 ADHD, 28 , 29 children who have experienced complex trauma 30 , 31 and/or children who have an intellectual disability (ID). 32 , 33 Several aspects of the COVID‐19 pandemic may have had a negative impact on parents of children with externalising difficulties. Restrictions imposed on social meetings are of concern, considering that poorer quality of life in parents of children with autism has been associated with child behavioural difficulties and lack of social support 34 and social support acts to reduce stress appraisals in parents of children with ADHD and autism. 35 In a cross‐sectional study of parents of children with neurodevelopmental disabilities, 36 76% reported COVID‐19 to have impacted on their well‐being, and in a qualitative study, all mothers of children with an ID discussed experiencing increased burden and stress during a lockdown period. 37
For children who experience externalising difficulties, access to services and supports in Ireland have been significantly reduced during the COVID‐19 pandemic. 38 This is worrying considering that hyperkinetic disorders, including ADHD, are frequently assigned to Community Child Adolescent Mental Health Service (CAMHS) Teams, 39 as mandated by the Health Service Executive in Ireland because of the high level of parents support needs in managing such externalising difficulties faced by the child. Research conducted in Italy during the COVID‐19 pandemic found parents of children with externalising difficulties reported increased intensity and frequency in their children's behavioural difficulties, 40 and parents of children diagnosed with a psychological or physical difficulty reported higher levels of parental burnout and less social support. 41
As services adjust to new ways of working, it is essential to consider the impact which the COVID‐19 pandemic has had on this cohort of parents to inform paediatric practice and appropriate supports. Our study aimed to address the following five research questions:
How does the presence or absence of significant levels of child externalising behaviour problems at the outset of the COVID‐19 pandemic, and the passage of time from the Delay and Mitigation Phase, through the Reopening of Society Phase following Wave 1, to the Wave 2 Case Acceleration Phase, affect parents’ perception of:
Sources of stress in their lives,
Their well‐being,
Their stress responses,
Their coping strategies, and
Their children's behavioural problems.
Following consideration of the evidence outlined in the above introduction, we have four hypotheses regarding the expected outcomes for these five research questions:
That parents of children with externalising difficulties, in comparison to parents of children without such difficulties, would have significantly poorer outcomes on variables in all domains, at all data points.
That there would be a significant difference between scores on variables in all domains obtained during the Delay and Mitigation Phase, the Reopening of Society Phase, and the Case Acceleration Phase.
That compared with parents of children without externalising difficulties, mean scores on variables of parents of children with externalising difficulties, would indicate poorer adjustment as the COVID‐19 pandemic progressed.
That compared with children without externalising difficulties, mean scores of children with externalising difficulties would indicate poorer adjustment on parent‐rated behavioural difficulties as the COVID‐19 pandemic progressed.
2. METHOD
2.1. Recruitment
Study information was disseminated online via Irish charities for children, school information platforms, and social media. Parents provided informed consent to be provided with a hyperlink via email to complete data entry at each time point. Each participant created an individual code to link their data from each time point. Individuals were eligible to participate if they were a parent of a child (4‐18 years) and were living in the Republic of Ireland. The term “parent” in this study referred to any individual who engaged in the act of parenting, for example, biological parents, foster parents/carers, kinship carers, etc. Participants who completed all time points were entered into a draw to win one of three 50‐euro retail vouchers.
2.2. Design
The study design was a longitudinal cohort study with 159 participants, divided into a clinical and a non‐clinical group. Data were collected at three time points during the COVID‐19 pandemic in Ireland. Time 1 data were collected during the Delay and Mitigation Phase (28 March 2020 to 18 May 2020), time 2 during the Reopening of Society Phase following Wave 1 (10 June 2020 to 19 July 2020) and time 3 during the Wave 2 Case Acceleration Phase (21 September 2020 to 21 October 2020) (Figures 1 and 2). Participants were assigned to the clinical group if they reported a clinical cut‐off score of ≥4 on the Conduct Problems scale or ≥7 on the Hyperactivity/Inattention Problems scale of the Strength and Difficulties Questionnaire (SDQ) 42 at Time 1. The “clinical” group was therefore made up of parents who reported their children had clinically elevated difficulties in the areas of conduct and/or hyperactive/inattention problems at Time 1, and the “non‐clinical” group was made up of parents who reported their children did not meet this threshold, at Time 1. These cut off points are based on a population‐based UK survey, with 10% of children reaching this clinical cut off point. 42
FIGURE 1.
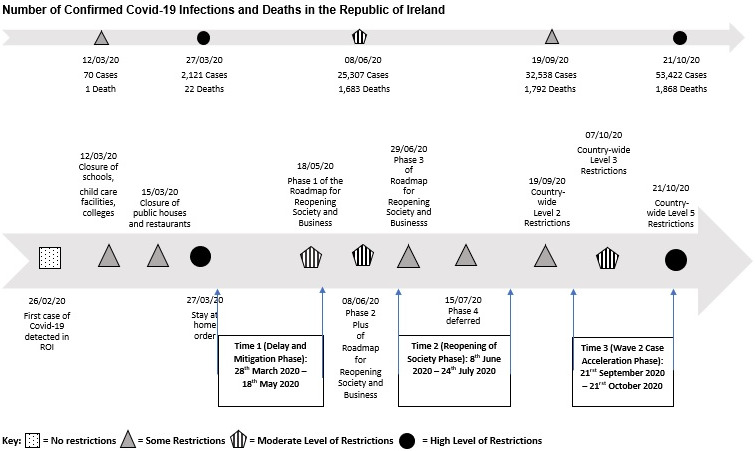
Timeline of wave 1 of the Covid‐19 pandemic in Ireland
FIGURE 2.
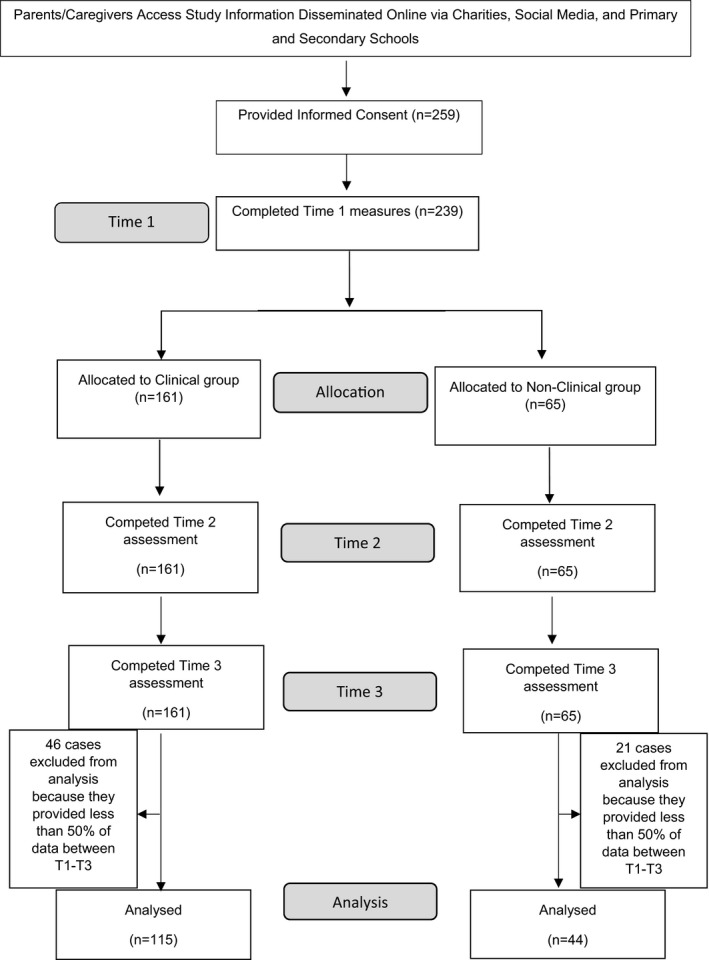
Flow diagram of study participants
2.3. Sample size
A power analysis, conducted with G*Power 3.1, 43 indicated that for one‐tailed statistical tests with P values of .05 and power values of 0.80 to detect moderate differences (d = 0.50) between groups, a sample size of 102 study‐completers (51 cases per cell) would be required.
