Abstract
Background:
Studies on the clinical outcomes of derotational femoral osteotomy to treat recurrent patellar dislocation in the presence of increased femoral anteversion are limited.
Purpose:
To investigate the role of derotational femoral osteotomy in the treatment of recurrent patellar dislocation in the presence of increased femoral anteversion.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was performed according to the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-analyses) by searching the Medline, Embase, Web of Science, and Cochrane Library databases through February 10, 2021. Included were studies of skeletally mature patients presenting with recurrent patellar dislocation and exhibiting increased femoral anteversion who subsequently underwent derotational femoral osteotomy. Methodological quality was assessed using the MINORS (Methodological Index for Nonrandomized Studies) score. The basic characteristics of each study were recorded and analyzed: characteristic information, radiological parameters, surgical techniques, patient-reported outcomes, and complications.
Results:
A total of 6 studies with 163 patients (170 knees) were included. Sample sizes ranged from 7 to 66 patients, and the patients were predominantly women (range, 79%-100%). The mean age and follow-up ranges were 18 to 28 years and 16 to 44 months, respectively. The mean femoral anteversion decreased significantly from 34° preoperatively to 12° postoperatively. In studies reporting pre- and postoperative outcomes, significant improvements were found in the Lysholm score (from 24.8 to 44.1), Kujala score (from 15.8 to 41.9), International Knee Documentation Committee score (from 11.0 to 28.0), and visual analog scale for pain (from 2.0 to 3.7). All studies reported postoperative complications, giving an overall reported complication rate of 4.7%, but no redislocations occurred during the follow-up period.
Conclusion:
For recurrent patellar dislocation in the presence of increased femoral anteversion, combination treatment with derotational femoral osteotomy led to favorable clinical outcomes with a low redislocation rate. However, there was no consensus among researchers on the indications for derotational femoral osteotomy in the treatment of recurrent patellar dislocation.
Keywords: derotational femoral osteotomy, femoral anteversion, recurrent patellar dislocation, clinical outcome
Medial patellofemoral ligament reconstruction (MPFL-R) has been considered the mainstay of treatment of recurrent patellar dislocation (RPD) over the past decade. 1,5,13,25,29 However, unfavorable clinical outcomes after MPFL-R have also been reported, and several risk factors have been recognized to cause these outcomes. 28
An increased femoral anteversion angle (FAA) has been recognized as a possible risk factor for RPD. 7,8,11,23,32 Recent biomechanical studies have revealed that an increased FAA can significantly increase the lateralizing force that acts on the patella and may be a cause of MPFL-R failure. 20,21 To date, the treatment of RPD in the presence of increased FAA is still debated. Some studies have found that increased femoral anteversion is correlated with inferior clinical outcomes and MPFL-R failure. 14,44 Given these reasons, derotational femoral osteotomy has been proposed as a treatment of RPD in the presence of increased femoral anteversion, and subsequent clinical studies have confirmed the clinical benefit of this procedure. 15,19,27,38,42 However, these studies are limited to small case series, and no study has attempted to analyze them in totality.
The purpose of this study was to investigate the role of derotational femoral osteotomy in treating RPD in the presence of increased femoral anteversion. It was hypothesized that favorable functional outcomes and low redislocation rates would be found after isolated and combined derotational femoral osteotomy.
Methods
Literature Research
A systematic review was performed following the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-analyses). 26 The Medline, Embase, Web of Science, and Cochrane Library databases were searched by all of the authors independently on February 10, 2021. The search terms were as follows: (patellar dislocation OR patellar instability OR patellar subluxation OR patellofemoral dislocation OR patellofemoral dysfunction) AND (rotational osteotomy OR derotational osteotomy OR torsional osteotomy).
Study Selection
All articles identified by these search terms were generally reviewed and then discussed among authors according to the inclusion or exclusion criteria. If there were any disagreements among the authors about a study’s inclusion, the final decision was made by the senior author (H.Z.). Full-text articles were then critically reviewed. Additionally, all references from the studies were reviewed and reconciled to verify that no relevant articles were missing from the systematic review. All studies were included that reported the clinical outcomes of derotational femoral osteotomy for RPD in the presence of increased femoral anteversion. The main purpose of this systematic review was to investigate the role of derotational femoral osteotomy for treating RPD in the presence of increased femoral anteversion; therefore, patients with a history of undergoing ipsilateral derotational tibial osteotomy were excluded. The detailed inclusion and exclusion criteria are described in Table 1.
