Abstract
Introduction:
We need to understand the continued concerns and acceptability of COVID-19 vaccines within marginalized communities in the United States. Our study explores the concerns and acceptability of COVID-19 vaccines, by language group, at a Federally Qualified Health Center (FQHC) in Rhode Island.
Methods:
We conducted an exploratory, mixed data collection telephone survey in languages spoken in the community (Spanish, Cape Verdean (CV) Creole/Portuguese, and English). Participants were asked about their COVID-19 vaccination status, as well as vaccine concerns and acceptability via 9 closed-ended and 2 open-ended questions. Chi squared and multivariate analysis was used to compare concerns and acceptability across languages. Coding and immersion/crystallization techniques were used to identify qualitative data themes.
Results:
The overall response rate was 58%. Side effects were cited as the most frequent (66%) concern among all language groups. Concern about the speed of vaccine development, vaccine ingredients, and being in a research trial varied significantly by language. Qualitative findings included concerns about chronic medical conditions and generalized fear of vaccine safety. English speakers were the most likely to report concerns and CV Creole/Portuguese speakers were the least likely to report concerns about the vaccine. Spanish and CV Creole/Portuguese participants who were not yet vaccinated reported higher acceptability to receive the vaccine compared to English speakers, with odds ratios of 2.00 (95% CI: 1.00-4.00) and 1.27 (95% CI: 0.62-2.60), respectively.
Conclusion:
To mitigate the effects of the COVID-19 pandemic and prepare for future pandemics, strategies must be based on understanding the beliefs and perceptions of marginalized communities.
Keywords: marginalized, underserved communities, COVID-19, vaccine, Spanish speaking, non-English speaking
Introduction
COVID-19 has now killed over 700 000 people in the United States (US), with a disproportionate impact on Black, Latinx, and other marginalized communities.1,2 Racial and ethnic disparities in rates of COVID-19 have been well documented.3,4 As with other diseases, a main driver of disparity appears to be systemic structural barriers to care.5,6
Slightly over 50% of the US population is now vaccinated against the virus, but a significantly higher percentage is needed to end the pandemic. 7 Along with access and distribution issues, lack of confidence in the vaccine remains a barrier to achieving target vaccination rates. 8 Vaccine hesitancy has been well documented in the US, though mainly with data collected from English-speaking populations. There is limited available data on the perceptions of COVID-19 vaccines among the underrepresented communities most impacted by this pandemic.9,10 To craft effective vaccination campaign strategies and messages, it is important to understand the specific concerns not only of English-speakers, but also of non-English-speakers in the US, and how these concerns might differ across language groups. Only a few studies have been documented that include Spanish speakers and compare results across language groups.11,12
In a Pew research survey conducted in February 2021, 30% of US adults reported that they did not plan to get the vaccine. Major concerns included vaccine side effects (72%), the speed of vaccine development and testing (67%), and a lack of understanding about how vaccines work (61%). Other factors included negative experiences in a healthcare system (46%) and perceived lack of benefit (42%). 13 Other studies have shown that COVID-19 vaccine concerns are similar to concerns expressed about other routine vaccines with the addition of new factors including targeted anti-vaccination campaigns and political affiliation.14 -16 Conversely, factors associated with vaccine confidence include healthcare provider recommendations and trust in news sources.17,18
One community heavily impacted by the COVID-19 virus is Central Falls, Rhode Island, which in June 2021 had the highest prevalence of cases in the state, at 22 892 cases per 100 000 people. 19 Between February and March 2021, COVID-19 vaccine eligibility was expanded in Central Falls and other hard-hit communities in Rhode Island, from only including adults 65 and over, to including all adults. 20 Central Falls has a diverse, traditionally marginalized population including Spanish speaking and Cape Verdean (CV) Creole/Portuguese speaking communities.21,22 There is a lack of COVID-19 vaccine hesitancy data based on ethnicity and race at the national level and no published data regarding marginalized communities in Rhode Island. Blackstone Valley Community Health Care (BVCHC), a Federally Qualified Health Center with a COVID-19 vaccination site, provides primary care to this community.
To directly inform an educational and early COVID-19 vaccine distribution campaign at BVCHC, we conducted an exploratory, mixed data collection survey to understand the factors associated with lack of confidence and acceptability of the COVID-19 vaccine. The diverse patient population of BVCHC allowed us a unique opportunity to examine the specific concerns of language sub-populations and other factors associated with COVID-19 vaccine concerns and acceptability.
Methods
BVCHC is a Federally Qualified Health Center serving 26 000 patients in the cities of Pawtucket, Providence, and Central Falls, Rhode Island. 23 About half of the patients (55%) identify as Hispanic or Latinx and 23% identify as Black or African American. According to electronic medical record (EMR) data, about half of the patients (55%) speak English as their primary language, 35% speak Spanish, 3% speak Portuguese, and 5% speak Cape Verdean Creole. Census data from 2019 show that over 25% of the Central Falls population is born outside of the US. 24 Due to high COVID-19 rates in the community, the clinic was prioritized by the state for distribution of the COVID-19 vaccine.
