Abstract
The outbreak of the novel severe acute respiratory syndrome coronavirus 2 infection in 2019 has posed major risks to global health and the economy. This coronavirus disease (COVID‐19) pandemic has changed many of our everyday habits, including how we function and socialize, how we eat, and food preferences and selection. The average intake and status of certain vitamins and minerals can result in reduced immunity, which makes people more susceptible to illnesses and exacerbates malnutrition. The most critical factors in this scenario are individual risk evaluation and management techniques. Until general therapies are administered, the nutritional status of each infected patient should be assessed. The differing clinical severity of COVID‐19 – from asymptomatic, to mild, to severe, to death – depends on the different metabolic status of the hosts who have contracted the virus, which is determined by their diet, age, gender, health, lifestyle, and environmental factors. A broad systematic exploration on studies of this disease was steered by means of electronic databases and was limited to articles published in English (or with an English abstract) in publications using words like ‘health’, ‘diet’, ‘food’, ‘nutritional status’, ‘COVID‐19’, ‘pandemic’, ‘modifiable contributor’, ‘immune system’, ‘micronutrients’, ‘vitamin’, and so on. Careful individual consideration of the potential dietary, nutritional, medical, lifestyle, and environmental hazards, along with any supplementation with micronutrients wherever required to help to boost the body's natural defence system, with the intention to improve all levels of immunity and the use of effective risk management techniques are appropriate ways to handle the COVID‐19 pandemic. © 2021 Society of Chemical Industry.
Keywords: COVID‐19, health, pandemic, diet, nutritional status
INTRODUCTION
Coronavirus disease (COVID‐19) is caused by the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). The resulting pandemic has become the foremost universal menace to humanity. This coronavirus belongs to a large family of viruses that typically affect wild animals, and in human beings it primarily affects the respiratory system. 1 Experiences from other past disease outbreaks have demonstrated that, when an epidemic occurs, there seems to be an immediate requisite to broaden community well‐being, apart from unswerving medical treatment, and this should be expanded to include basic concepts of resource management and optimization. 2 For a long time, the state of nutrition of people has been a well thought‐out measure of pliability contrary to deterioration. 3 Inadequate nutrition and poor quality of diet are often associated not only with poor physical health but also with altered mental status. 4 , 5
METHODOLOGY
A broad systematic exploration on studies was steered by means of electronic databases and was limited to articles published in English or with an English abstract in publications using words like ‘health’, ‘diet’, ‘food’, ‘nutritional status’, ‘COVID‐19’, ‘pandemic’, ‘modifiable contributor’, ‘immune system’, ‘micronutrients’, ‘vitamin’, and so on. After careful selection of keywords, a MeSH® search was systematized accordingly: (‘Diet, Healthy’[mh]) AND ‘Nutritional Status’[mh]) AND ‘Food Quality’[mh]) AND ‘Risk Factors’[majr]) AND ‘Risk Factors’[mh]) AND ‘COVID‐19’[mh]) AND ‘Pandemics’[mh]) AND ‘Malnutrition’[mh]) AND ‘Health Behavior/education’[mh]) AND ‘Epidemiology’[mh]) AND ‘Nutritional Requirements’[mh]) AND ‘Immune System’[mh]) AND ‘Respiratory Tract Infections’[mh]) AND ‘Micronutrients’[mh]) AND ‘Vitamins’[mh]). Articles indicating a strong link between viral infections (particularly COVID‐19 infection) and micronutrients and the immune system were also selected. When required, the strategy was adapted to each database. This process yielded 95 related articles. Figure 1 shows the conceptual framework of search strategy.
Figure 1.
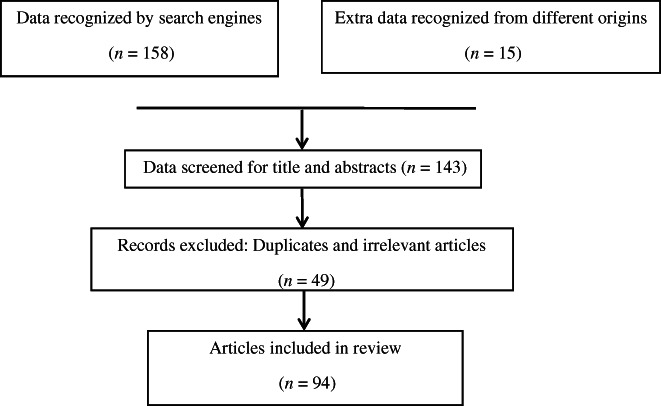
Conceptual framework: search strategy.
ROLE OF NUTRITION IN THE COVID‐19 PANDEMIC
Nutritional status impairments, both obesity and undernutrition, are critical to the clinical outcome of acute diseases. Oxidative stress, deterioration of the immune response, and related pre‐existing disorders (e.g. obesity‐related respiratory, cardiovascular, and metabolic syndromes) are the crucial factors that connect nutritional status and the course and outcome of COVID‐19. In activating an immune system response and inflammatory status, vitamins and minerals play an important role. Overall, the assessment of the nutritional status of the patient is not insignificant because of its consequences for therapy susceptibility, direction, intensity, and response in order to carry out a personalized nutritional intervention as an essential part of the care of COVID‐19 patients. 6 Medical nutrition therapy has been found to have a great impact in preventing and treating malnourishment. Insufficient dietary intake can lead to protein‐energy malnutrition, which can increase the burden of various diseases, as has been shown in previous scientific literature. Conversely, any exposure impairing immunity leads to malabsorption, increases catabolism, including infectious diseases, can raise the risk of malnutrition. According to the literature, symptoms like fever, cough, difficulty in breathing, muscle pain, headache, sore throat, pain in the chest, pneumonia, diarrhoea, nausea, vomiting, loss of sensations like taste and smell are commonly seen in those patients infected with COVID‐19, and all of these can affect nutritional status and eventually the immune function of the body. 7 , 8
Vicious cycle of malnutrition and COVID‐19
The important consequence of malnutrition on health aftermaths has often been verified by new evidence appraising people infected with COVID‐19. The peril of admission to an intensive care unit and impermanence arising from coronavirus infections is increased in persons with several comorbidities, which are usually elderly people or malnourished. Therefore, in the treatment and prevention of additional adverse effects on health from COVID‐19 infestations, nutritional care to recognize and resolve malnutrition is important. Here, Fig. 1, 2, 3 presents a proposed biological and environmental view of COVID‐19 and double burden of malnutrition interaction.
