Abstract
Background
Hand hygiene (HH) is a cost-effective measure to reduce health care-associated infections. The overall characteristics and changes of hand hygiene compliance (HHC) among health care providers during the COVID-19 pandemic provided evidence for targeted HH intervention measures.
Aim
To systematically review the literature and conduct a meta-analysis of studies investigating the rate of HHC and the characteristics of HH during the COVID-19 pandemic.
Methods
The PubMed, Embase, Cochrane Library, Web of Science, CNKI, WanFang Data, VIP, and CBM databases were searched. All the original articles with valid HHC data among health care providers during the COVID-19 pandemic (from January 1, 2020 to October 1, 2021) were included. Meta-analysis was performed using a DerSimonian and Laird model to yield a point estimate and a 95% CI for the HHC rate. The heterogeneity of the studies was evaluated using the Cochrane Q test and I2 statistics and a random-effects model was used to contrast between different occupations, the WHO 5-moments of HH and different observation methods. Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines were followed.
Findings
Seven studies with 2,377 health care providers reporting HHC were identified. The estimated overall HHC was 74%, which was higher than that reported in previous studies (5%-89%). Fever clinic has become a new key place for HHC observation. Nurses had the highest HHC (80%; 95% CI:74%-87%) while auxiliary workers (70%; 95%CI:62%-77%) had the lowest. For the WHO 5-moments, the health care providers had the highest HHC after contact with the body fluids of the patients (91%; 95% CI:88%-94%), while before contact with patient's health care providers had the lowest HHC (68%; 95% CI:62%-74%) which was consistent with before the pandemic. There existed great HHC differences among different monitoring methods (automatic monitoring system:53%; 95% CI:44%-63% versus openly and secretly observation: 91%; 95% CI: 90%-91%).
Conclusions
During the COVID-19 pandemic, the compliance of health care providers’ HH showed a great improvement. The fever clinics have become the focused departments for HH monitoring. The HHC of auxiliary workers and the HH opportunity for “before contact with patients” should be strengthened. In the future, it will be necessary to develop standardized HH monitoring tools for practical work.
Keywords: Hand hygiene improvement, Hand hygiene compliance, Health care-associated infection control, COVID-19, Review
Introduction
Health care-associated infections (HAIs) have had a negative impact on insurers and health systems globally due to prolonged hospitalization days, as well as increased hospitalization expenses, disease burdens, and waste of health resources.1 , 2 The additional total medical expenditure per HAI-Antimicrobial resistance inpatient was US$15,557.25 compared with that of the non-HAIs, and the additional length of per hospital stay of the HAI-Antimicrobial resistance inpatient was 41 days compared with that of the non-HAIs in China.3 It has been well established that hand hygiene (HH) is a cost-effective measure to reduce HAIs.4 A 3 year observational study showed a 10% improvement in HH associated with a 6% reduction in overall HAIs.5 During the COVID-19 pandemic, poor HH has been shown to increase transmission.6, 7 In a laboratory experiment SARS-CoV-2 was found to be stable on the skin up to 14 days at 4°C, 96 hours at 22°C and for at least 8 hours at 37°C.8 A designated hospital in Wuhan showed that the most SARS-CoV-2 contaminated objects were the self-service printers (20.0%), desktop/keyboard (16.8%), and doorknobs (16.0%) that were touched frequently by the hands of health care providers.9, 10 Especially in the moments including after contact with patients infected or doffing personal protective equipment, the contaminated hand not only lead to transmission pathogenic microorganisms but increased the risk of occupational exposure. An observational study conducted in an intensive care unit (ICU) found that 36% of the health care providers were contaminated with the target multidrug resistant organisms after patient interactions, including 4 (3.2%) on hands and 38 (30.4%) on the personal protective equipments.11 , 12 Effective HH is not only a key measure for preventing the spread of SARS-CoV-2 and for safe COVID-19 vaccinations, but it also reduces the burden of HAIs and the spread of antimicrobial resistance.
It is notable that there is a gap between the knowledge of HH and HH compliance (HHC) among health care providers.13, 14, 15 Previous studies have documented that the compliance of HH was affected by many factors, such as heavy workloads,16 interruption by other things,17 forgetting to wash hands, shortages of HH facilities,18 and intolerance to the hand skin disinfectant19 caused by frequent HH. From the front-line experience, during the outbreak of COVID-19, hospitals strengthened intervention measures for the HHC among health care providers, including strengthening education, increasing monitoring frequency, posting notices and warning signs, and other measures.20 , 21 In addition, health care providers may have had a higher self-awareness of and ability to perform HH compared with other daily working conditions in during the contingency status of COVID-19. However, it is not known whether HH behavior and compliance among health care providers changed and what kind of changes may have taken place after the outbreak.22
Therefore, the aim of this study was to evaluate the overall HHC rate and characteristics of HHC during the COVID-19 pandemic and conduct in-depth comparison with the situation before the epidemic so as to make evidence-based suggestions to improve the HHC in the future.
Methods
This meta-analysis was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) checklist.23 We developed a protocol and used systematic methods to identify relevant studies, screen study eligibility and assess the quality.
Literature search strategy
A comprehensive systematic literature search was conducted on October 1, 2021 without restrictions on region, publication type or language. We searched the PubMed, Embase, the Cochrane Library, Web of Science, CNKI, WanFang Data, VIP and CBM databases (covering the study period from January 1, 2020 to October 1, 2021) using the terms provided in Frame 1 (Supplementary Figure 1). To provide more evidence, we also searched the reference lists of the trials, previous reviews, meta-analyses, and clinical practice guidelines on the same topic. Two reviewers (WY and YJR) selected the relevant articles independently, and in case of any conflicts between the reviewers, they reached a consensus after discussion. Since the only 5 retrieved literatures reported the HHC comparison before and after the pandemic, the comparison data before COVID-19 were referred from the HHC regarded meta-analysis studies published from January 1, 2015 to December 31, 2019.27 , 29 , 33, 34, 35
Inclusion and exclusion criteria
Studies were considered to be eligible for further evaluation if they met the following inclusion criteria: (1) an original article with valid HHC data among health care providers during the COVID-19 pandemic with appropriate observation methods being used to monitor HHC. Appropriate observation methods referred to anonymous observation, openly observation and electronic instrument were used by a third party to monitoring HH practices among health care providers rather than the HH compliance were from the questionnaires observed or evaluated by themselves. The HHC both includes hand wash and alcohol-based hand rub; (2) English or Chinese language; and article types being either randomized controlled trials (RCT), cross-sectional studies, or before-after studies. The exclusion criteria were: inappropriate study design, such as letters, conference abstracts, commentaries, case reports, reviews, etc. with limited data, inaccessible literature, repetitive published papers, the HHC data was obtained from self-report of health care providers and questionnaire survey.