Ethical approval for this study was obtained from BVCHC leadership. The study did not require IRB approval nor an exempt determination because the primary purpose of data collection was to inform an education campaign at BVCHC by clinic staff.
Prior to BVCHC’s internal staff vaccination efforts in early December 2020, an anonymous open-ended questionnaire was distributed to employees to capture their concerns and questions regarding the COVID-19 vaccines. We used the results of this employee questionnaire, evaluated with face validity, to inform the development of survey questions for our study. BVCHC staff and leadership also provided input. A literature review of previous COVID-19 vaccine surveys and validated routine vaccine surveys was also conducted and used to inform the survey.14,16 -18,25 -27 The final survey tool is available as an Appendix.
All participants were asked if they had already received the COVID-19 vaccine. Participants who had not yet been vaccinated were asked closed-ended questions on 9 topics of potential concern: vaccine effectiveness, general side effects, infertility, speed of vaccine development, ingredients in the vaccine, participants’ medical conditions, participants’ medications, faith or religion, and being part of a research trial. Participants were asked if they were “not concerned,” “somewhat concerned,” or “very concerned” about each of these topics. Participants who had not yet been vaccinated were asked a final closed-ended question about acceptability of getting the vaccine: “Would you like to be put on a list to get the COVID vaccine from BVCHC?”
The survey also included 2 open-ended questions. Participants who had received the vaccine were asked why they chose to do so. Prior to being asked the closed-ended questions, those who were not yet vaccinated were asked an open-ended question on the concerns they had about the vaccine. Additionally, for every participant, we collected demographic data on language, age, gender, race/ethnicity, and education.
We aimed to obtain a sample that would allow us to calculate estimates that would be representative of the BVCHC patient population and to achieve sufficient precision for disaggregated estimates for the primary languages spoken in the community. To do this, we over-sampled CV Creole, Portuguese, and Spanish-speaking populations, and accounted for this over-sampling in data analysis. Portuguese and CV Creole speakers were combined into 1 group for analysis, as most participants listed as speaking Portuguese in EMR data spoke CV Creole, and all these participants identified as Cape Verdean when asked about their ethnicity. Stratified random sampling was used to generate a list of eligible participants aged 18 or older, seen at the clinic in the last 3 years, from EMR data. Patients on this list were grouped by language and from each group we randomly sampled 247 English-, 100 CV Creole/Portuguese-, and 174 Spanish-speaking patients. Assuming a 50% population proportion and 95% confidence interval, this was estimated to allow a margin of error of ±4 percentage points (pp) overall for the closed-ended, categorical questions in the survey, and ±6 pp for English, ±7 pp for Spanish, and ±10 CV Creole/Portuguese disaggregated results.
Surveys were administered via telephone in English, Spanish, CV Creole, and Portuguese between February 23rd, 2021, and April 5th, 2021, by 10 interviewers. Interviewers were volunteers, community health workers, clinic staff members, and master’s students who received training to administer the survey. We used Qualtrics survey software to capture participant responses during phone interviews. 28 Interviewers were instructed to type answers to open-ended questions verbatim, entering detailed notes into open text fields in Qualtrics. Eligible participants were called up to 4 times before being documented as “no response.” Weekly Zoom check-ins were conducted with study coordinators (MB, SV, DR) and interviewers to allow for quality checks, to ensure consistency in implementation, and to monitor non-response rates.
Statistical analyses were conducted using Stata Version 15. 29 De-identified secondary demographic data from the EMR were matched to the primary data from the survey. We report unweighted demographic statistics for participants who were vaccinated and those who were not yet vaccinated. For the remainder of the quantitative analyses, which considered only the responses of participants who were not yet vaccinated, we used Stata’s SVY commands to obtain correct population estimates and confidence intervals, accounting for oversampling, population weights, and non-response rates for each question. Records with missing answers to survey questions and demographic data were excluded from the analysis entirely. Chi-squared tests were used to compare vaccine concerns by language. Multivariate logistic regression was used to further assess the differences in concerns between individual language groups.
Bivariate and multivariate logistic regression were used to analyze the relationship between demographics and vaccine acceptability, producing unadjusted and adjusted odds ratios, respectively. The adjusted models included language, age, gender, and education as independent variables, and vaccine acceptability as the outcome of interest or dependent variable. Race and ethnicity were excluded due to significant collinearity with language.
A Microsoft Excel template was used to code the data from 2 open-ended questions. An iterative process of template-organizing-style coding with a codebook and immersion/crystallization through in-depth reading of the responses was used to identify key themes and patterns. 30 KL reviewed the open-ended responses and generated a preliminary coding sheet. MB, SV, DR also went through the responses independently. To finalize codes and organize responses, MB, SV, and DR worked together with qualitative expert REG.
Results
The response rate for the survey was 58%, with 303 out of 521 eligible participants completing the survey. Specifically, the response rate was 40% (n = 99) for English speakers, 72% (n = 126) for Spanish speakers, 78% (n = 78) for CV Creole/Portuguese speakers. There was no difference in response rate by gender or age.