Figure 2.
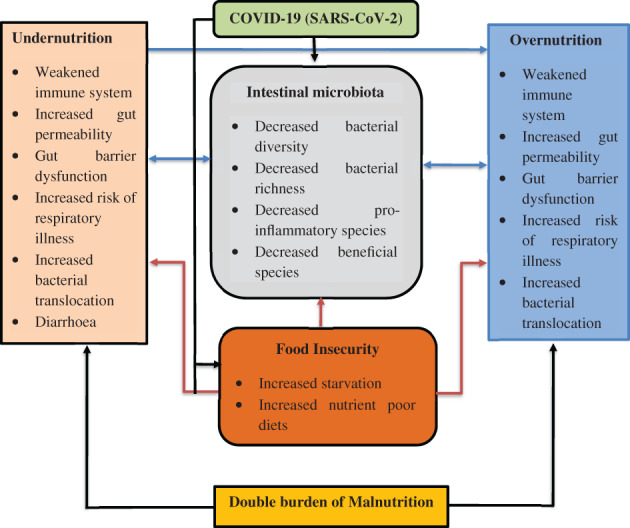
A conceptual biological and environmental interpretation of the relationship between COVID‐19 and the double burden of malnutrition.
Figure 3.
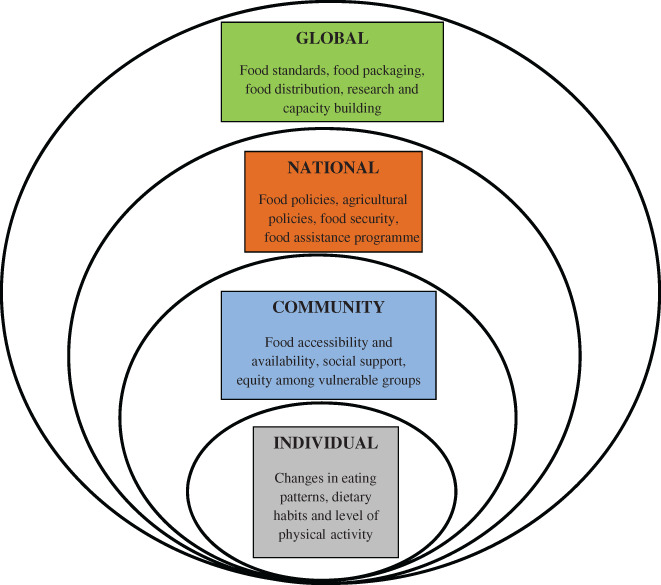
A multi‐stage outline of deed for sustenance of nutrition all through the COVID‐19 pandemic.
From the top: SARS‐CoV‐2 modulates the composition of the intestinal microbiota, resulting in decreases in diversity, abundance, beneficial species, and proinflammatory species enrichment. The double burden of malnutrition shows similar characteristics and dynamics of the intestinal microbiota, thereby predisposing to the severity of SARS‐CoV‐2 infection. COVID‐19 also influences food insecurity, contributing to under‑ and overnutrition, triggering both hunger and intake of ultra‐processed foods. The intestinal microbiota and body mass are both affected by the double burden of malnutrition due to this disruptive compressed relationship. 9
Ecological model of health behaviour to sustain optimal nutrition during COVID‐19
Optimal nutrition and dietary intake can play an important role in transcending the person and the society to achieving a global impact. 10 A structure for sustaining optimum nourishment at the personal, group, countrywide, and international levels is shown in Fig. 3 by means of an altered description of the natural archetype of a fit behaviour. 2
At all levels, whether individual, community, national, or global, the collective factor that governs the major nutrition and dietary interventions to counter viral infestations, like COVID‐19, lie within the connection among food items and immunity. Studies have shown that specific nutrient combinations may affect the immune system by activating cells, modifying production of signalling molecules and gene expression. Therefore, dietetic elements are essential factors of the microbial intestinal opus and can therefore define the properties of the body's immune reactions. Hence, the crucial point to maintaining an efficient immune system is to prevent nutrient insufficiencies that contribute a major part in activating, communicating, differentiating, or functional expression of immune cells. 2
REVIEW OF THE LITERATURE
The literature illustrates that dietary intake has a great influence on the vulnerability of individuals to ailments and that unique diets and/or combinations of nutrients can influence the immune system. 11 Dietetic components are critical for the bacterial communities of the gut or intestine and can, therefore, form the properties of the body's immune response. 12 Energy, protein, and explicit micronutrient deficiencies are correlated with poor immune responses and augmented predisposition to diseases. For looking after immunity, adequate consumption of various nutrients and micro‐elements, like iron (Fe), zinc, vitamins A and E, pyridoxine, and cyanocobalamin, is very important. 13 The best way to maintain an efficient immune system is to prevent nutritional deficiencies that play an important role in activating, communicating, differentiating, or adaptive activation of immune cells. 14 In every pandemic, the state of lockdown leading to internment has unswerving changes on one's way of life, as well as food behaviours, sleeping patterns including types of physical work done. Incarceration leads to an upsurge in sedentary habits involving activities with relatively low energy expenditure carried out mostly in a sitting position. This can adversely affect physical and mental health, leading to erratic consumption patterns with repeated snacking, which are concomitant with an increased intake of calories, leading to a higher risk of obesity. 15 , 16 During the COVID‐19 outbreak, shifts in dietary habits may also have been triggered by fear and anxiety of a lot of people across the world. 17 , 18 , 19 During the COVID‐19 pandemic, it is very important to make a reasonable effort to choose a balanced diet, consuming fruits and vegetables, undertake physical activities during leisure hours, strive to sustain a proper weight, and get enough sleep. In addition to taking care of one's food consumption, there is a mutual duty to prevent the dissemination of nutritional and dietary misinformation and COVID‐19. A fundamental shift has been forced on governments by the COVID‐19 pandemic, making it necessary to develop set‐ups with the private sector, global organizations, and native populations to secure vital nutritional food supplies. Community cognizance programmes, nutritional education agendas, emergency news bulletins, on‐air and television alerts, interviews, and the commitment of dedicated phone hotlines for non‐stop contact with administrative officials may be specific ways to educate people at large about sufficient dietary intake and adequate food consumption. 20
Dietary considerations
Since nutrition is very necessary to keep the immune system strong during the COVID‐19 pandemic, it is very important to consume healthy foods, and the diet must encourage good nutrition. 21 As it is recommended to stay at home most of the time, this leads to less chance of consuming fresh foods and being physically active. Increased consumption of highly processed foods, which appear to be having an increased content of fat, sugar, and salt, can have a detrimental impact on the immune system, the overall physical and mental health, and the global well‐being of individuals. In order to preserve optimum health, we must follow home‐based exercises (such as meditation, pranayama, yoga, free hand exercises, stretching, etc.), along with balanced food and nutrition. So, when purchasing and using foods, we have to be cautious and should follow good food‐handling methods, restricting the consumption of salt, sugar, and fat. 22 If a meal is prepared at home, that does not mean it is nutritious, and not everybody has the same chance to cook meals with healthy ingredients. Nutrition labels can help people to learn more about foods, especially if different foods are acquired due to temporary disturbances in the food supply chain or if more processed or packaged foods are purchased instead of natural foods. Choosing more foods and drinks that are richer in dietary fibre, vitamin D, calcium, Fe, and potassium, along with having less foods and drinks that are high in saturated fat, sodium, and added sugar, for instance, will help minimize the menace of a few mounting issues related to health, such as hypertension, cardiovascular disease, osteoporosis, and anaemia. 20
