Abstract
We aimed at examining the impact of wearing surgical face masks on exercise performance. Thirty‐two healthy adults (16 males and 16 females) completed a graded exercise test to measure peak oxygen uptake (VO2peak) and the ventilatory threshold (VT). Then, on separate days, all participants performed resting and standardized protocols (moderate intensity: 25% infra‐VT; severe intensity: 25% supra‐VT) on two different conditions (with and without a surgical mask). The use of masks reduced both VO2 and minute ventilation during moderate and severe exercise (p < 0.0001), and this effect was particularly pronounced during severe exercise. Time to exhaustion was also shortened by ~10% on the face mask condition (p = 0.014). In contrast, neither heart rate nor the respiratory exchange ratio was affected by masking. The submaximal VO2 was similar between the two epochs of analysis obtained during moderate cycling (i.e. 3–6 min vs. 7–10 min) and this occurred similarly between conditions. In conclusion, the impact of the surgical masks on exercise capacity is particularly pronounced during severe exercise performed at constant work rate. Ultimately, this may implicate a considerable impairment of structured or even unstructured strenuous physical activity. Clinical Trials registration number: NCT04963049.
Keywords: capacity, exercise, fatigue, oxygen uptake, ventilation
1. INTRODUCTION
The pandemic crisis caused by the coronavirus disease 2019 (COVID‐19) has had profound implications for humanity. This new coronavirus, better known as severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), was first identified in December 2019 in the city of Wuhan—China (Sun et al., 2020). There are three known factors related to proximity that potentiate the probability of SARS‐CoV‐2 horizontal transmission: (1) close contact, (2) duration the exposure, and (3) confinement of the interaction space (Leung, 2021). Although each factor has the individual capacity to inflate the risk of infection, their co‐occurrence further exacerbates the number of positive transmissions (Leung, 2021). For this reason, the current recommendations related to the prevention against the spread of COVID‐19 include wearing face masks (Centers for Disease Control & Prevention, 2020; World Health Organization, 2020). Based on the premise that the use of masks during exertion may attenuate the risk of transmission between practitioners, several nations extended its compulsory wearing to exercise conditions (mostly during the escalation of the pandemic crisis). Despite the discomfort caused by the prolonged use of masks has been well documented in the available literature (Scarano et al., 2020), it is generally believed that its use does not affect general motor performance or the ability to function in everyday tasks (Person et al., 2018; Samannan et al., 2021; Shenal et al., 2012). Yet, whether this is sustained during motor tasks performed at high levels of intensity (sports and exercise) remains largely controversial. There is partial evidence that exercising with a face mask lowers the threshold for dyspnoea in persons with poor exercise capacity and that this may be caused by rebreathing of carbon dioxide (CO2) trapped in the face mask at each exhalation (Banzett et al., 1990; Chen et al., 2016; Person et al., 2018). Therefore, the World Health Organization advises that people should not wear masks during vigorous exercise because they may reduce the ability to breathe comfortably (Bull et al., 2020; WHO, 2020).
From a physiological standpoint, there is no evidence of negative repercussions resulting from wearing a mask during vigorous exercise in healthy individuals (Hopkins et al., 2021). However, it was recently observed that heart rate as well as perceived exertion both increase during walking with a face mask (Wong et al., 2020). Unfortunately, the authors did not explore changes in exercise performance (e.g. time to exhaustion or time trial). In other studies, it was reported that wearing face masks reduces the level of work output and ventilation achieved in response to graded exercise testing (GXT), both in untrained and trained males (Egger et al., 2021; Fikenzer et al., 2020). Masks were also shown to increase airway resistance, reduce VO2 and heighten the chronotropic response to constant cycling performed at work rates equivalent to maximal lactate steady state (Lassing et al., 2020). However, the negative impact of wearing a face mask during vigorous exercise is not a universal finding (Epstein et al., 2021; Shaw et al., 2020). In addition, a recent meta‐analysis showed that face masks can be worn during exercise with no influences on performance and minimal impact on physiological variables (Shaw et al., 2021). However, there is limited transferability of these conclusions to healthy young individuals because both healthy and clinical participants (of any age) were eligible for this study. Finally, it is currently unknown whether the effects of wearing a face mask on exercise capacity are more pronounced during constant severe vs. moderate exercise. This is relevant because training across disparate workloads (spanning different intensity domains) affects both the acute and chronic adaptations to exercise (Black et al., 2017; Esteve‐Lanao et al., 2007). Thus, we sought to explore whether wearing a surgical mask impacts performance in response to exercise performed below vs. above the ventilatory threshold (VT). It was hypothesized that while wearing a surgical mask may be particularly provocative during severe exercise (affecting the ventilatory compensation), this may not be the case during moderate exercise.
2. METHODS
2.1. Participants
Thirty‐two healthy and active volunteers (16 males and 16 females; age: 24.0 ± 3.3 years; height: 168.9 ± 7.9 cm; body mass: 67.6 ± 10.2 kg and body mass index: 23.5 ± 2.0 kg/m2), without medications and with normal blood pressure (all ≤120/80 mmHg) (Whelton et al., 2018), were included in this study. Exclusionary criteria involved active smoking status, known metabolic disease, cardiovascular disease, respiratory disorders including asthma and any orthopaedic issues that would limit exercise performance. Participants were recruited from the local communities and from the Faculty surroundings via word‐of‐mouth. Verbal information about the risks, requirements and procedures of the study was provided, and written informed consent was obtained from all participants prior to study entry, which was in accordance with the Declaration of Helsinki and approved by the Faculty ethics committee (CEFMH No 23/2021). This study is registered with ClinicalTrials.gov (registration number: NCT04963049, date of registration 15 July 2021).