At the time the survey was administered, 71% (n = 216) of participants were not yet vaccinated. Table 1 shows the participant characteristics at time of survey completion by vaccine status. Among all survey participants, 42% (n = 126) were Spanish speakers, 33% (n = 99) English speakers, and 26% (n = 78) were CV Creole/Portuguese speakers. More than half of all participants identified as Hispanic or Latinx (53.5%, n = 162) and around one third identified as Black or African American (35.0%, n = 106). The most frequent level of education reported for both vaccinated and not yet vaccinated participants was high school, with an overall percentage of 40.6% (n = 123).
Table 1.
Characteristics of Survey Participants by COVID-19 Vaccination Status, Unweighted. a
| Not yet vaccinated* % (n) | Already vaccinated % (n) | Total % (n) | |
|---|---|---|---|
| All | 71.3% (216) | 28.7% (87) | 100% (303) |
| Language | |||
| English | 30.1% (65) | 39.1% (34) | 32.7% (99) |
| CV Creole/Portuguese | 29.2% (63) | 17.2% (15) | 25.7% (78) |
| Spanish | 40.7% (88) | 43.7% (38) | 41.6% (126) |
| Age | |||
| 18-34 | 40.3% (87) | 17.2% (15) | 33.7% (102) |
| 35-49 | 35.2% (76) | 23.0% (20) | 31.7% (96) |
| 50-64 | 20.8% (45) | 34.5% (30) | 24.8% (75) |
| 65+ | 3.7% (8) | 25.3% (22) | 9.9% (30) |
| Gender | |||
| Male | 28.2% (61) | 42.5% (37) | 32.3% (98) |
| Female | 71.8% (155) | 57.5% (50) | 67.7% (205) |
| Race and ethnicity | |||
| American Indian or Alaska Native | 0.5% (1) | 0.0% (0) | 0.3% (1) |
| Black or African American | 36.1% (78) | 32.2% (28) | 35.0% (106) |
| Hispanic or Latino (all races) | 53.2% (115) | 54.0% (47) | 53.5% (162) |
| White | 9.7% (21) | 12.6% (11) | 10.5% (32) |
| Unreported or refused to report | 0.5% (1) | 1.2% (1) | 0.7% (2) |
| Education | |||
| No formal education | 4.2% (9) | 4.2% (9) | 4.0% (12) |
| Primary school | 26.9% (58) | 27.0% (58) | 27.0% (82) |
| High school | 42.6% (92) | 42.5% (92) | 40.6% (123) |
| College+ | 24.5% (53) | 24.5% (53) | 26.4% (80) |
| No answer | 1.8% (4) | 1.8% (4) | 2.0% (6) |
Most participants who had not yet received the vaccine were 18 to 34 years of age (40.3%, n = 87) or 35 to 49 years of age (25.2%, n = 76). Most participants who had already received the vaccine were 50 to 64 years of age (34.5%, n = 30) or 65 years of age or older (25.3%, n = 22). Female participants made up 71.8% (n = 155) of the not yet vaccinated group and 57.5% (n = 50) of the vaccinated group.
Participants who had not yet been vaccinated were asked in an open-ended question to share their concerns prior to being asked the specific closed-ended topic questions. The most common theme mentioned in this open-ended question, across all language groups, was side effects. Other topics mentioned by participants in all language groups were wanting to speak with a doctor first, chronic medical conditions, wanting to wait, conflicting information in the news, and general fear. Concern about vaccine ingredients was only mentioned by English speaking participants. CV Creole/Portuguese speaking participants more frequently expressed concern about the vaccine causing health problems than English or Spanish speaking participants.
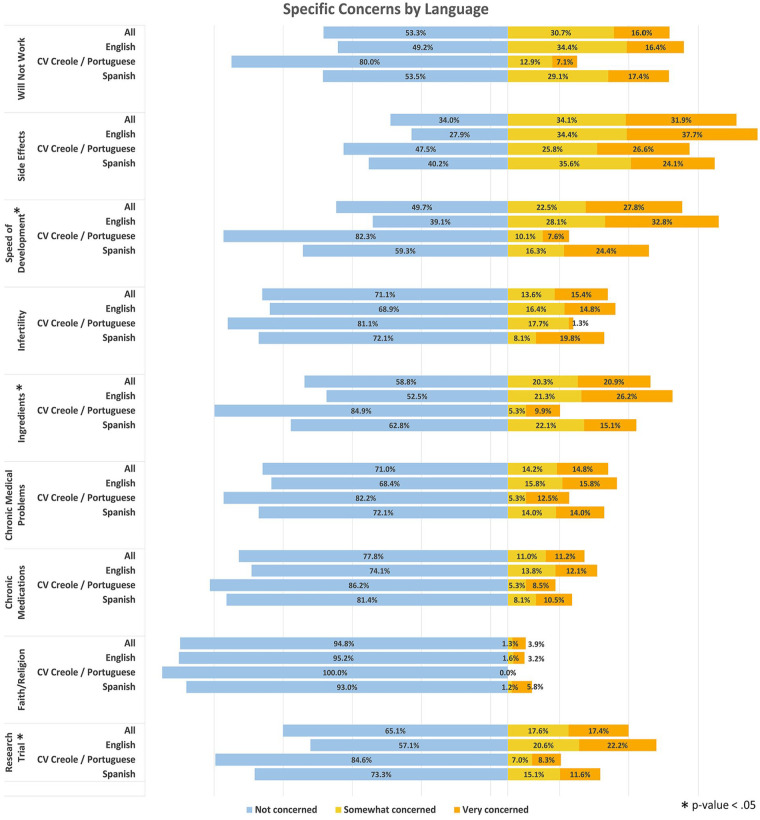
The Figure 1 shows the estimated percentages of the population not concerned, somewhat concerned, or very concerned about each of the 9 specific topics covered in the closed-ended questions of the survey. Side effects had the largest percentage of concern across all languages with 34% and 32% of people being somewhat and very concerned, respectively. Concern due to faith or religion had the lowest percentage of concern with 1.3% and 3.9% of people being somewhat and very concerned, respectively. The percentages of concern for 3 of the 9 topics—ingredients, speed of development, and research trial—were significantly different across language groups. English speakers had greater concern than CV Creole/Portuguese speakers across all topics and this was statistically significant for all topics. English speakers had greater concern than Spanish speakers across all topics except faith or religion, although this was only statistically significant for speed of vaccine development.
