Abstract
Background: To present a retrospective study on the outcomes of a modified version of suture suspension arthroplasty with trapeziectomy on patients with thumb basal joint arthritis and to evaluate the relationship between the degree of subsidence and functional outcome. Methods: We performed a chart review on 67 patients (75 thumbs) who were surgically treated for thumb carpometacarpal osteoarthritis with trapeziectomy and suture suspension arthroplasty from May 2010 to May 2016. Outcome measures included Disabilities of the Arm, Shoulder and Hand (DASH), grip strength, lateral/precision pinch strength, range of motion, and return to work/resumption of usual activities. Radiographic images were used to measure first metacarpal subsidence into the trapezial space. Results: Clinical outcomes were satisfactory, showing an initial postoperative DASH score of 45.94, which decreased to 27.93 at 6 months postoperatively and to 19.69 at 1 year postoperatively. Radiographic images revealed a mean first metacarpal subsidence of 39% compared with the preoperative images. Grip and pinch strengths showed steady improvement from initial postoperative to final follow-up visits, resulting in 90% recovery of gross grasp, 77% recovery of lateral pinch, and 79% recovery of precision pinch compared with the contralateral side. Conclusions: Our study has found that suture suspension arthroplasty with trapeziectomy is an effective treatment for thumb basal joint arthritis. Suture suspension arthroplasty allows for short immobilization time, avoids tendon sacrifice, avoids anchor use, and leaves a cosmetically appealing scar. Furthermore, a relationship of any significance between postoperative first metacarpal subsidence and functional outcomes does not appear.
Keywords: basal joint arthritis, suture suspension arthroplasty, trapeziectomy, subsidence, thumb, anatomy
Introduction
Thumb carpometacarpal (TMC) joint is the most common site of surgical reconstruction for osteoarthritis of the joints of the upper extremity.1,2 It is a very common condition, with a radiographic prevalence of 25% in men and 40% in women above the age of 75 years. 3 Initial management for early disease includes conservative modalities such as splinting, physical therapy, nonsteroidal anti-inflammatory drugs, and corticosteroid injections. When conservative treatment fails, surgical intervention is recommended.4,5 There are numerous surgical options described in the literature, all of which aim to relieve pain and improve range of motion and function. No one technique has yet proven superior.6,7
Most basal joint reconstructive procedures involve some form of partial or complete excision of the trapezium, followed by interposition and suspension arthroplasty with tendon graft or repositioning, implant arthroplasty, or a combination of both.1,6 After the initial description of ligament reconstruction and tendon interposition (LRTI), many anchoring techniques were devised involving tendon harvest.8-11 Although these methods are viable options for the treatment of TMC arthritis, they are not without morbidity. Del Signore and Accardi 12 introduced an arthroplasty technique involving trapeziectomy followed by creation of a tendon suspension sling using a nonabsorbable suture to maintain trapezial space. The purpose of this study was to assess short- to intermediate-term radiographic and functional outcomes of a modified technique of suture suspension arthroplasty and trapeziectomy for the treatment of TMC arthritis. We cast special attention to the first metacarpal subsidence into the trapezial space following our modified suture suspension technique, specifically. We report on the relationship among subsidence, patient satisfaction, and clinical outcomes.
Materials and Methods
All participants involved in this study signed informed consent prior to participation, and record-keeping was in compliance with the Health Insurance Portability and Accountability Act. This study was not submitted to an institutional review board. There was no external source of funding for this study.
Clinical Study
A retrospective chart review was conducted on all patients seen at our office who were surgically treated for TMC osteoarthritis with trapeziectomy and suture suspension arthroplasty from May 2010 to May 2016. In 71 patients who consented to this study, 79 consecutive trapeziectomies with suture suspension arthroplasty were performed. Information was collected anonymously from individual patient records and compiled into a database. Data collected included age, sex, occupation, hand dominance, mechanism of injury, concomitant procedures, operation time, immobilization time, and time of return to work. Grip strength was evaluated by our certified hand occupational therapist based on gross grip, lateral pinch, and precision pinch at an average of 10 weeks, 6 months, 1 year, and at final follow-up. Grip strength of the contralateral side was used as a comparative value. Active range of motion (AROM) and thumb range of motion (TROM) were recorded at 10 weeks and 6 months. Disabilities of the Arm, Shoulder and Hand (DASH) questionnaires were distributed to patients at all follow-up appointments after surgery to assess subjective pain and functional outcome.
