Abstract
Background:
Assessments of the effects of realignment using opening-wedge high tibial osteotomy (OWHTO) on the medial, lateral, and patellofemoral compartments have been limited to cartilage evaluations.
Purpose/Hypothesis:
The purpose was to evaluate the effects of OWHTO on the meniscus and cartilage of each compartment as a cooperative unit (meniscochondral unit) using serial magnetic resonance imaging (MRI). It was hypothesized that (1) favorable changes in the meniscochondral unit would occur in the medial compartment and (2) that changes in the patellofemoral and lateral compartments would be negligible.
Study Design:
Case series; Level of evidence, 4.
Methods:
Included were 36 knees that underwent OWHTO from March 2014 to February 2016 and had postoperative serial MRI. The MRI was performed at 19.9 ± 7.4 and 52.3 ± 8.3 months postoperatively, and the cartilage and meniscal changes were evaluated by highlighting the regions of interest. We evaluated the T2 relaxation times of each cartilage and meniscal area, the cross-sectional area of the menisci, and the extrusion of the medial meniscus (MM). The meniscochondral unit was assessed using subgroup analyses according to the status of the MM.
Results:
Significant decreases were seen in T2 relaxation times in the medial femoral condyle (MFC) (P < .001) and medial tibial plateau (MTP) (P = .050), and significant increases were seen in the lateral femoral condyle (LFC) (P = .036). The change was more prominent in the MFC compared with the MTP and LFC (P = .003). No significant changes were observed in the lateral tibial plateau, patella, or trochlear groove. The area of the lateral meniscus (body and posterior horn) was decreased compared with preoperative MRI (P < .001 for both). The extent of MM extrusion decreased between the preoperative, first follow-up, and second follow-up MRIs (P < .001).
Conclusion:
OWHTO affected the medial compartment positively, the lateral compartment negatively, and the patellofemoral compartment negligibly. The effects were more prominent and consistent in the medial than in the lateral compartment.
Keywords: cartilage, magnetic resonance imaging, meniscus, opening wedge high tibial osteotomy, T2 relaxation time
Early medial knee osteoarthritis (OA) is often accompanied by knee varus deformity. It makes opening-wedge high tibial osteotomy (OWHTO) a rational approach to delay disease progression and reduce pain by altering the load distribution through the knee joint. 16,21,23 Several studies have reported on the effect of realignment using OWHTO on cartilage quality in the knee joint. 17,24,26 These studies attempted to observe the medial, lateral, and patellofemoral compartment status through follow-up magnetic resonance imaging (MRI) and second-look arthroscopy. However, the studies have been limited mostly to the cartilage status.
The cartilage and meniscal function in a cooperative manner for the maintenance of knee joint function. Loss of meniscal tissue can also lead to the deterioration of chondroprotective roles, thus accelerating cartilage degeneration. 11,20,30 Therefore, some trials have explored the relationship between meniscal lesions and cartilage loss. 6,20 MRI can be a noninvasive and excellent technique for the simultaneous evaluation of the cartilage and meniscus. Quantitative MRI has been increasingly applied for the evaluation of the success of joint-preserving OA therapies because it can detect the deterioration of cartilage composition. 25,33,34 A well-validated and widely used quantitative MRI technique for the articular cartilage is T2 mapping, which measures collagen content and network integrity, expressed as T2 relaxation times. 8 Clinical studies using T2-mapping images have demonstrated that increased T2 values correlate with the degree of cartilage degeneration. 2,14
Several studies have reported the fractional results of quantitative MRI after OWHTO in patients with varus-malaligned, early stage, medial compartment OA. 17,24,32 In those studies, cartilage thickness in the medial femoral condyle (MFC) was increased and the T2 relaxation time of the MFC was decreased significantly after surgery. 24,34 In addition, axial load shifting after OWHTO can affect not only the cartilage but also the meniscus. Because the meniscus plays a crucial role in the long-term health of the knee, it is important to understand the changes that occur over time in the cartilage and meniscus after OWHTO in patients with early OA. Therefore, the concept of the meniscochondral unit can be used to analyze how the individual status of the meniscus and cartilage affect each other.
The purpose of this study was to evaluate the effects of medial OWHTO on each compartment by examining the meniscus and cartilage of each compartment as a cooperative unit (meniscochondral unit) with serial MRI assessments up to the midterm follow-up. The hypotheses of this study were that (1) favorable changes in the meniscochondral unit would occur in the medial compartment after OWHTO and (2) changes in the patellofemoral and lateral compartments would be negligible.
Methods
Patients
Included in this study were 36 consecutive knees (32 patients) that underwent biplanar OWHTO from March 2014 to February 2016 followed by serial MRI assessments during follow-up. The flowchart for enrollment is shown in Figure 1. There were 4 patients who underwent OWHTO on both knees; the remaining 28 were patients who received unilateral OWHTO because 1 knee was asymptomatic without severe deformity. The inclusion criteria were as follows: (1) primary degenerative OA, (2) radiographic evidence of prominent medial compartmental OA of Kellgren-Lawrence (K-L) grades 1 to 3, (3) concurrent varus deformity of the lower limb (5° to 15° varus deformity), and (4) patients who underwent serial MRIs more than 2 times after surgery. The exclusion criteria were as follows: (1) history of joint infection, (2) symptomatic OA of the lateral compartment, (3) history of ligament surgery, (4) combined ligament injury, (5) double osteotomy (combined distal femoral osteotomy), and (6) revision OWHTO. The study protocol received institutional review board approval from our hospital.
