Abstract
Background:
Androgenetic alopecia (AGA) is a common stressful form of hair loss caused by androgen excess, genetic factors, and exposure to oxidative stress (OS) with the formation of reactive oxygen species (ROS). Paraoxonase 1 (PON1) is an enzyme synthesized in the liver bound to high-density lipoproteins to prevent lipid peroxidation.
Aim:
The aim of our work is to estimate serum PON1 level in patients with AGA and correlate its levels with disease severity which may help in determining if there is a role of ROS in pathogenesis of AGA.
Subjects and Methods:
This study was carried out as a case and control on 40 patients with AGA (diagnosed by typical clinical and dermoscopic finding) versus 40 control subjects. Blood samples were taken from all subjects to assess serum PON1enzyme using enzyme-linked immunosorbent assay kits.
Results:
There was a significant decrease in serum PON1 concentration level in AGA patients in comparison to controls, in addition, there was a significant decrease correlated with AGA severity (P < 0,001). The study proved that PON1 is considered highly sensitive and specific for AGA cases and a good predictive factor of AGA in healthy subjects.
Conclusion:
This is the first study done to reveal that the level of PON1 significantly decreased in AGA patients, which may give additional proof that OS has role in the pathogenesis of AGA and hence may help in the management of AGA by adding antioxidants in treatment.
Key words: Androgenetic alopecia, antioxidants, oxidative stress, paraoxonase 1, reactive oxygen species
INTRODUCTION
Androgenetic alopecia (AGA) is a common form of hair loss occurring in 80% of men and 50% of women.[1] It is experienced as a moderately stressful condition that diminishes body image satisfaction.[2] It is characterized by a progressive reduction in the diameter, length, and pigmentation of hair due to androgen excess, genetic factors, and exposure to oxidative stress (OS) with the formation of reactive oxygen species (ROS).[3] It is thought that lipid peroxidation, glutathione derivatives, and nitric oxide are indicators of cellular destruction by ROS.[4]
Inflammation is suggested to be a feature in AGA, evidenced by the presence of activated T-cells infiltrating the lower portions of follicular infundibula, with concentric layers of perifollicular collagen deposition, in 40% of cases of AGA versus 10% of normal controls.[5] A considerable difference in the inflammatory infiltrate has been observed between balding and nonbalding scalp.[6]
Paraoxonase 1 (PON1) is a member of a family of proteins that also includes PON2 and PON3.[7] It is an enzyme synthesized in the liver and has lactonase and esterase activities toward lipid peroxides and circulates in plasma bound to high-density lipoproteins (HDL).[8] HDL-associated PON1 has been frequently shown to have antioxidant and anti-inflammatory potential mainly by protecting lipids of HDLs and low-density lipoproteins from oxidative modifications.[9,10]
In the skin, reduction in PON1 level in vitiligo patients revealed their role in ROS pathogenesis and the diminution of PON1 activity in OS.[11] Lower PON1 activity was also observed in the sera of psoriasis patients compared with healthy subjects, confirming that psoriasis is associated with OS, and impairment of the antioxidant system in the plasma of patients may play a role in pathogenesis and progression of psoriasis and related complications.[12]
In Alopecia areata (AA), there is a proved alteration in oxygen-free radical scavenging process manifested by decreases in lymphocytes and plasma total antioxidant status and erythrocytes GSH.[13] PON1 activity was found to be lowered in patient with AA, which may be related to an increase in oxidant and a decrease in antioxidant levels.[14]
The aim of our work is to estimate serum PON1 level in patients with AGA and correlate its levels with disease severity, which may help in determining if there is a role of ROS in the pathogenesis of AGA, and consequently, could help in the management of AGA by adding antioxidants in the treatment protocols.
SUBJECTS AND METHODS
This research work was designed as a case–control study at the outpatient clinic of Dermatology Department of Mansoura University Hospital, Mansoura, Egypt, during the period from December 2018 to June 2019. The study was approved by Institutional Research Board with approval code “MS.18.05.128.”