Table 1.
Inclusion and Exclusion Criteria of the Systematic Review
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Patients with recurrent patellar dislocation History of derotational femoral osteotomy A minimum follow-up of 12 mo Evidence levels 1-4 |
History of ipsilateral tibial osteotomy Cadaveric, biomechanical, or animal study Surgical technique article Systematic review or meta-analysis Patient duplication Non–English language publication |
Data Abstraction
Data extraction was performed independently by 2 reviewers (Z.Z. and H.Z.). Each full-text article was abstracted regarding study characteristics, patient characteristics, surgical techniques, and outcome measures. Data on pre- and postoperative outcome measurements were extracted as means and standard deviations. The decision tree of von Elm et al 36 was used to identify and exclude duplicate studies. Any discrepancies were resolved through discussion with a third author (T.Z.).
Study characteristics included publication date, study design, level of evidence, number of patients/knees, and length of follow-up. Characteristic data consisted of patient sex and age. Surgical techniques for derotational femoral osteotomy and combined procedures were summarized according to the descriptions in the studies.
Outcome measures consisted of pre- and postoperative clinical and radiographic evaluations. Clinical assessments included patient-reported function scores and objective patellar stability (eg, MPFL residual laxity). Radiographic measurements included the pre- and postoperative FAA and patellar tilt angle.
Risk-of-Bias Assessment
The methodological quality of each study was assessed independently by 2 review authors (Z.Z. and H.Z.) according to the MINORS (Methodological Index for Nonrandomized Studies) score. 31 The items on the questionnaire were scored as follows: 0 if not reported, 1 when reported but inadequate, and 2 when reported and adequate; there was a maximum possible score of 16 for noncomparative studies and 24 for comparative studies. MINORS scores of 13 to 16 for noncomparative studies and 21 to 23 for comparative studies were considered low risk of bias, and scores ≤12 and ≤20 were deemed high risk for noncomparative and comparative studies, respectively. Any discrepancies in scores were settled by consensus between the review authors.
Data Analysis
Individual study heterogeneity regarding patient populations and treatment prevented meta-analysis calculations. Therefore, descriptive statistics were used for numerical characteristic data (age and follow-up) and clinical and radiological outcomes. Reliability statistics were calculated using the Cohen κ coefficient to quantify the degree of agreement between the raters for the MINORS scores. When the standard deviation was not available, the authors were contacted to provide the missing data, or it was calculated according to the Cochrane handbook. 17
Results
Study Identification
Of the 193 studies identified, 34 proceeded to full-text review. Ultimately, 6 studies were represented in the systematic review (Figure 1). Five studies were retrospective case series (level 4), 2,15,19,27,38 and 1 study was a retrospective cohort study (level 3). 40 The mean MINORS score was 12.0 ± 0.7 (range, 11-13) for the 5 noncomparative studies, 2,15,19,27,38 and the score was 20 for the 1 comparative study (Table 2). 40 Of the 6 studies, 5 were assessed as having a high risk of bias (MINORS score <13 for a noncomparative study or <21 for a comparative study). 2,15,19,27,38 The Cohen κ coefficient for interrater reliability was 0.94, indicating almost-perfect agreement.
Figure 1.
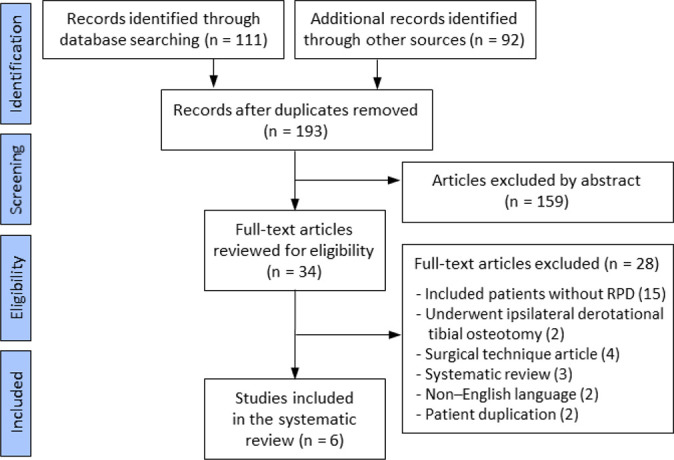
Flowchart of the search strategy following the PRISMA guidelines. RPD, recurrent patellar dislocation.
