Abstract
Background:
Limited attention has been paid to the natural history, management, and treatment outcomes related to the posterior cruciate ligament (PCL)–deficient knee joint.
Purpose:
To perform a comprehensive bibliometric analysis to evaluate the 50 top-cited articles in PCL research.
Study Design:
Cross-sectional study.
Methods:
We performed a keyword-based search in the Thomson Reuters Web of Science to generate a list of the 50 most cited articles relevant to the PCL. The included articles were analyzed according to journal, country of origin, publication year, total number of citations, citations per year, citation trends, and type of study (clinical vs basic science).
Results:
The 50 top-cited articles were published between 1975 and 2012, and the number of individual article citations ranged between 98 and 410. The listed articles were published in 7 journals, with the American Journal of Sports Medicine contributing to more than half of the articles and citations. The United States contributed the most articles (84%) and citations (n = 4873). There were 32 clinical studies and 18 basic science studies. All clinical studies had level 4 clinical evidence, and topics included the natural history of PCL tears, factors predicting the need for surgical intervention, and long-term outcomes of isolated PCL injuries and combined capsuloligamentous injuries. Most (77.8%) of the top-cited basic science articles consisted of experimental or biomechanical studies on human cadaveric knees.
Conclusion:
The current analysis suggests that PCL research is still evolving and needs high-quality prospective evidence to establish sound recommendations.
Keywords: top-cited, bibliometric analysis, PCL, posterior cruciate ligament, sports medicine
The posterior cruciate ligament (PCL) is the primary posterior stabilizer of the knee joint. The PCL is the largest and strongest ligament of the knee joint, intra-articular but extrasynovial in location. 25 The ligament plays multiple functions besides anteroposterior stabilization, including a supplementary role in rotational, varus, and valgus stresses. 29 Traffic accidents and athletic injuries are the most common causes of PCL injury. 46 The majority of PCL injuries (>60%) are associated with additional capsuloligamentous injuries, of which posterolateral corner (PLC) injuries are the most common. 26 Isolated PCL injuries are uncommon, with an estimated annual incidence of 2 per 100,000 people. 45 With the majority of attention being focused on anterior cruciate ligament (ACL) and meniscal injuries, limited evidence is available concerning the natural history and outcomes of a PCL-deficient knee joint. 56 The overall incidence rate of PCL injuries, although relatively low compared with that of ACL injuries, is rising with increased sports participation. Thus, orthopaedic surgeons need to be well versed in evolving concepts, especially anatomy, function, biomechanics, and treatment options for PCL injuries, to achieve favorable results.
With the increasing evidence on management of PCL injuries, a focus on the top-cited literature can highlight the relevant concepts and trending PCL-related research. Such a focus can also help determine the deficiencies and conflicting issues that can pave the way for further research. A bibliometric analysis of the top-cited evidence offers a list of the most referenced sources and helps in exploring and identifying the major contributions.
The purpose of this study was to identify the 50 most cited research articles in PCL research and analyze their characteristics. We hypothesized that such analysis would help highlight the consensus-building and controversial evidence concerning the diagnosis and management of PCL injuries.
Methods
Two authors (A.K. and S.S.) independently searched the Thomson Reuters Web of Science database using specific keywords: “posterior cruciate ligament,” “posterior cruciate,” and “PCL” separated by the “OR” operator and under the “title” option in April 2021. The search was confined to English-language articles without any time frame restriction. The sources of the articles were refined using the Web of Science Categories under “orthopedics,” “sport sciences,” and “surgery.” The search results were arranged in order of the total citations per article. If the citation count of ≥2 articles matched, the number of citations per year from the year of publication was used as the arranging criterion. A list of 50 top-cited original articles with the primary focus on human PCL or related disorders was prepared after screening of the titles and abstracts of the search results. Animal studies, review articles, case reports, abstract-only publications, letters, editorials, and original articles not focusing on the PCL were sequentially excluded until a list of 50 top-cited original articles was reached. A secondary search using the “topic” option for the aforementioned keywords was conducted to look for any eligible article that could have been missed in the primary search. Any disagreement between the 2 researchers was resolved via reanalysis and mutual discussion.
We used Bibliometrix R-package software (Source: https://www.bibliometrix.org) for the data analysis. The 50 top-cited articles were analyzed for their source journal, country of the corresponding author, publication year, total number of citations, citations per year, and publication trends. Articles were then categorized according to the study types (clinical, basic science). The clinical studies were further classified as therapeutic, prognostic, and diagnostic according to the outcomes studied. The basic science studies were then classified into cadaveric anatomy studies, cadaveric experimental/biomechanical studies, and radiological studies. The level of evidence was assigned for all clinical articles using the Journal of Bone and Joint Surgery ranking system, 57 which was updated in early 2015. Two senior authors (R.A. and S.G) then reviewed all the included articles for qualitative synthesis and discussion.
Results
The search strategy yielded a total of 4625 results, of which 1628 entries belonged to the predefined categories (“orthopedics,” “sports sciences,” and “surgery”). Titles and abstracts of 78 published studies were screened to reach the list of 50 top-cited research articles matching the inclusion criteria. The 28 articles that were excluded from the list included 1 animal study, 1 case report, 6 review articles, and 20 original articles that focused on other capsuloligamentous structures of the knee or knee arthroplasty.
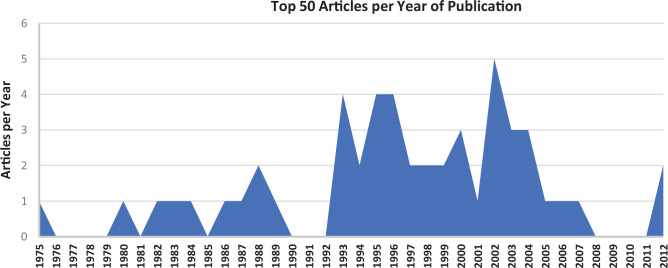
The 50 top-cited articles are shown in Appendix Table A1. All articles were published between 1975 and 2012. A total of 137 authors with 182 appearances contributed to these articles. The individual article citations ranged between 98 and 410. The listed articles belonged to 7 journal sources. The average number of citations per article was 149, and the average number of citations per article per year was 6.13. In total, 44% of the studies were published between 1991 and 2000 (Figure 1).
Figure 1.
The 50 top-cited articles in posterior cruciate ligament research by year of publication.