2.2. Study design
This study followed a randomized crossover design. Testing was carried out during the afternoon period (between 13.00 and 16.00 h), in a laboratory with an environmental temperature between 22 and 24°C and a relative humidity between 44 and 56%. All participants were requested to avoid any form of exercise for at least 24 h before testing and to have nothing to drink or eat for at least 3 h pre‐testing. Each participant was tested on three non‐consecutive days. On the first visit, body mass measurements were obtained, to the nearest 0.01 kg, on a digital scale (BG 42; Breuer GmbH) with the participants wearing light‐weight clothes and no shoes. Measurements of standing height were taken to the nearest 0.5 cm using a stadiometer. Body mass index was calculated by dividing the participants’ mass in kilograms by the square of their height in metres. Then, participants performed a GXT on a cycle ergometer (Monark, Ergomedic 839E) to measure peak oxygen uptake (VO2peak) and to enable the individualization of subsequent exercise trials based on the VT of each participant. On the subsequent visits, all participants performed resting and standardized cycle ergometer submaximal protocols on two different conditions (with and without a surgical mask type II [Zhejiang Hongyu Medical Commodity Co., Ltd]), within a 1‐week period. The order of conditions was presented in a randomized (computer‐generated algorithm), counterbalanced manner. As depicted in Figure 1, participants exercised either with (experimental) or without (control) a surgical mask at constant intensity below and above the VT (25% infra‐ and 25% supra‐VT, respectively). Exercise intensity was normalized to VT to discriminate the effects of masking on moderate and severe exercise (Whipp & Wasserman, 1972). It is important to note that past research has shown that wearing a surgical mask has no impact on the individual VT (Egger et al., 2021). Therefore, the VT was selected for setting a predetermined exercise intensity, either with or without masking. Additionally, the O2 pulse, which can be used as a surrogate marker of stroke volume, was calculated as the ratio between VO2 and heart rate obtained during submaximal and maximal exercise (Crisafulli et al., 2007). Expired gas measurements were taken using a portable mixing chamber (MetaMax® I; Cortex), which was calibrated before each test with a known volume and a known gas concentration. Heart rate was measured during the last 3 min of rest and during exercise (Polar RS 800 G3 RR recorder; Polar Electro). Blood pressure was also taken at resting conditions (Tango SunTech Medical Morrisville).
Figure 1.
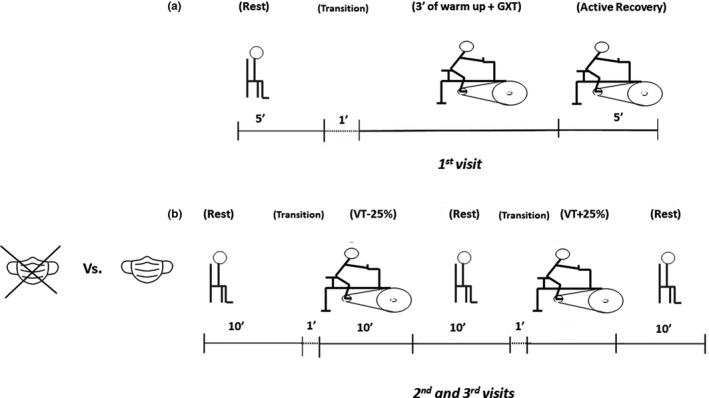
Schematic representation of the study protocol. The experimental design consisted of three visits to the laboratory. (a) On the first visit, the participants performed 5‐min of seated rest. Then, 1 min was allowed for transition from the chair to the cycle ergometer. A 3‐min warm‐up period at 60 W was then respected. Subsequently, without any interruption from warm‐up, the work rate was increased by 15 W min−1 until the participant was unable to continue (graded exercise testing—GXT). (b) On the second and third visits (without vs. with mask on a randomized fashion), each participant rested quietly in a seated position for 10 min. Subsequently, 1 min was allowed for transition from the chair to the cycle ergometer. Then, the participants performed 10 min of moderate cycling at ventilatory threshold (VT) work rate −25%. Then, after 10 min of passive recovery, each participant exercised at an intensity above the VT (25% supra‐VT) until volitional exhaustion. Oxygen uptake and heart rate were continuously monitored during all visits
2.3. Graded exercise test
Cardiorespiratory exercise data were obtained using an incremental cycle ergometer ramp protocol. Following a 3‐min warm‐up period at 60 W (initial work rate), the work rate was increased by 15 W min−1 until the participant was unable to continue. The participants cycled at a self‐selected pedal rate (60–90 rev min−1) and the saddle as well as handlebar height configuration were recorded and reproduced in all subsequent visits to the laboratory. The VO2 and heart rate data, measured throughout the incremental test, were displayed as 30‐s averages. The highest VO2 attained at the end of the test was taken as VO2peak if a plateau in the VO2 with an increase in exercise work rate was observed, or in accordance with the British Association of Sports and Exercise Science criteria (Bird & Davidson, 1997). Peak heart rate was identified as the highest value recorded during each test. For each participant, the VT was determined from the time course of the relationship between Ve/VO2 and Ve/VCO2 by two independent investigators. Accordingly, the VT was defined as the minimal work rate at which the Ve/VO2 exhibited a systematic increase without a concomitant increase in Ve/VCO2 (Wasserman et al., 1973). The VT was expressed both in terms of absolute (W) and relative intensities (%VO2peak).
2.4. Constant intensity exercise tests
To ensure that all participants exercised at the same intensities relative to VT, cycling work rates were individualized (moderate exercise: VT work rate—25%; severe exercise: VT work rate +25%). As depicted in Figure 1B, before exercising, each participant rested quietly in a seated position for 10 min. The mean of the last 3 min of the 10‐min baseline period was defined as the participants’ resting VO2. Subsequently, participants performed 10 min of moderate cycling at VT work rate −25%. Mean values of cardiorespiratory data obtained during moderate exercise were calculated using 3‐min epochs: (1) 3rd to 6th min and (2) 7th to 10th min. This was done to determine whether wearing a surgical mask affected the attainment of steady state during constant moderate exercise. In addition, the increment in the values of the cardiorespiratory variables obtained between the 7th and 10th min (ΔVO2 [10‐7]) was also determined to confirm steady‐state attainment in both conditions during the last minutes of moderate exercise. Then, after 10 min of passive recovery, each participant exercised at an intensity above the VT (25% supra‐VT) until volitional exhaustion (when the 60–90 rev min−1 pedalling rate could not be maintained by >10 s). Mean values of cardiorespiratory data obtained during severe exercise were displayed as 30‐s averages and the highest VO2 was taken. Peak heart rate was identified as the highest value recorded during each test.