Figure 1.
Flowchart for study selection. ACLR, anterior cruciate ligament reconstruction; HTO, high tibial osteotomy; MRI, magnetic resonance imaging; OWHTO, opening-wedge high tibial osteotomy.
The preoperative patient demographics and clinical and radiologic data are summarized in Table 1. Of the patients, 75% (24/32) were women. The mean patient age was 55.8 ± 4.4 years, and the mean body mass index was 26.8 ± 3.6 kg/m2. Concurrent surgeries (microfracture, meniscectomy, and meniscal repair) that affect MRI evaluation were assessed. Concurrent microfracture was performed in the MFC (21 knees) and medial tibial plateau (MTP) (9 knees). For the management of medial meniscal (MM) tears, partial meniscectomy (16 knees) and meniscal repair (5 knees) were performed. Partial lateral meniscal (LM) meniscectomy was performed in LM tears (6 knees) and discoid LM (2 knees).
TABLE 1.
Demographics, Preoperative Clinical, and Radiographic Data a
| Variable | Value |
|---|---|
| Age, years | 55.8 ± 4.4 |
| Sex, male/female | 10/26 |
| Body mass index (kg/m2) | 26.8 ± 3.6 |
| HKA angle | Varus 7.1° ± 1.46° |
| WBL ratio (%) | 20.23 ± 10.97 |
| K-L grade, 1/2/3 | 12/14/10 |
| Flexion contracture | 8.1° ± 4.1° |
| Further flexion | 117.2° ± 6.1° |
a Data are presented as mean ± SD or No. HKA, hip-knee-ankle; K-L, Kellgren-Lawrence; WBL, weightbearing line.
Radiographic and Clinical Evaluation
Full-length standing anteroposterior radiographs were obtained preoperatively, immediately after the index surgery, and at the final follow-up for routine evaluation. The preoperative hip-knee-ankle (HKA) angle, weightbearing line (WBL) ratio, and K-L grade were evaluated. To calculate the HKA angle, we used the angle between a line drawn from the center of the femoral head to the center of the knee and a line drawn from the center of the knee to the center of the talus. The WBL ratio was calculated as the percentage of the crossing point of the mechanical axis from the medial edge of the tibial plateau to the entire width of the tibial plateau.
The clinical outcomes were assessed preoperatively and at the postoperative final follow-up, 50.2 ± 7.0 months after surgery. Range of motion, including flexion contracture and maximal flexion, was measured using a goniometer with the patient in the supine position. The American Knee Society Score (AKSS; knee and function scores) was used to assess the degree of OA of the knee. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score was used to assess 5 items on pain, 2 items on stiffness, and 17 items on physical function. In addition, we evaluated 8 health concepts using the 36-Item Short Form Health Survey (SF-36): limitations in physical activities because of health problems; limitations in social activities because of physical or mental health problems; limitations in usual role activities because of physical health problems; bodily pain; general mental health; limitations in usual role activities because of mental health problems; vitality (energy and fatigue); and general health perceptions.
Surgical Technique
All surgeries were performed by a single author (Y.S.L.). An incision of approximately 5 cm was made longitudinally at the anteromedial aspect of the proximal tibia. After dissecting the subcutaneous area, the superior border of the pes anserinus and the anterior border of the medial collateral ligament were mobilized from the tibia and released by inserting a periosteal elevator. A protective cutting system was used with intraoperative fluoroscopy guidance. Horizontal osteotomy was performed along guiding pins in an effort to preserve the lateral cortex. After biplanar osteotomy, the osteotomy site was distracted in accordance with the preoperative plan, and fixation was performed using a long locking plate (Decisive Wedge Locking Plate; TDM). All patients underwent arthroscopy at the time of OWHTO. The arthroscopic procedures included joint debridement, meniscectomy of MM tears, removal of loose bodies, and microfracture.
Serial MRI Evaluation
All MRI scans were obtained using a 3-T magnetic resonance scanner (Achieva; Philips Medical Systems). MRI was performed preoperatively and at the follow-up assessments (first follow-up MRI, 19.9 ± 7.4 months; second follow-up MRI, 52.3 ± 8.3 months). A 3-dimensional (3-D) multiecho spin-echo T2-weighted sequence was used (repetition time/echo time, 3500 milliseconds/13, 26, 39, 52, 65, 78, and 91 milliseconds; field of view, 140 × 170 mm; pixel matrix, 420 × 260; 20 sections, 3-mm section thickness; 1 acquired signal, 5 minutes 18 s total acquisition time) to generate a sagittal T2 relaxation time map. Quantitative T2 maps were analyzed using data obtained throughout the knee joint in a dedicated software (IntelliSpace Portal; Philips Medical Systems). The T2 maps were color coded from 1 to 81 milliseconds on a pixel-by-pixel basis and shown as a fused overlay on the original data with an echo time of 13 milliseconds.