Subjects
The subjects were classified into two groups, Group I included 40 patients complaining of AGA, and Group II, that included 40 apparently healthy age- and sex-matched controls. All patients were below 50 years (as investigations reported a progressive decrease in PON1 activity in elderly subjects).[15] Patients included in the study were those with AGA who didnot use topical treatment or stopped it for at least 3 months before being enrolled. . Patients were excluded as follows: patients using systemic treatment such as steroids and immunosuppressive drugs that likely can cause regrowth of hair within the past 3 months, those with associated diseases that alter serum PON1 level as vitiligo, psoriasis, thyroid, liver, renal, cardiovascular diseases, diabetes, and other conditions that affect PON1 level as pregnancy, smoking, alcoholism, obesity.
A written informed consent was taken from all participants before the study. Full history taking includes personal history, history of present illness, previous medications, and the date of discontinuation, if any. Family history of AGA or other skin or systemic disease was recorded. General examination was done to exclude systemic diseases associated with hair loss. Clinical assessment of the degree of AGA according to Hamilton classification for clinical assessment of male pattern hair loss [Figure 1][16] and Ludwig classification for clinical assessment of female pattern hair loss [Figure 2].[17] Full dermoscopic examination using Dermlite 3 (3 Gen, USA) and the characteristic trichoscopic features of AGA were evaluated.
Figure 1.
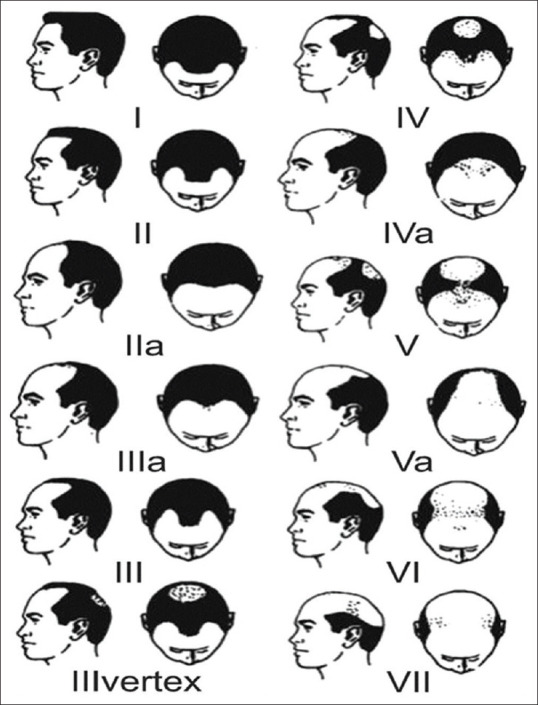
Hamilton–Norwood classification of male pattern hair loss 16
Figure 2.
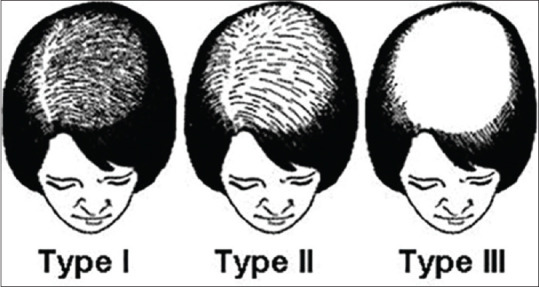
Ludwig classification of hair loss among females 17
Methods
Collection of blood samples
Five milliter of fasting (6–8 h) venous blood were collected from each subject participating in this study. Determination of serum (PON1) had been carried out using enzyme-linked immunosorbent assay kits supplied from Wuhan EIAab science CO., Ltd., with catalog no: E0243 h.
Data management and statistical analysis
The Statistical Package for the Social Science (Chicago: SPSS Inc) program version 17 was used for analysis of data. The data were summarized using descriptive statistics: mean, median, standard deviation (SD), minimal, and maximum values for quantitative variables and number and percentage for qualitative values. Statistical differences between groups were tested using Chi-square test for qualitative variables, independent sample t-test, and analysis of variance test for quantitative normally distributed variables. Simple linear correlation for quantitative data was also done. Value was considered weak if < 0.25, mild if >0.25−<0.5, moderate if >0.5−<0.75, and strong if >0.75.
RESULTS
Sociodemographic data
The present study was conducted on 40 cases with AGA, their mean age 34.2 years, they were 20 males (50%) and 20 females (50%) in addition to 40 healthy controls of matched age and gender. No significant differences were found in occupation between cases (data not shown).