Figure 1.
Response to 9 COVID-19 vaccine concern questions (weighted), by language.a
aSee Appendix for full wording of survey questions.
*Chi2 P value <.05.
Participants who had already received the COVID-19 vaccine were asked in an open-ended question why they chose to get the vaccine. The most frequently cited reason among English speaking participants was to protect themselves, whereas the most frequently cited reason among Spanish speaking participants was to protect others. CV Creole/Portuguese speaking participants mentioned both protection of themselves and others. Availability of the vaccine and employment in health care were reasons mentioned by participants in all languages. Additionally, some Spanish- and English-speaking participants discussed return to normalcy, trust in their doctor, and chronic medical conditions as other reasons for having been vaccinated.
Among those not yet vaccinated, 62% requested to be put on a list to get a COVID-19 vaccine, which we used as an indicator of acceptability of the vaccine. By language, 56% of English speakers, 71% of Spanish speakers, and 61% of CV Creole/Portuguese speakers indicated acceptability of the vaccine (Table 2).
Table 2.
Demographics Associated With COVID-19 Vaccine Acceptability Among Those Not Yet Vaccinated, Weighted Population Estimates and Unadjusted and Adjusted Odds Ratios (n = 216), Weighted.
| On list to get vaccinated | Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|---|
| % (n) | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Language | |||||||
| English | 55.6% (35) | 1.00 (ref) | 1.00 (ref) | ||||
| CV Creole/Portuguese | 61.4% (40) | 1.27 | 0.62-2.60 | .507 | 1.34 | 0.55-3.27 | .512 |
| Spanish | 71.4% (60) | 2.00 | 1.00-4.00 | .050 | 2.21 | 0.98-4.97 | .055 |
| Age | |||||||
| 18-34 | 53.8% (47) | 1.00 (ref) | 1.00 (ref) | ||||
| 35-49 | 62.7% (46) | 1.45 | 0.69-3.05 | .331 | 1.30 | 0.57-2.96 | .527 |
| 50-64 | 80.4% (37) | 3.52 | 1.23-10.10 | .020 | 2.63 | 0.89-7.76 | .080 |
| 65+ | 47.0% (5) | 0.76 | 0.10-5.91 | .794 | 0.69 | 0.08-5.74 | .727 |
| Gender | |||||||
| Female | 56.7% (91) | 1.00 (ref) | 1.00 (ref) | ||||
| Male | 74.4% (44) | 2.22 | 1.00-4.91 | .050 | 2.21 | 0.96-5.08 | .062 |
| Education | |||||||
| No formal education | 58.2% (6) | 1.00 (ref) | 1.00 (ref) | ||||
| Primary school | 63.3% (40) | 1.24 | 0.26-6.00 | .789 | 1.36 | 0.27-6.73 | .705 |
| High school | 63.5% (56) | 1.25 | 0.27-5.70 | .776 | 2.09 | 0.43-10.21 | .359 |
| College+ | 59.6% (32) | 1.06 | 0.22-5.04 | .945 | 1.97 | 0.35-10.95 | .439 |
In unadjusted logistic regression models, Spanish speakers had 2.00 (95% CI: 1.00-4.00) times greater odds of accepting the COVID-19 vaccine compared to English speakers. Participants aged 50 to 64 had 3.52 (95% CI: 1.23-10.10) times the odds of accepting the vaccine compared to participants aged 18 to 24. Male participants had 2.22 (95% CI: 1.00-4.91) times the odds of accepting the COVID-19 vaccine compared to females. In our multivariate adjusted model, we saw similar odds ratios, although there were no statistically significant associations (Table 2).
