Abstract
Background
Metatarsal fractures are among the most common foot and ankle injuries, with an annual incidence of 6.7 per 100 000 persons. Approximately 30% of metatarsal fractures affect the base of the fifth metatarsal bone. Nevertheless, no evidence-based treatment recommendations are available to date.
Methods
The three fracture localizations according to Lawrence and Botte (zone I, proximal to the intermetatarsal joint between the fourth and fifth metatarsal bones; zone II, in the area of the joint; zone III, at the distal end of the joint) are analyzed on the basis of a systematic literature search. Studies were included that compared the treatment of two types of fracture in the same manner, or that compared two different treatments for a single type of fracture.
Results
Nine studies compared different treatments of zone I fractures. Two of these were randomized controlled trials (RCTs); in one RCT, patients given functional therapy returned to work much sooner than those treated with immobilization (11 vs. 28 days; p = 0.001), with otherwise similar outcomes. The non-randomized studies revealed a faster return to full function (33 vs. 46 days; p<0.05) with early functional therapy, and similar outcomes for immobilization and surgery. One RCT that compared functional therapy with immobilization for zone II fractures revealed no statistically significant difference. Five studies compared fractures in zones I and II that were treated in the same manner, revealing similar outcomes. One RCT compared surgery and immobilization for zone III fractures: surgery led to statistically significant improvement of the outcome in all of the measured parameters.
Conclusion
Fractures in zones I and II should be treated with early functional therapy. There seems to be no reason to consider zone I and II fractures as two separate entities, as the outcomes in the two groups are similar. In contrast, fractures in zone III should primarily be treated surgically.
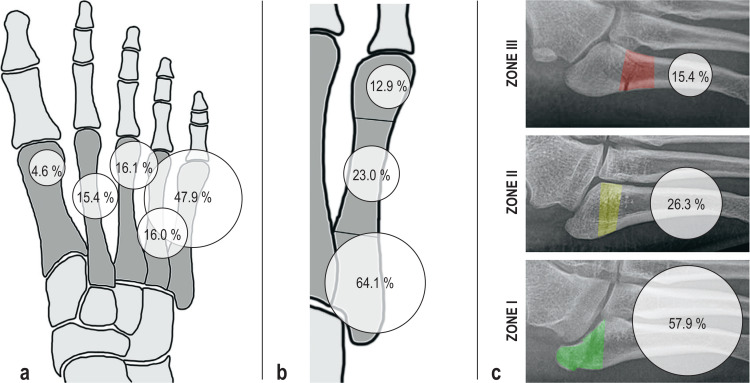
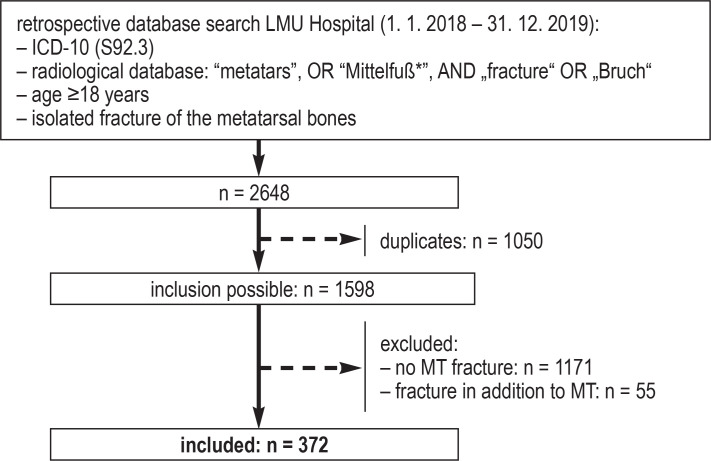
Metatarsal fractures are among the most common foot injuries, with an incidence of approx. 6.7 per 100 000 persons (1), with the base of the fifth metatarsal bone (MT5) being most commonly involved. For the present review, the authors conducted a retrospective analysis of their own patient population over a period of two years (eFlowchart). Of 372 isolated metatarsal fractures, 30% involved the base of MT5 (figure 1).
Figure 1.
Retrospective analysis of the distribution of metatarsal fractures within the authors’ own patient population. Schematic diagram of the distribution of fractures (a) of the metatarsals, (b) within the 5th metatarsal bone (base, shaft, distal) and (c) within the base of the 5th metatarsal (Lawrence and Botte three-zone classification [3])
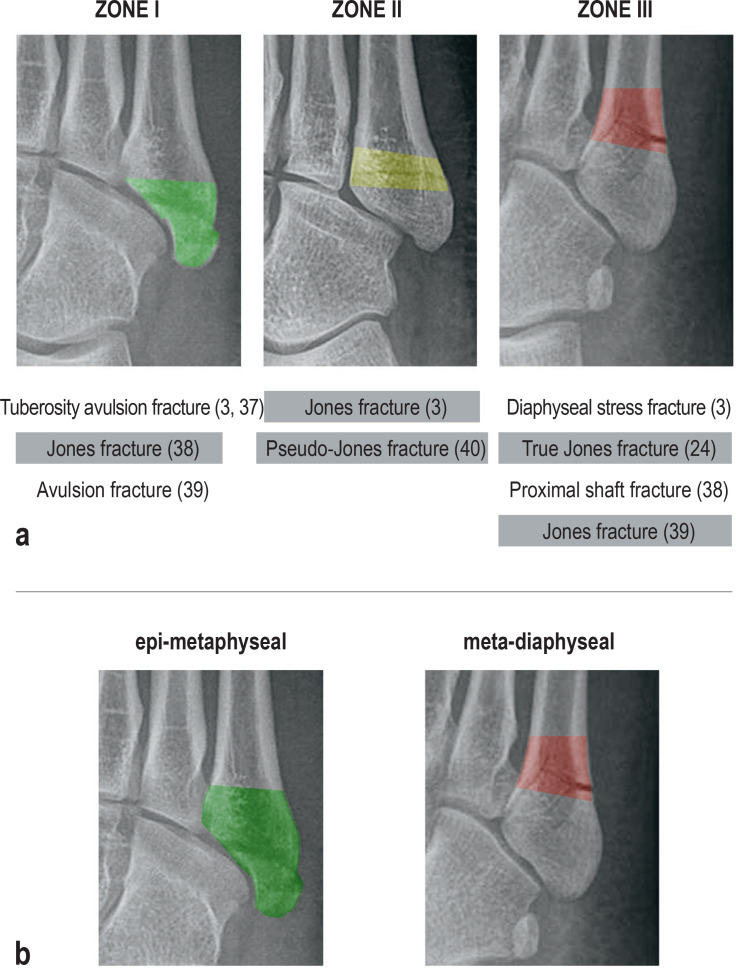
In 1902, Sir Robert Jones proved for the first time that sprains of the foot can result in fractures of the base of MT5 (2). The majority of these have been shown to heal quickly and uneventfully with time under conservative treatment, while others have developed painful non-unions. So, differentiation according to the different types of fracture at the base of MT5 would appear to be crucial for any treatment recommendation. The most commonly used classification at present was described by Lawrence und Botte (3) in 1993 and distinguishes three fracture types:
Zone 1: proximal to the 4th-5th intermetatarsal articulation (“avulsion fracture”)
Zone 2: at the level of the articulation (“Jones fracture”)
Zone 3: at the distal end of the articulation (“diaphyseal stress fracture”) (Figure 2a).
