Abstract
Non-steroidal anti-inflammatory drugs (NSAIDs) can cause small bowel damage, which could present in different ways, including abdominal pain and occult gastrointestinal bleeding. NSAID use can also result in small bowel strictures, which can be challenging to diagnose and manage. Here, we describe a case of a 49-year-old female who presented with chronic anaemia and intermittent abdominal pain, with a history of NSAID use. She underwent capsule endoscopy as part of the workup for anaemia and subsequently had capsule retention due to a small bowel stricture.
Keywords: Non-steroidal anti-inflammatory drugs, Small bowel diaphragm disease, Small bowel strictures, Capsule endoscopy
Introduction
NSAIDs are associated with small bowel injury in the form of erosions, ulcers, bleeding, perforation, and strictures [1]. NSAID-induced small bowel strictures are typically concentric diaphragm-like strictures and thus also called diaphragm disease. Diaphragm disease is rare and is considered to be pathognomonic of NSAID-induced damage. These strictures can lead to intermittent or complete small bowel obstruction. Patients with small bowel strictures can also present with severe iron deficiency anaemia requiring multiple investigations to ascertain the cause. Capsule endoscopy allows us to visualize the entire small bowel and is most commonly used to investigate GI blood loss when oesophagogastroscopy and colonoscopy have not revealed an aetiology. It can also be used to detect small bowel Crohn's disease, polyps, or tumours. It is a procedure where a tiny wireless camera is swallowed. It takes 1000s of images of the digestive tract during its passage from the mouth down to the rectum, which are transmitted to a recording device and subsequently downloaded for viewing. Performing a capsule endoscopy in cases with small bowel strictures can be complicated by capsule retention.
Case Report/Case Presentation
A 49-year-old female was initially referred by her GP 6 years ago with a history of intermittent abdominal pain for 2 years and iron deficiency anaemia. Abdominal pain was mild and located mainly in the centre but with some generalization throughout the abdomen. It was associated with mild nausea at times but no vomiting. She has a history of longstanding constipation, and pain would get worse during days of constipation. There was no history of weight loss. There was no other significant background history apart from some non-specific pelvic and knee joint pains for which she takes ibuprofen on and off. She does give an account of some irregular menstrual cycle but not massive bleeding. She underwent a gastroscopy, which was normal, but colonoscopy failed due to inadequate preparation. The impression was that her irregular menstrual cycle contributed to her anaemia and that she was suffering from slow-transit constipation, which resulted in poor bowel preparation. She was started on oral iron, and the plan was to monitor her haemoglobin and do a stool occult blood test; if this is positive, to repeat colonoscopy. Her stool occult blood test was negative on a couple of occasions, so she was continued per oral iron and kept under observation for anaemia. Due to ongoing issues with anaemia, she had a complete colonoscopy done in 2015, which was normal. She was re-referred by her GP in February 2019 with ongoing problems with chronic anaemia. Symptomatically, she complained of severe tiredness, and her abdominal pain had worsened with occasional episodes of severe abdominal pain, central in origin, which were related to her meals. She did give a history of nausea and episodic abdominal pains, but no vomiting and constipation had been getting worse lately. She required a couple of iron infusions with her GP to keep her iron reserves up.
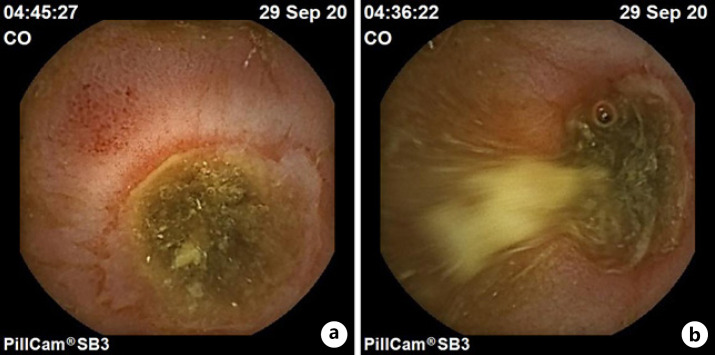
Her latest Hb was 7.5 g/dL, MCV − 62.3 fL, iron − 2.3 μmol/L, and ferritin − 1.8 ng/mL. Her systemic examination was unremarkable. At this stage, she had a repeat OGD, which showed a couple of shallow ulcers in the pylorus likely due to NSAIDs, and histology showed mild active inflammation but no metaplasia or dysplasia. Her repeat colonoscopy was unremarkable. She went onto have MRE to investigate for a cause of anaemia which was unremarkable, and of note, there was no stricture seen. She underwent capsule endoscopy in September 2020 as a part of investigations of her ongoing anaemia, which showed a large area of ulceration in the distal small bowel with an evident stricture. The capsule bounced back and forth here and then seemed to progress to an area that is blood-stained, ulcerated, and again stenosed. Prep was somewhat compromised in this area, so it was hard to be 100% confident that these are 2 distinct ulcers, but probably favoured 2 separate areas of ulcerations and strictures here.