Discussion
Our study provides insights into the concerns about and acceptability of the COVID-19 vaccine within a diverse, marginalized population in Rhode Island heavily impacted by the pandemic. We achieved a response rate (58%) comparable to other COVID-19 vaccine studies of similar size, and higher than many non-COVID-19 related surveys.31 -35 Key leaders from several community groups and individuals along the healthcare spectrum were instrumental in the design and distribution of the survey, which promoted outreach and enabled a robust response. Conducting the survey via telephone allowed for increased representation from the clinic communities where access to additional technology remains limited and literacy rates vary, as demonstrated by 4% of survey participants reporting no formal education.
This study is strengthened by the mixed data collection design, including open-ended and closed-ended questions. The qualitative data support the quantitative data findings obtained with the 9 closed-ended questions on specific concerns. Beyond this, they add additional concerns not captured in the closed-ended questions and insights into the perceptions on acceptability of those who had received the vaccine.
The predominant concern reported by respondents of all languages was vaccine side effects. This parallels similar studies that also note side effects as a common concern about the COVID-19 vaccine.13,36,37 This is an unsurprising finding given the higher rate of short-term side effects, including pain at injection site and fever, compared to the side effects from other vaccines.38,39 It is unclear if these short-term side effects were the concerns being referred to by our survey participants, as opposed to more serious or long-term side effects. Infertility was less of a concern than expected given the false news stories surrounding this topic, however we do not know the extent to which participants were concerned about other unsubstantiated vaccine side effects. 40
Generally, English speakers were most likely to express concerns about the COVID-19 vaccine and CV Creole/Portuguese speakers were least likely to express concerns. In addition, Spanish and CV Creole speakers were more likely to accept the vaccine compared to English speakers. These findings are particularly interesting given that earlier in the pandemic there was concern that marginalized groups would be more resistant to getting the vaccine.36,41
This study was specifically conducted to inform a vaccine campaign for the BVCHC clinic population. Our results suggest that different communities may benefit from different messaging. For English and Spanish speakers, the second most common concern was speed of development. For CV Creole/Portuguese speakers, the second most common concern was that the vaccine will not work. Tailoring educational messages could allow for more comprehensive and intentional strategies to improve vaccine acceptability.
Our study suggests that concerns about the vaccine are not necessarily an indication for vaccine refusal. Participants who expressed concerns also expressed their acceptability of the vaccine through their desire to be put on a list for future vaccination when available.
Some participants cited having trust in their doctor and having the vaccine available at their clinic as reasons for receiving the vaccine. This highlights the importance of provider-patient relationships and the trust that patients in this community put in their primary care providers to provide appropriate information and act in their best interests. This is an important strategy that can be utilized to help continue to promote vaccine uptake and instill further vaccine confidence. For those who are anxious or resistant, the primary care clinician is an effective source of reliable and trustworthy information.42 -46 Patients have better outcomes receiving medical care in their local community, and from clinicians who are culturally sensitive to their lived experiences. 42
While our study focused on concerns and acceptability of the vaccine, achieving high vaccination rates will also require that everyone has access to the vaccine. In our study, availability of the vaccine at BVCHC was named as a reason participants chose to get vaccinated. In addition, non-English-speaking participants reported fewer concerns and more willingness to receive the vaccine than did English speakers. This suggests that access to the vaccine, rather than lack of confidence, may be more important for getting vulnerable populations vaccinated.47 -52 Providing individuals access to the vaccine in a trusted space within their own communities will likely also increase demand. However, as with vaccine hesitancy, more research is needed to understand barriers to access in marginalized communities, and how access differs by sub-populations, which is likely to be highly context specific.
There were several limitations to our study. Individuals without telephones or with incorrectly listed phone numbers, and those unable to answer the phone during mostly daytime hours, would have been missed in our survey, possibly introducing selection bias. Additionally, response rates were different by language group, with English speakers less likely to respond. Our study did not take into account participant vaccine eligibility due to the fact that the study was conducted during a time period when vaccine eligibility and availability was rapidly evolving. Thus, direct comparison of those who were vaccinated and those who were not yet vaccinated at the time of our survey would be inappropriate. The concerns and perceptions of the community were also likely evolving, which could have created a variation of survey answers over the course of the 6-week survey period. Participants were not specifically asked about their personal medical history, which may have been an important factor in their responses regarding 2 of the specific concerns—chronic medical conditions and medications. We also recognize that our study was conducted with patients who are engaged in their medical care at a local community clinic, which limits the generalizability of this study. Individuals engaged in their medical care may not represent the views of those who are not established at a health center. Community residents who do not receive care from this health center or who are not patients of any primary care practice may hold different perspectives.
Although participants were asked about their concerns and reasons for being vaccinated, interviewers did not probe further for elaboration on these responses. There was variation in the richness of the qualitative data, likely due to the use of multiple interviewers and multiple survey languages. The immediacy of the pandemic and need for data to inform a vaccine campaign quickly were factors in survey development. It might otherwise have been useful to explore what participants meant by side effects and if their general sense of fear could be further delineated. Future studies should investigate the reasons why individuals ultimately choose to get the vaccine after lacking confidence initially; in other words, what changes people’s minds. This information is important to consider given the need for a COVID-19 vaccine booster, and may be applied more broadly to increase acceptability of other routine vaccines.