2.4. Assessment protocol
Demographic information was collected at Time 1 (Table 1). Parent‐reported measures for assessing dependent variables, described below, were administered at all three time points. Cronbach alpha reliability coefficients of almost all measures at all time points exceeded 0.70, indicating acceptable levels of internal consistency reliability. There were two exceptions, discussed below.
TABLE 1.
Demographic and clinical characteristics of participants (N = 159)
| Variable |
Clinical Group N = 115 |
Non‐clinical Group N = 44 |
χ2/Fisher's/ t test |
P | Variable |
Clinical Group N = 115 |
Non‐clinical Group N = 44 |
χ2/ Fisher's/ t test |
P | Variable |
Clinical Group N = 115 |
Non‐clinical Group N = 44 |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Respondent | Mother | 109 (94.78%) | 38 (86.36%) | 4.382 | .101 | SES | Professional workers | 17 (14.78%) | 10 (22.73%) | 13.041 | .044 | Parent training | Any | 63 (54.78%) | 8 (18.18%) |
| Father | 5 (4.35%) | 6 (13.64%) | Managerial & technical | 46 (40.00%) | 24 (54.55%) | Triple P |
11 (9.57%) |
2 (4.55%) | |||||||
| Other | 1 (0.87%) | 0 (0.00%) | Non‐manual | 16 (13.68%) | 8 (18.18%) | Parents Plus | 42 (36.52%) | 4 (9.09%) | |||||||
| Age | 20‐29 | 2 (1.74%) | 1 (2.27%) | 0.919 | .860 | Skilled manual | 20 (17.39%) | 1 (2.27%) | Incredible Years | 16 (13.91%) | 2 (4.55%) | ||||
| 30‐39 | 33 (28.70%) | 13 (29.55%) | Semi‐skilled manual | 9 (7.83%) | 1 (2.27%) | Other | 9 (7.83%) | 1 (2.27%) | |||||||
| 40‐49 | 64 (55.65%) | 26 (59.09%) | Gainfully occupied, not stated | 5 (4.35%) | 0 (0.00%) | Children's diagnoses | ADHD | 83 (72.17%) | 4 (9.09%) | ||||||
| 50‐59 | 16 (13.91%) | 4 (9.09%) | Unemployed | 1 (0.87%) | 0 (0.00%) | ASD |
37 (32.17%) |
3 (6.82%) | |||||||
| Marital status | Married | 80 (69.57%) | 34 (84.09%) | 4.184 | .224 | Country of origin | Ireland | 101 (87.83%) | 37 (84.09%) | 2.485 | .833 | Conduct Disorder | 4 (3.48%) | 0 (0.00%) | |
| Cohabiting | 12 (10.43%) | 4 (9.09%) | Other European | 4 (3.48%) | 1 (2.27%) | Other | 31 (26.96%) | 3 (6.82%) | |||||||
| Separated | 12 (10.43%) | 1 (2.27%) | Family of mixed origins | 6 (5.22%) | 2 (4.55%) | None | 26 (22.61%) | 39 (88.64%) | |||||||
| Single | 11 (9.57%) | 2 (4.55%) | US | 1 (0.87%) | 0 (0.00%) | ||||||||||
| Underlying health problem | 22 (19.13%) | 5 (11.36%) | 1.411 | .235 | South Africa | 1 (0.87%) | 1 (2.27%) | ||||||||
| No. of children | M (SD) | 2.29 (0.915) | 2.18 (1.018) | 0.017 | .531 | New Zealand | 1 (0.87%) | 1 (2.27%) | |||||||
| Missing | 1 (0.87%) | 2 (4.55%) |
A Bonferroni correction was made for 8 demographic variables (Respondent, age, marital status, SES, income, underlying health problem no of children and country of origin). For clarification, parents of 4 children with a diagnosis of ADHD and parents of 3 children with a diagnosis of ASD were included in the “non‐clinical” group, as they had reported a clinical cut‐off score on the Conduct Problems scale or on the Hyperactivity/Inattention Problems scale of the Strength and Difficulties Questionnaire (SDQ), 28 which did not meet the clinical cut off scores, at Time 1.
Abbreviations: ADHD, Attention deficit hyperactivity disorder; ASD, Autistic spectrum disorder; f, frequency; M, Mean; SD, Standard deviation; SES, socio‐economic status.
2.4.1. The Strengths and Difficulties Questionnaire—Parent version (SDQ). 42
The SDQ is a 25‐item screening instrument for assessing emotional and behavioural problems, which has been validated for use with children and adolescents aged 4‐17 years of age. 42 Responses are provided on three‐point scales. The measure has five subscales; emotional difficulties, conduct difficulties, hyperactivity/inattention difficulties, peer relationship problems, prosocial behaviour and a total difficulties score. A review of 48 studies has suggested the Hyperactivity/Inattention scale and Conduct Problems subscales have adequate psychometric properties. 44
2.4.2. The Parental Stress Scale (PSS) 45
The PSS is an 18‐item scale which measures the level of stress associated with raising children within four domains of parenting: rewards, stressors, loss of control and satisfaction. Responses are provided on a 5‐point scale and total scores range from 18 to 90, with higher scores indicating higher levels of parental stress. This measure has been used in recent research examining parental stress during the COVID‐19 pandemic. 46 , 47
2.4.3. The Effects of COVID‐19 Questionnaire (ECQ) 14
The ECQ is a 29‐item scale that evaluates perceptions of COVID‐related stresses, as well as gratitude arising from the COVID‐19 pandemic. This measure was developed for the current study by the authors. Items 1‐8 provide a COVID‐19 Parenting Stress score, items 9‐21 provide a COVID‐19 Personal/Family Stress score, and items 22‐29 provide a COVID‐19 Gratitude score, with responses provided on a 5‐point scale. An exploratory factor analysis of an extended version of the ECQ was conducted by Burke et al, 14 which included an additional subscale related to concerns regarding ageing parents during the COVID‐19 pandemic. Results of Burke et al 14 suggested that ECQ items produced factors that corresponded to a priori subscales, except for items in the Personal/Family Stress subscale which were loaded on two separate factors, however, the alpha value for this scale was found to be satisfactory. In the current study, Cronbach's alpha for the ECQ Gratitude Scale fell just below an acceptable level of reliability at time 3 (alpha = 0.694). With the removal of item 27, “In the past month, how much has your experience of the COVID‐19 crisis led you to feel grateful for your job?,” the ECQ Gratitude scale exceeded a Cronbach's alpha of 0.70 at all three time points. This item was therefore removed for subsequent analyses.
2.4.4. The Impact of Event Scale—Revised (IES‐R) 48
The IES‐R is a 22‐item measure which evaluates subjective distress related to a traumatic event. The IES‐R consists of three subscales characteristic of PTSD responses; intrusion, avoidance, and hyperarousal. The IES‐R has been employed in recent studies measuring subjective distress related to the COVID‐19 pandemic. 49 , 50
2.4.5. The World Health Organization Well‐Being Index (WHO‐5) 51
The WHO‐5 is a 5‐item scale which assesses subjective psychological well‐being. Items are scored on a 6‐point scale, with higher scores indicating higher levels of well‐being. The WHO‐5 has been found to have adequate validity both as a screening tool for depression and as an outcome measure in clinical trials. 51 This measure has been used in research assessing wellbeing during the COVID‐19 pandemic. 52 , 53
2.4.6. The Brief Coping Orientation to Problems Experienced Inventory (Brief COPE) 54
The Brief COPE is a 28‐item scale which measures how frequently positive and negative behaviours and cognitions are employed when coping with a specific stressful situation. Responses are provided on a 4‐point scale, with higher scores suggesting a stronger tendency to utilise the coping behaviour. Two major factors have been found to underlie the Brief COPE scale; avoidant‐focused coping and approach‐focused coping. 55 The Brief COPE Inventory has been utilised in studies investigating coping during the COVID‐19 pandemic 56 and has been found to have satisfactory psychometric properties. 54 In the current study, Cronbach's alpha for the avoidant‐focused coping subscale at all time points were from 0.64 to 0.66, indicating modest levels of internal consistency reliability.
