Abstract
Background: This systematic review assesses the current literature and reviews the clinical outcomes of treatment for sagittal band injuries and extensor tendon instability. Materials: A systematic search of MEDLINE, EMBASE, and the Cochrane databases was performed for English-language articles on the treatment of nonrheumatoid adult sagittal band injuries between 1969 and 2019. Two independent reviewers were involved in screening, data extraction, and critical appraisal. The level of evidence was assigned using the Sackett scale, and the methodological quality of the studies was evaluated using the Structured Effectiveness Quality Evaluation Scale (SEQES). Outcome measures were persistent pain, extensor lag, and recurrent tendon subluxation. Results: In all, 1653 abstracts were identified, with 43 articles reviewed in full text and 17 articles (429 treated digits) included in the final systematic review. There were 10 studies on surgical management, 3 on nonoperative management, and 4 on both. There were 4 retrospective case series and 13 retrospective case reports (Sackett level 4) with an average SEQES score of 15 (low quality). Studies on nonoperative management had on average more digits per study and higher SEQES scores (n = 27.7, SEQES = 19) compared with studies on surgical management (n = 11.8, SEQES = 13.8). Variability in reported outcome measures precluded meta-analysis. Conclusion: Qualitative synthesis of available literature suggests that acute sagittal band injuries can be successfully treated by splinting the injured digit in neutral or hyperextension. Patients with chronic injuries or those failing nonoperative management may benefit from surgical exploration. A lack of consistent outcome measures precluded comparison of surgical techniques.
Keywords: centralization, extensor tendon, sagittal band, subluxation
Introduction
The sagittal bands (SBs) arise from the volar plate and deep transverse metacarpal ligaments and act as the primary stabilizers of the extensor tendon. The SB envelopes the extensor tendon, with the thick deeper layer supporting the extensor tendon within a groove and the thin superficial layer traversing above the tendon. 1 Injury to the SB causes persistent swelling, pain, and extensor tendon instability, resulting in limitations to full active metacarpophalangeal (MCP) joint extension. Ulnar-sided tendon instability and dislocation are more common. The radial SBs are more prone to rupture compared to the ulnar SBs due to a combination of thinner and longer radial SBs and more substantial ulnar-sided juncturae tendinum causing increased radially directed forces.2,3 The prominence of the third metacarpal head and looser attachment of the transverse fibers also render it more susceptible to injury compared with the other digits.4,5 Disruptions of SB can be posttraumatic due to a direct blow or fall, spontaneous due to low-energy activities such as flicking or snapping, or congenital due to absence or attenuation. 6 In spontaneous SB injuries, the superficial layer is torn adjacent to the extensor tendon, whereas in traumatic SB injuries both layers are torn several millimeters away from the extensor tendon. 1
Rayan and Murray 5 classified SB injuries into 3 types. Type I injuries resulted in tenderness, but no tendon instability. Type II is associated with tendon subluxation, defined as lateral tendon displacement but maintenance of contact with the metacarpal condyle. Type III is marked by tendon dislocation, with displacement of the tendon within the groove between 2 metacarpal heads.
Injuries of SB are rare in nonrheumatoid patients, and there is a lack of treatment guidelines. The indications for surgical compared with nonoperative management greatly vary throughout the literature, especially for acute injuries. In addition, numerous reconstructive surgical techniques are described in isolated small case series without comparison of outcomes. The purpose of this systematic review is to assess the current literature and review the indications and clinical outcomes of treatment for adult nonrheumatoid SB injuries. We hypothesize that acute injuries can be successfully managed with splinting protocols and that chronic injuries will require surgical reconstruction.
Materials and Methods
This systematic review was conducted with clinical librarian assistance and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. 7 A broad search strategy was used with the keywords “sagittal band,” “extensor tendon,” “tear,” “rupture,” “dislocation,” and “subluxation” in MEDLINE (Pubmed), EMBASE (Ovid), and the Cochrane Central Register of Controlled Trials. The complete search strategy is available upon request. Publication language was restricted to English-language texts. Studies that reported on the outcomes of surgical or nonsurgical management of extensor tendon dislocations and SB injuries in at least 5 digits were included for data extraction and critical appraisal. There were no restrictions on publication date. Study exclusion data were as follows: fewer than 5 digits included in the study, pediatric patients, thumb involvement, patients with rheumatological and connective tissue diseases, congenital tendon dislocations, and Sackett level 5 evidence studies including expert opinion, single case studies, biomechanical studies, or surgical technique papers without outcome data (Table 1).