Conclusions
Our study provides insights into the concerns and acceptability of the COVID vaccine among a marginalized population in Rhode Island. As the world continues to mitigate the effects of the COVID-19 pandemic and prepare for future pandemics, it is imperative that these strategies are based on evidence, including evidence of people’s concerns, acceptability, and access to the vaccine. While differences in beliefs and perceptions by language group may be small, understanding these differences will nonetheless be the key to creating effective messaging within communities in the latter stages of the COVID-19 pandemic, and achieving sufficiently high vaccination rates. Non-English-speaking populations may be as willing or more willing to receive the vaccine, but may simultaneously face greater barriers to access. Greater understanding of community-specific disparities and needs will empower public health, primary care providers, and policy makers to craft tailored, community-contextual approaches to boost vaccination rates and increase access to health care for marginalized US populations.
Acknowledgments
We would like to acknowledge the following people for their meaningful contributions toward all aspects of this project: Scott Hewitt, Gloria Cardenas, Francisco Moret, Julissa Espejo, Doroteia Andrade, Carissa Damoura, Elsie Hernandez, Anne Saint Pierre, and Stephanie Aldana who helped to conduct the survey interviews. The staff and leadership at Blackstone Valley Community Health Care for their guidance and support during this project. Lastly and most importantly, we would like to thank the communities of patients at Blackstone Valley Community Health Care.
Appendix
Blackstone Valley Community Health Care Center COVID-19 Vaccine Survey
Have you received the COVID-19 vaccine?
Yes →
No
Not sure
→ If yes will prompt to
Why did you choose to get the vaccine?____________
→ Will then skip to demographic questions
Would you get the COVID-19 vaccine if it was offered to you?
Yes
No
Not sure
No answer
Are you concerned about the COVID-19 vaccine?
Not Concerned
Somewhat concerned→
Very concerned→
No answer
→ If very concerned or somewhat concerned will prompt to
Can you tell me about some of those concerns? _____
Are you concerned that the vaccine will not work?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned about side effects from the vaccine?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned about how fast the vaccine came out?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned that the vaccine causes infertility?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned about the ingredients in the vaccine?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned to get the vaccine because of your chronic medical problems?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned to get the vaccine because you are on medications?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned to get the vaccine because of your faith or religion?
Not Concerned
Somewhat concerned
Very concerned
No answer
Are you concerned to get the vaccine because it sounds like you will be part of a research trial?
Not Concerned
Somewhat concerned
Very concerned
No answer
What level of education have you completed?
No formal education
Some primary school
Completed primary school (8th grade)
Some high school
Graduated high school
Some college or technical school
Graduated college or technical school
Professional degree
No answer
What is your ethnicity (example country of origin or family country of origin)? ___________________
What is your gender?
Man
Woman
Trans man
Trans woman
Non-binary/gender nonconforming
No answer
Would you like to be put on a list to get the COVID vaccine from BVCHC? You will be called when it will be your turn.
Yes
No
No answer
Table A1.
Row Percentages Characteristics of Survey Participants by COVID-19 Vaccination Status, Unweighted.
| Not yet vaccinated* % (n) | Already vaccinated % (n) | |
|---|---|---|
| All | 71.3% (216) | 28.7% (87) |
| Language | ||
| English | 65.7% (65) | 34.3% (34) |
| CV Creole/Portuguese | 80.8% (63) | 19.2% (15) |
| Spanish | 69.8% (88) | 30.2% (38) |
| Age | ||
| 18-34 | 85.3% (87) | 14.7% (15) |
| 35-49 | 79.2% (76) | 20.8% (20) |
| 50-64 | 60.0% (45) | 40.0% (30) |
| 65+ | 26.7% (8) | 73.3% (22) |
| Gender | ||
| Male | 62.2% (61) | 37.7% (37) |
| Female | 75.6% (155) | 24.4% (50) |
| Race and ethnicity | ||
| American Indian or Alaska Native | 100.0% (1) | 0.0% (0) |
| Black or African American | 73.6% (78) | 26.4% (28) |
| Hispanic or Latino (all races) | 71.0% (155) | 29.0% (47) |
| White | 65.6% (21) | 34.4% (11) |
| Unreported or refused to report | 50.0% (1) | 50.0% (1) |
| Education | ||
| No formal education | 75.0% (9) | 25.0% (3) |
| Primary School | 70.7% (58) | 29.3% (24) |
| High School | 74.8% (92) | 25.2% (31) |
| College+ | 66.3% (53) | 33.7% (27) |
| No answer | 66.7% (4) | 33.3% (2) |
May not have been eligible for vaccination at time of survey.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Molly Bloom  https://orcid.org/0000-0002-2560-7859