2.5. Data analysis
Data collected were analysed using IBM Statistical Package for the Social Sciences (SPSS) Version 24.0. 57 Twenty multiple imputations were conducted to manage missing data. The imputation procedure was conducted via SPSS Version 24.0. As per scoring instructions for the SDQ, scores for scales were scaled up pro‐rata if at least three items were completed per scale. Missing data were therefore not imputed for SDQ scales which were possible to calculate based on this instruction. Multiple imputations were conducted for all other missing quantitative variables. Means for the clinical and non‐clinical groups during the Delay and Mitigation Phase (Time 1), the Reopening of Society Phase (Time 2), and the Wave 2 Case Acceleration Phase (Time 3), were analysed using 2 × 3 Mixed ANOVAs, following MANOVAs (Table 2). Significant effects of ANOVAs were only interpreted where significant effects (group, time or group X time interactions) had occurred in MANOVAs, as to avoid type I error. Effect sizes comparing means of the clinical and non‐clinical groups, as well as effect sizes comparing the means at three time points for each group were calculated (Table 3). The following criteria for effect sizes was followed; d = 0.20 small, d = 0.50 medium and d = 0.80 large. 58 The results below confirm the impressions given by the Panels in Figure 3.
TABLE 2.
Means of Clinical and Non‐clinical groups on summary variables at times 1, 2 and 3 (N = 159) and ANOVA results
| Clinical Group | Non‐clinical Group | Groups | Time | GXT | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time 1 | Time 2 | Time 3 | Time 1 | Time 2 | Time 3 | F | P | F | P | F | P | ||
| Child behaviour | |||||||||||||
| SDQ total difficulties | M | 21.81 | 20.53 | 19.15 | 9.11 | 10.69 | 10.09 | 152.767 | <.001 | 3.210 | .045 | 10.303 | <.001 |
| SD | 5.07 | 5.68 | 5.60 | 4.79 | 5.13 | 5.61 | |||||||
| Parental sources of stress | |||||||||||||
| PSS parenting stress | M | 48.77 | 48.90 | 47.30 | 40.12 | 39.51 | 38.81 | 36.440 | <.001 | 2.318 | .106 | 0.241 | .760 |
| SD | 9.50 | 9.46 | 9.94 | 8.79 | 9.05 | 8.41 | |||||||
| ECQ parenting stress | M | 19.18 | 20.69 | 17.56 | 15.66 | 17.36 | 15.04 | 10.308 | .002 | 10.272 | <.001 | 0.393 | .655 |
| SD | 7.25 | 7.61 | 6.67 | 5.76 | 5.50 | 5.38 | |||||||
| ECQ family stress | M | 32.72 | 29.98 | 28.83 | 27.73 | 27.35 | 25.74 | 7.590 | .007 | 6.459 | .002 | 1.178 | .309 |
| SD | 10.24 | 9.11 | 8.45 | 8.99 | 8.69 | 7.37 | |||||||
| Parental stress responses | |||||||||||||
| IES‐R total | M | 21.56 | 21.25 | 23.03 | 17.44 | 16.27 | 16.86 | 6.124 | .014 | 0.632 | .532 | 0.470 | .625 |
| SD | 14.09 | 14.63 | 13.20 | 12.94 | 11.43 | 12.13 | |||||||
| IES‐R avoidance | M | 7.46 | 7.40 | 7.46 | 6.02 | 5.62 | 5.81 | 4.051 | .046 | 0.120 | .887 | 0.062 | .940 |
| SD | 6.18 | 5.89 | 4.82 | 5.48 | 5.29 | 4.36 | |||||||
| IES‐R Intrusion | M | 8.44 | 7.61 | 8.59 | 6.74 | 6.56 | 6.25 | 3.653 | .058 | 0.566 | .568 | 0.869 | .420 |
| SD | 6.73 | 6.04 | 5.69 | 4.94 | 5.71 | 5.08 | |||||||
| IES‐R hyperarousal | M | 6.15 | 6.51 | 6.98 | 4.68 | 5.39 | 4.80 | 5.711 | .018 | 1.252 | .287 | 1.078 | .342 |
| SD | 4.28 | 4.95 | 4.35 | 4.06 | 4.69 | 3.96 | |||||||
| Parental well‐being | |||||||||||||
| WHO‐5 well‐being | M | 44.83 | 46.23 | 44.71 | 54.73 | 52.73 | 54.48 | 9.302 | .003 | 0.020 | .981 | 0.822 | .440 |
| SD | 20.15 | 18.43 | 17.63 | 18.36 | 21.12 | 17.76 | |||||||
| ECQ gratitude | M | 26.55 | 25.78 | 25.38 | 27.41 | 26.51 | 27.09 | 1.939 | .166 | 1.697 | .185 | 0.576 | .563 |
| SD | 5.65 | 6.19 | 5.27 | 4.64 | 5.09 | 5.04 | |||||||
| Parental coping | |||||||||||||
| Brief COPE Avoidant coping | M | 20.82 | 20.72 | 21.83 | 19.31 | 20.28 | 19.89 | 4.902 | .028 | 3.055 | .049 | 2.904 | .056 |
| SD | 4.07 | 3.65 | 3.94 | 3.49 | 4.38 | 3.87 | |||||||
| Brief COPE Approach coping | M | 32.69 | 31.93 | 30.85 | 32.13 | 30.73 | 28.62 | 2.816 | .095 | 14.327 | <.001 | 1.408 | .246 |
| SD | 5.39 | 5.62 | 5.44 | 6.36 | 5.02 | 5.63 | |||||||
Abbreviations: ECQ, Effects of COVID‐19 Questionnaire; F, F value form groups X time ANOVA; GXT, groups X time interaction from ANOVA; IES‐R, Impact of Event Scale—Revised; M, mean; PSS, Parenting stress scale; SD, Standard deviation; SDQ, Strengths and difficulties Questionnaire; WHO‐5, World Health Organization Well‐Being Index.
TABLE 3.
Effect sizes for comparisons of means in Clinical and Non‐clinical groups (N = 159)
| Clinical vs Non‐clinical Group | Clinical Group at Times 1, 2 and 3 | Non‐clinical Group at Times 1, 2 and 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Clinical vs Non‐clinical Gp at Time 1 | Clinical vs Non‐clinical Gp at Time 2 | Clinical vs Non‐clinical Gp at Time 3 | Clinical Gp Time 1 vs Time 2 | Clinical Gp Time 1 vs Time 3 | Clinical Gp Time 2 vs Time 3 | Non‐clinical Gp Time 1 vs Time 2 | Non‐clinical Gp Time 1 vs Time 3 | Non‐clinical Gp Time 2 vs Time 3 | ||
| Child behaviour | ||||||||||
| SDQ total difficulties | d | 2.54 | 1.78 | 1.62 | 0.24 | 0.50 | 0.24 | −0.32 | −0.19 | 0.11 |
| 95% CI | 2.10, 2.99 | 1.38, 2.18 | 1.23, 2.01 | −0.02, 0.50 | 0.24, 0.76 | −0.01, 0.50 | −0.74, 0.10 | −0.61, 0.23 | −0.31, 0.53 | |
| Parental sources of stress | ||||||||||
| PSS parenting stress | d | 0.93 | 0.95 | 0.89 | −0.01 | 0.15 | 0.16 | 0.07 | 0.15 | 0.08 |
| 95% CI | 0.57, 1.29 | 0.58, 1.31 | 0.53, 1.25 | −0.27, 0.24 | −0.12, 0.41 | −0.09, 0.42 | −0.35, 0.49 | −0.27, 0.57 | −0.34, 0.50 | |
| ECQ parenting stress | d | 0.51 | 0.47 | 0.40 | −0.20 | 0.23 | 0.44 | −0.30 | 0.11 | 0.43 |
| 95% CI | 0.16, 0.86 | 0.12, 0.82 | 0.05, 0.75 | −0.46, 0.06 | −0.03, 0.49 | 0.18, 0.70 | −0.72, 0.12 | −0.31, 0.53 | 0.01, 0.85 | |
| ECQ family stress | d | 0.50 | 0.29 | 0.38 | 0.28 | 0.42 | 0.13 | 0.04 | 0.24 | 0.20 |
| 95% CI | 0.15, 0.86 | −0.06, 0.64 | 0.03, 0.73 | 0.02, 0.54 | 0.15, 0.68 | −0.13, 0.39 | −0.37, 0.46 | −0.18, 0.66 | −0.22, 0.62 | |
| Parental stress responses | ||||||||||
| IES‐R total | d | 0.30 | 0.36 | 0.48 | 0.02 | −0.11 | −0.13 | 0.10 | 0.05 | −0.05 |
| 95% CI | −0.05, 0.65 | 0.01, 0.71 | 0.13, 0.83 | −0.24, 0.28 | −0.37, 0.15 | −0.39, 0.13 | −0.32, 0.51 | −0.37, 0.46 | −0.47, 0.37 | |
| Parental well‐being | ||||||||||
| WHO‐5 well‐being | d | −0.50 | −0.34 | −0.55 | −0.07 | 0.01 | 0.08 | 0.10 | 0.01 | −0.09 |
| 95% CI | −0.85, −0.15 | −0.69, 0.01 | −0.91, −0.20 | −0.33 0.19 | −0.25, 0.26 | −0.17, 0.34 | −0.32, 0.52 | −0.40, 0.43 | −0.51, 0.33 | |
| ECQ gratitude | d | −0.16 | −0.12 | −0.33 | 0.13 | 0.21 | 0.07 | 0.18 | 0.07 | −0.11 |
| 95% CI | −0.51, 0.19 | −0.47, 0.22 | −0.68, 0.02 | −0.13, 0.39 | −0.05, 0.47 | −0.19, 0.33 | −0.23, 0.60 | −0.35, 0.48 | −0.53, 0.30 | |
| Parental coping | ||||||||||
| Brief COPE avoidant coping | d | 0.39 | 0.11 | 0.49 | 0.03 | −0.25 | −0.29 | −0.25 | −0.16 | 0.09 |
| 95% CI | 0.04, 0.74 | −0.23, 0.46 | 0.14, 0.85 | −0.23, 0.28 | −0.51, 0.01 | −0.55, −0.03 | −0.66, 0.17 | −0.58, 0.26 | −0.32, 0.51 | |
| Brief COPE approach coping | d | 0.10 | 0.22 | 0.41 | 0.14 | 0.34 | 0.20 | 0.24 | 0.58 | 0.40 |
| 95% CI | −0.25, 0.45 | −0.13, 0.57 | 0.06, 0.76 | −0.12, 0.40 | 0.08, 0.60 | −0.06, 0.45 | −0.18, 0.66 | 0.16, 1.01 | −0.03, 0.82 | |
Abbreviations: CI, Confidence interval; d, effect size; ECQ, Effects of COVID‐19 Questionnaire; IES‐R, Impact of Event Scale—Revised; PSS, Parenting stress scale; SDQ, Strengths and difficulties Questionnaire; SDQ, Strengths and difficulties Questionnaire; Gp, Group; WHO‐5, World Health Organization Well‐Being Index.