Citation Information
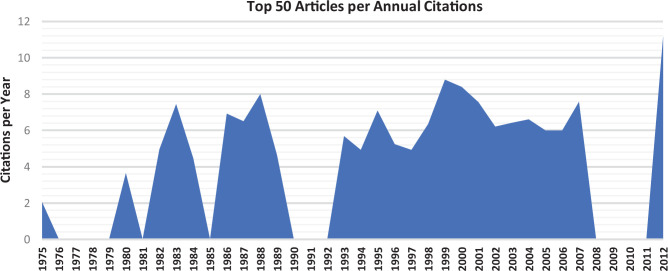
The listed articles had a total of 7908 citations. Appendix Table A1 provides the citation details of each of the 50 articles included in the list. Figure 2 shows the trend of the annual citations per article per year. Again, the decade 1991 to 2000 had the most citations per article per year. The top 10 articles with the most citations per year (ie, average annual citations from the year of publication) are listed in Table 1. Interestingly, 70% of these articles matched with the top 10 articles in terms of total citations.
Figure 2.
Annual citations per article for the 50 top-cited articles in posterior cruciate ligament research.
Table 1.
Top 10 Articles in Posterior Cruciate Ligament Research in Terms of Average Annual Citations
| Rank | Lead Author | Title | Journal a | Year | Citations per Year |
|---|---|---|---|---|---|
| 1 | Grood 22 | Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures | J Bone Joint Surg Am | 1988 | 13.38 |
| 2 | Shelbourne 50 | The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study | Am J Sports Med | 1999 | 13.10 |
| 3 | Harner 24 | Biomechanical analysis of a posterior cruciate ligament reconstruction: deficiency of the posterolateral structures as a cause of graft failure | Am J Sports Med | 2000 | 12.81 |
| 4 | Harner 23 | Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction | Am J Sports Med | 2000 | 12.63 |
| 5 | Seitlinger 47 | Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation | Am J Sports Med | 2012 | 12.25 |
| 6 | Anderson 1 | Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament | J Bone Joint Surg Am | 2012 | 12.20 |
| 7 | Fanelli 15 | Posterior cruciate ligament injuries in trauma patients, part II | Arthroscopy | 1995 | 10.06 |
| 8 | Fanelli 13 | Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up | Arthroscopy | 2002 | 9.86 |
| 9 | Race 43 | PCL reconstruction: in vitro biomechanical comparison of “isometric” versus single and double-bundled “anatomic” grafts | J Bone Joint Surg Br | 1998 | 9.80 |
| 10 | Keller 28 | Nonoperatively treated isolated posterior cruciate ligament injuries | Am J Sports Med | 1993 | 9.19 |
a Journal titles are abbreviated per PubMed format.
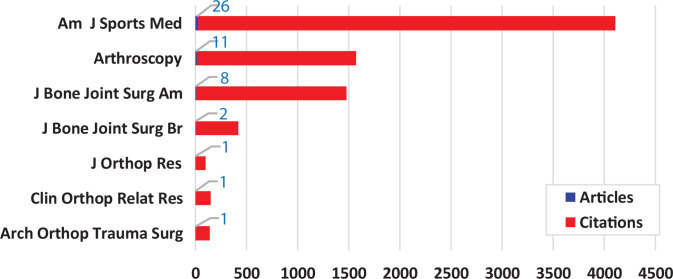
Journal Sources
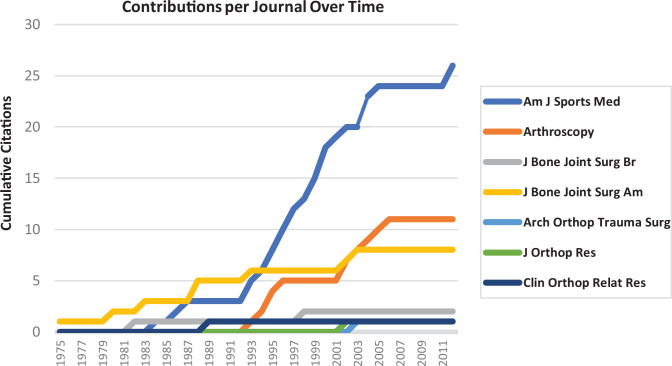
The American Journal of Sports Medicine (AJSM) contributed 26 (52%) of the articles on the list, with 4081 citations (51.6% of the total citations). Figure 3 shows the distribution of the 50 top-cited articles and total citations among different source journals. Figure 4 shows the source growth over time, suggesting each journal’s cumulative article contributions over years to the top 50 cited articles' list. Again, AJSM showed upward growth over the recent period.
Figure 3.
Distribution of the 50 top-cited articles in posterior cruciate ligament research and the number of related citations among different source journals. Journal titles are abbreviated per PubMed format.
Figure 4.
Cumulative contribution per journal per year to the 50 top-cited articles in posterior cruciate ligament research. Journal titles are abbreviated per PubMed format.
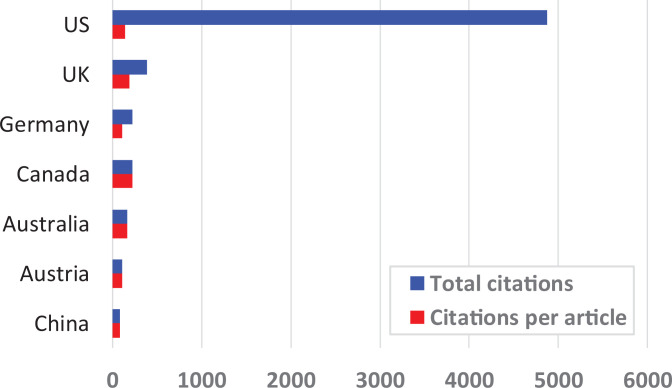
Source Countries
The United States contributed the most articles (84%) and citations (n = 4873). However, the average number of citations per article was larger for the articles from Canada (221 citations per article). Figure 5 shows the global contribution to the 50 top-cited articles.
Figure 5.
Global contribution to the 50 top-cited articles in posterior cruciate ligament research.
