Abstract
Behavioral interventions consolidating technology are underutilized and do not reach diverse populations such as African Americans with hypertension. This pilot study aimed to evaluate the effects of a theoretically derived, technology-based intervention in African Americans with hypertension. African Americans with hypertension (N = 18; age range 25-85; 72.22% females) were randomized to the technology-based plus positive psychological training (PPT) experimental group (n = 10) or the comparison group (n = 8) for 12 weeks. The technology-based intervention included analytic components (web-based education, self-monitoring of blood pressure [BP], and medication management using a commercially free app-Medisafe) and an emotional component (comprised of skills and behaviors directed at engaging 1 in positive activities to help build increasing healthy behaviors). The comparison group received the technology-based intervention alone. Demographic information, self-management cognitive processes, self-management behaviors, and health status outcomes were assessed. After completing the 12-week intervention, the groups did not significantly differ in health outcomes, health behavior outcomes, and technology utilization outcomes. Mean systolic BP decrease 6.02 mmHg (standard deviation [SD] = 22.75) in the comparison group and 1.1 mmHg (SD = 20.64; P = .439) in the experimental group. Diastolic BP decreased 0.1 mmHg (SD = 11.78) in the comparison group and 1.5 mmHg (SD = 12.7; P = .757) in the experimental group. Our findings suggest that behavioral interventions using technology have the potential to improve self-management outcomes among African American populations. Further research is warranted in a larger sample size and a longer time frame to identify the intervention’s effectiveness.
Keywords: African Americans, hypertension, cardiovascular disease, health technology, self-management, health disparities
Introduction
Self-management support has emerged as a vital component in improving cardiovascular health and outcomes. Innovative strategies using technology have been leveraged to deliver self-management support to improve patients’ attitudes, skills, and behaviors. Technology such as smartphones, mHealth applications (apps), personalized short message service (SMS), and text messaging have been expanded and used to manage and support various chronic conditions, including cardiovascular disease.1,2 These technologies are appealing for several reasons; including, the exchange of health information, the ability to prompt behavioral change, and the capability to give feedback to inform health decision-making. 2
Numerous intervention programs have been developed and implemented to improve self-management and health outcomes of persons living with hypertension,3,4 including the confluence of technology-based interventions. A few studies have focused on self-managing CVD with technology-enabled devices and/or apps and have shown some improvements in lifestyle modifications and blood pressure (BP) control.5,6 In addition to these benefits, technology-based interventions have demonstrated that they are adaptable for specific chronic disease management and are feasible and cost-effective. 2 However, behavioral interventions that incorporate technology are underutilized and do not reach diverse populations such as African Americans with hypertension. 7
Hypertension is a significant public health concern and directly attributable to high rates of hypertension-related diseases, particularly stroke, heart failure, and kidney disease.8,9 Over the last 5 years, the prevalence of hypertension has increased from 31% to 46% among American adults due to changes in the evidence base and the current U.S. hypertension guideline criteria, which defines hypertension as 130/80 mmHg or above. 9 More alarming, disparities in hypertension are more evident among African Americans, as the prevalence has increased to approximately 56% and is higher and control to <130/80 mmHg less (19.7%) compared to other racial-ethnic groups. 8 While tremendous strides have been made to improve hypertension treatment and management, African American adults are twice as likely to have uncontrolled BP as well as lower rates of self-managing their hypertension and medication adherence to antihypertensives when compared to their counterparts. 8 The stark disparity observed in uncontrolled hypertension rates among African Americans includes multifactorial mechanisms, particularly social determinants of health, including socioeconomic, cultural, and environmental factors, access to care, and health behaviors. 10
As such, meaningful strategies are critical and needed to reduce disparities in hypertension, and the use of technology-based interventions should be considered.1,2 Therefore, unique self-management support programs to improve BP control and medication adherence should focus on understanding the efficacy of patient-centered, technology-based interventions to support African Americans manage their hypertension.
Conceptual Framework
Much of the empirical knowledge about self-management of chronic conditions incorporates evidence that empowers patients by increasing their knowledge, problem-solving skills, and self-efficacy to manage a chronic condition. 4 Another widely used model suggests that self-management is a process that takes into account multidimensional constructs, including the individual and family, the context of risk and protective factors specific to the chronic disease, and physical and social environments which influence engagement in self-management behaviors (proximal outcomes) and subsequently improves health (distal outcomes). 11 However, most self-management models are focused on the cognitive-behavioral aspects and do not take into account the biological processes underlying self-management. 12
Therefore, this study was guided by the Model of Brain-Behavior Connection in Self-Management of Health and Illness framework, 13 which emphasizes the biological and brain processes of self-management in addition to the psychosocial and behavioral factors traditionally included in self-management models. This model postulates that individuals who optimally process both analytic (fact-focused) and emotional (feelings/empathic-focused) health information are more likely to act on that information to self-manage their chronic condition and health. Therefore, the interventions being compared in this investigation were designed with differing amounts of emotion-focused content.
Purpose
The purpose of this study was to evaluate the effects of a theoretically derived, technology-based intervention, TechSupport, to improve BP, QOL), and psychological health (depressive symptoms, anxiety, and affective well-being) in African Americans with hypertension. We hypothesized that individuals assigned to the TechSupport intervention comprised of both analytic and empathic components for self-managing hypertension would have improved BP and better positive affect and well-being QOL (PAW-QOL) and psychological health than the comparison group, which received primarily analytic-focused self-management information.
