Abstract
Background:
Maternal mortality remains a problem in low-income countries (LICs). In Zimbabwe, there has been an unprecedented increase in maternal mortality in the last 2.5 decades. Effective prenatal care delivery, particularly early visits, appropriate number of visits, and receiving recommended care is viewed as key to reducing fatal care outcomes.
Aims:
This study sought to model and identify gaps requiring service and care delivery improvement in prenatal care pathways for pregnant women visiting Mpilo Central Hospital in Bulawayo, Zimbabwe.
Methods:
This was a case study of the services offered by an antenatal care department at Mpilo Central Hospital in Bulawayo, Zimbabwe. Evidence from literature in low-income countries was used to develop prenatal care pathway guidelines as a tool to guide care delivery and identify gaps in care and service delivery. One hundred cases of prenatal care records were reviewed to determine the prenatal care pathway and care delivered to pregnant women. This data was complemented by interviews with 20 maternity care clinicians.
Results:
In 100 maternity case records studied, 53% booked for prenatal care. Of the 53% (n = 53) pregnant women who booked, their first visit on their pregnancy was late at an average gestational age of 27.1 weeks with extremes of 30 to 40 weeks in 38% (n = 20) cases. Missing scheduled prenatal care appointments was prevalent, with only 11% (n = 6) having attended all the expected 5 visits, whilst 60% (n = 32) missed 3 or more. There were inadequacies in the care delivered to women in each visit compared to that expected in such areas as obstetrics, physical examinations and haematological tests. Maternity care clinicians attributed the cost of prenatal booking fees in the background of poverty and poor family support systems as key factors hindering women’s access to prenatal services.
Conclusions:
The current prenatal care pathway at MCH requires improvement in the areas of referral, adherence to appointment by pregnant women and visiting prenatal care early. Clinicians also need to adhere to standard clinical tests recommended for each specific pregnant woman’s visit. In the Zimbabwean setting with limited resources, where the number of visits is already low, pathways with reduced visits may not be appropriate. An investment into prenatal care by the government is recommended to enable the utilisation of interventions such as e-health technologies that may improve care delivery as well as adherence to best practices. E-health and mobile health technologies involving e-referrals, e-booking, decision support, and reminder systems are recommended for clinicians to manage and deliver appropriate care to patients as well as pregnant women to adhere to scheduled visits.
Keywords: prenatal care, care pathway modelling, maternal mortality, Zimbabwe
Introduction
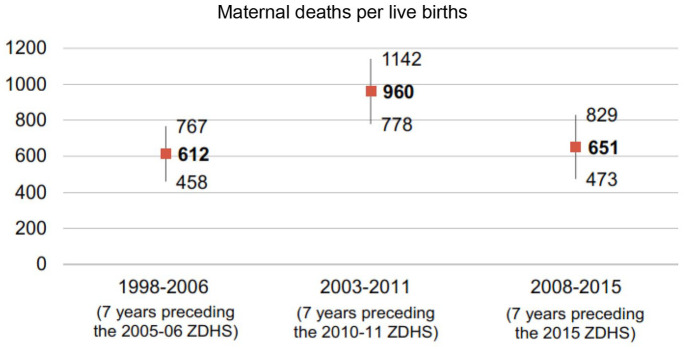
Maternal mortality remains a problem in low-income countries (LICs). In Zimbabwe, there has been an unprecedented increase in maternal mortality in the last 2.5 decades 1 (see Figure 1). As in many LICs, there is a heavy burden of high maternal, neonatal and child mortality when compared to middle and high-income countries. At its peak in 2011, maternal mortality ratio (MMR) was at 960/100 000 live births (Figure 1). At that time, Zimbabwe was amongst 40 countries in the world with high MMR 2 which attracted interest in the investigation reported in this paper. The goal was to identify service improvement areas in maternal care delivery pathway.
Figure 1.
Trends in maternal mortality ratios in Zimbabwe with confidence intervals. 3
Appropriate prenatal care is important in the early identification and mitigation of risk factors in pregnancy. The whole antenatal period is important for providing pregnant women with advice and support that are vital to their care and that of their infants. 4 An evidence-based quality ANC pathway has the potential to improve maternal and newborn health.5,6 For example, Bhutta et al 6 found that a carefully planned ANC pathway can be used to inform women about danger signs, symptoms and risks factors. This enables early interventions before adverse effects from diseases such as eclampsia, anaemia and gestational diabetes mellitus.7,8
Purpose, premise and objectives
The purpose of this study was to assess evidence-based prenatal care pathways that can be used to improve prenatal care in Zimbabwe. This centred on improving clinical workflow by modelling process workflow and identifying redundant practices as well as recommending the use of health technologies where repetitive and labour-intensive processes can be automated. The full model of the care delivery was first drafted in the form of prenatal care pathway guidelines based on literature on ANC delivery in low-income countries with specific emphasis on Zimbabwe.
This study was based on the premise that, the development and use of a ‘best-practice’ care pathway model can help to identify service improvement areas in prenatal care. This implies that process anomalies can be identified through prenatal care service evaluation using a model care pathway developed from literature and ‘best-practice’ guidelines. Specific objectives were:
(i) To establish the booking, referral and appointment processes involved in prenatal care delivery for pregnant women visiting the hospital
(ii) To establish trends of prenatal care visits made by pregnant women before pregnancy delivery
(iii) To establish documented care offered to pregnant women visiting prenatal care
(iv) To identify and model the system used to remind and follow up on pregnant women visiting prenatal care
(v) To identify discernible general care paths followed by pregnant women at hospital and compare them with a developed ‘best-practice’ model
Methods
This study was carried out at a Mpilo Central Hospital in Zimbabwe. It was a mixed methods study with retrospective medical record data and clinician interviews. There were 100 cases retrospectively reviewed. Both quantitative and qualitative data were collected, analysed and presented in this study.
Quantitative data collection
Quantitative data from records for women who delivered at MCH regardless of parity formed part of this study’s population. Simple random sampling was possible as the registry of maternity care records in which prenatal records reside were available and provided a census group of cases. We were not granted specific access to ALL prenatal records as some of the records where classified even within the batch that we were granted access to (ie, women who had delivered in 2015 by the end of the month of June). Additionally, as these were (then) current records we could not determine the total number of cases from which to select study subjects. File numbers were randomly generated from a spreadsheet for women who had delivered in 2015 from which 100 prenatal records were further randomly selected without replacement. One hundred records were chosen because these could be reviewed in the time available during this study, with a minimum margin of error. Randomisation was provided by the Health Information Office at MCH. They also anonymised the records by removing personally identifiable information before making them available to the researchers. To establish the types of screening information and related services offered to pregnant women, an audit of demographic, obstetric and social data as well as medical data, physical examinations, urine/blood tests, health promotion and documentation of care was made for the 100 cases reviewed. The audit recorded the existence of each item (ie, not frequency, eg, of tests).