Table 2.
Study Characteristics a
| Lead Author | Year | Study Design | LOE | MINORS Score | Patients (Knees), No. | Mean Age, y | Female/Male, No. | Mean Follow-up, mo |
|---|---|---|---|---|---|---|---|---|
| Zhang 40 | 2021 | Cohort study b | 3 | 20/24 | 66 (66) | 21 | 59/7 | 37 |
| Biedert 2 | 2020 | Case series | 4 | 12/16 | 7 (9) | 22 | 7/0 | 25 |
| Yang 38 | 2019 | Case series | 4 | 12/16 | 20 (20) | 21 | 18/2 | 18 |
| Frings 15 | 2019 | Case series c | 4 | 11/16 | 16 (19) | 21 | 15/4 | 26 |
| Imhoff 19 | 2019 | Case series | 4 | 13/16 | 42 (44) | 28 | NR | 44 |
| Nelitz 27 | 2015 | Case series | 4 | 12/16 | 12 (12) | 18 | 12/0 | 16 |
a LOE, level of evidence; MINORS, Methodological Index for Nonrandomized Studies; NR, not reported.
b This study compared the results of patients undergoing derotational femoral osteotomy vs a nonderotational osteotomy procedure.
c This study reported clinical results after combined distal femoral osteotomy, which included 19 derotational femoral osteotomies and 12 varus osteotomies. Only patients who underwent derotational femoral osteotomy were included in the systematic review.
Patient Characteristics
The 6 studies comprised 163 patients (170 knees). Table 2 summarizes each study. Age was cited in all 6 studies, with the mean ranging from 18 to 28 years. Sex distribution was 111 women (90%, range 79%-100%) and 13 men (10%) in 5 studies. 2,15,27,38,40 All studies noted the follow-up intervals, resulting in a mean follow-up from 16 to 44 months.
Surgical Techniques
Table 3 depicts the surgical details across the studies. All studies reported the cutoff value of femoral anteversion for derotational femoral osteotomy (range, 20°-30°). The preoperative mean FAA ranged from 31° to 39° (mean, 34°) in all studies, and the postoperative mean FAA mean ranged from 10° to 16° (mean, 12°) in 4 studies. 15,19,38,40 Supracondylar derotational osteotomy was performed in all studies. A total of 62.4% of the patients underwent combined MPFL-R, 19,27,40 and 28.2% of the patients underwent medial reefing to stabilize the patella. 2,15,38 Of the 6 studies, 4 reported that additional bony procedures were performed to correct concurrent bony deformities 2,15,19,40 such as tibial tubercle transfer (29.4%), 15,19,40 valgus/varus correction (15.9%), 15,19 and trochleoplasty (8.8%). 2,19
Table 3.
Operative Procedure Data a
| Lead Author | Cutoff Value for Osteotomy | Mean Pre/Post FAA (Modality) | Surgical Approach | Patellar Stabilization Procedure, No. b | Combined Bony Procedures |
|---|---|---|---|---|---|
| Zhang 40 | 30° | 34°/10° (3D CT) | Lateral | 66/0/0 | TT transfer (n = 30) |
| Biedert 2 | 27° | 38°/NR (axial CT) | Lateral | 0/9/0 | Trochleoplasty (n = 9) |
| Yang 38 | 25° | 31°/16° (axial CT) | Lateral | 0/20/0 | None |
| Frings 15 | >20° c | 39°/11° (axial CT or MRI) | Lateral, medial | 0/19/0 | TT transfer (n = 14) Valgus correction (n = 5) |
| Imhoff 19 | >25° d | 31°/12° (axial MRI) | Lateral | 28/0/16 | TT transfer (n = 6) Valgus correction (n = 22) Trochleoplasty (n = 6) |
| Nelitz 27 | 25° | 34°/NR (axial MRI) | Lateral | 12/0/0 | None |
a Osteotomy level for each study: distal femur. 3D, 3-dimensional; CT, computed tomography; FAA, femoral anteversion angle; MPFL-R, medial patellofemoral ligament reconstruction; MRI, magnetic resonance imaging; NR, not reported; Pre/Post, pre- and postoperative; TT, tibial tubercle.
b MPFL-R/reefing/none.
c In this article, derotational femoral osteotomy was indicated when the FAA exceeded the normal value by 10°. According to Dejour et al 8 (normal value, 10.8°), the cutoff value of femoral anteversion should have been ≥20° in this article.
d The original article did not report the indication of derotational femoral anteversion. We tried to contact the corresponding author by email but failed to obtain a response. In this article, the author declared that femoral anteversion >25° was a severe risk factor for patellofemoral instability; therefore, it seems reasonable to assume that the cutoff value of femoral anteversion for derotational femoral osteotomy was at least 25°.