Cartilage Evaluation
Regions of interest (ROIs) were drawn manually to delineate the cartilage areas on the T2-mapping images, so that they encompassed the entire thickness of the cartilage. The mean T2 relaxation time was measured over the MFC, lateral femoral condyle (LFC), MTP, lateral tibial plateau (LTP), patella, and trochlear groove (TG) (Figure 2). To reduce artifacts near the bone-cartilage interface, ROIs on the medial and lateral compartments (MFC, MTP, LFC, and LTP) were drawn at the most prominent point of each femoral condyle and tibial plateau using the coronal image to match the slices. In the patellofemoral compartment, ROIs were drawn on the ridge of the patella and the deepest point of the TG, and the T2 relaxation time was measured.
Figure 2.

Regions of interest were drawn manually to delineate cartilage areas of the T2 mapping images. The T2 maps were color-coded on the drawn regions of interest (ROIs) from 1 to 81 milliseconds on a pixel-by-pixel basis. (A, C, E) Scout images for selecting the cut that draws the ROIs. (B, D, F) Sagittal cuts of red dashed line points on A, C, and E images. The ROIs for the (B) medial and (D) lateral compartment were drawn at the most prominent point of each femoral condyle using the coronal scout images to match the slices (dashed lines in A and C). (F) The ROIs for the patellofemoral compartment were drawn on the ridge of the patella (dashed line in E) and the deepest point of the trochlear groove.
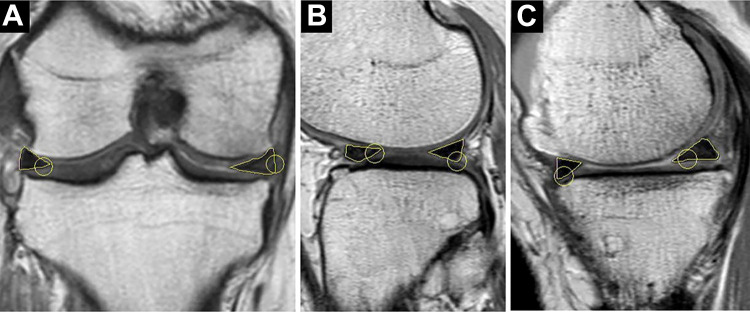
Meniscal Evaluation
For the evaluation of the T2 relaxation time in the meniscus, 4 ROIs were defined per patient: anterior horn of the medial meniscus (MMAH), posterior horn of the medial meniscus (MMPH), anterior horn of the lateral meniscus (LMAH), and posterior horn of lateral meniscus (LMPH) (Figure 3). The meniscal body was excluded because of partial volume effects, which were characterized by a change in the signal intensity of the meniscus compared with the signal intensity of the adjacent sections. 36 The anatomic landmarks defined for the segmentation of the meniscus have been previously described. 29
Figure 3.
Evaluation of T2 relaxation time in the medial and lateral menisci. The regions of interest (ROIs) were drawn separately on the anterior and posterior horn of the (A) medial meniscus and (B) lateral meniscus. The T2 maps were color- coded on the drawn ROIs from 1 to 81 milliseconds on a pixel-by-pixel basis.
The cross-sectional area of each meniscal segment (body, anterior, and posterior horn) and the extent of extrusion of the MM were also measured in the preoperative, first follow-up, and second follow-up MRI assessments (Figure 4). MRI scout views, obtained using T2-weighted imaging in the coronal and axial planes, were used to select the correct image for the setting of the ROIs. Most central images were identified through the MM and LM, defined as the sagittal slice depicting the maximum width of the anterior horn and posterior horn as individual triangles along with the neighboring slices. 10 The same process was used for both the MM and LM. The extent of MM extrusion was measured from the medial margin of the tibial plateau to the medial margin of the MM on the image at the midpoint of the femoral condyle (Figure 5). 35
Figure 4.
Measuring the cross-sectional area of the meniscus. The (A) meniscal body, (B) anterior and posterior horn were segmented separately for the lateral (B) and medial (C) meniscus, and the cross-sectional area of each segment was measured using regions of interest drawn by hand.
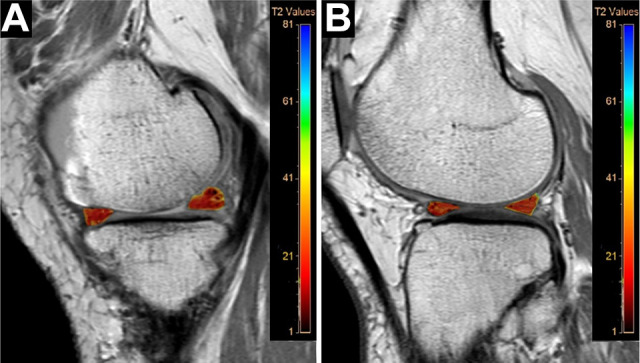
Figure 5.

The extent of the medial meniscal extrusion on magnetic resonance imaging. The extent of medial meniscal extrusion was measured from the medial margin of the tibial plateau (right yellow arrow) to the medial margin of the medial meniscus (left yellow arrow) on the image at the midpoint of the medial femoral condyle.
Intrarater and Interrater Reliability
Reliability was evaluated for all quantitative measurements of each cartilage and meniscal region. First, under the supervision of an experienced musculoskeletal radiologist (Y.S.K.), the MRI image number to be used for each measurement was assigned. After that, the average T2 relaxation time, meniscal area, and extrusion of MM were measured within the specified image at each interval. Two observers (H.G.C. and J.S.K., sports medicine fellows) performed the quantitative evaluation. Measurements were performed 2 times within a 6-week interval to evaluate intraobserver reliability.