Qualitative data collection
Interviews were used to collect qualitative data, targetting all qualified ANC clinicians in the ANC Department (nurses, midwives, obstetricians, gynaecologists, etc.). There were 40 ANC clinicians available. However, provisions of the Health Research Policy of the hospital stated that only 50% of the clinical staff complement would be available for research at each time for a permitted study (see Table 1; Mpilo Central Hospital, 2010). Therefore, 20 clinicians were offered to take part in the study. None declined the invitation, thus 20 provided their consent and participated in one-to-one semi-structured interviews.
Table 1.
Distribution of clinician type amongst the interviewees.
| Sample and respondents | Clinicians at MCH’s ANC* | Clinicians interviewed | Clinicians not interviewed | |||
|---|---|---|---|---|---|---|
| Type of clinician | No. | % (n/40) | No. | % (n/20) | No. | % (n/20) |
| ANC Matron | 1 | 2.5 | 1 | 5 | 0 | 0 |
| ANC Deputy Matron | 1 | 2.5 | 1 | 5 | 0 | 0 |
| ANC Midwife | 13 | 32.5 | 11 | 55 | 2 | 10 |
| ANC Nurse | 20 | 50 | 2 | 10 | 18 | 90 |
| Gynaecologist | 3 | 7.5 | 3 | 15 | 0 | 0 |
| Obstetrician | 2 | 5 | 2 | 10 | 0 | 0 |
| Grant Totals | 40 | 100 | 20 | 100 | 20 | 100 |
Represents clinicians at the time of conducting the study (July-August 2015).
Using a Minimum Set of Tests (see Table 3), the ANC clinicians were asked whether the table reflected their daily experience in terms of providing scheduled routine prenatal care to pregnant women at specific stages during their pregnancy. Their responses were recorded and are presented to reflect the opinions of the clinicians in Table 3. They were also asked about the methods they use to deliver health promotion material. The results are presented in Table 4.
Table 3.
Care delivered to pregnant women visiting prenatal care: comments on minimum tests carried out by maternity care clinicians.
| Minimum set of tests | Timing | Comment |
|---|---|---|
| Blood pressure | All routine appointments | Carried out routinely |
| Urine test for proteinuria | All routine appointments | Should be carried out routinely but there is a shortage of Uri-sticks for carrying out tests |
| Blood group and rhesus D status | At booking | Carried out routinely *Note the discrepancy with records review data |
| Haemoglobino pathies screen | At booking | Not done |
| Hepatitis B virus screen | At booking | Not done |
| HIV screen | At booking | Carried out routinely |
| Rubella susceptibility | At booking | Not done |
| MSU for asymptomatic bacteriuria | At booking | Not done |
| Height, weight and body mass index | At booking | Should be done but the measuring equipment currently not available |
| Haemoglobin | At booking and 28 wk | Carried out once *Note the discrepancy with records review data |
| Ultrasound scan to determine gestational age | Between 10 wk 0 d and13 wk 6 d | Not done |
| Down’s syndrome screen |
Combined test: between 10 and
14 wk Serum quadruple test: 14-20 wk |
Not done |
| Ultrasound screen for structural anomalies | Between 18 wk 0 d and 20 wk 6 d | Normally not done – but can be outsourced for patients with special complications |
| Measure of symphysis–fundal height | Not done *Note the discrepancy with records review data | |
| Foetal presentation | All routine appointments from 25 to 36 wk |
Carried out routinely from the third visit for women first visiting at 10-15 wk |
Table 4.
Clinicians’ methods of providing health promotion material to pregnant women.
| Questions | Yes | No | ||
|---|---|---|---|---|
| n | % | n | % | |
| The Internet | 1 | 5 | 19 | 95 |
| Lecture presentations | 20 | 100 | 0 | 0 |
| Individual discussions | 17 | 85 | 3 | 15 |
| Pamphlets | 8 | 40 | 12 | 60 |
| Do women ask you about information they have seen/read over the internet? | 6 | 30 | 14 | 70 |
| Social media | 4 | 20 | 16 | 80 |
| 3 | 15 | 17 | 85 | |
| In-house television | 0 | 0 | 20 | 100 |
| Other content | 0 | 0 | 20 | 100 |
Tools used in data collection
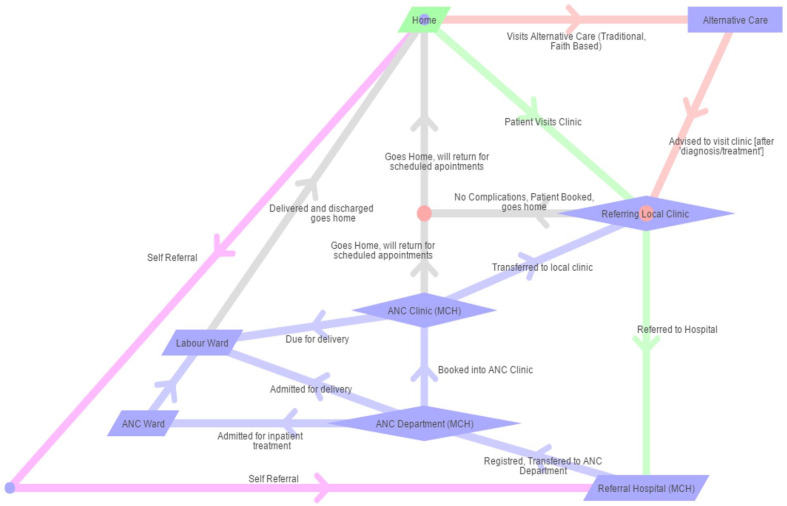