Figure 2.
Inconsistent use of the term “Jones-fracture” in the various classifications (Figure 2a) and a new proposal for a treatment-based classification (Figure 2b)
Unfortunately, the literature does not use uniform terminology here, with the result that the various studies report different treatment outcomes supposedly for the same fracture. Consequently, there have been no consistent treatment recommendations to date (4). Moreover, the majority of those that do exist are not evidence-based. Recommended treatment has therefore been a matter of debate ever since the times of Sir Robert.
The aim of the present review article was to develop evidence-based treatment recommendations for fractures of the base of MT5, based on a systematic search of the literature.
Methods
The systematic literature search was conducted according to the PRISMA statement (5) and PICOS model (etable 1) (6) in MEDLINE (PubMed), CINAHL, Scopus, EMBASE, CENTRAL from database inceptions until 05. 07. 2020. The study protocol was prospectively registered in PROSPERO (CRD42020185294). The systematic literature search was conducted by two independent examiners (VH, HP) using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). The included articles were analyzed according to Lawrence and Botte’s (3) classification of fracture location (Figure 2a). The Methodological Index for Non-randomized Studies (MINORS) was used to evaluate the methodological quality of the study (7). Evaluation of the level of evidence was conducted according to the criteria described by Wright et al. (8). A detailed description of the methodology can be found in the eMethods section.
eTable 1. PICOS criteria.
| Participants | female and male patients ≥ 18 years with acute fractures of the base of the fifth metatarsal bone |
| Intervention | any surgical or conservative form of management |
| Comparison | at least two fracture types treated in the same way or one fracture type treated in different ways |
| Results | functional/subjective outcome, consolidation rate or time, regaining sports/work ability, re-fractures |
| Study design | no restrictions |
Results
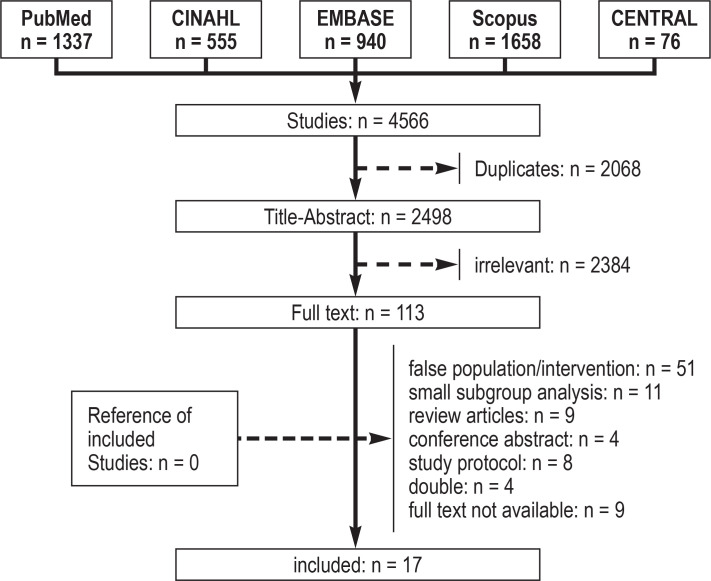
The study selection according to the PRISMA guidelines is presented in Figure 3. The search strategy identified 2498 articles. After excluding all irrelevant hits, 17 of the 113 full texts examined met the inclusion criteria (eTable 2, Figure 3). Using the MINORS criteria, an average of 82% of the maximum score was achieved for study quality. A meta-analysis was not possible due to the large variance of the follow-up periods (12.4 ± 12.9 months; 2–53 months) and the different target parameters.
eTable 2. Overview of the included review articles.
| Author – Year | Study design (level of evidence*1) | Fracture type*2 (n) | Intervention | Quality level (MINORS*3) |
| Akimau 2016 (9) | RCT (I) | I (60) | early functional | 22/24 |
| immobilization | ||||
| Baumbach 2017 (18) | prospective registry-based study (II) | I (23) | early functional | 12/16 |
| II (16) | ||||
| Bayram 2020 (10) | RCT (I) | I (65) | early functional | 22/24 |
| immobilization | ||||
| Brocchini 1992 (21) | prospective interventional study (II) | I (12) | early functional | 12/16 |
| II (24) | ||||
| Choi 2013 (22) | prospective interventional study (II) | I (6) | plate fixation | 12/16 |
| II (11) | ||||
| Gray 2008 (11) | prospective interventional study (II) | I (37) | early functional | 18/24 |
| immobilization | ||||
| Kim 2017 (16) | prospective case-control study (III) | I (30) | screw fixation | 18/24 |
| plate fixation | ||||
| Lee 2016 (15) | RCT (I) | I (18) | immobilization | 19/24 |
| ORIF | ||||
| Mahajan 2011 (23) | prospective interventional study (II) | I (6) | screw fixation | 12/16 |
| II (17) | ||||
| Mologne 2005 (24) | RCT (I) | III (37) | immobilization | 22/24 |
| screw fixation | ||||
| Nishikawa 2020 (12) | prospective case-control study (III) | I (72) | early functional | 18/24 |
| immobilization | ||||
| de Oliveira Massada 2011 (25) | case series (III) | II (8) | screw fixation | 12/16 |
| III (9) | ||||
| Piyapittayanun 2019 (19) | RCT (I) | II (72) | early functional | 21/24 |
| immobilization | ||||
| Van Aaken 2007 (20) | prospective cohort study (II) | I (15) | early functional | 12/16 |
| II (8) | ||||
| Wiener 1997 (13) | prospective interventional study (II) | I (60) | early functional | 17/24 |
| immobilization | ||||
| Wu 2018 (14) | RCT (I) | I (41) | immobilization | 20/24 |
| screw fixation | ||||
| Xie 2017 (17) | prospective cohort study (II) | I (43) | screw fixation | 18/24 |
| plate fixation |
Figure 3.