2.5. Statistical analyses
Standard descriptive statistics (mean and standard deviation) were computed to summarize the data. All data were tested for normality using Shapiro–Wilk test. An independent researcher in our laboratory, who was blinded to treatment allocation, performed statistical analyses. Based on previous research, if heart rate during peak exercise corresponds to 187 ± 8.3 and 183 ± 9.2 bpm with and without the use of a face mask, respectively (Fikenzer et al., 2020), a sample size of 32 participants was estimated to achieve more than 80% power of correctly rejecting the null hypothesis. Paired t tests were used to explore differences on time to exhaustion between conditions (in response to supra‐VT exercise). A two‐way ANOVA [condition (without vs. with face mask) by time (rest vs. VT work rate −25% vs. VT work rate +25%)] with repeated measures was conducted on all dependent variables to determine the effects of wearing a surgical mask on the physiological response to sustained exercise performed below and above the VT. When a significant effect was detected at p < 0.05, follow‐up t tests were used for post hoc comparisons. Adjustment for multiple comparisons was made with Bonferroni's correction (significance was set at p < 0.01). Attainment of steady‐state VO2 during exercise was confirmed by exploring if ΔVO2 [10‐7], in each condition, differed significantly from zero. Statistical significance was set at p < 0.05 (except for multiple comparisons). Data analysis was carried out using Statistical Package for the Social Sciences (version 25.0, SPSS Inc.).
3. RESULTS
Table 1 shows the cardiorespiratory, metabolic and mechanic parameters obtained during GXT with no mask. Comparisons of select data between conditions (without vs. with mask) at different time points (rest vs. moderate vs. severe exercise) are depicted in Figure 2. We obtained a significant condition‐by‐time interaction for VO2 (F = 33.6, p < 0.0001) and minute ventilation (F = 42.7, p < 0.0001). Post hoc analyses showed that wearing a surgical mask at resting conditions did not affect VO2 or minute ventilation (p > 0.01). In contrast, the mask reduced both VO2 and minute ventilation during moderate and severe exercise (p < 0.0001). Moreover, as can be seen in Figure 2a and c, this effect was particularly pronounced during severe exercise. The participants’ time to volitional exhaustion was also shortened by wearing a surgical mask during severe cycling (without: 6.7 ± 2.7; with mask: 6.0 ± 2.4 min, p = 0.014). On the other hand, heart rate and RER were not affected by masking at either time point (Figure 2b and d) (p > 0.05).
Table 1.
Cardiorespiratory, metabolic and mechanic parameters recorded during graded exercise testing without a surgical mask
| Variable | Participants (n = 32) |
|---|---|
| VO2peak (mL kg−1 min−1) | 52.2 ± 7.0 |
| WRpeak (W) | 231.1 ± 35.8 |
| Vepeak (L min−1) | 119.7 ± 30.2 |
| TVpeak (mL min−1) | 2369.7 ± 502.4 |
| RRpeak (cpm) | 50.8 ± 9.1 |
| RERpeak | 1.10 ± 0.06 |
| Heart ratepeak (bpm) | 189.6 ± 9.0 |
| O2 pulsepeak (mL/beat) | 18.8 ± 4.2 |
| VT (mL kg−1 min−1) | 37.2 ± 4.8 |
| VT (%) | 71.6 ± 7.3 |
| WRVT (W) | 162.8 ± 35.8 |
Values are mean ± SD.
Abbreviations: O2 pulsepeak, peak oxygen pulse; RERpeak, peak respiratory exchange ratio; RRpeak, peak respiratory rate; TVpeak, peak tidal volume; Vepeak, peak minute ventilation; VO2peak, peak oxygen uptake; VT, ventilatory threshold, WRVT, work rate at the ventilatory threshold; WRpeak, peak work rate.
Figure 2.
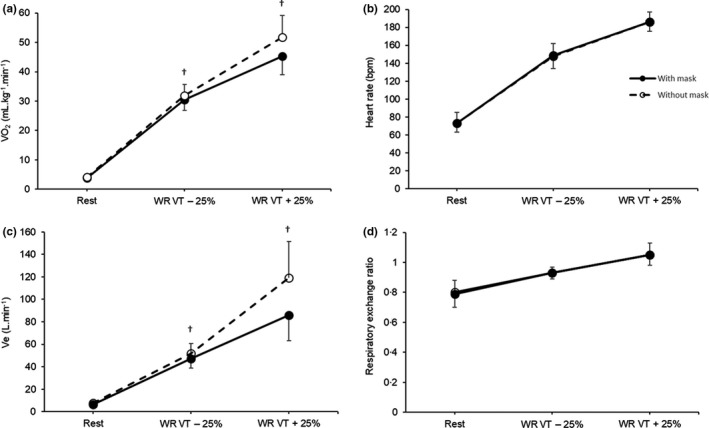
Oxygen uptake (VO2; a), heart rate (b), minute ventilation (Ve; c) and respiratory exchange ratio (d; RER) obtained at rest and in response to cycling (moderate and severe intensity domain) with and without a surgical face mask. Moderate cycling was performed at a work rate 25% below the ventilatory threshold (VT) and severe cycling was completed at a work rate 25% above the VT. †Significant differences between conditions (p < 0.01)
As shown in Table 2, comparisons between cardiorespiratory data obtained during GXT and severe exercise performed to volitional exhaustion without mask usage revealed no differences for VO2, minute ventilation or the O2 pulse (p > 0.05). Heart rate was also similar between both exercise tests (p > 0.05). In contrast, compared to that observed during GXT, wearing a face mask reduced VO2, minute ventilation and the O2 pulse (p < 0.0001). As described for the non‐mask condition, the chronotropic response to severe exercise while wearing a face mask was similar to that seen during GXT (p > 0.05).
Table 2.