Data extraction
Each study was screened by 2 independent reviewers (WY and YJR) according to the study eligibility criteria and the retrieved data from all the publications meeting the inclusion criteria. The retrieved data were crosschecked to ensure accuracy, and any disagreements were resolved by consensus through discussion. The information extracted included: (1) publication data: name of first author, publication year, geographic location, literature types (randomized clinical trials; cross-sectional study or before-after study), and HH monitoring period; (2) social demographic characteristics of the study population: sample size, age, gender, department, years of work, and whether the hospital/ward was designated for COVID-19; (3) the HH characteristics: HHC rates, actual number of HH actions, and number of HH opportunities; (4) the subgroups divided according to occupation (doctors, nurses, and others), the WHO 5 moments of HH (before touching a patient, before clean/aseptic procedure, after body fluid exposure risk, after touching a patient, and after touching patient surroundings),24 and observation methods (openly, secretly, and automatic HH monitoring system). The 3 researchers (WY, YJR, and LL) extracted the information, and discrepancies were discussed in order to reach a consensus.
Quality assessment
We used the Newcastle-Ottawa quality assessment scale to assess the methodological quality and risk of bias for each included study.24 Studies received as many as 9 points based on participant selection (4 points), study comparability (2 points), and outcome of interest (3 points). Studies were classified as having high (≤3 points), moderate (4-6 points), and low (≥7 points) risk of bias. One of the authors (LL) evaluated study quality. RevMan software was used to perform a sensitivity analysis by excluding one study at a time to validate the stability of the results in our meta-analysis. Subgroup analyses were also performed by occupation, the WHO 5 moments of HH, or observation methods to analyze the sources of potential heterogeneity.
Statistics analysis
The HHC rates were chosen as the primary outcome, which were measured by the HH actions (X) and HH opportunities (N). To implement a non-contrast binary data meta-analysis, the DerSimonian and Laird model was used to yield a point estimate and a 95% CI for HHC rate; the data were processed to give the rate of HHC and standard error (SE): Rate of HHC (P) =X/N × 100%; SE=.25 The heterogeneity of the studies was evaluated using the Cochrane Q test and I2 statistics, which quantified the inconsistencies among the studies. Heterogeneity was considered significant if the P-value was less than .05, and the I2 was greater than 50%. A random-effects model was used for comparisons when heterogeneity was observed; otherwise, a fixed-effects model was used. For comparisons across covariates (ie, occupations, the WHO 5 moments of HH, and observation methods), the study was treated as a random effect. The analyses were performed using the Review Manager software (version 5.4.1, The Cochrane Collaboration, Oxford, UK). Publication bias was assessed using funnel plots. A symmetrical inspection of the inverted funnel was regarded as having no significant publication bias. In contrast, skewed and asymmetrical funnels showed a bias.
Results
Study characteristics
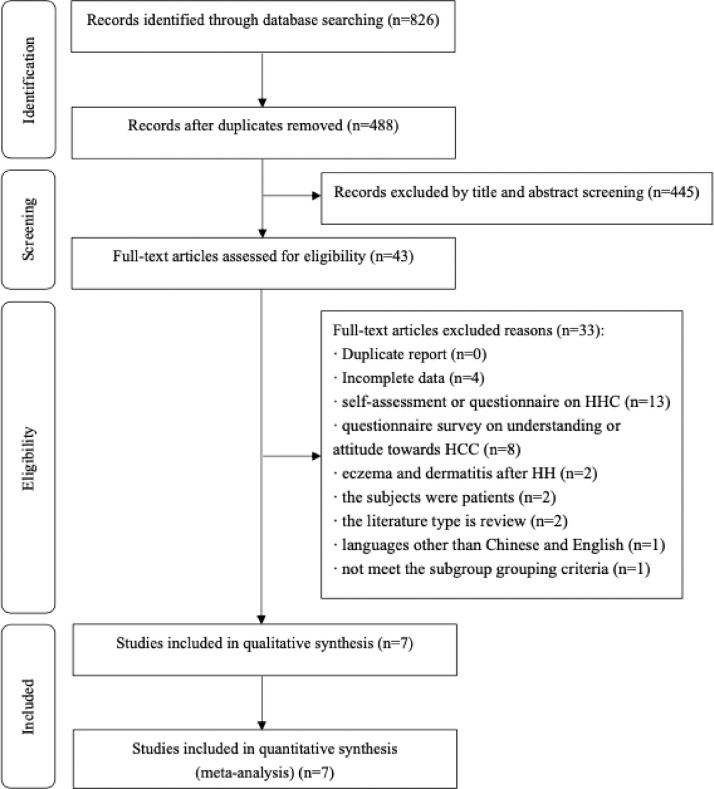
The initial database search obtained 826 unique citations, of which 488 were removed for duplicates. 43 were retrieved based on their title and abstract content. Of the 43 retrieved articles, 4 articles reported incomplete data and 29articles unable to extract outcome data (supplementary materials). Ten eligible studies were identified for the meta-analysis.26, 27, 28, 29, 30, 31, 32, 33, 34, 35 The list of excluded studies and reasons for exclusion are shown in Figure 1 . Among the 10 included studies, 6 studies were carried out in China,26, 27, 28, 29 , 32 , 33 1 in America,30 1 in Germany,31 1 in Italy34 and 1 in India,35 including 3 cross-sectional surveys,27 , 28 , 32 6 before-after studies,29, 30, 31 , 33, 34, 35 and one randomized controlled trial (RCT) study.26 All the studies were conducted between December, 2019 and April, 2021, and the HHC rates ranged from 46% to 100% (Table 1 ).