FIGURE 3.
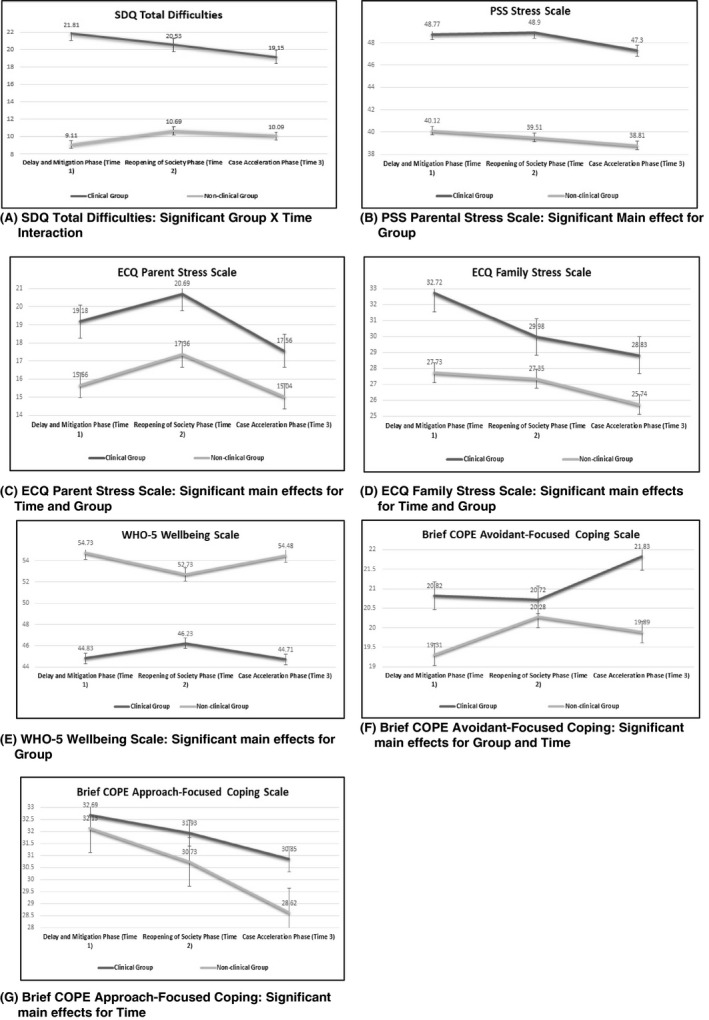
Means of clinical and non‐clinical groups at the Delay and mitigation phase (Time 1), the reopening of society phase (Time 2), and the case acceleration phase (Time 3) on measures of child behaviour problems, parental stress, parental well‐being, and coping
3. RESULTS
3.1. Parental sources of stress
The first research question concerned the effect of presence or absence of significant levels of child externalising behaviour problems at the outset of the COVID‐19 pandemic and the passage of time on variables in the Parental Sources of Stress, as measured by the PSS, the Parenting Stress scale of the ECQ and the Personal/Family Stress scale of the ECQ. A significant multivariate effect for group (Wilks’ λ = 0.795, F(3, 155) = 13.289, P =< .001, partial eta squared = 0.205) and for time were identified (Wilks’ λ = 0.802, F(6, 152) = 6.247, P =< .001, partial eta squared = 0.198). ANOVA results identified significant main effects for group on all three variables in this domain, indicating that parents in the clinical group, compared with parents in the non‐clinical group, displayed significantly higher levels of stress related to being a parent, of large effect (d = 0.89‐0.95), stress related to parenting during the COVID‐19 pandemic, of small to medium effect (d = 0.40‐0.51) and stress related to the impact of the COVID‐19 pandemic on personal/family factors, of small to medium effect (d = 0.29‐0.50). A significant main effect for time was documented for both the ECQ Parenting Stress and Personal/Family Stress scales. Pairwise comparisons for the ECQ Parenting Stress scale suggested that the Clinical group exhibited a significant increase in stress related to parenting during the COVID‐19 pandemic, of small effect between the Delay and Mitigation Phase (Time 1) and the Reopening of Society Phase (Time 2) (P = .006; d = −0.20), followed by a significant decrease in stress of small effect, between the Reopening of Society Phase (Time 2) and the Case Acceleration Phase (Time 3) (P =< .001; d = 0.44). The non‐clinical group demonstrated a similar pattern, exhibiting a significant increase of small effect between the Delay and Mitigation Phase (Time 1) and the Reopening of Society Phase (Time 2) (P = .038; d = −0.30), followed by a significant decrease in stress related to parenting during the COVID‐19 pandemic between the Reopening of Society Phase (Time 2) and the Case Acceleration Phase (Time 3) (P = .010; d = 0.43). Pairwise comparisons for the ECQ Personal/Family Stress scale suggested that the clinical group exhibited a significant downward trajectory of a reduction in stress related to the impact of COVID‐19 on the family from Time 1 to Time 3, of small effect (P =< .001; d = 0.42).
3.2. Parental wellbeing
The second research question concerned the effect of presence or absence of significant levels of child externalising behaviour problems at the outset of the COVID‐19 pandemic and the passage of time on variables in the Parental Wellbeing domain, as measured by the WHO‐5 and the ECQ Gratitude scale. A significant multivariate group effect was found for this domain (Wilks’ λ = .931, F(2, 156) = 5.822, P = .004, partial eta squared = 0.069). ANOVA results indicated a significant effect for group on parent wellbeing, as measured by the WHO‐5 scale, with the clinical group experiencing significantly lower levels of wellbeing, in comparison to the non‐clinical group. Effect sizes for the WHO‐5 suggest that parents in the clinical group displayed poorer wellbeing of medium effect size at Time 1 (d = −0.50), of small effect at Time 2 (d = −0.34), and of medium effect at Time 3 (d = −0.55).