Peak cardiorespiratory parameters recorded during graded exercise testing (GXT) and exercise performed above the ventilatory threshold (VT) to volitional exhaustion with and without a surgical mask
| GXT |
WRVT + 25% No mask |
WRVT + 25% Mask |
|
|---|---|---|---|
| VO2peak (mL kg−1 min−1) | 52.2 ± 7.0 | 51.7 ± 7.5 | 45.2 ± 6.3 a |
| Vepeak (L min−1) | 119.7 ± 30.1 | 119.2 ± 32.3 | 85.9 ± 22.5 a |
| Heart ratepeak (bpm) | 189.6 ± 9.0 | 186.3 ± 10.9 | 186.2 ± 10.3 |
| O2 pulsepeak (mL/beat) | 18.8 ± 4.2 | 18.8 ± 4.6 | 16.3 ± 3.5 a |
Values are mean ± SD.
Abbreviations: O2 pulsepeak, peak oxygen pulse; Vepeak, peak minute ventilation; VO2peak, peak oxygen uptake.
Significantly different from the GXT condition (p < 0.05).
After accounting for the decrease in VO2peak resulting from wearing a surgical mask (i.e. redefining VO2peak as the peak value obtained in response to severe exercise performed to volitional exhaustion with masking), we found that the mask usage increased the fractional utilization (relative intensity) of VO2peak during moderate cycling (without: 62.3 ± 7.1; with mask: 67.8 ± 6.9%, p < 0.0001).
As shown in Table 3, we also obtained significant condition‐by‐time interactions for tidal volume (F = 8.6, p = 0.001), respiratory rate (F = 16.5, p < 0.0001), Ve/VO2 (F = 13.5, p < 0.0001), Ve/VCO2, (F = 6.6, p = 0.007), end‐tidal fractional O2 concentration (F = 9.9, p = 0.001), end‐tidal fractional CO2 concentration (F = 14.4, p < 0.0001) and the O2 pulse (F = 23.6, p < 0.0001). With the exception of the respiratory rate that was slightly decreased by wearing a mask (p = 0.001), there were no other differences between conditions at rest. Cycling with a face mask at moderate intensity affected the physiological response of all variables included in Table 3 (p < 0.05), except tidal volume. During both moderate and severe exercise, the mask condition led to significant reductions in the respiratory rate, Ve/VO2, Ve/VCO2, end‐tidal fractional O2 concentration and O2 pulse (all p < 0.01). Contrasting with that seen in response to moderate cycling, tidal volume was significantly blunted by wearing a face mask during severe exercise (p < 0.0001). Finally, end‐tidal fractional CO2 concentration was heightened by the mask condition during exercise performed at both levels of intensity (p = 0.003).
Table 3.
Cardiorespiratory parameters recorded at rest as well as during exercise performed below and above the ventilatory threshold (VT) with and without a surgical mask
| Condition | Rest | WRVT −25% | WRVT +25% | |
|---|---|---|---|---|
| TV (mL min−1) a , c | Mask | 550.3 ± 242.3 | 1873.4 ± 425.3 | 2178.4 ± 499.4 d |
| No mask | 569.4 ± 205.3 | 1907.2 ± 414.2 | 2394.0 ± 535.5 | |
| RR (cpm) a , c | Mask | 11.6 ± 3.5 d | 26.1 ± 5.2 d | 39.9 ± 7.7 d |
| No mask | 13.9 ± 3.7 | 28.0 ± 4.5 | 50.1 ± 9.9 | |
| Ve/VO2 a , c | Mask | 25.5 ± 3.1 | 23.1 ± 2.5 d | 28.5 ± 3.7 d |
| No mask | 26.9 ± 3.8 | 24.1 ± 2.6 | 33.5 ± 3.9 | |
| Ve/VCO2 a , c | Mask | 32.9 ± 5.6 | 24.9 ± 3.4 d | 27.0 ± 3.9 d |
| No mask | 34.2 ± 7.4 | 26.2 ± 3.7 | 31.9 ± 4.1 | |
| FETO2 (%) a , b , c | Mask | 16.4 ± 0.5 | 15.9 ± 0.6 d | 16.9 ± 0.6 d |
| No mask | 16.6 ± 0.5 | 16.2 ± 0.5 | 17.5 ± 0.4 | |
| FETCO2 (%) a , b , c | Mask | 3.9 ± 0.5 | 4.7 ± 0.6 d | 4.3 ± 0.6 d |
| No mask | 3.8 ± 0.5 | 4.5 ± 0.6 | 3.6 ± 0.5 | |
| O2 pulse (mL/beat) a , b , c | Mask | 3.5 ± 0.8 | 13.8 ± 3.2 d | 16.3 ± 3.5 d |
| No mask | 3.7 ± 0.8 | 14.6 ± 3.3 | 18.8 ± 4.6 |
Values are mean ± SD.
Abbreviations: FETCO2, end‐tidal fractional carbon dioxide concentration; FETO2, end‐tidal fractional oxygen concentration; RR, respiratory rate; TV, tidal volume; Ve/VCO2, ventilatory equivalent for carbon dioxide; Ve/VO2, ventilatory equivalent for oxygen.
Time main effect (p < 0.05).
Condition main effect (p < 0.05).
Condition x time interaction (p < 0.05).
Significant differences between conditions (p < 0.01).
Table 4 shows that VO2 and RER attained steady‐state conditions between the 3rd and 6th min of moderate cycling, either with or without the face mask. This is corroborated by the lack of differences in submaximal VO2 and RER between the two epochs of analysis (i.e. 3–6 min vs. 7–10 min) (p > 0.05). In opposition, heart rate and minute ventilation exhibited a slight increase over time (p < 0.05), and this occurred similarly between conditions. With the exception of heart rate, the Δ 10‐7 of all the remaining variables included in Table 4 did not differ from zero (p > 0.05).
Table 4.