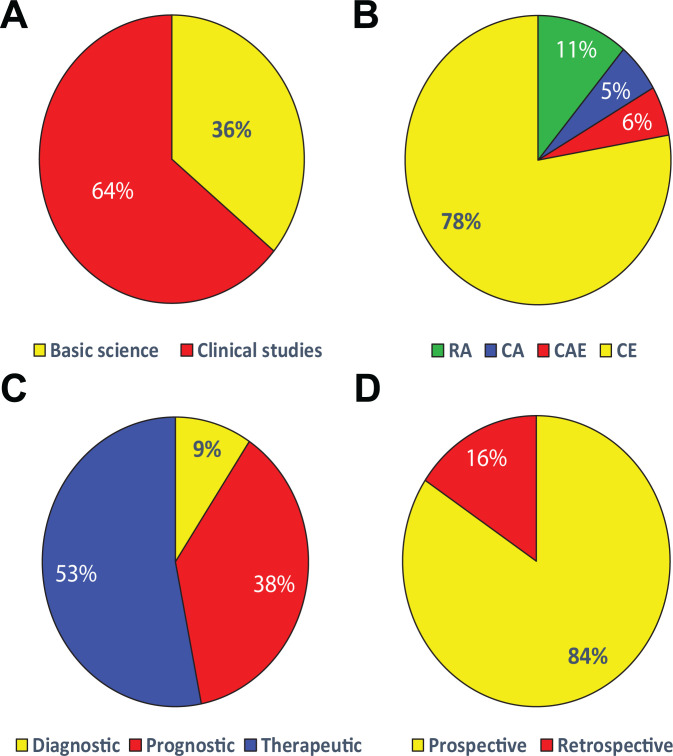
Nature of Published Articles and Level of Evidence
Among the 50 top-cited articles, there were 32 clinical studies and 18 basic science studies (Figure 6). Among the clinical studies, 53.1% were therapeutic, 37.5% were prognostic, and 9.4% were diagnostic studies. All clinical studies had level 4 clinical evidence (all were case series); 84.4% were retrospective, and 15.6% were prospective studies. Among the basic science studies, 77.8% were experimental or biomechanical studies on human cadaveric knees, 5.6% were anatomy studies on human cadaveric knees, 5.6% were combined anatomy and biomechanical studies on cadaveric knees, and 11.1% were radiological studies.
Figure 6.
Types of research studies and their numbers included in the bibliometric analysis: (A) clinical versus basic science studies, (B) types of basic science studies, (C) types of clinical studies, and (D) prospective versus retrospective studies. CA, cadaveric anatomy; CAE, cadaveric anatomy and experimental; CE, cadaveric experimental; RA, radiological.
Discussion
The current bibliometric analysis of the top-cited research on the PCL suggests a relatively lower influence than the citation profiles of research articles on the ACL and meniscus. 9,54 The relevant basic and clinical advances in PCL injury management started evolving from 1975 onward with marked improvement in the 1991 to 2000 decade, which consistently produced top-cited articles. The trend seems to have been maintained with subsequent research, considering that 50% of the 10 top-cited articles were published from 2000 onward. All of the listed articles came from only 7 journals, and 74% of the articles were from just 2 journals (AJSM and Arthroscopy), suggesting the maintained influence of these journals over the years and the readers’ and surgeons’ trust in them. The steeply rising trend of citations from AJSM compared with the other contributing journals suggests increasing research interest in the journal. The country and affiliation profiles of the listed articles indicated that the majority of the studies were from the United States and only a small fraction were from other countries. There was a notable lack of top-cited evidence from Asian and African nations. The annual citation rate of an individual article is an indicator of the maintained interest in that research article, which might not be reflected in cumulative citations, especially for the newer articles. In total, 60% of the top 10 annually cited articles were basic science studies, suggesting that PCL biomechanics and anatomy are still popular among researchers and form the basis of newer advances. The nature of clinical evidence suggests a balanced contribution from clinical and basic science studies. The clinical studies were a good mixture of therapeutic, prognostic, and diagnostic studies. However, the quality of evidence was limited, considering that all of the listed studies provided level 4 evidence and 84.4% of the studies were retrospective.
Qualitative Review of the Clinical Research
The clinical evidence provided by the listed articles mainly focused on the following major questions, which are briefly discussed here.
How Reliable Is the Clinical and Radiological Evaluation of PCL Injuries?
The clinical findings (subjective and objective) in PCL injuries may not always be appreciable. 4,27 Fanelli and Edson 14,15 observed that the incidence of PCL tears in knee injuries with hemarthrosis was 38%. The posterior drawer test, the most specific test for PCL injury, can often be absent. The experience of researchers is mixed in this regard, with some authors reporting high sensitivity compared with others. 6,10,27 Rubinstein et al 44 attempted to address the concerns about lack of clinical findings in patients with PCL tears. Those authors found that among fellowship-trained orthopaedic surgeons, a thorough and precise physical examination, coupled with patient history, had high accuracy in detecting PCL tears. However, their findings were related to chronic tears only. Daniel et al 11 described the quadriceps active test as a reliable method of assessing PCL tear-related laxity. The test used active quadriceps contraction to bring the tibia forward into a neutral position from a posteriorly sagging position. Hewett et al 26 analyzed the effectiveness of stress radiography in diagnosing PCL tears and found it superior to both arthrometer and clinical posterior drawer testing. In the current scenario, imaging modalities like stress radiography, magnetic resonance imaging (MRI), and diagnostic arthroscopy can supplement clinical findings. Among the important concomitant injuries that can be missed during the initial evaluation, PLC injuries are critical. Besides adding posterolateral stability, the PLC integrity is an important factor in successful PCL recovery.
Is Nonoperative Management Sufficient for PCL Tears?
The majority of patients do not need PCL repair or reconstruction. PCL injuries are often missed, and therefore the incidence of PCL injuries is difficult to estimate. 46 Dandy and Pusey 10 observed satisfactory function in 90% of PCL tears with long-leg cast-based management. Parolie and Bergfeld 42 observed an 80% patient satisfaction rate, with 84% patients returning to their original sports.
What Is the Natural History of Nonoperatively Treated PCL Tears?