https://orcid.org/0000-0002-2560-7859
References
- 1. The COVID Tracking Project. Analysis & updates | The state of COVID-19 race and ethnicity data. Accessed October 17, 2021. https://covidtracking.com/analysis-updates/state-of-COVID-race-and-ethnicity-data
- 2. WHO. United States of America: WHO Coronavirus disease (COVID-19) dashboard with vaccination data. Accessed October 17, 2021. https://covid19.who.int/region/amro/country/us
- 3. Abedi V, Olulana O, Avula V, et al. Racial, economic, and health inequality and COVID-19 infection in the United States. J Racial Ethn Health Disparities. 2021;8(3):732-742. doi: 10.1007/s40615-020-00833-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. APM Research Lab. Color of coronavirus: COVID-19 deaths analyzed by race and ethnicity. Accessed October 17, 2021. https://www.apmresearchlab.org/covid/deaths-by-race
- 5. Carethers JM. Insights into disparities observed with COVID-19. J Intern Med. 2021;289(4):463-473. doi: 10.1111/joim.13199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yehia BR, Winegar A, Fogel R, et al. Association of race with mortality among patients hospitalized with coronavirus disease 2019 (COVID-19) at 92 US hospitals. JAMA Netw Open. 2020;3(8):e2018039. doi: 10.1001/jamanetworkopen.2020.18039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. CDC. COVID data tracker. Accessed October 17, 2021. https://covid.cdc.gov/covid-data-tracker/#vaccinations
- 8. Willis DE, Andersen JA, Bryant-Moore K, et al. COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin Transl Sci. Published online July 2, 2021. doi: 10.1111/CTS.13077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. 2021;9:16. doi: 10.3390/VACCINES9010016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kreps S, Prasad S, Brownstein JS, et al. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020;3(10):e2025594. doi: 10.1001/jamanetworkopen.2020.25594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Garcia P, Montez-Rath ME, Moore H, et al. SARS-CoV-2 vaccine acceptability in patients on hemodialysis: a nationwide survey. J Am Soc Nephrol. 2021;32(7):1575-1581. doi: 10.1681/ASN.2021010104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sutton D, D’Alton M, Zhang Y, et al. COVID-19 vaccine acceptance among pregnant, breastfeeding, and nonpregnant reproductive-aged women. Am J Obstet Gynecol MFM. 2021;3(5):100403. doi: 10.1016/j.ajogmf.2021.100403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pew Research Center. Growing share of Americans say they plan to get a COVID-19 vaccine – or already have. Accessed June 17, 2021. https://www.pewresearch.org/science/2021/03/05/growing-share-of-americans-say-they-plan-to-get-a-covid-19-vaccine-or-already-have/
- 14. Larson HJ, Jarrett C, Schulz WS, et al. Measuring vaccine hesitancy: the development of a survey tool. Vaccine. 2015;33(34):4165-4175. doi: 10.1016/j.vaccine.2015.04.037 [DOI] [PubMed] [Google Scholar]
- 15. Amin AB, Bednarczyk RA, Ray CE, et al. Association of moral values with vaccine hesitancy. Nat Hum Behav. 2017;1(12):873-880. doi: 10.1038/s41562-017-0256-5 [DOI] [PubMed] [Google Scholar]
- 16. Opel DJ, Taylor JA, Mangione-Smith R, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29:6598-6605. doi: 10.1016/j.vaccine.2011.06.115 [DOI] [PubMed] [Google Scholar]
- 17. Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500-6507. doi: 10.1016/j.vaccine.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rhode Island Department of Health. Rhode Island COVID-19 Towns and Cities Data. Accessed June 18, 2021. https://ridoh-covid-19-response-city-town-data-rihealth.hub.arcgis.com/
- 20. Rhode Island Department of Health. COVID-19 vaccination update. Published 2021. Accessed October 3, 2021. https://us2.campaign-archive.com/?u=ece9b1661b3bf3b864a6894d1&id=4cdf8b6e42
- 21. Raynor EM. Factors affecting care in non-English-speaking patients and families. Clin Pediatr. 2016;55:145-149. doi: 10.1177/0009922815586052 [DOI] [PubMed] [Google Scholar]
- 22. Lau M, Lin H, Flores G. Racial/ethnic disparities in health and health care among U.S. adolescents. Health Serv Res. 2012;47(5):2031-2059. doi: 10.1111/j.1475-6773.2012.01394.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Blackstone Valley Community Health Care – Our History, Mission, Vision. Who we are. Accessed September 22, 2021. https://www.bvchc.org/about-us/who-we-are
- 24. U.S. Census Bureau. QuickFacts: Central Falls city, Rhode Island. Accessed September 22, 2021. https://www.census.gov/quickfacts/centralfallscityrhodeisland
- 25. Lazarus JV, Ratzan SC, Palayew A, et al. Author correction: a global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:354. doi: 10.1038/s41591-020-01226-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46:270-277. doi: 10.1007/s10900-020-00958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13(12):e0208601. doi: 10.1371/journal.pone.0208601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Qualtrics software. Version XM of Qualtrics. Qualtrics; 2021. [Google Scholar]
- 29. StataCorp. Stata Statistical Software: Release 15. StataCorp LLC; 2017. [Google Scholar]