Subjective Clinical Outcomes
Six patient-reported outcomes were described in the articles. The visual analog scale for pain, International Knee Documentation Committee score, Tegner score, Kujala score, and Lysholm score were used as outcome measures in ≥3 studies and are summarized in Table 4. Significant pre- to postoperative improvement was seen in all except for the Tegner score.
Table 4.
Functional Scores a
| Tegner Score | VAS Score | IKDC Score | Kujala Score | Lysholm Score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lead Author | Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop | Preop | Postop |
| Zhang 40,b | 3.2 ± 0.6 | 4.4 ± 0.8 | 56.7 ± 11.2 | 83.1 ± 10.4 | 53.8 ± 11.2 | 82.3 ± 8.4 | 58.2 ± 10.2 | 83.7 ± 9.0 | ||
| Biedert 2 | 2.7 | 6.0 | 41.2 | 83.1 | ||||||
| Yang 38 | 5.5 ± 2.5 | 5.8 ± 1.4 | 4.2 ± 2.1 | 1.3 ± 1.1 | 70.6 ± 21.4 | 90.8 ± 14.3 | 72.4 ± 19.9 | 88.2 ± 12.3 | ||
| Frings 15 | 2.2 ± 1.3 | 3.7 ± 1.2 | 4.9 ± 2.6 | 1.2 ± 1.5 | 47.7 ± 27 | 84.4 ± 16 | 40.5 ± 20.4 | 84.6 ± 15.2 | ||
| Imhoff 19 | 4 | 4 | 4 ± 3 | 2 ± 2 | 54 ± 13 | 65 ± 17 | 46 ± 21 | 71 ± 24 | ||
| Nelitz 27 | 4 | 4.5 | 4 | 1.5 | 60 | 85 | 69 | 92.5 | ||
a Blank cells indicate not reported. Values are presented as mean ± SD. IKDC, International Knee Documentation Committee; Postop, postoperative; Preop, preoperative; VAS, visual analog scale.
b The postoperative functional scores were significantly higher in the derotational group than in the control group.
Patient satisfaction was reported in 5 studies, 2,15,19,27,38 with a postoperative satisfaction rate ranging from 72% to 100% (Table 5). One study compared the clinical outcomes of MPFL-R with and without derotational femoral osteotomy for treating RPD with an FAA >30°, 40 which demonstrated that the former yielded more favorable subjective outcomes than MPFL-R alone, and this circumstance was more remarkable when the patients had a preoperative high-grade J-sign.
Table 5.
Complication, Satisfaction Rate, and Radiological Assessments a
| Lead Author | Complications | Satisfaction, % b | Other Assessments |
|---|---|---|---|
| Zhang 40 | None | Not reported | Residual J-sign, patellar medial laxity index |
| Biedert 2 | Persisting pain (n = 1) | 89/0/11 | Cartilage injury grade |
| Yang 38 | Limited knee flexion (n = 1) | 100/0/0 | Congruence angle and patellar tilt |
| Frings 15 |
|
100/0/0 | None |
| Imhoff 19 |
|
72/15/13 | None |
| Nelitz 27 | Limited knee flexion (n = 2) | 92/8/0 | None |
a No patients experienced patellar redislocation; however, 6% of patients after derotational femoral osteotomy showed medial patellofemoral ligament residual graft laxity.
b Satisfied/partially satisfied/dissatisfied.
Radiological and Objective Clinical Outcomes
Pre- and postoperative patellar tilt was reported in 1 study. 38 The mean preoperative patellar tilt was 30.4°, while the mean postoperative patellar tilt was 15.8°. One study used patellofemoral stress radiography to measure the postoperative MPFL graft residual laxity (if the patellar medial laxity index exceeded 50%, MPFL residual graft laxity was considered for the reconstructed ligament), 40 showing a 6% rate of MPFL residual graft laxity (Table 5).
Complications
All but the comparative study reported postoperative complications (Table 5). A total of 8 complications were noted for a rate of 4.7%. Major and minor complications were reported. The most common complication was limited knee flexion (1.8%), which was resolved by enhanced rehabilitation or manipulation under anesthesia. No patients experienced patellar subluxation or redislocation postoperatively.