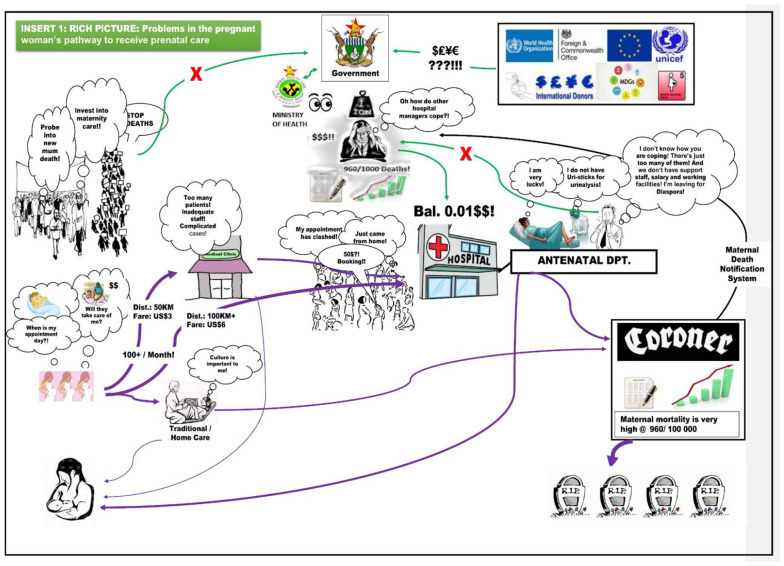
Care pathway modelling and systems thinking theory was used to assist in data collection. This was done by using concepts and techniques such as Care Pathway Modelling (CPM) theory 9 and creating rich pictures using Checkland and Poulter’s 10 (2006) Soft System Methodology (SSM). A rich picture was used during interviews to illustrate and validate preliminary findings through a high-level overview of prenatal care delivery at the hospital (Appendix B). This iterative process of getting back to the study participants, as well as the vivid nature of rich pictures were key justifications of SSM application. 11 A discussion with the head clinicians (who were part of the 20 interviewees, see Table 1) was carried out using this technique and was supportive as it uncovered subtle issues often overlooked in care delivery. Based on discussions with clinicians and available material from reviewing patient records, a pregnant women’s antenatal care pathway was also demonstrated using Network Tools for Intervention Modelling with Intelligent Simulation (NETIMIS) (Network Tools Network Tools for Intervention Modelling with Intelligent Simulation [NETIMIS] is a web-based software tool which uses intelligent simulation to visually explore the way in which organisations deliver care pathways. The software was developed by a UK-based health technology company, X-Lab: https://www.x-labsystems.co.uk/WhatsGoingOn/160318/ [Last accessed 20-October-2021]). This revealed the ‘spaghetti’ nature of the routes taken by a pregnant woman seeking maternity care. These tools were supportive in generating ideas for understanding the prenatal care pathway better as well as pointing to possible improvement areas.
Permission and ethics
Permission to conduct the study was granted by the Mpilo Central Hospital Board. The Medical Research Council of Zimbabwe reviewed and granted ethical approval to conduct this study under reference MRCZ/B/897. A similar review by the University of Leeds, School of Medicine Research Ethics Committee was also done, and ethical approval was granted under reference SoMREC/14/095.
Results
Profile of maternity care records and participants interviewed
From the 100 maternity case records reviewed, the ages of women recorded ranged from 17 to 40 years, with mean age of 24.2 years. Only 15% of the women were employed, 8% were self-employed and 62% were unemployed whilst employment status was not recorded on 15% of the records. Of these 100 cases, 65% were married, 15% were unmarried and the marital status was not indicated in 20% of the cases. It was the first pregnancy for 76%, the second pregnancy for 15% and the third and fourth pregnancy for 9% of these 100 cases.
All the expected 20 clinicians took part in the study through interview sessions. The distribution according to clinician type is shown in Table 1. As shown, more than half of the 20 interviewees (55%) were ANC midwives. This was a good representation of clinicians in the ANC department considering that, the other 20 who were not interviewed were largely ANC nurses (Table 1).
Booking status and missing of booked appointments
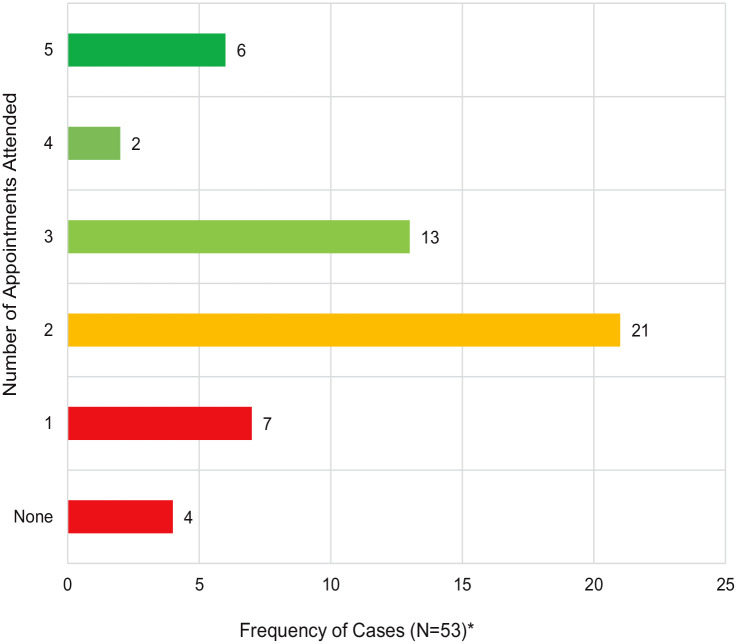
After reviewing the 100 records, it was established that 47 (47%) had not booked for prenatal care whilst 53 (53%) had booked. Missing of scheduled prenatal care appointments was also prevalent in these 53 cases, with only 11% (n = 6) having attended all the expected 5 visits whilst 60% (n = 32) missed 3 or more (Figure 2).
Figure 2.
Number of attended appointments, depicting the missed appointments in the 53 booked cases.
*Actual number of women who attended.
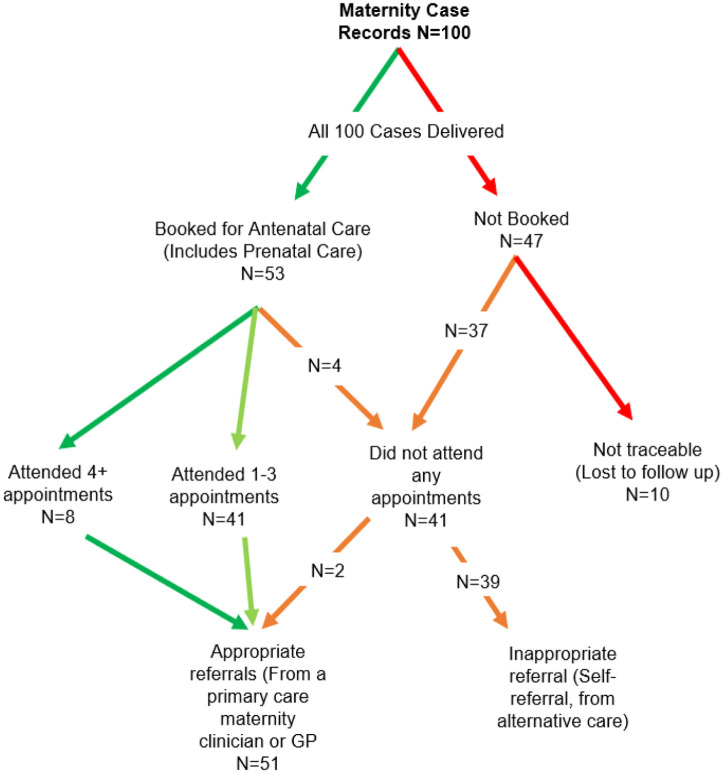
A decision tree was used to model the booking, appointment visits and referral paths followed by pregnant women from the 100 maternity case records analysed (Figure 3). This brought out new insights particularly on the relationship between appropriate referrals, booking and adherence to scheduled appointments.