Although most PCL injuries remain asymptomatic and may not require intervention, it is crucial to know the natural history of nonoperatively managed PCL tears to understand their prognosis. Clancy et al 6 and Fowler and Messieh 18 observed that patients with PCL tears had a high risk of medial condylar articular injury with delayed presentation. Factors like additional ligamentous injuries and high-energy trauma can influence the outcomes of PCL tears and increase the risk of patellofemoral and medial compartment arthritis. Quadriceps strength was found to have a positive correlation with patient satisfaction. 8,42 Cross and Powell 8 and Torg et al 53 observed that severe injury patterns and additional capsuloligamentous injuries such as those that occur in motor vehicle accidents resulted in poor outcomes compared with sports injuries or low-energy trauma, which had mostly good to excellent outcomes. Keller et al 28 suggested that although patients may return to activity and may not have severe enough symptoms to seek medical consultations, they might have intermittent symptoms that can result in patellofemoral and medial joint degeneration without timely treatment. The authors linked the progression of degeneration to the amount of laxity and time interval from injury. Shelbourne et al 50 observed that most PCL injuries healed spontaneously with minimal laxity that did not increase over time. The clinical findings did not correlate with subjective findings, progression of knee arthrosis did not correlate with PCL laxity, and most patients returned to the same sports irrespective of laxity. Strobel et al 52 reviewed the arthroscopy records of nonsurgically managed PCL tears. At 5 years of follow-up, 77.8% of the patients had medial femoral condyle cartilage lesions, and 46.7% had patellar cartilage lesions. The lesions progressively increased with time and significantly correlated with the laxity and involvement of the PLC.
Which Patients Require Operative Management, and What Are the Indications?
Operative management is preferable for patients with persistent symptomatic laxity and instability and those not responding symptomatically to nonoperative management. 8,53 These patients are at risk of developing early arthritic changes of patellofemoral and medial compartments of the knee. 48 Further, a delay in operative management increases this risk. In addition, concomitant collateral ligaments injuries, PCL injuries, and ACL tears indicate high-energy trauma mechanisms, and simultaneous ligamentous reconstruction according to the instability patterns can result in favorable outcomes. 7 Hughston et al 27 recommended operative management of PCL tears in the form of repair or reconstruction in patients with multiligamentous injuries. Clancy et al 6 reported the outcomes of operative management of acute and chronic PCL tears in young patients receiving bone–patellar tendon–bone (BPTB) graft. The reconstruction outcomes were favorable in both the acute and chronic tear groups, with 1 failure in the chronic tear group. The authors advocated for reconstructive procedures for patients who had persistent or progressive functional disability. Considering the PCL to be a vital ligament of the knee, the authors also advocated for ligamentous repair in addition to reconstruction in acute injuries.
Displaced avulsion injuries of the PCL should be treated with operative repair of the avulsion fragment considering the highly unstable nature of these injuries, even if displacement is minimal. A close follow-up of minimally displaced injuries is required to prevent management delay. 39
What Are the Preferred Surgical Techniques for PCL Reconstruction?
Among surgical techniques, avulsion repair, PCL tear repair, and PCL reconstruction were described in the listed articles. Reconstruction is preferred over repair in midsubstance tears. Avulsion fragments can be repaired using sutures in small fragments or using screw fixation in large fragments. 39 For reconstruction purposes, medial meniscal, hamstring tendon, and BPTB allografts have been suggested. Most studies advocated BPTB autografts or allografts, considering their thickness and strength to be ideal for PCL dimensions. 6,17 The Achilles tendon allograft is an effective alternative. 17 Chen et al 5 compared the outcomes of isolated PLC reconstruction using quadriceps tendon graft and quadruple hamstring tendon graft. Satisfactory results were obtained with both graft types. Mild laxity in most cases in each group did not affect the functional status of the joint. Cooper and Stewart 7 found no difference in outcomes with allografts and autografts. Among the techniques described, the femoral fixation was invariably tunnel-based. The tibial fixation varied between tunnel placement and inlay graft fixation at the tibial PCL insertion site. 2,16,17 Clinical outcomes were slightly superior with inlay grafting. 35 A potential role of more anatomic repair and lack of graft wear due to an oblique tibial tunnel has been implicated in the inlay graft technique.
Is Double-Bundle PCL Reconstruction Better Than Single-Bundle Reconstruction?
The current evidence suggests that both single-bundle and double-bundle techniques for PCL reconstruction are comparable in restoring knee stability and function. 31 Among the listed clinical studies, only single-bundle reconstruction or repair of the tears was studied. Reconstruction should be preferred over repair considering the higher risk of failure in the latter. 40 Double-bundle reconstruction might have biomechanical superiority over single-bundle reconstruction, but this has not been clinically established. 43
What Are the Outcome Predictors in Surgically Treated PCL Injuries?
The factors affecting the outcomes of PCL repair or reconstruction are still being investigated. Lipscomb et al 34 presented their experience in operative management of isolated midsubstance PCL tears using hamstring autograft via an intra-articular or extra-articular procedure. They reported that >50% of the patients had persistent laxity and patellofemoral and medial compartment degeneration. Noyes and Barber-Westin 40 provided a comprehensive analysis of factors associated with failure of PCL reconstruction. Persistent instability and lack of reconstruction of other ligamentous structures, especially the PLC, were the most common contributing factors. Suture repair and improper tunnel placement were additional contributing factors. Fanelli and Edson 14 presented a long-term follow-up (2-10 years) of chronic PCL and PLC combined tears treated with PCL reconstruction and biceps femoris tendon tenodesis for PLC reconstruction. Functional outcomes were satisfactory, and objective assessments suggested near-normal posterior translation for the PCL and minimal laxity or tightness of the PLC. The same authors, in 2002, published long-term outcomes (2-10 years) of multiligamentous injuries involving the ACL, PCL, medial collateral ligament (MCL), and PLC. 13 The methods were similar to their previous techniques, and their findings suggested that favorable outcomes are long-lasting with combined reconstruction. Shapiro and Freedman 49 shared their experiences of combined early ACL and PCL reconstruction using allografts in patients with traumatic knee dislocation. The results were mostly excellent, and the authors stressed the need for early aggressive rehabilitation with joint mobilization because of increased risk of arthrofibrosis and heterotopic ossification. Wascher et al 55 and Noyes and Barber-Westin 41 reported similar conclusions.
Qualitative Review of Basic Science Research
The basic science research among the listed articles mainly focused on the following 2 aspects.