Methods
Design and sample
This was a 2-arm pilot randomized control study conducted in Cleveland, OH. Study participants were recruited from October 2018 to March 2019 to participate in a 12-week intervention study. Using aspects of a convenience sampling approach, we employed diverse strategies to minimize our risk of selection bias. Potential participants were recruited from a local academic medical hospital and affiliated community clinics using clinician referrals. Participants were also recruited from community events, social media platforms (Facebook), and targeted advertisements (ie, fliers, brochures, and kiosk displays). In addition, participants would also refer individuals from the social networks.
The participants were eligible if they met the following criteria: (1) self-identify as African American, (2) age 25 years or older, (3) diagnosed with hypertension (defined as BP ≥ 130/80 mmHg), (4) on at least 1 antihypertensive medication, and (5) own a smartphone. The exclusion criteria were (1) unable to give informed consent or judged to have impaired cognitive ability or severe memory deficits and (2) currently practicing positive psychological training. Also, because a subset of our participants underwent brain functional magnetic resonance imaging (fMRI), we also excluded those individuals with having a history of medical conditions or procedures that are contraindicated for fMRI scanning (cardiac pacemaker, sternal wires, or metal implants) and those with a history of claustrophobia requiring anxiolytics or sedation.
Technology-based intervention
The technology-based intervention was comprised of both analytic and emotional components that are further described in Table 1. The experimental group, TechSupport, integrates analytic (technology-based components) and emotional/empathic components (positive psychological training [PPT]). The technology component included web-based education, self-monitoring of BP with a study-provided device, and medication management using a commercially free app called Medisafe. The Medisafe app is a personalized medication manager which supports an individual to adhere to a complex drug regimen through SMS (Short Message Service) alerts, medication refill reminders, and drug information and interaction warnings, accessible on most digital devices, including mobile phones (www.medisafe.com). The emotional component of TechSupport is adapted from 2 PPT programs,14,15 that are comprised of a range of skills and behaviors directed at engaging 1 in positive activities (optimism, resilience, well-being, self-confidence, and compassion) to help build increasing amounts of healthy behaviors. 16 To deliver PPT as a technology component, we constructed 6 weekly educational interactive modules designed with Vimeo and embedded in Qualtrics software to teach and engage individuals to self-manage their emotions. A trained research assistant, unblinded to group assignments, instructed participants how to use each component of the technology-based intervention during a 1-h session. The comparison group received all components of the technology-based intervention, but was not exposed to the emotional component, PPT (Table 1).
Table 1.
Details of the Technology-Based Intervention, TechSupport.
| Analytic components | |
|---|---|
| Technology-based components | |
| Web-based education | Hypertension knowledge and skills content is delivered as 6 weekly web-based modules of <10 min in duration, accessible by smartphone, iPad, and computer. |
| -Session 1: overview and understanding of hypertension | |
| -Session 2: self-monitoring your blood pressure | |
| -Session 3: importance of adherence to antihypertensives therapy | |
| -Session 4: modifying behaviors—increase physical activity | |
| -Session 5: modifying behaviors—diet and nutrition | |
| -Session 6: understanding health consequences of hypertension | |
| Medication adherence support application (app) | Medisafe medication management app |
| -Provides alerts of when it’s time to take medication | |
| -Generates weekly adherence reports | |
| -Tracks and monitors biometric data (once entered into app) | |
| Self-monitoring blood pressure | Participants instructed to monitor and record blood pressure 2 nonconsecutive days/week, twice a day, for a total of 12 weeks with an Omron 10 Series home BP monitor provided by study. |
| Emotional component | |
| Positive psychological training | |
| Web-based training | Six weekly training modules on a range of skills and behaviors directed at engaging 1 in positive activities (optimism, resilience, well-being, self-confidence, and compassion) to help build increasing amounts of healthy behaviors. Each session is <10 min in duration. |
| -Session 1: exploring and expressing gratitude for positive events | |
| -Session 2: identify your personal strengths | |
| -Session 3: engaging in enjoyable and meaningful activities | |
| -Session 4: reflecting and capitalizing on past success | |
| -Session 5: acts of kindness | |
| -Session 6: personal choice—repeat a session from weeks 1 to 5 | |
Study procedures
This study was approved by University Hospitals of Cleveland’s Institutional Review Board. All participants received written and oral information about the study prior to enrollment. Participants who provided informed consent were randomized 1:1 to either the experimental group or the comparison group. All study visits (baseline, 8 and 12 weeks) were conducted on a clinical research unit by a registered nurse and a trained research assistant. Data collected by the research nurse included height, weight, and blood and hair specimens to measure markers of stress and inflammation (cortisol, Interleukin 6). Participants completed study questionnaires using the web-based, secure platform, Research Electronic Data Capture (REDCap), with support from a trained research assistant, if needed. Demographics were collected at baseline, while self-management cognitive processes (self-efficacy, patient activation, and decision-making), self-management behaviors (physical activity and dietary intake), and health status outcomes (BP, HRQOL, affect, anxiety, and depression) were collected at baseline and 8 and 12 weeks. A subset of participants underwent brain fMRI scans (not discussed in this paper) that were completed at baseline and at 8 weeks following the intervention. Each visit lasted approximately 2 h, and study participants were given an honorarium of $25 for completion of the baseline and 8-week visits, and $50 for completion of the 12-week visits.