Figure 3.
Booking, appointment visits and referral paths for delivery from the 100 maternity case records reviewed.
Analysis of prenatal care visits: The first visit
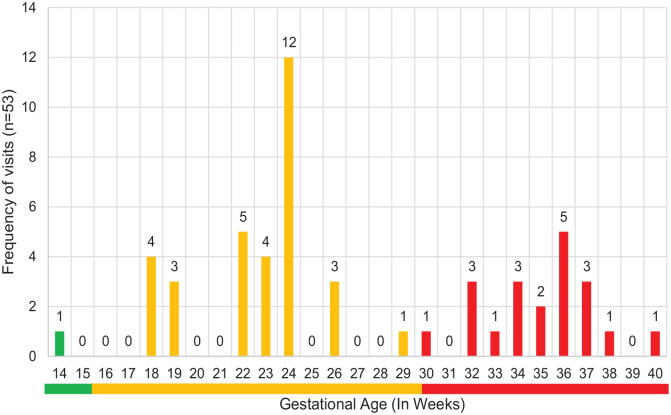
Another key element investigated in determining the improvement areas in the pregnant woman’s care pathway was their gestational age at first visit to receive care. In 100 maternity case records, 53 booked for prenatal care, whilst 47 did not (Figure 3). Of the 53 who booked, they arrived late for their first visit at an average gestational age of 27.1 weeks with extremes of 30 to 40 weeks in 38% cases (Figure 4).
Figure 4.
Gestational age distribution at first visit to receive prenatal care.
N = 53, Mean = 27.1, Mode = 24 and Median = 24.
Reasons often given for missing appointments by women
Clinicians were further asked to state the reasons for missing scheduled appointments given by women. There were various responses which have been grouped into the main themes from the interviews. This provides a detailed account of what the clinicians thought were the reasons why women miss scheduled appointments. One of the main issues was related to costs. The booking fee and the cost of travel to the hospital were key costs areas that prohibit women from visiting the hospital. This was exacerbated by the fact that the hospital serviced a large rural community that live in over a 100 km radius and the distances extends the cost of travelling to access maternity care. Another issue is related to missing appointments because there were no effective ways to remind women when their next appointments are due. Some women with booked appointments ‘just need to be reminded. The dates are far apart, so they tend to forget. We write the dates of their next visits on their hand-held notes but some of them still forget anyway so reminders are required’ (Respondent 16 – see Table 2). Additionally, the use of (often risky) alternative care such a faith-based care and untested traditional systems were also reported as prevalent. Thus, in summary, clinicians attributed prenatal booking fees in the background of poverty and poor family support systems as key factors hindering women’s access to prenatal services. This is made worse by the long distances to the health facility, and the use of risky alternative care and cultural influences.
Table 2.
Reasons for low visits and missing appointments.
| Themes | Data |
|---|---|
| Cost – Booking – Medications – Services – Transportation |
Respondent 4:
Transport costs are a hindrance. As a referral
centre, we cover quite a large area and most mothers in
rural and remote areas have to travel long distances as
trained clinicians are not available in their local
areas or usually, they would have been referred or
having complications. It costs
US$6
to travel a distance of over
100 km
and some of them
cannot afford
to pay that much for all the required 5-6 visits
during the course of their pregnancy
Respondent 6: Some women just come here to register for their pregnancy only, they do not want to come for regular check-ups. Perhaps they view them as unimportant or do not want to pay the ANC booking fee of US$50 which we currently charge. Respondent 12: Money and cost of care. We charge US$50 to book for pregnancy care and most women do not afford this so they tend to have one visit to just register for delivery and go away. It is sad because some of them die as they are not regularly checked. Respondent 13: Women miss appointments for various reasons. Cost , family commitments and attendance to alternative care, sometimes traditional, home-based care and faith-based care. So, you find that you register one woman here, but they are receiving care elsewhere where they are not paying, or it is cheaper. Respondent 14: Transport costs to visit the hospital for the rural women is a big hindrance. I have a case of one mother who had complications and was supposed to have regular visits but could not afford as she was travelling from Insiza. It is about 100 km from here and she could not keep travelling to and from as this was costing her. We had to refer her to Gweru, but the transport cost is almost the same anyway! Respondent 18: They don’t have money to pay for booking as the second visit is normally for booking. You see, they come for first visit, and we encourage them to pay for their pregnancy care booking for the other appointments so that is why they do not come. |
| Reminders |
Respondent 16:
Some women miss appointments because they
just
need to be reminded
. The dates are far apart, so they tend to
forget. We write the dates of their next visits on their
hand-held notes but some of them still forget anyway so
reminders are required
Respondent 17: We write their next dates on their hand-held notes. Some of them lose them so they will be unsure of the dates . Some of them just forget. It is common that they come on the wrong dates, you just have to accommodate them, what can you do? |
| Alternative care |
Respondent 3:
Cultural reasons. Some mother come on their own on
the first visit. When they then discuss the issue with
their husbands, some of them end up not coming as they
prefer to visit their
faith-based care
. This is common among the
apostolic religion members
. What can you do in such
circumstances?