Importance of the PCL in the Human Knee Joint
It is well known that the PCL provides the primary restraint to posterior tibial translation at the knee joint. Anderson et al 1 provided a detailed analysis of the anatomic features of the 2 bundles of PCL and their arthroscopic implications for double-bundle reconstruction. Normally, the 2 PCL bundles have a wide separation, and care must be taken to restore this separation during surgical reconstruction. The anterolateral bundle is more anterior and closer to the cartilage, whereas the posteromedial bundle is located around 8.6 mm proximal to the articular cartilage on the medial femoral condyle. The study by Grood et al 22 was the landmark cadaveric study and the most cited study that characterized the role of the PCL and the PLC in translational and rotational stability of the knee joint. The major takeaway points from this cadaveric study were that the posterior drawer test is best appreciated in 90° of flexion because of laxity of the posterior capsule and that lateral collateral ligament injury alone does not contribute to varus laxity. Varus laxity results from injury of the PLC structures, especially popliteal and arcuate ligaments, and from injury of the PCL, given that the intact PCL acts as a restraint for varus opening in flexion. Li et al 32 found increased posterior translation and external rotation in PCL-deficient knees under simulated quadriceps and hamstring loads. Additionally, the sectioning of posterolateral structures resulted in increased external rotation at 30° of knee flexion, and with further flexion, the PCL acted as a restraint to external rotation. This rotational change forms the basis of the dial test for PLC and PCL injuries. PCL injury alone does not affect the rotational limit of the knee joint as long as medial or lateral ligamentous structures are intact. The clinical findings regarding medial compartment and patellofemoral degeneration were supported by Skyhar et al, 51 who observed significantly increased medial compartment pressure and patellofemoral contact forces with PCL or PLC sectioning in simulated resistive extension models of cadaveric knees.
Structure and Biomechanics of the PCL and PCL Reconstruction
Harner et al 25 studied the morphology, microarchitecture, and biomechanics of the PCL and observed that it had a larger cross section at the femoral insertion than the tibial insertion, opposite to the pattern of the ACL. The decrease in the cross-sectional area was accompanied by a decrease in the diameter of collagen fibrils. Two discrete bundles were reported, a posteromedial bundle that was taut in extension and an anterolateral bundle that was taut in flexion. Galloway et al 20 performed in vitro experiments to analyze the effect of graft positioning on the femoral and tibial attachments. Those authors observed that variation in the tibial attachment had only a minor effect on the limits of posterior translation. A nonisometric femoral attachment that was slightly distal but within the PCL anatomic footprint most closely reproduced the normal knee motion. This finding correlates with comparable clinical outcomes with single- and double-bundle reconstructions, as discussed earlier. However, Race and Amis 43 observed that the single-bundle graft was lax beyond 60° of flexion whereas the double-bundle graft maintained the restraint similar to a normal PCL. The findings were supported by Harner et al. 24 However, the instability pattern of the whole knee can be guided by several other dynamic and static restraints; therefore, clinical implications of graft laxity may vary.
In a cadaveric analysis with a posterior tibial load, Fox et al 19 observed that contrary to the general portrayal of one bundle being lax and the other bundle being taut with changes in load, in situ forces were maximum in the posteromedial bundle at 90° of flexion and the anterolateral bundle at 60° of flexion, suggesting the role of posterior restraint by both bundles. These findings were later supported by Li et al, 32 who found that contrary to in vitro cadaveric studies, an in vivo computer-based analysis of initial MRI scans and fluoroscopic films during loading showed elongation of both bundles with knee flexion. The elongation was higher in the anterolateral bundle. Mannor et al 36 further performed a detailed simulated cadaveric analysis of the femoral attachment-based effect on single- and double-bundle grafts. A shallow position of a single-bundle graft had minor variations from a PCL-intact knee throughout the range of motion. A deeper attachment triggered posterior translation >45°. For double-bundle grafts, the shallow locations of 2 bundles resulted in both bundles becoming taut in flexion. Further, 1 shallow and 1 deep arrangement of 2 bundles resulted in a taut, shallow bundle in flexion and a taut, deep bundle in extension. These points need to be considered in single-bundle and double-bundle reconstructions.
The importance of simultaneous PCL and PLC reconstruction in combined injuries was highlighted by Harner et al 24 and LaPrade et al. 30 They found increased posterior translation, external rotation, and additional load on PCL grafts in simulated cadaveric models with PLC deficiency. Bergfeld et al, 3 later supported by Markolf et al, 38 found significantly greater anteroposterior laxity using a tunnel placement technique compared with an inlay graft technique. As well, the tunnel technique had signs of mechanical wear due to the obliquity of the graft. These findings correlate well with clinical studies preferring the inlay graft technique. Markolf et al 37 later analyzed the effect of quadriceps and hamstring forces on the PCL and found that hamstring activity significantly increased forces in the PCL beyond approximately 30° of flexion. The clinical implications were that hamstring exercises should be avoided during PCL rehabilitation and quadriceps strengthening should be continued.
Giffin et al, 21 drawing on cadaveric knee experiments, suggested tibial slope reduction osteotomy as an alternative for reconstruction in chronic PCL instability. In cadaveric knees, an anterior closing wedge osteotomy of the proximal tibia significantly reduced the posterior sag in PCL-deficient knees. In an actual scenario, such an osteotomy component in high tibial osteotomy of medial compartment osteoarthritis can help address chronic PCL insufficiency. Seitlinger et al, 47 using MRI evaluation, found that the axial distance from the medial edge of the PCL is a reliable measurement of tibial tubercle malformation that is not influenced by trochlear position, knee flexion, and tibial rotation. This measurement is a valid alternative for cases of trochlear dysplasia in which the tibial tuberosity–trochlear groove distance may not be reliable.
Lacunae in the Top-Cited Evidence
Although the current analysis covers a wide range of PCL-related issues, some critical aspects have been missed. Superior-quality evidence in the form of prospective studies and randomized trials is required to establish reliable recommendations. With all top-cited clinical evidence coming from case series, it is difficult to formulate sound recommendations. Nevertheless, the basic science research has addressed several structural and biomechanical aspects of the PCL and provided valid raw material for the formulation of clinical research. The topics that were either missed or inadequately discussed in the 50 top-cited articles include the following:
There is a lack of comprehensive clinical research on the techniques of PCL reconstruction concerning tunnel position, graft selection, graft thickness, fixation devices, and single-bundle versus double-bundle reconstructions.
Studies that determine the ideal rehabilitation program for surgically and nonsurgically managed PCL injuries are lacking.
Multicentric and large-volume studies that can identify candidates for operative and nonoperative management based on patient- and injury-related parameters are needed.
Although PCL injuries have been linked to patellofemoral and medial compartment degeneration, the factors that cause the individual variations of such outcomes have not been adequately studied.
The outcomes of multiligamentous reconstructions have been shown to be satisfactory in most patients. However, the severity of individual and combined capsuloligamentous injuries and their effect on PCL reconstruction need to be studied more extensively.
