Abstract
Aim
The aims of this research were to analyse the urological literature published during the COVID‐19 pandemic and to guide future research.
Material and methods
Between 2019 and 2021, the Web of Science (WoS) All Databases collection was searched for publications related to COVID‐19 and Urology. The keywords used during this search were coronavirus‐19, COVID‐19, SARS‐CoV‐2, novel coronavirus, 2019‐nCoV, pandemic and/or urology. The top 50 cited (T50) publications were also identified and summarized. Exported Microsoft Excel files, Visualization of Similarities viewer (VOSviewer) software and descriptive assessment were used for bibliometric and statistical analyses of the publications.
Results
In total, 582 publications related to COVID‐19 and urology were identified. In these publications, the most active author, journal, country and organisation were Francesco Porpiglia, European Urology, the United States of America (USA) and La Paz University Hospital, respectively. The most commonly used keywords were telemedicine‐telehealth, SARS‐CoV‐2, coronavirus, pandemic, residency, testicle, semen, kidney transplantation, endourology and surgery. The most worrying issues in the articles are the negative impact of COVID‐19 on resident training and permanent damage to urological organs.
Conclusions
We analysed all the articles related to COVID‐19 and urology published to date in the WoS All Databases collection. The most commonly published articles were based on clinical and outpatient practice, telemedicine, residency training, transplantation, and testicles. The long‐term adverse effects of the pandemic on urology practice and especially urological organs will need to be assessed further in future research.
What's known
Although there are articles and reviews about COVID‐19 and urology, a bibliometric article has not been written before.
This study is the first that aims to direct future studies by conducting a bibliometric analysis of publications concerning COVID‐19 and urology.
What's new
This article provides a comprehensive and analytical perspective on COVID‐19 and urology.
This article will reveal which issues urologists and other clinicians should address regarding COVID‐19 and urology.
1. INTRODUCTION
Coronavirus disease 2019 (COVID‐19) is caused by the 2019 novel coronavirus (2019‐nCoV) isolated and sequenced on 7 January 2020. 1 On 11 March 2020, the World Health Organization (WHO) declared COVID‐19 as a pandemic. 2 According to WHO data, the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) caused 122,521,281 confirmed cases and 2,703,548 deaths as of 20 March 2021. 3 Approximately 305,29 million people have been vaccinated in the past 3 months; this corresponds to 4.5% of the world's population. 4 The vaccine has not yet reached many countries, and it remains unclear what viral mutations will cause, how long the pandemic will continue, or when life will normalize. 5 These uncertainties are also affecting all areas of urology.
At the beginning of the pandemic, publications and suggestions for adaptation to this unusual process were shared by major associations and journals. 6 , 7 Subsequently, urologists have conducted relevant research in many fields. For instance, they have evaluated the effect of the COVID‐19 pandemic on urology practice, urological organs, kidney transplantation, infertility, resident training and telemedicine. 8 , 9 New articles continue to be published every day in all areas of urology.
Bibliometrics refers to the objective and mathematical analysis of scientific publications related to a specific matter. 10 It can reveal the scope and quality of an article and shed light on the key points related to a specific topic. In addition, it can guide future studies and raise curiosity among researchers about unknown issues.
At present, the Thomson Reuters Web of Science (WoS) database is one of the most commonly used bibliometric tools. The Visualization of Similarities viewer (VOSviewer) software enables statistical, graphical and figural assessment of the information present in the WoS database for easy understanding. There are many bibliometric studies on COVID‐19 in the literature. 11 However, there is no bibliometric analysis related to COVID‐19 and urology so far.
In the present study, we aimed to analyse publications related to COVID‐19 and urology from a bibliometric perspective and to determine the top 50 cited (T50) publications for guiding future research.
2. METHODS
This was a bibliometric citation analysis study. Two reviewers (MS and YOD) independently searched the literature. The WoS All Databases collection (Philadelphia, Pennsylvania, USA) was used in this bibliometric citation study. Global literature related to COVID‐19 and urology published between 2019 and 2021 was scanned on 9 March 2021. Coronavirus‐19, COVID‐19, SARS‐CoV‐2, novel coronavirus, 2019‐nCoV, pandemic and urology were used as keywords to scan the title, abstract and keywords in order to identify relevant publications. The contents of the publications were examined one by one. Publications not related to COVID‐19 and urology were excluded from the study. The authors, countries, organisations, journals and impact factors (IFs), WoS research categories, document types, distribution of publications by months, most used keywords and T50 publications were exported via comma‐separated values (CSV) and Microsoft Excel files. Graphical mapping of the keywords via VOSviewer software was done to assess the current research focus during the pandemic. For some publications, MEDLINE/PubMed (the US National Library of Medicine database) and Google Scholar were used to add missing data. The T50 publications were also identified and analysed. Exported Microsoft Excel worksheets, VOSviewer software (version 1.6.16) and descriptive assessment was used for bibliometric and statistical analyses of the publications.