Flowchart of study selection using the PRISMA specifications (5)
Zone 1 fractures
Nine studies compared different forms of treatment for zone 1 fractures (9– 17), and five (9– 13) compared early functional conservative management with immobilization (table 1). Two of these were prospective randomized controlled studies (RCT) (9, 10). Akimau et al. found no statistically significant differences in their results for the “Visual Analogue Scale Foot and Ankle” and the EQ-5D (Health-related Quality of Life) (9). Bayram et al. observed a statistically significant faster return to work, as well as statistically significant higher VAS-FA scores with functional therapy (10). The other three studies were prospective, but not randomized (11– 13). Wiener et al. observed a statistically significant faster return to pre-injury levels with early functional management (13), Nishikawa et al. a statistically significant shorter average time for bone healing with immobilization (12). Otherwise, there were no statistically significant differences with regard to consolidation rate or functional outcome.
Table 1. Overview of comparative studies with different treatment regimens for zone 1 fractures (according to L & B).
| Author – Year(Reference) | Fracture type (n) according to L % B (3) | Treatment (n) | Follow-up period | Fit for work/full function after | Consolidation % (time) | Objective treatment result*1 |
| Comparison zone 1 – conservative | ||||||
| Akimau 2016 (9) |
I (60) | early functional*2 (36) | 6 months | n.s./n.s. | n.s. | VAS-FA: 93 EQ-5D VAS: 95 |
| Immobilisation*3 (24) | VAS-FA: 93 EQ-5D VAS: 94 |
|||||
| Bayram 2020 (10) |
I (65) | early functional (33) | 24 weeks | 11 ± 6 T*4/n.s. | 97 % | VAS-FA: 95 EQ-5D VAS: 96 |
| immobilization (32) | 28 ± 11 T*4/n.s. | 97 % | VAS-FA: 93 EQ-5D VAS: 94 |
|||
| Gray 2008 (11) |
I (37) | early functional (17) | 12 weeks | n.s./n.s. | 88 % | MFSS: 90 |
| immobilization (20) | 90 % | MFSS: 90 | ||||
| Nishikawa 2020 (12) |
I (72) | early functional (33) | 24 weeks | n.s./10 weeks | 100 % (9 wks; 95% CI: [7.9; 9.4]*4 |
AOFAS: 12 wks 99 VAS: 12 wks 0.2 |
| immobilization (39) | n.s./8 weeks | 97 % (7 wks [6.5; 7.9]*4 |
AOFAS: 12 wks 98 VAS: 12 wks 0.2 |
|||
| Wiener 1997 (13) |
I (60) | early functional (30) | 12 weeks | n.s./33 T*4 | 100 % (43 T) | Mod FS: 86 |
| immobilization (30) | n.s./46 T*4 | 100 % (45 T) | Mod FS: 92 | |||
| Comparison zone 1 – conservative versus surgical | ||||||
| Wu 2018 (14) |
I (41) | immobilization (non-weight bearing) (20) | 14 months | 9 ± 1 wks*4/n.s. | 85 % | AOFAS: 87 VAS-FA: 1.1 ± 1*4 |
| CRIF/screw (21) | 8 ± 1 wks*4/n.s. | 100 % | AOFAS: 88 VAS-FA: 0.4 ± 0.5*4 |
|||
| Lee 2016 (15) |
I (18) | immobilization (non-weight bearing) (9) | 9 weeks | n.s./n.s. | 100 % (9 ± 2 wks)*4 | AOFAS: 88 VAS: 0.6 |
| ORIF (9) | 100 % (7 ± 1 wks)*4 | AOFAS: 89 VAS: 0.9 |
||||
| Comparison zone 1 – surgical | ||||||
| Kim 2017 (16) |
I (30) | CRIF/screw (15) | 13 months | n.s./n.s. | 100 % (54 ± 9 T)*4 |
AOFAS: 98 |
| ORIF/plate (15) | 100 % (42 ± 7 T)*4 |
AOFAS: 98 | ||||
| Xie 2017 (17) |
I (43) | CRIF/screw (18) | 12 months | n.s./13 weeks | 100 % (10 ± 0.6 wks)*4 | AOFAS: 88 ± 0.2*4 |
| ORIF/plate (25) | n.s./12 weeks | 100 % (8 ± 0.1 wks)*4 | AOFAS: 94 ± 0.3*4 | |||
*1 objective treatment outcome at the end of the follow-up period with the exception of Nishikawa (12 weeks); all studies allow immediate full weight-bearing with the exception of Wu (14), Lee (15).
*2 early functional treatment involves: elasticated bandaging/dressing, soft orthosis, hard-soled shoe, and full weight-bearing as tolerated.
*3 immobilization involves: below knee cast (walker boot).
*4 statistically significant difference (p <0.05)
AOFAS, American Orthopedic Foot and Ankle Score; CRIF, closed reduction and internal fixation; EQ-5D, health-related quality of life questionnaire; n.s. not specified; L & B, Lawrence and Botte; MFSS, Mid-Foot Scoring System; Mod FS, Modified Foot Score; ORIF, open reduction and internal fixation; d, days; VAS, visual analogue scale; VAS-FA, visual analogue scale foot and ankle; wks, weeks; 95% CI, 95% confidence interval
Two RCTs compared surgical treatment with restrictive conservative management (immobilization and non-weight bearing) (14, 15). Wu et al. (14) observed statistically significant shorter work incapacity and Lee et al. (15) a statistically significant shorter time for bone healing with surgery. Both studies demonstrated very good results with no clinically relevant differences between the treatment groups with regard to patient-reported treatment outcomes (VAS, VAS-FA, AOFAS [American Orthopedic Foot and Ankle Society Score]).
Two studies compared different surgical procedures (16, 17). Both articles reported a faster rate of bony consolidation after open reduction.
Three studies (10, 15, 18) assessed the impact of different fracture patterns (displacement [> 2 mm], intra-articular involvement [>30% of the cuboid articular surface], number of fragments) on treatment outcome. None of the fracture characteristics had an effect on the working/sports ability or the functional result with early functional management.