Measures
Health outcomes
Table 2 describes the study variables and measures. The primary health outcomes of this study were BP, PAW-QOL, and psychological health (depression, anxiety). BP (the average of 3 readings) was measured by a research nurse at each visit using a validated automated BP device (Omron HEM-907 XL) and best practices for collecting BP, such as using the appropriate cuff size and allowing the participants to rest at least 5 min prior to collecting their BP measurements.9,17 Home BPs were measured using the Omron 10-Series home BP monitor. Participants were trained and provided instructions to monitor their BP twice a day, 2 days a week, over the 12-week study period, then asked to record BPs on a study-provided tracking log. Participants also completed the 9-item Patient-Reported Outcomes Measurement Information System (PROMIS) Short Form, Positive Affect and Well-Being Quality of Life (PAW-QOL). This PROMIS Short Form used 5-point Likert-type responses (eg, “1 = never” to “5 = always”) with scores ranging from 9 to 45, where higher scores indicated better QOL. 18 In addition, psychological health components, affective well-being, depression, and anxiety were measured with the PROMIS-29. 18
Table 2.
Study Variables, Measures, and Reliability.
| Variable | Measure | Reliability |
|---|---|---|
| Health status indications (distal outcomes) | ||
| Blood pressure (BP) | Omron 907XL9,17 | |
| Quality of life/well-being | Positive affect and well-being-short form 15a 18 | 0.95 |
| Depression symptoms | Patient-reported outcomes measurement information system (PROMIS-29) 18 | 0.98 |
| Anxiety | PROMIS-2918 | 0.98 |
| Self-management behaviors (proximal outcomes) | ||
| Systolic/diastolic home BP | Home blood pressure monitoring, Omron series 10 | |
| Medication adherence | K-Wood-medication adherence scale (MAS-4) 19 | 0.66-0.76 |
| Diet | 24-h Standardized dietary recall Bialostosky et al 26 | |
| Physical activity | Actigraph 22 | 0.80 |
| Self-management cognitive process | ||
| Patient activation | Patient activation measure 24 | 0.87 |
| Self-efficacy | Self-efficacy for chronic disease management (PROMIS) 25 | 0.91 |
| Demographics and covariates | ||
| Demographics | Age, gender, marital status, income, education level, comorbidities, and body mass index (BMI), hypertension characteristics | |
| Hypertension knowledge | Hypertension knowledge-level scale (HK-LS) 19 | 0.82 |
| Positive emotion | Positive and negative affect schedule (PANAS) short form 28 | 0.87 |
| Technology utilization | Usefulness, satisfaction, and ease of use (USE) questionnaire,20,21 | |
Self-Management Behaviors and Cognitive Process
Medication adherence
Self-report of medication adherence was measured using the 4-item Krousel-Wood et al 19 Medication Adherence Scale (K-Wood-MAS-4), which assessed 4 domains of adherence behaviors: self-efficacy, physical function, intentional medication-taking, and forgetfulness. Scores on the K-Wood-MS-4 ranged from 0 to 4, with higher scores indicating worse adherence. In addition, medication adherence was supported and monitored with a smartphone medication management app, Medisafe (www.medisafe.com). By design, Medisafe prompts, monitors, and gives feedback to participants, which was further conceptualized by us to facilitate behavior change and support self-management behaviors. Participants responded to daily reminders on their smartphones as to whether or not they took their prescribed antihypertensive medications. In addition, we assessed technology utilization on the System Usability Scale (SUS).20,21 The SUS is a 30-item questionnaire on a 7-point Likert scale (1 = Strongly Disagree, to 7 = Strongly Agree) used to measure a global view of technology usability in 4 domains—use, ease, learning, and satisfaction with technology (α = .98). Mean scores were computed for each domain, and higher scores indicated good usability within each domain.
Physical activity
After participants were taught to use the Medisafe app, each person was provided an ActiGraph wGT3X-BT accelerometer (ActiGraph, LLC, Pensacola, FL) to measure their physical activity. 22 Participants were instructed to wear the ActiGraph on their non-dominant hip during waking hours for 7 consecutive days and to remove it daily before bed or water activities. The ActiGraphs were returned to the study staff by mail in a prepaid postage envelope. Moderate-to-vigorous physical activity (MVPA) was considered 10 min of activity (≥2690 counts/min), and valid wear time was considered a minimum of at least 4 days and at least 10 h/day. 23 Actigraphy data were analyzed with ActiLife v6.13.3 at a 60-s epoch length.
Cognitive process
To assess participants’ knowledge, confidence, and skills of self-management, the 10-item Patient Activation Measures was used. 24 Scores range from 0 to 100 with higher scores indicating more patient activation. Self-efficacy was also measured using the 6-item Chronic Disease Self-Efficacy Scale by Lorig et al 25 The items are scored from 0 to 10 for a total score and higher scores indicate more self-efficacy.