Respondent 13: Women miss appointments for various reasons. Cost, family commitments and attendance to alternative care, sometimes traditional, home-based care and faith-based care . So, you find that you register one woman here, but they are receiving care elsewhere where they are not paying, or it is cheaper. |
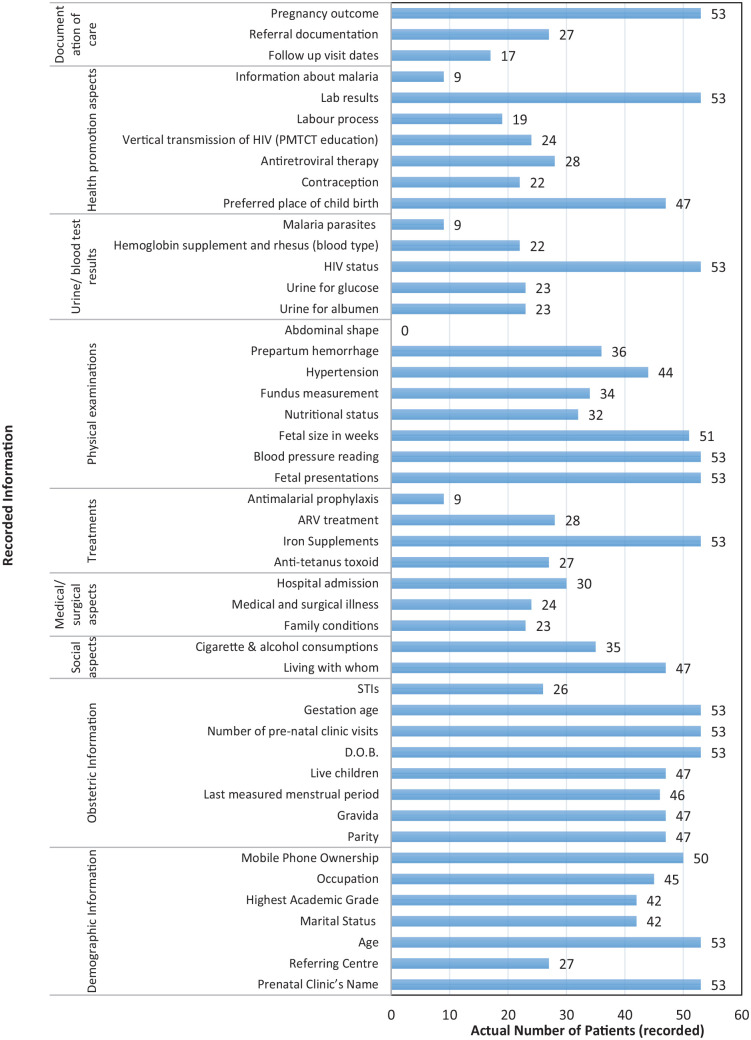
Care delivered to pregnant women visiting prenatal care
Figure 5 shows the types of screening information and related services offered to pregnant women. This covers demographic, obstetric and social data as well as medical data, physical examinations, urine/blood tests, health promotion and documentation of care delivered to pregnant women at MCH.
Figure 5.
Documented care delivered to pregnant women visiting prenatal care (n = 53).
In terms of routine scheduled prenatal care, clinicians also provided information based on their experiences. They commented on whether care is delivered on each of the items in the Minimum Set of Tests that should be carried out at various stages of pregnancy. Their responses were recorded and are presented Table 3. They show some of the missed investigations as well as challenges in delivering scheduled care, such as absence of required resources.
Concerning the promotion of good health practice, maternity care clinicians preferred to use lecture presentations and individual discussions compared to online-based options when delivering antenatal care information to pregnant women (Table 4).
In terms of continuity of high quality, prenatal care there appeared to be a shortage of specialised maternity care staff and a trained ANC clinician (Table 5) may not always attend to women. Notably, spousal support was highly encouraged.
Table 5.
Guidelines for continuity of care during pregnancy.
| Questions | Yes | No | ||
|---|---|---|---|---|
| n | % | n | % | |
| Have you ever encouraged prenatal care appointment attendance by the husband or family member of a pregnant woman? | 19 | 95 | 1 | 5 |
| Is it always possible to transfer a pregnant woman without complications back to primary care maternity services that are closer to their residential community? | 5 | 25 | 15 | 75 |
| Do you think the number of specialists (eg, midwives, gynaecologists, obstetricians) available at MCH is enough to attend to women on each key prenatal care visit? | 6 | 30 | 14 | 70 |
| In your experience, does a trained clinician always attend to a pregnant woman during their pre-natal care visits in the ANC? | 4 | 20 | 16 | 80 |
Overview of the prenatal care pathway
Patient’s journey and the external environment
Considering the data presented so far, a rich picture (Checkland and Poulter 2006) was developed to display the general scenario of the path followed by pregnant women visiting MCH to receive full ANC (Appendix B). This had earlier on been developed as part of the finding out stage of the broader intended research and was updated to represent the research findings. It details the problematic situation from both the internal patient’s journey and the broader political and global influences on the situation. This tool was intended to provide a general overview of the pathway and the range of challenges faced.
Patient pathway: The ‘Spaghetti’ outlook
For a more vivid visualisation of a pregnant woman’s trail without competing external influences (as in the rich picture), NETIMIS was used to model the pathway particularly focussing on prenatal care and showing the referral points (Appendix A). It depicts the haphazard nature of primary care and how these pathways form a sort of ‘spaghetti’ system that requires streamlining to avoid congestion or inappropriate referrals (for instance, cases that could have been dealt with at primary care). It shows that the woman has choices to visit secondary care by self-referral, primary care clinician referral and referral from alternative care (alternative care in the Zimbabwean context is other form of non-conventional care offered by persons who have not been formally trained and attested to medical practice).
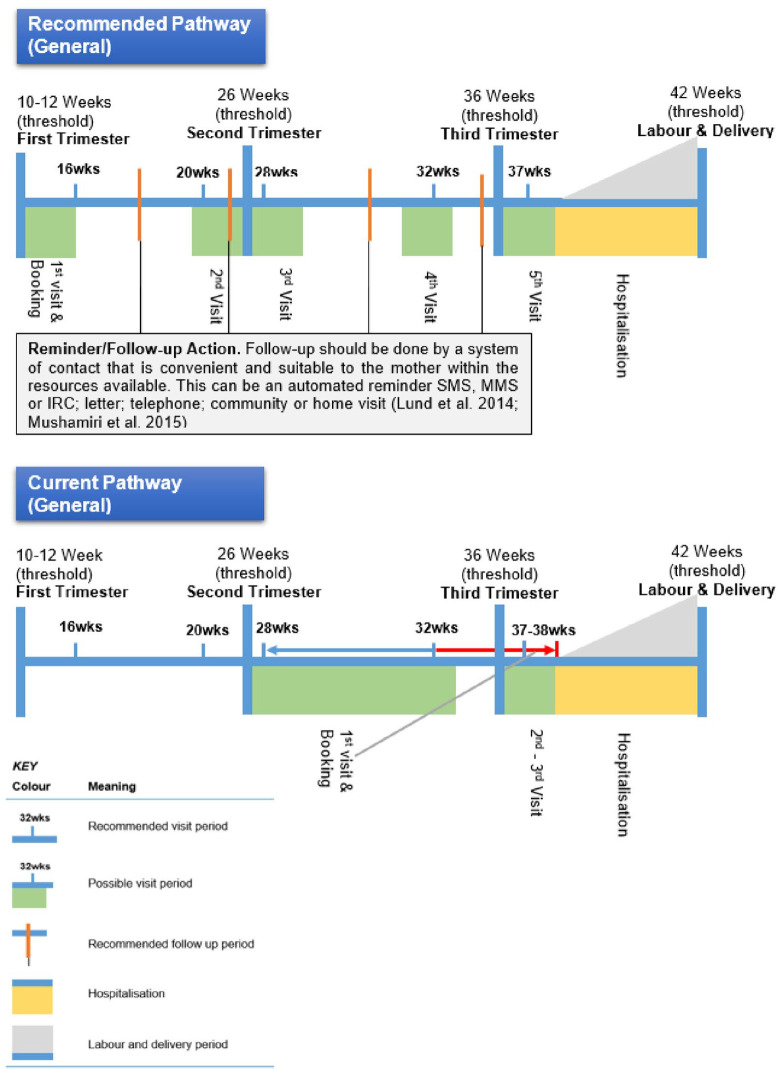
Pregnancy timeline: Recommended and current pathway scenarios
A pathway based on data analysed and presented so far and displayed on a woman’s pregnancy timeline (the 3 trimesters). The proposed ‘ideal’ pathway based on the developed guidelines was compared to the current pathway to identify and illustrate the areas that need attention. As shown in Figure 6, late visits are a key challenge that need to be addressed.