Zone 2 fractures
Piyapittayanun et al. undertook a prospective randomized comparison between early functional conservative management and immobilization for zone 2 fractures (19). There were no statistically significant differences in the functional outcomes after eight weeks (table 2).
Table 2. Overview of comparative studies with different treatment regimens for zone 2 fractures (according to L & B) or the same treatment for zone 1 and zone 2 fractures.
|
Author – Year (Reference) |
Fracture type (n) according to L % B (3) | Treatment (n) | Follow-up period | Fit for wksrk/full function after | Consolidation % (time) | Objective treatment result*1 |
| Comparison zone 2 – conservative | ||||||
| Piyapittayanun 2019 (19) | II (72) | early functional *2 (36) | 8 weeks | n.s./n.s. | n.s. | VAS: 0.1 AOFAS: 98 |
| Immobilisation*3 (36) | VAS: 0.1 AOFAS: 99 | |||||
| Comparison zone 1 versus zone 2 – conservative | ||||||
| Baumbach 2017 (18) | I (23) | early functional | 22 months | 15 d/47 d | n.s. | VAS-FA: 97 SF-12: PCS 58; MCS 51 |
| II (16) | 20 d/63 d | VAS-FA: 95 SF-12: PCS 55; MCS 51 | ||||
| Van Aaken 2007 (20) | I (15) | early functional | 12 weeks | 21 d/n.s. | 100 % (7 wks) | Mod FS: no significant difference (all good to excellent) |
| II (8) | 4 d/n.s. | 100 % (7 wks) | ||||
| Brocchini 1992 (21) | I (12) | early functional | 6 months | n.s./n.s. | 100 % | n.s. |
| II (14) | 93 % | |||||
| Comparison zone 1 versus zone 2 – surgical | ||||||
| Choi 2013 (22) | I (6) | ORIF/plate | 12 months | n.s./73 d | 100 % (50 d) | AOFAS: 93 |
| II (11) | n.s./75 d | 100 % (57 d) | AOFAS: 90 | |||
| Mahajan 2011 (23) | I (6) | CRIF/screw | 23 months | n.s./n.s. | 100 % (5 wks) | AOFAS 6 months: 94 |
| II (17) | 100 % (7 wks) | AOFAS 6 months: 94 | ||||
*1 objective treatment outcome, unless stated otherwise, at the end of the follow-up period
*2 early functional treatment involves: elasticated bandaging/dressing, soft orthosis, hard-soled shoe, and full weight-bearing as tolerated.
*3 immobilization involves: below knee cast (Walker Boot).
AOFAS, American Orthopedic Foot and Ankle Score; CRIF, open reduction and internal fixation; n.s., not specified; L & B, Lawrence and Botte; MCS, Mental Component Score; Mod FS, Modified Foot Score; ORIF, open reduction and internal fixation; PCS, Physical Component Score; SF-12, Short-Form Health Survey; d, days; VAS-FA, Visual Analogue Scale Foot and Ankle; wks, weeks
Five studies compared zone 1 with zone 2 fractures treated in the same manner (18, 20– 23) (table 2). Three involved early functional conservative management (18, 20, 21). The articles reported no statistically significant differences between the two fracture types which had very good functional results. Choi et al. and Mahajan et al. compared fractures in zones 1 and 2 after surgical management and also discovered no statistically significant differences (22, 23). In the study by Choi et al., hardware irritation developed which resulted in plate removal (22); in one case, Mahajan et al. had to exchange screw fixation for tension band wiring (23).
Zone 3 fractures
Two articles examined fractures in zone 3 (24, 25). Mologne et al. (24) conducted a prospective randomized comparison between conservative and surgical treatment (table 3). Surgical treatment produced significantly better results for all of the study parameters. Oliveira Massada et al. compared fractures in zones 2 and 3 after screw fixation and discovered no statistically significant differences (25).
Table 3. Overview of comparative studies with different treatment regimens for zone 2 fractures (according to L & B) or the same treatment for zone 1 and zone 2 fractures.
|
Author – Year
(Reference) |
Fracture type (n) according to L % B (3) | Treatment (n) | Follow-up period | Fit for work/full function after | Consolidation % (time) | Objective treatment result*1 |
| Mologne 2005 (24) | III (37) | immobilization *1 (18) | 25 months | n.s./16 ± 4 wks*2 | 72 % (15 ± 5 wks)*2 | n.s. |
| CRIF/screw (19) | n.s./8 ± 2 wks*2 | 95 % (8 ± 2 wks)*2 | ||||
| de Oliveira Massada 2011 (25) | II (8) | CRIF/screw (19) | 54 moths | 8 wks/7 wks | 100 % (7 wks) | for both: AOFAS: pain 38: function 45; TAS: 9 |
| III (11) |
*1 immobilization involves: below knee cast (walker boot) and full weight-bearing as tolerated (exception Mologne: 8 weeks non-weight bearing).
*2 statistically significant difference (p <0.05)
AOFAS, American Orthopedic Foot and Ankle Society Score; CRIF, closed reduction and internal fixation; n.s., not specified; L & B, Lawrence and Botte; TAS, Tegner Activity Scale; wks, weeks
Discussion
Overall, there was a limited number of studies available for comparison, and their quality was at times restricted. Nevertheless, after due differentiated consideration, treatment recommendations for the different fracture types involving the base of MT5 can be derived.
Zone 1 fractures
Most authors recommend conservative treatment for extra-articular, non-displaced fractures in zone 1 (9, 26). The recommendations vary from early functional management to immobilization or non-weight bearing (27, 28). Analysis of the studies showed that early functional treatment was superior to immobilization or surgery with regard to time until return to work/restoration of full function (10, 12– 14, 17). Consolidation and re-fracture rates, return to full function, and results for pain (VAS-FA, VAS), quality of life (EQ-5D) and foot function (AOFAS, ModFS [“modified foot score”]) were comparable for all treatment modalities. Immobilization or surgery was superior to functional conservative management only for time until radiological consolidation. The time until radiological consolidation is irrelevant to the patient, however. There was no indication for change of treatment, even for a case of asymptomatic non-union. For this reason, some authors recommend dispensing with scheduled follow-up radiographs altogether (27). Accordingly, the authors only obtain a follow-up radiograph for pain persisting longer than six weeks.