Fig 1.
Flow chart of study identification.
Table 1.
Basic information of studies
| Study | Country | Article type | Study period | Main conclusions |
|---|---|---|---|---|
| Du Miao 2020 | Beijing, China | Randomized controlled trial | Jan-May,2020 | Under Hawthorne effect, the HHC rate of health care provider in open observation (82.82%) was higher than that in secret observation (71.45%) (P < .05), and it was most obvious among doctors (Hawthorne effect = 16.33). |
| Zhang Xuan 2020 | Shandong, China | Cross-sectional study | Feb,2020 | The overall high HHC rate (81.46%) may be related to the professional training before supporting Wuhan and protection experience of the front line. |
| Zhang Xiangxiang 2020 | Fujian, China | Cross-sectional study | Dec 1,2019-May 31,2020 | The HHC rate of health care provider was significantly higher (90.52%) than that in nonpandemic period (70.67%) (P < .001). |
| Liu Sidi 2020 | Hunan, China | Before-after study | Jan-Aug,2020 | Under the influence of COVID-19, health care providers have a strong sense of self-protection. Before and during pandemic, HHC rate was 71.65% vs 84.16% (P < .001). |
| Moore 2021 | Ohio, USA | Before-after study | Jan 5-Mar 14,2020 (before the school closures); Mar 15-May 17,2020 (after the school closures) |
HHC rates increased from 46% to 56% in the months preceding pandemic-related school closures (P < .001), which was followed by a 6% upward shift at the time school closures occurred. |
| Derksen 2020 | Bremen, German | Before-after study | Jan 1-Jan 28,2020 (pre-COVID-19 pandemic period); Jan 29-Feb 23,2020 (heightened awareness); Feb 24-Mar 15,2020 (strict precautions) |
Facing COVID-19 pandemic, health care providers adapt their HH behavior and the HHC were increased following 3 period: 47% in pre-COVID-19 pandemic period, 79% in heightened awareness period, and 100% in strict precautions period (P < .001). |
| Zhou Qian 2020 | Wuhan, China | Cross-sectional survey | Mar 5- Mar 7, 2020 | HHC rate was highest in HH behavior (96.71%), followed by HH procedure (95.74%), duration (88.93%), and hand drying method (88.42%) (P < .001). |
| Zhao Tingting 2021 | Hangzhou, China | Before-after study | Feb 1,2019-May 31,2019 (pre- COVID-19 period); Feb 1,2020-May 31,2020 (during COVID-19 period) |
The psychological pressure brought by the spread of COVID-19 may promote the HHC rate of doctors and nurses from 75.93% to 81.14% (P < .001) |
| Ragusa 2021 | Catania, Italy | Before-after study | Jan 1,2015-Dec 31,2020 | Compared with the HHC rate of 62% in 2016 and 66% in 2020, the HHC rate has not increased greatly, which may be related to the shortage of medical materials and poor working environment, the health care providers probably already did the maximum. |
| Anguraj 2021 | Pondicherry, South India | Before-after study | Nov,2020-Apr,2021 | Auditing HH and providing timely feedback significantly improved HHC from 26.7% in November 2020 to 68.4% in April 2021. |
According to the information in the literature, 2377 health care providers were included in the study. A total 1360 of nurses participated in the study, which was the main observation population accounting for 57.21%, followed by 833 doctors (35.04%) and 184 other health care providers (7.74%). Five studies were performed in designated COVID-19 hospitals or wards.26 , 28 , 32 , 33 , 35 Most of the studies (6/10) took the hospital as the whole unit to conduct the overall study.29, 30, 31, 32, 33, 34 Among all the health care providers included, 64 (48.85%) worked in ICU, accounting for the vast majority, followed by 46 (35.11%) in surgery and 21 (16.03%) in internal medicine. A total of 1891664 HH actions and 3591681 HH opportunities were observed in 10 studies. For the observation method of HHC, the researchers adopted the secret observation method (3 groups),26 , 29 , 32 open observation method (6 groups),26 , 27 , 31 , 33, 34, 35 mixed secret and open observation method (one group),28 and automated monitoring system (one group)30 separately. Six studies reported the HHC rate of different occupations26 , 29 , 30 , 33, 34, 35, 6 studies reported the HHC rate at different WHO 5 HH opportunities,26 , 29, 30, 31 , 33 , 35 and all 10 studies reported different observation methods of HH26, 27, 28, 29, 30, 31, 32, 33, 34, 35 (Table 2 ).
Table 2.
Social demographic characteristics of health care providers
| Study | No. of health care providers | Occupation (Doctor/Nurse/Other#) | Working department | Observation method | HHC rate (HH actions/opportunities) | SE | Subgroup |
|---|---|---|---|---|---|---|---|
| Du Miao,a 2020* | 34 | 5/25/4 | ICU | Secretly | 0.71450 (468/655) | 0.01765 | ①②③ |
| Du Miao,b 2020 | 34 | 5/25/4 | ICU | Openly | 0.86156 (641/744) | 0.01266 | |
| Zhang Xuan 2020 | 100 | 0/100/0 | ICU: 30; Surgery: 46; Internal:21; Other: 3 |
Openly | 0.81405 (788/968) | 0.01251 | ③ |
| Zhang Xiangxiang 2020* | 1189 | 427/603/159 | Fever clinic | Secretly + Openly |
0.90524 (7604/8400) | 0.00320 | ①②③ |
| Liu Sidi 2020 | NA | NA | One tertiary A-level hospital | Secretly | 0.84161(28751/34162) | 0.00198 | ①②③ |
| Moore 2021 | NA | NA | Nine hospitals | Automated monitoring | 0.48477 (1044060/2153702) | 0.00034 | ③ |
| Derksen 2020 | 115 | 44/50/21 | Two obstetric university hospitals | Openly | 0.57989 (801707/1382512) | 0.00042 | ②③ |
| Zhou Qian 2020* | NA | NA | One tertiary A-level hospital | Secretly | 0.47297 (70/148) | 0.04104 | ③ |
| Zhao Tingting 2021* | 939 | 357/582/0 | 45 clinical departments | Openly | 0.81142 (3580/4412) | 0.00589 | ①②③ |
| Ragusa 2021 | NA | NA | NA | Openly | 0.66015 (2092/3169) | 0.00841 | ①③ |
| Anguraj 2021* | NA | NA | COVID ICUs | Openly | 0.65323 (1458/2232) | 0.01007 | ①②③ |
Note:
Designated hospital/ward for COVID-19.