3. RESULTS
3.1. Number and monthly distribution of publications
In total, 582 publications related to COVID‐19 and urology were identified. Of these, 503 (86.4%) papers were published in 2020, while the remaining 79 (13.6%) were published in 2021 (until 9 March 2021). Assessment of the monthly distribution of the publications revealed that most articles were published in July 2020 (Figure 1). The number of publications tended to decrease thereafter. There was no publication related to COVID‐19 and urology in 2019. The language distribution of the publications was as follows: English, 532 (91.4%); Spanish, 35 (6.2%); German, 10 (1.7%); French, 4 (0.6%) and Russian, 1 (0.1%).
FIGURE 1.
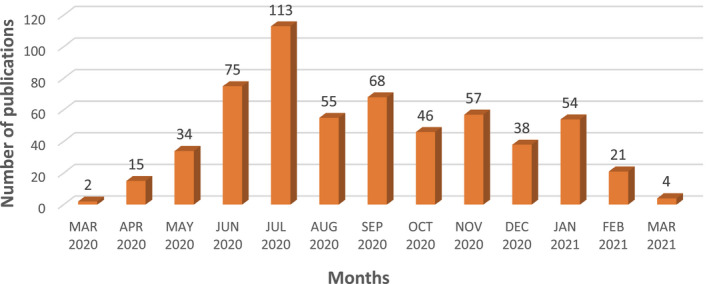
Distribution of COVID‐19 and urology publications by months
3.2. The most active authors, countries and organisations
The top 10 most active COVID‐19 and urology publication authors, countries and organisations are listed in Table 1. Scientific contributions were made by 65 countries and more than 1100 centres. Looking at the top contributing authors, Francesco Porpiglia from the University of Turin has 16 publications, with 315 citations. The countries with the highest numbers of publications are the USA, with 161 (27.6%, with 978 citations) and Italy, with 116 (19.9%, with 1052 citations). The centres with the highest numbers of publications are La Paz University Hospital, with 24 (4.1%, with 46 citations) and Sapienza University Rome, with 23 (3.9%, with 348 citations).
TABLE 1.
The top ten most active author, country and organisation of COVID‐19 and urology publications
| Number of publications (n, %) | Count of citations (n) | |
|---|---|---|
| Authors (first author/co‐author) | ||
| Porpiglia F (2/14) | 16 (2,7%) | 315 |
| Roupret M (0/15) | 15 (2,5%) | 158 |
| Esperto F (2/10) | 12 (2%) | 145 |
| Checcucci E (1/10) | 11 (1,8%) | 169 |
| Minervini A (0/11) | 11 (1,8%) | 76 |
| Rivas JG (2/9) | 11 (1,8%) | 39 |
| Rocco B (2/9) | 11 (1,8%) | 120 |
| Campi R (3/7) | 10 (1,7%) | 159 |
| Amparore D (3/7) | 10 (1,7%) | 157 |
| Dasgupta P (1/8) | 9 (1,5%) | 160 |
| Countries | ||
| USA | 161 (27,6%) | 978 |
| Italy | 116 (19,9%) | 1052 |
| England | 86 (14,7%) | 627 |
| Spain | 67 (11,5%) | 183 |
| China | 43 (7,3%) | 480 |
| Turkey | 41 (7%) | 94 |
| Germany | 40 (6,8%) | 201 |
| France | 37 (6,3%) | 227 |
| Brazil | 33 (5,6%) | 192 |
| Canada | 25 (4,2%) | 51 |
| Organisations | ||
| La Paz University Hospital | 24 (4,1%) | 46 |
| Sapienza University Rome | 23 (3,9%) | 348 |
| University of Florence | 23 (3,9%) | 218 |
| University of London | 23 (3,9%) | 228 |
| Assistance Publique‐Hôpitaux de Paris | 20 (3,4%) | 102 |
| University of Turin | 20 (3,4%) | 347 |
| Careggi University Hospital | 18 (3,1%) | 182 |
| Pitie Salpetriere University Hospital | 17 (2,9%) | 86 |
| Sorbonne University Hospital | 17 (2,9%) | 86 |
| University of Padua | 17 (2,9%) | 241 |
3.3. The most active journals, Web of Science categories and document types
The top 10 most active COVID‐19 and urology publication journals, WoS categories and document types are listed in Table 2. The journal with the highest number of publications (58 [9.9%]) and citations (691) is European Urology. As expected, Urology‐Nephrology was the largest Web of Science (WoS) research category, with 451 (77.4%) publications and 2513 citations. The most active document types were research articles 259 (44.5%), editorial materials 129 (22.1%), letters 98 (16.8%) and review articles 96 (16.6%).