Discussion
The most important finding of this systematic review was that derotational femoral osteotomy in the treatment of RPD in the presence of increased FAA results in favorable subjective and objective outcomes with low rates of redislocation. However, there is no consensus among researchers on the indications for derotational femoral osteotomy in the treatment of RPD.
Isolated MPFL-R has gained much popularity over the last few years in the treatment of RPD, given its lower surgical trauma and favorable clinical outcomes. 3,22,30 Erickson et al 12 performed 90 isolated MPFL-R procedures regardless of increased femoral anteversion and other bony pathologies and noted a significant improvement in outcome scores, with a low redislocation rate (1.1%). Similarly, in the study by Blanke et al, 3 isolated MPFL-R resulted in superior clinical outcomes and patellar stability irrespective of the value of femoral anteversion and subgroup analysis demonstrated that increased femoral anteversion (>20°) did not lead to worse outcomes than in patients with an FAA <20°. Therefore, the question is whether derotational femoral osteotomy should be performed in the treatment of patients with increased FAA.
The indications for derotational femoral osteotomy in the treatment of RPD is a question worth researching. Many studies performed derotational femoral osteotomy when preoperative femoral anteversion reached a specific threshold, which usually varied from 20° to 30° based on the experience and preference of the surgeon. 2,15,19,27,38,40 The current biomechanical and clinical evidence regarding the threshold of derotational femoral anteversion for RPD is limited. A recent biomechanical study found a persistent increased lateralizing force vector acting on the patella after MPFL-R when the FAA was 20°, which might increase the stress on the reconstructed MPFL and lead to MPFL failure and patellar redislocation. 21 Therefore, the authors proposed an additional derotational femoral osteotomy in such cases to neutralize the abnormal force vector produced by the increased FAA. Franciozi et al 14 investigated the influence of an increased FAA on clinical outcomes in patients with RPD treated by MPFL-R with tibial tubercle transfer and found that an FAA >30° was associated with worse functional outcomes. Similarly, Teitge 35 indicated that derotational femoral osteotomy is beneficial if the FAA is >30°. In the study by Zhang et al, 44 patients were divided into 3 FAA groups: low (<20°), medium (20°-30°), and high (>30°). The authors noted that patient-reported outcomes and patellar stability in the medium FAA group were comparable to those in the low FAA group but significantly better than those in the high FAA group; therefore, they speculated that patients with a high FAA (>30°) were possible candidates for derotational femoral osteotomy.
Another view holds that the severity of patellar maltracking should be taken into consideration when determining whether to perform derotational femoral osteotomy in patients with RPD and increased FAAs. In the treatment algorithm for RPD proposed by Frosch and Schmeling, 16 isolated MPFL-R was advocated when patellar tracking was normal, regardless of the increased FAA, and derotational femoral osteotomy was to be performed only in the presence of patellar maltracking. Zhang et al 43 analyzed the risk factors for severe patellar maltracking of RPD and found that an increased FAA was strongly associated with a high-grade J-sign; therefore, given the adverse impact of severe patellar maltracking on the outcomes after MPFL-R, the authors suggested that derotational femoral osteotomy should be performed when an increased FAA is coupled with a high-grade J-sign. Zhang et al 40 recently conducted another study to investigate whether patients with an increased FAA could benefit from combined derotational femoral osteotomy. This study compared the clinical outcomes of MPFL-R alone versus MPFL-R with derotational femoral osteotomy for treating RPD with an increased FAA (>30°), and it determined that the derotational osteotomy group had significantly better patient-reported outcomes and a lower rate of MPFL residual graft laxity than the control group. A subgroup analysis was then performed by stratifying the results regarding severity of preoperative patellar maltracking (low- vs high-grade J-sign) and revealed that patients with a high-grade J-sign could benefit more from the combined derotational osteotomy than patients with a low-grade J-sign. Therefore, the authors concluded that derotational femoral osteotomy should be considered for patients with an increased FAA (>30°) and concurrent high-grade J-sign.