Health and nutrition recommendations during the COVID‐19 pandemic
The following recommendations have been made by the World Health Organization, the United Nations Children's Fund, and the American Society of Nutrition during the COVID‐19 pandemic: 23 , 24 , 25
It is really important to have good nutrition and hydration.
It is important to drink at least eight to ten glasses of warm water every day. Other beverages, such as lime juice (diluted in water and unsweetened), lemon tea, and coffee, can also be taken. But it is not suggested to consume a lot of caffeine and sweet fruit juices, syrups, fruit juice concentrates, or effervescent and carbonated drinks.
With improved immune systems and lower probabilities of prolonged illnesses and contagious diseases, individuals who consume a well‐balanced diet are likely to be in good health.
To get vitamins, minerals, dietary fibre, protein, and antioxidants that the body requires, a range of fresh and organic foods should be eaten daily.
It is best to evade sugar, fat, and salt, which can dramatically decrease the peril of obesity, heart diseases, stroke, diabetes, and some cancer forms.
It is important to store healthier snack options, such as bread, rice, fruits, vegetables, milk, eggs, and so on.
It is necessary to consume moderate amounts of fat and oil. Instead of red meat, the preference is for white meat (e.g. poultry) and fish, as they are usually lower in fat. Since they are high in fat and salt, processed meats should be avoided. One should opt for low‐fat forms of milk and dairy foodstuffs should where appropriate.
Cooking and eating should be part of the family routine and should be fun and meaningful.
Other substantial general preventive recommendations
While coughing, sneezing, and cooking, there are a few substantial general preventive recommendations that involve regular hand washing, mouth and nose covering. 23
Social isolation helps prevent direct contact with people who are symptomatic and asymptomatic. 23
In all public health interventions, individual behaviours will minimize the risk of infection and control the rigorousness of clinical outcomes that are critical. 26
Epidemiological correlates, like nutritional factors and age, in the causation of various illnesses, including COVID‐19
Research indicates that there are links between age, diet, nutrients, and immunity. 26 In older people, clinical or subclinical micronutrient deficiency is prevalent, leading to many age‐related illnesses and reducing immune functions. 27 , 28 This prevalence is possibly due to a low appetite in the elderly and the nature of little differentiation in their dietary habits. In order to decide the risk of infection, the course of disease, and the outcome of COVID‐19 in older people, nutritional evaluation and careful management are important. 29 The dietary pattern of the host is a crucial component of the culture, structure, and function of gut microbiota. 30 , 31 A diet consisting of prebiotics, probiotics, and polyphenols improves healthy gut microflora 32 and enhances the efficiency of diets in people susceptible to COVID‐19 and different viral diseases, reducing their risk of serious infections. 33 , 34 , 35 , 36 Bidirectional links exist between diet, nutrition, infection, and immunity. A shift in one element has an effect on the others. 37 Antioxidants and anti‐inflammatory nutrients, including β‐carotene, vitamin C, vitamin E, and polyphenolic compounds, are provided by these micro‑ and phytonutrients, which modulate the immune system. 38 , 39 The anti‐inflammatory approach by foods and medicines is a possible alternative for COVID‐19. 40 , 41 An individual's nutritional status also raises the risk of infection with SARS‐CoV‐2, its clinical path, and the results of COVID‐19. Therefore, a major preventive measure for COVID‐19 is the preservation of host macro‑ and micronutrient status. Various micronutrients, particularly vitamins A, C, D, E, and B, iron, selenium, and zinc, are important for immune integrity. For the preservation of individual nutritional status, dietary pattern is vital. 38
Nutritional requirements during COVID‐19
Vitamin D
According to several meta‐analyses and systematic reviews, vitamin D supplements can help in the resistance to respiratory infections, such as of coronavirus, and reduce the severity of the disease in those who are infected. 42 , 43 , 44 , 45 , 46 , 47 According to the literature, increased case‐fatality rates with chronic disease comorbidity and age where lower 25‐hydroxyvitamin D concentrations have been recorded can illustrate the successful role of vitamin D in reducing the risks associated with COVID‐19. Vitamin D deficiency is prevalent globally, particularly in the elderly. 48 More than half of the elderly and nursing‐home residents in hospital are vitamin D deficit. 49 , 50 This high prevalence might lead to the outbreak of COVID‐19 and the high mortality rate in older adults. 51 , 52 , 53 , 54 Sitting at the side of the window or any place in the house where sunlight reaches, along with consuming a well‐balanced diet, will help to ensure the normal functioning of the immune system in this pandemic, as it is difficult to get enough vitamin D from food alone. Although sunlight is the natural source of vitamin D, some foods can be rich sources of vitamin D: oily or fatty fish, such as sardines and salmon; eggs; some fortified breakfast cereals, margarines, and yoghurts; fortified milk and plant‐milk products; cheese; fortified juice; and tofu and mushrooms. 56