The effect of fracture characteristics is currently the subject of intensive discussions in the literature. Many authors recommend surgery for displacement (>2 mm), intra-articular involvement (30%) or multifragmental fractures, but without scientific studies to back this up. These are therefore expert opinions and not study-based recommendations (29). Three studies looked explicitly at the impact of these fracture characteristics (10, 15, 18). In none of them was there an effect on treatment outcome. One reason for recommending surgery is concern for post-traumatic osteoarthritis. The follow-up period of most of the studies was too short, however, to be able to exclude this. The authors conducted follow-up reviews after 5.7 years for their own patient population. These results had remained excellent when compared with those after two years (18), irrespective of the fracture characteristics (30). It would also have been expected that the authors would be regularly confronted with cases of post-traumatic osteoarthritis. However, these do not appear to play a role in everyday clinical practice (31).
Conclusion: Based on the available studies, early functional therapy is recommended for zone 1 fractures. This also applies to displaced, intra-articular and comminuted fractures.
Zone 2 fractures
There are conflicting recommendations for the management of zone 2 fractures. Some authors report very good results for early functional conservative management (18– 20), while others report better outcomes after surgery (22, 23, 25). One likely reason for this is the use of the eponym “Jones fracture” for both zone 2 and zone 3 fractures. Although only one study compared immobilization with early functional treatment for zone 2 fractures (19), it did show very good results for early functional treatment. Unfortunately, there are no studies currently available comparing surgical and conservative management of zone 2 fractures. On looking at the results of those studies applying conservative treatment for zone 1 and zone 2 fractures, return to full function after 47–63 days is evident, compared with 73 and 75 days, respectively, after surgery. The AOFAS after functional treatment was 89–99 points and 90–94 points after surgery. In this respect, functional therapy appears to result in a faster return to full function and to comparable/better functional outcomes (AOFAS). Comparative studies are required for any conclusive assessment.
Conclusion: Early functional treatment produces very good functional results for zone 2 fractures. When compared with studies which undertook surgical management, functional therapy appears to result in a faster return to full function and to at least equivalent functional outcomes.
Zone 3 fractures
Many authors recommend surgery primarily for patients with a high functional demand and conservative management for patients with a low demand (3, 32). However, in an RCT, Mologne et al. demonstrated better statistically significant results for all study parameters after screw fixation in comparison with conservative treatment. The differences were very impressive, with 44% treatment failures after conservative management as compared with 5% after surgery, which involved an eight-week shorter time until full weight-bearing (24). The long period of immobilization of eight weeks in the conservatively treated group should be noted. However, the majority of authors recommend immobilization during conservative management of these fracture types for at least six, and up to 20, weeks (3, 33). Given the high rate of treatment failures and the significantly prolonged immobilization/non-weight bearing time during conservative treatment, the present authors do not consider it justified to reserve surgery only for patients with high functional demands—it should be recommended to all patients.
Conclusion: Surgical management of zone 3 fractures with screw fixation appears to be significantly superior to conservative treatment; primary surgical management should therefore be recommended to all affected patients.
Recent review articles
Some systematic reviews on the subject are already available. In the following, the three most recent reviews from the year 2020 (34– 36) are considered by way of example. Wang et al. (34) did not distinguish between fracture types, but instead pooled all fractures of the base of MT5 together – which would not appear to make sense, according to current knowledge. Rikken et al. (35) analyzed the different Lawrence und Botte fracture types, while Khan et al. (36) focused on “tuberosity fractures” and excluded “true Jones fractures”— yet without actually defining the terms, so that it remains unclear which fractures were ultimately examined. In none of the three studies was any distinction made between the various forms of conservative management, but instead all modalities were grouped together. None of the articles were confined to comparative studies, but also included case series. Nevertheless, all treatment outcomes were pooled and assessed together, regardless of when the data was collected. Furthermore, no study analyzed the fracture characteristics. The weaknesses of current systematic reviews underline the value of a differentiated analysis of existing studies.
Terminology
There is a lack of uniform terminology applied in daily clinical practice for fractures of the base of MT5. This observation was also confirmed during the analysis of the included studies. In six of the 17 included studies there was no clear differentiation based on a classification system (11, 13, 14, 19, 21, 25). Different expressions were used in the various studies for zone 1 fractures (“avulsion fracture”, “tuberosity fracture”, “tuberosity avulsion fracture”). The term “Jones fracture” appeared in different variations (“Jones fracture”, “true Jones fracture”, “pseudo-Jones avulsion fracture”) in nine articles (11, 13, 17– 20, 23– 25). The term “Jones” was used for zone 2 fractures in seven of the nine studies (13, 17– 20, 23, 25) and for zone 3 fractures in two studies (11, 24).
This vagueness is a fundamental problem, as it means that the terms used do not clearly specify the fracture types. The result is that various studies report different treatment results for the supposedly same type of fracture; however, the fracture types were in fact different. Accordingly, in the authors‘ view, the term „Jones fracture“ should be avoided altogether. More than this, however, a clear designation according to anatomical criteria would appear more appropriate. Since there does not appear to be any differences between zone 1 and zone 2 fractures, regardless of treatment, they should all be described as epi-metaphyseal fractures. They should be distinguished from meta-diaphyseal fractures at the distal end of the MT 4–5 articulation (Figure 2b).
Limitations
The main limitation of this systematic review was the small number of available studies for the individual fracture types and the limited number of cases. Yet, it is precisely the differentiated, zone-specific analysis of the available studies that is essential for providing any valid treatment recommendation. Furthermore, the quality of the included studies was at times limited, as evidenced by the results for the MINORS score. The risk of bias due to the restricted study quality must be borne in mind when interpreting the results; nevertheless, more than one third of the included studies were indeed prospectively randomized. Although the number of available studies is limited, a differentiated view still shows a clear trend that does allow recommendations. Future studies on zone 1 and 2 fractures, irrespective of the group under investigation, should include early functional treatment as a control group since they have so far produced the best outcomes. Unfortunately, this was not the case in all of the included studies.