Dietary intake
The 24-h dietary recall was used to assess food descriptions, preparation methods, and portion sizes consumed within the past 3 days. Nutrition and dietary history interviews were conducted by a registered dietitian using the 24-h diet recall and took approximately 20 min to complete. Data was entered into the Nutrient Data System for Research (NDSR) software using a multiple pass approach, 26 then computed for macronutrients, vitamins, minerals, and Healthy Eating Index score (HEI, composite score of diet quality). HEI scores range from 0 to 100, with higher scores indicating better dietary intake. 26
Demographic information and covariates
Participants completed a survey focused on self-reported demographic characteristics. Data on age, gender, marital status, income, education level, comorbidities, and body mass index (BMI) were collected. In addition, information was collected on years diagnosed with hypertension and the number of antihypertensive medications prescribed. Hypertension knowledge was measured at baseline using the Hypertension Knowledge-Level Scale (HK-LS), and scores can range from 0 to 22, with higher scores indicating greater hypertension knowledge. 27 In addition, the Positive and Negative Affect Schedule (PANAS) was used to assess an individual’s feelings and emotions over a period of weeks. 28 This measure consists of 20 items (10 that measure positive affect and 10 that measure negative affect) on a 5-point Likert scale, with scores ranging from 10 to 50. High scores on the positive subscale indicate higher levels of positive affect, while low scores on the negative affect scale indicate lower levels of negative affect.
Data Analysis
Data were analyzed using descriptive and analytic statistics using IBM SPSS version 27.0 and SAS 9.4 (Cary, NC). Descriptive statistics were used to evaluate the demographic characteristics and all study variables. Independent 2-sample T-test and chi-square/Fisher’s exact test were used to examine the differences between the experimental and comparison groups for baseline and hypertension-related characteristics. Nonparametric tests, the Mann-Whitney U was used to examine the comparison between the experimental groups at baseline and 12 weeks. We also used a repeated measures linear mixed model with unstructured covariance structured covariance structure fitted using SAS Proc Mixed to examine the effect of the technology-based intervention on health status indicators (outcomes) over time. Given the aim of this pilot study was to investigate the efficacy of a technology-based intervention based on a novel theory to enhance BP management and improve QOL, the statistical significance level was set at P < .10 (2-sided).
Results
A convenience sample of 18 African Americans with hypertension were enrolled in this study; 8 participants were assigned to the comparison group and 10 participants were assigned to the experimental group. The demographic and hypertension-related characteristics of participants by groups are shown in Table 3. Age varied between 25 and 85 years and the mean age of the participants was 57.22 (SD = 15.79). Females represented 72.22% of the participants, and 55.6% were unemployed. There were significant differences between the groups in terms of gender (P = .19), employment status (P = .20), and being prescribed a calcium channel blocker antihypertension medication (P = .058). The sample reported a mean history of hypertension of 16.35 years (SD = 9.73) years (17 and 11 years in the experimental and comparison groups, respectively). Of note, the sample was prescribed an average of 2.44 antihypertensive medications. The mean BMI was significantly different between the comparison and experimental group (P = .020), with the comparison group being more obese compared to the experimental group at baseline.
Table 3.
Baseline and Hypertension-Related Characteristics of the Sample (N = 18).
| Variable | Control group (n = 8) | Intervention group (n = 10) | t | P-value |
|---|---|---|---|---|
| Demographics | ||||
| Age, in years (range 25-85), mean (SD) | 51.38 (9.0) | 61.90 (18.79) | −1.450 | .166 |
| Female sex, n (%) | 8 (100) | 5 (50.0) | .036* | |
| Marital status, not married, n (%) | 5 (62.5) | 6 (80.0) | .608 | |
| Education, n (%) | 1.000 | |||
| Some college/associated degree | 3 (37.5) | 4 (40.0) | ||
| 4-year college degree or higher | 5 (62.5) | 6 (60.0) | ||
| Employment, n (%) | .054* | |||
| Employed | 6 (75.0) | 2 (20.0) | ||
| Unemployed | 2 (25.0) | 8 (80.0) | ||
| Income, n (%) | .504 | |||
| <$20 000 | 3 (37.5) | 3 (30.0) | ||
| $20 000-$39 000 | 4 (50.0) | 3 (30.0) | ||
| >$40 000-$79 000 | 1 (12.5) | 4 (40.0) | ||
| Insurance type | .284 | |||
| Medicare/medicaid | 4 (57.1) | 4 (44.4) | ||
| Private | 3 (42.9) | 2 (22.2) | ||
| Out of pocket | 0 | 3 (33.3) | ||
| Health status | .255 | |||
| Excellent | 0 | 4 (40.0) | ||
| Good | 5 (62.5) | 4 (40.0) | ||
| Fair | 2 (25.0) | 1 (10.0) | ||
| Poor | 1 (12.5) | 1 (10.0) | ||
| Hypertension-related characteristics | ||||
| Hypertension knowledge, mean (SD) | 18.88 (1.36) | 19.40 (1.35) | −0.818 | .425 |
| No. of chronic conditions, mean (SD) | 3.63 (1.77) | 3.20 (1.99) | 0.47 | .643 |
| Hypertension, no. of years diagnosed, mean (SD) | 11.25 (10.25) | 21.30 (11.09) | −1.975 | .066* |
| Body mass index, mean (SD) | 42.78 (6.92) | 32.57 (9.29) | 2.46 | .020* |
| Dietary intake | ||||
| Health eating index, mean (SD) | 51.14 (16.18) | 55.44 (16.40) | −0.523 | .609 |
| Sodium (mg/day) | 3004.58 (1579.56) | 3521.49 (2614.39) | −0.460 | .653 |
| Caloric intake (kcals/day) | 1772.51 (687.94) | 1909.74 (1198.82) | −0.269 | .792 |
| No. of antihypertensives prescribed, mean (SD) | 2.13 (1.25) | 2.70 (1.57) | −0.844 | .411 |
| Class of antihypertensives prescribed, n (%) | ||||
| Thiazides-type | 5 (62.5) | 6 (60.0) | 0.012 | .914 |
| Calcium channel blocker | 2 (25.0) | 7 (70.0) | 3.60 | .058* |
| ACE inhibitors | 2 (25.0) | 0 | 2.813 | .094* |
| Angiotensin receptor blocker | 2 (25.0) | 3 (27.8) | 0.055 | .814 |
| Beta blocker | 3 (37.5) | 5 (50.0) | 0.281 | .596 |
Abbreviations: BP, blood pressure; No., number.