Values of characteristic parameters obtained at different epochs during exercise performed 25% below the ventilatory threshold with and without a surgical mask
| Condition | 3–6 min | 7–10 min | Δ 10‐7 | |
|---|---|---|---|---|
| VO2 (mL kg−1 min−1) | Mask | 30.1 ± 3.8 | 30.3 ± 3.5 | −0.04 ± 1.5 |
| No mask | 31.6 ± 3.9 | 32.0 ± 3.8 | 0.10 ± 1.2 | |
| Heart rate (bpm) | Mask | 142.5 ± 14.1 | 148.6 ± 14.5 a | 3.3 ± 3.0 b |
| No mask | 141.7 ± 13.9 | 147.8 ± 13.9 a | 3.8 ± 2.9 b | |
| Ve (L min−1) | Mask | 45.7 ± 9.1 | 47.2 ± 8.5 a | 0.8 ± 3.1 |
| No mask | 50.4 ± 8.4 | 51.9 ± 9.0 a | 0.7 ± 2.7 | |
| RER | Mask | 0.93 ± 0.05 | 0.93 ± 0.04 | −0.03 ± 0.02 |
| No mask | 0.94 ± 0.05 | 0.93 ± 0.05 | −0.01 ± 0.01 |
Values are mean ± SD.
Abbreviations: VO2, oxygen uptake; Ve, minute ventilation; RER, respiratory exchange ratio; Δ 7–10, change between the seventh and tenth minute of exercise.
Significant differences between time points (p < 0.05).
Δ value significantly different from 0 (p < 0.05).
4. DISCUSSION
The main findings of the present study are as follows. First, wearing a surgical face mask during constant work‐rate cycling exerts a negative impact on VO2, minute ventilation and the O2 pulse (seen both at moderate and severe exercise). Second, the magnitude of this impact is higher during severe exercise and this is in line with that hypothesized. Third, masking reduces the VO2peak and time to exhaustion in response to severe exercise by ~13 and 10%, respectively. Fourth, cycling with a surgical mask increases the relative intensity of moderate exercise performed at a given work rate. Lastly, our data indicate that masking does not affect steady‐state attainment during moderate cycling.
Aerodynamic studies indicate an increased potential range of droplet transfer between individuals during exercise due to increased minute ventilation (Blocken et al., 2020). However, the widespread usage of face masks in this context is limited largely by feeling that they are uncomfortable and concerns of inadequate gas exchange (Chandrasekaran & Fernandes, 2020). Nevertheless, it was recently recommended that face coverings should be used in any environment considered to be of a high (e.g. basketball, football, volleyball, indoor gyms, team sports training sessions) or moderate (e.g. racquet sports, track events, peloton cycling, rugby, running in a crowded place) transmission risk if tolerated and after individual risk assessment (Shurlock et al., 2021). Despite the relevance of these health‐related recommendations, according to our findings, young adults cannot exercise for as long or as hard while wearing a surgical face mask compared to when a mask is not used. Moreover, we also provided evidence that the magnitude of interference of the face mask with the physiological response to exercise increases as a function of intensity. In accordance, while masking exerts a negative impact on several ventilatory parameters during moderate exercise, this effect increases when cycling within the severe intensity domain—ultimately limiting VO2peak and time to exhaustion. These findings extend those of previous studies showing that, in healthy young people, the use of surgical masks affects the physiological responses to GXT and constant exercise at a work rate compatible with maximal lactate steady state (Egger et al., 2021; Fikenzer et al., 2020; Lassing et al., 2020; Li et al., 2021; Mapelli et al., 2021).
The negative effect of surgical masks on peak exercise performance, VO2 and minute ventilation of male adults had already been determined in one previous report (Egger et al., 2021). Our study adds to the available literature because we enrolled a mixed sample of males and females. Despite global data suggest that males appear at higher risk of infection and mortality from COVID‐19 with SARS‐CoV‐2, females can still contract the disease after direct exposure to the virus (Chakravarty et al., 2020). Thus, wearing a face mask during exercise for individual protection against infection in high‐risk environments represents a relevant measure for both males and females. For this reason, we enrolled mixed sample to better characterize the physiological impact of masking in both sexes during exercise. In addition, in the present study, severe exercise was performed at constant work rate to volitional exhaustion and this is different from the protocol used by Egger et al.—GXT (Egger et al., 2021). We designed a practical approach to this issue because exercise sessions do not typically involve performing GXTs for adaptation purposes. In contrast, the prescription of endurance exercise commonly consists of motor tasks engaging large muscle groups over a variable duration of time depending on exercise intensity (e.g. moderate, heavy or severe).
There is compelling evidence that the effects of increased inspiratory resistance on performance are felt most at very intense exercise (80–85% VO2peak). In specific, performance time decreases linearly with increased inspiratory resistance at this exercise intensity (Johnson et al., 1999). Since airway resistance is twofold higher when wearing a surgical mask (Lassing et al., 2020), this likely provides a partial explanation for our findings of decreased VO2 and time to exhaustion during severe exercise. Adding external resistance from a face mask increases the amount of work that must be supplied to breathe. In these circumstances, the O2 to supply the needs of ventilation cannot be used to supply the working muscles. Thus, the ventilatory demands associated with masking can limit the rate of work that can be performed individually (Johnson, 1976).
Wearing a face mask during moderate and severe exercise resulted in blunted ventilation, and this is well aligned with most studies focusing on this particular topic (Egger et al., 2021; Fikenzer et al., 2020; Lassing et al., 2020). There is general agreement that increased inspiratory resistance during exercise promotes hypoventilation of the wearer due to an extended inspiratory time (Lassing et al., 2020). The extended inspiratory time likely represents a compensatory mechanism that attempts to minimize the magnitude of fall in tidal volume during severe exercise performed with a surgical mask. Despite this, according to our data, a reduction in tidal volume still occurred with masking, thus leading to an inevitable reduction in alveolar ventilation and VO2.
Besides the added resistance to breathing, another issue with exercising with a face mask is the inspiration of previously exhaled tidal volume depleted of O2 and enriched with CO2 (i.e. increased dead space) (Hopkins et al., 2021). Our data partially corroborate this notion because we found that wearing a mask during severe exercise reduced tidal volume as well as end‐tidal fractional O2 concentration. In parallel, masking also heightened the end‐tidal fractional CO2 concentration during exercise. Since CO2 is a psychoactive gas that typically produces discomfort and performance decrements (Johnson et al., 2000), our findings of premature volitional exhaustion during severe exercise may also be mechanistically linked to rebreathing of CO2.