Conclusion
There is only a limited number of comparative studies dealing with the management of fractures of the base of MT5. Nevertheless, a differentiated analysis of the existing articles does allow treatment recommendations to be made. Fractures in zones 1 and 2 show very good results with early functional therapy. Displacement and joint involvement have no impact on treatment outcome. All these fractures may therefore be subjected to early functionally treatment. When the results of the only available RCT are analyzed, then surgical treatment is clearly superior to conservative management for fractures in zone 3. Surgical management of these fractures would therefore appear appropriate. Since there does not seem to be any difference between zone 1 and zone 2 fractures, they should all be grouped together as epi-metaphyseal fractures. At the same time, the present authors recommend the term meta-diaphyseal fractures for zone 3. The term „Jones fracture“ should be dispensed with altogether. Nevertheless, it should be noted that the results and treatment recommendations presented here are only based on a few studies and need to be verified in larger studies in the future.
Supplementary Material
eMETHODS
Search strategy and study selection
The systematic literature search was conducted according to the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-analyses) (12) in the databases MEDLINE (PubMed), CINAHL, Scopus, EMBASE, CENTRAL from database inceptions until 5. July 2020. In addition, a search for „grey literature“ in the form of conference papers was carried out in both Scopus and EMBASE, as well as a hand search in the references of included studies and reviews on the topic. The complete search strategies for all databases are shown below.
PubMed
(“fifth metatarsal*”[Title/Abstract] OR “5th metatarsal*”[Title/Abstract] OR “MT V”[Title/Abstract] OR “Jones”[Title/Abstract] OR “Lawrence”[Title/Abstract] OR “Metatarsal Bones/injuries” [Mesh Terms]) AND (“fracture*”[Title/Abstract] OR “Fractures, Bone”[Mesh Terms])
CINAHL
(TI “fifth metatarsal*” OR AB “fifth metatarsal*” OR TI “5th metatarsal*” OR AB “5th metatarsal*” OR TI “MT V” OR AB “MT V” OR TI “Jones” OR AB “Jones” OR TI “Lawrence” OR AB “Lawrence” OR (MH “Metatarsal Fractures”))
AND (TI “fracture*” OR AB “fracture*” OR (MH “Fractures”))
EMBASE
(‘fifth metatarsal*’:ti,ab OR ‘5th metatarsal*’:ti,ab OR ‘MT V‘:ti,ab OR ‘jones’:ti,ab OR ‘Lawrence’:ti,ab) AND (‘fracture*’:ti,ab OR exp Fracture)
Scopus
TITLE-ABS-KEY (“fifth metatarsal*” OR “5th metatarsal*” OR “MT V” OR “Jones” OR “Lawrence”) AND TITLE-ABS-KEY (“fracture*”)
CENTRAL
(“fifth metatarsal*”:ti,ab,kw OR “5th metatarsal*”:ti,ab,kw OR “MT V”:ti,ab,kw OR “Jones”: ti,ab,kw OR “Lawrence”: ti,ab,kw OR MeSH descriptor: [Metatarsal Bones]) AND “fracture*”:ti,ab,kw OR MeSH descriptor: [Fractures, Bone])
The classification used had no effect on the study selection. The Lawrence and Botte (3) classification was used for the analysis. Where a study used a different term, it was „translated“ into the Lawrence and Botte classification. Also analyzed were randomized cohort studies (RCT) or comparative cohort studies which either examined the same treatment for different fracture types (according to Lawrence and Botte) or different forms of treatment for the same fracture type of the base of MT5. Exclusion criterion was the presence of other injuries, apart from a fracture of the base of MT5 on the contralateral side. The inclusion criteria in terms of the PICOS framework (13) are presented in etable 1. The study protocol was prospectively registered in PROSPERO (CRD 42020185294, 5 July 2020).
The management and implementation of the systematic literature search was conducted using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia www.covidence.org). The relevant articles were identified in a stepwise fashion, first of all based on titles and abstracts, then on the full texts, in each case by two independent investigators (VH, HP). Any disagreements were finally decided by an independent third examiner (SB). The assessment of the study quality and data extraction were also conducted by the two independent examiners (VH, HP) using Microsoft Excel (Version 16.46, Microsoft Corporation, Redmond, Washington, USA). The study parameters are presented in etable 2.
Analysis of the papers included was made based on the fracture location classification according to Lawrence and Botte (3). This classification distinguishes between three fracture types, depending on the fracture pattern in relation to the base of the 4th–5th intermetatarsal articulation: Zone 1 – proximal to the intermetatarsal articulation, Zone 2 – in the region of the articulation, Zone 3 – at the distal end of the articulation (Figure 2a). The term “early functional conservative therapy” involves immediate full weight-bearing as tolerated without immobilization.
Rating of the quality of the studies
Evaluation of the studies was performed using the “Methodological index for non-randomized studies” score (MINORS score) (7). Although the MINORS tool was developed for non-randomized studies, it is also capable of rating the quality of randomized studies and has been validated for this purpose. All studies were evaluated using the MINORS tool to ensure a uniform presentation and comparability of the quality of the studies. A comparative study can thus achieve a maximum of 24, a non-comparative study a maximum of 16 points. Evaluation of the level of evidence was conducted according to the criteria described by Wright et al. (8).
eFigure.
Flowchart showing patient selection process from the clinical and radiological databases for the acquisition of the frequency of metatarsal fractures
Data collection was approved by the Ethics Committee of the LMU Hospital – Munich
(# 20–442).
MT, metatarsal; n, number
Acknowledgments
Translated from the original German by Dr. Grahame Larkin, MD
Footnotes
Conflict of interest statement
The authors declare that no conflicts of interest exists.