Meniscochondral Unit Analysis
To evaluate the correlation and interaction between the meniscus and cartilage, subgroup analysis was performed according to the MM status. The MM-preserved group included the following cases under the concept that the width of the MM was preserved: (1) the case of intact MM without tears, (2) those with a small size fraying on the inner side that requires simple debridement, and (3) the case of repaired MM tears. The MM-meniscectomy group included cases in which more than one-third of the full width of the MM was resected or in which the continuity of the meniscus was destroyed. The delta T2 relaxation time of each cartilage region, calculated by subtracting the T2 relaxation time of the second follow-up MRI from the T2 relaxation time of the first follow-up MRI, was used for a comparison between subgroups.
Statistical Analysis
The intra- and interobserver reliability of measurements was assessed using intraclass correlation coefficients (ICCs) calculated with the 1-way random-effects model, in which ICC <0.40 indicates poor agreement, 0.40 to 0.75 indicates fair to good (moderate) agreement, and 0.76 to 1.00 indicates excellent agreement. A paired t test was performed to compare the change in T2 relaxation times between the first and second follow-up MRIs. The cross-sectional area of each meniscus and extrusion of MM on preoperative, first, and second follow-up MRIs was compared using 1-way repeated-measures analysis of variance (ANOVA). A Bonferroni post hoc analysis was used to determine which time points were statistically significant on the ANOVA evaluation. The Student t test was used to compare the difference in T2 relaxation time between 2 subgroups: MM-preserved and MM-meniscectomy. Data were analyzed using SPSS statistical software (Version 25.0; IBM).
Results
Radiographic and Clinical Outcomes
Regarding the reliability of the MRI assessments, the intra- and interobserver agreements were considered good (ICC range, 0.711-0.746). In terms of postoperative alignment after OWHTO, the WBL ratio and HKA angle improved from preoperatively to final follow-up (P = .001 and P = .002, respectively). At the final follow-up, flexion contracture and maximal flexion improved compared with the preoperative status (P = .001 and P = .010, respectively). All clinical scores including WOMAC, AKSS, SF-36 physical component summary, and SF-36 mental component summary improved at the final follow-up (P = .002, P < .001, P < .001, and P < .001, respectively) (Table 2).
TABLE 2.
Radiographic and Clinical Outcomes a
| Preoperative | Final Follow-up | P | |
|---|---|---|---|
| WBL ratio, % | 16.5 ± 9.5 | 62.8 ± 6.4 | .001 |
| HKA angle | 7.1° ± 1.5° varus | 1.2° ± 1.1° valgus | .002 |
| Flexion contracture | 8.1° ± 4.1° | 1.8° ± 2.8° | .001 |
| Maximal flexion | 117.2° ± 6.1° | 134.0° ± 4.8° | .010 |
| WOMAC | |||
| Total | 39.1 ± 12.4 | 10.1 ± 6.4 | .002 |
| Pain | 9.6 ± 3.4 | 1.6 ± 1.4 | <.001 |
| Stiffness | 4.2 ± 2.5 | 1.2 ± 0.9 | .001 |
| Function | 25.3 ± 9.7 | 7.3 ± 4.6 | <.001 |
| AKSS | |||
| Knee | 52.4 ± 13.1 | 89.2 ± 10.6 | <.001 |
| Function | 54.9 ± 12.4 | 88.7 ± 10.4 | .002 |
| SF-36 | |||
| Physical | 39.2 ± 8.6 | 86.5 ± 11.4 | <.001 |
| Mental | 42.5 ± 12.1 | 88.1 ± 11.2 | <.001 |
a Values are presented as mean ± SD. Bolded P values indicate statistically significant difference between preoperative and final follow-up (P < .05). AKSS, American Knee Society Score; HKA, hip-knee-ankle angle; SF-36, 36-Item Short Form Health Survey; WBL, weightbearing line ratio; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Cartilage
The T2 relaxation times decreased significantly between the first and second follow-up MRI for the MFC (P < .001) and MTP (P = .050). In the lateral compartment, the T2 relaxation time of the LFC was significantly increased in the second follow-up MRI compared with the first follow-up MRI (P = .036). The delta values of the MFC, MTP, and LFC were 13.9 ± 3.3, 4.8 ± 2.4, and -1.9 ± 1.4 milliseconds, respectively. Among them, the absolute delta value was the smallest in the LFC and significantly smaller than that in the MFC (P = .003). In the LTP and patellofemoral compartment, no significant change in T2 relaxation time was observed (LTP, P = .821; patella, P = .818; and TG, P = .956) (Table 3).
TABLE 3.