Clinical assessment of androgenetic alopecia cases
AGA severity was assessed in all studied cases; 40% were mild, 37.5% were moderate, and 22.5% were severe cases. Mild cases included Grade I (according to Ludwig classification) and Grades I, II, III (according to Hamilton classification). Moderate cases included Grade II (according to Ludwig classification) and Grades IV and V (according to Hamilton classification). Severe cases included Grade III (according to Ludwig classification) and Grades VI and VII (according to Hamilton classification).
Comparison Paraoxonase 1 concentration between all studied groups
AGA cases showed significantly lower PON1 concentration when compared to control group (mean ± SD = 106.6 ± 31.5 versus 299.7 ± 71.9, respectively; P < 0.001) [Figure 3].
Figure 3.
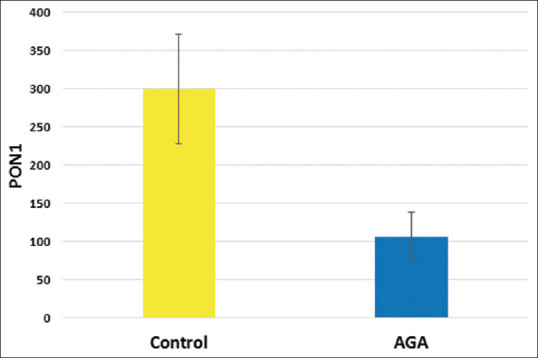
Paraoxonase 1 concentration in all studied groups
Receiver operating characteristic curve of serum PON1 was conducted for discrimination between AGA cases and control groups. Excellent area under curve (AUC) was found (AUC = 0.974, P < 0.001). At cutoff value of 191, sensitivity was 92.5%, specificity was 100%, positive predicted value (PPV) was 100%, negative predicted value (NPV) was 87%, and accuracy was 95% [Figure 4].
Figure 4.
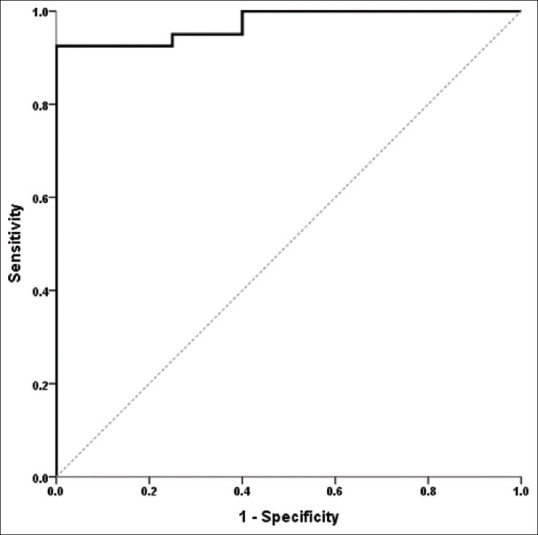
Receiver operating characteristic curve of serum Paraoxonase 1 for discrimination between androgenetic alopecia cases and control group.
No significant differences were found in PON1 level between gender, FH, onset in all AGA cases [Table 1]. Comparison of PON1 level between severity grades in all AGA cases showed that significantly lower PON1 level was associated with more severe grades in AGA patients [Table 2]. Using Pearson's correlation, PON1 showed significant negative correlation with severity (r = −0.541, P < 0.001). Otherwise, no significant correlations were found between PON1 level with other studied parameters in AGA cases (P > 0.05 for each) [Table 3].
Table 1.
Comparison of paraoxonase level between gender, family history, disease onset in all androgenetic alopecia cases
| PON1 level, mean±SD | P | |
|---|---|---|
| Gender | ||
| Male | 109.7±32.5 | 0.750 |
| Female | 103.4±29.6 | |
| FH | ||
| Negative FH | 114.3±32.9 | 0.435 |
| Positive FH | 98.9±27.9 | |
| Onset | ||
| Sudden onset | 105.1±32.3 | 0.905 |
| Gradual onset | 107.5±31.5 |
t-test. FH – Family history; PON1 – Paraoxonase; SD – Standard deviation
Table 2.