Posteroanterior (PA) radiography of the hand and wrist was taken preoperatively and postoperatively. Patient radiographic images were excluded if images were unavailable or performed using outdated technology. For consistency, only radiographs using Picture Archiving and Communication System technology were included in our analysis. Posteroanterior radiography was used to determine first metacarpal subsidence using the methods described by Kadiyala et al. 13 Two measurements were taken with PA radiography: the distance between the distal pole of the scaphoid and the base of the first metacarpal (α value) and the length of the proximal phalanx of the thumb (β value). The α value was divided by the β value to determine the trapzioscaphoid ratio, which provided a normative value to determine subsidence. Radiographs without measurable α or β values were excluded from calculations. A Spearman test of correlation was performed between total active motion (TaM) of the thumb and percent subsidence, between percent strength recovery and percent subsidence, and between final DASH scores and percent subsidence.
All diagnoses of basal joint arthritis were made by the primary and secondary authors (A.M. and J.B.M.) based on clinical and radiographic findings. Only patients with Eaton grades II, III, and IV were operated on. All patients failed conservative management and subsequently agreed to undergo surgical intervention. Patients with grade IV thumb carpometacarpal (CMC) arthritis, preoperatively and intraoperatively, were treated with a partial or complete removal of the trapezoid and were excluded from the study. All surgeries were performed by A.M. and J.B.M. at an outpatient ambulatory surgery center.
Surgical Technique
Our surgeons performed a slightly modified version of the suture suspension technique originally described by Del Signore et al. (2009). A modified Wagner incision (Figure 1) is made, and the trapezium is excised in a standard manner. The modified Wagner incision eliminates the longitudinal portion of the incision, only cutting transversely near the proximal crease of the wrist. Maintaining a palmar incision helps to avoid damage of the dorsal sensory branch of the radial nerve. As our modified incision falls within the wrist crease, it gives rise to a more cosmetically appealing scar.
Figure 1.

Modified Wagner incision. The longitudinal portion of the incision is eliminated, and only the transverse portion of the incision is made within the distal wrist crease.
Following excision of the trapezium, a suture of 0 fiber wire is passed through the abductor pollicis longus (APL) across the trapezial space, around and into the flexor carpi radialis (FCR) and back again deep to superficial through the APL (Figure 2). This is repeated again so that the suture passes through each tendon twice, and then the suture is tied off at the starting point. The suture is tied with the thumb held in abduction. The suture should not be too close to the metacarpal; otherwise, it may give rise to abduction contracture, nor should it be too loose to prevent a floppy thumb. If there is a capsule, a capsular closure can be done using bioabsorbable sutures. In most cases, we found it to be unnecessary to perform a capsular closure. However, in cases where enough tissue was present for a capsular closure, it was performed. This did not have an effect on patient outcomes.
Figure 2.
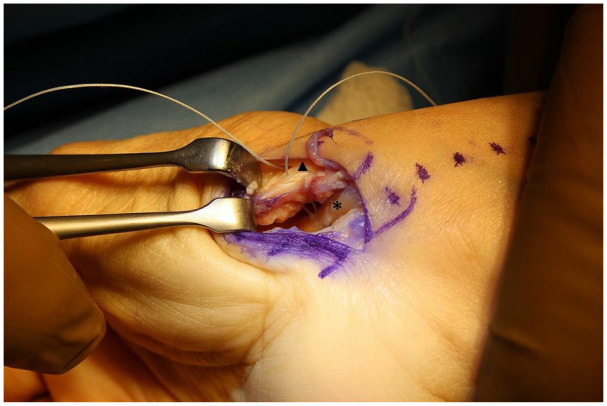
Sutures are tied to the flexor carpi radialis (*) and abductor pollicis longus (Δ) in the trapezial space as opposed to the base of the first metacarpal.