Values are reported as either n (%) or mean (M) and standard deviation (SD). The P-values are for Fisher exact test (categorical variables) and t-test (continuous variables). The hypertension knowledge-level scale (HK-LS) and scores range from 0 to 22, with higher scores indicating greater knowledge levels of hypertension.
Statistically significant at P < .10.
Group differences in health status indicators (BP, PAW-QOL) and self-management cognitive process and behaviors (self-efficacy, patient activation, physical activity, and medication adherence) are shown in Table 4. Analyses using the Mann-Whitney U test revealed there were significant improvements in participants’ PAW-QOL (P = .097) and diastolic home BP monitoring scores (P = .061) between baseline and 12 weeks in the experimental group. However, there were no health status indicators or self-management process and behavior differences in the comparison group between baseline and 12 weeks (P > .10). In terms of technology use (Table 5), 72.2% of the participants viewed more than 80% of the hypertension web-based education modules, and 70.1% monitored their BP at home for more than 9 weeks with a study-provided BP monitor. With regards to the mHealth medication app, use of the app was greater in African Americans with hypertension in the comparison group (50%) vs the experimental group (40%). Of those who were in the experimental group and received the PPT training, 60% of the group completed more than 80% of the modules.
Table 4.
Summary of Differences Between Groups Using Technology-Based Intervention for Hypertension Self-Management.
| Variables | Times | Comparison group (n = 8) | Experimental group (n = 10) | U | Z | P value | ||
|---|---|---|---|---|---|---|---|---|
| M (SD) | Mean ranking | M (SD) | Mean ranking | |||||
| Health status indictors | ||||||||
| Systolic BP, mmHg | Baseline | 148.13 (36.96) | 10.25 | 142.90 (15.83) | 8.90 | 34.00 | −0.534 | .594 |
| 12 weeks | 121.25 (29.27) | 5.00 | 139.44 (13.93) | 7.89 | 10.00 | −1.236 | .216 | |
| Diastolic BP, mmHg | Baseline | 94.50 (19.61) | 11.63 | 77.20 (16.20) | 7.80 | 23.00 | −1.514 | .130 |
| 12 weeks | 76.75 (15.39) | 7.25 | 76.77 (14.88) | 6.89 | 17.00 | −0.155 | .877 | |
| Positive affect/well-being QOL | Baseline | 35.75 (5.60) | 7.69 | 39.00 (2.53) | 10.95 | 54.50 | 1.297 | .195 |
| 12 weeks | 32.60 (8.53) | 5.30 | 39.80 (3.88) | 9.35 | 38.50 | 1.658 | .097* | |
| Self-management cognitive process and behaviors | ||||||||
| Self-efficacy | Baseline | 7.38 (1.74) | 7.44 | 8.38 (1.61) | 11.15 | 56.50 | −1.474 | .141 |
| 12 weeks | 10.00 (7.60) | 5.80 | 8.82 (1.91) | 9.10 | 36.00 | −1.372 | .170 | |
| Patient activation | Baseline | 62.20 (15.66) | 8.13 | 71.10 (17.82) | 10.60 | 51.00 | −0.981 | .327 |
| 12 weeks | 69.34 (13.40) | 6.70 | 75.54 (19.83) | 8.65 | 31.50 | −0.803 | .422 | |
| Medication adherence | Baseline | 1.00 (0.89) | 8.17 | 1.20 (1.14) | 8.70 | 32.00 | 0.227 | .820 |
| 12 weeks | 0.40 (0.89) | 5.90 | 1.30 (1.25) | 9.05 | 35.50 | 1.411 | .158 | |
| Moderate-to-vigorous physical activity (min/day) | Baseline | 18.67 (14.67) | 9.00 | 13.57 (17.25) | 7.13 | 21.00 | −0.810 | .418 |
| 12 weeks | 35.07 (36.66) | 7.50 | 15.81 (16.50) | 5.00 | 4.00 | −1.044 | .296 | |
| Systolic, home BP monitoring, mmHg | Baseline | 132.73 (14.38) | 5.25 | 141.24 (13.34) | 7.13 | 21.00 | 0.849 | .396 |
| 12 weeks | 141.56 (23.88) | 7.25 | 135.22 (17.70) | 6.13 | 13.00 | −0.510 | .610 | |