Vitamin A
Research indicates that the use of vitamin A supplements has substantial beneficial effects as an alternative therapy for some infectious diseases, such as pneumonia and measles, as well as diarrhoea and hand, foot, and mouth diseases. Vitamin A is essential for the establishment and maintenance of the immune system in humans. 57 Studies show that the intake of foods rich in vitamin A can be very effective in preventing many infectious diseases and improving the immune system. 58 , 59 , 60 , 61 , 62 β‐Carotene, which is converted into vitamin A, is important for a healthy immune system. Sweet potatoes, carrots, mangoes, apricots, spinach, kale, broccoli, squash, raw papaya, bottle gourd, and so on are healthy sources of β‐carotene. 56
Vitamin C
The immune‐modulating effects of vitamin C on respiratory infection are well known. 63 , 64 , 65 Mega doses of vitamin C administration before or after the onset of flu symptoms have been confirmed to prevent and alleviate flu symptoms. 66 , 67 According to studies, daily vitamin C supplementation has a modest but consistent impact on reducing the period of common cold symptoms without any adverse effects. 68 , 69 , 70 , 71 Vitamin C supplementation is therefore the sensible choice to prevent and encourage immune responses in individuals at risk of COVID‐19 who might have micronutrient deficiency. Rich sources of vitamin C include the following: Indian gooseberry or amla; citrus fruits, such as limes, oranges, lemons, mangoes, and guavas; tomatoes and tomato juice, potatoes; capsicums; strawberries; and green leafy vegetables. 57
Selenium
Selenium, owing to its antioxidant nature and redox signalling with homeostatic contributions, plays a vital role in the protection against many viral infections. 72 Selenium deficiency is also correlated with increased pathogenicity of numerous viral infections. 73 , 74 , 75 Selenium supplementation is very helpful for the prevention and treatment of viral infections in the deficient state. 76 , 77 , 78 Selenium intake thus differentially affects various forms of immune responses and key activities, suggesting that selenium supplementation has an important function in viral and infectious diseases, such as coronavirus infection. Rich sources of selenium are shellfish, red meat, grains, eggs, chicken, liver, garlic, yeast, wheat germ, and enriched breads. 73
Zinc
There is plenty of evidence that the mineral zinc plays a role in the antiviral immune mechanism against a variety of viruses, where zinc acts as an immune system gatekeeper and all immune cells are highly zinc dependent. 79 , 80 Zinc deficiency hinders antiviral immunity, especially with the common cold, herpes simplex virus, hepatitis C, and the human immune deficiency virus. 81 , 82 A meta‐analysis of oral zinc supplementation lessons indicate the advantageous effects on the reduction of symptoms and span of the common cold infection. 83 , 84 , 85 , 86 Ingestion of up to 50 mg of zinc per day can, therefore, serve as protection against the COVID‐19 pandemic, presumably by enhancing the resistance of the host to viral infection. 79 It has also been shown that patients with COVID‐19 are prescribed zinc by many hospitals and practitioners. According to clinical and in vitro evidence, zinc has antiviral effects that can slow the replication of coronaviruses. 87 Beans, chickpeas, lentils, tofu, fortified cereals, nuts, seeds, wheat germ, oysters, crab, lobster, beef, pork chop, dark meat poultry, and yogurt are good sources of zinc. 57
Protein
Protein, which is also considered as a fundamental building block for immune cells and antibodies, helps our immune system to work efficiently. Protein can be derived from both animal‑ and plant‐based sources . Some protein‐rich foods are fish, poultry, beef, milk, yogurt, eggs, and cottage cheese, as well as nuts, seeds, beans, lentils, and so on. Instead of protein‐devoid snacks, such as animal crackers, certain protein‐rich snacks can be consumed, such as roasted chickpeas. 57
Probiotics and prebiotics
The health of the microbiome, which strengthens the immune system, is improved by probiotics and prebiotics. Fermented dairy foods, such as yogurt and kefir, and aged cheeses, as well as fermented foods such as kimchi, sauerkraut, miso, tempeh, and sourdough bread, are sources of probiotics. Whole grains, bananas, onions, garlic, leeks, asparagus, artichokes, and beans are sources of prebiotics. 57
Iron
Iron is important for the host and pathogen. Where deficiency of iron can hinder host immunity, iron overload can also cause harmful viral mutations to spread oxidative stress. 88 Iron deficiency has been identified as a risk factor for the development of recurrent acute infections of the respiratory tract. Hence, consumption of iron‐rich foods is highly recommended. 89
Liquid
We should stay hydrated all the time. Slight dehydration in the body can be a physical stressor. A person should ingest at least 2.5–3.0 L of fluids a day, including all fluids and foods rich in water, such as fruit juices, vegetable juices, soups, tea, coffee, milk, and so on. 57
DISCUSSION AND CONCLUSION
The different metabolic status of virus‐infected hosts – as defined by their dietary habits, nutritional status, age, gender, medical ailments, lifestyle habits, and environmental factors – governs an individual's fate with regard to the differing clinical severity of COVID‐19 symptoms. Table 1 shows the role of micronutrients in respiratory infections.
Table 1.