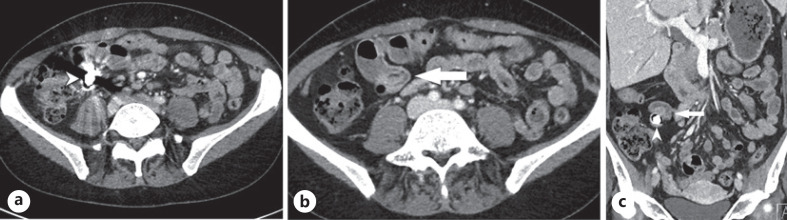
The capsule seemed to not progress beyond this point. A follow-up X-ray abdomen confirmed capsule retention, and subsequent CT abdomen with contrast also showed the presence of the capsule in the distal ileum just proximal to a small bowel stricture. A retrograde review of the MRE also raised the suspicion of stricture in the distal small bowel. The patient was asymptomatic from a capsule retention point of view. She was referred for double-balloon enteroscopy to remove the retained capsule, but unfortunately, the retrograde DBE attempt failed due to poor prep. After discussing the pros and cons of the retained capsule with the patient, it was mutually decided to leave the capsule in place for now as she is asymptomatic, start her on misoprostol, and avoid NSAIDs. She was advised to immediately contact the hospital emergency department if she developed any obstructive symptoms. Otherwise, she is being followed closely in OPD. She was also briefed not to have a pregnancy and an MRI scan. To date, she is doing well on misoprostol with no obstructive symptoms, and her Hb has been stable (Fig. 1, 2, 3).
Fig. 1.
a Capsule endoscopy showing a large semicircumferential ulcer in the distal small bowel. b The same ulcer from a different angle.
Fig. 2.
Axial (a, b) and coronal (c) images from a contrast-enhanced CT abdomen show a metallic marker (arrowhead, a–c) in the distal ileum, just proximal to a small bowel stricture (arrows, a, b).
Fig. 3.

Plain X-ray of the abdomen showing the presence of capsule in the lower abdomen.
Discussion/Conclusion
Small bowel diaphragm disease is a relatively rare entity first described in 1988 by Lang et al. [2]. Small bowel diaphragm disease is characterised by circumferential lesions of short length <5 cm, causing intrinsic stenosis of the small bowel lumen [3]. The pathogenesis is certainly multifactorial but still not entirely clear. It can result in GI bleeding and obstruction. Diagnosis of DD often requires endoscopy, gastrointestinal radiological techniques, and even laparotomy [1, 4]. Chronic abdominal pain and anaemia are the 2 most common presenting features of SBDD with 58% and 42% frequency and rarely can cause obstruction [5]. The exact duration of NSAID uses to cause small bowel strictures is not clear. In one of the studies, the mean duration of NSAIDs for disease development was 7 years [6]. In a capsule endoscopy study of 160 patients taking NSAIDS for >3 months, around 2% were found to have SBDD [7]. The main differentials of SBDD include Crohn's disease, malignancy, and NSAID-induced enteropathy.
The diagnostics of NSAID-induced small intestinal injuries has evolved since the advent of capsule endoscopy and double-balloon enteroscopy [1]. Nevertheless, a high index of suspicion and a clear history of NSAID use is crucial to clinching the diagnosis. Once a suspicion of diaphragm disease is raised, CT or MRI of the small bowel can be done for further evaluation. Push enteroscopy and DBE may be preferred as they can be therapeutic at the same time. The mainstay of treatment for NSAID-induced strictures (SBDD) is the discontinuation of NSAIDs [3]. Management of NSAID-induced stricture may include DBE +/− balloon dilatation, needle knife electro-incision, and/or surgical resection [6, 8].