There is very limited evidence regarding the predictors of successful outcomes and failures in surgically and nonsurgically treated PCL injuries.
There is a lack of publications from Asian and African countries. Various factors, including limitations of resources, could affect research activities in these developing regions. Although a large number of orthopaedic and sports journals from these regions are published in the English language, the exclusion of the non-English-language literature in the current analysis could have possibly masked the overall influence of publications from these regions.
Limitations of the Current Analysis
Like other such studies, the current bibliometric analysis has some limitations. First, this analysis is based on a single database (Web of Science). Although the database caters to many high-impact journals and indices, it is not an all-inclusive database and is bound to pose restrictions to the current analysis. Second, the analysis considered only those articles published in the English-language literature. Therefore, influencial publications from non-English-language journals could have been missed. Third, we arranged the articles in order of cumulative citations, and newer articles with high annual citation rates could have been missed. Most of the articles analyzed were published before 2008. The absence of recent articles that could potentially be influencial but could not be included due to the cross-sectional nature of the study is a major shortcoming of this analysis. Fourth, research published in nonorthopaedic, non–sport science, and nonsurgical journals was not included in the current analysis and could have potentially influenced the results.
Conclusion
The majority of the top-cited clinical research has focused on the natural history of PCL tears, factors predicting the need for surgical intervention, long-term outcomes of isolated PCL injuries, and outcomes for patients with additional capsuloligamentous injuries. The top-cited basic science studies established the importance of PCL bundles in limiting posterior translation of the tibia upon loading. Most of the top-cited research came from the United States, with AJSM being the top-cited journal. The current analysis suggests that the PCL research is still evolving and needs high-quality prospective evidence to establish sound recommendations.
APPENDIX
TABLE A1.
50 Top-Cited Articles in PCL Research Arranged in Order of Total Citations
| Rank | Lead Author | Title | Journal a | Year | Total Citations |
|---|---|---|---|---|---|
| 1 | Grood 22 | Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures | J Bone Joint Surg Am | 1988 | 410 |
| 2 | Clancy 6 | Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament: report of a new procedure | J Bone Joint Surg Am | 1983 | 292 |
| 3 | Shelbourne 50 | The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study | Am J Sports Med | 1999 | 275 |
| 4 | Parolie 42 | Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete | Am J Sports Med | 1986 | 253 |
| 5 | Keller 28 | Nonoperatively treated isolated posterior cruciate ligament injuries | Am J Sports Med | 1993 | 248 |
| 6 | Harner 24 | Biomechanical analysis of a posterior cruciate ligament reconstruction: deficiency of the posterolateral structures as a cause of graft failure | Am J Sports Med | 2000 | 245 |
| 7 | Fanelli 15 | Posterior cruciate ligament injuries in trauma patients, part II | Arthroscopy | 1995 | 245 |
| 8 | Harner 23 | Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction | Am J Sports Med | 2000 | 244 |
| 9 | Fowler 18 | Isolated posterior cruciate ligament injuries in athletes | Am J Sports Med | 1987 | 225 |
| 10 | Race 43 | PCL reconstruction: in vitro biomechanical comparison of “isometric” versus single and double-bundled “anatomic” grafts | J Bone Joint Surg Br | 1998 | 217 |
| 11 | Harner 25 | The human posterior cruciate ligament complex: an interdisciplinary study. Ligament morphology and biomechanical evaluation | Am J Sports Med | 1995 | 216 |
| 12 | Dandy 10 | The long-term results of unrepaired tears of the posterior cruciate ligament | J Bone Joint Surg Br | 1982 | 197 |
| 13 | Berg 2 | Posterior cruciate ligament tibial inlay reconstruction | Arthroscopy | 1995 | 192 |
| 14 | Fanelli 13 | Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up | Arthroscopy | 2002 | 181 |
| 15 | Fanelli 17 | Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction | Arthroscopy | 1996 | 179 |
| 16 | Boynton 4 | Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee | Am J Sports Med | 1996 | 168 |
| 17 | Cross 8 | Long-term followup of posterior cruciate ligament rupture: a study of 116 cases | Am J Sports Med | 1984 | 166 |
| 18 | Skyhar 51 | The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee | J Bone Joint Surg Am | 1993 | 165 |
| 19 | Hughston 27 | Acute tears of the posterior cruciate ligament: results of operative treatment | J Bone Joint Surg Am | 1980 | 158 |
| 20 | Bergfeld 3 | A biomechanical comparison of posterior cruciate ligament reconstruction techniques | Am J Sports Med | 2001 | 157 |
| 21 | Torg 53 | Natural history of the posterior cruciate ligament-deficient knee | Clin Orthop Relat Res | 1989 | 149 |
| 22 | LaPrade 30 | The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study | Am J Sports Med | 2002 | 146 |
| 23 | Noyes 41 | Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: use of early protected postoperative motion to decrease arthrofibrosis | Am J Sports Med | 1997 | 143 |
| 24 | Shapiro 49 | Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation | Am J Sports Med | 1995 | 143 |
| 25 | Wascher 55 | Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: results using fresh-frozen nonirradiated allografts | Am J Sports Med | 1999 | 139 |
| 26 | Schulz 46 | Epidemiology of posterior cruciate ligament injuries | Arch Orthop Trauma Surg | 2003 | 136 |
| 27 | Daniel 11 | Use of the quadriceps active test to diagnose posterior cruciate-ligament disruption and measure posterior laxity of the knee | J Bone Joint Surg Am | 1988 | 131 |
| 28 | Lipscomb 34 | Isolated posterior cruciate ligament reconstruction: long-term results | Am J Sports Med | 1993 | 127 |
| 29 | Fanelli 14 | Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year follow-up | Arthroscopy | 2004 | 125 |