Another potential indication for derotational femoral osteotomy is revisional surgery for RPD. Some authors have speculated that a neglected increased FAA is a common reason for MPFL-R failure. 16,28,37 Therefore, Weber et al 37 stated that derotational osteotomy for excessive femoral anteversion should be performed in patients with failed soft tissue procedures. For patients with failed primary MPFL-R and neglected increased FAA, Nelitz et al 28 performed derotational femoral osteotomy and MPFL-R, and a favorable clinical outcome was achieved in these revision cases. Similarly, Zhang et al 41 analyzed the risk factors for MPFL residual laxity and declared that the restoration of normal femoral anteversion by derotational femoral osteotomy was a critical step in the management of revision cases.
Other bony deformities may coexist in patients with an increased FAA. How to treat these concurrent bony deformities is still debated in the literature. Frings et al 15 declared that all predisposing risk factors—including rotational deformities, increased tibial tubercle–trochlear groove distance, patella alta, and genu valgum—should be addressed simultaneously to restore normal patellar tracking, similar to the “à la carte” approach introduced by the Lyon group. 6 In contrast, in the studies of Nelitz et al 27 and Yang et al, 38 derotational femoral osteotomy was performed as the isolated bony procedure. In fact, the concurrent mild to moderate valgus deformity could be corrected simultaneously by derotational femoral osteotomy without increasing treatment-related morbidity. 18 For patients with severe trochlear dysplasia, a recent meta-analysis found that combined trochleoplasty decreased the redislocation rate at the cost of a higher risk of postoperative range-of-motion limitation. 39 In the present systematic review, no redislocations occurred among the patients who did not undergo trochleoplasty. Therefore, based on the results of this systematic review, when derotational femoral osteotomy was performed to correct the increased FAA in patients with RPD, the combined trochleoplasty was usually not recommended owing to its potential morbidity.
Derotational femoral osteotomy was initially applied to address patients with idiopathic torsional deformities of the lower extremities or miserable malalignment syndrome associated with significant patellofemoral pain. 4,9,10,24,33,34 Teitge 35 was the first to systematically describe the clinical use of derotational femoral osteotomy in patellofemoral instability in 2006. Subsequently, several investigations reporting the successful outcomes of derotational femoral osteotomy have been published. 9,10,24,33,34 However, these publications were excluded from this systematic review because of the heterogeneity of the patients in these studies, such as those mixing patellar instability and anterior knee pain or mixing femoral and tibial derotational osteotomy.
There are several limitations to this study. The major limitations of this systematic review are the low levels of evidence, heterogeneity bias, and retrospective nature of most studies, such as several combined procedures (eg, tibial tubercle transfer and trochleoplasty). These limitations are not uncommon in systematic reviews of novel orthopaedic surgical procedures and are mostly unavoidable until higher-level studies of the current topic are conducted and published.
Conclusion
For RPD in the presence of increased femoral anteversion, combination treatment with derotational femoral osteotomy leads to favorable clinical outcomes with a low redislocation rate. However, there is no consensus among researchers on the indications for derotational femoral osteotomy in the treatment of RPD.
Footnotes
Final revision submitted August 17, 2021; accepted August 25, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for this study was received from the Capital’s Funds for Health Improvement and Research (grants 2020-1-2071 and 2020-2-2075) and the National Key R&D Program of China (grant 2019YFF0301700). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Allen M, Krych J, Johnson R, Mohan R, Stuart J, Dahm L. Combined tibial tubercle osteotomy and medial patellofemoral ligament reconstruction for recurrent lateral patellar instability in patients with multiple anatomic risk factors. Arthroscopy. 2018;34(8):2420–2426. [DOI] [PubMed] [Google Scholar]
- 2. Biedert M. Combined deepening trochleoplasty and supracondylar external rotation osteotomy for recurrent patellar instability in patients with trochlear dysplasia and increased femoral antetorsion. Knee. 2020;27(4):1158–1166. [DOI] [PubMed] [Google Scholar]