3.3. Parental stress responses
The third research question concerned the effect of presence or absence of significant levels of child externalising behaviour problems at the outset of the COVID‐19 pandemic and the passage of time on variables in the Parental Stress Responses domain, as measured by three IES‐R variables. The MANOVA for this domain did not find any significant multivariate effects and therefore ANOVA results were not interpreted.
3.4. Parental coping
The fourth research question concerned the effect of presence or absence of significant levels of child externalising behaviour problems at the outset of the COVID‐19 pandemic and the passage of time on variables in the Parental Coping domain, which consisted of the Brief COPE avoidant‐focused coping and approach‐focused coping scales. A significant multivariate effect for group (Wilks’ λ = 0.954, F(2, 156) = 3.794, P = .025, partial eta squared = 0.046) and for time (Wilks’ λ = 0.814, F(4, 154) = 8.774, P < .001, partial eta squared = 0.186) were identified. ANOVA results identified significant effects for group for avoidant‐focused coping, with the clinical group engaging in a significantly higher level of avoidant‐focused coping strategies in comparison to the non‐clinical group (P = .028), of small effect, at Time 1 (d = 0.39) and at Time 3 (d = 0.49). ANOVA results identified significant main effects of time for both avoidant‐focused coping and approach‐focused coping. Pairwise comparisons suggested that between the Reopening of Society Phase (Time 2) and the Case Acceleration Phase (Time 3), the clinical group displayed a significant increase, of small effect, in level of avoidant‐focused coping strategies employed (P = .004; d = −0.29) and a significant decrease, of small effect, in level of approach‐focused coping strategies employed (P = .046; d = 0.20). Between Time 1 and Time 3, the clinical group displayed a significant increase in use of avoidant‐focused coping strategies (P = .003), of small effect size (d = −0.25) and displayed a significant decrease in use of approach‐focused coping strategies (P =.001), of small effect size (d = 0.34).
A significant decrease in the use of approach‐focused coping strategies was identified in the non‐clinical group between the Reopening of Society Phase (Time 2) and the Case Acceleration Phase (Time 3) (P = .012; d = 0.40). Between Time 1 and Time 3, the non‐clinical group displayed a significant decrease in approach‐focused coping strategies (P = .002), of medium effect size (d = 0.58).
3.5. Child behaviour
The fifth research question concerned the effect of presence or absence of significant levels of parent‐reported child externalising behaviour problems at the outset of the COVID‐19 pandemic and the passage of time on variables in the child behaviour domain, which consisted of four SDQ variables. The MANOVA for this domain yielded a significant group X time interaction effect (Wilks’ λ = 0.748, F(8, 150) = 6.311, P < .001, partial eta squared = 0.252), and a significant effect for group (Wilks’ λ = 0.359, F(4, 154) = 68.718, P < .001, partial eta squared = 0.641). ANOVA results indicated that significant group X time interactions occurred on the following subscales of the SDQ: Total Difficulties, Conduct Problems, and Hyperactivity/Inattention Problems. The pattern of results was similar for all three subscales. As the Total Difficulties subscale incorporates items from the Conduct Problems, and Hyperactivity/Inattention Problems scales, tests of simple main effects on the Total Difficulties Scale are reported. On the SDQ Total Difficulties scale, there was a statistically significant difference between groups at all time points. Pairwise comparisons suggested the clinical group exhibited a downward trajectory of significant reductions in parent‐reported child emotional and behavioural problems, of small effect, between the Delay and Mitigation Phase (Time 1) and the Reopening of Society Phase (Time 2) (P = .001; d = 0.24) and between the Reopening of Society Phase (Time 2) and the Case Acceleration Phase (Time 3) (P = .007; d = 0.24). A medium effect (d = 0.50) for improvement in scores for parent‐reported child behaviour and emotional difficulties between the Delay and Mitigation Phase (Time 1) and the Case Acceleration Phase (Time 3) (P < .001) was identified, indicating that parents of children in the clinical group perceived their children to demonstrate positive adjustment as the COVID‐19 pandemic progressed. The non‐clinical group exhibited a significant increase, of small effect (d = −0.32), in parent‐reported child emotional and behavioural problems between the Delay and Mitigation Phase (Time 1) and the Reopening of Society Phase (Time 2) (P = .018).
4. DISCUSSION
The aim of this study was to determine how the presence or absence of significant levels of parent‐reported child externalising difficulties at the outset of the COVID‐19 pandemic, and the passage of time over three different phases of Wave 1 of the COVID‐19 pandemic, affected parents’ perception of their children's behavioural difficulties, sources of stress in their lives, their stress responses, their well‐being, and their coping strategies. Partial support was provided for hypothesis 1; that parents of children with externalising difficulties, in comparison to parents of children without such difficulties, would exhibit significantly poorer outcomes. Parents of children with externalising difficulties reported significantly higher levels of stress related to being a parent, stress related to parenting and personal/family factors during the COVID‐19 pandemic, significantly lower levels of wellbeing, and engaged in significantly higher levels of avoidant‐focused coping strategies, in comparison to parents of children without externalising difficulties. Similar results have been documented during the pandemic in parents of children with autism, 59 , 60 who have been found to report higher levels of parental stress, anxiety, depression, and lower levels of wellbeing, and in caregivers of children and adults with ID, 61 who reported significantly higher levels of anxiety, depression, and feelings of defeat/entrapment. Emerging research has identified the negative impact which stress experienced by parents during the COVID‐19 pandemic can have on their children, including an increase in the likelihood for child abuse and maltreatment, 62 , 63 highlighting the need for adequate interventions to support parents manage stress.
In our study, parents of children with externalising difficulties, however, did not report greater distress, as per the IES‐R, than parents of children without externalising difficulties. Recent research suggests that individuals who accessed psychiatric services prior to the COVID‐19 pandemic have significantly higher levels of trauma responses related to the pandemic, in comparison with individuals who did not access such services. 64 The majority of studies examining trauma responses to the pandemic in different cohorts, however, are cross‐sectional in nature, 65 and additional controlled studies are required. Further analysis of our data to determine the proportion of parents who met the cut‐off point for difficulties indicative of PTSD and variables associated with this elevated level of trauma response, would provide useful information to assist in identifying parents who may be most at risk of developing PTSD related to the pandemic.
Partial support was provided for hypothesis 2: that there would be a significant difference between scores on variables in all domains obtained across the three time points of the study. Parents in both groups documented a significant increase in stress related to parenting during the COVID‐19 pandemic between the Delay and Mitigation Phase (Time 1) and the Reopening of Society Phase (Time 2), followed by a significant decrease in stress of small effect, between the Reopening of Society Phase (Time 2) and the Case Acceleration Phase (Time 3). This may suggest that parents perceived parenting during the easing of restrictions as more stressful, in comparison to parenting during stay‐at‐home orders, which may reflect an increased level of responsibility in ensuring children's adherence to public health measures, as opportunities for socialising increased. Parental stress and anxiety in response to the reopening of schools during the COVID‐19 pandemic is an area in which research is emerging. 66 However, there is no published research yet, to our knowledge, examining parent responses to the easing of restrictions.
Of concern is that parents in both groups in our study, exhibited a significant downward trajectory in the use of approach‐focused coping strategies from Time 1 to Time 3, and that parents in the clinical group exhibited a significant increase in the use of avoidant‐focused strategies from Time 1 to Time 3. In parents of children with externalising difficulties, an avoidant‐focused coping style has been found to be involved in a process which predicts an increased level of parental depression. 67 Actively engaging in avoidant‐focused coping strategies during the COVID‐19 pandemic has been associated with mental health difficulties in adults. 68 These associations highlight the need for supports to assist parents in developing sustainable and helpful coping strategies.
There were no significant differences, however, found between time points for stress related to being a parent, distress responses to the COVID‐19 pandemic, psychological wellbeing or levels of gratitude experienced. This is somewhat similar to findings of a longitudinal study conducted in China, examining the impact of the COVID‐19 pandemic in the general population, 69 which found no significant changes in stress, anxiety and depression levels between two time points, four weeks apart, during the pandemic. A statistically significant longitudinal reduction in mean IES‐R scores was reported, however, the mean IES‐R scores were above the cut‐off scores, suggesting that the reduction in scores was not clinically significant. Our findings regarding wellbeing in parents differed in comparison to findings of longitudinal study conducted with the UK general population, 70 who reported an increase in positive well‐being in participants from Wave 1 to Wave 2, and from Wave 1 to Wave 3.