As it is well known, more intense exercise cannot be sustained for as long as less intense exercise. In specific, the amount of time that a person can be expected to endure is related to the relative intensity of the motor task being performed (Moritani et al., 1981). We found that wearing a surgical mask increases the relative intensity of moderate cycling (by ~5%) due to a significant decrease in VO2peak (~13%). This means that, besides reducing the time to exhaustion during severe exercise, wearing a surgical face mask may negatively affect work performance times during moderate cycling and this is of practical relevance. For instance, rest times are also dependent on the intensity of the task and individual VO2peak (Mann et al., 2014; Tomlin & Wenger, 2001). In general, the more intense the exercise, the longer will be the recovery time, but the relationship is non‐linear (Gore & Withers, 1990).
Masking resulted in a significant reduction in the ventilatory equivalent for CO2. Changes in the ventilatory equivalent for CO2 reflect modifications in PaCO2 and/or in the physiological dead space (Neder et al., 2017). While an increase in the ventilatory equivalent for CO2 is typically associated with poor ventilatory efficiency, a downward displacement (such as that seen in the present study) occurs when PaCO2 set point is raised due to hypoventilation (Mezzani, 2017). Our findings of heightened end‐tidal fractional CO2 concentration during exercise with face mask further indicate that this might be the case. End‐tidal CO2 represents a non‐invasive and reliable measure of PaCO2 in healthy persons (Jones et al., 1979) and has been consistently shown to be elevated in response to exercise with masking (Shaw et al., 2021). During exercise, end‐tidal CO2 is highly dependent on respiratory rate (Bussotti et al., 2008). For instance, at a given alveolar CO2, higher fractions of end‐tidal CO2 are compatible with lower respiratory rates. Thus, our data agree with the notion that exercising with a surgical mask raises PaCO2 due to a limited ability to ventilate effectively.
A higher PaCO2 is associated with greater tissue acidosis, which through a rightward shift on the oxyhaemoglobin saturation curve allows unloading more O2 from the blood into the muscle (Bussotti et al., 2008; Chandrasekaran & Fernandes, 2020). Ultimately, this might explain the increased ventilatory efficiency obtained for VO2 during exercise performed with a face mask—as indicated by a reduced ventilatory equivalent for O2. In accordance, a physiological compensation might therefore counteract limited ventilation with masking, thus enabling greater O2 utilization by the muscle during moderate and severe cycling. It is important to note that this effect could also be hypothetically explained by enhanced O2 delivery to contracting myocytes. However, since heart rate was not affected by mask usage during moderate or severe cycle, and the O2 pulse actually decreased with masking, this is highly unlikely. The reduction in the O2 pulse values indicates that masking attenuated VO2 per mL of heartbeat, and this is compatible with lower cardiovascular efficiency (Goran et al., 2000). Despite being a surrogate index of stroke volume, the O2 pulse is also dependent on the arteriovenous O2 difference (Crisafulli et al., 2007). Since there is preliminary evidence that wearing surgical masks does not impact submaximal stroke volume during steady‐state exercise (Lassing et al., 2020), our findings likely reflect a negative impact of masking on the arteriovenous O2 difference and this is in line with that shown in one previous report (Fikenzer et al., 2020),.
The timing for steady‐state attainment during moderate exercise is important because it largely determines the magnitude of the O2 deficit and the inherent anaerobic energy demand in transition from rest to exercise (Demarle et al., 2001). Our analyses show that, despite affecting the physiological response to moderate exercise (e.g. increasing the relative intensity of exercise), the use of face masks allowed VO2 and RER to reach a steady state at 3 min of cycling. Thus, when performed at an intensity below the VT, exercising with a surgical mask does not elicit a slow component in VO2 and this is important from a physiological and performance standpoint.
4.1. Limitations
First, the use of a surgical mask impedes heat loss from the face during exercise and this may cause individual discomfort due to facial temperature inside the mask (Johnson, 2016). We did not measure face temperature inside the masks worn by each participant during exercise. Thus, we cannot determine whether this particular aspect played an active role in decreasing work performance during severe exercise. Second, it has been argued that ventilation, tidal volume and respiratory rate may be difficult to measure while wearing a rubber mask over the face mask (Shaw et al., 2021). According to these authors, when placing a rubber mask for assessing ventilation over a surgical mask, there is a loss of seal and air most likely escapes, resulting in lower ventilation measures (Shaw et al., 2021). However, contrary to this concept, we showed that the reduction in ventilation while wearing a surgical mask during severe exercise performed at a constant work rate is accompanied by considerable magnitude of reduction in VO2peak and time to exhaustion. These results are internally consistent and, for this reason, they indicate that air leaking when testing the mask condition did not occur. Third, from a different perspective, it has also been suggested that placing a rubber mask over a surgical mask might not allow air to escape the sides of the mask—affecting its normal functioning during exercise (Egger et al., 2021). Under these circumstances, sealing of the face mask might lead to moisture retention within the mask, thus affecting the practical transfer of our findings (i.e. limited transfer to daily training conditions). Moreover, in comparison with that seen with the ‘normal’ use of a rather loose surgical face mask, this setup may have resulted in alterations in breathing pattern, hypoventilation, retention of CO2 and increase the work of breathing. Since these effects can be further accentuated during severe physical work (Louhevaara, 1984), this phenomenon might provide a partial explanation for the reduction in maximal exercise capacity seen in this study. Fourth, we did not measure pre‐exercise maximal voluntary ventilation. For this reason, the true impact of masking at the level of the ventilatory reserve could not be analysed during exercise. Fifth, the participants were not blinded to the masking condition and this may as well have affected our findings.
5. CONCLUSIONS
In conclusion, the impact of the surgical masks on exercise capacity is particularly pronounced during severe exercise performed at constant work rate and this may implicate a considerable impairment of structured (e.g. exercise training) or even unstructured (e.g. occupational motor tasks) strenuous physical activity.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ACKNOWLEDGEMENTS
This work was supported by the Fundação para a Ciência e Tecnologia, under Grant UIDB/00447/2020 to CIPER – Centro Interdisciplinar para o Estudo da Performance Humana (unit 447).