- 30. Borkan J. Immersion/crystallization. In: Crabtree B, Miller W, eds. Doing Qualitative Research, 2nd ed. SAGE Publications Inc; 1999: 179-194. [Google Scholar]
- 31. Levy AT, Singh S, Riley LE, Prabhu M. Acceptance of COVID-19 vaccination in pregnancy: a survey study. Am J Obstet Gynecol MFM. 2021;3:100399. doi: 10.1016/j.ajogmf.2021.100399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Silva J, Bratberg J, Lemay V. COVID-19 and influenza vaccine hesitancy among college students. J Am Pharm Assoc. Published online May 21, 2021. doi: 10.1016/j.japh.2021.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Li PC, Theis SR, Kelly D, et al. Impact of an education intervention on COVID-19 vaccine hesitancy in a military base population. Mil Med. Published online June 12, 2021. doi: 10.1093/milmed/usab230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hendra R, Hill A. Rethinking response rates: new evidence of little relationship between survey response rates and nonresponse bias. Eval Rev. 2019;43(5):307-330. doi: 10.1177/0193841X18807719 [DOI] [PubMed] [Google Scholar]
- 35. Fan W, Yan Z. Factors affecting response rates of the web survey: a systematic review. Comput Human Behav. 2010;26(2):132-139. doi: 10.1016/j.chb.2009.10.015 [DOI] [Google Scholar]
- 36. Nguyen KH, Srivastav A, Razzaghi H, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(6):217-222. doi: 10.15585/MMWR.MM7006E3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775-779. doi: 10.1007/s10654-020-00671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Johns Hopkins Bloomberg School of Public Health. Side effects and COVID-19 vaccines: what to expect – COVID-19. Accessed July 12, 2021. https://www.jhsph.edu/covid-19/articles/side-effects-and-covid-19-vaccines-what-to-expect.html
- 39. Samaritan Health Services. COVID vaccine side effects compared to flu & shingles shots. Accessed July 12, 2021. https://www.samhealth.org/about-samaritan/news-search/2021/02/09/covid-19-vaccine-side-effects-compared-to-other-vaccines
- 40. Sajjadi NB, Nowlin W, Nowlin R, et al. United States internet searches for “infertility” following COVID-19 vaccine misinformation. J Osteopath Med. 2021;121(6):583-587. doi: 10.1515/jom-2021-0059 [DOI] [PubMed] [Google Scholar]
- 41. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. Adults. Ann Intern Med. 2020;173(12):964-973. doi: 10.7326/M20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Katzman JG, Katzman JW. Primary care clinicians as COVID-19 vaccine ambassadors. J Prim Care Community Health. 2021;12:21501327211007026. doi: 10.1177/21501327211007026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. CDC. Expanding COVID-19 vaccine distribution to primary care providers to address disparities in immunization. 2021. Accessed October 3, 2021. https://www.cdc.gov/vaccines/covid-19/downloads/Guide-for-Jurisdictions-on-PCP-COVID-19-Vaccination.pdf
- 44. Gonzales A, Lee EC, Grigorescu V, Smith SR, De Lew N, Sommers BD. Overview of barriers and facilitators in COVID-19 vaccine outreach. U. S. Department of Health and Human Services; 2021. Research Report No. HP-2021-19. [Google Scholar]
- 45. Rust G, Melbourne M, Truman BI, Daniels E, Fry-Johnson Y, Curtin T. Role of the primary care safety net in pandemic influenza. Am J Public Health. 2009;99 Suppl 2:S316-S323. doi: 10.2105/AJPH.2009.161125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ratzan S, Schneider EC, Hatch H, Cacchione J. Missing the point – how primary care can overcome covid-19 vaccine “Hesitancy”. N Engl J Med. 2021;384(25):e100. doi: 10.1056/NEJMp2106137 [DOI] [PubMed] [Google Scholar]
- 47. Fisk RJ. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: experience from the United States. Glob Health J. 2021;5(1):51-55. doi: 10.1016/J.GLOHJ.2021.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Martin EG, Birkhead GS, Holtgrave DR. Maintaining a focus on health equity during the COVID-19 vaccine rollout. J Public Health Manag Pract. 2021;27(3):226-228. doi: 10.1097/PHH.0000000000001359 [DOI] [PubMed] [Google Scholar]
- 49. Kirksey L, Milam AJ, Curry CW, Sorour AA. Vaccine hesitance and vaccine access in minority communities. Cleve Clin J Med. Published online May 9, 2021. doi: 10.3949/ccjm.88a.ccc079 [DOI] [PubMed] [Google Scholar]
- 50. Hughes MM, Wang A, Grossman MK, et al. County-level COVID-19 vaccination coverage and social vulnerability-United States, December 14, 2020-March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):431-436. doi: 10.15585/mmwr.mm7012e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hooper M, Nápoles AM, Pérez-Stable EJ. No populations left behind: vaccine hesitancy and equitable diffusion of effective COVID-19 vaccines. J Gen Intern Med. 2021;36:2130-2133. doi: 10.1007/s11606-021-06698-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Alismail S, Chipidza W. Accessibility evaluation of COVID-19 vaccine registration websites across the United States. J Am Med Inform Assoc. 2021;28:1990-1995. doi: 10.1093/JAMIA/OCAB105 [DOI] [PMC free article] [PubMed] [Google Scholar]