Table 1.
Inclusion and Exclusion Criteria for Article Selection.
| Study Selection Criteria |
|---|
| Papers were selected for final review if they met the following criteria: 1. Type of study: Sackett levels 1-4 (randomized controlled trials, prospective trials, retrospective trials, and case series) 2. Type of patient: adults aged >18 years 3. Type of injury: sagittal band tear or rupture 4. Etiology of injury: traumatic or spontaneous 5. Digits involved: 5 or more Papers were excluded for final review if they met any of the following criteria: 1. Type of study: Sackett level 5 (expert opinion, biomechanical, individual case studies, review, technical, epidemiologic papers) 2. Type of patient: pediatric, patients with connective tissue diseases or rheumatoid arthritis 3. Type of injury: dorsal capsule ruptures, collateral ligament 4. Etiology of injury: congenital 5. Digits involved: thumb or less than 5 |
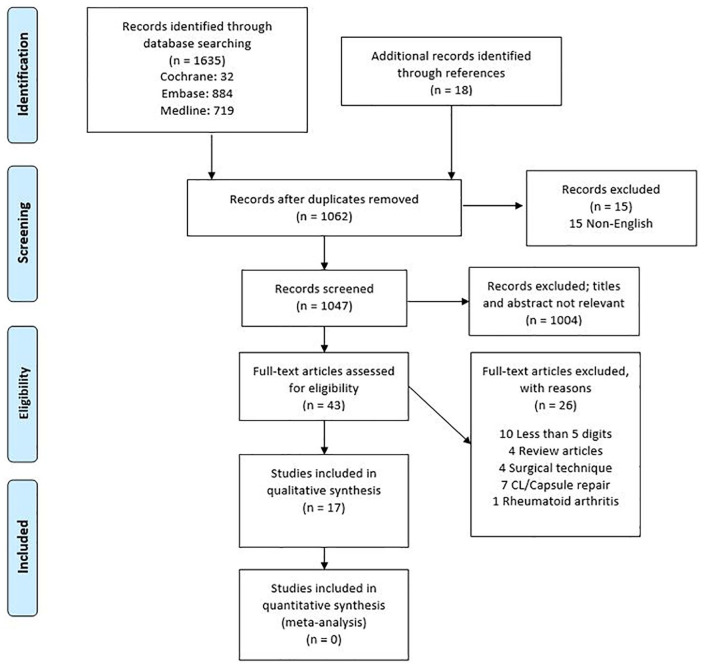
All the following steps were completed by 2 independent evaluators (K.W., G.M.) and discrepancies resolved by the senior author (N.S.). A total of 1635 articles published between 1969 and 2019 were identified through the bibliographical search, and after duplicates were removed, titles and abstracts were reviewed for studies meeting the inclusion/exclusion criteria. Reference lists of articles were also screened, further identifying 18 abstracts. After title and abstract screening, 1004 articles were excluded and 43 articles reviewed in full text. Articles describing both surgical and nonsurgical interventions were only included if there were at least 5 digits treated in each treatment method.
Data extraction was performed using a predefined data collection form by 2 independent reviewers and included study characteristics (authors, publication year, study design), patient demographics, affected digits, treatment type (surgical or nonsurgical), description of surgical technique or splinting protocol, length of follow-up, and outcome measures. When available, 3 separate outcomes were recorded, including persistent extensor tendon subluxation, range of motion and extensor lag, and persistent pain.
The methodological quality of included articles was assessed using the Structured Effectiveness Quality Evaluation Scale (SEQES). 8 This validated scale rates the study’s design, subjects, intervention, outcomes, analysis, and recommendations. Studies with a score of 0 to 16 were considered of low quality, 17 to 32 of moderate quality, and 33 to 48 of high quality. The level of evidence was evaluated using the Sackett level of evidence scale. 9 The variability in reported outcomes across studies precluded pooling of results for meta-analysis.
Results
The initial search yielded 1062 articles after removal of duplicates. After title and abstract screening, a total of 43 articles were considered for inclusion in the systematic review and were reviewed in full text. Of these, 10 articles were excluded due to inclusion of less than 5 treated digits, 4 were review articles, 4 were descriptions of surgical techniques without any reported patient outcome data, 7 described treatment and outcomes for MCP capsular tears or collateral ligament injuries, and 1 included patients with rheumatoid arthritis. A total of 17 articles were included in the final systematic review and qualitative synthesis1,3,5,10-23 (Figure 1).
Figure 1.
Flow diagram of systematic search strategy, reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement.