Change in T2 Relaxation Time of Each Cartilage and Meniscal Region a
| T2 Relaxation Time, milliseconds | ||||
|---|---|---|---|---|
| First MRI (19.9 ± 7.4 months) |
Second MRI (52.3 ± 8.3 months) |
Δ First vs Second MRI | P | |
| Cartilage regions | ||||
| MFC | 61.4 ± 15.8 | 47.5 ± 14.8 | 13.9 ± 3.3 | <.001 |
| MTP | 31.1 ± 10.7 | 26.3 ± 6.5 | 4.8 ± 2.4 | .050 |
| LFC | 47.2 ± 8.7 | 49.1 ± 7.3 | -1.9 ± 1.4 | .036 |
| LTP | 27.3 ± 9.7 | 27.7 ± 7.0 | -0.5 ± 1.1 | .821 |
| Patella | 40.2 ± 8.6 | 39.8 ± 7.6 | 0.4 ± 1.3 | .818 |
| TG | 52.1 ± 10.7 | 52.2 ± 10.9 | -0.2 ± 0.9 | .956 |
| Meniscal regions | ||||
| MMAH | 24.2 ± 10.0 | 23.8 ± 9.9 | 0.8 ± 1.1 | .841 |
| MMPH | 32.2 ± 15.7 | 30.5 ± 10.8 | 1.7 ± 1.3 | .426 |
| LMAH | 25.1 ± 13.5 | 26.2 ± 7.8 | -1.1 ± 2.1 | .610 |
| LMPH | 17.9 ± 9.7 | 20.9 ± 9.4 | -2.9 ± 0.7 | .154 |
a Data are presented as mean ± SD. Bolded P values indicate statistically significant difference between first and second MRI (P < .05). LFC, lateral femoral condyle; LMAH, lateral meniscus anterior horn; LMPH, lateral meniscus posterior horn; LTP, lateral tibial plateau; MFC, medial femoral condyle; MMAH, medial meniscus anterior horn; MMPH, medial meniscus posterior horn; MRI, magnetic resonance imaging; MTP, medial tibial plateau; TG, trochlear groove.
Meniscus
The T2 relaxation times of each meniscal component did not significantly change between the first and second follow-up. In the cross-sectional area of the MM component, the area of the MMAH, MM body, and MMPH was not significantly different between the 3 MRI acquisitions (Table 4). In the LM component, the measured cross-sectional area of the LM body and LMPH significantly decreased over time (P = .033 and P = .005, respectively). In addition, the extent of MM extrusion significantly decreased compared with the preoperative MRI (P < .001).
TABLE 4.
Changes in Cross-Sectional Area and MM Extrusion a
| Preoperative | First MRI | Second MRI | P | |
|---|---|---|---|---|
| MMAH, mm2 | 20.7 ± 7.4 | 21.7 ± 7.8 | 22.6 ± 7.4 | .142 |
| MM body, mm2 | 21.8 ± 8.9 | 22.7 ± 9.3 | 23.9 ± 9.4 | .188 |
| MMPH, mm2 | 24.4 ± 9.8 | 25.9 ± 10.2 | 24.5 ± 12.1 | .450 |
| LMAH, mm2 | 23.5 ± 7.5 | 21.9 ± 8.2 | 21.2 ± 8.0 | .120 |
| LM body, mm2 | 29.6 ± 9.6 | 28.9 ± 9.6 | 25.7 ± 7.6 | .033 |
| LMPH, mm2 | 23.9 ± 8.9 | 22.7 ± 9.0 | 20.1 ± 6.3 | .005 |
| MM extrusion, mm | 5.3 ± 1.6 | 4.9 ± 1.8 | 3.9 ± 1.8 | <.001 |
a Values are presented as mean ± SD. Bolded P values indicate statistically significant difference between groups (P < .05, Bonferroni correction for multiple comparisons). LM, lateral meniscus; LMAH, lateral meniscus anterior horn; LMPH, lateral meniscus posterior horn; MM, medial meniscus; MMAH, medial meniscus anterior horn; MMPH, medial meniscus posterior horn; MRI, magnetic resonance imaging.
The Bonferroni post hoc analysis of the MRI time points showed that a significant change occurred in the LM body between the preoperative and first follow-up MRI (P < .001), but not between the other times. In the LMPH, significant changes occurred in the first follow-up MRI (P < .001) and second follow-up MRI (P = .005) compared with the preoperative MRI. The post hoc analysis of MM extrusion showed a significant difference between the preoperative, first follow-up, and second follow-up MRI (P = .001, P < .001, and P < .001, respectively) (Table 5).
TABLE 5.
Post Hoc Analysis: LM body, LMPH, and MM Extrusion a
| LM body, mm2 | LMPH, mm2 | MM extrusion, mm | ||||
|---|---|---|---|---|---|---|
| Δ | P | Δ | P | Δ | P | |
| Preoperative vs first MRI | 0.67 | <.001 | 1.26 | <.001 | 0.40 | .001 |
| Preoperative vs second MRI | 3.93 | .067 | 3.87 | .005 | 1.43 | <.001 |
| First MRI vs second MRI | 3.26 | .164 | 2.60 | .087 | 1.02 | <.001 |
a Bold P values indicate statistically significant difference between groups compared (P < .05). LM, lateral meniscus; LMPH, lateral meniscus posterior horn; MM, medial meniscus; MRI, magnetic resonance imaging.
Meniscochondral Unit
Table 6 shows the results of the subgroup analysis comparing the change in T2 relaxation times (first vs second follow-up MRIs) between the MM-preserved group (20 knees) and the MM-meniscectomy group (16 knees). The delta value for the MFC was larger in the MM-preserved group (20.0 ± 12.6 milliseconds) than in the MM-meniscectomy group (15.9 ± 10.7 milliseconds); however, this difference was not statistically significant (P = .054). Further, no significant difference was found between the 2 groups in the delta T2 relaxation times of the other cartilage areas (Table 6).