Role of micronutrients in respiratory infections
| Micronutrient | Findings |
|---|---|
| Vitamin A | Vitamin A helps in a drastic reduction in mortality/morbidity rates with relief from the symptoms clinically and shortening duration of hospital stay |
| Vitamin C | Vitamin C supplementation has been shown to reduce mainly the severity of respiratory infections and its occurrence along with the duration and mortality due to pneumonia |
| Vitamin D | Association between vitamin D deficiency and augmented danger of community‐assimilated pneumonia demonstrates that a positive effect of vitamin D exists against respiratory tract infection |
| Zinc | Oral zinc supplementations have been shown not only to reduce the duration of the common cold but also the occurrence of pneumonia, and hence deficiency of this micronutrient is often associated with an increase in the susceptibility of an individual to recurrent respiratory tract infections |
Individual assessment along with adequate risk management, potential dietary, nutritional, lifestyle, and environmental modifications provides a utilitarian approach to dealing with the COVID‐19 pandemic. Though the scientific literature reveals that, during the COVID‐19 pandemic, adequate intakes of micronutrients like zinc and vitamins C and D have acted as a pharmacological tool acting to boost immunological responses – and clinical trials will help to clarify the underlying mechanisms 90 – overdoses of these essential elements might lead to serious adverse effects. 91 The personal risk of having the disease is driven by individual preventive and protective measures. 92 To restrict spread of the virus, flatten the incidence rate curve, and, finally, infection control, the steps of individual seclusion and social distancing are found to be critical. These initiatives, on the other hand, have a serious effect on accessibility and consumption of food. The availability of food items depends on dynamics that extend beyond the person and are specifically associated with regional, national, and universal strategies. 2 A summary overview of these recommendations is given in Table 2.
Table 2.
Recommendations to alleviate influence of COVID‐19 on nutritional aspects and food safety
| Level | Nutrition approvals during COVID‐19 pandemic |
|---|---|
| Individual |
|
| Community |
|
| Country |
|
| Global |
|
The immune system can only operate properly if it gets enough micronutrients. Immunity is suppressed by micronutrient insufficiency, which affects innate, T‐cell‐mediated, and adapted antibody responses, resulting in a disruption of the regulated host immune response. This condition makes people more vulnerable to infections, which leads to higher morbidity and death. Infections also exacerbate micronutrient deficits by lowering nutrient uptake, raising fluxes, and disrupting the utilization of metabolic pathways. Micronutrients promote physical barriers (skin/mucosa), cellular immunity, and antibody synthesis, all of which contribute to the body's natural defences on three levels. Vitamins A, C, and E, as well as mineral zinc, help to improve skin barrier function. The vitamins A, B6, B12, C, D, E, and folic acid, as well as the minerals iron, zinc, copper, and selenium, work together to promote immune cell defensive functions. Finally, excluding vitamin C and iron, all of these micronutrients are required for antibody synthesis. An average intake and status of certain vitamins and minerals can result in reduced immunity, which makes people more susceptible to illnesses and exacerbates malnutrition. As a result, supplementing with these micronutrients can help to boost the body's natural defence system by improving all three levels of immunity. 93
The key purpose of the guidelines is to sustain individual health status (by both physical actions and mental outlook), community resilience, and national and worldwide food security. 2 Interdependence of these different levels is illustrated by a specific aspect of this pandemic, whereby the well‐being of the person depends on individual's choices, solidarity of the population, vigilance of the government, and eventually the universal commitment to this danger. 2
CONFLICT OF INTEREST
No conflicts of interest are declared.
ACKNOWLEDGEMENTS
We thank the faculty from the Department of Community Medicine, Yenepoya Medical College, Yenepoya (Deemed to be University), Deralakatte, Mangalore, Karnataka, India, and the Department of Physiology, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, India, for their useful suggestions and support.
REFERENCES
- 1. Bogoch II, Watts A, Thomas‐Bachli A, Huber C, Kraemer MU and Khan K, Pneumonia of unknown etiology in Wuhan, China: potential for international spread via commercial air travel. J Travel Med 272:taaa008 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Naja F and Hamadeh R, Nutrition amid the COVID‐19 pandemic: a multi‐level framework for action. Eur J Clin Nutr 20:1117–1121 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cobb TD, Reclaiming Our Food: How the Grassroots Food Movement is Changing the Way We Eat. Storey Publishing, North Adams, MA: (2011). [Google Scholar]
- 4. Yousafzai AK, Rasheed MA and Bhutta ZA, Annual research review: improved nutrition – a pathway to resilience. J Child Psychol Psychiatry 54:367–377 (2013). [DOI] [PubMed] [Google Scholar]
- 5. Hislop TG, Bajdik CD, Balneaves LG, Holmes A, Chan S, Wu E et al., Physical and emotional health effects and social consequences after participation in a low‐fat, high‐carbohydrate dietary trial for more than 5years. J Clin Oncol 24:2311–2317 (2006). [DOI] [PubMed] [Google Scholar]