Of the 17 articles included in the systematic review, 10 discussed surgical management with descriptions of varying techniques for direct repair or extensor centralization, 3 discussed nonoperative management and splinting protocols, and 4 included both treatment strategies. There were a total of 429 digits treated. Most patients were men (68% men, 32% women) with a mean age of 40 years (mean age = 19-83 years). Of the studies that specified the affected digit, the long finger was the most commonly involved (65%), followed by the ring (15%), small (12%) and index (8%) fingers. Extensor tendon subluxation was predominantly in the ulnar direction (87%) compared with radial (13%). However, when border digits are involved, either the extensor digitorum communis (EDC) tendon dislocates radially and the extensor indicis propius/extensor digiti minimi tendon dislocates ulnarly, or both dislocate ulnarly.5,11,14 The mean length of follow-up was 22 months (range, 3-71 months).
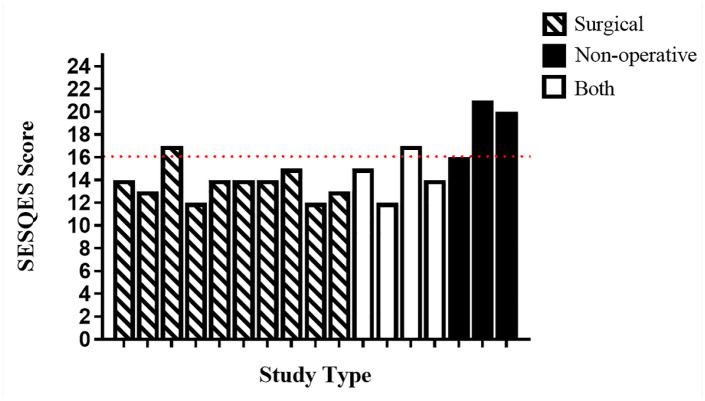
Critical appraisal of the studies shows that most are of low quality. Four studies were single-center retrospective case series (Sackett level 4) with the defined inclusion and exclusion criteria,13,14,17,22 and the remaining 13 were retrospective case reports (Sackett level 4). According to the SEQES scores, only 4 articles were considered to be of moderate quality (scores 17-32),13,14,17,22 with the remaining being ranked as low-quality articles (scores 0-16). The mean SEQES score was 15 (range, 12-21), with no article achieving a high-quality rating (Figure 2). Studies on nonoperative management had on average more digits per study and higher SEQES scores (n = 27.7, SEQES = 19) compared with studies on surgical management (n = 11.8, SEQES = 13.8).
Figure 2.
SEQES score stratified by study type (surgical, nonoperative, or both). Red dotted line shows delineation of low-quality studies (scores 0-16) and moderate-quality studies (scores 17-32).
Note. SEQES = Structured Effectiveness Quality Evaluation Scale.
Nonoperative Management
The literature search revealed 7 studies discussing nonoperative treatment of SB injuries, including 3 retrospective case series14,17,22 and 4 retrospective case reports.3,5,12,19 Rayan and Murray 5 described the treatment of acute SB injuries presenting within 3 weeks of injury with a palmar splint with the MCP joint in neutral position for type II or III injuries and Velcro buddy splinting for type I injuries. Patients were splinted for 3 weeks, followed by 3 more weeks of protected range of motion. Of the 18 digits treated, 4 had painless tendon subluxation/dislocation at 24 months (1 type II, 3 type III); however, all patients were pain-free with resistive motion and maintained full range of motion. In contrast, Arai et al 19 reported similar splinting protocols that failed in all patients; however, the average time from injury to presentation was 7 weeks. All patients went on to surgical exploration, and the extensor hood was found to be ruptured in all 8 cases and the joint capsule ruptured in 6 cases. The authors hypothesized decreased success with nonoperative management in cases of associated capsular injury and longer time to presentation.
Catalano et al 3 used a low-profile thermoplastic “sagittal band bridge” splint that held the injured MCP joint in an additional degree of extension relative to the uninjured digits, rather than in neutral. The proximal and distal interphalangeal joints were unrestricted and left free for active range of motion. Patients were splinted for 8 weeks; however, only 8 of 11 patients were compliant with the entire duration of splinting. Of the 11 patients evaluated, all with type III injuries, 3 patients (27%) failed conservative management with persistent painful subluxation. A larger study of 101 digits treated with the SB bridge splint for 6 weeks, followed by part-time splinting for 2 to 4 weeks shows an overall success rate of 84%, with complete resolution of symptoms at 13 weeks. 17 Some authors14,24 believe that splinting should only be offered to patients presenting less than 10 days from injury, but subgroup analysis in this study shows 94% resolution of symptoms in acute (<3 weeks), 90% in subacute (3-6 weeks), and 62% in chronic (>6 weeks) injuries.