- 3. Blanke F, Watermann K, Haenle M, Feitenhansl A, Camathias C, Vogt S. Isolated medial patellofemoral ligament reconstruction can be an effective procedure in patellofemoral instability with risk factors. J Knee Surg. 2020;33(10):992–997. [DOI] [PubMed] [Google Scholar]
- 4. Bruce D, Stevens M. Surgical correction of miserable malalignment syndrome. J Pediatr Orthop. 2004;24(4):392–396. [DOI] [PubMed] [Google Scholar]
- 5. Burnham M, Howard S, Hayes B, Lattermann C. Medial patellofemoral ligament reconstruction with concomitant tibial tubercle transfer: a systematic review of outcomes and complications. Arthroscopy. 2016;32(6):1185–1195. [DOI] [PubMed] [Google Scholar]
- 6. Dejour D. The patellofemoral joint and its historical roots: the Lyon School of Knee Surgery. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1482–1494. [DOI] [PubMed] [Google Scholar]
- 7. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15(1):39–46. [DOI] [PubMed] [Google Scholar]
- 8. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. [DOI] [PubMed] [Google Scholar]
- 9. Dickschas J, Harrer J, Pfefferkorn R, Strecker W. Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg. 2012;132(3):289–298. [DOI] [PubMed] [Google Scholar]
- 10. Dickschas J, Harrer J, Reuter B, Schwitulla J, Strecker W. Torsional osteotomies of the femur. J Orthop Res. 2015;33(3):318–324. [DOI] [PubMed] [Google Scholar]
- 11. Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S. Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med. 2013;41(1):51–57. [DOI] [PubMed] [Google Scholar]
- 12. Erickson J, Nguyen J, Gasik K, Gruber S, Brady J, Shubin Stein E. Isolated medial patellofemoral ligament reconstruction for patellar instability regardless of tibial tubercle-trochlear groove distance and patellar height: outcomes at 1 and 2 years. Am J Sports Med. 2019;47(6):1331–1337. [DOI] [PubMed] [Google Scholar]
- 13. Franciozi E, Ambra F, Albertoni B, et al. Anteromedial tibial tubercle osteotomy improves results of medial patellofemoral ligament reconstruction for recurrent patellar instability in patients with tibial tuberosity–trochlear groove distance of 17 to 20 mm. Arthroscopy. 2019;35(2):566–574. [DOI] [PubMed] [Google Scholar]
- 14. Franciozi E, Ambra F, Albertoni J, et al. Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy. 2017;33(3):633–640. [DOI] [PubMed] [Google Scholar]
- 15. Frings J, Krause M, Akoto R, Frosch H. Clinical results after combined distal femoral osteotomy in patients with patellar maltracking and recurrent dislocations. J Knee Surg. 2019;32(9):924–933. [DOI] [PubMed] [Google Scholar]
- 16. Frosch H, Schmeling A. A new classification system of patellar instability and patellar maltracking. Arch Orthop Trauma Surg. 2016;136(4):485–497. [DOI] [PubMed] [Google Scholar]
- 17. Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; 2019. [Google Scholar]
- 18. Imhoff B, Beitzel K, Zakko P, et al. Derotational osteotomy of the distal femur for the treatment of patellofemoral instability simultaneously leads to the correction of frontal alignment: a laboratory cadaveric study. Orthop J Sports Med. 2018;6(6):2325967118775664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Imhoff B, Cotic M, Liska F, et al. Derotational osteotomy at the distal femur is effective to treat patients with patellar instability. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):652–658. [DOI] [PubMed] [Google Scholar]
- 20. Kaiser P, Schmoelz W, Schoettle P, Zwierzina M, Heinrichs C, Attal R. Increased internal femoral torsion can be regarded as a risk factor for patellar instability-A biomechanical study. Clin Biomech (Bristol, Avon). 2017;47(4):103–109. [DOI] [PubMed] [Google Scholar]
- 21. Kaiser P, Schmoelz W, Schöttle B, Heinrichs C, Zwierzina M, Attal R. Isolated medial patellofemoral ligament reconstruction for patella instability is insufficient for higher degrees of internal femoral torsion. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):758–765. [DOI] [PubMed] [Google Scholar]
- 22. Kita K, Tanaka Y, Toritsuka Y, et al. Factors affecting the outcomes of double-bundle medial patellofemoral ligament reconstruction for recurrent patellar dislocations evaluated by multivariate analysis. Am J Sports Med. 2015;43(12):2988–2996. [DOI] [PubMed] [Google Scholar]
- 23. Lee Q, Anzel H, Bennett A, Pang D, Kim C. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res. 1994;(302):69–74. [PubMed] [Google Scholar]