Comparison of paraoxonase level between severity grades in all androgenetic alopecia cases
| PON1 level, mean±SD | P | |
|---|---|---|
| Mild | 146±34.7 | 0.001 |
| Moderate | 90±25.7 | |
| Severe | 64.2±21.9 |
ANOVA test. ANOVA – Analysis of variance; PON1 – Paraoxonase; SD – Standard deviation
Table 3.
Correlation of paraoxonase level with other studied parameters in all androgenetic alopecia cases
| PON1 |
||
|---|---|---|
| r | P | |
| Age (years) | 0.065 | 0.692 |
| Gender | −0.052 | 0.750 |
| FH | −0.127 | 0.435 |
| Duration (years) | −0.127 | 0.436 |
| Onset | 0.020 | 0.905 |
| Severity | −0.541 | <0.001 |
Pearson’s correlation was used. r – Pearson’s correlation coefficient; FH – Family history; PON1 – Paraoxonase
Prediction of androgenetic alopecia development and severity within healthy subjects
Logistic regression analysis was conducted for the prediction of AGA development within healthy subjects, using age, gender, and PON1 as covariates. Low PON1 level was considered as independent risk factor for the development of AGA [Table 4]. Ordinal regression analysis was conducted for the prediction of severity of AGA cases using age, gender, clinical data, and PON1 as covariates. Lower PON1 was the only predictor for higher severity in studied AGA patients [Table 5].
Table 4.
Logistic regression analysis for prediction of androgenetic alopecia development within healthy subjects
| P | OR | 95% CI | |
|---|---|---|---|
| Age (years) | 0.983 | 0.999 | 0.938-1.064 |
| Gender | 0.070 | 0.333 | 0.102-1.092 |
| PON1 | <0.001 | 0.969 | 0.954-0.985 |
OR – Odds ratio; CI – Confidence interval; PON1 – Paraoxonase
Table 5.
Prediction of severity of androgenetic alopecia cases
| P | OR | 95% CI | |
|---|---|---|---|
| Age (years) | 0.873 | 0.997 | 0.956-1.039 |
| Gender | 0.513 | 1.263 | 0.628-2.538 |
| Duration | 0.966 | 0.989 | 0.593-1.651 |
| Onset | 0.260 | 0.662 | 0.322-1.358 |
| PON1 | 0.001 | 0.982 | 0.971-0.992 |
OR – Odds ratio; CI – Confidence interval; PON1 – Paraoxonase
DISCUSSION
Being a widespread psychologically distressing disease,[1,2] AGA pathogenesis has been the focus of different studies in the past years.[3,4,5,6] The involvement of genetic, hormonal factors (androgens),[18] in addition to inflammation,[5,6] was suggested. Histological studies confirmed the presence of perifollicular inflammation in the upper third[5,6] together with OS in dermal papilla of the hair follicles the patients with AGA.[3,6]
PON1 is an HDL-associated antioxidant enzyme capable of hydrolyzing lipid peroxides.[19] Previous studies have shown that the activity of PON1 in human serum is downregulated by OS.[20,21] The current study was conducted to detect serum PON1 level in patients with AGA and correlate it with disease severity which may help to determine if there is a role of ROS in pathogenesis of AGA.
Several research groups have studied the relationship between OS and AGA. Prie et al. conducted a study to measure the several enzymes and products of OS in the blood of patients with AGA. They found a significantly decreased (P < 0.01) superoxide dismutase activity in patients with AGA compared to controls.[22] Another study by Kaya Erdogan et al. measured total oxidant levels (TOS), total antioxidant levels (TAS), and oxidative stress index (OSI). They found that TOS and OSI were significantly higher in patient group, but when TAS, TOS, and OSI levels were assessed according to AGA stage, there was no significant difference between groups.[23]
To the best of our knowledge, the relationship between serum PON1 and disease activity in AGA subjects has not been studied or published before. This explains that there are no previously reported results, in literature, to compare with our findings. Although it had been studied in other forms of hair loss, such as AA,[14,24]
Regarding the prevalence and severity of AGA among the different age groups, different results have been reported, particularly in males. The present study was conducted on 40 cases with AGA, their mean age 34.2 years, they were 20 males (50%) and 20 females (50%) versus 40 healthy control group of matched age and gender. There is no statistically significant difference between the two groups in this respect.