The wound is closed via a subcuticular closure, and the patient is placed in a thumb spica splint for 2 weeks. After 2 weeks, the patient returns for inspection of the wound and referral to an occupational therapist for fabrication of a custom orthosis. Most of our patients were seen by our in-office occupational therapist; however, some patients pursued alternate therapists. Patients who were not followed by our therapist were excluded from the study. Therapy was instructed to begin with AROM under supervision for 4 weeks. The patient is permitted to remove orthosis only for hygiene purposes with careful instruction not to challenge the thumb by heavy gripping or pinching. At 6 weeks, the orthosis is weaned out, and the patient is permitted to do light activities until the 12th week, after which the patient is allowed full unrestricted activity. Patients were interviewed at subsequent follow-up visits to confirm that they were following the necessary postoperative protocol.
Results
Four patients were excluded from the study based on a diagnosis of Eaton stage IV and subsequent partial removal of the trapezoid. Therefore, 75 thumbs of 67 patients were treated with trapeziectomy and our modified technique of suture suspension arthroplasty. The mean age of the study population was 63.7 years (range: 34-84 years). Forty-eight patients (71.6%) were women, and 19 (28.4%) were men. There were 41 right-hand injuries and 34 left-hand injuries. Eight patients had both hands operated on, 6 of them being women. There were 32 dominant injuries and 43 nondominant injuries.
The average time from surgery to final follow-up was 35 months (range: 2-99 months). The mean operative time from time in to time out was 61 minutes (range: 26-131 minutes), and the mean immobilization (n = 63) time following surgery was 2.9 weeks (range: 0.9-32.4 weeks). Only 1 patient was immobilized for longer than 8 weeks. The average time to return to work (n = 43) was 130 days (range: 7-775 days). Gross grip (n = 43), lateral pinch (n = 43), and precision pinch (n = 40) recovered 90%, 77%, and 79%, respectively, at final follow-up (Table 1). Mean extension/flexion of the CMC, metacarpal phalangeal (MP), and interphalangeal (IP) joints of the thumb at 6 months were 24°/20°, −1.2°/50°, and −1.2°/61°, respectively. The mean TaM of the thumb at 6 months was 155. At an average of 6 months postoperatively, dorsiflexion, volar flexion, radial deviation, ulnar deviation, pronation, and supination were 64°, 59°, 19°, 27°, 89°, and 85°, respectively (Table 2). Mean DASH scores decreased from 45.94 postoperatively to 23.16 at final follow-up.
Table 1.
Postoperative Grip Strength (kg).
| Grip strength | GG | LP | PP |
|---|---|---|---|
| Contralateral | 22.1 ± 12 | 5.4 ± 3 | 3.8 ± 2 |
| 10 weeks | 11.9 ± 8 | 2.8 ± 2 | 2.3 ± 1 |
| 6 months | 14.2 ± 10 | 3.3 ± 2 | 2.5 ± 1 |
| 1 year | 15.7 ± 8 | 3.5 ± 1 | 2.5 ± 1 |
| Final | 19.9 ± 13 | 4.2 ± 2 | 3.0 ± 2 |
| % Recovered | 90 | 77 | 79 |
Note. GG = gross grip; LP = lateral pinch; PP = precision pinch
Table 2.
TROM and AROM.
| Variable | 10 Weeks | 6 Months |
|---|---|---|
| TROM | ||
| Metacarpal phalangeal (extension/flexion) | −0.5°/47.6° | −1.2°/49.9°−1.2°/60.7°24.4°/19.9° |
| Interphalangeal (extension/flexion) | 0.0°/62.9° | |
| Carpometacarpal (extension/flexion) | 20.3°/20.4° | |
| Total active motion | 158.0 | 155.0 |
| AROM | ||
| Dorsiflexion | 63.8° ± 8.5° | 63.9° ± 7.8° |
| Volarflexion | 58.8° ± 12.4° | 59.4° ± 13.3° |
| Radial deviation | 20.3° ± 4.2° | 19.0° ± 5.8° |
| Ulnar deviation | 28.3° ± 6.4° | 27.4° ± 7.4° |
| Pronation | 88.0° ± 7.6° | 88.9° ± 2.8° |
| Supination | 83.9° ± 7.0° | 84.6° ± 7.4° |
Note. TROM = thumb range of motion; AROM = active range of motion.