Parents of children with externalising difficulties did not demonstrate a trajectory of decreasing adjustment over time, in comparison to parents of children without externalising difficulties, for parenting stress, stress related to the COVID‐19 pandemic, wellbeing, distress responses to the COVID‐19 pandemic, or coping. This did not support hypothesis 3: That compared with parents of children without externalising difficulties, parents of children with externalising difficulties would report poorer adjustment as the COVID‐19 pandemic progressed. Instead, the clinical group, but not the non‐clinical group, exhibited a significant downward trajectory of reduction in stress related to the impact of the COVID‐19 pandemic on personal/family factors from Time 1 to Time 3. This may reflect the ability of parents of children with externalising difficulties to adapt over time to the changes in family life brought about by the COVID‐19 pandemic, which could be understood in the context of resilience. 71 One hypothesis to explain this is that the experiences in raising a child with an externalising difficulty has enabled parents to develop the ability to adapt to novel stressful situations experienced within their family systems. Many families of children with neurodevelopmental diagnoses display resilience in response to behavioural, service‐based, and societal challenges. 72 Recent research, however, has found families of youth with comorbid ADHD and autism to have significantly lower levels of family resilience than youth with solely ADHD, or youth without autism or ADHD, 73 suggesting that resilience in this cohort is an area requiring further exploration. Another possibility is that this result reflects regression to the mean, which is a phenomenon which may occur in repeated measurements research, because of values being observed with random error. 74 Children with externalising difficulties, in comparison to children without such difficulties, showed significant improvements in adjustment over three time points during Wave 1 of the COVID‐19 pandemic, as per the parent report. This result did not support hypothesis 4, which predicted that children with externalising difficulties would show poorer adjustment on parent‐reported indices of behavioural difficulties as the COVID‐19 pandemic progressed. Although longitudinal data from the UK found a gradual decrease in child internalising and externalising behaviour during the COVID‐19 pandemic, children who had higher levels of externalising behaviour prior to lockdown, experienced more stress during lockdown, resulting in an increase in externalising behaviour, 75 which is not consistent with our findings.
The resilience theory discussed above is one hypothesis for our results, whereby children with externalising difficulties exhibited a better ability to adjust and adapt as time progressed. Another factor which may have contributed to this finding is that schools were closed in Ireland for the duration of this study. Children with externalising difficulties often experience difficulties in school, such as children with ADHD may have difficulty maintaining concentration or staying seated, or children with autism may struggle with social interactions with peers and may experience distress related to transitions. For children with such difficulties, a break from the demands of an environment which is bound by many rules and social expectations may have been experienced as a relief. Thematic analysis of reports of parents of children with ADHD during the COVID‐19 pandemic in France, 76 suggested an improvement children's anxiety prior to the pandemic, which was related to less school‐related strain and flexible schedules. Another possibility is that children with externalising difficulties may have benefited from increased time spent with, and availability of, family members. Strengthening relationships and development of skills, such as tolerance, during stay‐at‐home orders has been reported by Australian families. 77 As parental responsiveness progressively supports the child's modulation, gradation, and containment of strong affect, 78 it is possible that children benefited from increased proximity to caregivers who could support this process. As highlighted above, it is possible that this result also may reflect regression to the mean. It is important to note that we are unable to make a comparison to pre‐pandemic levels of externalising difficulties experienced by this cohort. Cross‐sectional studies have suggested a deterioration in parental report of children's ADHD difficulties, such as inattention and hyperactivity, during the pandemic, in comparison to prior to the pandemic. 79 A strength of our study, however, is the longitudinal design, in comparison with cross‐sectional studies, which rely on retrospective report.
This preliminary research adds to the expanding evidence base of the impact of the COVID‐19 pandemic. Our findings have advanced knowledge in the field as this is the first longitudinal study, to our knowledge, examining the impact of the COVID‐19 pandemic on parents of children with externalising difficulties in Ireland. Our results provide important information regarding the trajectory of psychological outcomes in parents of children with externalising difficulties, and in their children themselves, over the first wave of the COVID‐19 pandemic. These results will be useful to clinicians engaging with families of children with externalising difficulties and our results have provided useful preliminary evidence to be further explored and expanded on in subsequent research.
5. LIMITATIONS AND FUTURE RESEARCH
Limitations of the current study included that data collected was not compared with data collected in pre‐pandemic circumstances, in addition to unequal group sizes. Additionally, a high level of attrition resulted in a reduction in sample size (N = 239‐159) as only participants who provided >50% of data over the three time points were included in analyses, as it has been suggested that when imputing data, if proportions of missing data are very large on important variables, then results may only be considered as hypothesis generating. 80 Future research is recommended to examine mediating or moderating variables that may have impacted our results, for example, closure of schools, reduction of access to services, increased level of time spent at home, reduction of social interaction, and change in routine. Research of outcomes for this cohort during subsequent second and third waves in Ireland would provide useful information regarding trends as the COVID‐19 pandemic progressed, in addition to a qualitative exploration of the experiences of parents of children with externalising difficulties during different phases of the pandemic. Considering the significant reduction in parent‐reported child behavioural and emotional difficulties documented in the clinical group in our study, future research should measure resilience and possible stress‐related growth in this population in response to the COVID‐19 pandemic.
Practical implications of these results include the need for Irish health services to adapt to support the psychological wellbeing of parents of children with externalising difficulties. Intervention for externalising difficulties, in the context of ADHD or autism, generally includes psychoeducation, medication, family intervention to promote rule‐following at home, school intervention focusing on the management of school‐based learning difficulties and conduct problems; child‐focused social skills training, and dietary assessment and intervention. 81 Interventions specifically addressing parent wellbeing do not seem to be standard practice in Irish public health services. Despite this, research has highlighted the positive benefits of intervention for parents of children with externalising difficulties which focus on parental wellbeing 82 or which have an added component specifically addressing parental stress. 83 A second implication of this study is recognising the ability of children with externalising difficulties, and their parents, to adapt and cope with challenging circumstances, such as the COVID‐19 pandemic. This highlights the importance of adopting a strengths‐based approach when working with children with externalising difficulties and their parents, which can be encouraged through positive psychology. Adopting a strengths‐based perspective, opposed an approach which is deficit‐focused, involves emphasising the positives and strengths held by the child and focuses on building well‐being and resilience. 84 Preliminary research has identified the positive impact of adopting a strengths‐based intervention to managing externalising difficulties. 85 However, controlled trials in this area are required.
6. CONCLUSION
This study provides important information regarding the trajectory of psychological outcomes in parents of children with externalising difficulties over the first wave of the COVID‐19 pandemic. Results highlight the need for the provision of adequate supports to assist this cohort to manage stress, improve wellbeing, and to develop sustainable coping strategies. Results also demonstrate the ability of children with externalising difficulties to adjust and adapt during the COVID‐19 pandemic.
DISCLOSURE
no
ACKNOWLEDGEMENTS
The authors would like to thank the participants, who took part in this research during the COVID‐19 pandemic. The authors would also like to thank Niki Nearchou, Assist Professor / Ad Astra Fellow, UCD, who was consulted regarding statistical queries which arose during the course of the research. The primary author would like to thank HSE CHO 8 (Laois/Offaly), who sponsor her position as Trainee Clinical Psychologist.