References
- 1.Petrisor BA, Ekrol I, Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int. 2006;27:172–174. doi: 10.1177/107110070602700303. [DOI] [PubMed] [Google Scholar]
- 2.Jones R. I. Fracture of the base of the fifth metatarsal bone by indirect violence. Ann Surg. 1902;35 [PMC free article] [PubMed] [Google Scholar]
- 3.Lawrence SJ, Botte MJ. Jones‘ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle Int. 1993;14:358–365. doi: 10.1177/107110079301400610. [DOI] [PubMed] [Google Scholar]
- 4.Baumbach S, Prall W, Braunstein M, Böcker W, Polzer S, Polzer H. Frakturen der Metatarsale Fünf Basis-eine Neubetrachtung. Unfallchirurg. 2018;121:723–729. doi: 10.1007/s00113-018-0507-6. [DOI] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman D. Bevorzugte Report Items für systematische Übersichten und Meta-Analysen: Das PRISMA-Statement. DMW-Deutsche Medizinische Wochenschrift. 2011;136:e9–e15. [Google Scholar]
- 6.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006 DOI:10.13140/2.1.1018.4643. [Google Scholar]
- 7.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for nonrandomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 8.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85:1–3. [PubMed] [Google Scholar]
- 9.Akimau P, Cawthron K, Dakin W, Chadwick C, Blundell C, Davies M. Symptomatic treatment or cast immobilisation for avulsion fractures of the base of the fifth metatarsal: a prospective, randomised, single-blinded non-inferiority controlled trial. Bone Joint J. 2016;98:806–811. doi: 10.1302/0301-620X.98B6.36329. [DOI] [PubMed] [Google Scholar]
- 10.Bayram S, Kendirci AŞ, Kiral D, et al. Isokinetic strength comparison of tuberosity fractures of the proximal fifth metatarsal treated with elastic bandage vs cast. Foot Ankle Int. 2020:;41:674–682. doi: 10.1177/1071100720916429. [DOI] [PubMed] [Google Scholar]
- 11.Gray AC, Rooney BP, Ingram R. A prospective comparison of two treatment options for tuberosity fractures of the proximal fifth metatarsal. Foot (Edinb) 2008;18:156–158. doi: 10.1016/j.foot.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Nishikawa DRC, Aires Duarte F, Saito GH, et al. Treatment of zone 1 fractures of the proximal fifth metatarsal with CAM-walker boot vs hard-soled shoes. Foot Ankle Int. 2020;41:508–512. doi: 10.1177/1071100720903259. [DOI] [PubMed] [Google Scholar]
- 13.Wiener BD, Linder JF, Giattini JF. Treatment of fractures of the fifth metatarsal: a prospective study. Foot Ankle Int. 1997;18:267–269. doi: 10.1177/107110079701800504. [DOI] [PubMed] [Google Scholar]
- 14.Wu GB, Li B, Yang YF. Comparative study of surgical and conservative treatments for fifth metatarsal base avulsion fractures (type I) in young adults or athletes. J Orthop Surg (Hong Kong) 2018;26 doi: 10.1177/2309499017747128. 2309499017747128. [DOI] [PubMed] [Google Scholar]
- 15.Lee TH, Lee JH, Chay SW, Jang KS, Kim HJ. Comparison of clinical and radiologic outcomes between non-operative and operative treatment in 5th metatarsal base fractures (Zone 1) Injury. 2016;47:1789–1793. doi: 10.1016/j.injury.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 16.Kim JB, Song IS, Park BS, Ahn CH, Kim CU. Comparison of the outcomes between headless cannulated screw fixation and fixation using a locking compression distal ulna hook plate in fracture of fifth metatarsal base. J Foot Ankle Surg. 2017;56:713–717. doi: 10.1053/j.jfas.2017.01.048. [DOI] [PubMed] [Google Scholar]
- 17.Xie L, Guo X, Zhang SJ, Fang ZH. Locking compression plate distal ulna hook plate fixation versus intramedullary screw fixation for displaced avulsion fifth metatarsal base fractures: a comparative retrospective cohort study. BMC Musculoskelet Disord. 2017;18 doi: 10.1186/s12891-017-1766-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baumbach SF, Prall WC, Kramer M, Braunstein M, Böcker W, Polzer H. Functional treatment for fractures to the base of the 5th metatarsal-influence of fracture location and fracture characteristics. BMC Musculoskelet Disord. 2017;18:1–7. doi: 10.1186/s12891-017-1893-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piyapittayanun P, Mutthakalin K, Arirachakaran A, Kongtharvonskul J. Comparative outcomes of foot cast and short leg cast in pseudo-Jones avulsion fracture: a single blinded randomized controlled trial. J Foot Ankle Res. 2019;12 doi: 10.1186/s13047-019-0359-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Aaken J, Berli M, Noger M, Gambirasio R, Fritschy D. Symptomatic treatment of non-displaced avulsion and Jones fractures of the fifth metatarsal: a prospective study. Rev Med Suisse. 2007;3:1792–1794. [PubMed] [Google Scholar]
- 21.Brocchini ETG, Zugnoni M, Artuso D. Le fratture della base del V metatarso. Minerva Ortop Traumatol. 1992;43:621–626. [Google Scholar]
- 22.Choi JH, Lee KT, Lee YK, Lee JY, Kim HR. Surgical results of zones I and II fifth metatarsal base fractures using hook plates. Orthopedics. 2013;36:e71–e74. doi: 10.3928/01477447-20121217-21. [DOI] [PubMed] [Google Scholar]
- 23.Mahajan V, Chung HW, Suh JS. Fractures of the proximal fifth metatarsal: percutaneous bicortical fixation. Clin Orthop Surg. 2011;3:140–146. doi: 10.4055/cios.2011.3.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mologne TS, Lundeen JM, Clapper MF, O’Brien TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 33:970–975. doi: 10.1177/0363546504272262. [DOI] [PubMed] [Google Scholar]
- 25.de Oliveira Massada MMT, Pereira MANPG, de Sousa RJG, Costa PG, da Rocha Massada JL. Intramedullary screw fixation of proximal fifth metatarsal fractures in athletes. Acta Ortop Bras. 2012;20 doi: 10.1590/S1413-78522012000500003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schmoz S, Voelcker A, Burchhardt H, et al. Konservatives Therapiekonzept bei Metatarsale-V-Basisfrakturen-Retrospektive und prospektive Analyse. Sportverletz Sportschaden. 2014;28:211–217. doi: 10.1055/s-0034-1385611. [DOI] [PubMed] [Google Scholar]
- 27.Nagar M, Forrest N, Maceachern CF. Utility of follow-up radiographs in conservatively managed acute fifth metatarsal fractures. Foot (Edinb) 2014;24:17–20. doi: 10.1016/j.foot.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 28.Polzer H, Polzer S, Mutschler W, Prall WC. Acute fractures to the proximal fifth metatarsal bone: development of classification and treatment recommendations based on the current evidence. Injury. 2012;43:1626–1632. doi: 10.1016/j.injury.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 29.Rettig AC, Shelbourne KD, Wilckens J. The surgical treatment of symptomatic nonunions of the proximal (metaphyseal) fifth metatarsal in athletes. Am J Sports Med. 1992;20:50–54. doi: 10.1177/036354659202000113. [DOI] [PubMed] [Google Scholar]