Persistent iron deficiency anaemia is the most common indication for capsule endoscopy. One of the potential complications of capsule endoscopy is the retention of the capsule in the small bowel. Capsule retention has been reported in approximately 1.4% of CE procedures [9, 10]. The most common reasons for capsule retention are Crohn's disease, obstructive tumour, and diaphragm disease due to the side effects of NSAIDs [9, 11]. NSAID use has been recognized as one of the significant risk factors for capsule retention [9]. The small bowel is the most common site for capsule retention [12].
Management of retained capsule in small bowel poses a challenge, and the decision to remove it or leave it with the watch and wait strategy needs to be made in agreement with the patient. Conservative observation or treatment with drugs for the underlying condition such as steroids for Crohn's disease, cessation of NSAIDS, and giving misoprostol in diaphragm disease or attempt to remove the retained capsule via DBE or surgery can be considered depending upon the patient's condition and consent. A randomized trial reported that misoprostol effectively healed small bowel ulcers in 54% of patients taking NSAIDs and aspirin [13]. Another trial showed that misoprostol is superior to a placebo in healing small bowel ulcers in patients taking long-term aspirin [14].
The presence of abdominal symptoms such as pain and small bowel thickening on CT scan are the 2 most significant factors requiring intervention. Age, sex, history of GI surgery, and reason for CE are less significant [12]. A large Korean study of 2,705 patients with capsule endoscopy showed spontaneous resolution of the retained capsule in 15% (within 85 days) of patients, whereas 10% of capsules dislodged after steroid therapy. Endoscopic removal was done in 30% by DBE; surgical intervention was required in 45% and no CR-related death. In the same study, one of the patients was diagnosed with NSAID enteropathy in the ileum, and after cessation of NSAIDs, the capsule spontaneously passed 75 days after CR [12]. Another study showed that conservative measures induce spontaneous passage of capsule in 52.4% of cases [15].
Double-balloon enteroscopy can be performed instead of surgery/laparotomy for retrieving retained capsules and balloon dilatation of strictures in SBDD, thereby preventing the need for potentially complicated surgery [6]. In short, both conservative and endoscopic management has shown successful results, and if the patient is asymptomatic, both the strategies can be considered with surgical option as a last resort.
NSAID-induced small bowel strictures remain an underdiagnosed and challenging entity. Diagnosis of SBDD requires early suspicion of the same by the clinicians. Such cases need to be discussed with radiology colleagues to keep in mind the differential of diaphragm disease while reporting CT and MRI scans of the small bowel. In our case, small bowel stricture was initially missed on MRI of the small bowel, leading to capsule endoscopy and eventually retention of the capsule. A systematic approach and knowledge of the disease are required to make a timely diagnosis and treat this condition.
Statement of Ethics
Written informed consent was obtained from the patient to publish this case report and the accompanying images. This case report was exempted from the Institutional Review Board of the University Hospital Galway as per its policy.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was obtained for the publication of this case report.
Author Contributions
The first author is responsible for writing the manuscript. The second author is the primary consultant of the patient and has provided the details about the medical aspect of the case. The third author is the consultant who performed the capsule endoscopy on the patient and has provided relevant details of capsule endoscopy and the images. The second and third authors have reviewed the manuscript and advised changes incorporated in the final version. All 3 authors reviewed the case report before submission.
Data Availability Statement
Data sharing is not applicable to this case report as no datasets were generated or analysed for writing this case report.