- 6. Fedele D, De Francesco A, Riso S and Collo A, Obesity, malnutrition and trace elements deficiency in the COVID‐19 pandemic: an overview. Nutrition 2020:111016 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Handu D, Moloney L, Rozga M and Cheng FW, Malnutrition care during the COVID‐19 pandemic: considerations for registered dietitian nutritionists. J Acad Nutr Diet 121:979–987 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cuevas A and Barquera S, COVID‐19, obesity, and undernutrition: a major challenge for Latin American Countries. Obesity 28:1791–1792 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Littlejohn P and Finlay BB, When a pandemic and an epidemic collide: COVID‐19, gut microbiota, and the double burden of malnutrition. BMC Med 19:1–8 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ma YJ and Lee HH, Understanding consumption behaviours for fair trade non‐food products: focusing on self‐transcendence and openness to change values. Int J Consum Stud 36:622–634 (2012). [Google Scholar]
- 11. Valdés‐Ramos R, Martínez‐Carrillo BE, Aranda‐González II, Guadarrama AL, Pardo‐Morales RV, Tlatempa P et al., Diet, exercise and gut mucosal immunity. Proc Nutr Soc 69:644–650 (2010). [DOI] [PubMed] [Google Scholar]
- 12. Wypych TP, Marsland BJ and Ubags ND, The impact of diet on immunity and respiratory diseases. Ann Am Thorac Soc 14:S339–S347 (2017). [DOI] [PubMed] [Google Scholar]
- 13. Gleeson M, Nieman DC and Pedersen BK, Exercise, nutrition and immune function. J Sports Sci 22:115–125 (2004). [DOI] [PubMed] [Google Scholar]
- 14. Haug A, Brand‐Miller JC, Christophersen OA, McArthur J, Fayet F and Truswell SA, Food ‘lifeboat’: food and nutrition considerations in the event of a pandemic or other catastrophe. Med J Aust 187:674–676 (2007). [DOI] [PubMed] [Google Scholar]
- 15. Hobbs M, Pearson N, Foster PJ and Biddle SJ, Sedentary behaviour and diet across the lifespan: an updated systematic review. Br J Sports Med 49:1179–1188 (2015). [DOI] [PubMed] [Google Scholar]
- 16. Scully M, Dixon H and Wakefield M, Association between commercial television exposure and fast‐food consumption among adults. Public Health Nutr 12:105–110 (2009). [DOI] [PubMed] [Google Scholar]
- 17. Anton SD and Miller PM, Do negative emotions predict alcohol consumption, saturated fat intake, and physical activity in older adults? Behav Modif 29:677–688 (2005). [DOI] [PubMed] [Google Scholar]
- 18. Macht M, Characteristics of eating in anger, fear, sadness and joy. Appetite 33:129–139 (1999). [DOI] [PubMed] [Google Scholar]
- 19. Macht M, How emotions affect eating: a five‐way model. Appetite 50:1–11 (2008). [DOI] [PubMed] [Google Scholar]
- 20. Pan American Health Organization Food security and livelihoods. Tool 11: distribution of emergency food during a pandemic. [Online]. Food and Culture Organization of the United Nations (2020). Available: https://www.paho.org/disasters/index.php?option=com_docman&view=download&category_slug=tools&alias=538‐pandinflu‐leadershipduring‐tool11&itemid=1179&lang=en
- 21. US Food and Drug Administration . Tips on good nutrition and using the updated nutrition facts label during the coronavirus pandemic. [Online]. US Food and Drug Administration (2020). Available: https://www.fda.gov/consumers/consumer‐updates/tips‐good‐nutrition‐and‐using‐updated‐nutrition‐facts‐label‐during‐coronavirus‐pandemic
- 22. World Health Organization . Food and nutrition during self‐quarantine: what to choose and how to eat healthily. [Online]. World Health Organization (WHO/Europe) (2020). Available: http://www.euro.who.int/en/health‐topics/health‐emergencies/coronavirus‐covid‐19/news/news/2020/3/food‐and‐nutrition‐during‐self‐quarantine‐what‐to‐choose‐and‐how‐to‐eat‐healthily
- 23. World Health Organization , Regional office for the Eastern Mediterranean. Nutrition advice for adults during the COVID‐19 outbreak. [Online]. WHO (2020). Available: http://www.emro.who.int/nutrition/nutrition‐infocus/nutrition‐advice‐for‐adults‐during‐the‐covid‐19‐outbreak.html
- 24. UNICEF . Easy, affordable and healthy eating tips during the coronavirus disease (COVID 19) outbreak: ideas to help your family maintain a nutritious diet. [Online]. UNICEF (2020). Available: https://www.unicef.org/coronavirus/easy‐affordable‐and‐healthy‐eating‐tips‐during‐coronavirus‐disease‐covid‐19‐outbreak
- 25. ASN (EST, 1928) , Making health and nutrition a priority during the coronavirus (COVID‐19) pandemic 2020. [Online]. American Society for Nutrition (2020). Available: https://nutrition.org/making‐health‐and‐nutrition‐a‐priority‐during‐the‐coronavirus‐covid‐19‐pandemic/
- 26. Young TK and Zampella JG, Supplements for COVID‐19: a modifiable environmental risk. Clin Immunol 216:108465 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang Y, Li W, Zhang Q, Zhang L, Cheung T and Xiang YT, Mental health services for older adults in China during the COVID‐19 outbreak. Lancet Psychiatry 7:e19 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hoffman R, Micronutrient deficiencies in the elderly – could ready meals be part of the solution? J Nutr Sci 6:1–4 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Conzade R, Koenig W, Heier M, Schneider A, Grill E, Peters A et al., Prevalence and predictors of subclinical micronutrient deficiency in German older adults: results from the population‐based KORA‐age study. Nutrients 9:1276–1294 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lipsitch M, Swerdlow DL and Finelli L, Defining the epidemiology of Covid‐19 – studies needed. N Engl J Med 382:1194–1196 (2020). [DOI] [PubMed] [Google Scholar]
- 31. Kolodziejczyk AA, Zheng D and Elinav E, Diet–microbiota interactions and personalized nutrition. Nat Rev Microbiol 17:742–753 (2019). [DOI] [PubMed] [Google Scholar]
- 32. Zmora N, Suez J and Elinav E, You are what you eat: diet, health and the gut microbiota. Nat Rev Gastroenterol Hepatol 16:35–56 (2019). [DOI] [PubMed] [Google Scholar]
- 33. Edwards DK, Jasny E, Yoon H, Horscroft N, Schanen B, Geter T et al., Adjuvant effects of a sequence‐engineered mRNA vaccine: translational profiling demonstrates similar human and murine innate response. J Transl Med 15:1–8 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Trompette A, Gollwitzer ES, Pattaroni C, Lopez‐Mejia IC, Riva E, Pernot J et al., Dietary fiber confers protection against flu by shaping Ly6c– patrolling monocyte hematopoiesis and CD8+ T cell metabolism. Immunity 48:992–1005 (2018). [DOI] [PubMed] [Google Scholar]