- 30.Baumbach SF, Urresti-Gundlach M, Böcker W, Vosseller JT, Polzer H. Results of functional treatment of epi-metaphyseal fractures of the base of the fifth metatarsal. Foot Ankle Int. 2020:;41:666–673. doi: 10.1177/1071100720907391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roddy E, Menz HB. Foot osteoarthritis: latest evidence and developmentsT. her Adv Musculoskelet Dis. 2018;10:91–103. doi: 10.1177/1759720X17753337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruta DJ, Parker D. Jones Fracture Management in Athletes. Orthop Clin North Am. 2020;51:541–553. doi: 10.1016/j.ocl.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 33.Zwitser E, Breederveld R. Fractures of the fifth metatarsal; diagnosis and treatment. Injury. 2010;41:555–562. doi: 10.1016/j.injury.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Gan X, Li K, Ma T, Zhang Y. Comparison of operative and non-operative management of fifth metatarsal base fracture: a meta-analysis. PLOS One. 2020;15 doi: 10.1371/journal.pone.0237151. e0237151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rikken Q, Dahmen J, Hagemeijer N, Sierevelt I, Kerkhoffs G, ¬DiGiovanni C. Adequate union rates for the treatment of acute proximal fifth metatarsal fractures. Knee Surg Sports Traumatol ¬Arthrosc. 2021;291:284–293. doi: 10.1007/s00167-020-06072-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khan S, Axelrod D, Paul R, et al. Acute fifth metatarsal tuberosity fractures: a systematic review of nonoperative treatment. PM R. 2021;13:405–411. doi: 10.1002/pmrj.12427. [DOI] [PubMed] [Google Scholar]
- 37.Quill Jr GE. Fractures of the proximal fifth metatarsal. Orthop Clin North Am. 1995;26:353–361. [PubMed] [Google Scholar]
- 38.Dameron Jr TB. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. JBJS. 1975;57:788–792. [PubMed] [Google Scholar]
- 39.Stewart I. Jones‘s fracture: fracture of base of fifth metatarsal. Clin ¬Orthop. 1960;16:190–198. [PubMed] [Google Scholar]
- 40.Ding BC, Weatherall JM, Mroczek KJ, Sheskier SC. Fractures of the proximal fifth metatarsal: keeping up with the Joneses. Bull NYU Hosp Jt Dis. 2012;70:49–55. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMETHODS
Search strategy and study selection
The systematic literature search was conducted according to the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-analyses) (12) in the databases MEDLINE (PubMed), CINAHL, Scopus, EMBASE, CENTRAL from database inceptions until 5. July 2020. In addition, a search for „grey literature“ in the form of conference papers was carried out in both Scopus and EMBASE, as well as a hand search in the references of included studies and reviews on the topic. The complete search strategies for all databases are shown below.
PubMed
(“fifth metatarsal*”[Title/Abstract] OR “5th metatarsal*”[Title/Abstract] OR “MT V”[Title/Abstract] OR “Jones”[Title/Abstract] OR “Lawrence”[Title/Abstract] OR “Metatarsal Bones/injuries” [Mesh Terms]) AND (“fracture*”[Title/Abstract] OR “Fractures, Bone”[Mesh Terms])
CINAHL
(TI “fifth metatarsal*” OR AB “fifth metatarsal*” OR TI “5th metatarsal*” OR AB “5th metatarsal*” OR TI “MT V” OR AB “MT V” OR TI “Jones” OR AB “Jones” OR TI “Lawrence” OR AB “Lawrence” OR (MH “Metatarsal Fractures”))
AND (TI “fracture*” OR AB “fracture*” OR (MH “Fractures”))
EMBASE
(‘fifth metatarsal*’:ti,ab OR ‘5th metatarsal*’:ti,ab OR ‘MT V‘:ti,ab OR ‘jones’:ti,ab OR ‘Lawrence’:ti,ab) AND (‘fracture*’:ti,ab OR exp Fracture)
Scopus
TITLE-ABS-KEY (“fifth metatarsal*” OR “5th metatarsal*” OR “MT V” OR “Jones” OR “Lawrence”) AND TITLE-ABS-KEY (“fracture*”)
CENTRAL
(“fifth metatarsal*”:ti,ab,kw OR “5th metatarsal*”:ti,ab,kw OR “MT V”:ti,ab,kw OR “Jones”: ti,ab,kw OR “Lawrence”: ti,ab,kw OR MeSH descriptor: [Metatarsal Bones]) AND “fracture*”:ti,ab,kw OR MeSH descriptor: [Fractures, Bone])
The classification used had no effect on the study selection. The Lawrence and Botte (3) classification was used for the analysis. Where a study used a different term, it was „translated“ into the Lawrence and Botte classification. Also analyzed were randomized cohort studies (RCT) or comparative cohort studies which either examined the same treatment for different fracture types (according to Lawrence and Botte) or different forms of treatment for the same fracture type of the base of MT5. Exclusion criterion was the presence of other injuries, apart from a fracture of the base of MT5 on the contralateral side. The inclusion criteria in terms of the PICOS framework (13) are presented in etable 1. The study protocol was prospectively registered in PROSPERO (CRD 42020185294, 5 July 2020).
The management and implementation of the systematic literature search was conducted using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia www.covidence.org). The relevant articles were identified in a stepwise fashion, first of all based on titles and abstracts, then on the full texts, in each case by two independent investigators (VH, HP). Any disagreements were finally decided by an independent third examiner (SB). The assessment of the study quality and data extraction were also conducted by the two independent examiners (VH, HP) using Microsoft Excel (Version 16.46, Microsoft Corporation, Redmond, Washington, USA). The study parameters are presented in etable 2.
Analysis of the papers included was made based on the fracture location classification according to Lawrence and Botte (3). This classification distinguishes between three fracture types, depending on the fracture pattern in relation to the base of the 4th–5th intermetatarsal articulation: Zone 1 – proximal to the intermetatarsal articulation, Zone 2 – in the region of the articulation, Zone 3 – at the distal end of the articulation (Figure 2a). The term “early functional conservative therapy” involves immediate full weight-bearing as tolerated without immobilization.
Rating of the quality of the studies
Evaluation of the studies was performed using the “Methodological index for non-randomized studies” score (MINORS score) (7). Although the MINORS tool was developed for non-randomized studies, it is also capable of rating the quality of randomized studies and has been validated for this purpose. All studies were evaluated using the MINORS tool to ensure a uniform presentation and comparability of the quality of the studies. A comparative study can thus achieve a maximum of 24, a non-comparative study a maximum of 16 points. Evaluation of the level of evidence was conducted according to the criteria described by Wright et al. (8).