Figure 6.
Prenatal care pathway: comparisons between the guideline and current scenarios.
Discussion
Few visits and late attendance to ANC by pregnant women
ANC records assessment showed that 47% (n = 47) of the 100 cases of pregnant woman studied did not book for prenatal care whilst 53% (n = 53) did. Of the 53 cases of women who attended prenatal care, gestational age (GA) at first visit averaged 27.1 weeks with the most frequent GA being 24 weeks. This shows a huge gap from the expected first time visit of 10 to 15 weeks (WHO).3,12,13 Women who did not attend prenatal care (n = 47) and those coming late for prenatal care at 30 weeks or later (20/100) were at high risk of undetected complications such as anaemia, pre-eclampsia and gestational diabetes mellitus.7,8 Follow ups of ANC patients were also not being made. Follow-ups have been reported to significantly increase adherence to prenatal visits with positive outcomes especially in early identification of pregnancy risks.14-16
Cost of antenatal care
Clinicians attributed the cost of prenatal booking fees in the background of poverty and poor family support systems as key factors hindering women’s access prenatal services. The cost of receiving antenatal care from state, church and privately-run clinics and hospitals in Zimbabwe is unpredictable and mirrors the unstable economic and political environment they exist. At the time of this study, participants reported that charges range between $40 and $50, a significantly high figure even by the standards in Sub-Saharan Africa. Similar charges, ranging between US$35 and US$60 were also reported by other sources such as state media (https://www.herald.co.zw/medical-consultation-fees-up-100pc/), lobby groups (https://www.one.org/us/2017/09/14/maternity-clinic-zimbabwe-foreign-aid/) and World Bank reports (http://www.worldbank.org/en/news/feature/2012/11/30/in-rural-zimbabwe-no-fees-better-care-for-women-children). This study also found that the low status of women in society, distance to the health facility, risky alternative care and cultural influences were emphasised as key hindrance factors. Interviewed nurses reported that the women are very often committed with job-related activities, which may explain the case of women who would have booked and paid for care, but still missed 3 or more scheduled appointments (32 women, see Figure 2).
Documentation and the absence of an electronic tracking system
Paper records were the key mode of referral, registration and booking of antenatal appointments. This appeared to be a problem considering the cumbersome nature of the paper files and the difficulty of constant reference to them especially – to schedule, track or monitor appointment adherence. Also, by using a paper referral system, there was a disjointed relationship between the ANC Department at MCH and the primary care services that make referrals of pregnant women. A follow up on patient referrals and transfers would be easier with electronic tracking. Clinicians indicated that they require an e-booking and e-referral system that allows several functionalities such as tracking of referrals, appointments and automated reminders to women, all of which the current paper system cannot achieve effectively. This is a prerequisite for best practice in prenatal care.
Inadequate care delivered at each visit
Data analysed on specific care delivery areas provided important insights into the improvements required in optimising care delivery at MCH. Fundus measurements were only reported in 34 of the 53 (64%) cases of women who had booked and visited prenatal care. Surprisingly, foetal size in weeks had been indicated in almost all (51, 96%) of the records (see Figure 5). According to Chaibva et al 7 determining foetal sizes in weeks, without taking any fundus measurements, might amount to guess work. Urine test results for albumen and glucose were recorded in 23 (43%) of the 53 cases only (also see Figure 5). According to Choudhary 17 , these tests are necessary in determining danger signs for diabetes mellitus and eclampsia. Information about haemoglobin levels was only recorded in 22 of the 53 (41%) records. Haemoglobin levels need to be monitored as this informs requirements for nutrient supplements necessary particularly iron and is of course especially important for pregnant women prone to anaemia. 4 Considering the frequency of key data missed on physical, surgical and obstetric tests and assuming that this was care delivered, it appears that assistance to care delivery using decision support and reminder systems for the clinicians during each care session with a pregnant woman may be beneficial. Studies on the use of electronic decision support systems for improving compliance to maternity care protocols18-20 indicate that in sub-Saharan Africa, e-health technology can bridge the ‘know-do gap’ and has potential for improving the quality of maternal care. This includes the treatment of diseases, including HIV-AIDS, 21 and Malaria treatment. 22
Inadequate methods of health promotion
Maternity care clinicians preferred to use lecture presentations and individual discussions compared to online-based options when delivering antenatal care information to pregnant women (Table 4). The information and advice need of women increase during pregnancy. Shaw et al 23 studied patient access to a web based personalised ANC Record and showed in a randomised control trial that the mean number of log-ins to a web based personalised ANC Record was 10.4 (SD 17.8, n = 97) whereas for the group in which general information was provided, it was 1.8 (SD 1.4, n = 96) (P < .001). Therefore, for the entire 11 months period of that study, personalised ANC information was accessed almost 6 times more than when general pregnancy information alone was provided. In another cluster randomised control trial, Jareethum et al 24 studied prenatal care support using SMS messages and showed that satisfaction levels of the women in the intervention group were higher than those who did not receive the messages both in the antenatal period (9.25 vs 8.00, P < .001) and during labour (9.09 vs 7.90, P = .007). They also found out that in the SMS using group, the confidence level was higher (8.91 vs 7.79, P = .001) and the anxiety level was lower (2.78 vs 4.93, P = .002) than the control group. Therefore, MCH departments can potentially improve their health promotion efforts through electronic health information delivery channels.