- 35. Kanauchi O, Andoh A, AbuBakar S and Yamamoto N, Probiotics and paraprobiotics in viral infection: clinical application and effects on the innate and acquired immune systems. Curr Pharm Des 24:710–717 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Eguchi K, Fujitani N, Nakagawa H and Miyazaki T, Prevention of respiratory syncytial virus infection with probiotic lactic acid bacterium Lactobacillus gasseri SBT2055. Sci Rep 9:1–11 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lehtoranta L, Pitkäranta A and Korpela R, Probiotics in respiratory virus infections. Eur J Clin Microbiol Infect Dis 33:1289–1302 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Maggini S, Pierre A and Calder PC, Immune function and micronutrient requirements change over the life course. Nutrients 10:1531 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zhang L and Liu Y, Potential interventions for novel coronavirus in China: a systematic review. J Med Virol 92:479–490 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Calder PC, Carr AC, Gombart AF and Eggersdorfer M, Optimal nutritional status for a well‐functioning immune system is an important factor to protect against viral infections. Nutrients 12:1181 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kritas SK, Ronconi G, Caraffa A, Gallenga CE, Ross R and Conti P, Mast cells contribute to coronavirus‐induced inflammation: new anti‐inflammatory strategy. J Biol Regul Homeostatic Agents 34:9–14 (2020). [DOI] [PubMed] [Google Scholar]
- 42. Conti P, Ronconi G, Caraffa AL, Gallenga CE, Ross R, Frydas I et al., Induction of pro‐inflammatory cytokines (IL‐1 and IL‐6) and lung inflammation by coronavirus‐19 (COVI‐19 or SARS‐CoV‐2): anti‐inflammatory strategies. J Biol Regul Homeostatic Agents 34:327–331 (2020). [DOI] [PubMed] [Google Scholar]
- 43. Bergman P, Lindh ÅU, Björkhem‐Bergman L and Lindh JD, Vitamin D and respiratory tract infections: a systematic review and meta‐analysis of randomized controlled trials. PloS One 8:e65835 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Charan J, Goyal JP, Saxena D and Yadav P, Vitamin D for prevention of respiratory tract infections: a systematic review and meta‐analysis. J Pharmacol Pharmacother 3:300–303 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta‐analysis of individual participant data. BMJ 356–369 (2017). doi: 10.1136/bmj.i6583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov‐Raz G et al., Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta‐analysis. Health Technol Assess 23:1–44 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Teymoori‐Rad M, Shokri F, Salimi V and Marashi SM, The interplay between vitamin D and viral infections. Rev Med Virol 29:e2032 (2019). [DOI] [PubMed] [Google Scholar]
- 48. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL et al., Evidence that vitamin D supplementation could reduce risk of influenza and COVID‐19 infections and deaths. Nutrients 12:988 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Nair R and Maseeh A, Vitamin D: the ‘sunshine’ vitamin. J Pharmacol Pharmacother. 3:118–126 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Heck AM, Yanovski JA and Calis KA, Orlistat, a new lipase inhibitor for the management of obesity. Pharmacotherapy 20:270–279 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kennel KA, Drake MT and Hurley DL, Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc 85:752–758 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Holick MF, Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80:1678S–1688S (2004). [DOI] [PubMed] [Google Scholar]
- 53. Nonnecke BJ, McGill JL, Ridpath JF, Sacco RE, Lippolis JD and Reinhardt TA, Acute phase response elicited by experimental bovine diarrhea virus (BVDV) infection is associated with decreased vitamin D and E status of vitamin‐replete preruminant calves. J Dairy Sci 97:5566–5579 (2014). [DOI] [PubMed] [Google Scholar]
- 54. Greiller CL and Martineau AR, Modulation of the immune response to respiratory viruses by vitamin D. Nutrients 7:4240–4270 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Science M, Maguire JL, Russell ML, Smieja M, Walter SD and Loeb M, Low serum 25‐hydroxyvitamin D level and risk of upper respiratory tract infection in children and adolescents. Clin Infect Dis 57:392–397 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wimalawansa SJ, Global epidemic of coronavirus – COVID‐19: what can we do to minimize risks. Eur J Biomed Pharm Sci 7:432–438 (2020). [Google Scholar]
- 57. Drayer L. How to strengthen your immunity during the coronavirus pandemic: exercise, meditation, sleep and stress management. CNN Health (2020). Available: https://edition.cnn.com/2020/03/25/health/immunity-diet-food-coronavirus-drayer-wellness/index.html
- 58. Semba RD, Vitamin A and immunity to viral, bacterial and protozoan infections. Proc Nutr Soc 58:719–727 (1999). [DOI] [PubMed] [Google Scholar]
- 59. Boy E. Coronavirus pandemic s need to ensure good nutrition. [Online]. Harvest Plus (2020). Available: https://www.harvestplus.org/knowledge-market/in-the-news/coronavirus-pandemic- s‐need‐ensure‐good‐nutrition
- 60. McGill JL, Kelly SM, Guerra‐Maupome M, Winkley E, Henningson J, Narasimhan B et al., Vitamin A deficiency impairs the immune response to intranasal vaccination and RSV infection in neonatal calves. Sci Rep 9:1–4 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Patel N, Penkert RR, Jones BG, Sealy RE, Surman SL, Sun Y et al., Baseline serum vitamin A and D levels determine benefit of oral vitamin A&D supplements to humoral immune responses following pediatric influenza vaccination. Viruses 11:907 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Jee J, Hoet AE, Azevedo MP, Vlasova AN, Loerch SC, Pickworth CL et al., Effects of dietary vitamin A content on antibody responses of feedlot calves inoculated intramuscularly with an inactivated bovine coronavirus vaccine. Am J Vet Res 74:1353–1362 (2013). [DOI] [PubMed] [Google Scholar]