TABLE 2.
The top ten most active Journals, Web of Science Research Categories and Document Types of COVID‐19 and Urology publications
| Number of publications (n, %) | Count of citations (n) | |
|---|---|---|
| Journals (impact factors, 2019) | ||
| European Urology (18.728) | 58 (9,9%) | 691 |
| International Braz J Urol (1.046) | 42 (7,2%) | 73 |
| Urology (1.861) | 38 (6,5%) | 136 |
| BJU International (4.524) | 34 (5,8%) | 244 |
| Journal of Urology (5.647) | 33 (5,6%) | 125 |
| Archivos Espanoles de Urologia (0.335) | 21 (3,6%) | 8 |
| World Journal of Urology (2.761) | 21 (3,6%) | 52 |
| European Urology Focus (4,827) | 16 (2,7%) | 76 |
| Actas Urologicas Espanolas (1.136) | 13 (2,2%) | 12 |
| Urologia Internationalis (1.401) | 13 (2,2%) | 25 |
| Web of Science Research Categories | ||
| Urology Nephrology | 451 (77,4%) | 2513 |
| Oncology | 24 (4,1%) | 517 |
| General Internal Medicine | 23 (3,9%) | 69 |
| Endocrinology Metabolism | 22 (3,7%) | 222 |
| Surgery | 22 (3,7%) | 1032 |
| Infectious Diseases | 13 (2,2%) | 2422 |
| Transplantation | 13 (2,2%) | 291 |
| Reproductive Biology | 11 (1,8%) | 389 |
| Obstetrics Gynecology | 10 (1,7%) | 157 |
| Pediatrics | 10 (1,7%) | 182 |
| Document types | ||
| Article | 259 (44,5%) | 2075 |
| Editorial material | 129 (22,1%) | 699 |
| Letter | 98 (16,8%) | 451 |
| Review | 96(16,6%) | 455 |
3.4. The most used keywords and T50 publications
The most used COVID‐19 and urology keywords and T50 publications are shown in Figure 2 and the Supplementary Material. Among the 582 publications, 647 keywords provided by paper authors and occurring more than five times in the WoS database were enrolled in the final analysis. Of the 647 keywords, 33 met the threshold. The keywords that appeared most were “COVID‐19” (total link strength 143) and “urology” (total link strength 68), which had a strong link to “telemedicine” and “telehealth.” The other most used keywords were “SARS‐CoV‐2,” “coronavirus,” “pandemic,” “residency,” “testicle,” “semen,” “kidney transplantation,” “endourology” and “surgery.”
FIGURE 2.

The most used keywords of COVID‐19 and urology publications
The median and the average number of citations for the T50 publications were 25 and 33.2, respectively (range from 12 to 106) (Supplementary Material). The article “There is no evidence of severe acute respiratory syndrome‐coronavirus 2 in the semen of men recovering from 2019 coronavirus disease” published in Fertility and Sterility received the most citations (106). In the T50 publications, European Urology published the largest number of publications (16) and was the most cited (553) journal.
4. DISCUSSION
The COVID‐19 pandemic is an unfamiliar period for the world and scientists, and more than ever there is a need for a bibliometric study to summarize the process and shed light on the future. Because of its nature and format, citation studies provide tremendous information about institutions, authors, and countries and identify landmark papers and high‐impact journals. This information not only indicates a scientific trend but also affects the scientific process and course in the future. It will help enthusiastic scientists who do not know or are wondering what topics they should research in any field or challenging process such as pandemic. The answers to these unknown questions provide guidance for scientists who are preparing to write an article on this subject or planning a study. By contacting or tracking these centres and authors can be an opportunity to work and benefit from the experiences of these scientists.