| Diastolic, home BP monitoring, mmHg | Baseline | 92.52 (9.56) | 8.25 | 83.04 (15.78) | 5.63 | 9.00 | −1.189 | .234 |
| 12 weeks | 92.43 (11.53) | 9.25 | 81.53 (7.35) | 5.13 | 5.00 | −0.872 | .061* | |
| Technology utilization categories | ||||||||
| Ease of learning technology | Baseline | 5.63 (1.93) | 7.42 | 5.64 (2.35) | 8.39 | 30.50 | −0.435 | .663 |
| 12 weeks | 6.35 (0.86) | 8.20 | 5.75 (2.22) | 7.90 | 24.00 | −0.127 | .899 | |
| Technology usefulness | Baseline | 3.92 (2.40) | 6.42 | 4.88 (1.43) | 9.06 | 36.50 | −1.126 | .260 |
| 12 weeks | 3.95 (2.09) | 7.70 | 4.04 (2.37) | 8.15 | 26.50 | −0.185 | .859 | |
| Ease of use of technology | Baseline | 5.24 (1.69) | 7.25 | 5.65 (1.67) | 8.50 | 22.50 | −0.535 | .593 |
| 12 weeks | 5.73 (0.89) | 6.80 | 5.61 (2.19) | 8.60 | 31.50 | −0.739 | .460 | |
| Satisfaction with technology | Baseline | 4.93 (1.89) | 8.92 | 4.44 (1.34) | 7.39 | 21.50 | −0.651 | .515 |
| 12 weeks | 4.43 (1.79) | 8.40 | 4.11 (2.16) | 7.80 | 23.00 | −0.245 | .806 | |
Abbreviations: BP, blood pressure; M, mean; QOL, quality of life; SD, standard deviation.
P-values form Mann-Whitney U test and statistically significant at P < .10.
Table 5.
Responsivity to Technology Utilization by Group.
| Technology-based components | Overall sample (N = 18) | Comparison group (n = 8) | Experimental group (n = 10) |
|---|---|---|---|
| Web-based education, % | |||
| <80% response | 22.2 | 25 | 20 |
| ≥80% response | 72.2 | 62.5 | 80 |
| Medication management app use, % | |||
| No | 55.6 | 40 | 60 |
| Yes | 44.4 | 50 | 40 |
| Self-monitoring BP, in weeks, mean (SD) | 7.8 (5.9) | ||
| <4 weeks, % | 29.4 | 50 | 11.1 |
| 5-8 weeks, % | — | — | — |
| ≥9 weeks, % | 70.6 | 45.8 | 88.8 |
| Positive psychological training, (experimental group only) | |||
| <80% response, % | — | — | 40 |
| ≥80% response, % | — | — | 60 |
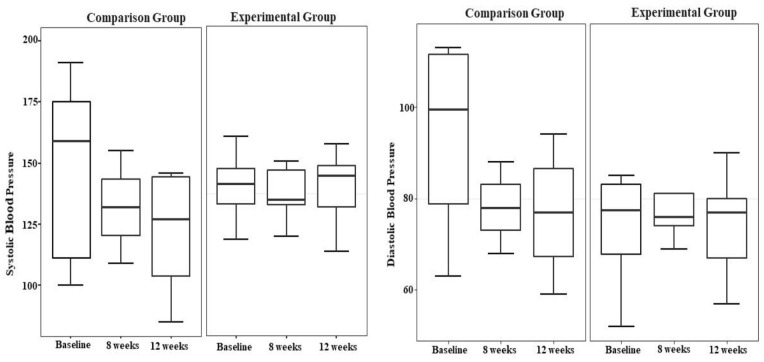
In analyzing the change in BP over time, within-group analyses showed no effect of the TechSupport intervention on systolic and diastolic BP (Figure 1). Additionally, to understand how the technology-based intervention affects health status indicators (BP, PAW QOL, anxiety, depression, positive/negative affect), a repeated measures linear models adjusted for age and years of having hypertension was conducted and showed a few significant relationships (Table 6). Participants in the experimental group improved their both office and home diastolic BP (P = .068 and .016), PAW QOL (P = .042), and positive affect (P = .035) scores over time. There was no effect on anxiety and depression.
Figure 1.
Change in blood pressure over 12 weeks by group.
Table 6.
Associations Between the Technology-Base Intervention and Health Status Indicators.
| Variables b | B | SE | 95% CI | P-value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Systolic BP | 0.095 | 0.069 | −0.052 | 0.242 | .188 |
| Diastolic BP | −0.128 | 0.065 | −0.267 | 0.011 | .068* |
| Home systolic BP | 0.008 | 0.072 | −0.157 | 0.173 | .914 |
| Home diastolic BP | −0.173 | 0.057 | −0.305 | −0.042 | .016* |
| PAW QOL | 0.168 | 0.079 | 0.006 | 0.329 | .042* |
| Negative affect a | −0.045 | 0.171 | −0.412 | 0.323 | .797 |
| Positive affect a | 0.222 | 0.095 | 0.018 | 0.426 | .035* |
| Anxiety | −0.045 | 0.177 | −0.424 | 0.334 | .803 |
| Depression | −0.310 | 0.191 | −0.721 | 0.100 | .127 |
Abbreviations: CI, confidence interval; PAW QOL, positive affective well-being quality of life.