TABLE 6.
Subgroup Analysis for the Meniscochondral Unit: MM-Preserved vs MM-Meniscectomy Group a
| T2 Relaxation Time, milliseconds | |||
|---|---|---|---|
| First vs second MRI, Δ | MM-Preserved (n = 20 knees) b |
MM-Meniscectomy (n = 16 knees) |
P |
| MFC | 20.0 ± 12.6 | 15.9 ± 10.7 | .054 |
| MTP | 4.8 ± 1.7 | 4.91 ± 1.1 | .980 |
| LFC | -1.6 ± 4.9 | -1.9 ± 3.2 | .649 |
| LTP | 1.0 ± 1.1 | 0.90 ± 1.9 | .096 |
| Patella | 2.4 ± 1.1 | 2.7 ± 0.9 | .072 |
| TG | 1.4 ± 1.4 | 1.3 ± 1.2 | .871 |
a Data are presented as mean ± SD. LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femoral condyle; MM, medial meniscus; MTP, medial tibial plateau; TG, trochlear groove.
b The MM-preserved group included cases of intact MM without tear, small-size fraying on the inner side that required simple debridement, and repaired MM tear.
Discussion
The principal findings of this study were that the T2 relaxation time was significantly decreased in the MFC and MTP and increased in the LFC, which was evaluated by serial MRI assessments up to the midterm follow-up. However, the change was more prominent in the medial compartment (MFC and MTP) than in the LFC. OWHTO improved MM extrusion in the medial compartment but had a negative effect on the LM body and LMPH. The positive effect of MM extrusion consistently improved during serial MRI assessments; however, the negative effects on the LM body and LMPH were not progressive. In the subgroup analysis for the concept of the meniscochondral unit, the reduction of the T2 relaxation time on the MFC showed a trend toward being greater in the MM-preserved group than in the MM-meniscectomy group, although the difference was not statistically significant.
OWHTO is a popular surgical procedure in the management of medial unicompartmental knee OA. 21,23 Medial OWHTO can delay the progression of degeneration and deformity due to pathology existing in the medial compartment by shifting the axial load laterally. 17,24,26 Therefore, patients with indications for OWHTO often have accompanying intra-articular pathologies, such as in the meniscus and cartilage. 17,26 MRI not only enables the direct visualization of joint structures such as the meniscus and cartilage but also allows the quantitative assessment of changes over time. A well-validated and widely used quantitative MRI technique for articular cartilage is T2 mapping, which measures collagen content and network integrity, expressed as T2 relaxation times. 8,14,24,36 Buckwalter and Mankin 5 have reviewed the mechanism of cartilage degradation in detail and have described the initial stage of OA changes to increase water mobility in the cartilage. Furthermore, Lüssea et al 19 demonstrated a positive correlation between increases in T2 relaxation time and cartilage water content in ex vivo cartilage from patients with OA who underwent total knee replacement surgery. In contrast, Dunn et al 9 reported that underlying cartilage changes leading to higher T2 values that occur in early OA do not progress as much as degenerative changes; hence, very little difference is seen between patients with mild OA and those with severe OA.
Compared with the articular cartilage, which has a type 2 collagen concentration of 10% to 20%, the meniscus has a type 1 collagen concentration of 15% to 25%. 22 The higher collagen concentration in the meniscus may partly explain the lower meniscal T2 values than the cartilage T2 values. T2 mapping allows a relatively wide range of echo times, with echo time values short enough to assess the meniscus but long enough to assess the articular cartilage. 18,25,28 In this study, the preoperative average T2 relaxation times of the MMAH (24.2 ± 10.0 millseconds), MMPH (32.2 ± 15.7 millseconds), LMAH (25.1 ± 13.5 millseconds), and LMPH (17.9 ± 9.7 millseconds) were relatively lower than those of the femoral (MFC, 61.4 ± 15.8 millseconds; LFC, 47.2 ± 8.7 millseconds) and patellofemoral (patella, 40.2 ± 8.6 millseconds; TG, 52.1 ± 10.7 millseconds) cartilage. In the study by Rauscher et al, 29 the meniscal T2 values of control participants were significantly different from those of the OA groups. In this study, the T2 relaxation times of both the MM and the LM were not changed significantly in the serial MRI assessments. This means that the meniscal tissue deterioration effect according to OWHTO was not significant. However, the meniscal fibrocartilage contains a dense and multidirectional network of longitudinally organized collagen fibers. 27 The 3-D organization of the collagen network limits water mobility and causes a magic angle effect during the measurement of the T2 relaxation time. 13 Because of these characteristics, it seems necessary to conduct further research on a larger scale using more diverse protocols.
The position, integrity, and volume of the meniscus may play a pivotal role in OA development and progression. 7,10,35,36 In this study, the cross-sectional area was measured at the anterior, body, and posterior horns of the MM and LM to indirectly evaluate changes in meniscal volume over time after OWHTO. The cross-sectional area of the MM (MMAH, body, and MMPH) was not changed significantly; that of the LM body and LMPH decreased significantly over time. Post hoc analysis showed that the cross-sectional area of the LM body significantly decreased between the preoperative and first follow-up MRI, and the cross-sectional area of the LMPH decreased significantly in the first and second follow-up MRI compared with that in the preoperative MRI assessment. This was considered to be the result of 8 cases of LM partial meniscectomy (6 cases of LM tear and 2 cases of discoid LM) performed simultaneously at the time of surgery, indicating that the serial changes after surgery were insignificant.