The world has experienced many pandemics, and the COVID‐19 pandemic will probably not be the last. The COVID‐19 pandemic took hold very quickly worldwide, and this unusual situation brought a lot of uncertainty. All urological priorities were changed to manage these difficulties and uncertainties. Despite the lack of evidence‐based data at the beginning of the pandemic, the European Association of Urology Guidelines Office Rapid Reaction Group presented a classification according to case priority and published a list of suggestions. 6 Since then, various publications on approaches to urological cases and triage have been published to guide urologists. 12 In this setting, several urological journals and associations created special tags and webpages (ie, the European Urology and BJU International COVID‐19 resource webpages) to update COVID‐19 information for urologists. 7 , 13 Also, almost all publishers announced that COVID‐19‐related publications would be open access.
As of 9 March 2021, the WoS database contained 98,482 publications on COVID‐19, and the bibliometric analysis of literature has great significance for understanding current research. We found 582 COVID‐19 and urology publications, and these publications were analysed in this comprehensive study based on the WoS database because of a lack of bibliometric analysis related to COVID‐19 and urology.
Most of the articles on COVID‐19 and urology were published in the USA (Table 1). This result can be attributed to the USA being the country most affected by the pandemic and having strong data management and academic systems. The journal with the highest number of publications was European Urology, with 58 publications (Table 2), which can be explained by the efforts and effectiveness of European Urology in this process and the interest of researchers in this journal. Looking at the monthly distribution of publications, most articles were published in mid‐2020 (Figure 1). Since then, the number of articles published has decreased. When this situation was investigated, similar issues started to be published, and it was seen that original research and results are now needed.
The keywords that appeared most were “COVID‐19” (total link strength 143) and “urology” (total link strength 68), which had a strong link to telemedicine and telehealth (Figure 2). The other most used keywords were “SARS‐CoV‐2,” “coronavirus,” “pandemic,” “residency,” “testicle,” “semen,” “kidney transplantation,” “endourology” and “surgery.”
When the most used keywords and T50 publications were evaluated, COVID‐19 and urology literature commonly included the following four perspectives: impact on urological surgeries and mortality, the effect on the urinary tract and clinical characteristics, residency training, outpatient clinics and telemedicine.
At the beginning of the pandemic, the main concern was the impact of COVID‐19 on urological surgery and mortality. Publications on this subject were mostly written in April, May and June 2020. Looking at the details of the publications on this subject, 19 articles were included in the T50 publications, with 590 citations. Although priority‐based classifications are made on triage, almost all surgeries and outpatient examinations have been disrupted worldwide. 14 Urologists, including many healthcare professionals, have faced the dilemma of caring for their patients or protecting themselves and other healthcare staff. In this process, the main question was about which surgeries could be performed and which could be postponed for how long. It is understood that elective cases that were delayed can no longer be postponed. In general, the recommendations on this issue were to provide basic personal healthcare protection, simplify the diagnosis process, carry out preoperative COVID‐19 testing, increase local anaesthesia or spinal block procedures, prefer open surgical procedures to laparoscopic procedures, maintain negative room pressure and air filters during minimally invasive procedures and reduce outpatient visits. 15 The most important issue that needs to be investigated in publications on this subject is the long‐term consequences of morbidity in postponed cases. The impact of delays in surgical management will require future study.
Another issue was the effect of SARS‐CoV‐2 on the urinary tract and organs. Initially, it was thought to only affect the respiratory system, but later it was learned that it caused pathology in almost all organs (ie, heart, blood vessel, kidney, testis, bladder, thyroid gland, liver, pancreas, rectum and lungs). 16 SARS‐CoV‐2 RNA has been detected in urine, blood and faeces. 17 It is understood that this systemic effect occurred by the mechanism of the angiotensin‐converting enzyme‐2 (ACE‐2) receptor and the transmembrane protease‐serine 2 (TMPRSS2) protein in human epithelial cells. 17 Looking at the details of the publications on this subject, 14 articles were included in the T50 publications, with 403 citations. Nine of them were related to testis and male reproductive functions, two to kidney and urine, two to prostate and one to bladder cancer and intravesical bacillus Calmette−Guérin (BCG) treatment. Various viral infections are known to cause orchitis, and many cases of orchitis associated with COVID‐19 have been reported. 18 , 19 , 20 , 21 , 22 Although SARS‐CoV‐2 cannot be demonstrated in testicular tissue, it causes seminiferous tubular damage, decreased numbers of Leydig cells and lymphocytic inflammation and creates impaired sex‐related hormones and spermatogenesis. 23 The question in the articles was whether this damage is permanent and its mechanism and long‐term consequences.