Other occupations include medical interns, regular training students, hospital cleaners, logistics personnel, etc.
①Subgroup for different occupations; ②Subgroup for WHO five moments of HH; ③Subgroup for differential observation methods.
Risk of bias
As the extracted information was not affected by the intervention factors, the Newcastle-Ottawa quality assessment scale was used to evaluate the quality of the literature. Consequently, only 1 of 10 studies (10%) had a moderate risk of bias and 9 (90%) had a low moderate risk of bias (Supplementary Table 1).
Meta-analysis outcome
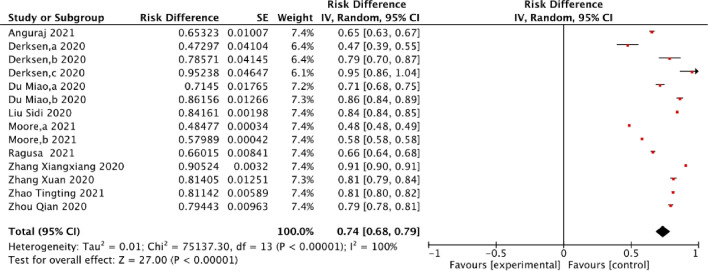
More than 2 subgroups were observed in 5 studies,26 , 30 , 31 , 33 , 35 and finally 16 subgroups were included in the meta-analysis. The overall compliance rate of HH was 74% (I 2=100%, P < .0001; 95% CI: 68%-79%). The highest and lowest HH compliance reports were 95% and 47%, respectively, which were all from the subgroup data of 3 COVID-19 pandemic periods in Germany.26 Of the data, 60% reported that HHC was higher than 80%26, 27, 28, 29 , 31 , 33 (Fig 2 ). Overall, the HHC of the health care providers were at a high level during the COVID-19 pandemic.
Fig 2.
Forest plot of HHC of health care providers during COVID-19 pandemic.
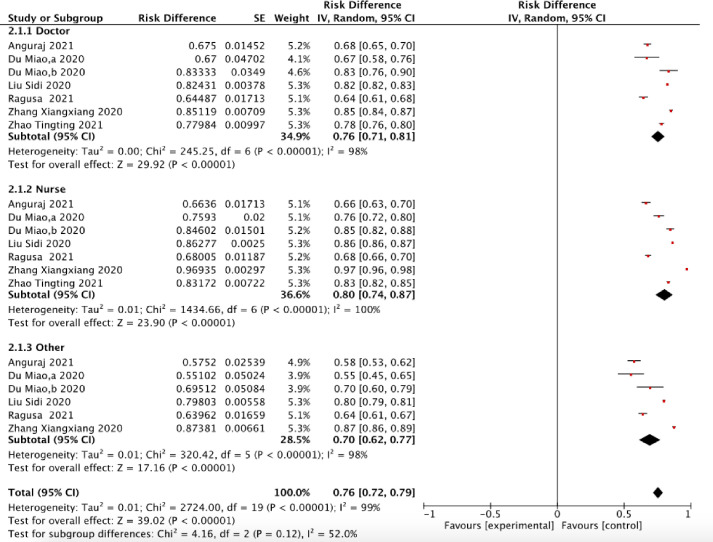
Seven groups of studies reported the HH of health care providers for different occupations.26 , 29 , 30 , 33, 34, 35 The overall HHC was 76% (I 2 = 100%, P < .0001, 95% CI: 72%-79%). As shown in Figure 3 , nurses had the highest HHC (80%; 95% CI: 74%-87%), followed by doctors (76%; 95% CI: 71%-81%), and the lowest was for other staff (70%; 95% CI: 62%-77%). Among the other staff, the reported lowest HHC was only 55%.26 The HHC of nurses was 10% higher than that of other staff. There was a gap in the HHC of different occupations in the hospital, so the education of HHC should be strengthened for auxiliary workers in the hospital.
Fig 3.
Forest plot of HHC of health care providers among different occupations during COVID-19 pandemic.