All of the interview participants (n = 20) indicated that there was currently no systematic way of reminding pregnant women to attend the minimum 5, goal-oriented appointments. Only 4 of the 20 respondents indicated that they discussed the next review dates. In addition, all the participants pointed out that they write the next review dates on the patients’ ANC handbook with the expectation that the women would read this to remind them of their next appointment. However, this information was poorly recorded, with only 17 of the 53 cases reviewed in this study showing follow updates (Figure 5). All the participants also indicated that they did not use any electronic or telecommunication system such as telephone, SMS, MMS or the commonly used WhatsApp messaging application to remind women to attend prenatal care despite the prevalence of missed appointments. Here again, opportunities to increase the number of pregnant women in the care pathway were being missed. Ngabo et al 25 showed how a simple mobile SMS system was used to monitor and follow up on 11 502 pregnancies within a year in a low resource country. They also found a positive result on adherence to booking and appointments. This is shown by an increase in facility-based delivery from 72% 12 months before to 92% at the end of the 12 months pilot phase.
Challenges in the prenatal care pathway
Looking at the pregnancy timeline pathway (Figure 6) was insightful by comparing the recommended and current scenarios. MCH uses a focussed and goal-oriented approach to deliver prenatal care by streamlining the number of visits to 5 goal-oriented visits, one of which is the initial risk assessment, health education and delivery plan visit and the others distributed after the first trimester. Several empirical studies using randomised controlled trials in low resource countries support the use of 5 goal-oriented visits over more visits.12,13,26,27 However, this study shows that there is a huge discrepancy between the expected visits, those actually attended by pregnant women and the timing of the attendance. Of the 53 pregnant women who booked to receive care, most of them came late (at an average GA of 27.1 weeks, n = 53) and had fewer visits, with many attending 0 to 3 visits only (45 of the 53 booked cases reviewed) (Figure 2).
Considering the late visits reported in this study and in several other related studies in LICs,15,16,28-30 it is doubtful that the reduced visits model is ideal where pregnant women are already attending fewer appointments. In fact, Dowswell et al’s 31 Cochrane review findings buttresses this notion, with evidence that in settings with limited resources, where the number of visits is already low, programmes of ANC with reduced visits are associated with an increase in perinatal mortality. Whilst visiting prenatal care early is highly recommended in this study, a more flexible pathway allowing more visits, from the time a pregnant woman books for prenatal care (the average of which is 27.1 weeks in this study) is also suggested as it potentially enables more attention to those women who come late. However, at the current study’s stage, this is a tentative suggestion, and more evidence is required. Critically reflecting on the methods used in this study, a longitudinal study that gathers more evidence and follows up on patient outcomes could provide strengthening evidence to the insights muted by this study.
A glance of the rich picture that details a broader view of the prenatal care journey for pregnant women exhibits complexities in the care delivery models that are underway at MCH within broader socio-economic, political and global environment. Combining this with causal loop projections tend to indicate the need for investment into both e-health technologies (particularly e-referral and reminder systems) and hospital capacity. The education of women and consideration of cultural issues are also salient and highlighted in this pathway. However, key to all this is that a clear and evidence-based ANC strategy, accompanied by pathway guidelines is required.
In addition, the ‘spaghetti’ outlook of the NETIMIS model depicts the haphazard nature of the broader health care delivery system in Zimbabwe. It also shows how this requires streamlining to avoid congestion and inappropriate referrals for prenatal care. Currently, the deficiency is that the care delivery systems between primary and secondary care have no guidelines for patient pathways for ANC. Evidence-based care pathway guidelines such as those developed in this study are recommended here. This together with buy-in and monitoring from the top level Ministry of Health and Child Care, and reduced booking costs for women with limited resources should ensure adherence to a more orderly and traceable pathway.
Recommendations and Conclusions
Key findings and suggestions for future work
At policy level, Ministry of Health and Child Care is recommended to create evidence-based care pathway for maternity care. This implies that further assessment of evidence for the effectiveness of the current regime of maternity care is required. For instance, our single case study finds that it is doubtful that the reduced visits model is ideal where women are already attending fewer appointments.
More research is required to create national guidelines for maternity care as this can improve prenatal care uptake. Prenatal care uptake has been reported to improve outcomes of care delivery. 16
At national level, Ministry of Health and Child Care is also recommended to adopt a mobile health strategy for following up on women so that they adhere to the already streamlined 5 focussed care prenatal care visits. A simple automated SMS reminder system has brought substantial benefits to adherence in similar care settings. 25 On the same point, among reasons for missing appointments – distance to the health facility was one of the most hindrance factors (noted by 75% of the clinicians). Therefore, the availability of trained clinicians in local areas is one of the key factors for better quality.
onsidering the frequency of missing key data on physical, surgical and obstetric tests, a checklist system for the clinicians during each care session with a pregnant woman, along with regular auditing of data facilitated by an electronic system would likely improve care.
MCH as well as the Ministry of Health and Child Care are further recommended to scale up the education of women, particularly on the importance of prenatal care using targetted and more personalised solutions which can be enabled by mobile technologies as most women already own and use mobile phones.
MCH is recommended to utilise evidence from this and related studies to write a convincing business case for deploying a clinical information system that supports electronic health records, clinical decision support and electronic referral. This can improve care delivered to women and reduce the paper trail that makes it difficult to follow up women, especially those that disappear along the pathway.
Appendix
Appendix A.
NETIMIS illustration of the possible pregnant women’s pathways.
Appendix B.
Rich picture – problems in the pregnant woman’s pathway to receive prenatal care.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Fraser was a Marie Skłodowska-Curie Fellow, funded from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 661289: ‘Global eHealth’.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: RD conceptualised the research, collected and analysed data. RE and HF were supervisors of this research. They contributed to interpreting data analysis, article writing and multiple revisions.
Ethical Approval/Patient Consent: Permission to conduct the study was granted by the Mpilo Central Hospital Board. The Medical Research Council of Zimbabwe reviewed and granted ethical approval to conduct this study under reference MRCZ/B/897. A similar review by the University of Leeds, School of Medicine Research Ethics Committee was also done, and ethical approval was granted under reference SoMREC/14/095.