A more recent study by Roh et al 22 including 94 digits (20 type I, 38 type II, 36 type III) treated with 7 weeks of splinting (5 weeks full-time, 2 weeks part-time) with a hand-based thermoplastic MCP extension (P1 blocking) splint showed 71% success in resolution of symptomatic tendon subluxation/dislocation. Multivariate analyses indicate occupation as a manual laborer, longer time to presentation, and type III injuries as predictive of higher likelihood of treatment failures.
Surgical Management
The literature search revealed 14 studies focusing on operative management of SB injuries, including 2 retrospective case series13,14 and 12 retrospective case reports.1,5,10-12,15,16,18-21,23 Indications for surgical management of SB injuries differed among studies and included patients who failed a trial of splinting, with delayed presentation, and inability to tolerate prolonged splinting such as in professional athletes. Broadly, the surgical management of SB injuries is divided into direct repair techniques and reconstructive techniques to recreate the pulley formed by the SBs.
In acute injuries, exploration and direct repair of the SB produces good results overall1,5,10-14,19,20; however, authors differ in their preference for imbrication of the torn SB,5,12,20 release of the nonaffected SB,5,10,20 and repair of the dorsal capsule.11,19 Most authors performed these procedures under local anesthetic to confirm tendon stability and proper tensioning through a full range of motion. Hong et al 13 reported on 26 patients with spontaneous SB injuries (20 type II, 6 type III) treated with direct repair of the SB to the lateral side of the extensor tendon with a continuous interlocking 3-0 Ethibond suture. All patients regained full range of motion without any extensor tendon instability, and only 1 patient had persistent intermittent pain at 6 months. In cases where both superficial and deep SBs are torn, Ishizuki 1 supported the use of 2 anchoring sutures between the extensor tendon and deep SB, in addition to repair of the superficial layer to the extensor tendon.
Arai et al 19 and Koniuch et al 12 advocated for the repair of both the SB and dorsal capsule in separate layers if also torn, whereas Hame and Melone 11 recommended against repair of the capsule to avoid tension over the repair and loss of motion. They reported on the direct repair of 11 digits with the MCP joint in 60° to 70° of flexion and demonstrated that repair of the capsule is not necessary, with all 8 patients returning to professional sports within 5 months. Another study by Lee et al 10 described separating the radial SB from the joint capsule, suturing the radial aspect of the radial SB to the paratenon of the extensor tendon, draping this across the extensor tendon, and then suturing the radial SB to the ulnar SB. A series of 13 patients treated with this method had full range of motion, complete resolution of pain, and no further tendon instability. When direct repair alone is not enough to centralize the extensor tendon, a combination of release of tight ulnar structures (ulnar SB, ulnar collateral ligament, juncturae tendinum) and imbrication or reefing of the radial SB may be necessary.5,20 Using these techniques, Love and MacLean 20 successfully treated 7 digits with complete resolution of symptoms and extensor instability, except for 1 patient who was overcorrected and had asymptomatic radial deviation.
When SB tissue is deficient and repair is not possible, SB reconstruction is necessary to centralize the extensor tendon. Most of the reconstructive methods in the literature are based on the Kilgore et al 25 technique using the radial one-third of the EDC tendon as a distally based graft. The tendon graft is used to anchor the extensor tendon around the radial collateral ligament as a pulley before being sewn or weaved back on itself. The original 1975 paper was a description of this surgical technique for ulnar EDC subluxation without patient outcomes, and thus had been excluded from this systematic review.