The pandemic has caused serious damage to both undergraduate and urology resident training programmes worldwide. 24 According to the results of a survey of 107 centres in 22 countries, 72.9% of the urologists believed that the pandemic had negatively affected scientific, academic and educational activities. 25 Although resident didactic teaching (lectures) has been carried out online, resident surgical education (hands‐on training) has been disrupted because of reduced numbers of elective surgeries performed by senior surgeons and the minimisation of operating times and complications. 26 Serious concerns have arisen regarding this issue, and many articles have been published on it. Looking at the details of the publications on this subject, six articles were included in the T50 publications, with 141 citations. Various urology departments have developed adaptation programmes in this regard, which could be adopted by other urology departments. 9 , 27 Although it does not replace hands‐on training, online practice questions, virtual classroom models, simulations and the use of surgical videos may decrease the loss of learning goals. 28 At this point, the urological video‐training websites of the associations may be made open access, such as COVID‐19 publications. Residents can also request an extension of their training schedule to complete their learning curves.
At the beginning of the pandemic, outpatient urology visits decreased or were cancelled to avoid the spread of COVID‐19. Only nondeferrable surgeries (life‐threatening if delayed) or urological emergencies were recommended to visit urology clinics. Telehealth‐integrated patient management has come to the fore to replace face‐to‐face interviews to prevent possible contamination and protect healthcare workers and patients. 6 , 29 In a study on patient compliance, a large proportion (54.1%) of patients were eligible and willing to participate in telemedicine online visits. 29 Looking at the details of the publications on this subject, six articles were included in the T50 publications, with 139 citations. The most frequently used keywords linked with “COVID‐19” and “urology” were related to “telemedicine” and “telehealth” (Figure 2). The advantages of telemedicine appear to be that it is easy, accessible and inexpensive. The lack of physical examination of patients, software problems, ethics‐privacy and forensic risks are interesting unsolved questions. 30
5. CONCLUSIONS
Although COVID‐19 vaccine applications have recently increased, mutations and the number of people dying as a result of the pandemic have also risen. The most worrying issues in the articles are the negative impact of COVID‐19 on resident training and permanent damage to urological organs. New articles are being published daily within the scope of new data and experiences. Evaluating the quality and content of publications is vital to help future studies. Our study analysed all the COVID‐19 and urology publications to date in the WoS database, and it seems that the long‐term effects of the pandemic on disrupted urology practice and urological organs will be investigated further.
DISCLOSURE
The authors declare that they have no conflict of interest.
ETHICS APPROVAL
Not applicable.
INFORMED CONSENT
Not applicable.
Supporting information
Supplementary Material
Soytas M, Danacioglu YO, Boz MY, Horuz R, Albayrak S. sCOVID‐19 and urology: A bibliometric analysis of the literature. Int J Clin Pract. 2021;75:e14965. doi: 10.1111/ijcp.14965
Funding information
No funding received.
DATA AVAILABILITY STATEMENT
All data used during the study are available from the corresponding author by request.
REFERENCES
- 1. Hui DS, I Azhar E, Madani TA, et al. novel coronavirus outbreak in Wuhan. China. Int J Infect Dis. 2019;2020(91):264‐266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO . Coronavirus disease 2019 (COVID‐19) Situation Report – 51. 11 March 2020. World Health Organization In: https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200311‐sitrep‐51‐covid‐19.pdf?sfvrsn=1ba62e57_10. Accessed 8 May 2021
- 3. WHO . Coronavirus disease 2019 (COVID‐19). Weekly operational update on COVID‐19 ‐ World Health Organization. https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019. Accessed 4 April 2021
- 4. Our World in Data . Coronavirus (COVID‐19) Vaccinations. https://ourworldindata.org/covid‐vaccinations. Accessed 4 April 2021
- 5. The Centers for Disease Control and Prevention (CDC) . Emerging SARS‐CoV‐2 Variants. https://www.cdc.gov/coronavirus/2019‐ncov/more/science‐and‐research/scientific‐brief‐emerging‐variants.html. Accessed 4 April 2021 [PubMed]