First, according to Hamilton's study in 1951, by the age of 30, the mean prevalence was 30%, 40% in mid-forties, and this rate rose to 50% by the age of 50 in Caucasian men.[25] In a recent study from Turkey, these rates were, respectively, 71.1%, 77.2%, and 83.3%.[26] In studies from US, Italy, Norway, and Australia, similar results to Hamilton's study were reported.[27,28,29,30] Birch et al. reported that the prevalence of female type AGA in women younger than 50 years was 6%, whereas in women older than 50 years was 52.6% in England.[31] Paik et al. found that the prevalence of AGA in Korea was 14.1% in men and 5.6% in women.[32]
We found that half of patients with AGA had positive family history, all patients had history of stress. None of them was smoker, had systemic disease, or received medications. AGA severity was assessed in all studied cases; 40% were mild, 37.5% were moderate, and 22.5% were severe cases. This came in agreement with Paik et al. who showed that among patients with AGA included in his study, 50% had a family history of AGA.[32] In the study conducted by Kaya Erdogan et al., family history in AGA was present in 66.7% (22 of 33 patients), and the Hamilton–Norwood scale was Stage 3 in 72.7% of patients and Stage 4 in 27.3%.[23]
In our study, the mean level of PON1 in the cases with AGA was statistically significant lower as compared with the control group. Furthermore, a significantly lower PON1 level was associated with more severe grades of AGA. Interestingly, the best cutoff of PON1 to differentiate between AGA and control was 191, with a sensitivity of 92.5%, specificity 100%, PPV was 100%, NPV was 87%, and accuracy was 95%, i.e. PON1 can be used as a predictor of AGA in the healthy.
In the study conducted by Bilgili et al., to investigate serum PON1 activity and oxidative status in subjects with AA, they showed that PON1 activity was significantly lower in the subjects with AA than controls (P = 0.001).[14] Dizen-Namdar et al. included 60 AA and 50 healthy control subjects to test serum PON1 in cases with AA. They showed that serum PON1 activities were significantly lower in the patients with AA compared to the control group (P < 0.001).[24] Putting in consideration that studies on the role of OS in AA have been preceding those carried out on AGA,[33,34] it might be worthy to study, in depth, the role of OS in AGA, and hence, predict similar changes.
CONCLUSION
This study is considered the first to investigate the PON1 enzyme level in subjects with AGA, our results revealed that the level of PON1 decreased significantly in most of cases with significant decrease in severe grades, and this may prove that OS is considered one of the aggravating factors of AGA, which in turn may help in the management of AGA by adding antioxidants in treatment.
Some limitations were encountered in this study, being a single-center study with a relatively small sample size. Furthermore, the study assessed the enzyme level in sera of AGA patients but not from tissue samples.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Vary JC., Jr Selected disorders of skin appendages-Acne, alopecia, hyperhidrosis. Med Clin North Am. 2015;99:1195–211. doi: 10.1016/j.mcna.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Cash TF. The psychosocial consequences of androgenetic alopecia: A review of the research literature. Br J Dermatol. 1999;141:398–405. doi: 10.1046/j.1365-2133.1999.03030.x. [DOI] [PubMed] [Google Scholar]
- 3.Upton JH, Hannen RF, Bahta AW, Farjo N, Farjo B, Philpott MP. Oxidative stress-associated senescence in dermal papilla cells of men with androgenetic alopecia. J Invest Dermatol. 2015;135:1244–52. doi: 10.1038/jid.2015.28. [DOI] [PubMed] [Google Scholar]