Modifications based on the Kilgore 16 technique include anchoring the tendon around deep transverse metacarpal ligament or using the ulnar one-third of the EDC tendon instead to create greater radial tethering force.16,18,23 Most of these studies report excellent results with no recurrent tendon subluxation and pain-free full range of motion. Vaccaro et al 18 reported on a series of 26 digits treated with an ulnarly based tether with recurrence of subluxation of 3 digits in 1 patient. The reconstructed SB/tether point must be carefully chosen and passed through an isometric point. 26 Placement too proximally will limit full MP extension, and placement too distally will lead to persistent tendon instability. Watson et al 16 used a radial strip started 4 cm proximal to the MCP joint looped around the deep transverse metacarpal ligament and reported that the tether should be 8 to 14 mm proximal to the articular surface of the proximal phalanx with the MCP joint in flexion. This repair was protected with Kirscher wire immobilization of the MCP joint in 15° to 20° of flexion for 3 weeks and demonstrated good results, with all 7 patients returning to their prior occupation within an average of 48 days. For radial SB reconstruction in the long finger, Shiode and Moritomo 21 described the use of a distally based half-slip of the index EDC tendon, redirected 90° and passed through the long finger EDC at the MCP joint, and then sutured on itself to create a tether between the extensor tendons. Postoperatively, patients are buddy taped for 3 weeks, and a case series of 6 digits show complete resolution of symptoms. A final technique uses a 3- to 4-cm palmaris longus (PL) graft woven through a bone tunnel through the metacarpal neck and then back through itself to create a pulley around the EDC tendon, 15 with good results and resolution of symptoms in 6 digits.
Discussion
The available literature shows that acute SB injuries presenting less than 3 weeks from injury can be successfully treated with nonoperative management and splinting for 3 to 6 weeks. Surgical intervention may be considered in patients who are manual labors or those with type III injuries or subacute/chronic injuries that have failed nonoperative management. When possible, direct repair of the ruptured SBs is the simplest option. Procedures performed under wide-awake local anesthetic will aid in intraoperative decision as to the necessity of dorsal capsule repair, SB imbrication or reefing, and release of tight structures, including juncturae tendinum, noninjured SB, or collateral ligaments, to ensure tendon relocation without compromising the range of motion. When the ruptured SBs are attenuated, EDC or PL tendon graft can be used to recreate the SB pulley anchored around the radial collateral ligaments, deep transverse metacarpal ligaments, or metacarpal itself.
The 17 studies included in this systematic review were of low to moderate quality, and limited to retrospective case series or reports, which precluded direct comparison of techniques for superiority. All studies reporting on surgical SB reconstruction consisted of nonconsecutive case reports of a small group of patients with high risk of bias, and thus prevented any direct comparison of outcomes. The lack of standardized reporting of patient demographics, degree of injury, time from injury, and variable follow-up time prevented conclusive recommendations. Furthermore, SB injuries represent a spectrum of severity from simple tears to complete tendon dislocation. Few studies reported on Rayan-Murray injury type, and thus outcomes are difficult to interpret within a heterogeneous population.
Limitations of the study include the use of nonindependent sample sizes. Most studies included both patients with isolated and multiple affected digits. Except for 1 study, 11 those on surgical management were either on digits that had failed splinting or did not explicitly specify. Furthermore, we were not able to select patients who received treatment of only isolated digits, and thus, only a narrative review of the data available is provided. A high-quality long-term prospective study of isolated single-digit injuries with stratification by Rayan-Murray type is required to compare the efficacy of various surgical techniques and to develop evidence-based treatment guidelines for nonrheumatoid SB injuries.
Footnotes
Ethical Approval: This study is exempt from institutional review board approval.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was not obtained as the study was a systematic review of the literature.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kitty Wu  https://orcid.org/0000-0002-9389-1740
https://orcid.org/0000-0002-9389-1740
References