Jesus, J. P. , Gomes, M. , Dias-Gonçalves, A. , Correia, J. M. , Pezarat‐Correia, P. , & Mendonca, G. V. (2022). Effects of surgical masks on the responses to constant work‐rate cycling performed at different intensity domains. Clinical Physiology and Functional Imaging, 42, 43–52. Available from: 10.1111/cpf.12734
REFERENCES
- Banzett, R.B. , Lansing, R.W. , Brown, R. , Topulos, G.P. , Yager, D. , Steele, S.M. et al. (1990) ‘Air hunger’ from increased PCO2 persists after complete neuromuscular block in humans. Respiration Physiology, 81, 1–17. [DOI] [PubMed] [Google Scholar]
- Bird, S. & Davidson, R. (1997) Guidelines for Physiological Testing of Athtletes. British Association of Sport and Exercise Sciences. Physiology Section. [Google Scholar]
- Black, M.I. , Jones, A.M. , Blackwell, J.R. , Bailey, S.J. , Wylie, L.J. , McDonagh, S.T. et al. (2017). Muscle metabolic and neuromuscular determinants of fatigue during cycling in different exercise intensity domains. Journal of Applied Physiology, 122, 446–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blocken, B. , Malizia, F. , van Druenen, T. & Marchal, T. (2020). Towards aerodynamically equivalent covid‐19 1.5 m social distancing for walking and running . Accessed on 28 June 2021.
- Bull, F.C. , Al‐Ansari, S.S. , Biddle, S. , Borodulin, K. , Buman, M.P. , Cardon, G. et al. (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicine, 54, 1451–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussotti, M. , Magri, D. , Previtali, E. , Farina, S. , Torri, A. , Matturri, M. et al. (2008) End‐tidal pressure of CO2 and exercise performance in healthy subjects. European Journal of Applied Physiology, 103, 727–732. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020). Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community‐Based Transmission . Available from: https://stacks.cdc.gov/view/cdc/86440
- Chakravarty, D. , Nair, S.S. , Hammouda, N. , Ratnani, P. , Gharib, Y. , Wagaskar, V. et al. (2020) Sex differences in SARS‐CoV‐2 infection rates and the potential link to prostate cancer. Communications Biology, 3, 374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekaran, B. & Fernandes, S. (2020) "Exercise with facemask; Are we handling a devil's sword?" – a physiological hypothesis. Medical Hypotheses, 144, 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y. , Yang, Z. , Wang, J. & Gong, H. (2016) Physiological and subjective responses to breathing resistance of N95 filtering facepiece respirators in still‐sitting and walking. International Journal of Industrial Ergonomics, 53, 93–101. [Google Scholar]
- Crisafulli, A. , Piras, F. , Chiappori, P. , Vitelli, S. , Caria, M.A. , Lobina, A. et al. (2007) Estimating stroke volume from oxygen pulse during exercise. Physiological Measurement, 28, 1201–1212. [DOI] [PubMed] [Google Scholar]
- Demarle, A.P. , Slawinski, J.J. , Laffite, L.P. , Bocquet, V.G. , Koralsztein, J.P. & Billat, V.L. (2001). Decrease of O(2) deficit is a potential factor in increased time to exhaustion after specific endurance training. Journal of Applied Physiology, 90, 947–953. [DOI] [PubMed] [Google Scholar]
- Egger, F. , Blumenauer, D. , Fischer, P. , Venhorst, A. , Kulenthiran, S. , Bewarder, Y. et al. (2021) Effects of face masks on performance and cardiorespiratory response in well‐trained athletes. Clinical Research in Cardiology, 6, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein, D. , Korytny, A. , Isenberg, Y. , Marcusohn, E. , Zukermann, R. , Bishop, B. et al. (2021) Return to training in the COVID‐19 era: The physiological effects of face masks during exercise. Scandinavian Journal of Medicine and Science in Sports, 31, 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esteve‐Lanao, J. , Foster, C. , Seiler, S. & Lucia, A. (2007) Impact of training intensity distribution on performance in endurance athletes. Journal of Strength and Conditioning Research, 21, 943–949. [DOI] [PubMed] [Google Scholar]
- Fikenzer, S. , Uhe, T. , Lavall, D. , Rudolph, U. , Falz, R. , Busse, M. et al. (2020) Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clinical Research in Cardiology, 109, 1522–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goran, M. , Fields, D.A. , Hunter, G.R. , Herd, S.L. & Weinsier, R.L. (2000) Total body fat does not influence maximal aerobic capacity. International Journal of Obesity and Related Metabolic Disorders, 24, 841–848. [DOI] [PubMed] [Google Scholar]
- Gore, C.J. & Withers, R.T. (1990). Effect of exercise intensity and duration on postexercise metabolism. Journal of Applied Physiology, 68, 2362–2368. [DOI] [PubMed] [Google Scholar]
- Hopkins, S.R. , Dominelli, P.B. , Davis, C.K. , Guenette, J.A. , Luks, A.M. , Molgat‐Seon, Y. et al. (2021) Face masks and the cardiorespiratory response to physical activity in health and disease. Annals of the American Thoracic Society, 18, 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, A.T. (1976) The energetics of mask wear. American Industrial Hygiene Association Journal, 37, 479–488. [DOI] [PubMed] [Google Scholar]
- Johnson, A.T. (2016) Respirator masks protect health but impact performance: a review. Journal of Biological Engineering, 10, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, A.T. , Scott, W.H. , Lausted, C.G. , Benjamin, M.B. , Coyne, K.M. , Sahota, M.S. et al. (1999) Effect of respirator inspiratory resistance level on constant load treadmill work performance. American Industrial Hygiene Association Journal, 60, 474–479. [DOI] [PubMed] [Google Scholar]
- Johnson, A.T. , Scott, W.H. , Lausted, C.G. , Coyne, K.M. , Sahota, M.S. & Johnson, M.M. (2000) Effect of external dead volume on performance while wearing a respirator. American Industrial Hygiene Association Journal, 61, 678–684. [DOI] [PubMed] [Google Scholar]