| 30 | Li 32 | In vivo elongation of the anterior cruciate ligament and posterior cruciate ligament during knee flexion | Am J Sports Med | 2004 | 124 |
| 31 | Fanelli 12 | Posterior cruciate ligament injuries in trauma patients | Arthroscopy | 1993 | 119 |
| 32 | Fanelli 16 | Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction | Arthroscopy | 1996 | 117 |
| 33 | Rubinstein 44 | The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries | Am J Sports Med | 1994 | 115 |
| 34 | Giffin 21 | Importance of tibial slope for stability of the posterior cruciate ligament deficient knee | Am J Sports Med | 2007 | 114 |
| 35 | Markolf 38 | Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods | J Bone Joint Surg Am | 2002 | 114 |
| 36 | Seitlinger 47 | Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation | Am J Sports Med | 2012 | 108 |
| 37 | Cooper 7 | Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10-year follow-up | Am J Sports Med | 2004 | 108 |
| 38 | Hewett 26 | Diagnosis of complete and partial posterior cruciate ligament ruptures: stress radiography compared with KT-1000 arthrometer and posterior drawer testing | Am J Sports Med | 1997 | 108 |
| 39 | Sekiya 48 | Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction | Arthroscopy | 2005 | 104 |
| 40 | Markolf 37 | Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments | Am J Sports Med | 2004 | 104 |
| 41 | Fox 19 | Determination of the in situ forces in the human posterior cruciate ligament using robotic technology: a cadaveric study | Am J Sports Med | 1998 | 104 |
| 42 | Mannor 36 | Two-bundle posterior cruciate ligament reconstruction: an in vitro analysis of graft placement and tension | Am J Sports Med | 2000 | 103 |
| 43 | Anderson 1 | Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament | J Bone Joint Surg Am | 2012 | 102 |
| 44 | MacGillivray 35 | Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up | Arthroscopy | 2006 | 102 |
| 45 | Galloway 20 | Posterior cruciate ligament reconstruction: an in vitro study of femoral and tibial graft placement | Am J Sports Med | 1996 | 100 |
| 46 | Noyes 40 | Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations | Am J Sports Med | 2005 | 98 |
| 47 | Strobel 52 | Arthroscopic evaluation of articular cartilage lesions in posterior-cruciate-ligament-deficient knees | Arthroscopy | 2003 | 98 |
| 48 | Chen 5 | Arthroscopic reconstruction of the posterior cruciate ligament: a comparison of quadriceps tendon autograft and quadruple hamstring tendon graft | Arthroscopy | 2002 | 98 |
| 49 | Li 33 | Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads—an in vitro experimental study | J Orthop Res | 2002 | 98 |
| 50 | Meyers 39 | Isolated avulsion of the tibial attachment of the posterior cruciate ligament of the knee | J Bone Joint Surg Am | 1975 | 98 |
a Journal titles are abbreviated per PubMed format.
Footnotes
Final revision submitted July 20, 2021; accepted August 24, 2021.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94(21):1936–1945. [DOI] [PubMed] [Google Scholar]
- 2. Berg EE. Posterior cruciate ligament tibial inlay reconstruction. Arthroscopy. 1995;11(1):69–76. [DOI] [PubMed] [Google Scholar]
- 3. Bergfeld JA, McAllister DR, Parker RD, Valdevit AD, Kambic HE. A biomechanical comparison of posterior cruciate ligament reconstruction techniques. Am J Sports Med. 2001;29(2):129–136. [DOI] [PubMed] [Google Scholar]
- 4. Boynton MD, Tietjens BR. Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med. 1996;24(3):306–310. [DOI] [PubMed] [Google Scholar]
- 5. Chen CH, Chen WJ, Shih CH. Arthroscopic reconstruction of the posterior cruciate ligament: a comparison of quadriceps tendon autograft and quadruple hamstring tendon graft. Arthroscopy. 2002;18(6):603–612. [DOI] [PubMed] [Google Scholar]
- 6. Clancy WG, Jr, Shelbourne KD, Zoellner GB, Keene JS, Reider B, Rosenberg TD. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament: report of a new procedure. J Bone Joint Surg Am. 1983;65(3):310–322. [PubMed] [Google Scholar]
- 7. Cooper DE, Stewart D. Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10-year follow-up. Am J Sports Med. 2004;32(2):346–360. [DOI] [PubMed] [Google Scholar]
- 8. Cross MJ, Powell JF. Long-term followup of posterior cruciate ligament rupture: a study of 116 cases. Am J Sports Med. 1984;12(4):292–297. [DOI] [PubMed] [Google Scholar]
- 9. Damodar D, Plotsker E, Greif D, Rizzo MG, Jr, Baraga MG, Kaplan LD. The 50 most cited articles in meniscal injury research. Orthop J Sports Med. 2021;9(4):2325967121994909. doi:10.1177/2325967121994909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dandy DJ, Pusey RJ. The long-term results of unrepaired tears of the posterior cruciate ligament. J Bone Joint Surg Br. 1982;64(1):92–94. [DOI] [PubMed] [Google Scholar]
- 11. Daniel DM, Stone ML, Barnett P, Sachs R. Use of the quadriceps active test to diagnose posterior cruciate-ligament disruption and measure posterior laxity of the knee. J Bone Joint Surg Am. 1988;70(3):386–391. [PubMed] [Google Scholar]
- 12. Fanelli GC. Posterior cruciate ligament injuries in trauma patients. Arthroscopy. 1993;9(3):291–294. [DOI] [PubMed] [Google Scholar]
- 13. Fanelli GC, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18(7):703–714. [DOI] [PubMed] [Google Scholar]
- 14. Fanelli GC, Edson CJ. Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis: 2- to 10-year follow-up. Arthroscopy. 2004;20(4):339–345. [DOI] [PubMed] [Google Scholar]
- 15. Fanelli GC, Edson CJ. Posterior cruciate ligament injuries in trauma patients, part II. Arthroscopy. 1995;11(5):526–529. [DOI] [PubMed] [Google Scholar]
- 16. Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction. Arthroscopy. 1996;12(1):5–14. [DOI] [PubMed] [Google Scholar]
- 17. Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy. 1996;12(5):521–530. [DOI] [PubMed] [Google Scholar]
- 18. Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15(6):553–557. [DOI] [PubMed] [Google Scholar]
- 19. Fox RJ, Harner CD, Sakane M, Carlin GJ, Woo SL. Determination of the in situ forces in the human posterior cruciate ligament using robotic technology: a cadaveric study. Am J Sports Med. 1998;26(3):395–401. [DOI] [PubMed] [Google Scholar]
- 20. Galloway MT, Grood ES, Mehalik JN, Levy M, Saddler SC, Noyes FR. Posterior cruciate ligament reconstruction: an in vitro study of femoral and tibial graft placement. Am J Sports Med. 1996;24(4):437–445. [DOI] [PubMed] [Google Scholar]