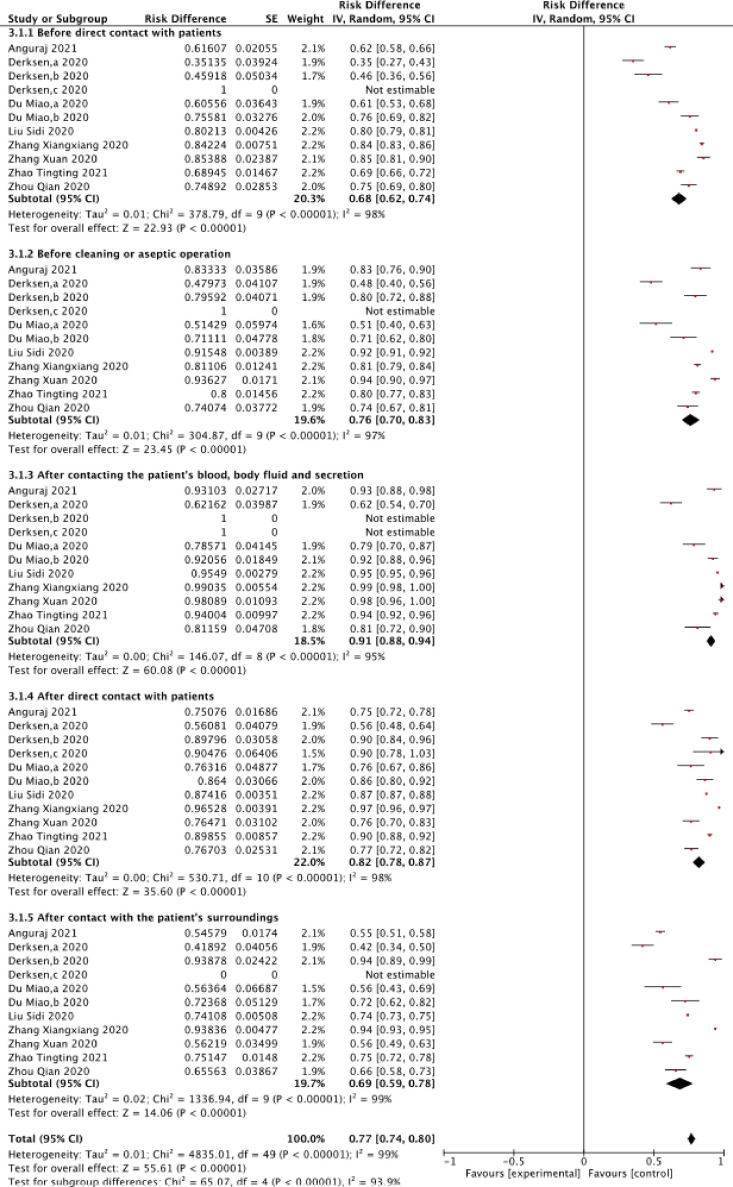
Twelve groups reported the HH at 5 different opportunities and the overall compliance was 77% (I 2=99%, P<0.0001, 95% CI: 74%-80%).26 , 29, 30, 31 , 33 , 35 According to different HH opportunities, the compliance rate of HH ranged from 68% to 91%. Figure 4 shows that health care providers had the highest HHC of the opportunity “after contact with body fluids of the patients” (91%; 95% CI: 88%-94%). Among the 5 opportunities, “before contacting the patients” have the lowest HHC (68%; 95% CI: 62%-74%). The HHC of “before contacting patients” reported in twelve groups ranged from 35% to 85%, and that of “after contacting the patient's surroundings” ranged from 42% to 94%. On the whole, health care providers paid more attention to HH opportunity “after contacting the patient's body fluid or blood”, but paid less attention to HH opportunity “before contacting the patient.”
Fig 4.
Forest plot of HHC of health care providers among different washing opportunities during COVID-19 pandemic.
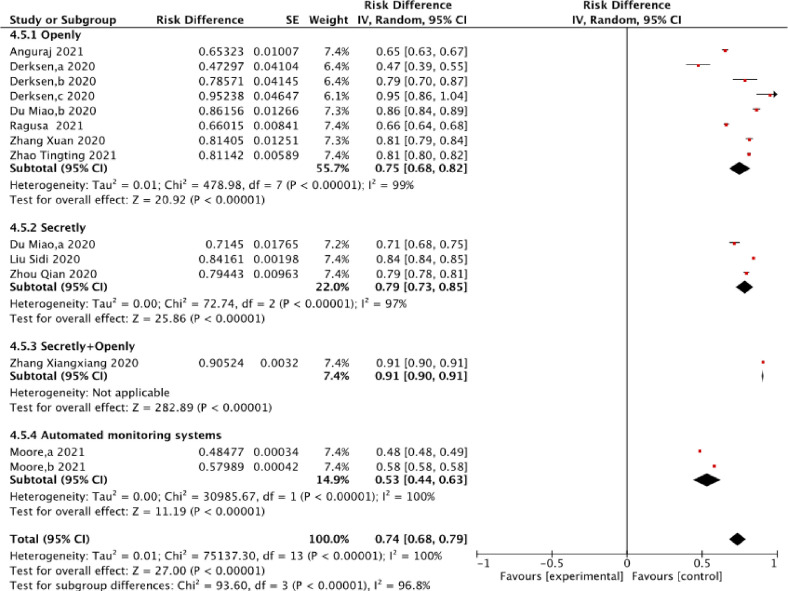
For the different HH monitoring methods, the HHC rate ranged from 53% to 91%, with significant heterogeneity (I 2 = 100%, P < .0001, 95% CI: 68%-79%).26, 27, 28, 29, 30, 31, 32, 33, 34, 35 The highest compliance rate of HH was 91% (95% CI: 90%-91%), with open monitoring combined with anonymous monitoring, and the lowest compliance rate was 53% (95% CI: 44%-63%) using an automatic monitoring system. Under the automatic monitoring system, the compliance of the HH was lower than 60% (Fig 5 ).30 The HHC of open monitoring combined with anonymous monitoring was 41.8% higher than that of anonymous monitoring. There was a gap in the compliance of the HH under different monitoring conditions.
Fig 5.
Forest plot of HHC rate of health care providers among different observation methods during COVID-19 pandemic.
Sensitivity analysis
After deleting the included studies 1 by 1, no significant changes in the effect value and confidence interval were found in the overall HHC rate and HHC in different occupations, hand washing moments, and observation methods, indicating that the results were relatively stable.
Publication bias
A funnel plot was performed to evaluate the potential publication bias of the 4 outcome indicators, including the overall HHC, HHC in occupation, hand washing moments, and observation methods. It can be seen that the distribution of each study was basically symmetrical, suggesting that the possibility of publication bias was small (Supplementary Fig 2-5).