- 63. Kańtoch M, Litwińska B, Szkoda M and Siennicka J, Importance of vitamin A deficiency in pathology and immunology of viral infections. Rocz Panstw Zakl Hig 53:385–392 (2002). (in Polish). [PubMed] [Google Scholar]
- 64. Hess AF, Diet, nutrition and infection. N Engl J Med 207:637–644 (1933). [Google Scholar]
- 65. Robertson EC, The vitamins and resistance to infection. Medicine 13:123–206 (1934). [Google Scholar]
- 66. Hemilä H, Vitamin C and infections. Nutrients 9:339 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Van Driel ML, Beller EM, Thielemans E, Deckx L, Price‐Haywood E, Clark J et al., Oral vitamin C supplements to prevent and treat acute upper respiratory tract infections. Cochrane Database Syst Rev 3:1–13 (2019). [Google Scholar]
- 68. Hemilä H and Chalker E, Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev 1:1–103 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Colunga Biancatelli RM, Berrill M and Marik PE, The antiviral properties of vitamin C. Expert Rev Anti‐Infect Ther 18:99–101 (2020). [DOI] [PubMed] [Google Scholar]
- 70. Gorton HC and Jarvis K, The effectiveness of vitamin C in preventing and relieving the symptoms of virus‐induced respiratory infections. J Manipulative Physiol Ther 22:530–533 (1999). [DOI] [PubMed] [Google Scholar]
- 71. Maggini S, Beveridge S and Suter M, A combination of high‐dose vitamin C plus zinc for the common cold. J Int Med Res 40:28–42 (2012). [DOI] [PubMed] [Google Scholar]
- 72. Guillin OM, Vindry C, Ohlmann T and Chavatte L, Selenium, selenoproteins and viral infection. Nutrients 11:1–33 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Beck MA, Nelson HK, Shi Q, Van Dael P, Schiffrin EJ, Blum S et al., Selenium deficiency increases the pathology of an influenza virus infection. FASEB J 15:1481–1483 (2001). [PubMed] [Google Scholar]
- 74. Beck MA, Kolbeck PC, Rohr LH, Shi Q, Morris VC and Levander OA, Benign human enterovirus becomes virulent in selenium‐deficient mice. J Med Virol 43:166–170 (1994). [DOI] [PubMed] [Google Scholar]
- 75. Watkins H, Conner D, Thierfelder L, Jarcho JA, MacRae C, McKenna WJ et al., Mutations in the cardiac myosin binding protein‐C gene on chromosome 11 cause familial hypertrophic cardiomyopathy. Nat Genet 11:434–437 (1995). [DOI] [PubMed] [Google Scholar]
- 76. Harthill M, Micronutrient selenium deficiency influences evolution of some viral infectious diseases. Biol Trace Elem Res 143:1325–1336 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Rayman MP, Selenium and human health. Lancet 379:1256–1268 (2012). [DOI] [PubMed] [Google Scholar]
- 78. Shojadoost B, Kulkarni RR, Yitbarek A, Laursen A, Taha‐Abdelaziz K, Alkie TN et al., Dietary selenium supplementation enhances antiviral immunity in chickens challenged with low pathogenic avian influenza virus subtype H9N2. Vet Immunol Immunopathol 207:62–68 (2019). [DOI] [PubMed] [Google Scholar]
- 79. Razzaque MS, COVID‐19 pandemic: can maintaining optimal zinc balance enhance host resistance? Tohoku J Exp Med 251:175–181 (2020). [DOI] [PubMed] [Google Scholar]
- 80. Shankar AH and Prasad AS, Zinc and immune function: the biological basis of altered resistance to infection. Am J Clin Nutr 68:447S–463S (1998). [DOI] [PubMed] [Google Scholar]
- 81. Read SA, Obeid S, Ahlenstiel C and Ahlenstiel G, The role of zinc in antiviral immunity. Adv Nutr 10:696–710 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Maares M and Haase H, Zinc and immunity: an essential interrelation. Arch Biochem Biophys 611:58–65 (2016). [DOI] [PubMed] [Google Scholar]
- 83. Science M, Johnstone J, Roth DE, Guyatt G and Loeb M, Zinc for the treatment of the common cold: a systematic review and meta‐analysis of randomized controlled trials. CMAJ 184:E551–E561 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Saigal P and Hanekom D, Does zinc improve symptoms of viral upper respiratory tract infection? Evid Based Pract 23:37–39 (2020). [Google Scholar]
- 85. Awotiwon AA, Oduwole O, Sinha A and Okwundu CI, Zinc supplementation for the treatment of measles in children. Cochrane Database Syst Rev 6:1–22 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Read SA, Parnell G, Booth D, Douglas MW, George J and Ahlenstiel G, The antiviral role of zinc and metallothioneins in hepatitis C infection. J Viral Hepatitis 25:491–501 (2018). [DOI] [PubMed] [Google Scholar]
- 87. Te Velthuis AJ, van den Worm SH, Sims AC, Baric RS, Snijder EJ and van Hemert MJ, Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog 6:e1001176 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Wessling‐Resnick M, Crossing the iron gate: why and how transferrin receptors mediate viral entry. Annu Rev Nutr 38:431–458 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Jayaweera J, Reyes M and Joseph A, Childhood iron deficiency anemia leads to recurrent respiratory tract infections and gastroenteritis. Sci Rep 9:12637 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 90. Gasmi A, Noor S, Tippairote T, Dadar M, Menzel A and Bjørklund G, Individual risk management strategy and potential therapeutic options for the COVID‐19 pandemic. J Clin Immunol 215:108409 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Shmerling RH Do vitamin D, zinc, and other supplements help prevent COVID‐19 or hasten healing? [Online]. Harvard Medical School (2021). Available: https://www.health.harvard.edu/blog/do-vitamin-d-zinc-and-other-supplements-help-prevent-covid-19-or-hasten-healing-2021040522310
- 92. Souza AC, Vasconcelos AR, Prado PS and Pereira CP, Zinc, vitamin D and vitamin C: perspectives for COVID‐19 with a focus on physical tissue barrier integrity. Front Nutr 7:295 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Maggini S, Wintergerst ES, Beveridge S and Hornig DH, Selected vitamins and trace elements support immune function by strengthening epithelial barriers and cellular and humoral immune responses. Br J Nutr 98:S29–S35 (2007). [DOI] [PubMed] [Google Scholar]