Meniscal extrusion, a condition in which partial or full meniscal displacement uncovers the cartilage, represents another meniscal pathology that may coexist with meniscal tears in knee OA. 1,7,12 Meniscal extrusion can indicate disruption of meniscal hoop tension. A previous study reported that an MM extrusion of ≥ 3 mm was associated strongly with degenerative joint disease. 31 In this study, the results of MM extrusion decreased with time after OWHTO, and all were significant between the 3 time points in post hoc analysis. Because MM extrusion is related to the disruption of meniscal hoop tension, which affects future degenerative changes, the results of this study suggest the preventive effect of OWHTO against OA progression.
The cartilage and meniscus cooperate to maintain the knee joint. Previous studies have demonstrated a relationship between meniscal lesions and the development and progression of knee OA. 3,4,11,15,30 Therefore, some effort has been made to explore the relationship between meniscal lesions and cartilage loss. 6,20 Lynch et al 20 found that in knees with OA or at a high risk of developing OA, medial cartilage score worsening was associated with MM tears. In this study, subgroup analyses were performed according to the concept of the meniscochondral unit. The absolute delta T2 relaxation time of the MFC showed a trend toward being larger in the MM-preserved group than in the MM-meniscectomy group, although the difference was not statistically significant.
This study had some strengths. Serial quantitative MRI assessments over a midterm follow-up were performed in all compartments. We also simultaneously evaluated the meniscus and cartilage as a cooperative unit, which was named the meniscochondral unit. Thus, the results provided insights not only on how alignment correction affects the cartilage and meniscus of each compartment but also on the kind of interaction between the cartilage and meniscus over time.
This study also had several limitations that should be considered. First, the sample size was small. Because MRI is a relatively expensive evaluation method, all serial MRI assessments were performed only when the patients voluntarily underwent the procedure. In future studies, a design with a smaller selection bias by securing a larger sample size will be needed. Second, serial MRI assessments were performed at slightly different times for each patient, not at a certain point after surgery. This can cause differences in the status of the meniscus and cartilage. Third, a comparison of the T2 relaxation time between the preoperative MRI and serial follow-up MRI assessments could not be performed because preoperative MRI evaluations were performed at different institutions without quantitative T2 maps. Fourth, because of the characteristics of the study design, there was no control group to compare with.
Conclusion
With a focus on the cartilage and meniscus, OWHTO affects the medial compartment positively, the lateral compartment negatively, and the patellofemoral compartment negligibly. The effects were more prominent and consistent in the medial compartment than in the lateral compartment in this study.
Footnotes
Final revision submitted June 1, 2021; accepted July 5, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Seoul National University Bundang Hospital (study No. B-2006/621-112).
References
- 1. Adams J, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54(8):502–506. [DOI] [PubMed] [Google Scholar]
- 2. Baum T, Joseph G, Karampinos D, et al. Cartilage and meniscal T2 relaxation time as non-invasive biomarker for knee osteoarthritis and cartilage repair procedures. Osteoarthritis Cartilage. 2013;21(10):1474–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berthiaume M-J, Raynauld J-P, Martel-Pelletier J, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64(4):556–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Biswal S, Hastie T, Andriacchi TP, et al. Risk factors for progressive cartilage loss in the knee: a longitudinal magnetic resonance imaging study in forty-three patients. Arthritis Rheum. 2002;46(11):2884–2892. [DOI] [PubMed] [Google Scholar]
- 5. Buckwalter J, Mankin H. Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect. 1998;47:487–504. [PubMed] [Google Scholar]
- 6. Chang A, Moisio K, Chmiel JS, et al. Subregional effects of meniscal tears on cartilage loss over 2 years in knee osteoarthritis. Ann Rheum Dis. 2011;70(1):74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. [DOI] [PubMed] [Google Scholar]
- 8. David-Vaudey E, Ghosh S, Ries M, Majumdar S. T2 relaxation time measurements in osteoarthritis. Magn Reson Imaging. 2004;22(5):673–682. [DOI] [PubMed] [Google Scholar]
- 9. Dunn TC, Lu Y, Jin H, Ries MD, Majumdar S. T2 relaxation time of cartilage at MR imaging: comparison with severity of knee osteoarthritis. Radiology. 2004;232(2):592–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eijgenraam SM, Bovendeert FA, Verschueren J, et al. T 2 mapping of the meniscus is a biomarker for early osteoarthritis. Eur Radiol. 2019;29(10):5664–5672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Englund M, Guermazi A, Roemer FW, et al. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: the Multicenter Osteoarthritis Study. Arthritis Rheum. 2009;60(3):831–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gale D, Chaisson C, Totterman S, et al. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage. 1999;7(6):526–532. [DOI] [PubMed] [Google Scholar]