- 21. Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35(9):1443–1449. [DOI] [PubMed] [Google Scholar]
- 22. Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988;70(1):88–97. [PubMed] [Google Scholar]
- 23. Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin TM, Woo SL. Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med. 2000;28(2):144–151. [DOI] [PubMed] [Google Scholar]
- 24. Harner CD, Vogrin TM, Höher J, Ma CB, Woo SL. Biomechanical analysis of a posterior cruciate ligament reconstruction: deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med. 2000;28(1):32–39. [DOI] [PubMed] [Google Scholar]
- 25. Harner CD, Xerogeanes JW, Livesay GA, et al. The human posterior cruciate ligament complex: an interdisciplinary study. Ligament morphology and biomechanical evaluation. Am J Sports Med. 1995;23(6):736–745. [DOI] [PubMed] [Google Scholar]
- 26. Hewett TE, Noyes FR, Lee MD. Diagnosis of complete and partial posterior cruciate ligament ruptures: stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med. 1997;25(5):648–655. [DOI] [PubMed] [Google Scholar]
- 27. Hughston JC, Bowden JA, Andrews JR, Norwood LA. Acute tears of the posterior cruciate ligament: results of operative treatment. J Bone Joint Surg Am. 1980;62(3):438–450. [PubMed] [Google Scholar]
- 28. Keller PM, Shelbourne KD, McCarroll JR, Rettig AC. Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med. 1993;21(1):132–136. [DOI] [PubMed] [Google Scholar]
- 29. Kennedy NI, Wijdicks CA, Goldsmith MT, et al. Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. 2013;41(12):2828–2838. [DOI] [PubMed] [Google Scholar]
- 30. LaPrade RF, Muench C, Wentorf F, Lewis JL. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med. 2002;30(2):233–238. [DOI] [PubMed] [Google Scholar]
- 31. Lee DY, Park YJ. Single-bundle versus double-bundle posterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials. Knee Surg Relat Res. 2017;29(4):246–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li G, DeFrate LE, Sun H, Gill TJ. In vivo elongation of the anterior cruciate ligament and posterior cruciate ligament during knee flexion. Am J Sports Med. 2004;32(6):1415–1420. [DOI] [PubMed] [Google Scholar]
- 33. Li G, Gill TJ, DeFrate LE, Zayontz S, Glatt V, Zarins B. Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads—an in vitro experimental study. J Orthop Res. 2002;20(4):887–892. [DOI] [PubMed] [Google Scholar]
- 34. Lipscomb AB, Jr, Anderson AF, Norwig ED, Hovis WD, Brown DL. Isolated posterior cruciate ligament reconstruction: long-term results. Am J Sports Med. 1993;21(4):490–496. [DOI] [PubMed] [Google Scholar]
- 35. MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF. Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy. 2006;22(3):320–328. [DOI] [PubMed] [Google Scholar]
- 36. Mannor DA, Shearn JT, Grood ES, Noyes FR, Levy MS. Two-bundle posterior cruciate ligament reconstruction: an in vitro analysis of graft placement and tension. Am J Sports Med. 2000;28(6):833–845. [DOI] [PubMed] [Google Scholar]
- 37. Markolf KL, O’Neill G, Jackson SR, McAllister DR. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32(5):1144–1149. [DOI] [PubMed] [Google Scholar]
- 38. Markolf KL, Zemanovic JR, McAllister DR. Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods. J Bone Joint Surg Am. 2002;84(4):518–524. [DOI] [PubMed] [Google Scholar]
- 39. Meyers MH. Isolated avulsion of the tibial attachment of the posterior cruciate ligament of the knee. J Bone Joint Surg Am. 1975;57(5):669–672. [PubMed] [Google Scholar]
- 40. Noyes FR, Barber-Westin SD. Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33(5):646–654. [DOI] [PubMed] [Google Scholar]
- 41. Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med. 1997;25(6):769–778. [DOI] [PubMed] [Google Scholar]
- 42. Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14(1):35–38. [DOI] [PubMed] [Google Scholar]
- 43. Race A, Amis AA. PCL reconstruction: in vitro biomechanical comparison of “isometric” versus single and double-bundled “anatomic” grafts. J Bone Joint Surg Br. 1998;80(1):173–179. [DOI] [PubMed] [Google Scholar]
- 44. Rubinstein RA, Jr, Shelbourne KD, McCarroll JR, VanMeter CD, Rettig AC. The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med. 1994;22(4):550–557. [DOI] [PubMed] [Google Scholar]
- 45. Sanders TL, Pareek A, Barrett IJ, et al. Incidence and long-term follow-up of isolated posterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc. 2017;25(10):3017–3023. [DOI] [PubMed] [Google Scholar]
- 46. Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186–191. [DOI] [PubMed] [Google Scholar]
- 47. Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S. Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med. 2012;40(5):1119–1125. [DOI] [PubMed] [Google Scholar]
- 48. Sekiya JK, West RV, Ong BC, Irrgang JJ, Fu FH, Harner CD. Clinical outcomes after isolated arthroscopic single-bundle posterior cruciate ligament reconstruction. Arthroscopy. 2005;21(9):1042–1050. [DOI] [PubMed] [Google Scholar]
- 49. Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med. 1995;23(5):580–587. [DOI] [PubMed] [Google Scholar]
- 50. Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1999;27(3):276–283. [DOI] [PubMed] [Google Scholar]
- 51. Skyhar MJ, Warren RF, Ortiz GJ, Schwartz E, Otis JC. The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. J Bone Joint Surg Am. 1993;75(5):694–699. [DOI] [PubMed] [Google Scholar]
- 52. Strobel MJ, Weiler A, Schulz MS, Russe K, Eichhorn HJ. Arthroscopic evaluation of articular cartilage lesions in posterior-cruciate-ligament-deficient knees. Arthroscopy. 2003;19(3):262–268. [DOI] [PubMed] [Google Scholar]
- 53. Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989;246:208–216. [PubMed] [Google Scholar]
- 54. Vielgut I, Dauwe J, Leithner A, Holzer LA. The fifty highest cited papers in anterior cruciate ligament injury. Int Orthop. 2017;41(7):1405–1412. [DOI] [PubMed] [Google Scholar]
- 55. Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27(2):189–196. [DOI] [PubMed] [Google Scholar]
- 56. Watsend AM, Osestad TM, Jakobsen RB, Engebretsen L. Clinical studies on posterior cruciate ligament tears have weak design. Knee Surg Sports Traumatol Arthrosc. 2009;17(2):140–149. [DOI] [PubMed] [Google Scholar]
- 57. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]