ORCID iD: Rodreck David  https://orcid.org/0000-0002-0546-765X
https://orcid.org/0000-0002-0546-765X
References
- 1. Dodzo MK, Mhloyi M. Home is best: why women in rural Zimbabwe deliver in the community. PLoS One. 2017;12:e0181771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. United Nations in Zimbabwe. Maternal Mortality in Zimbabwe: Evidence, Costs, and Implications. Office of the UN Resident Coordinator; 2013. [Google Scholar]
- 3. Zimbabwe National Statistics Agency and ICF International. 2016. Zimbabwe Demographic and Health Survey 2015: Key Indicators. Rockville, Maryland, USA. Accessed November 23, 2021. https://zimbabwe.unfpa.org/sites/default/files/pub-pdf/ZDHS%20Preliminary%20Results.pdf [Google Scholar]
- 4. World Health Organisation. 2016. WHO recommendations on antenatal care for a positive pregnancy experience. Accessed October 6, 2021. https://www.who.int/publications/i/item/9789241549912 [PubMed]
- 5. Bergman DA. Evidence-based guidelines and critical pathways for quality improvement. Pediatrics. 1999;103:225-232. [PubMed] [Google Scholar]
- 6. Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics. 2005;115:519-617. [DOI] [PubMed] [Google Scholar]
- 7. Chaibva CN, Ehlers VJ, Roos JH. Audits of adolescent prenatal care rendered in Bulawayo, Zimbabwe. Midwifery. 2011;27:e201-e207. [DOI] [PubMed] [Google Scholar]
- 8. Ndaboine EM, Kihunrwa A, Rumanyika R, Im HB, Massinde AN. Maternal and perinatal outcomes among eclamptic patients admitted to Bugando medical centre, Mwanza, Tanzania. Afr J Reprod Health. 2012;16:35-41. [PubMed] [Google Scholar]
- 9. Schrijvers G, van Hoorn A, Huiskes N. The care pathway: concepts and theories: an introduction. Int J Integr Care. 2012;12:e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Checkland P, Poulter J. Learning for action: a short definitive account of soft systems methodology and its use for practitioner, teachers, and students. Chichester: Wiley; 2006. [Google Scholar]
- 11. Bell S, Morse S. How people use rich pictures to help them think and act. Syst Pract Action Res. 2013;26:331-348. [Google Scholar]
- 12. Villar J, Carroli G, Khan-Neelofur D, Piaggio G, Gülmezoglu M. Patterns of routine antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2001;4:CD000934. [DOI] [PubMed] [Google Scholar]
- 13. Majoko F, Munjanja S, Nyström L, Mason E, Lindmark G. Randomised controlled trial of two antenatal care models in rural Zimbabwe. BJOG. 2007;114:802-811. [DOI] [PubMed] [Google Scholar]
- 14. Lund S, Nielsen BB, Hemed M, et al. Mobile phones improve antenatal care attendance in Zanzibar: a cluster randomized controlled trial. BMC Pregnancy Childbirth. 2014;14:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hagey J, Rulisa S, Pérez-Escamilla R. Barriers and solutions for timely initiation of antenatal care in Kigali, Rwanda: health facility professionals’ perspective. Midwifery. 2014;30:96-102. [DOI] [PubMed] [Google Scholar]
- 16. Mushamiri I, Luo C, Iiams-Hauser C, Ben Amor Y. Evaluation of the impact of a mobile health system on adherence to antenatal and postnatal care and prevention of mother-to-child transmission of HIV programs in Kenya. BMC Public Health. 2015;15:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Choudhary P. Eclampsia: a hospital based retrospective study. Kathmandu Univ Med J. 2003;1(14):237-241. [PubMed] [Google Scholar]
- 18. Blank A, Prytherch H, Kaltschmidt J, et al. “Quality of prenatal and maternal care: bridging the know-do gap” (QUALMAT study): an electronic clinical decision support system for rural Sub-Saharan Africa. BMC Med Inform Decis Mak. 2013;13:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Horner V, Rautenbach P, Mbananga N, Mashamba T, Kwinda H. An e-health decision support system for improving compliance of health workers to the maternity care protocols in South Africa. Appl Clin Inform. 2013;4:25-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dalaba MA, Akweongo P, Williams J, et al. Costs associated with implementation of computer-assisted clinical decision support system for antenatal and delivery care: case study of Kassena-Nankana district of northern Ghana. PLoS One. 2014;9:e106416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oluoch T, Katana A, Ssempijja V, et al. Electronic medical record systems are associated with appropriate placement of HIV patients on antiretroviral therapy in rural health facilities in Kenya: a retrospective pre-post study. J Am Med Inform Assoc. 2014;21:1009-1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zurovac D, Talisuna AO, Snow RW. Mobile phone text messaging: tool for malaria control in Africa. PLoS Med. 2012;9:e1001176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shaw E, Howard M, Chan D, et al. Access to web-based personalized antenatal health records for pregnant women: a randomized controlled trial. J Obstet Gynaecol Can. 2008;30:38-43. [DOI] [PubMed] [Google Scholar]
- 24. Jareethum R, Titapant V, Tienthai C, Viboonchart S, Chuenwattana P, Chatchainoppakhun J. Satisfaction of healthy pregnant women receiving short message service via mobile phone for prenatal support: a randomized controlled trial. Med J Med Assoc Thai. 2008;91:458. [PubMed] [Google Scholar]
- 25. Ngabo F, Nguimfack J, Nwaigwe F, et al. Designing and implementing an innovative SMS-based alert system (RapidSMS-MCH) to monitor pregnancy and reduce maternal and child deaths in Rwanda. Pan Afr Med J. 2012;13:31. [PMC free article] [PubMed] [Google Scholar]
- 26. Munjanja SP, Lindmark G, Nyström L. Randomised controlled trial of a reduced-visits programme of antenatal care in Harare, Zimbabwe. Lancet. 1996;348:364-369. [DOI] [PubMed] [Google Scholar]
- 27. Carroli G, Villar J, Piaggio G, et al.; WHO Antenatal Care Trial Research Group. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357:1565-1570. [DOI] [PubMed] [Google Scholar]
- 28. Myer L, Harrison A. Why do women seek antenatal care late? Perspectives from rural south africa. J Midwifery Womens Health. 2003;48:268-272. [DOI] [PubMed] [Google Scholar]
- 29. Simkhada B, Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. 2008;61:244-260. [DOI] [PubMed] [Google Scholar]
- 30. Kisuule I, Kaye DK, Najjuka F, et al. Timing and reasons for coming late for the first antenatal care visit by pregnant women at Mulago hospital, Kampala Uganda. BMC Pregnancy Childbirth. 2013;13:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2010;10:CD000934. [DOI] [PMC free article] [PubMed] [Google Scholar]