Discussion
During the COVID-19 pandemic, the compliance of HH among health care providers showed a significant increase compared with the situation before the outbreak. The HHC reported by the WHO, previous meta-analyses, and other research systems before COVID-19 was 5%-89%, and levels of HHC for high-income countries rarely exceed 70%.36 Among the studies included in this paper, a total of 6 studies researched the health care providers’ HHC rate changes before and after the pandemic, including 2 cross-sectional surveys28 , 29 and 4 time before-after studies.30 , 31 , 33 , 34 Zhang Xiangxiang28 found that during the non-COVID period from June 1, 2019 to November 30, 2019, the HHC rate of health care providers in the fever clinic was 70.67%, while during COVID-19, HHC rates increased to 90.52%. Liu Sidi29 found that from 2016 to 2019, the HHC rate of health care providers in a grade A class 3 hospital increased year by year, 71.65% in 2016, 73.27% in 2017, 75.94% in 2018 and 77.04% in 2019, while from January to August 2020, the compliance rates increased significantly to 84.16%. For the changes of HHC before and after the COVID of health care providers, Moore,30 Derksen,31 Zhao Tingting33 and Ragusa34 reported that the HHC increased from 46% to 56%, 47% to 100%, 76% to 81%, and 62% to 66% before and after the pandemic, respectively.
Moreover, 5 meta-analyses of HHC before COVID-19 were included. All the 5 literatures were comparative analysis focused on before and after HH intervention. The lowest HHC before intervention was 29%, and the highest HHC reported after intervention was 80.1% (sTable 2). The research on HHC before the pandemic paid close attention on the exploration of intervention measures.37, 38, 39, 40, 41 The main intervention measures included information monitoring, education, training, encouragement, facility provision and so on. However, with the outbreak of COVID-19, medical personnel pay more attention to HH, which may be caused by the improvement of health care providers’ self-protection awareness, the psychological pressure brought by the spread of the pandemic, etc. Consciousness of HH among health care providers were an unprecedented unity during the COVID-19. From the systematic review of this study, the literatures related to HH published during COVID-19 generally lack the research on the precise transmission path of hand as a media. In addition, there was a lack of direct quantitative research that HH caused environmental contamination of SARS-Cov-2 and population infected with COVID-19.
Notably, a series of characteristic changes have taken place in HH behavior among health care providers during the pandemic. Our study found that the concern about HH behavior during the pandemic period was based mainly in fever clinics, ICUs, and designated COVID-19 wards. Before the outbreak, the reporting departments of HHC monitoring were carried out mainly in the ICU or the whole hospital, and targeted less on fever clinics and infectious disease-related departments.42 At present, given that HH needs to be carried out in any diagnosis and treatment situation, the actual implementation is difficult. The results of this study suggest that infectious disease-related diagnosis and treatment departments can be a breakthrough point to improve HHC. Additionally, another change in HHC was observed in the group. This study showed that during the COVID-19 pandemic, the HHC of other auxiliary staff was the lowest, except for doctors and nurses, while a 3-year HH monitoring report conducted in China from 2016 to 2019 showed that doctors were the group with the lowest HHC.29 It showed that while the HHC of doctors had improved greatly after the pandemic, the HH of other auxiliary staff may have been ignored. The observation from Novák indicated that the reasons for decreased compliance with hand washing protocols may have been related to forgetting to wash the hands or not being acquainted with hand washing protocols at all.43 It is generally accepted that the hand of the auxiliary staff, including the cleaning personnel, specimen transfer personnel, and logistics personnel, have carried pathogens and viruses easily.44 The WHO-5 opportunities of HH, showed that the compliance with HH was the lowest for “before contact with patients,” and the highest for “after contact with patients’ body fluids or blood,” which was consistent with the relevant reports of HH before the epidemic. We speculated that obvious visible stains on the hands of health care providers after contacting the body fluids or blood of patients increased the frequency of hand washing.45 The behavior of "before contacting patients" occurs frequently in daily diagnosis, treatment and emergency rescue, which affects the implementation of HH to a certain extent.
It is important to highlight the monitoring mode of the HHC. The literature included in this study was mainly mentioned open monitoring and anonymous monitoring. Only one study has reported the use of an automatic monitoring system for supervising HHC. According to our study, there was significant differences in HHC between manual and automatic monitoring. When we reviewed the literature, we found that there were many kinds of interventions to improve HHC.46 However, it is precisely that the observation and monitoring of HHC itself cannot achieve relative consistency and is affected by whether the monitors are professionally trained, the personal observation bias of the monitors.47, 48, 49 The state of the World's HAND HYGIENE documented that there is also growing interesting in electronic monitoring, focused on the point of care, as reliable systems are developed.50 In addition, the manual monitoring of HH also costs a certain amount of manpower, and it cannot be systematic and sustainable. Therefore, in the future, we will call for more artificial intelligence and AI technology to be used in HH monitoring.
This study had some limitations. The data of areas without reported HHC were not available during the time of the study; therefore, the assessment of HHC during the global pandemic was limited to the reported areas. However, we consider that the limitations of the present study cannot offset the main results of this study. To sum up, this was the first study to comprehensively and systematically analyze the compliance of HH during the pandemic, and compared with the situation before the pandemic. It provided a comprehensive evidence-based basis for us to comprehensively understand the situation of HH during the epidemic.
Conclusion
During the COVID-19 pandemic, the compliance of the health care providers’ HH showed a great improvement. The fever clinics have become the focused departments for monitoring HH. The HHC of auxiliary workers and the opportunity of “before contact with patients” should be strengthened. In the future, it will be necessary to develop standardized HH monitoring tools for practical work.
Footnotes
Funding/support: This work is supported by special fund of Beijing Key Laboratory of Indoor Air Quality Evaluation and Control (No. BZ0344KF20-02).
Conflicts of Interests: None to report.
Author Contributions: LL and YYF contributed to the study concept. WY and YJR drafted the manuscript. Acquisition, analysis, or interpretation of data: All authors. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: All authors. All authors approved the final version of the manuscript.
Ethics approval and consent to participate: Ethical approval or informed consent was not necessary for this meta-analysis because our study has not affected participants directly, and required data were extracted from previous published studies.