Repeated measures linear model analysis (SAS Proc Mixed) was adjusted for covariates age and years of having hypertension.
Positive and negative affect schedule (PANAS) scale.
Outcome variables were transformed using the natural logarithm.
Statistically significant at P < .10.
Discussion
This study aimed to evaluate the effects of a technology-based intervention containing emotion-focused content in addition to analytic information for hypertension self-management in African Americans with uncontrolled BP. This is the first longitudinal study to examine the effects of a technology-based intervention on health status indicators, guided by a new theoretical framework to explore neurocognitive processing of health information and self-management behaviors. 13 Although most outcomes did not reach statistical significance, the general pattern over time reflected reduction in BP in the experimental group, though the comparison group tended to show greater reduction in their BP. A similar but less obvious pattern of improvements was found for self-efficacy, patient activation, and medication adherence.
Although no statistically significant differences over time were found in BP in either study group; the technology-based components (used in both study groups) were effective in reducing systolic and diastolic BP numbers—an important clinical finding. Participants in both groups were found to have nonsignificant reductions in both systolic and diastolic BP, with the comparison group had slightly higher mean BP reduction of 22.0/9.0 mmHg compared to 3.56/0.11 mmHg in the experimental group after 12 weeks, suggesting a clinically relevant finding. For example, research suggests that systolic BP reductions of 10 mmHg or more is associated with a decreased risk of major cardiovascular disease events, stroke, and heart failure by 20%, 17%, and 28%, respectively. 9 In addition, our findings yielded similar results to the studies aiming to improve BP control and medication adherence using mHealth and/or related technology.29,30 Reducing BP is critical for reducing health disparities related to hypertension in African Americans.
Our intervention also demonstrated important improvements in self-managing behaviors in African Americans with uncontrolled hypertension; specifically, medication adherence, self-efficacy, and patient activation. We found that self-reported medication adherence scores tended to remain steady or improve in both groups, with better adherence scores observed in the comparison group. One explanation for this observation is that the integrated mHealth app component could have promoted and maintained medication-taking adherence behaviors during the study. In terms of using the technology, responsivity to each component varied in both groups. Similar to other studies,5,31 our web-based education and self-monitoring home BP components had high rates of use throughout the study and suggest participants perceived value in using the technology to self-manage their hypertension. Participants in both groups also reported that they agreed that the technology components were easy to learn and use, with slightly higher scores observed in the comparison group, which were sustained throughout the study. This could be explained by the experimental group having more technology components, which included the PPT training when compared to the comparison group.
This study has several strengths. First, it evaluated the effects of a theoretically derived, technology-based intervention, TechSupport, combining analytic and emotional components to improve BP and QOL in African Americans with hypertension guided by a novel framework, the Model of Brain-Behavior Connection in Self-Management of Health and Illness. Our findings suggest that the analytic component of the technology-based intervention may benefit African Americans with hypertension. We were also able to demonstrate initial responsiveness for using a multicomponent, technology-based intervention for self-managing hypertension, and showed a clinically relevant change in BP over time.
The study limitations included the use of a small and convenient sample. In addition, the brevity of the 12-week follow-up limited our ability to observe the full benefits of the intervention in this pilot study. Follow-up studies will expand the study period and target heterogeneity in sociodemographic characteristics (eg, sex). Additionally, future studies will benefit from examining each technology-based component’s level of functionality and user satisfaction using a mixed-method approach.
Conclusion
Technology is increasingly being used to promote and support self-management of chronic conditions, and opportunities exist to improve self-managing hypertension in African Americans with uncontrolled hypertension. Our findings suggest that using a behavioral self-management intervention incorporating technology are clinically useful and can be used to empower this group to assume a more active role in self-managing their hypertension. This pilot supports further research to examine this strategy for hypertension self-management in this high-risk population.
Acknowledgments
The authors would like to thank Phuong Dang and Tangela Peavy for their work on the project.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research reported in this article was supported by the National Institute of Nursing Research of the National Institutes of Health (NIH) under Award Number 5P30NR015326, the Clinical and Translational Science Collaborative of Cleveland KL2TR000440), and the National Center for Advancing Translational Sciences component of the NIH and NIH Roadmap for Medical Research.