- Jones, N.L. , Robertson, D.G. & Kane, J.W. (1979) Difference between end‐tidal and arterial PCO2 in exercise. Journal of Applied Physiology: Respiratory, Environmental and Exercise Physiology, 47, 954–960. [DOI] [PubMed] [Google Scholar]
- Lassing, J. , Falz, R. , Pokel, C. , Fikenzer, S. , Laufs, U. , Schulze, A. et al. (2020) Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Scientific Reports, 10, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung, N.H.L. (2021) Transmissibility and transmission of respiratory viruses. Nature Reviews Microbiology, 19(8), 528–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, M. , Ou, H. , Li, Q. , Liang, J. , Liao, W. , Lang, S. et al. (2021) Effects of surgical masks on cardiopulmonary function in healthy subjects. Journal of Visualized Experiments, 168, e62121. [DOI] [PubMed] [Google Scholar]
- Louhevaara, V.A. (1984) Physiological effects associated with the use of respiratory protective devices. A review. Scandinavian Journal of Work, Environment and Health, 10, 275–281. [DOI] [PubMed] [Google Scholar]
- Mann, T.N. , Webster, C. , Lamberts, R.P. & Lambert, M.I. (2014) Effect of exercise intensity on post‐exercise oxygen consumption and heart rate recovery. European Journal of Applied Physiology, 114, 1809–1820. [DOI] [PubMed] [Google Scholar]
- Mapelli, M. , Salvioni, E. , De Martino, F. , Mattavelli, I. , Gugliandolo, P. , Vignati, C. et al. (2021). "You can leave your mask on": effects on cardiopulmonary parameters of different airway protection masks at rest and during maximal exercise. European Respiratory Journal, 58(3), 2004473. 10.1183/13993003.04473-2020. Online ahead of print [DOI] [PubMed] [Google Scholar]
- Mezzani, A. (2017) Cardiopulmonary exercise testing: basics of methodology and measurements. Annals of the American Thoracic Society, 14, S3–S11. [DOI] [PubMed] [Google Scholar]
- Moritani, T. , Nagata, A. , deVries, H.A. & Muro, M. (1981) Critical power as a measure of physical work capacity and anaerobic threshold. Ergonomics, 24, 339–350. [DOI] [PubMed] [Google Scholar]
- Neder, J.A. , Berton, D.C. , Arbex, F.F. , Alencar, M.C. , Rocha, A. , Sperandio, P.A. et al. (2017) Physiological and clinical relevance of exercise ventilatory efficiency in COPD. European Respiratory Journal, 49(3), 1602036. [DOI] [PubMed] [Google Scholar]
- Person, E. , Lemercier, C. , Royer, A. & Reychler, G. (2018) Effect of a surgical mask on six minute walking distance. Revue Des Maladies Respiratoires, 35, 264–268. [DOI] [PubMed] [Google Scholar]
- Samannan, R. , Holt, G. , Calderon‐Candelario, R. , Mirsaeidi, M. & Campos, M. (2021) Effect of face masks on gas exchange in healthy persons and patients with chronic obstructive pulmonary disease. Annals of the American Thoracic Society, 18, 541–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarano, A. , Inchingolo, F. & Lorusso, F. (2020) Facial skin temperature and discomfort when wearing protective face masks: thermal infrared imaging evaluation and hands moving the mask. International Journal of Environmental Research and Public Health, 17(13), 4624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, K. , Butcher, S. , Ko, J. , Zello, G.A. & Chilibeck, P.D. (2020) Wearing of cloth or disposable surgical face masks has no effect on vigorous exercise performance in healthy individuals. International Journal of Environmental Research and Public Health, 17(21), 8110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, K.A. , Zello, G.A. , Butcher, S.J. , Ko, J.B. , Bertrand, L. & Chilibeck, P.D. (2021) The impact of face masks on performance and physiological outcomes during exercise: a systematic review and meta‐analysis. Applied Physiology, Nutrition and Metabolism, 46(7), 693–703. [DOI] [PubMed] [Google Scholar]
- Shenal, B.V. , Radonovich, L.J. Jr , Cheng, J. , Hodgson, M. & Bender, B.S. (2012) Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. Journal of Occupational and Environmental Hygiene, 9, 59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shurlock, J. , Muniz‐Pardos, B. , Tucker, R. , Bachl, N. , Papadopoulou, T. , Holloway, G. et al. Recommendations for face coverings while exercising during the COVID‐19 pandemic. Sports Medicine ‐ Open, 7(1), 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, J. , He, W.T. , Wang, L. , Lai, A. , Ji, X. , Zhai, X. et al. (2020) COVID‐19: epidemiology, evolution, and cross‐disciplinary perspectives. Trends in Molecular Medicine, 26, 483–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlin, D.L. & Wenger, H.A. (2001) The relationship between aerobic fitness and recovery from high intensity intermittent exercise. Sports Medicine, 31, 1–11. [DOI] [PubMed] [Google Scholar]
- Wasserman, K. , Whipp, B.J. , Koyl, S.N. & Beaver, W.L. (1973) Anaerobic threshold and respiratory gas exchange during exercise. Journal of Applied Physiology, 35, 236–243. [DOI] [PubMed] [Google Scholar]
- Whelton, P.K. , Carey, R.M. , Aronow, W.S. , Casey, D.E. Jr , Collins, K.J. , Dennison Himmelfarb, C. et al. (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension, 71, 1269–1324. [DOI] [PubMed] [Google Scholar]
- Whipp, B.J. & Wasserman, K. (1972) Oxygen uptake kinetics for various intensities of constant‐load work. Journal of Applied Physiology, 33, 351–356. [DOI] [PubMed] [Google Scholar]
- Wong, A.Y. , Ling, S.K. , Louie, L.H. , Law, G.Y. , So, R.C. , Lee, D.C. et al. (2020) Impact of the COVID‐19 pandemic on sports and exercise. Asia‐Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology, 22, 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). Mask use in the context of COVID‐19: interim guidance. 1 December 2020 . Available from https://apps.who.int/iris/handle/10665/337199