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.ajic.2021.11.030.
Appendix. SUPPLEMENTARY MATERIALS
References
- 1.Clancy C, Delungahawatta T, Dunne CP. Hand hygiene-related clinical trials reported between 2014 and 2020: a comprehensive systematic review. J Hosp Infect. 2021;111:6–26. doi: 10.1016/j.jhin.2021.03.007. S0195-6701:00102-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377:228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 3.Liu X, Cui D, Li H, et al. Direct medical burden of antimicrobial-resistant healthcare-associated infections: empirical evidence from China. J Hosp Infect. 2020;105:295–305. doi: 10.1016/j.jhin.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Tchouaket Nguemeleu E, Beogo I, Sia D, et al. Economic analysis of healthcare-associated infection prevention and control interventions in medical and surgical units: systematic review using a discounting approach. J Hosp Infect. 2020;106:134–154. doi: 10.1016/j.jhin.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sickbert-Bennett EE, DiBiase LM, Willis TM, et al. Reduction of healthcare-associated infections by exceeding high compliance with hand hygiene practices. Emerg Infect Dis. 2016;22:1628–1630. doi: 10.3201/eid2209.151440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gon G, Dancer S, Dreibelbis R, et al. Reducing hand recontamination of healthcare workers during COVID-19. Infect Control Hosp Epidemiol. 2020;41:870–871. doi: 10.1017/ice.2020.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh D, Joshi K, Samuel A, et al. Alcohol-based hand sanitisers as first line of defence against SARS-CoV-2: a review of biology, chemistry and formulations. Epidemiol Infect. 2020;148:e229. doi: 10.1017/S0950268820002319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harbourt DE, Haddow AD, Piper AE, et al. Modeling the stability of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on skin, currency, and clothing. PLoS Negl Trop Dis. 2020;14 doi: 10.1371/journal.pntd.0008831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ye G, Lin H, Chen S, et al. Environmental contamination of SARS-CoV-2 in healthcare premises. J Infect. 2020;81:e1–e5. doi: 10.1016/j.jinf.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Feng H, Zhang S, et al. SARS-CoV-2 RNA detection of hospital isolation wards hygiene monitoring during the Coronavirus Disease 2019 outbreak in a Chinese hospital. Int J Infect Dis. 2020;94:103–106. doi: 10.1016/j.ijid.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hegde S. Which type of personal protective equipment (PPE) and which method of donning or doffing PPE carries the least risk of infection for healthcare workers? Evid Based Dent. 2020;21:74–76. doi: 10.1038/s41432-020-0097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okamoto K, Rhee Y, Schoeny M, et al. Impact of doffing errors on healthcare worker self-contamination when caring for patients on contact precautions. Infect Control Hosp Epidemiol. 2019;40:559–565. doi: 10.1017/ice.2019.33. [DOI] [PubMed] [Google Scholar]
- 13.Sagar M, Sharma S, Chaudhary A, et al. A mixed-method study to assess the knowledge-practice gap regarding hand hygiene among healthcare providers in a tertiary care hospital. J Anaesthesiol Clin Pharmacol. 2020;36:359–365. doi: 10.4103/joacp.JOACP_331_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mortell M. Hand hygiene compliance: is there a theory-practice-ethics gap? Br J Nurs. 2012;21:1011–1014. doi: 10.12968/bjon.2012.21.17.1011. [DOI] [PubMed] [Google Scholar]
- 15.Labrague LJ, McEnroe-Petitte DM, van de Mortel T, et al. A systematic review on hand hygiene knowledge and compliance in student nurses. Int Nurs Rev. 2018;65:336–348. doi: 10.1111/inr.12410. [DOI] [PubMed] [Google Scholar]
- 16.Sadule-Rios N, Aguilera G. Nurses' perceptions of reasons for persistent low rates in hand hygiene compliance. Intensive Crit Care Nurs. 2017;42:17–21. doi: 10.1016/j.iccn.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Sands M, Aunger R. Determinants of hand hygiene compliance among nurses in US hospitals: a formative research study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0230573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ataiyero Y, Dyson J, Graham M. Barriers to hand hygiene practices among health care workers in sub-Saharan African countries: a narrative review. Am J Infect Control. 2019;47:565–573. doi: 10.1016/j.ajic.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Santosaningsih D, Erikawati D, Santoso S, et al. Intervening with healthcare workers' hand hygiene compliance, knowledge, and perception in a limited-resource hospital in Indonesia: a randomized controlled trial study. Antimicrob Resist Infect Control. 2017;6:23. doi: 10.1186/s13756-017-0179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang F, Armando M, Dufau S, et al. COVID-19 outbreak and healthcare worker behavioural change toward hand hygiene practices. J Hosp Infect. 2021;111:27–34. doi: 10.1016/j.jhin.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bani-Issa WA, Al Nusair H, Altamimi A, et al. Self-report assessment of nurses' risk for infection after exposure to patients with coronavirus disease (COVID-19) in the United Arab Emirates. J Nurs Scholarsh. 2021;53:171–179. doi: 10.1111/jnu.12625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Modi PD, Nair G, Uppe A, et al. COVID-19 awareness among healthcare students and professionals in mumbai metropolitan region: a questionnaire-based survey. Cureus. 2020;12:e7514. doi: 10.7759/cureus.7514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Liberati A, Tetzlaff J, et al. The PRISMA Group (2009) preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 24.World Health Organization . 2009. WHO guidelines on hand hygiene in health care: a summary. Geneva.https://apps.who.int/iris/handle/10665/70126?show=full AAvailable at. Accessed May 23, 2021. [Google Scholar]
- 25.Chen YH, Du L, Geng XY, et al. Implementation of meta-analysis of non-controlled binary data in Revman software. Chin J Evid Based Med. 2014;14:889–896. [Google Scholar]
