Approximately half of the patients admitted to intensive care units (ICUs) experience moderate to severe pain during their stay [1]. Regional analgesia has been underused in ICUs despite the well-known importance of pain control in admitted patients and the available evidence on its efficacy and good safety profile. A review of regional analgesia techniques for pain management in patients admitted to the ICU has recently been published [2].
Critical trauma patients generally have several injuries that cause severe pain; some blocks have been studied in this subset of patients [3], but this is the first case report of ultrasound-guided infiltration of the lateral femoral cutaneous nerve (LFCN) in a critical care patient.
Meralgia paresthetica is an entrapment neuropathy of the LFCN, characterized by paresthesia and numbness on the anterolateral side of the thigh. It has also been described in an avulsion fracture of the anterior superior iliac spine [4] and recently in two prone-positioned patients to treat COVID-19-associated acute respiratory distress syndrome [5].
We present a 57-year-old male patient who was transferred to the emergency department of the University General Hospital of Valencia after suffering a crush while working, having been trapped by a truck. After a physical examination and computed tomography scan, a pelvic fracture, bladder injury, and perisplenic hematoma were observed, probably related to a contained subcapsular rupture of the spleen. Initially, an exploratory laparotomy was performed, 4 L of blood was evacuated, and splenectomy was performed. In addition, a tear of the sigmoid mesocolon was observed with bruising and active bleeding, and resection was performed. A massive transfusion of blood products was performed, and the patient was transferred to the ICU. In the second half of the next day, another intervention by the traumatology team was performed to treat the pelvic fracture (the left iliac fracture reaching the ipsilateral sacroiliac joint with a diastasis of the same, multiple sacral fractures with the involvement of the right sacroiliac joint, the comminuted fracture of the left ischiopubic and iliopubic branches that extend to the ipsilateral acetabulum). An Orthofix® (ORTHOFIX Srl, Italy) fixator was placed, and it was removed after the fracture had healed 56 days later. Admission to the ICU was prolonged, remaining sedated during the moments of greatest instability, and later, the patient was weaned from the ventilator, followed by progressive rehabilitation. During the last phase of admission, the patient reported severe pain with a numerical rating scale (NRS) of 8–9 that worsened with mobilization. The pain remained severe despite the treatment regimen with continuous infusion of oxycodone 8 mg/h, fentanyl 75 µg/h in patch, pregabalin 75 mg/12 h, and acetaminophen 1 g/8 h. On examination, the patient expressed localized pain on the outer face of the right thigh, from the iliac crest to the middle third of the thigh. The main suspicion was the lesion of the LFCN during the surgery for the placement and removal of the pelvic fixator (Fig. 1A). The radiograph shows the pelvic fixator placed on the patient (Fig. 1B).
Fig. 1.
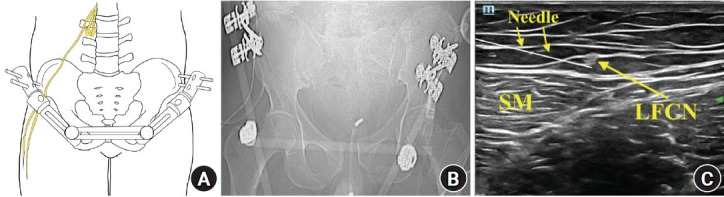
(A) Representation of the lateral femoral cutaneous nerve (LFCN) in relation to the pelvic fixator. (B) X-ray with the pelvic fixator placed on the patient. (C) Ultrasound-guided infiltration of the LFCN. SM: sartorius muscle.
The ultrasound-guided infiltration of the right femoral cutaneous nerve was performed (Fig. 1C). Levo-bupivacaine 0.5% 10 mL and triamcinolone 40 mg were administered. One hour after the blockade, the patient presented an improvement of pain > 75%, shifting from NRS 9 to NRS 2. This improvement allowed the reduction of oxycodone from 8 to 6 mg/h at 1 h post-block, from 6 to 3 mg/h at 3 h post-block, from 3 to 1 mg/h at 6 h post-block, and then its final withdrawal 1 day later. The patient had stable pain relief, with an NRS score of 3 at 48 h after the LFCN block. The technique was repeated for four consecutive days. One week later, the patient’s NRS score remained at 3. Pain control during the period between the blockade and discharge from the ICU kept the patient comfortable and helped to avoid the administration of high-dose opioids.
Ultrasound-guided regional analgesia techniques must be incorporated in the ICU care portfolio for the daily practice of anesthesiologists and intensive care physicians. They provide excellent pain control in several situations where high opioid doses are necessary, avoiding the side effects and dependence phenomena associated with opioids.
Footnotes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Pablo Kot (Conceptualization; Writing – original draft)
Ruben Rubio-Haro (Writing – original draft)
Clara Bordes-García (Resources)
Carolina Ferrer-Gómez (Supervision; Validation)
Jose De Andrés (Supervision)
References
- 1.Stanik-Hutt JA, Soeken KL, Belcher AE, Fontaine DK, Gift AG. Pain experiences of traumatically injured patients in a critical care setting. Am J Crit Care. 2001;10:252–9. [PubMed] [Google Scholar]
- 2.Rubio-Haro R, Morales-Sarabia J, Ferrer-Gomez C, De Andres J. Regional analgesia techniques for pain management in patients admitted to the intensive care unit. Minerva Anestesiol. 2019;85:1118–28. doi: 10.23736/S0375-9393.19.13447-5. [DOI] [PubMed] [Google Scholar]
- 3.Wiebalck A, Grau T. Ultrasound imaging techniques for regional blocks in intensive care patients. Crit Care Med. 2007;35(5 Suppl):S268–74. doi: 10.1097/01.CCM.0000260676.90475.00. [DOI] [PubMed] [Google Scholar]
- 4.Hayashi S, Nishiyama T, Fujishiro T, Kanzaki N, Kurosaka M. Avulsion-fracture of the anterior superior iliac spine with meralgia paresthetica: a case report. J Orthop Surg (Hong Kong) 2011;19:384–5. doi: 10.1177/230949901101900327. [DOI] [PubMed] [Google Scholar]
- 5.Bellinghausen AL, LaBuzetta JN, Chu F, Novelli F, Rodelo AR, Owens RL. Lessons from an ICU recovery clinic: two cases of meralgia paresthetica after prone positioning to treat COVID-19-associated ARDS and modification of unit practices. Crit Care. 2020;24:580. doi: 10.1186/s13054-020-03289-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