- 4.Giralt M, Cervello I, Nogues MR, Puerto AM, Ortin F, Argany N, et al. Glutathione, glutathione S-transferase and reactive oxygen species of human scalp sebaceous glands in male pattern baldness. J Invest Dermatol. 1996;107:154–8. doi: 10.1111/1523-1747.ep12329551. [DOI] [PubMed] [Google Scholar]
- 5.Aslani FS, Dastgheib L, Banihashemi BM. Hair counts in scalp biopsy of males and females with androgenetic alopecia compared with normal subjects. J Cutan Pathol. 2009;36:734–9. doi: 10.1111/j.1600-0560.2008.01149.x. [DOI] [PubMed] [Google Scholar]
- 6.Magro CM, Rossi A, Poe J, Manhas-Bhutani S, Sadick N. The role of inflammation and immunity in the pathogenesis of androgenetic alopecia. J Drugs Dermatol. 2011;10:1404–11. [PubMed] [Google Scholar]
- 7.Primo-Parmo SL, Sorenson RC, Teiber J, La Du BN. The human serum paraoxonase/arylesterase gene (PON1) is one member of a multigene family. Genomics. 1996;33:498–507. doi: 10.1006/geno.1996.0225. [DOI] [PubMed] [Google Scholar]
- 8.Mackness MI. Possible medical significance of human serum paraoxonase. In: Reiner E, Aldridge WN, Hoskin FCG, editors. Enzymes Hydrolyzing Organophosphorus Compounds. Chichester, UK: Ellis-Horwood; 1989. pp. 202–13. [Google Scholar]
- 9.Mackness MI, Arrol S, Durrington PN. Paraoxonase prevents accumulation of lipoperoxides in low-density lipoprotein. FEBS Lett. 1991;286:152–4. doi: 10.1016/0014-5793(91)80962-3. [DOI] [PubMed] [Google Scholar]
- 10.Aviram M, Rosenblat M, Bisgaier CL, Newton RS, Primo-Parmo SL, La Du BN. Paraoxonase inhibits high-density lipoprotein oxidation and preserves its functions. A possible peroxidative role for paraoxonase. J Clin Invest. 1998;101:1581–90. doi: 10.1172/JCI1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yesilova Y, Turan E, Ucmak D, Selek S, Halil Yavuz İ, Tanrıkulu O. Reduced serum paraoxonase-1 levels in vitiligo: Further evidence of oxidative stress. Redox Rep. 2012;17:214–8. doi: 10.1179/1351000212Y.0000000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferretti G, Bacchetti T, Campanati A, Simonetti O, Liberati G, Offidani A. Correlation between lipoprotein (a) and lipid peroxidation in psoriasis: Role of the enzyme paraoxonase-1. Br J Dermatol. 2012;166:204–7. doi: 10.1111/j.1365-2133.2011.10539.x. [DOI] [PubMed] [Google Scholar]
- 13.Al-Gaff AN, Humadi S, Wohaieb SA, Muhi eldeen AR. Effect of nutrient antioxidants on oxidative stress indicators in patients with alopecia areata. Almustansiriyah J Pharm Sci. 2007;4:110–24. [Google Scholar]
- 14.Bilgili SG, Ozkol H, Karadag AS, Ozkol HU, Seker A, Calka O, et al. Serum paraoxonase activity and oxidative status in subjects with alopecia areata. Cutan Ocul Toxicol. 2013;32:290–3. doi: 10.3109/15569527.2013.781616. [DOI] [PubMed] [Google Scholar]
- 15.Seres I, Paragh G, Deschene E, Fulop T, Jr, Khalil A. Study of factors influencing the decreased HDL associated PON1 activity with aging. Exp Gerontol. 2004;39:59–66. doi: 10.1016/j.exger.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Norwood OT. Male pattern baldness: Classification and incidence. South Med J. 1975;68:1359–65. doi: 10.1097/00007611-197511000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Ludwig E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol. 1977;97:247–54. doi: 10.1111/j.1365-2133.1977.tb15179.x. [DOI] [PubMed] [Google Scholar]
- 18.Torres F. Androgenetic, diffuse and senescent alopecia in men: Practical evaluation and management. Curr Probl Dermatol. 2015;47:33–44. doi: 10.1159/000369403. [DOI] [PubMed] [Google Scholar]