- 26.Du M. Effect of Hawthorne effect on improving hand hygiene compliance of ICU medical staff during New Coronavirus pneumonia outbreak. Integrat Tradition Chin West Med Nurs. 2020;6:327–329. [Google Scholar]
- 27.Zhang X, Zhang CL, Jiang M, et al. Novel coronavirus pneumonia clinical compliance among nurses in the first line of care. Qilu J Nurs. 2020;26:56–58. [Google Scholar]
- 28.Zhang XX, Chen KY, Su JJ, et al. Novel coronavirus pneumonia before and after the outbreak of a fever outpatient clinic medical staff compliance analysis of hand hygiene. Chin J Disinfect. 2020;37:690–692. [Google Scholar]
- 29.Liu SD, Huang X, Li CH, et al. Investigation on hand hygiene compliance of medical staff in a tertiary hospital from 2016 to 2020. Chin J Nosocom Infect. 2020;30:3823–3827. [Google Scholar]
- 30.Moore LD, Robbins G, Quinn J, et al. The impact of COVID-19 pandemic on hand hygiene performance in hospitals. Am J Infect Contro.l. 2021;49:30–33. doi: 10.1016/j.ajic.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Derksen C, Keller FM, Lippke S. Obstetric healthcare workers' adherence to hand hygiene recommendations during the COVID-19 pandemic: observations and social-cognitive determinants. Appl Psychol Health Well Being. 2020;12:1286–1305. doi: 10.1111/aphw.12240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou Q, Lai X, Zhang X, et al. Compliance measurement and observed influencing factors of hand hygiene based on COVID-19 guidelines in China. Am J Infect Control. 2020;48:1074–1079. doi: 10.1016/j.ajic.2020.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao TT, Zhao HY, Wang J, et al. Hand hygiene compliance investigation and analysis before and after COVID-19 in a third-class A hospital. Chin J Disinfect. 2021;38:589–591. [Google Scholar]
- 34.Ragusa R, Marranzano M, Lombardo A, et al. Has the COVID 19 virus changed adherence to hand washing among healthcare workers? Behav Sci (Basel) 2021;11:53. doi: 10.3390/bs11040053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Anguraj S, Ketan P, Sivaradjy M, et al. The effect of hand hygiene audit in COVID intensive care units in a tertiary care hospital in South India. Am J Infect Control. 2021;49:1247–1251. doi: 10.1016/j.ajic.2021.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. WHO guidelines on Key facts and figures on World Hand Hygiene Day 2021. Geneva, 2021. Available at: https://www.who.int/campaigns/world-hand-hygiene-day/2021/key-facts-and-figures. Accessed May 23, 2021.
- 37.Ofek Shlomai N, Rao S, Patole S. Efficacy of interventions to improve hand hygiene compliance in neonatal units: a systematic review and meta-analysis. Eur J Clin Microbiol Infect Dis. 2015;34:887–897. doi: 10.1007/s10096-015-2313-1. [DOI] [PubMed] [Google Scholar]
- 38.Luangasanatip N, Hongsuwan M, Limmathurotsakul D, et al. Comparative efficacy of interventions to promote hand hygiene in hospital: systematic review and network meta-analysis. BMJ. 2015;351:h3728. doi: 10.1136/bmj.h3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alshehari AA, Park S, Rashid H. Strategies to improve hand hygiene compliance among healthcare workers in adult intensive care units: a mini systematic review. J Hosp Infect. 2018;100:152–158. doi: 10.1016/j.jhin.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 40.Martos-Cabrera MB, Mota-Romero E, Martos-García R, et al. Hand hHygiene teaching strategies among nursing staff: a systematic review. Int J Environ Res Public Health. 2019;16:3039. doi: 10.3390/ijerph16173039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin TY, Lin CT, Chen KM, et al. Information technology on hand hygiene compliance among health care professionals: a systematic review and meta-analysis. J Nurs Manag. 2021 doi: 10.1111/jonm.13316. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 42.Lambe KA, Lydon S, Madden C, et al. Hand hygiene compliance in the ICU: a systematic review. Crit Care Med. 2019;47:1251–1257. doi: 10.1097/CCM.0000000000003868. [DOI] [PubMed] [Google Scholar]
- 43.Novák M, Breznický J, Kompaníková J, et al. Impact of hand hygiene knowledge on the hand hygiene compliance. Med Glas (Zenica) 2020;17:194–199. doi: 10.17392/1051-20. [DOI] [PubMed] [Google Scholar]
- 44.Arias AV, Garcell HG, Ochoa YR, et al. Assessment of hand hygiene techniques using the World Health Organization's six steps. J Infect Public Health. 2016;9:366–369. doi: 10.1016/j.jiph.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 45.Sax H, Allegranzi B, Uçkay I, et al. My five moments for hand hygiene': a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67:9–21. doi: 10.1016/j.jhin.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 46.Kingston L, O'Connell NH, Dunne CP. Hand hygiene-related clinical trials reported since 2010: a systematic review. J Hosp Infect. 2016;92:309–320. doi: 10.1016/j.jhin.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 47.Brotfain E, Livshiz-Riven I, Gushansky A, et al. Monitoring the hand hygiene compliance of health care workers in a general intensive care unit: use of continuous closed circle television versus overt observation. Am J Infect Control. 2017;45:849–854. doi: 10.1016/j.ajic.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 48.Cheng VC, Tai JW, Ho SK, et al. Introduction of an electronic monitoring system for monitoring compliance with Moments 1 and 4 of the WHO "My 5 Moments for Hand Hygiene" methodology. BMC Infect Dis. 2011;11:151. doi: 10.1186/1471-2334-11-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clancy C, Delungahawatta T, Dunne CP. Hand-hygiene-related clinical trials reported between 2014 and 2020: a comprehensive systematic review. J Hosp Infect. 2021;111:6–26. doi: 10.1016/j.jhin.2021.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.World Health Organization. State of the world's hand hygiene, 2021.Geneva, 2021. Available at: https://www.who.int/publications/i/item/9789240036444. Accessed October 15, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.