We observed 4 complications in our cohort. One patient had a suture abscess with infection that was drained and resolved without requiring any further intervention. Three of our patients reported issues with the FiberWire as it was protruding and causing pain and discomfort. All 3 cases returned to the operating room for removal of sutures. There was no further complication in all 3 cases. Following this complication, extra care was taken to bury the knot deeper into the tissue. Since this complication, there have not been any further incidences of FiberWire protrusion.
Forty-one preoperative and postoperative radiographs were available with measurable α and β values. Final postoperative radiographs were taken at a mean of 393 days (range: 20-2828 days) after surgery. Trapzioscaphoid ratio decreased by an average of 0.15 between preoperative and postoperative radiographs, equating to 39% subsidence following our technique of suture suspension arthroplasty (Table 3). Pearson correlation test was performed between TaM, percent gross grip strength recovery, and final DASH scores and percent subsidence. The correlation coefficient was 0.31 between TaM and percent subsidence, 0.08 between percent strength recovery and percent subsidence, and −0.09 between final DASH scores and percent subsidence (Figure 3).
Table 3.
Preoperative and Postoperative Radiographic Results of Subsidence Into the Trapezial Space.
| Subsidence | α (mm) | β (mm) | Trapzioscaphoid ratio |
|---|---|---|---|
| Preoperative | 11.21 ± 1.8 | 29.92 ± 2.7 | 0.38 ± 0.05 |
| Postoperative | 6.76 ± 2.4 | 29.48 ± 3.1 | 0.23 ± 0.07 |
| Difference | −0.15 | ||
| Percent subsidence | 39% | ||
Figure 3.
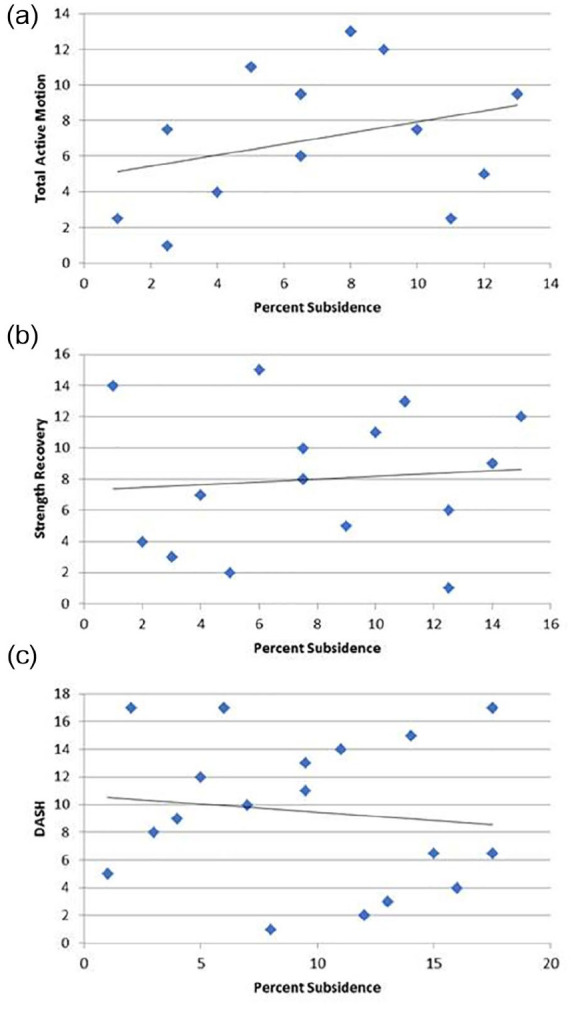
(a) Percent subsidence versus total active motion of the thumb, (b) percent subsidence versus percent strength recovery, and (c) percent subsidence versus final DASH scores.
Note. DASH = Disabilities of the Arm, Shoulder and Hand.
Discussion
Our modified suture suspension arthroplasty technique has shown acceptable short- to intermediate-term results in our cohort. Juxtaposed with previously described techniques, suture suspension arthroplasty avoids the potential complications associated with tendon harvest and prolonged immobilization. We have been performing suture suspension arthroplasty since Del Signore et al originally published their technique article in 2009, and it is our opinion that this procedure is a reliable and an easily reproducible procedure for the treatment of TMC arthritis.