Berry A, Burke T, Carr A. The impact of the first wave of the Covid‐19 pandemic on parents of children with externalising difficulties in ireland: A longitudinal cohort study. Int J Clin Pract. 2021;75:e14941. doi: 10.1111/ijcp.14941
A preprint of a previous manuscript was posted on Authorea, Wiley's under review service, which can be accessed at https://www.authorea.com/users/412075/articles/520881‐the‐impact‐of‐the‐first‐wave‐of‐the‐COVID‐19‐pandemic‐on‐parents‐of‐children‐with‐externalising‐difficulties‐in‐ireland‐a‐longitudinal‐cohort‐study
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Perumal V, Curran T, Hunter M. First case of COVID‐19 in Ireland. Ulster Med J. 2020;89(2):128. [PMC free article] [PubMed] [Google Scholar]
- 2. Department of Education . COVID‐19 ‐ Statement from the Department of Education and Skills. https://www.gov.ie/en/press‐release/92724a‐COVID‐19‐statement‐from‐the‐department‐of‐education‐and‐skills/ (Accessed 20 May 2020)
- 3. Department of the Taoiseach . Speech of an Taoiseach, Leo Varadkar TD, Government Buildings, 27 March 2020. https://www.gov.ie/en/speech/f27026‐speech‐of‐an‐taoiseach‐leo‐varadkar‐td‐government‐buildings‐27‐march/ (Accessed 20 May 2020)
- 4. Department of the Taoiseach . Roadmap for Reopening Society & Business. Government of Ireland. https://www.gov.ie/en/press‐release/e5e599‐government‐publishes‐roadmap‐to‐ease‐COVID‐19‐restrictions‐and‐reope/ (Accessed 20 May 2020)
- 5. Government of Ireland . COVID‐19 Resilience and Recovery 2021: The Path Ahead. https://www.gov.ie/en/campaigns/resilience‐recovery‐2020‐2021‐plan‐for‐living‐with‐COVID‐19/ (Accessed 27 July 2020)
- 6. Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID‐19 pandemic: a systematic review and meta‐analysis. J Affect Disord. 2021;281:91‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu X, Zhu M, Zhang R, et al. Public mental health problems during COVID‐19 pandemic: a large‐scale meta‐analysis of the evidence. Transl Psychiatry. 2021;11(1):384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Phiri P, Ramakrishnan R, Rathod S, et al. An evaluation of the mental health impact of SARS‐CoV‐2 on patients, general public and healthcare professionals: a systematic review and meta‐analysis. E Clin Med. 2021;34:100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Salari N, Hosseinian‐Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID‐19 pandemic: a systematic review and meta‐analysis. Glob Health. 2020;16(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883‐892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van der Velden P, Hyland P, Contino C, von Gaudecker H, Muffels R, Das M. Anxiety and depression symptoms, the recovery from symptoms, and loneliness before and after the COVID‐19 outbreak among the general population: findings from a Dutch population‐based longitudinal study. PLoS One. 2021;16(1):e0245057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hyland P, Shevlin M, McBride O, et al. Anxiety and depression in the Republic of Ireland during the COVID‐19 pandemic. Acta Psychiatr Scand. 2020;142(3):249‐256. [DOI] [PubMed] [Google Scholar]
- 13. Karatzias T, Shevlin M, Murphy J, et al. Posttraumatic stress symptoms and associated comorbidity during the COVID‐19 pandemic in Ireland: a population‐based study. J Trauma Stress. 2020;33(4):365‐370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Burke T, Berry A, Taylor LK, et al. Increased psychological distress during COVID‐19 and quarantine in Ireland: a national survey. J Clin Med. 2020;9(11):3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stafford O, Berry A, Taylor LK, et al. Comorbidity and COVID‐19: investigating the relationship between medical and psychological well‐being. Irish J Psychol Med. 2021;9:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hyland P, Shevlin M, Murphy J, et al. A longitudinal assessment of depression and anxiety in the Republic of Ireland before and during the COVID‐19 pandemic. Psychiatry Res. 2021;300:113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nearchou F, Douglas E. Traumatic distress of COVID‐19 and depression in the general population: exploring the role of resilience, anxiety, and hope. Int J Environ Res Public Health. 2021;18(16):8485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Feinberg ME, Mogle J, Lee J‐K, et al. Impact of the COVID‐19 pandemic on parent, child, and family functioning. Fam Process. 2021;10(10):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gassman‐Pines A, Ananat E, Fitz‐Henley J. COVID‐19 and parent‐child psychological well‐being. Pediatrics. 2020;146(4):e2020007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Westrupp EM, Bennett C, Berkowitz T, et al. Child, parent, and family mental health and functioning in Australia during COVID‐19: comparison to pre‐pandemic data. Eur Child Adolesc Psychiatry. 2021. 10.1007/s00787-021-01861-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chung G, Lanier P, Wong P. Mediating effects of parental stress on harsh parenting and parent‐child relationship during Coronavirus (COVID‐19) pandemic in Singapore. J Family Violence. 2020;1‐12. 10.1007/s10896-020-00200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barroso N, Mendez L, Graziano P, Bagner D. Parenting stress through the lens of different clinical groups: a systematic review & meta‐analysis. J Abnorm Child Psychol. 2017;46(3):449‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Theule J, Wiener J, Tannock R, Jenkins J. Parenting stress in families of children with ADHD. J Emot Behav Disord. 2010;21(1):3‐17. [Google Scholar]
- 24. Chatterjee S, Barikar CM, Mukherjee A. Impact of COVID‐19 pandemic on pre‐existing mental health problems. Asian J Psychiatry. 2020;51:102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Neece C, Green S, Baker B. Parenting stress and child behavior problems: a transactional relationship across time. Am J Intellect Dev Disabil. 2012;117(1):48‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hill AP, Zuckerman KE, Hagen AD, et al. Aggressive behavior problems in children with autism spectrum disorders: Prevalence and correlates in a large clinical sample. Res Autism Spectr Disord. 2014;8(9):1121‐1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bauminger N, Solomon M, Rogers S. Externalizing and internalizing behaviors in ASD. Autism Res. 2010;3(3):101‐112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Psychiatric Association . Diagnostic and statistical manual of mental disorders: diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 29. Ahmad S, Hinshaw S. Attention‐deficit/hyperactivity disorder, trait impulsivity, and externalizing behavior in a longitudinal sample. J Abnorm Child Psychol. 2016;45(6):1077‐1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lieberman A, Chu A, Van Horn P, Harris W. Trauma in early childhood: empirical evidence and clinical implications. Dev Psychopathol. 2011;23(2):397‐410. [DOI] [PubMed] [Google Scholar]
- 31. Ford J, Chapman J, Connor D, Cruise K. Complex trauma and aggression in secure juvenile justice settings. Crim Justice Behav. 2012;39(6):694‐724. [Google Scholar]
- 32. Dekker M, Koot H, Ende J, Verhulst F. Emotional and behavioral problems in children and adolescents with and without intellectual disability. J Child Psychol Psychiatry. 2002;43(8):1087‐1098. [DOI] [PubMed] [Google Scholar]
- 33. Benson B, Brooks W. Aggressive challenging behaviour and intellectual disability. Curr Opin Psychiatry. 2008;21(5):454‐458. [DOI] [PubMed] [Google Scholar]
- 34. Vasilopoulou E, Nisbet J. The quality of life of parents of children with autism spectrum disorder: a systematic review. Res Autism Spectr Disord. 2016;23:36‐49. [Google Scholar]
- 35. Lovell B, Moss M, Wetherell M. With a little help from my friends: Psychological, endocrine and health corollaries of social support in parental caregivers of children with autism or ADHD. Res Dev Disabil. 2012;33(2):682‐687. [DOI] [PubMed] [Google Scholar]
- 36. Masi A, Mendoza Diaz A, Tully L, et al. Impact of the COVID‐19 pandemic on the well‐being of children with neurodevelopmental disabilities and their parents. J Paediatr Child Health. 2021;57(5):631‐636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rogers G, Perez‐Olivas G, Stenfert Kroese B, et al. The experiences of mothers of children and young people with intellectual disabilities during the first COVID‐19 lockdown period. J Appl Res Intellect Disabil. 2021;75:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Crowley P, Hughes A. The impact of COVID‐19 pandemic and the societal restrictions on health and wellbeing on service capacity and delivery: a plan for health care and population health recovery. Health Service Executive. 2021; Available from: https://www.hse.ie/eng/about/who/qid/COVID‐19‐qi‐learning/qi‐resources‐to‐support‐learning‐from‐covid19/COVID‐19‐pandemic‐impact‐paper‐2021.pdf
- 39. Health Service Executive . Fifth annual child & adolescent mental health service report: 2012–2013. Health Service Executive. 2014; Available from: https://www.hse.ie/eng/services/publications/mentalhealth/camhs12,13.pdf