- 13. Goodwin DW, Zhu H, Dunn JF. In vitro MR imaging of hyaline cartilage: correlation with scanning electron microscopy. AJR Am J Roentgenol. 2000;174(2):405–409. [DOI] [PubMed] [Google Scholar]
- 14. Hirose J, Nishioka H, Nakamura E, et al. T1ρ and T2 mapping of the proximal tibiofibular joint in relation to aging and cartilage degeneration. Eur J Radiol. 2012;81(10):2776–2782. [DOI] [PubMed] [Google Scholar]
- 15. Hunter D, Zhang Y, Niu J, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54(3):795–801. [DOI] [PubMed] [Google Scholar]
- 16. Kim H-J, Shin J-Y, Lee H-J, et al. Can medial stability be preserved after open wedge high tibial osteotomy? Knee Surg Relat Res. 2020;32(1):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee O-S, Lee SH, Mok SJ, Lee YS. Comparison of the regeneration of cartilage and the clinical outcomes after the open wedge high tibial osteotomy with or without microfracture: a retrospective case control study. BMC Musculoskelet Disord. 2019;20(1):267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Li X, Cheng J, Lin K, et al. Quantitative MRI using T1ρ and T2 in human osteoarthritic cartilage specimens: correlation with biochemical measurements and histology. Magn Reson Imaging. 2011;29(3):324–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lüssea S, Claassen H, Gehrke T, et al. Evaluation of water content by spatially resolved transverse relaxation times of human articular cartilage. Magn Reson Imaging. 2000;18(4):423–430. [DOI] [PubMed] [Google Scholar]
- 20. Lynch JA, Javaid MK, Roemer F, et al. Associations of medial meniscal tear and extrusion with the sites of cartilage loss in the knee: results from the MOST study. Abstract. Arthritis Rheum 2008;58:S235–S236. [Google Scholar]
- 21. Mirouse G, Dubory A, Roubineau F, et al. Failure of high tibial varus osteotomy for lateral tibio-femoral osteoarthritis with <10 degrees of valgus: outcomes in 19 patients. Orthop Traumatol Surg Res. 2017;103(6):953–958. [DOI] [PubMed] [Google Scholar]
- 22. Mow VC, Huiskes R. Basic Orthopaedic Biomechanics and Mechano-Biology. Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 23. Nha KW, Shin Y-S, Kwon HM, Sim JA, Na YG. Navigated versus conventional technique in high tibial osteotomy: a meta-analysis focusing on weight bearing effect. Knee Surg Relat Res. 2019;31(2):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nishioka H, Nakamura E, Hirose J, et al. MRI T1ρ and T2 mapping for the assessment of articular cartilage changes in patients with medial knee osteoarthritis after hemicallotasis osteotomy. Bone Joint Res. 2016;5(7):294–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Oei EH, van Tiel J, Robinson WH, Gold GE. Quantitative radiologic imaging techniques for articular cartilage composition: toward early diagnosis and development of disease-modifying therapeutics for osteoarthritis. Arthritis Care Res (Hoboken). 2014;66(8):1129–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Okahashi K, Fujisawa Y, Sugimoto K, Tanaka Y. Cartilage regeneration of knee OA after high tibial osteotomy. Tech Knee Surg. 2010;9(2):95–100. [Google Scholar]
- 27. Peterfy C, Janzen D, Tirman P, et al. “Magic-angle” phenomenon: a cause of increased signal in the normal lateral meniscus on short-TE MR images of the knee. AJR Am J Roentgenol. 1994;163(1):149–154. [DOI] [PubMed] [Google Scholar]
- 28. Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage. 2008;16(12):1433–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rauscher I, Stahl R, Cheng J, et al. Meniscal measurements of T1ρ and T2 at MR imaging in healthy subjects and patients with osteoarthritis. Radiology. 2008;249(2):591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sharma L, Eckstein F, Song J, et al. Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum. 2008;58(6):1716–1726. [DOI] [PubMed] [Google Scholar]
- 31. Shelburne KB, Kim HJ, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29(2):223–231. [DOI] [PubMed] [Google Scholar]
- 32. Verschueren J, Meuffels DE, Bron EE, et al. Possibility of quantitative T2-mapping MRI of cartilage near metal in high tibial osteotomy: a human cadaver study. J Orthop Res. 2018;36(4):1206–1212. [DOI] [PubMed] [Google Scholar]
- 33. Welsch GH, Mamisch TC, Domayer SE, et al. Cartilage T2 assessment at 3-T MR imaging: in vivo differentiation of normal hyaline cartilage from reparative tissue after two cartilage repair procedures—initial experience. Radiology. 2008;247(1):154–161. [DOI] [PubMed] [Google Scholar]
- 34. Welsch GH, Trattnig S, Scheffler K, et al. Magnetization transfer contrast and T2 mapping in the evaluation of cartilage repair tissue with 3 T MRI. J Magn Reson Imaging. 2008;28(4):979–986. [DOI] [PubMed] [Google Scholar]
- 35. Yamagami R, Taketomi S, Inui H, Tahara K, Tanaka S. The role of medial meniscus posterior root tear and proximal tibial morphology in the development of spontaneous osteonecrosis and osteoarthritis of the knee. Knee. 2017;24(2):390–395. [DOI] [PubMed] [Google Scholar]
- 36. Zarins Z, Bolbos R, Pialat J, et al. Cartilage and meniscus assessment using T1rho and T2 measurements in healthy subjects and patients with osteoarthritis. Osteoarthritis Cartilage. 2010;18(11):1408–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]