Numerous surgical techniques have been described for the treatment of advanced-stage TMC degenerative joint disease, including trapeziectomy, hematoma distraction arthroplasty, LRTI, APL suspensionplasty, implants, and hemiarthroplasty.8-11,14-16 All these methods are effective in certain facets of operative intervention for TMC arthritis; however, they have their drawbacks: Pin tract complications such as infection, nerve damage, and stiffness from prolonged immobilization can occur with methods that involve temporary pin fixation. Ligament reconstruction and tendon interposition techniques involve tendon sacrifice, entailing additional dissection and the potential for donor site morbidity. Carpometacarpal hemiarthroplasty risks include implant loosening, increased subluxation, increased dislocation rates, and osteonecrosis of the trapezium. 16 Implant instability serves as a top concern of implant arthroplasty techniques, with failure rates reported as high as 55% in the literature. 15 Incidence of up to 40% dislocation rate has also been reported following TMC silicone arthroplasty. 17
This study analyzes the short- to intermediate-term functional and radiographic outcomes of a slightly modified version of the Del Signore et al suture suspension arthroplasty technique. Our method differs from that of Del Signore et al in that we suture the APL and FCR together more proximally than done by Del Signore et al, and not at the insertion of the 2 tendons at the base of the first metacarpal. We believe that suturing the tendons at the base of the metacarpal may lead to abduction contracture. In addition, we have found that suturing the tendons in the trapezial space as opposed to the base of the metacarpal is easier to perform and produces positive results. Recently, we have begun inserting a Kirschner wire into the trapezium to act as a joystick to facilitate excision. Suture suspension arthroplasty remains steadfast to the basic principles of TMC arthritis treatment, which include excision of the trapezium, correction of subluxation, and maintenance of the joint space.
Our cohort reports excellent reduction of pain, with DASH scores decreasing from 45.94 at initial follow-up to a mean of 23.16 at final follow-up. Roy et al 18 suggest a minimal clinically important difference in DASH score to be 10.2. In a research study comparing the alternate approaches of hemitrapeziectomy with a costochondral allograft, LRTI, and hematoma distraction arthroplasty, Park et al 19 reported that all 3 approaches produced similar DASH scores at long-term follow-up. The mean DASH score for LRTI was 19.6, whereas hematoma distraction arthroplasty and costochondral allograft reported mean DASH scores of 23.5 and 19.0, respectively. 19 We found that our cohort presents mean DASH scores at final follow-up that are comparable to these alternate treatment protocols.
Park et al 19 also presented average lateral pinch strength recovery following the aforementioned treatments for TMC arthritis. Hematoma distraction arthroplasty showed the highest mean percent recovery of 76.6%, followed by costochondral allograft at 62.2% and LRTI at 53%. It was found that there was no statistical difference between the lateral pinch strengths of these 3 approaches. Our short- to intermediate-term cohort (Table 1) reported comparable results for pinch strength recovery at 77%. Avisar et al, 15 Heyworth et al,11 and Burton and Pellegrini 8 report on both gross grip and precision pinch strengths following treatment of TMC arthritis. Following a trapeziectomy with a tendon tie-in implant approach, the mean gross grip strength was 11.0 kg. 15 Basal joint interposition arthroplasty and LRTI arthroplasty reported mean gross grip strength of 18.2 kg 11 and 24.4 kg, 8 respectively. Our cohort showed similar results at final follow-up with a mean gross grip strength of 19.9 kg (Table 1). Precision pinch strengths were reported to be 3.3 11 and 2.9 kg 8 at final follow-up. We present similar precision pinch strength results of 3.0 kg at final follow-up (Table 1). Range of motion measurements (Table 2) also returned to normal functional values at 6 months postoperatively when compared with alternate methods of treatment.11,15 Ultimately, our suture suspension technique achieved functional and subjective outcomes at a short-term follow-up while also avoiding the potential complications of donor site morbidity.8,11,14,15,19
Trapeziectomy, LRTI, and capsular interposition arthroplasty have all shown satisfactory outcomes bar a high incidence of subsidence.20-22 However, previous literature also reports an inverse correlation between TMC subsidence, loss of trapezial height, and clinical outcomes following surgical treatment of basal joint arthritis.20,22,23 Therefore, our study aimed to understand the relationship between the degree of subsidence and functional outcomes following a suture suspension arthroplasty approach. We also wished to determine whether our relationships between subsidence and clinical outcomes are consistent with those of alternate arthroplasty techniques. As a way to evaluate this relationship, we performed a Spearman correlation test between the percent subsidence and TaM of the thumb, percent strength recovery, and DASH scores. Our reported subsidence was comparable to that of other results published in the scientific literature.22,24-26 The results of our Spearman correlation test demonstrate no correlation between grip strength or pain scores and subsidence (Figure 3). However, the results did show a small, albeit nonsignificant, positive correlation between TaM of the thumb and subsidence (Figure 3). This suggests that the TMC subsidence, following our modified suture suspension arthroplasty technique, does not correlate to short- to intermediate-term clinical outcomes or patient satisfaction. Although our results show no correlation, we would like to point out that the Spearman correlation test is limited by small sample sizes, and the correlation between subsidence and functionality should continue to be evaluated and compared with other techniques.