References
- 1.Ishihara M, Ohmiya N, Nakamura M, Funasaka K, Miyahara R, Ohno E, et al. Risk factors of symptomatic NSAID-induced small intestinal injury and diaphragm disease. Aliment Pharmacol Ther. 2014 Sep;40((5)):538–47. doi: 10.1111/apt.12858. [DOI] [PubMed] [Google Scholar]
- 2.Lang J, Price AB, Levi AJ, Burke M, Gumpel JM, Bjarnason I. Diaphragm disease: pathology of disease of the small intestine induced by non-steroidal anti-inflammatory drugs. J Clin Pathol. 1988 May;41((5)):516–26. doi: 10.1136/jcp.41.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pereira R, Slater K. Small bowel diaphragm disease from long-term non-steroidal anti-inflammatory use. BMJ Case Rep. 2019 Oct 5;12((10)):e230735. doi: 10.1136/bcr-2019-230735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang YZ, Sun G, Cai FC, Yang YS. Clinical features, diagnosis, and treatment strategies of gastrointestinal diaphragm disease associated with nonsteroidal anti-inflammatory drugs. Gastroenterol Res Pract. 2016;2016:3679741. doi: 10.1155/2016/3679741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meshikhes AW. Retained enteroscopy capsule in a patient with diaphragm disease. Ann R Coll Surg Engl. 2016 May;98((5)):e79–81. doi: 10.1308/rcsann.2016.0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slesser AA, Wharton R, Smith GV, Buchanan GN. Systematic review of small bowel diaphragm disease requiring surgery. Colorectal Dis. 2012 Jul;14((7)):804–13. doi: 10.1111/j.1463-1318.2011.02741.x. [DOI] [PubMed] [Google Scholar]
- 7.Maiden L, Thjodleifsson B, Seigal A, Bjarnason II, Scott D, Birgisson S, et al. Long-term effects of non-steroidal anti-inflammatory drugs cyclooxygenase-2 selective agents on the small bowel: a cross-sectional capsule enteroscopy study. Clin Gastroenterol Hepatol. 2007 Sep;5((9)):1040–5. doi: 10.1016/j.cgh.2007.04.031. [DOI] [PubMed] [Google Scholar]
- 8.Srinivasan A, De Cruz P. Review article: a practical approach to the clinical management of NSAID enteropathy. Scand J Gastroenterol. 2017 Sep;52((9)):941–7. doi: 10.1080/00365521.2017.1335769. [DOI] [PubMed] [Google Scholar]
- 9.Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010 Feb;71((2)):280–6. doi: 10.1016/j.gie.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 10.Höög CM, Bark LÅ, Arkani J, Gorsetman J, Broström O, Sjöqvist U. Capsule retentions and incomplete capsule endoscopy examinations: an analysis of 2300 examinations. Gastroenterol Res Pract. 2012;2012:518718. doi: 10.1155/2012/518718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li F, Gurudu SR, De Petris G, Sharma VK, Shiff AD, Heigh RI, et al. Retention of the capsule endoscope: a single-centre experience of 1000 capsule endoscopy procedures. Gastrointest Endosc. 2008 Jul;68((1)):174–80. doi: 10.1016/j.gie.2008.02.037. [DOI] [PubMed] [Google Scholar]
- 12.Lee HS, Lim YJ, Kim KO, Jang HJ, Chun J, Jeon SR, et al. Outcomes and management strategies for capsule retention: a Korean Capsule Endoscopy Nationwide Database Registry Study. Dig Dis Sci. 2019 Nov;64((11)):3240–6. doi: 10.1007/s10620-019-05659-7. [DOI] [PubMed] [Google Scholar]
- 13.Taha AS, McCloskey C, McSkimming P, McConnachie A. Misoprostol for small bowel ulcers in patients with obscure bleeding taking aspirin and non-steroidal anti-inflammatory drugs (MASTERS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Gastroenterol Hepatol. 2018 Jul;3((7)):469–76. doi: 10.1016/S2468-1253(18)30119-5. [DOI] [PubMed] [Google Scholar]
- 14.Kyaw MH, Otani K, Ching JYL, Higashimori A, Kee KM, Watanabe T, et al. Misoprostol heals small bowel ulcers in aspirin users with small bowel bleeding. Gastroenterology. 2018 Oct;155((4)):1090–e1. doi: 10.1053/j.gastro.2018.06.056. [DOI] [PubMed] [Google Scholar]
- 15.Cheon JH, Kim YS, Lee IS, Chang DK, Ryu JK, Lee KJ, et al. Can we predict spontaneous capsule passage after retention? A nationwide study to evaluate the incidence and clinical outcomes of capsule retention. Endoscopy. 2007 Dec;39((12)):1046–52. doi: 10.1055/s-2007-966978. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this case report as no datasets were generated or analysed for writing this case report.