- 6. Ribal MJ, Cornford P, Briganti A, et al. European Association of Urology Guidelines Office Rapid Reaction Group: An Organisation‐wide Collaborative Effort to Adapt the European Association of Urology Guidelines Recommendations to the Coronavirus Disease 2019 Era. Eur Urol. 2020;78(1):21‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. EAU . COVID‐19 Recommendations. https://uroweb.org/guideline/covid‐19‐recommendations/. Accessed 8 May 2021
- 8. Song CI, Wang Y, Li W, et al. Absence of 2019 novel coronavirus in semen and testes of COVID‐19 patients. Biol Reprod. 2020;103(1):4‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Porpiglia F, Checcucci E, Amparore D, et al. Slowdown of urology residents' learning curve during the COVID‐19 emergency. BJU Int. 2020;125(6):E15‐E17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Joshi MA. Bibliometric indicators for evaluating the quality of scientifc publications. J Contemp Dent Pract. 2014;15(2):258‐262. [DOI] [PubMed] [Google Scholar]
- 11. Yu Y, Li Y, Zhang Z, et al. A bibliometric analysis using VOSviewer of publications on COVID‐19. Ann Transl Med. 2020;8(13):816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chan MC, Kwok JL, Yeo SEK, Chong YL. Surgical Precautions for Urologists in the Era of COVID‐19. Urology. 2020;143:11‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. BJUI . Covid‐19: Collection of urology papers. https://www.bjuinternational.com/bjui‐blog/covid‐19‐collection‐of‐urology‐papers/. Accessed 8 May 2021
- 14. Teoh J‐C, Ong WLK, Gonzalez‐Padilla D, et al. A Global Survey on the Impact of COVID‐19 on Urological Services. Eur Urol. 2020;78(2):265‐275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thapa BB, Shrestha D, Bista S, et al. Urology during COVID‐19 Pandemic Crisis: A Systematic Review. Surg J (N Y). 2021;7(1):e3‐e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhu NA, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paoli D, Pallotti F, Colangelo S, et al. Study of SARS‐CoV‐2 in semen and urine samples of a volunteer with positive naso‐pharyngeal swab. J Endocrinol Invest. 2020;43(12):1819‐1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Xu J, Qi L, Chi X, et al. Orchitis: a complication of severe acute respiratory syndrome (SARS). Biol Reprod. 2006;74(2):410‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu W, Han R, Wu H, Han D. Viral threat to male fertility. Andrologia. 2018;50(11):e13140. [DOI] [PubMed] [Google Scholar]
- 20. Cardona Maya WD, Du Plessis SS, Velilla PA. SARS‐CoV‐2 and the testis: similarity with other viruses and routes of infection. Reprod Biomed Online. 2020;40(6):763‐764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Patel DP, Punjani N, Guo J, et al. The impact of SARS‐CoV‐2 and COVID‐19 on male reproduction and men's health. Fertil Steril. 2021;115:813‐823. S0015‐0282(20)32780‐1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kim J, Thomsen T, Sell N, Goldsmith AJ. Abdominal and testicular pain: An atypical presentation of COVID‐19. Am J Emerg Med. 2020;38(7):1542.e1‐1542.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yang M, Chen S, Huang BO, et al. Pathological Findings in the Testes of COVID‐19 Patients: Clinical Implications. Eur Urol Focus. 2020;6(5):1124‐1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pang KH, Carrion DM, Rivas JG, et al. The Impact of COVID‐19 on European Health Care and Urology Trainees. Eur Urol. 2020;78(1):6‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Heinze A, Umari P, Basulto‐Martínez M, et al. Impact of COVID‐19 on Clinical and Academic Urological Practice: A Survey from European Association of Urology Section of Uro‐technology. Eur Urol Open Sci. 2020;21:22‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kwon YS, Tabakin AL, Patel HV, et al. Adapting Urology Residency Training in the COVID‐19 Era. Urology. 2020;141:15‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vargo E, Ali M, Henry F, et al. Cleveland Clinic Akron General Urology Residency Program's COVID‐19 Experience. Urology. 2020;140:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chick RC, Clifton GT, Peace KM, et al. Using Technology to Maintain the Education of Residents During the COVID‐19 Pandemic. J Surg Educ. 2020;77(4):729‐732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boehm K, Ziewers S, Brandt MP, et al. Telemedicine Online Visits in Urology During the COVID‐19 Pandemic‐Potential, Risk Factors, and Patients' Perspective. Eur Urol. 2020;78(1):16‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gadzinski AJ, Ellimoottil C. Telehealth in urology after the COVID‐19 pandemic. Nat Rev Urol. 2020;17(7):363‐364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
All data used during the study are available from the corresponding author by request.