This study is not without limitations. One limitation is that it is a retrospective study with only results being compared with that of the current literature, rather than a comparison with a control group. Additional prospective studies, comparing our study’s surgical technique with other popular treatment modes including LRTI, are necessary. Although the current study effectively demonstrated short- to intermediate-term results of suture suspension arthroplasty, additional studies with long-term follow-up and larger sample size would certainly add to the validity of these results. Another major limitation of this study is the loss of patients after a particular follow-up period, limiting data collection at longer follow-up intervals. Although we can postulate that patients are satisfied with the outcome and feel they no longer need treatment, it does limit the completeness of our database.
Conclusions
Although the search for the superior procedure continues, we can conclude that suture suspension arthroplasty results in satisfactory functional outcomes, sufficiently short immobilization times, and a low rate of complication. We also demonstrate that this procedure can be accomplished with a modified incision that avoids the sensory branches of the radial nerve, and that subsidence of the first metacarpal has less of an effect on outcomes than previously believed. However, further long-term, prospective analysis is needed to confirm the relationship between subsidence and function.
Acknowledgments
The authors thank Patricia A. Meyer, MOT, OTR/L, CHT, and Kristen Kaplan, MSOT, OTR/L, for exceptional occupational therapy work and postoperative evaluations as well as essential proofreading and revision efforts and Danielle Vitale for her assistance in the early stages of the manuscript.
Footnotes
Ethical Approval: This study is exempt from institutional review board approval.
Statement of Human and Animal Rights: All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Statement of Informed Consent: Informed consent was obtained from all participants of the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ather Mirza  https://orcid.org/0000-0002-3406-0699
https://orcid.org/0000-0002-3406-0699
References
- 1. Van Heest AE, Kallemeier P. Thumb carpal metacarpal arthritis. J Am Acad Orthop Surg. 2008;16:140-151. [DOI] [PubMed] [Google Scholar]
- 2. Gillis J, Calder K. Review of thumb carpometacarpal arthritis classification, treatment and outcomes. Can J Plast Surg. 2011;19(4, Winter):134-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Br. 1994;19:340-341. [DOI] [PubMed] [Google Scholar]
- 4. Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55:1655-1666. [PubMed] [Google Scholar]
- 5. Eaton RG, Glickel SZ. Trapeziometacarpal osteoarthritis: staging as a rationale for treatment. Hand Clin. 1987;3:455-471. [PubMed] [Google Scholar]
- 6. Fitzgerald BT, Hofmeister EP. Treatment of advanced carpometacarpal joint disease: trapeziectomy and hematoma arthroplasty. Hand Clin. 2008;24(3):271-276. [DOI] [PubMed] [Google Scholar]
- 7. Kokkalis ZT, Zanaros G, Weiser RW, et al. Trapezium resection with suspension and interposition arthroplasty using acellular dermal allograft for thumb carpometacarpal arthritis. J Hand Surg Am. 2009;34:1029-1036. [DOI] [PubMed] [Google Scholar]
- 8. Burton RI, Pellegrini VD., Jr. Surgical management of basal joint arthritis of the thumbpart II: ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11:324-332. [DOI] [PubMed] [Google Scholar]