ORCID iD: Carolyn H. Still  https://orcid.org/0000-0002-7106-9246
https://orcid.org/0000-0002-7106-9246
References
- 1. Schorr EN, Gepner AD, Dolansky MA, et al. Harnessing mobile health technology for secondary cardiovascular disease prevention in older adults: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes. 2021;14(5):e000103. doi: 10.1161/HCQ.0000000000000103 [DOI] [PubMed] [Google Scholar]
- 2. Burke LE, Ma J, Azar KM, et al. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2015;132(12):1157-1213. doi: 10.1161/CIR.0000000000000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health. 2014;104(8):e25-e31. doi: 10.2105/AJPH.2014.302041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1-7. [DOI] [PubMed] [Google Scholar]
- 5. Band R, Bradbury K, Morton K, et al. Intervention planning for a digital intervention for self-management of hypertension: a theory-, evidence- and person-based approach. Implement Sci. 2017;12(1):25. doi: 10.1186/s13012-017-0553-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bobrow K, Farmer AJ, Springer D, et al. Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-text adherence support [StAR]): a single-blind, randomized trial. Circulation. 2016;133(6):592-600. doi: 10.1161/CIRCULATIONAHA.115.017530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Still CH, Jones LM, Moss KO, Variath M, Wright KD. African American older adults’ perceived use of technology for hypertension self-management. Res Gerontol Nurs. 2018;11(5):249-256. doi: 10.3928/19404921-20180809-02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Center for Disease Control and Prevention. Facts about Hypertension. Accessed May 5, 2021. https://www.cdc.gov/bloodpressure/facts.htm
- 9. Whelton PK, Carey RM, Aronow W, et al. ACC/AHA/AAPA/ABC/ACPM/AGS /APhAASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2017;2017;71(6):1269-1324. doi: 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- 10. Howard G, Cushman M, Moy CS, et al. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA. 2018;320(13):1338-1348. doi: 10.1001/jama.2018.13467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ryan P, Sawin KJ. The individual and family self-management theory: background and perspectives on context process and outcomes. Nurs Outlook. 2009;57:217-225.e6. doi: 10.1016/j.outlook.2008.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jack AI, Dawson AJ, Begany KL, et al. fMRI reveals reciprocal inhibition between social and physical cognitive domains. Neuroimage. 2013;66:385-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moore SM, Musil CM, Jack AI, et al. Characterization of brain signatures to add precision to self-management health information interventions. Nurs Res. 2019;68(2):127-134. doi: 10.1097/NNR.0000000000000331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alberts H, Pennock SF. Positive psychology coaching; Manuals for coach and client. 2013. Accessed September 12, 2018. http://www.positivepsychologyprogram.com
- 15. Huffman JC, DuBois CM, Millstein RA, Celano CM, Wexler D. Positive psychological interventions for patients with type 2 diabetes: rationale, theoretical model, and intervention development. J Diabetes Res. 2015;2015:428349. doi: 10.1155/2015/428349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Huntley CD, Fisher PL. Examining the role of positive and negative metacognitive beliefs in depression. Scand J Psychol. 2016;57(5):446-452. doi: 10.1111/sjop.12306 [DOI] [PubMed] [Google Scholar]
- 17. Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension. 2019;73(5):e35-e66. doi: 10.1161/HYP.0000000000000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179-1194. doi: 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Krousel-Wood M, Peacock E, Joyce C, et al. A hybrid 4-item Krousel-Wood medication adherence scale predicts cardiovascular events in older hypertensive adults. J Hypertens. 2019;37(4):851-859. doi: 10.1097/HJH.0000000000001955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bangor A, Kortum PT, Miller JT. An empirical evaluation of the system usability scale. Int J Hum Comput Interact. 2008;24(6):574-594. doi: 10.1080/10447310802205776 [DOI] [Google Scholar]
- 21. Gao M, Kortum P, Oswald F. Psychometric evaluation of the USE (usefulness, satisfaction, and ease of use) questionnaire for reliability and validity. Proc Hum Factors Ergon Soc Annu Meet. 2018;62(1):1414-1418. doi: 10.1177/1541931218621322 [DOI] [Google Scholar]
- 22. Van Remoortel H, Giavedoni S, Raste Y, et al. Validity of activity monitors in health and chronic disease: a systematic review. The Int J Behav Nutr Phys Act. 2012;9(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821-1845. doi: 10.1007/s40279-017-0716-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918-1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4(6):256-262. [PubMed] [Google Scholar]
- 26. Bialostosky K, Wright JD, Kennedy-Stephenson J, McDowell M, Johnson CL. Dietary intake of macronutrients, micronutrients, and other dietary constituents: United States 1988-94. Vital Health Stat 11. 2002;245:1-158. [PubMed] [Google Scholar]
- 27. Erkoc SB, Isikli B, Metintas S, Kalyoncu C. Hypertension knowledge-level scale (HK-LS): a study on development, validity and reliability. Int J Environ Res Public Health. 2012;9(3):1018-1029. doi: 10.3390/ijerph9031018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063-1070. [DOI] [PubMed] [Google Scholar]
- 29. Buis L, Hirzel L, Dawood RM, et al. Text messaging to improve hypertension medication adherence in African Americans from primary care and emergency department settings: results from two randomized feasibility studies. JMIR Mhealth Uhealth. 2017;5(2):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Morawski K, Ghazinouri R, Krumme A, et al. Association of a smartphone application with medication adherence and blood pressure control: the MedISAFE-BP randomized clinical trial. JAMA Intern Med. 2018;178(6):802-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kebede MM, Pischke CR. Corrigendum: popular diabetes apps and the impact of diabetes app use on self-care behaviour: a survey among the digital community of persons with diabetes on social media. Front Endocrinol. 2019;10(135):220. doi: 10.3389/fendo.2019.00135 [DOI] [PMC free article] [PubMed] [Google Scholar]