- 40. Colizzi M, Sironi E, Antonini F, Ciceri M, Bovo C, Zoccante L. Psychosocial and behavioral impact of COVID‐19 in autism spectrum disorder: an online parent survey. Brain Sciences. 2020;10(6):341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fontanesi L, Marchetti D, Mazza C, Di Giandomenico S, Roma P, Verrocchio M. The effect of the COVID‐19 lockdown on parents: a call to adopt urgent measures. Psychol Trauma: Theory Res Pract Policy. 2020;12(S1):S79‐S81. [DOI] [PubMed] [Google Scholar]
- 42. Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1337‐1345. [DOI] [PubMed] [Google Scholar]
- 43. Faul F, Erdfelder E, Buchner A, Lang A. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149‐1160. [DOI] [PubMed] [Google Scholar]
- 44. Stone L, Otten R, Engels R, Vermulst A, Janssens J. Psychometric properties of the parent and teacher versions of the strengths and difficulties questionnaire for 4‐ to 12‐year‐olds: a review. Clin Child Fam Psychol Rev. 2010;13(3):254‐274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Berry J, Jones W. The parental stress scale: initial psychometric evidence. J Soc Pers Relat. 1995;12(3):463‐472. [Google Scholar]
- 46. Limbers C, McCollum C, Greenwood E. Physical activity moderates the association between parenting stress and quality of life in working mothers during the COVID‐19 pandemic. Ment Health Phys Act. 2020;19:100358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Miller J, Cooley M, Mihalec‐Adkins B. Examining the impact of COVID‐19 on parental stress: a study of foster parents. Child Adolesc Soc Work J. 2020;1‐10. 10.1007/s10560-020-00725-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Weiss DS. The impact of event scale: revised. In: Marsella AJ, ed. Cross‐cultural assessment of psychological trauma and PTSD. Boston: Springer; 2007:219‐238. [Google Scholar]
- 49. Gobbi S, Płomecka MB, Ashraf Z, et al. Worsening of preexisting psychiatric conditions during the COVID‐19 pandemic. Front Psychiatry. 2020;11:1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID‐19 outbreak. Brain Behav Immun. 2020;88:559‐565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Topp C, Østergaard S, Søndergaard S, Bech P. The WHO‐5 well‐being index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167‐176. [DOI] [PubMed] [Google Scholar]
- 52. Smith B, Twohy A, Smith G. Psychological inflexibility and intolerance of uncertainty moderate the relationship between social isolation and mental health outcomes during COVID‐19. J Context Behav Sci. 2020;18:162‐174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sønderskov K, Dinesen P, Santini Z, Østergaard S. The depressive state of Denmark during the COVID‐19 pandemic. Acta Neuropsychiatrica. 2020;32(4):226‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Carver C. You want to measure coping but your protocol’ too long: Consider the brief cope. Int J Behav Med. 1997;4(1):92‐100. [DOI] [PubMed] [Google Scholar]
- 55. Eisenberg S, Shen B, Schwarz E, Mallon S. Avoidant coping moderates the association between anxiety and patient‐rated physical functioning in heart failure patients. J Behav Med. 2011;35(3):253‐261. [DOI] [PubMed] [Google Scholar]
- 56. Dawson D, Golijani‐Moghaddam N. COVID‐19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J Context Behav Sci. 2020;17:126‐134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. IBM Statistical Package for the Social Sciences (SPSS). ; 2016.
- 58. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; 1988. [Google Scholar]
- 59. Alhuzimi T. Stress and emotional wellbeing of parents due to change in routine for children with Autism Spectrum Disorder (ASD) at home during COVID‐19 pandemic in Saudi Arabia. Res Dev Disabil. 2021;108:103822. [DOI] [PubMed] [Google Scholar]
- 60. Wang L, Li D, Pan S, et al. The relationship between 2019‐nCoV and psychological distress among parents of children with autism spectrum disorder. Global Health. 2021;17(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Willner P, Rose J, Stenfert Kroese B, et al. Effect of the COVID‐19 pandemic on the mental health of carers of people with intellectual disabilities. J Appl Res Intellect Disabil. 2020;33(6):1523‐1533. [DOI] [PubMed] [Google Scholar]
- 62. Lawson M, Piel M, Simon M. Child maltreatment during the COVID‐19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 2020;110:104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Griffith A. Parental burnout and child maltreatment during the COVID‐19 pandemic. J Fam Violence. 2020;1‐7. 10.1007/s10896-020-00172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Hao F, Tan W, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID‐19 pandemic and lockdown? A case‐control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Yue J, Zang X, Le Y, An Y. Anxiety, depression and PTSD among children and their parent during 2019 novel coronavirus disease (COVID‐19) outbreak in China. Curr Psychol. 2020. 10.1007/s12144-020-01191-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Jeffs E, Lucas N, Walls T. CoVID‐19: Parent and caregiver concerns about reopening New Zealand schools. J Paediatr Child Health. 2020;57(3):403‐408. [DOI] [PubMed] [Google Scholar]
- 67. Craig F, Savino R, Fanizza I, Lucarelli E, Russo L, Trabacca A. A systematic review of coping strategies in parents of children with attention deficit hyperactivity disorder (ADHD). Res Dev Disabil. 2020;98:103571. [DOI] [PubMed] [Google Scholar]
- 68. Agha S. Mental well‐being and association of the four factors coping structure model: a perspective of people living in lockdown during COVID‐19. Ethics, Med Public Health. 2021;16:100605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID‐19 epidemic in China. Brain Behav Immun. 2020;87:40‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. O'Connor R, Wetherall K, Cleare S, et al. Mental health and well‐being during the COVID‐19 pandemic: longitudinal analyses of adults in the UK COVID‐19 Mental Health & Wellbeing study. Br J Psychiatry. 2020;218(6):326‐333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Gavidia‐payne S, Denny B, Davis K, Francis A, Jackson M. Parental resilience: a neglected construct in resilience research. Clin Psychol. 2015;19(3):111‐121. [Google Scholar]
- 72. Bayat M. Evidence of resilience in families of children with autism. J Intellect Disabil Res. 2007;51(9):702‐714. [DOI] [PubMed] [Google Scholar]
- 73. Schneider M, VanOrmer J, Zlomke K. Adverse childhood experiences and family resilience among children with autism spectrum disorder and attention‐deficit/hyperactivity disorder. J Dev Behav Pediatr. 2019;40(8):573‐580. [DOI] [PubMed] [Google Scholar]
- 74. Barnett A. Regression to the mean: what it is and how to deal with it. Int J Epidemiol. 2004;34(1):215‐220. [DOI] [PubMed] [Google Scholar]
- 75. Achterberg M, Dobbelaar S, Boer O, Crone E. Perceived stress as mediator for longitudinal effects of the COVID‐19 lockdown on wellbeing of parents and children. Sci Rep. 2021;11(1):2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bobo E, Lin L, Acquaviva E, et al. How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID‐19 outbreak? Encephale. 2020;46(3):S85‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Evans S, Mikocka‐Walus A, Klas A, et al. From “It Has Stopped Our Lives” to “Spending More Time Together Has Strengthened Bonds”: the varied experiences of Australian families during COVID‐19. Frontiers in Psychology. 2020;11(2906). 10.3389/fpsyg.2020.588667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Finzi‐Dottan R, Manor I, Tyano S. ADHD, temperament, and parental style as predictors of the child’s attachment patterns. Child Psychiatry Hum Dev. 2006;37(2):103‐114. [DOI] [PubMed] [Google Scholar]
- 79. Zhang J, Shuai L, Yu H, et al. Acute stress, behavioural symptoms and mood states among school‐age children with attention‐deficit/hyperactive disorder during the COVID‐19 outbreak. Asian J Psychiatry. 2020;51:102077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Jakobsen J, Gluud C, Wetterslev J, Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials – a practical guide with flowcharts. BMC Med Res Methodol. 2017;17(1):162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Carr A. The handbook of child and adolescent clinical psychology: a contextual approach. London: Routledge; 2016. [Google Scholar]
- 82. Evans S, Ling M, Hill B, Rinehart N, Austin D, Sciberras E. Systematic review of meditation‐based interventions for children with ADHD. Eur Child Adolesc Psychiatry. 2017;27(1):9‐27. [DOI] [PubMed] [Google Scholar]
- 83. Kazdin A, Whitley M. Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. J Consult Clin Psychol. 2003;71(3):504‐515. [DOI] [PubMed] [Google Scholar]
- 84. Climie E, Mastoras S. ADHD in schools: adopting a strengths‐based perspective. Can Psychol. 2015;56(3):295‐300. [Google Scholar]
- 85. Senior C, Godovich S, Habayeb S, Alvord M, Rich B. The effects of a resilience‐based group intervention for youth with ADHD. J Child Adoles Counsel. 2020;6(3):200‐214. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