- 9. Weilby A. Tendon interposition arthroplasty of the first carpometacarpal joint. J Hand Surg Am. 1988;13:421-425. [DOI] [PubMed] [Google Scholar]
- 10. Lanzetta M, Foucher G. A comparison of different surgical techniques in treating degenerative arthrosis of the CMC joint of the thumb. J Hand Surg Am. 1995;20:105-110. [DOI] [PubMed] [Google Scholar]
- 11. Heyworth BE, Jobin CM, Monica JT, et al. Long-term follow-up of basal joint resection arthroplasty of the thumb with transfer of the abductor pollicis brevis origin to the flexor carpi radialis tendon. J Hand Surg Am. 2009;34(6):1021-1028. [DOI] [PubMed] [Google Scholar]
- 12. Del Signore JL, Accardi KZ. Suture suspension arthroplasty technique for basal joint arthritis reconstruction. Tech Hand Up Extrem Surg. 2009;13:166-172. [DOI] [PubMed] [Google Scholar]
- 13. Kadiyala RK, Gelberman RH, Kwon B. Radiographic assessment of the trapezial space before and after ligament reconstruction and tendon interposition arthroplasty. J Hand Surg Br. 1996;21:177-181. [DOI] [PubMed] [Google Scholar]
- 14. Gervis WH. Excision of trapezium for osteoarthritis of the trapezio-metacarpal joint. J Bone Joint Surg Br. 1949;31B:537-539. [PubMed] [Google Scholar]
- 15. Avisar E, Elvey M, Tzang C, et al. Trapeziectomy with a tendon tie-in implant for osteoarthritis of the trapeziometacarpal Joint. J Hand Surg Am. 2015;40(7):1292-1297. [DOI] [PubMed] [Google Scholar]
- 16. Florez GB, Rubio F. Carpometacarpal hemiarthroplasty. Open Access J Surg. 2017;5(4):555668. [Google Scholar]
- 17. Minami A, Iwasaki N, Kutsumi K, et al. A long-term follow-up of silicone-rubber interposition arthroplasty for osteoarthritis of the thumb metacarpal joint. J Hand Surg. 2005;10(1):77-82. [DOI] [PubMed] [Google Scholar]
- 18. Roy J-S, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009;61(5):623-632. [DOI] [PubMed] [Google Scholar]
- 19. Park MJ, Lichtman G, Christian JB, et al. Surgical treatment of thumb carpometacarpal joint arthritis: a single institution experience from 1995-2005. Hand. 2008;3(4):304-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Trumble T, Rafijah G, Heaton D. Thumb carpometacarpal arthroplasty with ligament reconstruction and interposition costochondral arthroplasty. J Wrist Surg. 2013;2(3):220-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yang SS, Weiland AJ. First metacarpal subsidence during pinch after ligament reconstruction and tendon interposition basal joint arthroplasty of the thumb. J Hand Surg Am. 1998;23(5):879-883. [DOI] [PubMed] [Google Scholar]
- 22. Salas C, Mercer DM, O’Mahony G, et al. Thumb metacarpal subsidence after partial trapeziectomy with capsular interposition arthroplasty: a biomechanical study. Hand. 2016;11(4):444-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Putnam MD, Rattay R, Wentorf F. Biomechanical test of three methods to treat thumb CMC arthritis. J Wrist Surg. 2014;3(2):107-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tomaino MM, Pellegrini VD, Jr, Burton RI. Arthroplasty of the basal joint of the thumb: long-term follow-up after ligament reconstruction with tendon interposition. J Bone Joint Surg Am. 1995;77:346-355. [DOI] [PubMed] [Google Scholar]
- 25. Gray KY, Meals RA. Hematoma distraction arthroplasty for thumb basal joint osteoarthritis: minimum 6.5 yr follow-up evaluation. J Hand Surg Am. 2007;32:23-29. [DOI] [PubMed] [Google Scholar]
- 26. Yang Y, Tien HY, Kumar KK, et al. Ligament reconstruction with tendon interposition arthroplasty for first carpometacarpal joint osteoarthritis. Chin Med J. 2014;127(22):3921-3925. [PubMed] [Google Scholar]