- 19.Rosenblat M, Gaidukov L, Khersonsky O, Vaya J, Oren R, Tawfik DS, et al. The catalytic histidine dyad of high density lipoprotein-associated serum paraoxonase-1 (PON1) is essential for PON1-mediated inhibition of low density lipoprotein oxidation and stimulation of macrophage cholesterol efflux. J Biol Chem. 2006;281:7657–65. doi: 10.1074/jbc.M512595200. [DOI] [PubMed] [Google Scholar]
- 20.Aslan M, Kosecik M, Horoz M, Selek S, Celik H, Erel O. Assessment of paraoxonase and arylesterase activities in patients with iron deficiency anemia. Atherosclerosis. 2007;191:397–402. doi: 10.1016/j.atherosclerosis.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Kotur-Stevuljevic J, Bogavac-Stanojevic N, Jelic-Ivanovic Z, Stefanovic A, Gojkovic T, Joksic J, et al. Oxidative stress and paraoxonase 1 status in acute ischemic stroke patients. Atherosclerosis. 2015;241:192–8. doi: 10.1016/j.atherosclerosis.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 22.Prie BE, Iosif L, Tivig I, Stoian I, Giurcaneanu C. Oxidative stress in androgenetic alopecia. J Med Life. 2016;9:79–83. [PMC free article] [PubMed] [Google Scholar]
- 23.Kaya Erdogan H, Bulur I, Kocaturk E, Yildiz B, Saracoglu ZN, Alatas O. The role of oxidative stress in early-onset androgenetic alopecia. J Cosmet Dermatol. 2017;16:527–30. doi: 10.1111/jocd.12300. [DOI] [PubMed] [Google Scholar]
- 24.Dizen-Namdar N, Emel Kocak F, Kidir M, Sarici G, Tak H, Altuntas I. Evaluation of serum paraoxonase, arylesterase, prolidase activities and oxidative stress in patients with alopecia areata. Skin Pharmacol Physiol. 2019;32:59–64. doi: 10.1159/000494690. [DOI] [PubMed] [Google Scholar]
- 25.Hamilton JB. Patterned loss of hair in man; types and incidence. Ann N Y Acad Sci. 1951;53:708–28. doi: 10.1111/j.1749-6632.1951.tb31971.x. [DOI] [PubMed] [Google Scholar]
- 26.Salman KE, Altunay IK, Kucukunal NA, Cerman AA. Frequency, severity and related factors of androgenetic alopecia in dermatology outpatient clinic: Hospital-based cross-sectional study in Turkey. An Bras Dermatol. 2017;92:35–40. doi: 10.1590/abd1806-4841.20175241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhodes T, Girman CJ, Savin RC, Kaufman KD, Guo S, Lilly FR, et al. Prevalence of male pattern hair loss in 18-49 year old men. Dermatol Surg. 1998;24:1330–2. doi: 10.1111/j.1524-4725.1998.tb00009.x. [DOI] [PubMed] [Google Scholar]
- 28.DeMuro-Mercon C, Rhodes T, Girman CJ, Vatten L. Male-pattern hair loss in Norwegian men: A community-based study. Dermatology. 2000;200:219–22. doi: 10.1159/000018386. [DOI] [PubMed] [Google Scholar]
- 29.Gan DC, Sinclair RD. Prevalence of male and female pattern hair loss in Maryborough. J Investig Dermatol Symp Proc. 2005;10:184–9. doi: 10.1111/j.1087-0024.2005.10102.x. [DOI] [PubMed] [Google Scholar]
- 30.Otberg N, Finner AM, Shapiro J. Androgenetic alopecia. Endocrinol Metab Clin North Am. 2007;36:379–98. doi: 10.1016/j.ecl.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Birch MP, Messenger JF, Messenger AG. Hair density, hair diameter and the prevalence of female pattern hair loss. Br J Dermatol. 2001;144:297–304. doi: 10.1046/j.1365-2133.2001.04018.x. [DOI] [PubMed] [Google Scholar]
- 32.Paik JH, Yoon JB, Sim WY, Kim BS, Kim NI. The prevalence and types of androgenetic alopecia in Korean men and women. Br J Dermatol. 2001;145:95–9. doi: 10.1046/j.1365-2133.2001.04289.x. [DOI] [PubMed] [Google Scholar]
- 33.Naziroglu M, Kokcam I. Antioxidants and lipid peroxidation status in the blood of patients with alopecia. Cell Biochem Funct. 2000;18:169–73. doi: 10.1002/1099-0844(200009)18:3<169::AID-CBF870>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 34.Akar A, Arca E, Erbil H, Akay C, Sayal A, Gür AR. Antioxidant enzymes and lipid peroxidation in the scalp of patients with alopecia areata. J Dermatol Sci. 2002;29:85–90. doi: 10.1016/s0923-1811(02)00015-4. [DOI] [PubMed] [Google Scholar]