- 24. Leonardi F, Rivera F, Zorzan A, Ali M. Bilateral double osteotomy in severe torsional malalignment syndrome: 16 years follow-up. J Orthop Traumatol. 2014;15(2):131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Longo G, Berton A, Salvatore G, et al. Medial patellofemoral ligament reconstruction combined with bony procedures for patellar instability: current indications, outcomes, and complications. Arthroscopy. 2016;32(7):1421–1427. [DOI] [PubMed] [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. [DOI] [PubMed] [Google Scholar]
- 27. Nelitz M, Dreyhaupt J, Williams R, Dornacher D. Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop. 2015;39(12):2355–2362. [DOI] [PubMed] [Google Scholar]
- 28. Nelitz M, Williams S, Lippacher S, Reichel H, Dornacher D. Analysis of failure and clinical outcome after unsuccessful medial patellofemoral ligament reconstruction in young patients. Int Orthop. 2014;38(11):2265–2272. [DOI] [PubMed] [Google Scholar]
- 29. Neri T, Parker A, Beach A, et al. Medial patellofemoral ligament reconstruction with or without tibial tubercle transfer is an effective treatment for patellofemoral instability. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):805–813. [DOI] [PubMed] [Google Scholar]
- 30. Sappey-Marinier E, Sonnery-Cottet B, O’Loughlin P, et al. Clinical outcomes and predictive factors for failure with isolated MPFL reconstruction for recurrent patellar instability: a series of 211 reconstructions with a minimum follow-up of 3 years. Am J Sports Med. 2019;47(6):1323–1330. [DOI] [PubMed] [Google Scholar]
- 31. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 32. Souza B, Draper E, Fredericson M, Powers M. Femur rotation and patellofemoral joint kinematics: a weight-bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40(5):277–285. [DOI] [PubMed] [Google Scholar]
- 33. Stambough B, Davis L, Szymanski A, Smith C, Schoenecker L, Gordon E. Knee pain and activity outcomes after femoral derotation osteotomy for excessive femoral anteversion. J Pediatr Orthop. 2018;38(10):503–509. [DOI] [PubMed] [Google Scholar]
- 34. Strecker W, Dickschas J. Torsional osteotomy: operative treatment of patellofemoral maltracking. Oper Orthop Traumatol. 2015;27(6):505–524. [DOI] [PubMed] [Google Scholar]
- 35. Teitge RA. Osteotomy in the treatment of patellofemoral instability. Tech Knee Surg. 2006;5(1):2–18. [Google Scholar]
- 36. von Elm E, Poglia G, Walder B, Tramèr MR. Different patterns of duplicate publication: an analysis of articles used in systematic reviews. JAMA. 2004;291(8):974–980. [DOI] [PubMed] [Google Scholar]
- 37. Weber E, Nathani A, Dines S, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417–427. [DOI] [PubMed] [Google Scholar]
- 38. Yang M, Wang Y, Zuo X, Li Q, Dai K, Wang F. Good outcomes of combined femoral derotation osteotomy and medial retinaculum plasty in patients with recurrent patellar dislocation. Orthop Surg. 2019;11(4):578–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Zaffagnini S, Previtali D, Tamborini S, Pagliazzi G, Filardo G, Candrian C. Recurrent patellar dislocations: trochleoplasty improves the results of medial patellofemoral ligament surgery only in severe trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3599–3613. [DOI] [PubMed] [Google Scholar]
- 40. Zhang Z, Song G, Li Y, et al. Medial patellofemoral ligament reconstruction with or without derotational distal femoral osteotomy in treating recurrent patellar dislocation with increased femoral anteversion: a retrospective comparative study. Am J Sports Med. 2021;49(1):200–206. [DOI] [PubMed] [Google Scholar]
- 41. Zhang Z, Song G, Zheng T, Ni Q, Feng H, Zhang H. The presence of a preoperative high-grade J-sign and femoral tunnel malposition are associated with residual graft laxity after MPFL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1183–1190. [DOI] [PubMed] [Google Scholar]
- 42. Zhang Z, Zhang H, Song G, et al. A high-grade j sign is more likely to yield higher postoperative patellar laxity and residual maltracking in patients with recurrent patellar dislocation treated with derotational distal femoral osteotomy. Am J Sports Med. 2020;48(1):117–127. [DOI] [PubMed] [Google Scholar]
- 43. Zhang Z, Zhang H, Song G, Zheng T, Feng H. A pre-operative grade 3 J-sign adversely affects short-term clinical outcome and is more likely to yield MPFL residual graft laxity in recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2147–2156. [DOI] [PubMed] [Google Scholar]
- 44. Zhang Z, Zhang H, Song G, Zheng T, Ni Q, Feng H. Increased femoral anteversion is associated with inferior clinical outcomes after MPFL reconstruction and combined tibial tubercle osteotomy for the treatment of recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2261–2269. [DOI] [PubMed] [Google Scholar]