- 1. Ishizuki M. Traumatic and spontaneous dislocation of extensor tendon of the long finger. J Hand Surg Am. 1990;15(6):967-972. [DOI] [PubMed] [Google Scholar]
- 2. Saldana MJ, McGuire RA. Chronic painful subluxation of the metacarpal phalangeal joint extensor tendons. J Hand Surg Am. 1986;11(3):420-423. [DOI] [PubMed] [Google Scholar]
- 3. Catalano LW, III, Gupta S, Ragland R, III, et al. Closed treatment of nonrheumatoid extensor tendon dislocations at the metacarpophalangeal joint. J Hand Surg Am. 2006;31(2):242-245. [DOI] [PubMed] [Google Scholar]
- 4. Kettelkamp DB, Flatt AE, Moulds R. Traumatic dislocation of the long-finger extensor tendon. A clinical, anatomical, and biomechanical study. J Bone Joint Surg Am. 1971;53(2):229-240. [PubMed] [Google Scholar]
- 5. Rayan GM, Murray D. Classification and treatment of closed sagittal band injuries. J Hand Surg Am. 1994;19(4):590-594. [DOI] [PubMed] [Google Scholar]
- 6. Kleinhenz BP, Adams BD. Closed sagittal band injury of the metacarpophalangeal joint. J Am Acad Orthop Surg. 2015;23(7):415-423. [DOI] [PubMed] [Google Scholar]
- 7. Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- 8. Suh N, Benson EC, Faber KJ, et al. Treatment of acute scaphoid fractures: a systematic review and meta-analysis. Hand. 2010;5(4):345-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Muller M, Tsui D, Schnurr R, et al. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17(2):210-228. [DOI] [PubMed] [Google Scholar]
- 10. Lee JH, Baek JH, Lee JS. A reconstructive stabilization technique for nontraumatic or chronic traumatic extensor tendon subluxation. J Hand Surg Am. 2017;42(1):e61-e65. [DOI] [PubMed] [Google Scholar]
- 11. Hame SL, Melone CP., Jr. Boxer’s knuckle in the professional athlete. Am J Sports Med. 2000;28(6):879-882. [DOI] [PubMed] [Google Scholar]
- 12. Koniuch MP, Peimer CA, VanGorder T, et al. Closed crush injury of the metacarpophalangeal joint. J Hand Surg Am. 1987;12(5 Pt. 1):750-757. [DOI] [PubMed] [Google Scholar]
- 13. Hong IT, Oh CH, Sim YS, Han SH. Direct repair of the sagittal band for extensor tendon subluxation caused by finger flicking. Orthopade. 2017;46(9):755-760. [DOI] [PubMed] [Google Scholar]
- 14. Inoue G, Tamura Y. Dislocation of the extensor tendons over the metacarpophalangeal joints. J Hand Surg Am. 1996;21(3):464-469. [DOI] [PubMed] [Google Scholar]
- 15. Kang L, Carlson MG. Extensor tendon centralization at the metacarpophalangeal joint: surgical technique. J Hand Surg Am. 2010;35(7):1194-1197. [DOI] [PubMed] [Google Scholar]
- 16. Watson HK, Weinzweig J, Guidera PM. Sagittal band reconstruction. J Hand Surg Am. 1997;22(3):452-456. [DOI] [PubMed] [Google Scholar]
- 17. Peelman J, Markiewitz A, Kiefhaber T, et al. Splintage in the treatment of sagittal band incompetence and extensor tendon subluxation. J Hand Surg Eur Vol. 2015;40(3):287-290. [DOI] [PubMed] [Google Scholar]
- 18. Vaccaro AR, Kupcha P, Schneider LH. The operative repair of chronic nontraumatic extensor tendon subluxations in the hand. Hand Clin. 1995;11(3):431-440. [PubMed] [Google Scholar]
- 19. Arai K, Toh S, Nakahara K, et al. Treatment of soft tissue injuries to the dorsum of the metacarpophalangeal joint (Boxer’s knuckle). J Hand Surg Br. 2002;27(1):90-95. [DOI] [PubMed] [Google Scholar]
- 20. Love GJ, MacLean JG. Ulnar subluxation of the extensor tendons in elderly osteoarthritic females: a neglected diagnosis. J Hand Surg Eur Vol. 2007;32(1):45-49. [DOI] [PubMed] [Google Scholar]
- 21. Shiode R, Moritomo H. Tether creation between the second and third extensor digitorum communis for third extensor tendon subluxation at the metacarpophalangeal joint. Tech Hand Up Extrem Surg. 2018;22(4):146-149. [DOI] [PubMed] [Google Scholar]
- 22. Roh YH, Hong SW, Gong HS, et al. Prognostic factors for nonsurgically treated sagittal band injuries of the metacarpophalangeal joint. J Hand Surg Am. 2019;44(10):897.e1-897.e5. [DOI] [PubMed] [Google Scholar]
- 23. Carroll C, Moore JR, Weiland AJ. Posttraumatic ulnar subluxation of the extensor tendons: a reconstructive technique. J Hand Surg Am. 1987;12:227-231. [DOI] [PubMed] [Google Scholar]
- 24. Araki S, Ohtani T, Tanaka T. Acute dislocation of the extensor digitorum communis tendon at the metacarpophalangeal joint. A report of five cases. J Bone Joint Surg Am. 1987;69(4):616-619. [PubMed] [Google Scholar]
- 25. Kilgore ES, Graham WP, Newmeyer WL, et al. Correction of ulnar subluxation of the extensor communis. Hand. 1975;7(3):272-274. [DOI] [PubMed] [Google Scholar]
- 26. Andruss RJ, Herndon JH. Ulnar subluxation of the extensor digitorum communis tendon: a case report and review of the literature. Iowa Orthop J. 1993;13:208-213. [PMC free article] [PubMed] [Google Scholar]